Abstract
The socioecological framework is a multilevel conceptualization of health that includes intrapersonal, interpersonal, organizational, environmental, and public policy factors. The socioecological framework emphasizes multiple levels of influence and supports the idea that behaviors both affect and are affected by various contexts. At present, the sports medicine community's understanding and application of the socioecological framework are limited. In this article, we use the socioecological framework to describe potential avenues for interventions to reduce sport-related deaths among adolescent participants.
Keywords: intervention adoption, health behavior, sudden death
Sport participation has many potential benefits, such as improved physical fitness and overall health status.1 However, it also introduces the risk of injury and, in rare circumstances, death. Approximately 800 cases of sport-related death were documented between 1982 and 2013 in the United States, with the majority occurring at the high school level.2 Although it is difficult to say how many of these could have been prevented, well-designed interventions are critical for reducing sport-related deaths. For other conditions,3–5 those interventions that considered numerous levels of influence—from the at-risk individual to the overarching policy at the local, state, or national level—tended to have the greatest effect in addressing the adverse outcomes of interest. As a result, effective prevention strategies for reducing mortality in sports may benefit from identification of the relevant level(s) at which intervention is needed while integrating existing evidence and behavioral theory.6
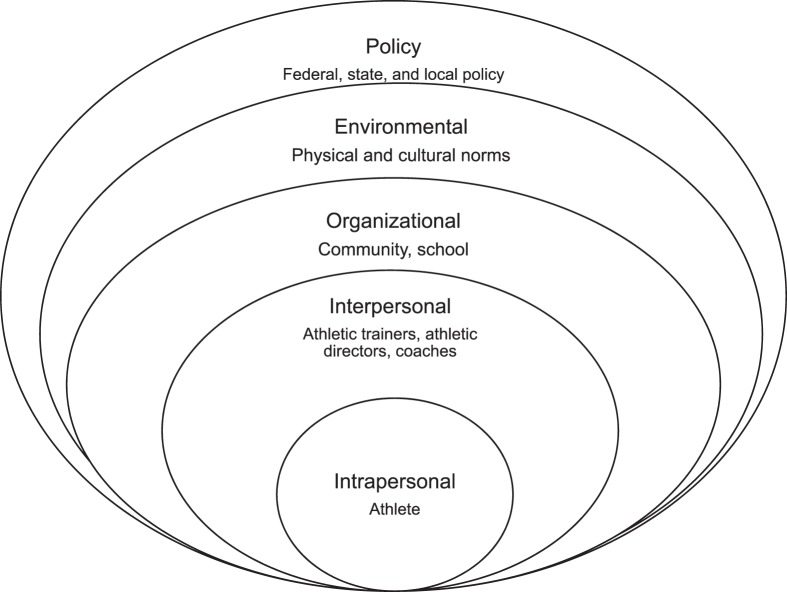
The public health literature has often focused on theories, frameworks, and models to facilitate the adoption of interventions for traditional public health concerns (eg, alcohol abuse, food safety, human immunodeficiency virus, heart disease). However, these models have typically not been applied to the sports medicine realm.7,8 We propose that the socioecological framework be used as a guide for organizing and summarizing the evidence concerning various risk factors associated with sport-related death and determinants of potentially promising interventions.9,10 The socioecological framework was first suggested by Broffenbrenner11 in the 1970s as an ecological systems theory and was later redefined by McLeroy et al9 as a framework to promote health-related behavioral change. The framework typically includes 5 levels of influence: (1) intrapersonal (eg, individual, athlete), (2) interpersonal (eg, athletic trainer [AT], coach, parent, athletic director), (3) organizational (eg, community, school), (4) environmental (eg, cultural norms, physical environment), and (5) policy (eg, state high school association, local, state, federal legislation; Figure). Despite the utility of the socioecological framework as a possible foundation for critically assessing and using the range of factors associated with sport-related injury, it has not frequently been applied to adoption strategies for sports medicine interventions.
Figure.
The 5 levels of the socioecological framework.
To date, we identified only 3 published articles7,8,12 that systematically applied the socioecological framework to a sports medicine topic. Failing to use a structure to organize and apply the evidence on sport-related death for end users prevents a systematic approach to improving interventions and promoting the adoption of best practices. The purpose of our article was to highlight the ways that secondary school ATs can use knowledge of the socioecological framework to improve the adoption of interventions to reduce sport-related deaths. As an example in this short report, we use exertional heat stroke (EHS) prevention, recognition, and management. However, the socioecological model can and should be applied to preventing all potential causes of sport-related death (Table).
Table.
Examples of the Socioecological Framework Within Individual Factors Associated With Sport-Related Death
| Intrapersonal |
Interpersonal |
Organizational |
Environmental |
Policy |
|
| Sudden cardiac arrest (SCA) | Cardiovascular screening allowed for knowledge of athlete status and potential for SCA13 | Approximately 59% of states required cardiopulmonary resuscitation/first-aid training of all coaches14 | School-based automated external defibrillator programs resulted in high survival rate for SCAs on campus15 | Access to and application of automated external defibrillator within 3 minutes demonstrated survival rates of up to 90%16 | 71% of states did not require schools to have an emergency action plan14 |
| Exertional heat stroke (EHS) | Low physical fitness level, sleep deprivation, body weight, dehydration, inadequate water intake increased risk for EHS17 | Coaches lacked knowledge on general EHS; fewer than 20% of athletic trainers obtained body temperature to diagnose EHS18 | a | Rate of exertional heat illness increased when the environmental conditions measured by wet- bulb globe temperature > 82°F19 | 35% of states mandated comprehensive heat-acclimatization protocol14 |
| Traumatic head injuries | Head contact, high sticking, elbowing, athlete knowledge associated with disclosure20 | Team, coach-athlete, parent-athlete interactions affected concussion reporting21 | Despite 100% of states mandating a concussion policy, school district compliance was 30%–100%22 | Properly fitted equipment23,24 | 100% of states required some form of a concussion policy; however, a majority of states did not require a comprehensive concussion policy14 |
| Exertional collapse associated with sickle cell trait | Despite mandatory screening and disclosure of sickle cell trait at birth, 52% of young African-American adults were uncertain about their status25 | a | a | a | a |
| Spinal cord injuries | Athlete knowledge of proper tackling technique26 | a | a | a | a |
| Asthma | Known history of asthma status allowed preventive measures to reduce triggers27 | a | a | a | Limited policy adoption at federal, state, or local level27 |
| Anaphylaxis | Known history of allergies allowed for access to quick-acting epinephrine28 | a | a | a | a |
| Traumatic internal injuries | a | a | a | a | |
| Lightning | a | a | “When thunder roars, go indoors!”29 | a | |
| Diabetes | Lack of adherence to diabetes management plan30 | a | a | a | a |
Indicates a gap in the literature.
Intrapersonal Level
The intrapersonal level of the socioecological framework considers the physical and cognitive characteristics of the athlete as well as his or her prior experiences.9,11 Although this level is based on the at-risk individual, it is strongly influenced by all other levels of the socioecological framework. Physical characteristics include the athlete's sex, age, genetics, and previous medical conditions, among other intrinsic factors. Cognitive characteristics may consist of relevant knowledge and attitude about factors related to sport-related injury and illness, such as risk- and prevention-related behaviors. Factors associated with the intrapersonal level are likely the product of interpersonal interactions and broader sociocultural influences. For example, athlete-specific factors that may place one at increased risk for EHS include a history of heat illness, low level of physical fitness, sleep deprivation, increased body weight, dehydration, and inadequate water intake.17 Therefore, athletes should be knowledgeable about their own risk level for adverse health outcomes to alert those at the interpersonal level who are supervising and providing care to them.
Interpersonal Level
The interpersonal level of the socioecological framework includes the community that surround the athlete and can influence his or her safety, such as ATs, athletic directors, coaches, parents, and fans.9 These external stakeholders influence athlete safety at the interpersonal level through their interactions with at-risk athletes. For example, if a coach believes that a lack of water intake indicates physical and mental toughness, the athlete may be placed at increased risk of EHS solely because of that coach's attitudes and resulting behaviors. In addition, athletes' attitudes and behaviors can be affected by external stakeholders. The theory of normative social behavior proposes that descriptive norms (ie, perceptions about what other people do) are controlled by injunctive norms (ie, perceptions about what you are expected to do) as well as the expectations of anticipated outcomes.31,32 Such behavioral norms have been discussed in the context of other injuries, such as concussion: athletes' willingness to report a concussion may be affected by the thoughts, attitudes, and perceptions of those around them who influence their decisions.21 In contrast, the EHS literature offers little discussion of how stakeholders may affect athletes' intentions to disclose EHS-related symptoms. Factors that impede these intentions must be addressed, as EHS requires immediate care to reduce its severity.17
The comfort and skill level of an AT may also influence the level of care an athlete receives for an injury. Mazerolle et al18 found that fewer than 20% of ATs described rectal thermometry as their standard method of diagnosing EHS, demonstrating a low level of compliance with best practices. Therefore, barriers, whether perceived or actual, that inhibit ATs' use of best practices may directly influence whether an athlete is likely to survive a catastrophic event. Designing interventions to address multiple stakeholders, rather than only the athletes, is imperative to improving the effectiveness of interventions.21
Organizational Factors
The organizational level considers the structured communities to which groups of individuals belong, such as a school or other sport institution.9 For the purpose of this article, the organizational level is the secondary school itself, as the entity that oversees and thus directly affects the at-risk athletes. Formal guidelines, such as written procedures, or informal guidelines, such as environmental culture, influence the behavior of these organizations.9,11 Both formal and informal policies and procedures help shape cultural norms within these organizations and establish expectations about the consequences of engaging in specific behaviors.9,11 This in turn influences individual behavior and interpersonal interactions. For example, fire drills, active-shooter drills, and bomb-threat drills, along with various other precautions taken in high schools, directly reflect policy mandates and current perceptions of safety in educational environments. The same policy mandates for school safety may extend to school athletics, potentially influencing stakeholders to adopt sport-safety standards to reduce the risk of sport-related death. However, although policy mandates may occur at the higher levels of influence, such as via state or national legislation, an individual organization may not “buy in” to such mandates. For example, if a state high school athletics association sets a mandate for a heat policy, but no specific guidelines are given, a school could choose to not comply with the mandate, to not implement the created policy, or to create or implement a policy that does not follow best practices.
Environmental Factors
The environmental level can be described as the broader context surrounding an athlete, including the cultural and physical environments.11 In the context of this article, the environmental level refers to the social, cultural, and physical environments. Cultural values or norms refer to perceived standards of acceptable attitudes and behaviors within networks. For example, wrestling athletes may believe that competing in a dehydrated state is part of the sport and may not recognize the health risk this poses to them. Education and advocacy efforts have been used to attempt to change this perception, and although the effects have been largely positive, unsafe cultural norms reflecting incorrect information persist in some settings.33
When the socioecological framework was redefined by McLeroy et al9 in 1988, the environmental level also included the physical environment, such as access to parks and transportation. In sports medicine, the environmental level may also refer to the actual environmental and playing-field conditions, and interventions can be designed to directly address these factors (eg, cancel activity during extreme weather, ensure playing conditions are safe). For example, as wet-bulb globe temperature increases, the risk for EHS seems to increase.19 By knowing the best practice for handling an environmental hazard, ATs at the interpersonal level must use the supported evidence to protect their athletes from unsafe situations. It should be noted that subjective appraisals of the threat of environmental hazards may influence individuals' behavior, even when they are highly motivated to follow the best-known precautions (eg, false sense of security).9,34
Policy Factors
Finally, policies construct the outermost layer of the framework. Policies are enacted to safeguard athletes and can be developed through the state high school association or state or national legislation. Theoretically, policies should aid in improving the adoption and implementation of the best practices required to reduce the risk of sport-related fatalities. For effective policy implementation, all levels of the socioecological framework should be considered in an adoption and implementation strategy. Policies may also be used to directly set practice standards. Policies for preventing or managing catastrophic injuries, such as emergency action plan preparedness or heat acclimatization for the prevention of EHS, are lacking across the nation. Seventy-one percent of states did not require high schools to have an emergency action plan, and only 8 states met the minimum best practice guidelines for heat acclimatization policies.14 The lack of uniform mandates regarding safety in sports at the state or federal level leaves athletes vulnerable to preventable catastrophic injuries and fatalities. Using a top-down approach in the socioecological framework, secondary school ATs can influence change at the policy level in 2 ways. First, they can ensure that their own school setting is adopting the best practices for preventing sport-related deaths. Second, schools can become involved with state and national initiatives to assist other, nonmedical personnel (eg, executive directors of state associations) in understanding the importance of policy mandates in preventing sport-related deaths.
Clinical Significance
To design effective interventions that reduce sport-related deaths, it is critical to consider the range of possible influences that may lead to a catastrophic outcome. The socioecological framework can help secondary school ATs target key levels or stakeholders in their own setting to improve the adoption of best practices. Effective interventions are predicated on identifying the level(s) at which intervention is needed and building on existing evidence and behavioral theory while developing them.6 In other conditions,3–5 interventions that address multiple levels of the socioecological framework tend to be more lasting and effective than interventions that address only 1 level. Although previous authors35 suggested that interventions adopted at the policy level tend to influence all levels, we must stress that policy should be implemented in practice, which requires efforts at the individual, interpersonal, organizational, and environmental levels. An example is the evaluation of organizational compliance with concussion policies; despite 100% of states mandating some form of a concussion policy, organizational compliance has ranged from 30% to 100%.22 When considering strategies to increase the adoption of best practices and the implementation of measures to protect athletes, ATs should consider the interplay of all levels of the socioecological framework to improve their clinical decisions and promote athlete safety.
CONCLUSIONS
The prevention of sport-related death may be facilitated by actions at a variety of levels across multiple domains. Through the collaborative and interdisciplinary efforts within sports medicine, we believe the socioecological framework provides a preliminary road map for constructing effective interventions to reduce sport-related deaths.
ACKNOWLEDGMENTS
We thank Michael Norell for his review of this short report.
REFERENCES
- 1.Warburton DER, Nicol CW, Bredin SSD. Health benefits of physical activity: the evidence. CMAJ. 2006;174(6):801–809. doi: 10.1503/cmaj.051351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mueller FO, Kucera KL, Cox MS, Cantu RC. Catastrophic Sports Injury Research Thirty-First Annual Report: Fall 1982—Spring 2013. Vol 31. Chapel Hill: University of North Carolina, National Center for Catastrophic Sport Injury Research; 2015. p. 737. [Google Scholar]
- 3.Kumar S, Quinn SC, Kim KH, Musa D, Hilyard KM, Freimuth VS. The social ecological model as a framework for determinants of 2009 H1N1 influenza vaccine uptake in the United States. Health Educ Behav. 2012;39(2):229–243. doi: 10.1177/1090198111415105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kirby D. Emerging Answers. Research Findings on Programs to Reduce Teen Pregnancy and Sexually Transmitted Diseases. Washington, DC: The National Campaign to Prevent Teen and Unplanned Pregnancy;; 2007. [Google Scholar]
- 5.DiClemente RJ, Salazar LF, Crosby RA. A review of STD/HIV preventive interventions for adolescents: sustaining effects using an ecological approach. J Pediatr Psychol. 2007;32(8):888–906. doi: 10.1093/jpepsy/jsm056. [DOI] [PubMed] [Google Scholar]
- 6.Heffernan CJ. Review of: Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory Englewood Cliffs, NJ: Prentice Hall; 1986 Behav Change. 1988;5(1):37–38. reviewer. [Google Scholar]
- 7.Kerr ZY, Register-Mihalik JK, Marshall SW, Evenson KR, Mihalik JP, Guskiewicz KM. Disclosure and non-disclosure of concussion and concussion symptoms in athletes: review and application of the socio-ecological framework. Brain Inj. 2014;28(8):1009–1021. doi: 10.3109/02699052.2014.904049. [DOI] [PubMed] [Google Scholar]
- 8.Register-Mihalik J, Baugh C, Kroshus E, Kerr Z, Valovich McLeod TC. A multifactorial approach to sport-related concussion prevention and education: application of the socioecological framework. J Athl Train. 2017;52(3):195–205. doi: 10.4085/1062-6050-51.12.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McLeroy KR, Bibeau D, Steckler A, Glanz A. An ecological perspective on health promotion programs. Health Educ Q. 1988;15(4):351–377. doi: 10.1177/109019818801500401. [DOI] [PubMed] [Google Scholar]
- 10.Sallis JF, Owen N, Fisher EB. Ecological models of health behavior. In: Glanz K, Rimer BK, Viswanath K, editors. Health Education: Theory, Research, and Practice. San Francisco, CA: Jossey-Bass;; 2008. pp. 23–40. [Google Scholar]
- 11.Bronfenbrenner U. Toward an experimental ecology of human development. Am Psychol. 1977;32(7):513–531. [Google Scholar]
- 12.Register-Mihalik JK, Williams RM, Marshall SW, et al. Demographic, parental, and personal factors influence youth athletes' concussion-related knowledge and beliefs. J Athl Train. 2018;53(8):768–775. doi: 10.4085/1062-6050-223-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Drezner JA, Courson RW, Roberts WO, et al. Inter Association Task Force recommendations on emergency preparedness and management of sudden cardiac arrest in high school and college athletic programs: a consensus statement. Prehosp Emerg Care. 2007;11(3):253–271. doi: 10.1080/10903120701204839. [DOI] [PubMed] [Google Scholar]
- 14.Adams WM, Scarneo SE, Casa DJ. State-level implementation of health and safety policies to prevent sudden death and catastrophic injuries within secondary school athletics. Orthop J Sports Med. 2017;5(9):1–8. doi: 10.1177/2325967117727262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Drezner JA, Toresdahl BG, Rao AL, Huszti E, Harmon KG. Outcomes from sudden cardiac arrest in US high schools: a 2-year prospective study from the National Registry for AED Use in Sports. Br J Sports Med. 2013;47(18):1179–1183. doi: 10.1136/bjsports-2013-092786. [DOI] [PubMed] [Google Scholar]
- 16.Valenzuela TD, Roe DJ, Cretin S, Spaite DW, Larsen MP. Estimating effectiveness of cardiac arrest interventions: a logistic regression survival model. Circulation. 1997;96(10):3308–3313. doi: 10.1161/01.cir.96.10.3308. [DOI] [PubMed] [Google Scholar]
- 17.Rav-Acha M, Hadad E, Epstein Y, Heled Y, Moran DS. Fatal exertional heat stroke: a case series. Am J Med Sci. 2004;328(2):84–87. doi: 10.1097/00000441-200408000-00003. [DOI] [PubMed] [Google Scholar]
- 18.Mazerolle SM, Scruggs IC, Casa DJ, et al. Current knowledge, attitudes, and practices of certified athletic trainers regarding recognition and treatment of exertional heat stroke. J Athl Train. 2010;45(2):170–180. doi: 10.4085/1062-6050-45.2.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cooper ER, Ferrara MS, Casa DJ, et al. Exertional heat illness in American football players: when is the risk greatest? J Athl Train. 2016;51(8):593–600. doi: 10.4085/1062-6050-51.8.08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mihalik JP, Greenwald RM, Blackburn JT, Cantu RC, Marshall SW, Guskiewicz KM. Effect of infraction type on head impact severity in youth ice hockey. Med Sci Sports Exerc. 2010;42(8):1431–1438. doi: 10.1249/MSS.0b013e3181d2521a. [DOI] [PubMed] [Google Scholar]
- 21.Kroshus E, Garnett B, Hawrilenko M, Baugh CM, Calzo JP. Concussion under-reporting and pressure from coaches, teammates, fans, and parents. Soc Sci Med. 2015;134:66–75. doi: 10.1016/j.socscimed.2015.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kajankova M, Oswald JM, Terranova LM, et al. Response of school districts to the New York State Concussion Awareness and Management Act: review of policies and procedures. J Sch Health. 2017;87(6):409–415. doi: 10.1111/josh.12508. [DOI] [PubMed] [Google Scholar]
- 23.Kerr ZY, Hayden R, Dompier TP, Cohen R. Association of equipment worn and concussion injury rates in National Collegiate Athletic Association football practices: 2004–2005 to 2008–2009 academic years. Am J Sports Med. 2015;43(5):1134–1141. doi: 10.1177/0363546515570622. [DOI] [PubMed] [Google Scholar]
- 24.Schneider DK, Grandhi RK, Bansal P, et al. Current state of concussion prevention strategies: a systematic review and meta-analysis of prospective, controlled studies. Br J Sports Med. 2017;51(20):1473–1482. doi: 10.1136/bjsports-2015-095645. [DOI] [PubMed] [Google Scholar]
- 25.National Athletic Trainers' Association. Consensus Statement: Sickle Cell Trait and the Athlete. Dallas, TX: National Athletic Trainers' Association;; 2013. [Google Scholar]
- 26.Swartz EE, Broglio SP, Cook SB, et al. Early results of a helmetless-tackling intervention to decrease head impacts in football players. J Athl Train. 2015;50(12):1219–1222. doi: 10.4085/1062-6050-51.1.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lynn J, Oppenheimer S, Zimmer L. Using public policy to improve outcomes for asthmatic children in schools. J Allergy Clin Immunol. 2014;134(6):1238–1244. doi: 10.1016/j.jaci.2014.09.040. [DOI] [PubMed] [Google Scholar]
- 28.Sapien RE, Allen A. Emergency preparation in schools: a snapshot of a rural state. Pediatr Emerg Care. 2001;17(5):1–5. doi: 10.1097/00006565-200110000-00003. [DOI] [PubMed] [Google Scholar]
- 29.Walsh KM, Cooper MA, Holle R, et al. National Athletic Trainers' Association position statement: lightning safety for athletics and recreation. J Athl Train. 2013;48(2):258–270. doi: 10.4085/1062-6050-48.2.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Borus JS, Laffel L. Adherence challenges in the management of type 1 diabetes in adolescents: prevention and intervention. Curr Opin Pediatr. 2010;22(4):405–411. doi: 10.1097/MOP.0b013e32833a46a7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rimal RN, Real K. How behaviors are influenced by perceived norms: a test of the theory of normative social behavior. Commu Res. 2016;32(3):389–414. [Google Scholar]
- 32.Gamst FC. Foundations of social theory. Anthropol Work Review. 1991;12(3):19–25. [Google Scholar]
- 33.Khodaee M, Olewinski L, Shadgan B, Kiningham RR. Rapid weight loss in sports with weight classes. Curr Sports Med Rep. 2015;14(6):435–441. doi: 10.1249/JSR.0000000000000206. [DOI] [PubMed] [Google Scholar]
- 34.Smedley BD, Syme SL. Committee on Capitalizing on Social Science and Behavioral Research to Improve the Public's Health. Promoting health: intervention strategies from social and behavioral research. Am J Health Promot. 2001;15(3):149–166. doi: 10.4278/0890-1171-15.3.149. [DOI] [PubMed] [Google Scholar]
- 35.Emery CA, Hagel B, Morrongiello BA. Injury prevention in child and adolescent sport: whose responsibility is it? Clin J Sport Med. 2006;16(6):514–521. doi: 10.1097/01.jsm.0000251179.90840.58. [DOI] [PubMed] [Google Scholar]