Abstract
Objective
To conduct a systematic review with meta-analysis assessing the effectiveness of joint mobilizations for improving dorsiflexion range of motion (DFROM) and dynamic postural control in individuals with chronic ankle instability.
Data Sources
Electronic databases (PubMed, MEDLINE, CINAHL, and SPORTDiscus) were searched from inception to January 2017.
Study Selection
Included studies examined the isolated effects of joint mobilizations to enhance DFROM and dynamic postural control in individuals with chronic ankle instability and provided adequate data to calculate effect sizes (ESs) and 95% confidence intervals (CIs).
Data Extraction
Two investigators independently assessed the methodologic quality, level of evidence, and strength of recommendation using the Physiotherapy Evidence Database scale and the Strength of Recommendation Taxonomy. We extracted the sample sizes, means, and standard deviations for DFROM and dynamic postural control and filtered the data based on control-to-intervention and preintervention-to-postintervention (pre-post) comparisons.
Data Synthesis
We included 7 level 1 and 3 level 2 studies that had a median Physiotherapy Evidence Database score of 60% (range = 40%–80%). The magnitudes of control-to-intervention and pre-post differences were examined using bias-corrected Hedges g ESs. Random-effects meta-analyses were conducted for each outcome measure and comparison. Positive ESs indicated better outcome scores in the intervention group than in the control group and at postintervention than at preintervention. The α level was set at .05. Meta-analysis revealed weak and moderate ESs for overall control-to-intervention (ES = 0.41; 95% CI = 0.14, 0.68; P = .003) and pre-post (ES = 0.34; 95% CI = 0.20, 0.48; P < .001) DFROM analyses. Overall, dynamic postural control meta-analysis revealed moderate control-to-intervention (ES = 0.42; 95% CI = −0.14, 0.98; P = .14) and weak and moderate ESs for pre-post (ES = 0.37; 95% CI = −0.12, 0.87; P = .14) analyses.
Conclusions
We observed grade A evidence that joint mobilizations can mildly improve DFROM among individuals with chronic ankle instability compared with controls and preintervention. We observed grade B evidence that indicated conflicting effects of joint mobilizations on dynamic postural control compared with controls and preintervention.
Keywords: weight-bearing lunge test, Star Excursion Balance Test, Maitland mobilization, Mulligan mobilization
Key Points
Mulligan mobilizations with movement and Maitland mobilizations may moderately improve dorsiflexion range of motion and dynamic postural control in individuals with chronic ankle instability.
Dynamic postural control appeared to improve more from Mulligan mobilizations with movement than from Maitland mobilizations immediately after both a single intervention and multiple treatments.
Researchers should investigate the optimal treatment variables to enhance dorsiflexion range of motion and dynamic postural control in individuals with chronic ankle instability.
Lateral ankle sprains are among the most common orthopaedic injuries in the general and athletic populations.1 Up to 70% of acute ankle sprains result in residual symptoms and lead to a condition known as chronic ankle instability (CAI).2 Individuals with CAI experience symptoms, such as subsequent ankle sprains, episodes of “giving way” and instability, joint laxity, pain, swelling, and impaired ankle function. These symptoms are thought to be related to proprioceptive and neuromuscular deficits in this population.3 Furthermore, these symptoms and deficits are most likely due to a cascade of events after an acute ankle sprain and contribute to the development of CAI and the associated repetitive trauma.4,5 People with CAI often experience long-term problems, such as decreased health-related quality of life (HRQOL), decreased physical function, and an increased risk of developing posttraumatic osteoarthritis.6,7 Therefore, therapeutic interventions are needed to break this cycle of impairments that individuals with CAI experience.
Before discussing specific interventions, we need to identify the functional and mechanical factors that are the root cause of the repetitive trauma. People with CAI have commonly demonstrated impaired dorsiflexion range of motion (DFROM) during functional tasks and weight-bearing measurements.8,9 A decrease in DFROM has been associated with restricted posterior talar glide.10 After an injury to the talofibular ligament, the talus may sublux anteriorly and remain in this malposition until passively forced posteriorly into its anatomic position.10 Overall, these limitations in DFROM may affect the ability to execute functional activities and may contribute to repeated ankle sprains and episodes of giving way in individuals with CAI.4,8,11
As mentioned, DFROM limitations affect the entire lower extremity kinetic chain, not only during functional tasks, such as landing, but also during dynamic postural-control tasks.9,12 Whereas not as demanding as functional activities related to sport, dynamic postural-control assessment provides clinicians with an analysis of how patients maintain balance while incorporating movement.13 Dynamic postural-control tasks have demonstrated importance, as they have been linked to injury risk.13 Furthermore, dynamic postural control is important to the study of CAI interventions because it is a deficit commonly identified on the Star Excursion Balance Test (SEBT) and Y-Balance Test13,14 in this population. Therefore, dynamic postural control should be an important consideration during the rehabilitation of individuals with CAI.
Of the available evidence-based interventions, joint mobilizations have demonstrated the ability to enhance DFROM and dynamic postural control.15–18 Joint-mobilization techniques, primarily Maitland grade 3 talocrural anterior-to-posterior mobilization and Mulligan talocrural mobilizations with movement (MWMs), have shown efficacy in improving DFROM, as they are proposed to enhance the posterior translation of the talus.15,16,19,20 Furthermore, mechanical application of joint mobilizations may also stimulate the sensorimotor system, leading to improved postural control.20 Overall, these findings suggest that joint mobilizations can address DFROM and dynamic postural-control impairments in people with CAI.
Given the high rate of CAI and the negative effects on an individual's economic and physical wellbeing, evidence-based strategies that effectively treat the impairments associated with CAI need to be defined. No current systematic reviews, consensus statements, or recommendations on the effects of joint mobilizations on DFROM and dynamic postural control in people with CAI exist. Thus, the purpose of our systematic review with meta-analysis was to collect, critically appraise, and synthesize the current literature investigating the effects of various joint-mobilization techniques on DFROM and dynamic postural control in individuals with CAI.
METHODS
Search Strategy
We conducted a systematic search to investigate the effect of joint mobilizations on ankle DFROM and dynamic postural control based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.21 We searched PubMed and EBSCOHost (CINAHL, MEDLINE, SPORTDiscus) from inception through January 2017 using combinations of key words related to the original research question and the Boolean operators AND and OR (Table 1). The search was limited to studies involving human participants and written in English. The reference list of each article that was screened during the systematic search was hand searched to identify additional articles. The Boolean phrase creation, systematic search, and hand search were conducted by 2 investigators (C.J.P., R.A.V.).
Table 1.
Search Strategy
| Step |
Search Terms |
Boolean Operator |
EBSCO Host |
PubMed |
| 1 | Chronic ankle instability | OR | 3114 | 3291 |
| Functional ankle instability | ||||
| Ankle instability | ||||
| Mechanical ankle instability | ||||
| 2 | Manual therapy | OR | 188 137 | 166 098 |
| Joint mobilization | ||||
| Joint mobilisation | ||||
| Manipulation | ||||
| Maitland | ||||
| Mulligan | ||||
| 3 | 1, 2 | AND | 124 | 72 |
| Duplicates | 32a | |||
| Total identified | 164 | |||
Total number of duplicates between EBSCO and PubMed.
Selection Criteria
The eligibility of the articles identified in the systematic search was assessed by 2 investigators (C.J.P., R.A.V.) using the inclusion and exclusion criteria described in the following paragraphs. Initially, the titles and abstracts were screened to determine eligibility. If eligibility could not be determined from this initial screen, the full text of the manuscript was reviewed.
Inclusion Criteria
The following inclusion criteria were used to select and screen studies:
The primary aim was to investigate the effect of isolated joint mobilizations, manipulation, MWM, or traction for individuals with CAI.
Participants were described as having CAI, functional ankle instability, mechanical ankle instability, or recurrent ankle sprains.
The primary outcomes consisted of maximal DFROM or dynamic postural control, or both, as measured by the SEBT or Y-Balance Test.
Articles were peer-reviewed, full-text studies.
Exclusion Criteria
The following exclusion criteria were used to screen out studies:
Authors did not use joint-mobilization techniques as the primary intervention.
Investigators used other therapeutic interventions in combination with joint mobilizations.
Researchers did not use maximal DFROM or dynamic postural control assessed by the SEBT or Y-Balance Test as a primary outcome.
Authors did not report point measures or variability (means, standard deviations) to allow for the calculation of Hedges g effect sizes (ESs).
Articles were case studies, guidelines, systematic reviews, meta-analyses, or abstracts.
Articles were not published in English.
Methodologic Quality
The Physiotherapy Evidence Database (PEDro) scale was used to assess the quality of the included studies. The PEDro is a 10-item scale designed to evaluate the internal validity of randomized controlled trials and has demonstrated adequate reliability (intraclass correlation coefficient = 0.68).22 Studies that received a final score of ≥ 60% on the PEDro scale after final review were considered high-quality studies.14 The included studies were independently scored by 2 investigators (C.J.P., R.A.V.). After scoring each study independently, these investigators met to develop a consensus. A third investigator (S.L.G.) was consulted if a consensus could not be reached.
Data Extraction
The initial review was conducted by 2 independent reviewers (C.J.P., R.A.V.) who extracted the data, including the study aims, study quality, participant characteristics, inclusion criteria, intervention procedures, and outcome assessments. The reviewers discussed any discrepancies in data interpretation. If consensus could not be reached, the third reviewer (S.L.G.) was consulted.
The primary outcomes for this systematic review were DFROM and dynamic postural control. Means, standard deviations, and numbers of participants for these 2 variables were initially extracted and filtered based on comparison. All data were categorized either as control or sham versus intervention or as preintervention versus postintervention comparison. During extraction, scores for each reach direction of the SEBT and Y-Balance Test were extracted separately and classified as dynamic postural control.
To further categorize the participant groups, 4 moderator variables were created. We used mobilization type to categorize participants: Maitland, Mulligan MWM, or other. Maitland mobilization was used to describe participant groups that underwent anterior-to-posterior talocrural joint mobilizations. Mulligan MWM was used to describe participant groups that experienced a talocrural joint mobilization combined with movement to increase anterior translation of the tibia on the talus. Other described participant groups that were given other forms of mobilization (high velocity, traction, tibiofibular joint). We used treatment length to categorize mobilization protocols by the number of treatment sessions completed and included 2 levels: single treatment and multiple treatments. Measurement time was used to categorize participant groups by the timeframe during which measurements were made: immediate and follow up. Lastly, for dynamic postural-control data, only the moderator variable of reach direction was used: anterior, posteromedial, or posterolateral.
Statistical Analysis
Separate summary meta-analyses were performed for each outcome variable (DFROM, dynamic postural control) for each comparison (control or sham versus intervention, preintervention versus postintervention). A total of 4 summary meta-analyses were completed. For the summary analyses, multiple point estimates from the same group were pooled to reduce sample-size inflation. For example, SEBT and Y-Balance Test reach directions were pooled for each included investigation. Subanalyses also were conducted for each moderator variable (mobilization type, treatment length, measurement time) for each outcome variable and comparison. Lastly, analyses were completed for the outcome measure of dynamic postural control for each comparison using the moderator reach direction.
Each meta-analysis was completed using a random-effects model in which individual point estimates were pooled from the included studies using bias-corrected Hedges g ESs and 95% confidence intervals (CIs) to determine the magnitude of the effect. Positive ESs indicated greater DFROM and dynamic postural control in the intervention than in the control group and at postintervention than at preintervention. All meta-analysis procedures were completed in Comprehensive Meta-Analysis (version 3.3.070; BioStat, Englewood, NJ). We interpreted ESs as weak (≤0.40), moderate (0.41–0.69), or strong (≥0.70).23 The α level was set a priori at .05. To further examine the data, we performed a qualitative assessment of ESs and CIs by assessing the differences in ES estimates between groups and determining whether the CIs crossed 0.
Assessment of Publication Bias
The Orwin fail-safe N test was used to assess the strength of the observed summary effects for each primary analysis. This test examines the number of studies with trivial effects (ES = 0.00) that would be needed to nullify the pooled ES of the included studies. Lastly, funnel plots and the trim-and-fill method were used to further assess publication bias. The trim-and-fill method estimates the number of missing studies based on funnel-plot asymmetry.24
Sensitivity Analysis
To examine the influence of a single participant group (point estimate) on the observed summary effect of each summary analysis, we completed a 1-study-removed analysis. This method determines the effect on the observed summary effect by repeating the meta-analysis multiple times with a single participant group (point estimate) removed each time.
Level of Evidence and Strength of Recommendation
The quality of the individual studies, as well as the body of evidence, was assessed using the Strength of Recommendation Taxonomy (SORT).25 Each included study's findings were labeled as level 1, 2, or 3 evidence. We considered level 1 evidence to be good-quality (PEDro score ≥ 60%), patient-oriented evidence; level 2 evidence, limited-quality (PEDro score < 60%), patient-oriented evidence; and level 3 evidence, other evidence.25 To assess the collective body of evidence, the SORT assigns a strength recommendation. The SORT considers a grade of A as consistent, good-quality, patient-oriented evidence; grade B, inconsistent or limited-quality, patient-oriented evidence; and grade C, consensus, disease-oriented evidence.25
RESULTS
Literature Search
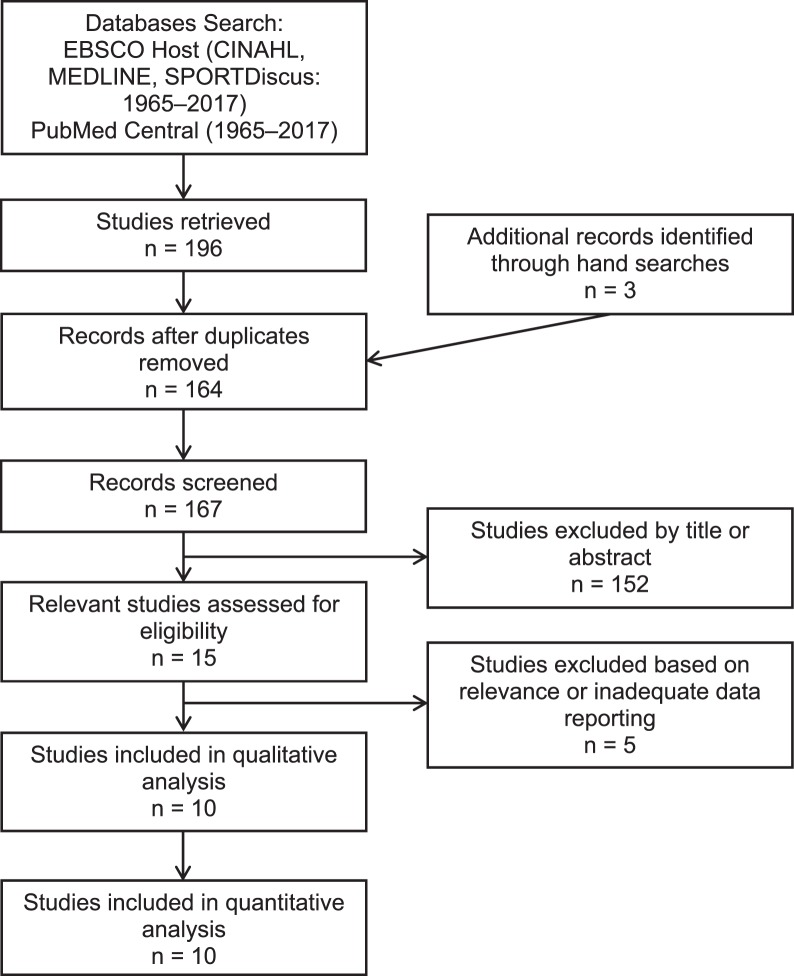
Of the initial 196 articles retrieved from the electronic and hand searches, 10 articles met the inclusion criteria for this systematic review (Figure 1). The authors of 10 articles15–20,26–29 had examined DFROM changes after a mobilization intervention. Of the 10 articles, preintervention-to-postintervention DFROM changes had been investigated in 9,15,17–20,26–29 and DFROM differences between a control or sham group and an intervention group had been investigated in 8.16,17,19,20,26–29 In 6 articles,15,16,18,19,26,27 the researchers had assessed SEBT changes after a mobilization intervention. The authors of 515,18,19,26,27 of these 6 articles had examined preintervention-to-postintervention SEBT changes, and the authors of 4 articles16,19,26,27 had examined SEBT differences between a control or sham group and an intervention group. A methodologic summary of the included studies is presented in Table 2.
Figure 1.
Flow chart of literature review.
Table 2.
Methodologic Summary of the Included Studies Continued on Next Page
| Authors and Design |
Sample Size and Group |
Participant Characteristics |
Intervention |
Intervention Frequency |
Outcome Measures |
Results |
| Vicenzino et al28 (2006), crossover study | 16 Recurrent ankle sprains | History of ≥2 ankle sprains, 20-mm weight-bearing DFROM asymmetry, and no history of contralateral ankle sprain | Mulligan weight-bearing MWM: 4 sets of 4 glides held for 10 s at end range of motion Mulligan nonweight-bearing MWM: 4 sets of 4 glides held for 10 s at end range of motion Control: no treatment | 1 Intervention session | DFROM (weight-bearing–lunge test, cm) Immediate | Both MWM techniques immediately improved DFROM. No differences between techniques. |
| Hoch and McKeon16 (2011), crossover study | 20 CAI | History of ankle sprain, ≥2 episodes of giving way in the past 3 mo, ≥4 yes on the Ankle Instability Index, ≤90% on the FAAM-ADL, and ≤80% on the FAAM-Sport | Maitland grade 3 anterior-to-posterior talocrural joint mobilization: two 2-min sets with 1-min rest in between Control: no active contraction for 5 min | 1 Intervention session | DFROM (weight-bearing–lunge test, cm) SEBT (anterior, posteromedial, and posterolateral directions) Immediate | DFROM was greater in the mobilization than the control group. No SEBT differences. |
| Hoch et al15 (2012), prospective cohort study | 12 CAI | History of ankle sprain, ≥2 episodes of giving way in the past 3 mo, ≥4 yes on the Ankle Instability Index, ≤90% on the FAAM-ADL, and ≤80% on the FAAM-Sport | Maitland grade 2 talocrural joint traction: two 2-min sets Maitland grade 3 anterior-to-posterior talocrural joint mobilization: four 2-min sets with 1-min rest in between | 6 Intervention sessions over 2 wk | DFROM (weight-bearing–lunge test, cm) SEBT (anterior, posteromedial, and posterolateral directions) Immediate, 1-wk follow up | DFROM and SEBT in the anterior, posteromedial, and posterolateral directions all improved at postintervention and 1-wk follow up compared with preintervention. |
| Beazell et al29 (2012), randomized controlled trial | 43 CAI Proximal = 15, distal = 15, control = 15 | History of ankle sprain, episodes of giving way, ≥5° DFROM asymmetry, ≥85% on FAAM-Sport, or ≥3 on the Ankle Instability Index | Proximal tibiofibular-joint manipulation: 1–2 high-velocity, low-amplitude thrusts Distal tibiofibular-joint manipulation: 1–2 high-velocity, low-amplitude thrusts Control: no activity for 1–2 min | 4 Intervention sessions over 3 wk | DFROM (weight-bearing–lunge test, °) Immediate after each intervention | No DFROM differences. |
| Harkey et al19 (2014), randomized controlled trial | 30 CAI Maitland = 15, control = 15 | History of ankle sprain, >2 episodes of giving way in the past 6 mo, ≤90% on the FADI, and ≤80% on the FAAM-Sport | Maitland grade 3 talarcrural anterior-to-posterior joint mobilization: 3 sets of 1 min with 1-min rest between sets Control: no activity for 5 min | 1 Intervention session | DFROM (nonweight-bearing–lunge test,°) SEBT (anterior, posteromedial, and posterolateral directions) Immediate | DFROM improved compared with control. No SEBT group differences. |
| Gilbreath et al18 (2014), prospective cohort study | 11 CAI | History of ankle sprain, ≥1 episode of giving way in the past 3 mo, and ≤25 on the CAIT | Mulligan weight-bearing MWM: 2 sets of 4 glides held for 30 s at end range of motion with 1-min rest between sets | 3 Intervention sessions over 1 wk | DFROM (weight-bearing–lunge test, cm) SEBT (anterior, posteromedial, and posterolateral directions) Immediate | No change in DFROM or SEBT scores. |
| Cruz-Díaz et al26 (2015), randomized controlled trial | 90 CAI MWM = 29/30, sham = 28/31, control, 21/29 | History of ankle sprain, ≥2 sprains on same side in the last 2 y, reported episodes of giving way, >2-cm weight-bearing–lunge-test asymmetry, and no history of ankle sprain on contralateral side | Mulligan weight-bearing MWM: 2 sets of 10 glides Sham: fixed ankle while knee was flexed and extended for 2 sets of 10 glides Control: no interactions | 6 Intervention sessions over 3 wk | DFROM (weight-bearing–lunge test, cm) SEBT (anterior, posteromedial, and posterolateral directions) Immediate (single treatment), immediate (3 wk), 6-mo follow up | Greater DFROM and SEBT scores were identified at each time point for the MWM group compared with control. |
| Marrón-Gómez et al17 (2015), randomized controlled trial | 52 CAI MWM = 18, high-velocity, low-amplitude = 19, placebo = 15 | History of ankle sprain, current episodes of giving way, subjective pain or decreased function, and <24 on the CAIT | Mulligan weight-bearing MWM: 1 set of 10 glides High-velocity, low-amplitude: 1 set of 3 talocrural traction high-velocity, low-amplitude thrusts Placebo: mobilization with movement with absence of pressure for 1 set of 10 glides | 1 Intervention session | DFROM (weight-bearing–lunge test, cm) Immediate, 10 min, 24 h, and 48 h | Improvements in DFROM for both treatment groups compared with control. |
| McKeon and Wikstrom20 (2016), randomized controlled trial | 80 CAI Mobilization = 19/20, massage = 19/20, stretching = 18/20, control = 19/20 | History of ≥2 episodes of giving way in the past 6 mo, ≥5 on the Ankle Instability Index, ≤90% on the FAAM, and ≤80% on the FAAM-Sport | Maitland grade 3 anterior-to-posterior talocrural joint mobilization: 2 sets of 2 min with 1-min rest in between | 6 Intervention sessions over 2 wk | DFROM (weight-bearing–lunge test, cm) Immediate (single treatment), immediate (2 wk), 1-mo follow up | Mobilization improved DFROM at all time points compared with control. |
| Powden et al27 (2017), crossover study | 20 CAI | History of ankle sprain, ≥2 episodes of giving way in the last 3 mo, yes to ≥5 questions on the Ankle Instability Index, and ≤26 on the CAIT | Sustained Maitland grade 2 talocrural traction: 4 sets of 30-s holds with 1-min rest between sets Oscillatory Maitland grade 2 talocrural traction: 4 sets of 30-s oscillations with 1-min rest in between Sham: 4 sets of 30 s contact with no force | 1 Intervention session | DFROM (weight-bearing–lunge test, cm) SEBT (anterior direction) Immediate | No differences were identified for DFROM or SEBT. |
Abbreviations: CAI, chronic ankle instability; CAIT, Cumberland Ankle Instability Tool; DFROM, dorsiflexion range of motion; FAAM, Foot and Ankle Ability Measure; FAAM-ADL, FAAM–Activities of Daily Living subscale; FAAM-Sport, FAAM–Sport subscale; FADI, Foot and Ankle Disability Index; MWM, mobilizations with movement; SEBT, Star Excursion Balance Test.
Methodologic Quality
The results of the quality assessment can be found in Table 3. The 2 reviewers agreed on 90 of 100 (90%) items on the PEDro scale. The third investigator resolved disagreements in 2 instances. Overall, the quality scores of the included articles ranged from 40% to 80%, with a median of 60%. We found 7 level 1 studies16,17,19,20,26,28,29 and 3 level 2 studies.15,18,27 The overall quality score for the DFROM control-to-intervention comparison ranged from 60% to 80%, with a median of 70%. The overall quality score for the DFROM preintervention-to-postintervention comparison ranged from 40% to 80%, with a median of 60%. The overall quality score for the dynamic postural-control control-to-intervention comparison ranged from 40% to 80%, with a median of 60%. The overall quality score for the dynamic postural-control preintervention-to-postintervention comparison ranged from 40% to 80%, with a median of 60%. Individual quality scores and the level of evidence for each study are presented in Table 3.
Table 3.
Physiotherapy Evidence Database Scale Individual Items and Quality Index Scores for the Included Articles
| Item |
Vicenzino et al28 (2006) |
Hoch and McKeon16 (2011) |
Hoch et al15 (2012) |
Beazell et al29 (2012) |
Harkey et al19 (2014) |
Gilbreath et al18 (2014) |
Cruz-Díaz et al26 (2015) |
McKeon and Wikstrom20 (2016) |
Powden et al27 (2017) |
| 1. Random allocation | Yes | Yes | No | Yes | Yes | No | Yes | Yes | Yes |
| 2. Allocation concealed | No | Yes | No | No | Yes | No | Yes | Yes | Yes |
| 3. Similar at baseline | Yes | Yes | No | Yes | Yes | No | No | Yes | Yes |
| 4. Blinding of all subjects | No | No | No | No | No | No | No | No | No |
| 5. Blinding of all therapists | No | No | No | No | No | No | No | No | No |
| 6. Blinding of all assessors | Yes | Yes | No | Yes | Yes | No | Yes | No | Yes |
| 7. More than 85% of follow up | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 8. Intention to treat | Yes | Yes | Yes | No | Yes | Yes | Yes | No | Yes |
| 9. Between-groups statistical comparison | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 10. Point measures and variability | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 11. Eligibility criteria indicated | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Yes, No. (%)a | 7 (70) | 8 (80) | 4 (40) | 6 (60) | 8 (80) | 4 (40) | 7 (70) | 6 (60) | 8 (80) |
| Level of evidence | 1 | 1 | 2 | 1 | 1 | 2 | 1 | 1 | 2 |
Scores are based on items 1 through 10.
Data Synthesis
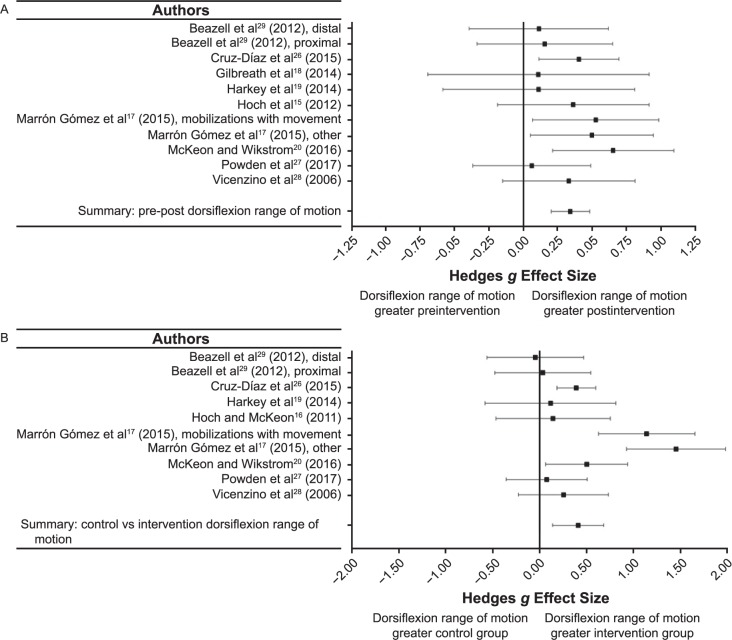
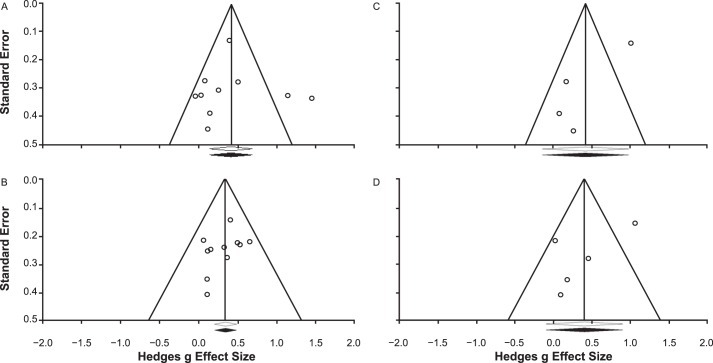
All individual ESs and cumulative effects are presented in Figures 2 and 3 and Tables 4 and 5.
Figure 2.
Summary of Hedges g effect sizes and 95% confidence intervals for the overall analyses. A, Dorsiflexion preintervention-to-postintervention comparison. B, Dorsiflexion control-to-intervention comparison. C, Dynamic postural control preintervention-to-postintervention comparison. D, Dynamic postural control control-to-intervention comparison. Continued on next page.
Figure 2.
Continued from previous page.
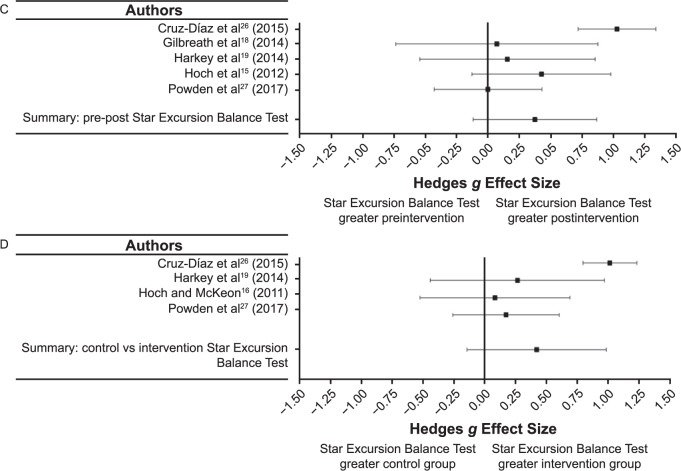
Figure 3.
Summary of Hedges g effect sizes and 95% confidence intervals for the subanalyses. A, Mobilization type. B, Treatment length. C, Measurement time. D, Reach direction. Abbreviation: MWM, mobilizations with movement.
Table 4.
Effect Sizes and 95% Confidence Intervals for Dorsiflexion Participant Groups
| Comparison |
Mobilization |
Length |
Time Measurement |
Hedges g Effect Size |
95% Confidence Interval |
P Value |
| Control/sham versus intervention | ||||||
| Vicenzino et al28 (2006) | Mulligan MWM weight bearing | Single | Immediate | 0.25 | −0.43, 0.93 | .47 |
| Vicenzino et al28 (2006) | Mulligan MWM non–weight bearing | Single | Immediate | 0.25 | −0.43, 0.93 | .47 |
| Hoch and McKeon16 (2011) | Maitland grade 3 | Single | Immediate | 0.14 | −0.47, 0.75 | .65 |
| Beazell et al29 (2012) | High-velocity, low-amplitude proximal tibiofibular joint | Single | Immediate | 0.04 | −0.68, 0.76 | .93 |
| Beazell et al29 (2012) | High-velocity, low amplitude distal tibiofibular joint | Single | Immediate | −0.07 | −0.80, 0.66 | .85 |
| Harkey et al19 (2014) | Maitland grade 3 | Single | Immediate | 0.11 | −0.58, 0.81 | .75 |
| Cruz Díaz et al26 (2015), control | Mulligan MWM weight bearing | Single | Immediate | 0.39 | −0.12, 0.90 | .13 |
| Cruz Díaz et al26 (2015), sham | Mulligan MWM weight bearing | Single | Immediate | 0.39 | −0.11, 0.89 | .13 |
| Marrón Gómez et al17 (2015) | High-velocity, low-amplitude | Single | Immediate | 1.54 | 0.79, 2.30 | <.001a |
| Marrón Gómez et al17 (2015) | High-velocity, low-amplitude | Single | 48 h | 1.36 | 0.62, 2.10 | <.001a |
| Marrón Gómez et al17 (2015) | Mulligan MWM weight bearing | Single | Immediate | 1.04 | 0.33, 1.76 | .004a |
| Marrón Gómez et al17 (2015) | Mulligan MWM weight bearing | Single | 48 h | 1.24 | 0.50, 1.97 | .001a |
| McKeon and Wikstrom20 (2016) | Maitland grade 3 | Single | Immediate | 0.33 | −0.28, 0.94 | .29 |
| Powden et al27 (2017) | Sustained traction | Single | Immediate | 0.00 | −0.60, 0.61 | .99 |
| Powden et al27 (2017) | Oscillatory traction | Single | Immediate | 0.14 | −0.46, 0.75 | .64 |
| Beazell et al29 (2012) | High-velocity, low-amplitude proximal tibiofibular joint | 3 wk | Immediate | 0.02 | −0.70, 0.74 | .95 |
| Beazell et al29 (2012) | High-velocity, low-amplitude distal tibiofibular joint | 3 wk | Immediate | −0.03 | −0.75, 0.69 | .94 |
| Cruz Díaz et al26 (2015), control | Mulligan MWM weight bearing | 3 wk | Immediate | 0.40 | −0.11, 0.91 | .12 |
| Cruz Díaz et al26 (2015), control | Mulligan MWM weight bearing | 3 wk | 6 mo | 0.39 | −0.12, 0.90 | .13 |
| Cruz Díaz et al26 (2015), sham | Mulligan MWM weight bearing | 3 wk | Immediate | 0.38 | −0.12, 0.88 | .14 |
| Cruz Díaz et al26 (2015), sham | Mulligan MWM weight bearing | 3 wk | 6 mo | 0.38 | −0.12, 0.88 | .14 |
| McKeon and Wikstrom20 (2016) | Maitland grade 3 | 3 wk | Immediate | 0.68 | 0.05, 1.30 | .03a |
| Summary | 0.41 | 0.14, 0.68 | .003a | |||
| Preintervention versus postintervention | ||||||
| Vicenzino et al28 (2006) | Mulligan MWM weight bearing | Single | Immediate | 0.38 | −0.30, 1.06 | .28 |
| Vicenzino et al28 (2006) | Mulligan MWM non–weight bearing | Single | Immediate | 0.28 | −0.39, 0.96 | .41 |
| Beazell et al29 (2012) | High-velocity, low-amplitude proximal tibiofibular joint | Single | Immediate | 0.10 | −0.60, 0.80 | .78 |
| Beazell et al29 (2012) | High-velocity, low-amplitude distal tibiofibular joint | Single | Immediate | 0.11 | −0.60, 0.82 | .76 |
| Harkey et al19 (2014) | Maitland grade 3 | Single | Immediate | 0.11 | −0.59, 0.81 | .75 |
| Cruz Díaz et al26 (2015) | Mulligan MWM weight bearing | Single | Immediate | 0.39 | −0.11, 0.90 | .13 |
| Marrón Gómez et al17 (2015) | High-velocity, low-amplitude | Single | Immediate | 0.56 | −0.07, 1.20 | .08 |
| Marrón Gómez et al17 (2015) | High-velocity, low-amplitude | Single | 48 h | 0.43 | −0.20, 1.06 | .18 |
| Marrón Gómez et al17 (2015) | Mulligan MWM weight bearing | Single | Immediate | 0.46 | −0.19, 1.10 | .17 |
| Marrón Gómez et al17 (2015) | Mulligan MWM weight bearing | Single | 48 h | 0.60 | −0.06, 1.25 | .07 |
| McKeon and Wikstrom20 (2016) | Maitland grade 3 | Single | Immediate | 0.53 | −0.09, 1.15 | .09 |
| Powden et al27 (2017) | Sustained traction | Single | Immediate | 0.04 | −0.56, 0.65 | .89 |
| Powden et al27 (2017) | Oscillatory traction | Single | Immediate | 0.08 | −0.53, 0.69 | .80 |
| Gilbreath et al18 (2014) | Mulligan MWM weight bearing | 1 wk | Immediate | 0.11 | −0.70, 0.91 | .79 |
| Hoch et al15 (2012) | Maitland grade 3 | 2 wk | Immediate | 0.35 | −0.43, 1.13 | .38 |
| Hoch et al15 (2012) | Maitland grade 3 | 2 wk | 1 wk | 0.38 | −0.40, 1.16 | .34 |
| Beazell et al29 (2012) | High-velocity, low-amplitude proximal tibiofibular joint | 3 wk | Immediate | 0.21 | −0.49, 0.91 | .55 |
| Beazell et al29 (2012) | High-velocity, low-amplitude distal tibiofibular joint | 3 wk | Immediate | 0.12 | −0.60, 0.84 | .75 |
| Cruz Díaz et al26 (2015) | Mulligan MWM weight bearing | 3 wk | Immediate | 0.41 | −0.10, 0.91 | .12 |
| Cruz Díaz et al26 (2015) | Mulligan MWM weight bearing | 3 wk | 6 mo | 0.41 | −0.09, 0.92 | .11 |
| McKeon and Wikstrom20 (2016) | Maitland grade 3 | 3 wk | Immediate | 0.78 | 0.15, 1.41 | .02 |
| Summary | 0.34 | 0.20, 0.48 | <.001a | |||
Abbreviation: MWM, mobilizations with movement.
P < .05.
Table 5.
Effect Sizes and 95% Confidence Intervals for Dynamic Postural-Control Participant Groups
| Comparison |
Mobilization |
Length |
Time Measurement |
Hedges g Effect Size |
95% Confidence Interval |
P Value |
| Control or sham versus intervention | ||||||
| Anterior direction | ||||||
| Harkey et al19 (2014) | Maitland grade 3 | Single | Immediate | −0.21 | −0.91, 0.49 | .55 |
| Cruz Díaz et al26 (2015), control | Mulligan MWM weight-bearing | Single | Immediate | 1.08 | 0.54, 1.62 | <.001a |
| Cruz Díaz et al26 (2015), sham | Mulligan MWM weight-bearing | Single | Immediate | 1.35 | 0.80, 1.90 | <.001a |
| Powden et al27 (2017) | Sustained traction | Single | Immediate | 0.00 | −0.61, 0.61 | >.99 |
| Powden et al27 (2017) | Oscillatory traction | Single | Immediate | 0.35 | −0.27, 0.96 | .27 |
| Hoch and McKeon16 (2011) | Maitland grade 3 | 2 wk | Immediate | 0.10 | −0.51, 0.71 | .74 |
| Cruz Díaz et al26 (2015), control | Mulligan MWM weight-bearing | 3 wk | Immediate | 1.32 | 0.76, 1.87 | <.001a |
| Cruz Díaz et al26 (2015), control | Mulligan MWM weight-bearing | 3 wk | 6 mo | 1.13 | 0.59, 1.68 | <.001a |
| Cruz Díaz et al26 (2015), sham | Mulligan MWM weight-bearing | 3 wk | Immediate | 1.37 | 0.82, 1.92 | <.001a |
| Cruz Díaz et al26 (2015), sham | Mulligan MWM weight-bearing | 3 wk | 6 mo | 1.35 | 0.80, 1.90 | <.001a |
| Posteromedial direction | ||||||
| Harkey et al19 (2014) | Maitland grade 3 | Single | Immediate | 0.54 | −0.17, 1.25 | .14 |
| Cruz Díaz et al26 (2015), control | Mulligan MWM weight-bearing | Single | Immediate | 0.62 | 0.11, 1.14 | .02a |
| Cruz Díaz et al26 (2015), sham | Mulligan MWM weight-bearing | Single | Immediate | 0.68 | 0.17, 1.19 | .009a |
| Hoch and McKeon16 (2011) | Maitland grade 3 | 2 wk | Immediate | 0.05 | −0.55, 0.66 | .86 |
| Cruz Díaz et al26 (2015), control | Mulligan MWM weight-bearing | 3 wk | Immediate | 0.74 | 0.22, 1.26 | .005a |
| Cruz Díaz et al26 (2015), control | Mulligan MWM weight-bearing | 3 wk | Immediate | 0.41 | −0.10, 0.92 | .12 |
| Cruz Díaz et al26 (2015), sham | Mulligan MWM weight-bearing | 3 wk | 6 mo | 0.80 | 0.29, 1.32 | .002a |
| Cruz Díaz et al26 (2015), sham | Mulligan MWM weight-bearing | 3 wk | 6 mo | 0.70 | 0.19, 1.21 | .007a |
| Posterolateral direction | ||||||
| Harkey et al19 (2014) | Maitland grade 3 | Single | Immediate | 0.47 | −0.24, 1.18 | .19 |
| Cruz Díaz et al26 (2015), control | Mulligan MWM weight-bearing | Single | Immediate | 0.96 | 0.42, 1.49 | <.001a |
| Cruz Díaz et al26 (2015), sham | Mulligan MWM weight-bearing | Single | Immediate | 0.68 | 0.17, 1.19 | .009a |
| Hoch and McKeon16 (2011) | Maitland grade 3 | 2 wk | Immediate | 0.09 | −0.52, 0.70 | .77 |
| Cruz Díaz et al26 (2015), control | Mulligan MWM weight-bearing | 3 wk | Immediate | 1.84 | 1.24, 2.45 | <.001a |
| Cruz Díaz et al26 (2015), control | Mulligan MWM weight-bearing | 3 wk | Immediate | 1.65 | 1.06, 2.23 | <.001a |
| Cruz Díaz et al26 (2015), sham | Mulligan MWM weight-bearing | 3 wk | 6 mo | 0.94 | 0.42, 1.47 | <.001a |
| Cruz Díaz et al26 (2015), sham | Mulligan MWM weight-bearing | 3 wk | 6 mo | 0.70 | 0.19, 1.21 | .007a |
| Summary | 0.42 | −0.14, 0.98 | .14 | |||
| Preintervention versus postintervention | ||||||
| Anterior direction | ||||||
| Harkey et al19 (2014) | Maitland grade 3 | Single | Immediate | 0.19 | −0.50, 0.89 | .59 |
| Cruz Díaz et al26 (2015) | Mulligan MWM weight-bearing | Single | Immediate | 1.34 | 0.78, 1.89 | <.001a |
| Powden et al27 (2017) | Sustained traction | Single | Immediate | 0.00 | −0.61, 0.61 | >.99 |
| Powden et al27 (2017) | Oscillatory traction | Single | Immediate | 0.00 | −0.61, 0.61 | >.99 |
| Gilbreath et al18 (2014) | Mulligan MWM weight-bearing | 1 wk | Immediate | 0.00 | −0.81, 0.80 | >.99 |
| Hoch et al15 (2012) | Maitland grade 3 | 2 wk | Immediate | 0.36 | −0.42, 1.14 | .37 |
| Hoch et al15 (2012) | Maitland grade 3 | 2 wk | 1 wk | 0.45 | −0.33, 1.24 | .26 |
| Cruz Díaz et al26 (2015) | Mulligan MWM weight-bearing | 3 wk | Immediate | 1.61 | 1.04, 2.19 | <.001a |
| Cruz Díaz et al26 (2015) | Mulligan MWM weight-bearing | 3 wk | 6 mo | 1.43 | 0.87, 2.00 | <.001a |
| Posteromedial direction | ||||||
| Harkey et al19 (2014) | Maitland grade 3 | Single | Immediate | 0.27 | −0.43, 0.97 | .45 |
| Cruz Díaz et al26 (2015) | Mulligan MWM weight-bearing | Single | Immediate | 1.01 | 0.48, 1.54 | <.001a |
| Gilbreath et al18 (2014) | Mulligan MWM weight-bearing | 1 wk | Immediate | 0.16 | −0.65, 0.96 | .70 |
| Hoch et al15 (2012) | Maitland grade 3 | 2 wk | Immediate | 0.39 | −0.39, 1.17 | .33 |
| Hoch et al15 (2012) | Maitland grade 3 | 2 wk | 1 wk | 0.45 | −0.33, 1.23 | .26 |
| Cruz Díaz et al26 (2015) | Mulligan MWM weight-bearing | 3 wk | Immediate | 1.19 | 0.65, 1.73 | <.001a |
| Cruz Díaz et al26 (2015) | Mulligan MWM weight-bearing | 3 wk | 6 mo | 0.86 | 0.34, 1.39 | .001a |
| Posterolateral direction | ||||||
| Harkey et al19 (2014) | Maitland grade 3 | Single | Immediate | 0.00 | −0.70, 0.70 | >.99 |
| Cruz Díaz et al26 (2015) | Mulligan MWM weight-bearing | Single | Immediate | 0.55 | 0.04, 1.06 | .03a |
| Gilbreath et al18 (2014) | Mulligan MWM weight-bearing | 1 wk | Immediate | 0.05 | −0.75, 0.85 | .90 |
| Hoch et al15 (2012) | Maitland grade 3 | 2 wk | Immediate | 0.40 | −0.38, 1.18 | .32 |
| Hoch et al15 (2012) | Maitland grade 3 | 2 wk | 1 wk | 0.50 | −0.28, 1.29 | .21 |
| Cruz Díaz et al26 (2015) | Mulligan MWM weight-bearing | 3 wk | Immediate | 0.55 | 0.04, 1.06 | .03a |
| Cruz Díaz et al26 (2015) | Mulligan MWM weight-bearing | 3 wk | 6 mo | 0.71 | 0.19, 1.22 | .007a |
| Summary | 0.37 | −0.12, 0.87 | .14 | |||
Abbreviation: MWM, mobilizations with movement.
P < .05.
Summary Analyses
For the DFROM control-to-intervention comparison, we noted an overall moderate summary effect for improving DFROM after a joint-mobilization intervention (ES = 0.41; 95% CI = 0.14, 0.68; P = .003). For the DFROM preintervention-to-postintervention comparison, we observed an overall weak summary effect for improving DFROM after joint-mobilization intervention (ES = 0.34; 95% CI = 0.20, 0.48; P < .001).
The analysis of the overall dynamic postural-control was not conclusive, as no difference was observed and each comparison included CIs that encompassed zero. For the SEBT control-to-intervention comparison, an overall moderate effect was present for improved dynamic postural control after a joint-mobilization intervention (ES = 0.42; 95% CI = −0.14, 0.98; P = .14). For the SEBT preintervention-to-postintervention comparison, we observed an overall weak effect for improving dynamic postural control after a joint-mobilization intervention (ES = 0.37; 95% CI = −0.12, 0.87; P = .14).
Mobilization Type
The results of the subanalysis of mobilization type for increasing DFROM in the intervention versus control group indicated a moderate positive effect for Mulligan MWM (ES = 0.56; 95% CI = 0.11, 1.01; P = .02), a weak positive effect for Maitland mobilization (ES = 0.32; 95% CI = 0.01, 0.64; P = .045), and a weak positive effect that was not different for the other interventions (ES = 0.37; 95% CI = −0.30, 1.04; P = .28). Increasing DFROM from preintervention to postintervention resulted in a moderate positive effect for Mulligan MWM (ES = 0.40; 95% CI = 0.18, 0.61; P < .001), a moderate positive effect for Maitland mobilization (ES = 0.46; 95% CI = 0.15, 0.76; P = .004), and a weak positive effect that was not different for the other interventions (ES = 0.21; 95% CI = −0.02, 0.44; P = .08).
The dynamic postural-control control-to-intervention comparison showed a strong positive effect for the Mulligan MWM (ES = 1.01; 95% CI = 0.79, 1.23; P < .001), a weak positive effect that was not different for the Maitland mobilization (ES = 0.16; 95% CI = −0.30, 0.62; P = .50), and a weak positive effect that was not different for the other interventions (ES = 0.17; 95% CI = −0.26, 0.60; P = .44). For the dynamic postural-control preintervention-to-postintervention comparison, we observed a strong positive effect for the Mulligan MWM (ES = 0.87; 95% CI = 0.48, 1.25; P < .001), a weak positive effect that was not different for the Maitland mobilization (ES = 0.32; 95% CI = −0.11, 0.75; P = .15), and a weak positive effect that was not different for the other interventions (ES = 0.00; 95% CI = −0.43, 0.43; P >.99).
Treatment Length
The subanalysis of treatment length for increasing DFROM in the intervention versus control group indicated a moderate positive effect for a single treatment (ES = 0.45; 95% CI = 0.21, 0.70; P < .001) and a weak positive effect for multiple treatments (ES = 0.35; 95% CI = 0.14, 0.57; P = .001). Increasing DFROM from preintervention to postintervention demonstrated a weak positive effect for a single treatment (ES = 0.32; 95% CI = 0.15, 0.50; P < .001) and a weak positive effect for multiple treatments (ES = 0.38; 95% CI = 0.15, 0.60; P = .001).
The SEBT control-to-intervention comparison displayed a moderate positive effect for a single treatment (ES = 0.51; 95% CI = 0.15, 0.88; P = .005) and a strong positive effect for multiple treatments (ES = 0.89; 95% CI = 0.51, 1.28; P < .001). For the SEBT preintervention-to-postintervention comparison, we observed a weak positive effect that was not different for a single treatment (ES = 0.30; 95% CI = −0.20, 0.80; P = .24) and a moderate positive effect for multiple treatments (ES = 0.69; 95% CI = 0.30, 1.08; P = .001).
Measurement Time
The subanalysis of measurement time for increasing DFROM in the intervention versus control group indicated a weak positive effect for immediate (ES = 0.33; 95% CI = 0.19, 0.48; P < .001) and a moderate positive effect for follow-up (ES = 0.68; 95% CI = 0.39, 0.97; P < .001) measurement times. Increasing DFROM from preintervention to postintervention produced a weak positive effect for the immediate (ES = 0.31; 95% CI = 0.16, 0.47; P < .001) and a moderate positive effect for the follow-up (ES = 0.45; 95% CI = 0.14, 0.76; P = .004) measurement times.
The dynamic postural-control control-to-intervention comparison demonstrated a moderate positive effect for the immediate (ES = 0.63; 95% CI = 0.29, 0.96; P < .001) and a strong positive effect for the follow-up (ES = 0.99; 95% CI = 0.61, 1.37; P < .001) measurement times. For the dynamic postural-control preintervention-to-postintervention comparison, we observed a moderate positive effect for the immediate (ES = 0.42; 95% CI = 0.03, 0.82; P = .04) and a strong positive effect for the follow-up (ES = 0.80; 95% CI = 0.36, 1.24; P < .001) measurement times.
Reach Direction
The subanalysis of SEBT reach direction for increasing dynamic postural control in the intervention versus control group displayed a weak effect that was not different for the anterior direction (ES = 0.33; 95% CI = −0.61, 0.61; P = .35), a moderate positive effect for the posterolateral direction (ES = 0.49; 95% CI = 0.14, 0.85; P = .006), and a moderate positive effect that was not different for the posteromedial direction (ES = 0.59; 95% CI = −0.07, 1.26; P = .08). Increasing dynamic postural control from preintervention to postintervention resulted in a weak effect that was not different for the anterior direction (ES = 0.37; 95% CI = −0.25, 1.00; P = .24), a moderate positive effect for the posterolateral direction (ES = 0.55; 95% CI = 0.09, 1.01; P = .02), and a moderate positive effect for the posteromedial direction (ES = 0.42; 95% CI = 0.15, 0.70; P = .003).
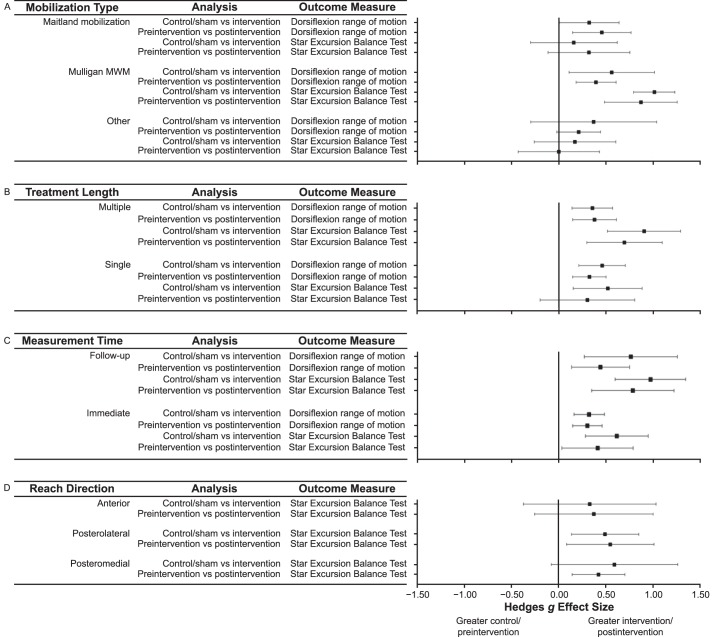
Publication Bias
We assessed the likelihood of publication bias for each primary summary analysis using funnel plots (Figure 4). It is unlikely that publication bias played a role in the results of the primary summary analyses based on the relative symmetry and even distribution of the studies in the funnel plots. Further support for the lack of publication bias was indicated via the trim-and-fill method, as no studies were inputted or removed. The Orwin fail-safe N tests showed that a range of 23 to 71 additional studies, based on a trivial effect range of the Hedges g from 0.10 to 0.05, would be needed to nullify the overall summary effects of the primary summary analyses. Therefore, publication bias is highly unlikely based on the aforementioned results.
Figure 4.
Funnel plot analyses for publication bias of overall analyses. A, Dorsiflexion range-of-motion control-to-intervention comparison. B, Dorsiflexion range-of-motion preintervention-to-postintervention comparison. C, Dynamic postural control control-to-intervention comparison. D, Dynamic postural control preintervention-to-postintervention comparison.
Sensitivity Analysis
The 1-study-removed method for the DFROM preintervention-to-postintervention changes demonstrated that the overall ES remained weak and ranged from 0.32 to 0.37 (95% CI = 0.20, 0.48). All P values were greater than .001, which indicated that no single group influenced the overall summary effect. The 1-study-removed method for the DFROM control-to-intervention comparison showed that the overall ES remained moderate and ranged from 0.30 to 0.46 (95% CI = 0.14, 0.68). The P values ranged from .002 to .02; thus, it was unlikely that a single group influenced the overall summary effect.
For dynamic postural control, according to the 1-study-removed method for the preintervention-to-postintervention comparison, the overall ES remained weak and ranged from 0.15 to 0.50 (95% CI = −0.12, 0.87). Whereas all P values were greater than .05, the P value approached a difference (P = .056) when Powden et al27 was removed. Furthermore, the ES increased to 0.50, and the 95% CI narrowed (−0.01, 1.00). The 1-study-removed method for the control-to-intervention comparison indicated that the overall ES remained moderate and ranged from 0.17 to 0.52 (95% CI = −0.14, 0.98). All P values were greater than .11, reflecting a low likelihood that a single group influenced the overall summary effect.
Level of Evidence and Strength of Recommendation
We observed grade A evidence that DFROM mildly improved from preintervention to postintervention after joint mobilization. This recommendation was derived from consistent findings from 6 level 117,19,20,26,28,29 and 3 level 215,18,27 studies. For the control-to-intervention comparison, we found grade B evidence that DFROM was mildly greater in the intervention than in the control group based on consistent results from 7 level 1 studies16,17,19,20,26,28,29 and 1 level 2 study.27
Grade B evidence indicated conflicting effects of joint mobilizations on dynamic postural control from preintervention to postintervention. This recommendation was based on 2 level 119,26 and 3 level 215,18,27 studies. Lastly, we found grade B evidence for conflicting effects of joint mobilizations on dynamic postural control when compared with a control group. This recommendation was derived from 3 level 1 studies16,19,26 and 1 level 2 study.27
DISCUSSION
The purpose of this systematic review with meta-analysis was to collect, critically appraise, and synthesize the current literature in which researchers have investigated the effects of various joint-mobilization techniques on DFROM and dynamic postural control in individuals with CAI. After we critically appraised and synthesized the literature, our findings suggested that joint mobilizations may have weak to moderate positive effects on both DFROM and dynamic postural control. Grade A and B evidence supported these results, as indicated from consistent level 1 and 2 evidence.
Dorsiflexion Range of Motion
We found grade B evidence that joint mobilizations effectively increased DFROM in individuals with CAI. The magnitude of these improvements was weak to moderate in our 2 overall summary analyses. Further evaluation of the effects of mobilizations on DFROM demonstrated that both the Mulligan MWM (ES range = 0.40–0.56) and Maitland mobilization (ES range = 0.32–0.46) produced moderate effects on DFROM with CIs that did not cross 0. The sets, repetitions, and lengths of application of the Mulligan MWM and Maitland procedures varied considerably within each investigation. The Mulligan MWM applications associated with the largest ESs (range = 0.39–1.24) consisted of a minimum of 1 set of 10 repetitions.17,26 In contrast, the smaller ESs were associated with applications that included holds at end range.18,28 Positive Maitland mobilization effects were associated with protocols that included a minimum of two 2-minute sets of mobilizations.15,20 Our subanalysis of treatment length identified no differences between a single application and multiple applications. However, inspection of only the Maitland protocols suggested that multiple sessions (average ES = 0.45) may result in more robust effects than a single intervention session (average ES = 0.22). Improvements in DFROM were identified both immediately and at follow-up measurement times. These improvements lasted from 48 hours17 to 6 months26 after joint mobilization. We found limited follow-up studies, however, and more research is needed to examine how long the improvements are maintained. Lastly, using isolated talocrural-joint traction did not improve DFROM when used in isolation. This may indicate that a mobilization targeted at improving posterior glide of the talus is needed to improve DFROM in those with CAI.
Dynamic Postural Control
We found grade B evidence that joint mobilizations may moderately improve dynamic postural control in those with CAI. However, the overall summary effects were associated with CIs that crossed 0. The inconclusive summary effects may have been due to the large discrepancy in summary effects between the Mulligan MWM (ES = 0.87) and Maitland mobilizations (ES = 0.32) that indicated the Mulligan MWM led to strong improvements in dynamic postural control. Yet these results may have been highly influenced by the Cruz-Diaz et al26 investigation in which the authors cited ESs greater than 1. Differences in dynamic postural-control improvements may be due to application differences between the mobilizations. The Mulligan MWM requires the patient to actively lunge forward in a movement similar to that used to perform the SEBT or Y-Balance Test. Regardless of these differences, mobilization interventions that used multiple treatment sessions (ES range = 0.69–0.89) produced more robust improvements in dynamic postural control than single treatments (ES range = 0.30–0.51).
The findings also suggested that improvements in dynamic postural control were greater at follow up (ES range = 0.80–0.99) than immediately after application (ES range = 0.42–0.62). These results may indicate that improvements in postural control require multiple sessions and time for changes to manifest. This could be due to the need for practice and repetition for motor control and subsequent postural-control adaptions to manifest.30
Finally, researchers9 have suggested that DFROM and the anterior-reach direction of the SEBT are related. Our results indicated that the anterior-reach direction of the SEBT was least affected, and the posteromedial- and posterolateral-reach directions were the most improved, by a joint-mobilization intervention designed to increase DFROM. Increases in DFROM possibly allowed for greater freedom of movement throughout the lower extremity that led to improvements in the posteromedial and posterolateral directions of the SEBT and Y-Balance Test.8 Improvements in these directions may also stem from stimulation of mechanoreceptors and the sensory system from joint mobilizations.20 Overall, these findings indicated the need for further research examining the effects of joint mobilizations on dynamic postural control to determine the optimal treatment guidelines.
Clinical Implications
This systematic review and meta-analysis demonstrated that joint mobilizations targeted at increasing the posterior glide of the talus can improve DFROM and dynamic postural control in individuals with CAI. Despite large variations in mobilization type, dosage, treatment lengths, and assessment time, some clinical recommendations can be provided based on our findings. Maitland mobilization and Mulligan MWM that target the posterior glide of the talus and manipulations of the talocrural joint demonstrated the greatest efficacy in improving DFROM and dynamic postural control in individuals with CAI. Traction and high-velocity manipulations to the tibiofibular joints for enhancing dynamic balance and range of motion were not supported. Specifically, researchers17,26 have suggested that 1 set of 10 continuous repetitions of Mulligan MWM may be superior to protocols that include holds during the Mulligan MWM procedure. An intervention of two 2-minute sets of the Maitland grade 3 anterior-to-posterior joint mobilization has also been suggested.15,20 Furthermore, Mulligan MWM seemed to provide the greatest efficacy in improving dynamic postural control, and these improvements may take time to fully manifest. However, it is still unclear how long the initial effects last and how long it takes for improvements to fully manifest. This highlights the need for further study to determine the optimal dosage, length of effects, and potential need for maintenance interventions to sustain the effects. Given the limited research in which investigators have directly compared MWM and Maitland mobilization, examined the long-term effects of joint mobilizations, and used comparable procedures, clinicians must apply their clinical experience and patient values in combination with our findings to make the best decision for each patient with CAI.
Limitations and Future Research
Whereas we conducted this systematic review based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines, our study had limitations. Our electronic search was conducted to find articles in databases that frequently publish articles related to the effect of joint mobilizations on CAI. It is possible that articles relevant to this review were not identified and included. For this review, the goal was to assess the isolated role of joint mobilizations on DFROM and dynamic postural control in individuals with CAI. In the clinical setting, rehabilitation plans will likely include other forms of treatments: for example, stretching, massage, and strengthening. Therefore, more research is needed to examine and summarize the effects of joint mobilizations used in combination with other forms of treatment to improve the common impairments associated with CAI. Another limitation was the low number of participant groups within the subanalyses, which made it difficult to compare groups and provide strong recommendations. This concern speaks to the variability in the literature regarding treatment guidelines and the need to work toward unified mobilization procedures. Lastly, future investigators need to evaluate the effectiveness of these mobilizations in clinical populations and develop systematic ways of tracking their effects over time.
CONCLUSIONS
Our synthesis and meta-analysis of the evidence suggested that Mulligan MWM and Maitland mobilization moderately improved DFROM and dynamic postural control in individuals with CAI. Mulligan MWM and Maitland mobilization both demonstrated weak to moderate ESs, indicating improvements in DFROM. Dynamic postural control seemed to be most improved by Mulligan MWM, as Maitland mobilization demonstrated weak ESs that were associated with CIs that crossed 0. Furthermore, these improvements were identified immediately after a single intervention, after multiple treatments, and up to 6 months after completing the intervention. Further research is needed to strengthen these recommendations and investigate optimal treatment guidelines to enhance DFROM and dynamic postural control in those with CAI.
REFERENCES
- 1.Waterman BR, Belmont PJ, Jr, Cameron KL, DeBerardino TM, Owens BD. Epidemiology of ankle sprain at the United States Military Academy. Am J Sports Med. 2010;38(4):797–803. doi: 10.1177/0363546509350757. [DOI] [PubMed] [Google Scholar]
- 2.Hintermann B, Boss A, Schäfer D. Arthroscopic findings in patients with chronic ankle instability. Am J Sports Med. 2002;30(3):402–409. doi: 10.1177/03635465020300031601. [DOI] [PubMed] [Google Scholar]
- 3.van Rijn RM, van Os AG, Bernsen RM, Luijsterburg PA, Koes BW, Bierma-Zeinstra SM. What is the clinical course of acute ankle sprains? A systematic literature review. Am J Med. 2008;121(4):324–331. doi: 10.1016/j.amjmed.2007.11.018. e6. [DOI] [PubMed] [Google Scholar]
- 4.Beynnon BD, Murphy DF, Alosa DM. Predictive factors for lateral ankle sprains: a literature review. J Athl Train. 2002;37(4):376–380. [PMC free article] [PubMed] [Google Scholar]
- 5.Tyler TF, McHugh MP, Mirabella MR, Mullaney MJ, Nicholas SJ. Risk factors for noncontact ankle sprains in high school football players: the role of previous ankle sprains and body mass index. Am J Sports Med. 2006;34(3):471–475. doi: 10.1177/0363546505280429. [DOI] [PubMed] [Google Scholar]
- 6.Houston MN, Van Lunen BL, Hoch MC. Health-related quality of life in individuals with chronic ankle instability. J Athl Train. 2014;49(6):758–763. doi: 10.4085/1062-6050-49.3.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Valderrabano V, Horisberger M, Russell I, Dougall H, Hintermann B. Etiology of ankle osteoarthritis. Clin Orthop Relat Res. 2009;467(7):1800–1806. doi: 10.1007/s11999-008-0543-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hoch MC, Farwell KE, Gaven SL, Weinhandl JT. Weight-bearing dorsiflexion range of motion and landing biomechanics in individuals with chronic ankle instability. J Athl Train. 2015;50(8):833–839. doi: 10.4085/1062-6050-50.5.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hoch MC, Staton GS, McKeon PO. Dorsiflexion range of motion significantly influences dynamic balance. J Sci Med Sport. 2011;14(1):90–92. doi: 10.1016/j.jsams.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 10.Wikstrom EA, Hubbard TJ. Talar positional fault in persons with chronic ankle instability. Arch Phys Med Rehabil. 2010;91(8):1267–1271. doi: 10.1016/j.apmr.2010.04.022. [DOI] [PubMed] [Google Scholar]
- 11.Grindstaff TL, Dolan N, Morton SK. Ankle dorsiflexion range of motion influences Lateral Step Down Test scores in individuals with chronic ankle instability. Phys Ther Sport. 2017;23:75–81. doi: 10.1016/j.ptsp.2016.07.008. [DOI] [PubMed] [Google Scholar]
- 12.Basnett CR, Hanish MJ, Wheeler TJ, et al. Ankle dorsiflexion range of motion influences dynamic balance in individuals with chronic ankle instability. Int J Sports Phys Ther. 2013;8(2):121–128. [PMC free article] [PubMed] [Google Scholar]
- 13.Gribble PA, Hertel J, Plisky P. Using the Star Excursion Balance Test to assess dynamic postural-control deficits and outcomes in lower extremity injury: a literature and systematic review. J Athl Train. 2012;47(3):339–357. doi: 10.4085/1062-6050-47.3.08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Munn J, Sullivan SJ, Schneiders AG. Evidence of sensorimotor deficits in functional ankle instability: a systematic review with meta-analysis. J Sci Med Sport. 2010;13(1):2–12. doi: 10.1016/j.jsams.2009.03.004. [DOI] [PubMed] [Google Scholar]
- 15.Hoch MC, Andreatta RD, Mullineaux DR, et al. Two-week joint mobilization intervention improves self-reported function, range of motion, and dynamic balance in those with chronic ankle instability. J Orthop Res. 2012;30(11):1798–1804. doi: 10.1002/jor.22150. [DOI] [PubMed] [Google Scholar]
- 16.Hoch MC, McKeon PO. Joint mobilization improves spatiotemporal postural control and range of motion in those with chronic ankle instability. J Orthop Res. 2011;29(3):326–332. doi: 10.1002/jor.21256. [DOI] [PubMed] [Google Scholar]
- 17.Marrón-Gómez D, Rodríguez-Fernández ÁL, Martín-Urrialde JA. The effect of two mobilization techniques on dorsiflexion in people with chronic ankle instability. Phys Ther Sport. 2015;16(1):10–15. doi: 10.1016/j.ptsp.2014.02.001. [DOI] [PubMed] [Google Scholar]
- 18.Gilbreath JP, Gaven SL, Van Lunen BL, Hoch MC. The effects of mobilization with movement on dorsiflexion range of motion, dynamic balance, and self-reported function in individuals with chronic ankle instability. Man Ther. 2014;19(2):152–157. doi: 10.1016/j.math.2013.10.001. [DOI] [PubMed] [Google Scholar]
- 19.Harkey M, McLeod M, Van Scoit A, et al. The immediate effects of an anterior-to-posterior talar mobilization on neural excitability, dorsiflexion range of motion, and dynamic balance in patients with chronic ankle instability. J Sport Rehabil. 2014;23(4):351–359. doi: 10.1123/jsr.2013-0085. [DOI] [PubMed] [Google Scholar]
- 20.McKeon PO, Wikstrom EA. Sensory-targeted ankle rehabilitation strategies for chronic ankle instability. Med Sci Sports Exerc. 2016;48(5):776–784. doi: 10.1249/MSS.0000000000000859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moher D, Liberati A, Tetzlaff J, Altman D, PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Maher CG, Sherrington C, Herbert RD, Moseley AM, Elkins M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003;83(8):713–721. [PubMed] [Google Scholar]
- 23.Cohen J. Statistical Power Analysis for the Behavioral Sciences 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates;; 1988. [Google Scholar]
- 24.Mavridis D, Salanti G. Exploring and accounting for publication bias in mental health: a brief overview of methods. Evid Based Ment Health. 2014;17(1):11–15. doi: 10.1136/eb-2013-101700. [DOI] [PubMed] [Google Scholar]
- 25.Ebell MH, Siwek J, Weiss BD, et al. Strength of recommendation taxonomy (SORT): a patient-centered approach to grading evidence in the medical literature. J Am Board Fam Pract. 2004;17(1):59–67. doi: 10.3122/jabfm.17.1.59. [DOI] [PubMed] [Google Scholar]
- 26.Cruz-Díaz D, Lomas Vega R, Osuna-Pérez MC, Hita-Contreras F, Martínez-Amat A. Effects of joint mobilization on chronic ankle instability: a randomized controlled trial. Disabil Rehabil. 2015;37(7):601–610. doi: 10.3109/09638288.2014.935877. [DOI] [PubMed] [Google Scholar]
- 27.Powden CJ, Hogan KK, Wikstrom EA, Hoch MC. The effect of two forms of talocrural joint traction on dorsiflexion range of motion and postural control in those with chronic ankle instability. J Sport Rehabil. 2017;26(3):239–244. doi: 10.1123/jsr.2015-0152. [DOI] [PubMed] [Google Scholar]
- 28.Vicenzino B, Branjerdporn M, Teys P, Jordan K. Initial changes in posterior talar glide and dorsiflexion of the ankle after mobilization with movement in individuals with recurrent ankle sprain. J Orthop Sports Phys Ther. 2006;36(7):464–471. doi: 10.2519/jospt.2006.2265. [DOI] [PubMed] [Google Scholar]
- 29.Beazell JR, Grindstaff TL, Sauer LD, Magrum EM, Ingersoll CD, Hertel J. Effects of a proximal or distal tibiofibular joint manipulation on ankle range of motion and functional outcomes in individuals with chronic ankle instability. J Orthop Sports Phys Ther. 2012;42(2):125–134. doi: 10.2519/jospt.2012.3729. [DOI] [PubMed] [Google Scholar]
- 30.Levin MF, Weiss PL, Keshner EA. Emergence of virtual reality as a tool for upper limb rehabilitation: incorporation of motor control and motor learning principles. Phys Ther. 2015;95(3):415–425. doi: 10.2522/ptj.20130579. [DOI] [PMC free article] [PubMed] [Google Scholar]