Abstract
OBJECTIVE:
Mood disorders lead to significant functional impairment and are the costliest conditions for health plans. Few individuals with mood disorders have access to evidence-based Collaborative Chronic Care Models (CCMs) because most are seen in small-group practices (<20 providers) with limited capacity to deliver CCMs. In this single-bling randomized controlled trial, we determined whether a CCM delivered nationally in a U.S. health plan improved 12-month outcomes compared to usual care among enrollees with mood disorders.
METHODS:
Aetna insurance enrollees (N=238, mean age=41.1 years, 66.1% female) recently hospitalized for unipolar major depression or bipolar disorder provided informed consent, completed baseline assessments, and were randomized to usual care or CCM. The CCM included 10 sessions of the Life Goals self-management program and brief contacts to determine symptom status, delivered by phone by a Care Manager. Primary outcomes were changes in depression symptoms (Patient Health Questionnaire-PHQ-9) and mental health-related quality of life (Short Form-SF-12-item score) in 12 months.
RESULTS:
Participants receiving CCM had significantly lower adjusted mean PHQ-9 scores by −2.34 (95% CL=−4.18, −0.50, p=0.01) and higher adjusted mean SF-12 mental health scores by 3.21 (95% CL=−0.97, 7.38. p=0.10) versus usual care.
CONCLUSIONS:
Individuals receiving CCM compared to usual care had improved clinical outcomes, although substantial attrition may limit impact of health plan-level delivery of CCMs. Further research on the use of health plan-level interventions such as CCMs as alternatives to practice-based models is warranted.
Keywords: Depression, Bipolar disorder, Care management, Health plans, Population health
BACKGROUND
One in five individuals in the United States suffers from a mood disorder (unipolar major depression or bipolar disorder)1,2, resulting in increased risk of long–term medical conditions3 and premature mortality4 including suicide.5 Up to 70% of treatment costs for mood disorders are outside the mental health sector, notably in primary care.6 In privately insured populations, mood disorders represent the most expensive conditions, with bipolar disorder incurring the most health care costs7. Effective treatments for mood disorders include psychosocial interventions in addition to medications; yet only 40% of individuals with mood disorders receive adequate treatment.2
Collaborative chronic care models (CCMs), which provide ongoing psychosocial support in conjunction with treatment coordination have demonstrated improved outcomes for persons with mood disorders at little to no net healthcare cost.8-10 Recent meta-analyses8,11 found that implementation of at least three core components of the CCM (e.g., self-management, care management, clinical information systems/case-finding) resulted in improved mental and physical outcomes for persons with mental disorders, at little to no net health care costs. Often implemented by care managers, CCMs also support healthcare delivery systems that are subject to bundled payments and shared savings under health care reform,12-14 and medical home mandates.15,16 However, CCMs for mood disorders have primarily been implemented in large, integrated health care systems that have the capacity to hire on-site care managers, and can scale up the necessary tools including clinical information systems.16-18 In contrast, over 90% of U.S. commercial health plan enrollees receive care from small practices (defined as <20 primary care physicians),16,19 which do not have the capacity to hire care managers at each site to provide CCM core components.
Another option is to implement CCMs remotely at the health plan level, as opposed to the individual practice level, which may allow for their further implementation and sustainability across patients who are seen in solo or small group practices. A key advantage of health plan-level implementation is an “economy of scale” through the deployment of virtual care managers and use of common information technologies.20 However, prior studies implementing CCMs at the population level have been limited to unipolar depression treatment21,22 in involving large practices.23,24
This article reports outcomes following intervention from a randomized trial at the health plan level of a CCM delivered across mood disorders (depression or bipolar disorder). Our primary hypothesis was that compared to those receiving usual care, patients in the U.S. recently hospitalized for a mood disorder receiving the plan level CCM have reduced 12-month depressive symptoms (Patient Health Questionnaire-PHQ-9) and improved mental health-related quality of life (Short Form 12-item survey-SF-12).
METHODS
This single-blind randomized controlled effectiveness trial included patients from Aetna health plan who were randomized to receive either the CCM for mood disorders delivered at the health plan level or usual care. Aetna health plan is one of the largest healthcare insurers in the country, serving approximately 12 million covered lives, with 244,971 providers.19 Over 90% of Aetna health plan enrollees receive care from primary or mental health practices with <20 physicians.19
Participants
Described in detail previously,25 eligible patients included Aetna health plan enrollees (beneficiaries or family members of beneficiaries) identified from Aetna claims data from across the lower 48 United States who were ages 21 or older and who had been recently hospitalized (past 6 months) for unipolar major depression or bipolar disorder (bipolar manic or depressed state). We chose recent hospitalization as the inclusion criterion because inpatient care indicates greater clinical severity that could benefit from CCMs.26 The study received Institutional Review Board (IRB) approval from local IRBs, and all patient participants provided verbal informed consent. Prior to randomization, participants were approached, consented, and enrolled by phone by the Aetna Care Manager, who used claims data on recent inpatient hospitalization history to identify potential participants. Recruitment began July, 2014 and ended July, 2015; follow-up assessments continued through July, 2017.
The Care Manager contacted participants by phone to confirm eligibility and enroll participants. The Care Manager was trained by study staff in CCM procedures, assessments, and human subjects protection using established CCM-based protocols.27 Participants were ineligible if they were no longer enrolled in Aetna health plan, deceased, or were unable to provide informed consent due to unstable condition, inpatient status, or unable to communicate in English.
Randomization
The study analyst randomized participants to CCM or usual care using a computer-generated algorithm stratified by diagnosis at hospitalization discharge (unipolar disorder/bipolar disorder). The allocation sequence was concealed from recruiters until interventions were assigned. Those randomized to the usual care arm received standard care from their practice provider, but none of the CCM components from the Care Manager.
Intervention
Patients randomized to the CCM received contacts and psychosocial intervention the Aetna Care Manager in addition to their usual care from their provider. The Care Manager, trained as a masters in clinical social work delivered the CCM intervention over a six-month period, which included the following core components: clinical information systems (Aetna clinical database to track and initially contact potentially eligible patients), self-management support (10 weekly sessions by phone), and ongoing care management.8,10,11 The self-management sessions were adapted from the evidence-based Life Goals program,27-31 a psychosocial intervention shown to improve outcomes for those with unipolar depression or bipolar disorder28,30,32-34 that focuses on symptom coping strategies to reduce stigma and promote wellness goals. Ongoing care management included up to 6 monthly brief contacts to determine status and symptoms. Fidelity to the CCM was supported through a 2-day training session for the Care Manager, as well as regular calls with the Care Manager to review session content and progress with patient contacts.27
Participants from both treatment arms who experience imminent risk (e.g., suicidal or assaultive ideation) were managed via protocols used in prior CCM studies25,27. The Care Manager and Research Assistant were trained to handle participants with suicidal ideation and were instructed to contact their providers on an as needed basis.
Data Collection and Outcomes
Thirty-minute baseline, 6-, and 12-month follow-up assessments included primary outcome measures and covariates. Baseline assessments were ascertained by the Care Manager at the time of enrollment, and included demographic information, health status, and baseline measures for primary outcomes. Follow-up assessments were conducted by a study Research Assistant not employed by Aetna, who was blinded to the patients’ randomization allocation status, and included follow-up measures of primary outcomes. Twelve-month assessments of clinical outcomes were included in order to assess durability of the 6-month CCM program.
The primary outcomes were changes in depressive symptoms based on the 9-item Patient Health Questionnaire (PHQ-9), a widely-used assessment of depressive symptoms35 and the mental health component score based on the Short-Form (SF) 12-item health-related quality of life survey.36 The PHQ-9 was chosen because depression symptoms are also a significant burden among individuals with bipolar disorder.
Covariate information ascertained from assessments included demographics (age, sex, race/ethnicity, education, employment status, living alone) and health behaviors including hazardous drinking (Alcohol Use Disorders Identification survey item on having 6 or more drinks on a single occasion within the past month),37 illicit drug use, and smoking. Other covariates ascertained from Aetna claims data included enrollment status (beneficiary versus family member) and primary mental health diagnosis (bipolar disorder or major depression).
Analyses
Primary clinical outcomes (change in PHQ-9 and SF-12 mental component summary (MCS) scores) were modeled using mixed effects models with random intercepts and baseline values of the outcome (at randomization), treatment arm indicator, time as a 12-month indicator, and the interaction of treatment arm by time as predictors. The interaction term was included to explore if the outcomes changed between 6 to 12 months.
Missing data patterns were explored, and to account for possible missing patterns and identify any relationship to outcomes or treatment arm, multivariable logistic regression models were run on dichotomous variables created to represent each missing pattern as a function of baseline patient characteristics, each outcome, and treatment arm. The final primary clinical outcomes models used multiple imputation methods. Variables employed in the imputation were empirically driven based on the association between the variables to be imputed and auxiliary variables, and included all model covariates, treatment indicators, and missing data pattern indicators. Twenty datasets were imputed, and results were pooled according to Rubin’s rule of combining datasets.38
RESULTS
A total of 9,121 potentially eligible patients from the Aetna database were identified using clinical information systems as having a diagnosis of unipolar depression or bipolar disorder from an inpatient discharge within 6 months. Of the 9,121, 7,335 were deemed to be ineligible (note <21 years old, not living within the 48 contiguous U.S., no longer covered by Aetna), leaving 1,786 potentially eligible patients. Of the 1,786 approached, 403 declined to participate, 999 could not be reached, and 104 were determined to be ineligible after approached. Out of the 238 enrolled, 115 were randomized at baseline to receive the CCM and 123 to usual care (see CONSORT Diagram in the online supplement. Based on the actual sample size of 73 (69% dropout), the resultant power to detect mean differences between treatment arm was 27% for Cohen’s d = 0.25 for PHQ-9 and 19% for Cohen’s d = 0.20 for SF-12 MCS scores.
At baseline, respondents (mean age=41, 65.5% female, 81.1% white, 58.4% employed) had a mean PHQ-9 score of 12.7±6.6, and a mean SF-12 MCS score of 35.6±15.2 (Table 1). Among those randomized to the CCM, the mean number of self-management sessions completed was 8/4 (±2.7) and the mean number of care management contacts was 4.7 (SD±2.6).
Table 1:
Baseline Factors and Outcomes among Enrollees Hospitalized with Depression or Bipolar Disorder
| Overall (N=238) |
Collaborative Care Model (N=115) |
Usual Care (N=123) |
||||
|---|---|---|---|---|---|---|
| Characteristics* | N | % | N | % | N | % |
| Primary enrollee (vs. family member) | 140 | 59 | 72 | 63 | 68 | 55 |
| Practice size: <20 providers | 197 | 87 | 97 | 89 | 100 | 86 |
| Female | 156 | 66 | 77 | 67 | 79 | 64 |
| White | 193 | 81 | 99 | 86 | 94 | 76 |
| College – any | 168 | 71 | 75 | 65 | 93 | 76 |
| Employed | 139 | 58 | 70 | 61 | 69 | 56 |
| Live alone | 53 | 22 | 30 | 26 | 12 | 19 |
| Alcohol use (Hazardous drinking)† | 66 | 28 | 34 | 30 | 32 | 26 |
| Other Substance use | 40 | 17 | 17 | 15 | 23 | 19 |
| Current Smoker | 69 | 29 | 38 | 33 | 31 | 25 |
| Primary diagnosis: | ||||||
| Major depression | 156 | 66 | 76 | 66 | 80 | 65 |
| Bipolar disorder | 82 | 35 | 39 | 34 | 43 | 35 |
| Mean± SD | Mean ± SD | Mean ± SD | ||||
| Age, years, mean ± standard deviation (SD) | 41.3 ± 13.1 | 42.8 ± 12.9 | 39.9 ± 13.2 | |||
| PHQ-9, mean ± standard deviation (SD) ‡ | 12.7 ± 6.6 | 13.0 ± 7.1 | 12.4 ± 6.1 | |||
| HRQOL SF-12, mean ±standard deviation§ | ||||||
| MCS | 35.6 ± 15.2 | 36.9 ± 15.3 | 34.4 ± 15.2 | |||
| PCS | 48.6 ± 13.2 | 47.2 ± 13.5 | 49.8 ± 12.7 | |||
% =percentage
None of the comparisons between CCM and usual care groups were statistically significant
Hazardous drinking was based on self-reported AUDIT-C (alcohol use disorders Identification test) which inquires about having 6 or more drinks on a single occasion within the past month. This was dichotomized as 0=no and 1=yes.
PHQ-9 (Patient Health Questionnaire, 9-item) ranges from 0-27, with higher scores indicating worse depressive symptoms.
Health-related quality of life (HRQOL) Short form (SF-12) includes a mental health component (MCS) and a physical health component (PCS). Each uses normed-based scoring derived from the general population, set to have a mean of 50 and standard deviation of 10 (range: 0-100). Higher scores indicate greater quality of life
Analyses of missingness pattern revealed an association between treatment arm and time of dropout, with earlier (6-months) dropout more likely for CCM (60.9%) than usual care (37.4%), while later dropout (by 12-months) more likely in usual care (28.5%) than CCM (12.2%). Indicators representing time of dropout (6- or 12-months) were included in the imputation process. By 12 months, lost coverage was the reason for dropout in more than 80% of participants who dropped out, which did not differ by study group.
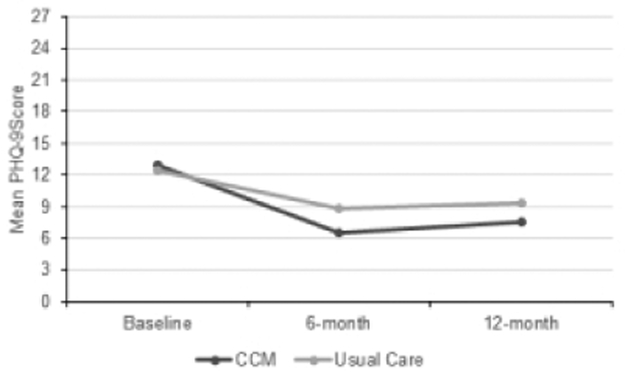
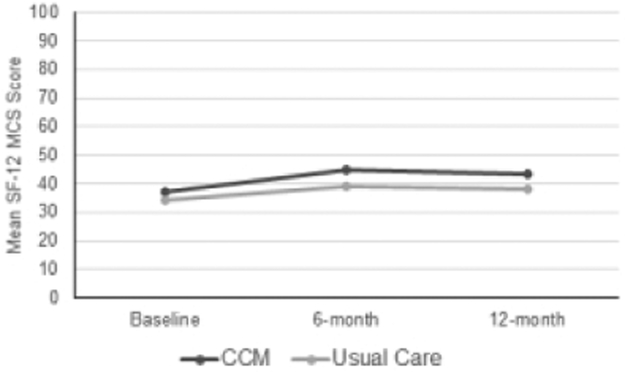
Figure 1 presents the unadjusted means of main outcomes at each assessment times for PHQ-9 and SF-12 MCS scores, demonstrating that the changes mainly occurred between baseline and 6 months. The final models did not include the interaction term as it was neither meaningfully nor statistically significant.
Figure 1: Mean Depression Symptom and Mental Health Quality of Life Scores by Treatment Arm Across Time (N=73).
The first figure enables the reader to see the unadjusted scores of depression symptoms (PHQ-9) by treatment arm across time. Higher scores reflect worse depression symptoms. The second figure enables the reader to see the unadjusted scores of mental health quality of life (SF-12 MCS) treatment arm across time. Higher scores reflect better quality of life.
Based on the model fit with main effects of 12-month indicator and treatment group (CCM) indicator, patients randomized to receive the CCM had an overall lower adjusted mean in PHQ-9 score by −2.34 (SE=0.92, 95% CL: −4.18, −0.50; P=0.004) compared to those randomized to receive usual care. Although not statistically significant, patients randomized to receive the CCM had on a higher (better quality of life) adjusted mean SF-12 MCS scores by 3.21 (SE=2.09, 95% CL: −0.97, 7.38; P=0.10) than those randomized to usual care.
Similar results were obtained from fitting the model to each outcome with an interaction term of time by treatment, where interaction terms were not significant for both outcomes (see Supplemental Appendix).
DISCUSSION
We describe 12-month results from, what is to our knowledge, the first study to implement a Collaborative Chronic Care Model (CCM) within a nationwide commercial health plan for patients hospitalized for unipolar depression or bipolar disorder. We found that after randomization, patients receiving CCM had less reported depression symptoms and a trend toward more improvement in mental health quality of life. Despite having private insurance, study participants reported substantial impairment in mental health quality of life (i.e., average 15-point lower score on the SF-12 mental health component score compared to the general population.36
The observed effects we found in this study of reduced mood disorder symptoms among patients randomized to CCM compared to usual care are reflective of prior studies that focused on those with major depression or bipolar disorder.8 The study also adds to the growing body of literature on the effectiveness of collaborative care on improving mental health outcomes across age groups22 and mental health conditions22,39-42 reflecting the potential for a more cost-efficient approach to providing evidence-based care remotely to patients without access to on-site CCMs.
CCMs to date have primarily been implemented solely for unipolar depression21,26,43-46 or within large integrated health systems which, unlike solo or small group primary care practices, have sufficient infrastructure to mount such integrated efforts. Implementing CCMs in health plans across mood disorders represent important efforts to overcome such geographic and administrative barriers.31 Most commercially insured individuals receive care from network-model health plans and within small practices, which have limited capacity to provide organized CCM/disease management interventions.16,19,11. CCMs that address the range of mood disorders including bipolar disorder might be able to address suicide notably through the reduction of depressive symptoms.47
There are several limitations to this study that warrant consideration. Only a fraction of potentially eligible patients was enrolled. Participants may have been less inclined to engage in a program when the offer came from an insurer rather than a care provider. Moreover, those who were recently hospitalized, especially from more rural settings, could be an especially difficult population to reach or engage21. Post-randomization dropout was also substantial; the primary reason for subject dropout was disenrollment from Aetna coverage, as enrollment in Aetna was a study inclusion criterion. While we did not have information on reasons for Aetna coverage change, loss of coverage can be triggered by changes in employer/employment status or premium increases.48 Evidence suggests that about half of Americans switch health plans within three years.49 Moreover, the Care Manager had limited contact with the patients’ providers, limiting their ability to help manage pharmacotherapy for patients; however, the Life Goals program was demonstrated to be effective as a stand-alone self-management program in previous trials.30,34 While the research assistant made every effort to follow up with patients using a brief survey, lack of available contact information once the individual dis-enrolled from the health plan and availability of subject compensation for surveys may have contributed to follow-up attrition. We also used multiple imputations to account for the high rate of loss at 12 months, however, the method is limited by the number of available variables to impute and does not solve the issue that the remaining participants may be highly selected. In addition, while this study employed the core components of the CCM found to be effective from previous meta-analyses (self-management, care management, clinical information systems)8,11, we were unable to fully implement provider clinical decision support in regards to mood disorders medication management across the multiple practices. Finally, while the study incorporated well-established clinical outcomes measures, clinical outcomes were self-reported.
CONCLUSIONS
Overall findings from this study indicate that health plan-level CCMs are effective in reducing depressive symptoms and improving health-related quality of life for a cross-diagnosis group of individuals with mood disorders (depression, bipolar disorder). However, protocol drop-out rates, primarily due to low initial acceptance of a health-plan level intervention and instability of health plan enrollment, mitigate the certainty of these conclusions, as well as the willingness of commercial insurers to invest in such plan-level interventions. Nonetheless, delivery of CCMs at the health plan level may be the sole approach to extend these evidence-based interventions to patients with mood disorders who are managed in venues likely too small to implement CCMs on-site. Additional methods to enhance implementation at the health plan level that warrant further investigation include virtual tools for the Care Manager to engage with the patients’ principle care providers, especially within small practices, additional mobile health or web-based programs39,50 for providers and patients to extend care coordination and self-management, and use of other implementation strategies such as practice-based facilitation or performance incentives.51 Ultimately, a health plan-based virtual CCM intervention is a potentially cost-efficient approach to delivering this evidence-based practice at the population level.
Supplementary Material
HIGHLIGHTS.
Mood disorders affect one in five individuals yet less than half receive adequate treatment due to the limited capacity of many practices in providing effective collaborative care models.
This randomized trial determined whether a health plan-level collaborative care model improved mental health outcomes for individuals with mood disorders.
Individuals hospitalized for unipolar major depression or bipolar disorder enrolled in a large national health plan were randomized to receive either the collaborative care model (self-management sessions and care management) by telephone, or usual care.
Compared to usual care, those receiving the collaborative care model had lower overall depression symptoms and potentially improved mental health quality of life in 12 months.
DISCLOSURES and ACKNOWLEDGEMENTS
Dr. Bauer receives royalties from Springer, and Drs. Bauer and Kilbourne receive royalties from New Harbinger Publishing for manuals related to the intervention. Dr. Un is employed by Aetna. The other authors report no financial relationships with commercial interests.
This research was supported by the U.S. Agency for Healthcare Research and Quality (R18 HS 21425). The funder (Agency for Healthcare Research and Quality) had no role in the data acquisition, analysis, or in the review or writing of this manuscript.
The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
Footnotes
Trial registration: ClinicalTrials.gov Identifier: NCT02041962; Registered January 3, 2014
References
- 1.Judd LL, Akiskal HS. The prevalence and disability of bipolar spectrum disorders in the US population: re-analysis of the ECA database taking into account subthreshold cases. Journal of affective disorders. 2003;73(1-2):123–131. [DOI] [PubMed] [Google Scholar]
- 2.Kessler RC, Wang PS. The descriptive epidemiology of commonly occurring mental disorders in the United States. Annual review of public health. 2008;29:115–129. [DOI] [PubMed] [Google Scholar]
- 3.Katon WJ, Lin EH, Von Korff M, et al. Collaborative care for patients with depression and chronic illnesses. The New England journal of medicine. 2010;363(27):2611–2620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA psychiatry. 2015;72(4):334–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ilgen MA, Bohnert AS, Ignacio RV, et al. Psychiatric diagnoses and risk of suicide in veterans. Archives of general psychiatry. 2010;67(11):1152–1158. [DOI] [PubMed] [Google Scholar]
- 6.Dilsaver SC. An estimate of the minimum economic burden of bipolar I and II disorders in the United States: 2009. Journal of affective disorders. 2011;129(1-3):79–83. [DOI] [PubMed] [Google Scholar]
- 7.Williams MD, Shah ND, Wagie AE, Wood DL, Frye MA. Direct costs of bipolar disorder versus other chronic conditions: an employer-based health plan analysis. Psychiatric services. 2011;62(9):1073–1078. [DOI] [PubMed] [Google Scholar]
- 8.Woltmann E, Grogan-Kaylor A, Perron B, Georges H, Kilbourne AM, Bauer MS. Comparative effectiveness of collaborative chronic care models for mental health conditions across primary, specialty, and behavioral health care settings: systematic review and meta-analysis. The American journal of psychiatry. 2012;169(8):790–804. [DOI] [PubMed] [Google Scholar]
- 9.Gilbody S, Bower P, Fletcher J, Richards D, Sutton AJ. Collaborative care for depression: a cumulative meta-analysis and review of longer-term outcomes. Archives of internal medicine. 2006;166(21):2314–2321. [DOI] [PubMed] [Google Scholar]
- 10.Coleman K, Austin BT, Brach C, Wagner EH. Evidence on the Chronic Care Model in the new millennium. Health affairs. 2009;28(1):75–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Miller CJ, Grogan-Kaylor A, Perron BE, Kilbourne AM, Woltmann E, Bauer MS. Collaborative chronic care models for mental health conditions: cumulative meta-analysis and metaregression to guide future research and implementation. Medical care. 2013;51(10):922–930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fisher ES, McClellan MB, Bertko J, et al. Fostering accountable health care: moving forward in medicare. Health affairs. 2009;28(2):w219–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Barnes AJ, Unruh L, Chukmaitov A, van Ginneken E. Accountable care organizations in the USA: types, developments and challenges. Health policy (Amsterdam, Netherlands). 2014; 118(1):1–7. [DOI] [PubMed] [Google Scholar]
- 14.Shortell SM, Casalino LP. Implementing qualifications criteria and technical assistance for accountable care organizations. Jama. 2010;303(17):1747–1748. [DOI] [PubMed] [Google Scholar]
- 15.Nutting PA, Miller WL, Crabtree BF, Jaen CR, Stewart EE, Stange KC. Initial lessons from the first national demonstration project on practice transformation to a patient-centered medical home. Annals of family medicine. 2009;7(3):254–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rittenhouse DR, Casalino LP, Shortell SM, et al. Small and medium-size physician practices use few patient-centered medical home processes. Health affairs. 2011;30(8):1575–1584. [DOI] [PubMed] [Google Scholar]
- 17.Rittenhouse DR, Shortell SM, Gillies RR, et al. Improving chronic illness care: findings from a national study of care management processes in large physician practices. Medical care research and review : MCRR 2010;67(3):301–320. [DOI] [PubMed] [Google Scholar]
- 18.Unutzer J, Katon W, Callahan CM, et al. Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. Jama. 2002;288(22):2836–2845. [DOI] [PubMed] [Google Scholar]
- 19.Bauer MS, Leader D, Un H, Lai Z, Kilbourne AM. Primary care and behavioral health practice size: the challenge for health care reform. Medical care. 2012;50(10):843–848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Peterson TA, Bernstein SJ, Spahlinger DA. Population Health: A New Paradigm for Medicine. The American journal of the medical sciences. 2016;351(1):26–32. [DOI] [PubMed] [Google Scholar]
- 21.Fortney JC, Enderle MA, Clothier JL, Otero JM, Williams JS, Pyne JM. Population level effectiveness of implementing collaborative care management for depression. General hospital psychiatry. 2013;35(5):455–460. [DOI] [PubMed] [Google Scholar]
- 22.Maust DT, Mavandadi S, Benson A, et al. Telephone-based care management for older adults initiated on psychotropic medication. International journal of geriatric psychiatry. 2013;28(4):410–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Simon GE, Ludman EJ, Operskalski BH. Randomized trial of a telephone care management program for outpatients starting antidepressant treatment. Psychiatric services. 2006;57(10):1441–1445. [DOI] [PubMed] [Google Scholar]
- 24.Simon GE, Ludman EJ, Rutter CM. Incremental benefit and cost of telephone care management and telephone psychotherapy for depression in primary care. Archives of general psychiatry. 2009;66(10):1081–1089. [DOI] [PubMed] [Google Scholar]
- 25.Kilbourne AM, Nord KM, Kyle J, et al. Randomized controlled trial of a health plan-level mood disorders psychosocial intervention for solo or small practices. BMC psychology. 2014;2(1):48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rollman BL, Belnap BH, LeMenager MS, et al. Telephone-delivered collaborative care for treating post-CABG depression: a randomized controlled trial. Jama. 2009;302(19):2095–2103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bauer MS, McBride L, Williford WO, et al. Collaborative care for bipolar disorder: part I. Intervention and implementation in a randomized effectiveness trial. Psychiatric services. 2006;57(7):927–936. [DOI] [PubMed] [Google Scholar]
- 28.Bauer MS, McBride L, Williford WO, et al. Collaborative care for bipolar disorder: Part II. Impact on clinical outcome, function, and costs. Psychiatric services. 2006;57(7):937–945. [DOI] [PubMed] [Google Scholar]
- 29.Simon GE, Ludman EJ, Bauer MS, Unutzer J, Operskalski B. Long-term effectiveness and cost of a systematic care program for bipolar disorder. Archives of general psychiatry. 2006;63(5):500–508. [DOI] [PubMed] [Google Scholar]
- 30.Kilbourne AM, Li D, Lai Z, Waxmonsky J, Ketter T. Pilot randomized trial of a cross-diagnosis collaborative care program for patients with mood disorders. Depression and anxiety. 2013;30(2):116–122. [DOI] [PubMed] [Google Scholar]
- 31.Bauer MS, Krawczyk L, Tuozzo K, et al. Implementing and Sustaining Team-Based Telecare for Bipolar Disorder: Lessons Learned from a Model-Guided, Mixed Methods Analysis. Telemedicine journal and e-health : the official journal of the American Telemedicine Association. 2018;24(1):45–53. [DOI] [PubMed] [Google Scholar]
- 32.Kilbourne AM, Post EP, Nossek A, Drill L, Cooley S, Bauer MS. Improving medical and psychiatric outcomes among individuals with bipolar disorder: a randomized controlled trial. Psychiatric services. 2008;59(7):760–768. [DOI] [PubMed] [Google Scholar]
- 33.Kilbourne AM, Goodrich DE, Lai Z, et al. Randomized controlled trial to assess reduction of cardiovascular disease risk in patients with bipolar disorder: the Self-Management Addressing Heart Risk Trial (SMAHRT). The Journal of clinical psychiatry. 2013;74(7):e655–662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kilbourne AM, Barbaresso MM, Lai Z, et al. Improving Physical Health in Patients With Chronic Mental Disorders: Twelve-Month Results From a Randomized Controlled Collaborative Care Trial. The Journal of clinical psychiatry. 2017;78(1):129–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. Journal of general internal medicine. 2001;16(9):606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ware J Jr., , Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Medical care. 1996;34(3):220–233. [DOI] [PubMed] [Google Scholar]
- 37.Dawson DA, Grant BF, Stinson FS. The AUDIT-C: screening for alcohol use disorders and risk drinking in the presence of other psychiatric disorders. Comprehensive psychiatry. 2005;46(6):405–416. [DOI] [PubMed] [Google Scholar]
- 38.D. R. Multiple imputation for non-response in surveys. Wiley, New York, NY: 1987. [Google Scholar]
- 39.Fortney JC, Pyne JM, Kimbrell TA, et al. Telemedicine-based collaborative care for posttraumatic stress disorder: a randomized clinical trial. JAMA psychiatry. 2015;72(1):58–67. [DOI] [PubMed] [Google Scholar]
- 40.Meredith LS, Eisenman DP, Han B, et al. Impact of Collaborative Care for Underserved Patients with PTSD in Primary Care: a Randomized Controlled Trial. Journal of general internal medicine. 2016;31(5):509–517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Grubbs KM, Fortney JC, Pyne J, Mittal D, Ray J, Hudson TJ. A Comparison of Collaborative Care Outcomes in Two Health Care Systems: VA Clinics and Federally Qualified Health Centers. Psychiatric services. 2018;69(4):431–437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gerlach LB, Mavandadi S, Maust DT, Streim JE, Oslin DW. Improving Access to Collaborative Behavioral Health Care for Rural-Dwelling Older Adults. Psychiatric services. 2018;69(1): 117–120. [DOI] [PubMed] [Google Scholar]
- 43.Gilbody S, Lewis H, Adamson J, et al. Effect of Collaborative Care vs Usual Care on Depressive Symptoms in Older Adults With Subthreshold Depression: The CASPER Randomized Clinical Trial. Jama. 2017;317(7):728–737. [DOI] [PubMed] [Google Scholar]
- 44.Solberg LI, Crain AL, Maciosek MV, et al. A stepped-wedge evaluation of an initiative to spread the collaborative care model for depression in primary care. Annals of family medicine. 2015;13(5):412–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mavandadi S, Benson A, DiFilippo S, Streim JE, Oslin D. A Telephone-Based Program to Provide Symptom Monitoring Alone vs Symptom Monitoring Plus Care Management for Late-Life Depression and Anxiety: A Randomized Clinical Trial. JAMA psychiatry. 2015;72(12):1211–1218. [DOI] [PubMed] [Google Scholar]
- 46.Richardson LP, Ludman E, McCauley E, et al. Collaborative care for adolescents with depression in primary care: a randomized clinical trial. Jama. 2014;312(8):809–816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ilgen MA, Czyz EK, Welsh DE, Zeber JE, Bauer MS, Kilbourne AM. A collaborative therapeutic relationship and risk of suicidal ideation in patients with bipolar disorder. Journal of affective disorders. 2009;115(1-2):246–251. [DOI] [PubMed] [Google Scholar]
- 48.Claxton G, Rae M, Panchal N, Whitmore H, Damico A, Kenward K. Health benefits in 2014: stability in premiums and coverage for employer-sponsored plans. Health affairs. 2014;33(10):1851–1860. [DOI] [PubMed] [Google Scholar]
- 49.Partners F. Finn Partners National Survey Reveals How Fragmented Health System Places Greater Burden On Patients. PR Newswire [website]. 2016; https://www.prnewswire.com/news-releases/finn-partners-national-survey-reveals-how-fragmented-health-system-places-greater-burden-on-patients-300217167.html. [Google Scholar]
- 50.Rollman BL, Herbeck Belnap B, Abebe KZ, et al. Effectiveness of Online Collaborative Care for Treating Mood and Anxiety Disorders in Primary Care: A Randomized Clinical Trial. JAMA psychiatry. 2018;75(1):56–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Powell BJ, Waltz TJ, Chinman MJ, et al. A refined compilation of implementation strategies: results from the Expert Recommendations for Implementing Change (ERIC) project. Implementation science : IS. 2015;10:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.