Abstract
Context:
During the past 45 years, exposure to lead has declined dramatically in the United States. This sustained decline is measured by blood and environmental lead levels and achieved through control of lead sources, emission reductions, federal regulations, and applied public health efforts.
Objective:
Explore regulatory factors that contributed to the decrease in exposure to lead among the US population since 1970.
Design/Setting:
We present historical information about the control of lead sources and the reduction of emissions through regulatory and selected applied public health efforts, which have contributed to decreases in lead exposure in the United States. Sources of lead exposure, exposure pathways, blood lead measurements, and special populations at risk are described.
Results:
From 1976-1980 to 2015-2016, the geometric mean blood lead level (BLL) of the US population aged 1 to 74 years dropped from 12.8 to 0.82 μg/dL, a decline of 93.6%. Yet, an estimated 500 000 children aged 1 to 5 years have BLLs at or above the blood lead reference value of 5 μg/dL established by the Centers for Disease Control and Prevention. Low levels of exposure can lead to adverse health effects. There is no safe level of lead exposure, and child BLLs less than 10 μg/dL are known to adversely affect IQ and behavior. When the exposure source is known, approximately 95% of BLLs of 25 μg/dL or higher are work-related among US adults. Despite much progress in reducing exposure to lead in the United States, there are challenges to eliminating exposure.
Conclusions:
There are future challenges, particularly from the inequitable distribution of lead hazards among some communities. Maintaining federal, state, and local capacity to identify and respond to populations at high risk can help eliminate lead exposure as a public health problem. The results of this review show that the use of strong evidence-based programs and practices, as well as regulatory authority, can help control or eliminate lead hazards before children and adults are exposed.
Keywords: blood lead levels, lead exposure, lead sources, regulation
Since 1971, the United States has seen a dramatic and sustained decline in population-level lead exposure. Blood lead levels (BLLs), a time-integrated measure of past and recent exposure, are the most common indicator of human exposure.1 In the late 1970s, the first nationally representative, population-based survey of BLLs in the United States found that 78% of persons aged 1 to 74 years had BLLs of 10 μg/dL or higher, and 88% of children aged 1 to 5 years had BLLs of 10 μg/dL or higher.2 Increasing awareness of the hazards of low levels of lead exposure among young children has led public health authorities to progressively lower the BLL considered elevated from 60 μg/dL (mid-1960s) to 10 μg/dL (1991). In 2012, the Centers for Disease Control and Prevention (CDC) accepted the recommendation from the Advisory Committee on Childhood Lead Poisoning Prevention to replace the term blood lead level of concern with a reference BLL value of 5 μg/dL or higher.3 From 1976-1980 to 2015-2016, the overall estimated geometric mean BLL of the US population aged 1 to 74 years decreased from 12.8 to 0.82 μg/dL, representing a decline of 93.6% (CDC, unpublished data, 2018).4 This decline was achieved through federal regulations and applied public health activities resulting in a range of lead source control measures and emission reductions (Figure 1). In 2015, the National Institute for Occupational Safety and Health designated a BLL of 5 μg/dL or higher as elevated for adults.5
Figure 1:
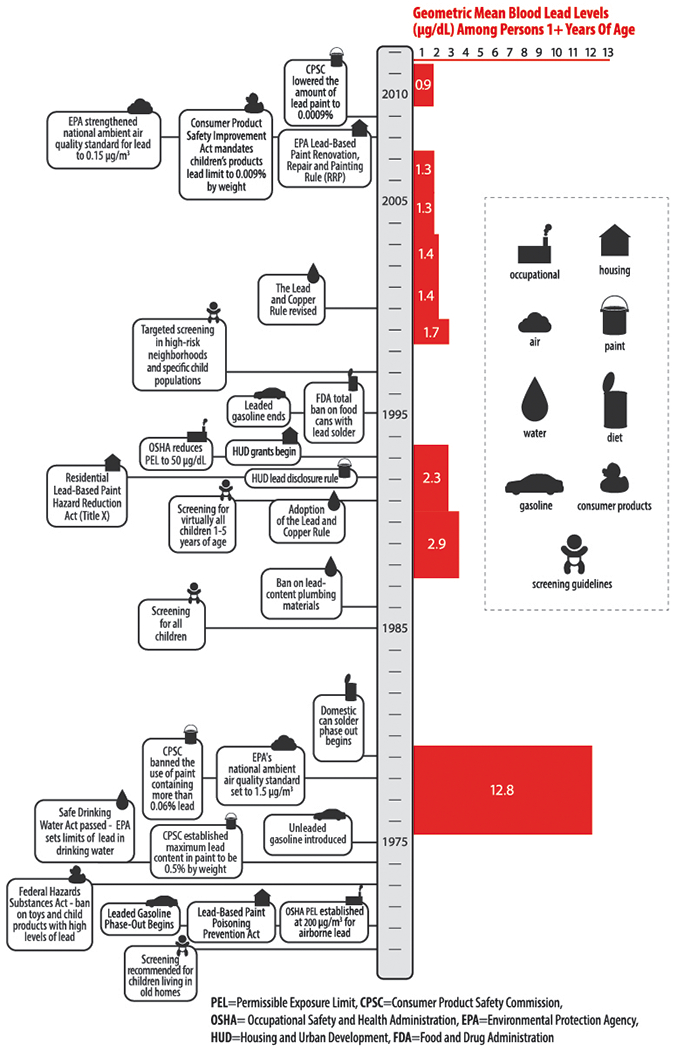
Selected Lead Control Measures, United States, 1970-2012
The CDC identified childhood lead poisoning prevention as 1 of 10 great US public health achievements during 2001 to 2010.6 Despite the success in reducing human exposures on average, the amount of lead used within the United States during the same period has increased.7 Lead exposure causes a wide range of adverse health effects among children and adults. In addition, mounting evidence suggests that there may be no threshold for the deleterious effects of lead, and that the rate of decline in IQ may be greater at lower than at higher BLLs,8 thus underscoring the critical importance of primary prevention to reduce lead exposure before it occurs.
The US government renewed its pledge in the Healthy People 2020 (HP2020) objective to reduce mean BLLs to 1.6 μg/dL among children aged 1 to 5 years, reduce child BLLs of 5 μg/dL or higher by 10%, and reduce by 10% the proportion of adult workers (aged 16 years or older) who have a BLL of 10 μg/dL or higher.9 As of 2009 to 2010, the overall HP2020 goals for children’s lead exposure have been met; however, the benefits have not been uniformly distributed, and disparities in exposure by income, race, and ethnicity remain significant.10 Currently (2015-2016), 0.2% of children aged 1 to 5 years have BLLs of 10 μg/dL or higher, and 1.3% have BLLs of 5 μg/dL or higher (CDC, unpublished data, 2018).
Sources of Lead in the Environment and Pathways of Exposure
An understanding of the sources of lead in the environment and the pathways of exposure is imperative to the development and implementation of regulations to reduce exposures. Lead is a naturally occurring heavy metal in the earth’s crust. Widespread extraction and use of lead have contaminated the environment, exposed people to lead, and created significant public health problems in many parts of the world. The primary pathways for human exposure to lead are inhalation and ingestion.1
Gasoline and air
Historically, the major source of lead in air was leaded gasoline exhaust. Tetraethyl lead was blended with gasoline primarily to boost octane beginning in the early 1920s.11 Although some public health advocates raised health concerns early, the lead industry successfully argued against limits on the use of lead in gasoline.12 A 1960s study showed that levels of lead in air were highest in heavy traffic zones, and that BLLs generally increased with air lead levels; however, the report concluded that the general population did not show evidence of exposure beyond “normal” levels.13
Nonetheless, in 1972, the Environmental Protection Agency (EPA) put forward a health-based regulation to remove lead from gasoline.14 An EPA cost-benefit analysis showed that tightening lead standards would lead to health benefits far outweighing the industrial costs of attaining those standards.15 In addition, the CDC released data demonstrating the close correlation between BLLs among the general population and gasoline lead concentrations during the late 1970s.16 Over time, lead in gasoline was reduced from an average 2.5 g per gallon in 1971 17 to 0.1 g per gallon in 1986.18 The Clean Air Act Amendments of 1990 resulted in a final ban on leaded gasoline for most motor vehicle use, effective January 1, 1996.19 Figure 2 shows the amount of leaded gasoline used in the United States during 1975 to 1996 and the quarterly average maximum concentrations of lead in air at EPA-monitoring sites during 1977 to 2016. During the period, the quarterly average maximum amount of lead in air decreased by 97.7% from 1.35 μg/m3 in 1977 to 0.03 μg/m3 in 2016.
Figure 2. Consumption of Leaded Gasoline and Average Air Lead Concentrations, U.S., 1975-2016.
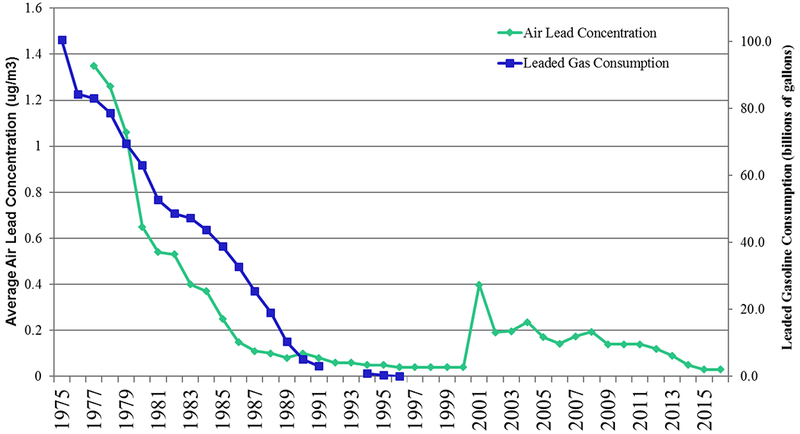
Note: Air lead concentration data are based on 122 ambient air quality monitoring stations during 1977-79, 216 stations during 1980-89, 175 stations during 1990-2000, 125 stations during 2001-2009, and 108 stations during 2010-2016. The increase in air lead concentration between 2000 and 2001 is likely due to changes at sites near stationary industrial sources. The decline in air lead concentrations between 2001 and 2002 is likely due to lower lead concentrations at sites in Herculaneum, Missouri.
Sources: personal communication, Jim Caldwell, USEPA, 1996; USEPA, 1998; USEPA, 2001; USEPA, 2003; USEPA, 2018 (https://www.epa.gov/air-trends/lead-trends)
Although gasoline exhaust has been the largest contributor to air lead levels, emissions from most other sources have decreased, too. For example, air lead emissions from industrial processes, such as metals processing, which accounted for 78% of air lead emissions in 2001, were 89% lower than in 1975.20 Leaded aviation gasoline is still used by approximately 167 000 piston-powered US aircrafts for engine safety, which accounts for about half of current lead emissions into air.21 Gasoline with alkyl-lead additives is also used to boost octane in fuels for racing cars, boats, and trucks, as well as for recreational marine vessels.22
The EPA’s National Ambient Air Quality Standard for lead of 1.5 μg/m3 was set in 1978.23 In 2001, 2.7 million people were living in counties that failed to meet this standard.24 All of these sites were near industrial point sources, such as lead smelters and battery manufacturers. The EPA lead-monitoring strategy currently focuses on emissions from point sources because industrial processes are responsible for all violations of the lead standard. In 2008, the EPA strengthened the National Ambient Air Quality Standard to 0.15 μg/m3, not to be exceeded as an average for any 3-month period within 3 years on the basis of lead in total suspended particles.25 In response to the more conservative standard to lead in air, the EPA revised the ambient monitoring rules to require that any source emitting more than 0.5 ton per year must have a monitor placed nearby. In 2015, the EPA revised air emissions reporting requirements, which lowered the threshold for reporting lead emissions sources as point sources to 0.5 tons per year of actual emissions.26
Lead-based paint
Use of lead in paint in the United States expanded in the early 1900s, when the paint industry burgeoned and the first pigments produced on a large commercial scale were made of lead. For many years, white lead was the principal opaque pigment used for interior and exterior paints and, on average, interior paints used before 1940 contained about 50% lead.27 Lead use in residential paint was unregulated until 1955, when the paint industry adopted a voluntary standard of no more than 1% lead by weight for paint for interior uses.28 Other lead-based pigments for exterior paints and primers for metal structures and vehicles continued in use into the early 1970s.
In 1971, the Lead-Based Paint Poisoning Prevention Act required the Secretary of Health, Education, and Welfare (now Department of Health & Human Services) to prohibit lead-based paint in residential structures constructed or rehabilitated by the federal government or with federal assistance (ban effective in 1978). This legislation defined lead-based paint as paint containing more than 1% lead by weight, and paint chips as the primary hazard source, and set the BLL of concern at 60 μg/dL.29 An estimated 23 million housing units have 1 or more lead-based paint hazards, including 3.6 million households with children aged 6 years or younger.30
In 1992, Title X of the Housing and Community Development Act, also known as the Residential Lead-Based Paint Hazard Reduction Act of 1992, amended the Lead-Based Paint Poisoning Prevention Act. This act expanded the concept of lead-based hazards in homes from paint chips to lead-contaminated dust and soil; shifted response to lead-based hazards from reactive to preventive through a national strategy to eliminate those hazards; and recognized the need to use emerging technology for evaluating and reducing the risk of hazards.31 The Renovation, Repair, and Painting Rule, established in 2008 and fully effective by 2010, requires renovation, repair, and painting firms working in pre-1978 housing or child-occupied facilities to be certified by the EPA; to assign to each job a certified renovator trained in lead-safe work practices by an EPA or authorized state-accredited training provider; and to use lead-safe work practices.32 The National Health and Safety Performance Standards require all family-based daycare centers to be lead-safe and not have flaking or peeling paint.33
Toys and other consumer products
Lead is used to augment paints and pigments on some toys. Toys themselves may be made of lead. Under the 1973 Federal Hazardous Substances Act, the US Consumer Product Safety Commission (CPSC) banned hazardous amounts of lead in toys and other products intended for use by children and required warning labels on other lead-containing products. In 1978, the CPSC banned furniture, toys, and other articles with a surface lead content of 0.06% or higher by weight intended for use by children.34 In 2008, following several high-profile lead-tainted toy recalls, Congress enacted the Consumer Product Safety Improvement Act, which mandated reduction of the lead limit in these products to 0.009% by weight,35 the lowest lead limits for children’s products in the world, and allowed for seizure and destruction of those toys that are lead-tainted.36 Despite this, many products containing lead still enter the marketplace. From 1977 to 2014, the CPSC issued 350 recalls of more than 200 million consumer items for violations of the lead paint standard or other lead exposure risks (CPSC, unpublished data, 2015).
Foods and diet
The Pure Food and Drugs Act of 1906 created the predecessor to the US Food and Drug Administration (FDA)—the US Department of Agriculture’s Bureau of Chemistry. Early investigations from this bureau involved the confiscation and destruction of several bags of lead chromate-coated coffee, identification of lead in gelatin, and the use of lead-containing foils for wrapping food.37 The first concerted effort to reduce lead content of foods occurred in the early 1930s when the FDA initiated an enforcement program on lead-based pesticides in fruits and vegetables.38 After World War II, such pesticides were replaced with other formulations for most uses and banned completely in 1988.39
In the 1960s, the first attempts to calculate dietary lead intake reported lead intakes of 0.12 to 0.30 mg/d and maximum levels of 0.35 mg/d during that period.40 During the 1970s and 1980s, the FDA actively issued regulatory statements and worked with industry to reduce dietary lead exposure, targeting removal of lead solder from food cans.41 Efforts to reduce exposing infants and young children to lead from food packaging resulted in average lead levels from baby foods declining from 0.15 mg/kg in the early 1970s to 0.003 mg/kg in 1990.41 In 1993, the FDA limited lead to 80 parts per billion (ppb) in canned fruit drinks and 250 ppb in other canned foods until all lead-soldered cans were banned. A total ban on food cans with lead solder, including imported cans, became effective in 1995.42
The FDA has taken actions to reduce lead exposures from lead-glazed ceramic pottery, leaded crystal glassware, and lead foil wraps for wine bottles. In addition, the FDA established guidance to limit lead in wine at 300 ppb and later proposed a regulation to prohibit further use of lead foil wraps on wine bottles.43 For ceramic ware, such as cups, mugs, and pitchers that hold food and drink for long periods, the FDA established 0.5 ppm as the maximum permissible lead level in glaze.44 The FDA’s more recent focus is on limiting lead in food and bottled water (eg, 5 ppb maximum lead level), especially those consumed by children (eg, maximum lead level of 0.1 ppm in candy).45 However, a recent Environmental Defense Fund report analyzed 11 years of FDA data and found that 20% of baby food samples, compared with 14% for other foods, had detectable amounts of lead and estimated that more than 1 million children consume lead in amounts greater than FDA’s former limit.46
Finally, exposure investigations have found lead associated with numerous items, including illegally distilled alcoholic beverages, traditional folk medicines and cosmetics, herbal and Ayurvedic remedies, ethnic foods, imported candy wrappers, and certain spices.47–50
Drinking water
Lead enters drinking water primarily through corrosion of lead-containing plumbing and fixtures.51 Lead pipes were popular for constructing main service lines in the late 1800s and early 1900s because of their pliability and relative resistance to corrosion compared with iron and steel.52 The Safe Drinking Water Act, passed in 1974 and amended in 1986 and 1996, gives the EPA authority to set limits on levels of lead and other contaminants in drinking water. Interim drinking water standards set in 1975 called for lead in drinking water to be less than 50 μg/L (50 ppb).53 The 1986 amendment to the Safe Drinking Water Act required lead-free solder, flux, fittings, and pipes as of June 1988.54
Growing recognition of the contribution of corrosion of lead pipes and service lines to the levels of lead in tap water led to the adoption of the 1991 Lead and Copper Rule.55 Under this rule, the largest utilities (ie, systems serving >50 000 residents) are required to optimize corrosiveness control. All water utilities are required to monitor tap water lead levels and take appropriate actions (eg, public education, water treatment, and lead service line replacement) if more than 10% of samples exceed EPA’s current 15-ppb action level.54 The long-term goal is to remove all lead pipes. However, water supply–specific use of orthophosphate has been shown to effectively control corrosion and, in 99% of cases, results in compliance with the World Health Organization Guideline Value of 10 ppb.56
In 1991, the EPA estimated that around 20% (10.2 million) of all public water distribution systems currently had some lead service lines or connections.54 The Lead and Copper Rule originally required replacement of the public and private service pipelines; however, the rule was revised in 2000 to allow for only partial service line replacement in the publicly owned sectors.55 Partial replacement of lead-containing pipe is now recognized to be a source for elevated concentrations of lead in water. The repair work can disrupt the buildup of minerals coating the pipes, thus releasing lead-containing minerals into the water.57 Because of recent high-profile events in Washington, District of Columbia, and Flint, Michigan,57,58 among others, significant efforts are now being undertaken to remove and replace lead service lines. However, cost of replacement of private lines connecting homes to the public water supply and distribution most often is borne by the homeowner, which contributes to potential inequitable distribution of exposure. Nationally, an estimated 6.1 million lead-containing service lines exist today.59
Workplace and “take-home” lead exposure
Occupational lead exposure was a well-recognized hazard when the Occupational Safety and Health Administration (OSHA) was created within the US Department of Labor in 1970 through the Occupational Safety and Health Act of 1970.60 Lead is used in more than 100 industries, and many job activities involve the use or disturbance of lead.61 Industry sectors reporting the greatest numbers of lead-exposed workers are manufacturing, construction, and mining.61 Major occupations known to expose workers to lead include the following: radiator repair, battery manufacturing and reclamation, primary smelting, home renovation, steel structures renovation, foundry work, pottery production, scrap metal recycling, munitions production and use, construction demolition, and working with lead-based paint.61
In 1971, through the Occupational Safety and Health Administration Act of 1970, OSHA set an initial permissible exposure limit (PEL) for airborne lead of 200 μg/m3 (averaged over 8 hours) for general industry and for construction. The PEL was lowered to 50 μg/m3 for general industry workers in 1978 but remained at 200 μg/m3 for construction industry workers until 1993, when it too was lowered to 50 μg/m3.63 Employers must implement engineering and work practice controls to the extent feasible to keep employee exposures below the PEL. If these controls are inadequate in maintaining exposures below the PEL, employers must provide personal protective equipment, including respirators.64
The OSHA lead standards call for biological monitoring of employees when their airborne lead exposures are 30 μg/m3 or higher. The BLL triggering removal was lowered from 80 μg/dL in 1979 to 50 μg/dL in 1983.65 Among workers who voluntarily agree to employer-offered medical surveillance, those with elevated BLLs of 50 μg/dL or higher (construction industry) or BLLs of 60 μg/dL or higher (general industry) must be removed from the job of lead exposure and offered the same pay and benefits (medical removal protection) until their BLLs drop to less than 40 μg/dL. In 2010, the CDC issued guidance that health care providers can use to trigger medical workplace removal for pregnant women with BLLs of 10 μg/dL or higher.66 There is evidence that many lead-exposed workers are not offered the mandated BLL testing that triggers medical removal protection or other requirements of the OSHA standards.67 Furthermore, OSHA requirements do not cover those working in small businesses and self-employed workers, such as individual contractors.68
Workers can inadvertently transport hazardous materials into their vehicles and homes on their own tools, clothing, hair, and skin, creating an exposure hazard for their children.69 A 1999 meta-analysis estimated that these take-home exposures were responsible for about 2.5% of the elevated BLLs among US children younger than 6 years.70 Requiring workers to wear protective clothing, shower, or change clothes before leaving work for home—or a combination of these measures—can mitigate this risk.
Mining and smelting
Primary production of lead from mining and smelting activities in the United States, ongoing since the early 18th century, ceased when the last active US lead smelter, St Louis-based Doe Run Co, the world’s third largest producer of lead from mines, terminated operations as part of a $65 million agreement with the EPA and the state of Missouri. In 2018, lead was present as a contaminant in at least 1076 (80%) of 1346 US hazardous waste sites on the EPA National Priorities List.71 Lead ranks number 1 on the Hazardous Substance Priority List potential threat to human health because of its known or suspected toxicity and potential for human exposure at National Priorities List sites.1 Persons living near any lead mining, smelting, or reclamation operations can have increased exposure to lead in air, dust, water, and soil.1
Lead ore is still mined in many countries around the world with most world output coming from China, Australia, Peru, Canada, Mexico, and Sweden. Because lead is mined, smelted, and then moved around in the environment, but never destroyed, there is also a secondary market for the toxic metal. In 2016, about 1.07 million tons of secondary lead were produced in the United States, an amount equivalent to 69% of apparent domestic lead consumption.7
Discussion/Conclusions
In the United States today, deteriorating lead-based paint in older homes and buildings is the most highly concentrated and significant source of lead exposure among children, accounting for up to 70% of elevated childhood BLLs.72 Lead dust and paint chip hazards arise through the following: friction between interior surfaces, such as doorframes or windowsills, home renovations that disturb lead paint, and transport from outdoor sources, such as soil and exterior paint, and lead can be transferred from surfaces to hands and ingested by young children via normal hand-to-mouth activity. At least 2 areas in the United States (Washington, District of Columbia, and Maryland) require residential rental properties built before 1978 to meet lead risk reduction standards.73,74
Recent events involving lead-contaminated drinking water have highlighted the need to remove lead service lines; however, corrosion control water treatments remain an important component to lead-safe water. The Water Infrastructure Improvements for the Nation Act (WIIN Act; PL 114-322), enacted December 16, 2016, provides for several provisions across multiple agencies to improve water resources and critical infrastructure in the United States.
Today’s major use of lead is in lead-acid batteries, representing almost 70% of apparent US lead consumption—a significant shift from previous patterns of lead use in gasoline, paint, and water systems several decades ago. Consumption of lead worldwide is expected to increase as the demand for lead batteries increases with the use of automobiles, computers, telecommunications equipment, and solar and wind energy.75 Some other uses of lead today include soundproofing buildings, blocking radiation in health care settings and nuclear installations, ammunition, cable covering, piping, bearing metals for machinery, and sheet lead.1 Leaded gasoline is still the fuel of choice for piston-powered aircraft, racing cars, and watercraft.21 Paint intended for bridges and marine vessel usage may also contain lead.22 Finally, although US manufacturers discontinued use of lead pigment in automobile paint finishes in the early 1990s, paint used by automotive repair shops and aftermarket refinishers may still contain lead, creating occupational exposure potential.65
In addition, the marketplace of consumer goods continues to expand, and many products come directly from trading partners outside of the United States, making it a challenge to regulate the thousands of product types. Lead hazards frequently arise during the early stages of the product supply chain (ie, selection and use of raw materials) and during the disposal and recycling process. The CPSC is aggressively targeting industry stakeholders early in the manufacturing process by encouraging participation in voluntary standard activities, training regarding regulatory requirements and hazard identification best practices, and implementing international protocols that prohibit the use of lead paint. Lead contamination of food, which is associated with a handful of industrial processes, was decidedly reduced in the United States during the 20th century. However, because of increasing global travel and trade, certain imported food and food-related items may cause certain subpopulations to require continued monitoring for lead exposure.36
The decrease in population exposures to lead, as evidenced by BLLs in the United States, has been substantial and sustained during the past 40 years. The remaining affected children are not randomly dispersed throughout the population—they are primarily concentrated in neighborhoods characterized by older homes, lower family incomes, lower housing values, higher population densities, higher proportions of rental properties, and higher proportions of minority, immigrant, and refugee residents.76,77 Point sources of lead, although not significant at the national level, can have a large effect on communities and local residents, contributing to concerns about inequitable exposures. Racial and socioeconomic disparities continue to exist near hazardous waste sites and among persons living in deteriorated neighborhoods.78 Another source of lead is the global transport of airborne lead particulates, making lead exposure a global concern, as outlined in the Basel Convention on controlling the movement of hazardous wastes.79
Similarly, although tremendous strides have been made in reducing workplace lead exposures, these hazards remain a considerable public health concern. Lowering lead exposure in the workplace would benefit workers and their children. In a limited meta-analysis, an estimated one-half of workers currently exposed to lead in the workplace will, from taking home hazardous amounts of lead dust on their clothes, cause elevated BLLs among their children younger than 6 years.70 The OSHA and PEL rules are more than 40 years old and may not protect workers’ health, even when the rules are followed. Continued declines in human exposures to lead seem a reasonable expectation when considering the noted improvements in air and water quality and the reduction in numbers of older housing with lead hazards. The US government has renewed its pledge in the HP2020 goals to eliminate lead poisoning as a public health problem by 2020.9 A focus on primary prevention to lead exposure may involve federal, state, and local agencies initiating and maintaining active, productive collaborations with traditional and nontraditional partners to reduce exposure to point sources and occupational hazards. Remaining engaged in control efforts could help these partners ensure that lead hazard control measures are maintained and effective.
Implications for Policy & Practice
Despite much progress in reducing exposure to lead in the United States, there are challenges to eliminating exposure. The following is a short list of important policies and procedures.
Approximately 23 million housing units contain significant lead-based paint hazards, and 6.1 million have lead water service lines. Low-income, poorly maintained rental properties may be the first priority to eliminate or control these hazards, but resources are also needed for single-family-owned properties.
In most cases, all sources of lead will not be eliminated. Thus, policies and practices that institutionalize the maintenance of control measures are essential to prevent any recurrence of lead hazards among properties that have not been made lead-free.
Integrating federal, state, and local primary prevention plans can help eliminate lead exposure. Studies indicate that diverse public-private partnerships are critical elements for developing, supporting, promoting, and monitoring comprehensive, evidence-based interventions to control and eliminate lead hazards from the environment.
Blood lead testing of at-risk children and quick medical management of children with blood lead levels of 5 μg/dL or higher can help, but not at the expense of primary prevention interventions. Special attention can be considered to the testing of immigrant and refugee children who may be exposed to lead sources that are uncommon among the US population.
Footnotes
The authors are indebted to the following people who provided unpublished data, helped them find information sources, and provided editorial or graphical comments: Warren A. Galke (deceased), Adrienne Ettinger, Warren Friedman, and Steve Mann.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
The authors declare no conflicts of interest.
References
- 1.Agency for Toxic Substances and Disease Registry. Toxicological profile for lead. https://www.atsdr.cdc.gov/toxprofiles/tp13.pdf. Published August 2007 Accessed March 2, 2016. [PubMed]
- 2.Mahaffey KR, Annest JL, Roberts J, Murphy RS. National estimates of blood lead levels: United States 1976-1980. N Engl J Med. 1982;307:573–579. Bibliographic Links [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. Low Level Lead Exposure Harms Children: A Renewed Call for Primary Prevention. Atlanta, GA: US Department of Health & Human Services; 2012. http://www.cdc.gov/nceh/lead/acclpp/final_document_030712.pdf Accessed July 25, 2017. [Google Scholar]
- 4.Pirkle JL, Brody DJ, Gunter EW, et al. The decline of blood lead levels in the United States: the National Health and Nutrition Examination Surveys (NHANES). JAMA. 1994;272:284–291. Bibliographic Links [PubMed] [Google Scholar]
- 5.National Institute for Occupational Safety and Health. Adult blood lead epidemiology and surveillance. Reference blood lead level for adults. https://www.cdc.gov/niosh/topics/ables/description.html. Published 2015 Accessed June 7, 2018.
- 6.Centers for Disease Control and Prevention, Ten great public health achievements—United States, 2001-2010. MMWR Morb Mortal Wkly Rep. 2011;60:619–623. [PubMed] [Google Scholar]
- 7.US Geological Survey, Mineral Commodity Summaries. Lead. https://minerals.usgs.gov/minerals/pubs/commodity/lead/mcs-2017-lead.pdf. Published January 2017 Accessed April 10, 2018.
- 8.Bellinger DC. Very low lead exposures and children’s neurodevelopment. Curr Opin Pediatr. 2008;20:172–177. Ovid Full Text Bibliographic Links [DOI] [PubMed] [Google Scholar]
- 9.US Department of Health & Human Services. Healthy people 2020. http://healthypeople.gov/2020/topicsobjectives2020/overview.aspx?topicid=12. Published 2010 Accessed March 22, 2012.
- 10.Whitehead LS, Buchanan SD. Childhood lead poisoning: a perpetual environmental justice issue? J Public Health Manag Pract. 2019;25(1 Supp):S115–S120. Ovid Full Text Bibliographic Links [DOI] [PubMed] [Google Scholar]
- 11.Nriagu JO. The rise and fall of leaded gasoline. Sci Total Environ. 1990;92:13–28. [Google Scholar]
- 12.Kitman JL. The secret history of lead. Nation. 2000;20:11–44. [Google Scholar]
- 13.Working Group on Lead Contamination. Survey of Lead in the Atmosphere of Three Urban Communities. Public Health Service Publication No. 999-AP-12. Cincinnati, OH: US Department of Health, Education and Welfare, Public Health Service; http://nepis.epa.gov/Exe/ZyPURL.cgi?Dockey=9101GK06.txt. Published 1965 Accessed February 25, 2015. [Google Scholar]
- 14.US Environmental Protection Agency. Regulation of fuels and fuel additives: notice of proposed rulemaking. Fed Regist. 1972;37(36):3882–3884. [Google Scholar]
- 15.US Environmental Protection Agency. Costs and benefits of reducing lead in gasoline: final regulatory impact analysis. USEPA-230-05-85-006. http://yosemite.epa.gov/ee/epa/eerm.nsf/vwAN/EE-0034-1.pdf/$file/EE-0034-1.pdf. Published 1985 Accessed February 25, 2015. [Google Scholar]
- 16.Annest JL, Pirkle JL, Makuc D, Neese JW, Bayse DD, Kovar MG. Chronological trend in BLLs between 1976 and 1980. N Eng J Med. 1983;308:1373–1377. [DOI] [PubMed] [Google Scholar]
- 17.US Environmental Protection Agency. 42 CFR Part 479. Regulation of Fuel Additives: Advance Notice of Proposed Rulemaking. Washington, DC: US Environmental Protection Agency; 1971. 34 FR 1186. [Google Scholar]
- 18.US Environmental Protection Agency. National Air Pollutant Emission Trends, 1900-1998. Washington, DC: US Environmental Protection Agency, Office of Air Quality; 1997. EPA 454/R-97-011. https://nepis.epa.gov/Exe/ZyPDF.cgi/2000ETJA.PDF?Dockey=2000ETJA.PDF. Published 1997 Accessed May 29, 2018. [Google Scholar]
- 19.US Environmental Protection Agency. Prohibition on gasoline containing lead or lead additives for highway use. 1996. 40 CFR part 80. 61 FR 3832-3838. [Google Scholar]
- 20.US Environmental Protection Agency. EPA-454/R-12-001. Our nation’s air status and trends through 2010. https://www.epa.gov/sites/production/files/2017-11/documents/trends_brochure_2010.pdf. Published 2012 Accessed May 22, 2018.
- 21.US Environmental Protection Agency. 40 CFR Part 87. Advance notice of proposed rulemaking on lead emissions from piston-engine aircraft using leaded aviation gasoline. 75 FR 22439. http://www.gpo.gov/fdsys/pkg/FR-2010-04-28/pdf/2010-9603.pdf. Published 2010 Accessed February 26, 2015.
- 22.Rom WN. Environmental and Occupational Medicine. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2007: 957–982. [Google Scholar]
- 23.US Environmental Protection Agency. 40 CFR 50, 53, 58. National Ambient Air Quality Standard for Lead: final rules and proposed rulemaking. 43 FR 46246-46277. https://www.epa.gov/sites/production/files/2016-03/documents/43fedreg46246.pdf. Published 1978 Accessed February 26, 2015.
- 24.US Environmental Protection Agency. Latest findings on national air quality. 2001 status and trends. EPA 454/K-02-001. http://www.epa.gov/airtrends/aqtrnd02/2002_airtrends_final.pdf. Published 2002 Accessed March 8, 2011.
- 25.US Environmental Protection Agency. National Ambient Air Quality Standards for Lead. 40 CFR 50.16. 73 FR 66934. http://www.epa.gov/fedrgstr/EPA-AIR/2008/November/Day-12/a25654.pdf. Published 2008 Accessed August 24, 2011.
- 26.US Environmental Protection Agency. 40 CFR 51. Revisions to the air emissions reporting requirements: revisions to lead (Pb) reporting threshold and clarifications to technical reporting details. 80 FR 8787. http://www.gpo.gov/fdsys/pkg/FR-2015-02-19/pdf/2015-03470.pdf. Published 2015 Accessed April 22, 2015.
- 27.National Academy of Sciences. Report of the Ad Hoc Committee to Evaluate the Hazard of Lead in Paint National Research Council, prepared for the Consumer Product Safety Commission. Washington, DC: National Academy of Sciences; 1973. [Google Scholar]
- 28.US Department of Housing and Urban Development. Comprehensive and Workable Plan for the Abatement of Lead-Based Paint in Privately Owned Housing: A Report to Congress. Washington, DC: US Department of Housing and Urban Development; 1990. [Google Scholar]
- 29.US Department of Health, Education, and Welfare. Medical aspects of childhood lead poisoning. HSMHA Health Rep. 1971;86(2):140–143. Bibliographic Links [PMC free article] [PubMed] [Google Scholar]
- 30.US Department of Housing and Urban Development. American Healthy Homes Survey: lead and arsenic findings. http://portal.hud.gov/hudportal/documents/huddoc?id=AHHS_REPORT.pdf. Published 2011 Accessed August 21, 2011.
- 31.US Department of Housing and Urban Development. Legislative history of lead-based paint. http://www.hud.gov/offices/cpd/affordablehousing/training/web/leadsafe/ruleoverview/legislativehistory.pdf. Published 1992 Accessed August 23, 2015.
- 32.US Environmental Protection Agency. Renovation, repair and painting program. http://www2.epa.gov/lead/renovation-repair-and-painting-program. Published 2015 Accessed September 3, 2015.
- 33.American Academy of Pediatrics, American Public Health Association, National Resource Center for Health and Safety in Child Care and Early Education. Standard 5.2.9.13. Caring for Our Children: National Health and Safety Performance Standards; Guidelines for Early Care and Education Programs. 3rd ed. Elk Grove Village, IL; Washington, DC: American Public Health Association; 2011. http://cfoc.nrckids.org/StandardView/5.2.9.13 Accessed May 13, 2015. [Google Scholar]
- 34.US Consumer Product Safety Commission. Staff Report on Lead and Cadmium in Children’s Polyvinyl Chloride (PVC) Products. Bethesda, MD: US Consumer Product Safety Commission; http://www.cpsc.gov//PageFiles/95613/Pbcdtoys.pdf. Published 1997 Accessed May 28, 2018. [Google Scholar]
- 35.US Consumer Product Safety Commission. 16 CFR Part 1303.1 Ban of Lead-Containing Paint and Certain Consumer Products Bearing Lead-Containing Paint. Bethesda, MD: US Consumer Product Safety Commission; 2008. 42 FR 44199 and 73 FR 77493. [Google Scholar]
- 36.US Consumer Product Safety Commission. U.S. Consumer Product Safety Commission Strategic Plan. Bethesda, MD: US Consumer Product Safety Commission; 2014. http://www.cpsc.gov//PageFiles/123374/2011strategic.pdf Accessed August 28, 2015. [Google Scholar]
- 37.Kashtock ME. Lead in food: the neo-classical contaminant In: Al-Taher F, Jackson L, DeVries J, eds. Intentional and Unintentional Contaminants in Food and Feed. American Chemical Society; Washington, DC: ACS Symposium Series 1020; 2009:229–253. [Google Scholar]
- 38.US Food and Drug Administration. Statement for the Record. Subcommittee on Toxic Substances, Environmental Oversight, Research and Development. Washington, DC: US Senate Committee on Environment and Public Works; 1993. [Google Scholar]
- 39.US Environmental Protection Agency. Inorganic arsenicals; intent to cancel registrations for pesticide products registered for non-wood preservative use; conclusion of special review. 53 FR 24787. https://www.beyondpesticides.org/assets/media/documents/wood/wp_complaint_12_10_02.pdf. Published 1988 Accessed May 28, 2018.
- 40.Kehoe RA. Normal metabolism of lead. Arch Environ Health. 1964;8:232–243. Bibliographic Links [DOI] [PubMed] [Google Scholar]
- 41.Bolger PM, Yess NJ, Gunderson EL, Troxell TC, Carrington CD. Identification and reduction of sources of dietary lead in the United States. Food Addit Contam. 1996;13:53–60. Bibliographic Links [DOI] [PubMed] [Google Scholar]
- 42.US Food and Drug Administration. 21 CFR 189.240. Lead-soldered food cans. 60 FR 33106-33109. http://www.gpo.gov/fdsys/pkg/FR-1995-06-27/pdf/95-15593.pdf. Published 1995 Accessed February 25, 2015.
- 43.US Food and Drug Administration. 21 CFR 189.301. Tin-coated lead foil capsules for wine bottles. 61 FR 4816-4820. http://www.gpo.gov/fdsys/pkg/FR-1996-02-08/pdf/96-2665.pdf. Published 1996 Accessed February 25, 2015.
- 44.US Food and Drug Administration. Compliance policy guide (CPG) Sec. 545.450 pottery (ceramics); import and domestic–lead contamination. http://www.fda.gov/ICECI/ComplianceManuals/CompliancePolicyGuidanceManual/ucm074516.htm. Published 2005 Accessed March 30, 2011.
- 45.US Food and Drug Administration. Supporting document for recommended maximum level for lead in candy likely to be consumed frequently by small children. https://www.fda.gov/Food/FoodborneIllnessContaminants/Metals/ucm172050.htm. Published 2006 Accessed May 28, 2018.
- 46.Environmental Defense Fund. New EPA model enables comparison of various sources of childhood exposure to lead. http://blogs.edf.org/health/2017/09/14/new-epa-model-lead/ Published 2017 Accessed May 17, 2018.
- 47.Centers for Disease Control and Prevention. Childhood lead poisoning associated with tamarind candy and folk remedies—California, 1999-2000. Morb Mortal Wkly Rep. 2002;51, 684–686. [PubMed] [Google Scholar]
- 48.Morgan BW, Barnes L, Parramore CS, Kaufmann RB. Elevated blood lead levels associated with the consumption of moonshine among emergency department patients in Atlanta, Georgia. Ann Emerg Med. 2003;42:351–358. Ovid Full Text Bibliographic Links [DOI] [PubMed] [Google Scholar]
- 49.Centers for Disease Control and Prevention. Lead poisoning associated with Ayurvedic medications—five states, 2000-2003. MMWR Morb Mortal Wkly Rep. 2004;53:582–584. [PMC free article] [PubMed] [Google Scholar]
- 50.Centers for Disease Control and Prevention, Lead poisoning associated with use of litargirio—Rhode Island, 2003. MMWR Morb Mortal Wkly Rep. 2005;54:227–229. [PubMed] [Google Scholar]
- 51.Lassovsky P, Cohen J. Lead in drinking water USA, sources and controls in buildings. In: Technical Proceedings of the 1992 CIB/W62 International Symposium on Water Supply and Drainage for Buildings; September 21-24, 1992; Westlake Village, CA: American Society of Plumbing Engineers, Rosemont, Illinois. [Google Scholar]
- 52.Troesken W, Beeson PE. The significance of lead water mains in American cities: some historical evidence In: Costa DL, ed. Health and Labor Force Participation Over the Life Course. Chicago, IL: University of Chicago Press; 2003:191–202. [Google Scholar]
- 53.US Environmental Protection Agency. Part 141—National Interim Primary Drinking Water Regulations. Washington, DC: US Environmental Protection Agency; 1975. 40 FR 59566. [Google Scholar]
- 54.US Environmental Protection Agency. Lead and Copper Rule Revisions White Paper. Washington, DC: Office of Water; https://www.epa.gov/sites/production/files/2016-10/documents/508_lcr_revisions_white_paper_final_10.26.16.pdf. Published 2016 Accessed May 28, 2018. [Google Scholar]
- 55.US Environmental Protection Agency. 40 CFR Parts 9, 141 and 142. National Primary Drinking Water Regulations and Lead and Copper. Washington, DC: US Environmental Protection Agency; 2000. 65 FR 1950-2015. [Google Scholar]
- 56.Hayes C, ed. Best Practice Guide on the Control of Lead in Drinking Water. London, United Kingdom: IWA Publishing; 2010. [Google Scholar]
- 57.Brown MJ, Raymond J, Homa D, Kennedy C, Sinks T. Association between children’s blood lead levels, lead service lines, and water disinfection, Washington, DC, 1998-2006. Environ Res. 2011;111:67–74. Bibliographic Links [DOI] [PubMed] [Google Scholar]
- 58.Kennedy C, Yard E, Dignam T, et al. Blood lead levels among children aged <6 years—Flint, Michigan, 2013-2016. MMWR Morb Mortal Wkly Rep. 2016;65(25):650–654. Bibliographic Links [DOI] [PubMed] [Google Scholar]
- 59.Cornwell DA, Brown RA, Via SH. National survey of lead service line occurrence. J Am Water Works Assoc. 2016;108(4):182–191. [Google Scholar]
- 60.Occupational Safety and Health Act of 1970. Pub L No. 91-596, 29 USCS §§651 et seq. https://www.osha.gov/pls/oshaweb/owadisp.show_document?p_id=2743&p_table=OSHACT Accessed May 29, 2018.
- 61.Association of Occupational and Environmental Clinics. Medical management guidelines for lead-exposed adults. http://aoec.org/documents/positions/MMG_FINAL.pdf. Published 2007 Accessed November 16, 2011.
- 62.Centers for Disease Control and Prevention. Adult blood lead epidemiology and surveillance—United States, 2008-2009. MMWR Morb Mortal Wkly Rep. 2011;60(25):841–845. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6025a2.htm Accessed November 16, 2011. [PubMed] [Google Scholar]
- 63.Occupational Safety and Health Administration. Department of Labor. 29 CFR 1926.62. Safety and Health Regulations for Construction. 57 FR 26627. https://www.osha.gov/pls/oshaweb/owadisp.show_document?p_table=STANDARDS&p_id=10641. Published 1993 Accessed May 29, 2018.
- 64.Occupational Safety and Health Administration. Department of Labor. 29 CFR 1910.1025. Lead. Occupational Safety and Health Standards. 29, Volume 6 FR 104-135. http://www.gpo.gov/fdsys/pkg/CFR-2011-title29-vol6/pdf/CFR-2011-title29-vol6-sec1910-1025.pdf. Published 2001 Accessed February 27, 2015.
- 65.Western Automotive Finishes. DIMENSION acrylic enamel system material safety data sheet. http://www.lbxco.com/MSDS/Paint/Paint%20MSDS%20%20Technical%20Data.pdf. Published 2003 Accessed July 15, 2011.
- 66.Centers for Disease Control and Prevention. Guidelines for the identification and management of lead exposure in pregnant and lactating women. http://www.cdc.gov/nceh/lead/publications/LeadandPregnancy2010.pdf. Published 2010 Accessed November 8, 2011.
- 67.Tak S, Roscoe RJ, Alarcon W, Ju J, Sestito JP, Sussell AL, Calvert GM. Characteristics of U.S. workers whose blood lead levels trigger the medical removal protection provision, and conformity with biological monitoring requirements, 2003-2005. Am J Ind Med. 2008;51:691–700. Bibliographic Links [DOI] [PubMed] [Google Scholar]
- 68.Occupational Safety and Health Administration. Standard interpretations: application of OSHA requirements to self-employed construction workers. http://www.osha.gov/pls/oshaweb/owadisp.show_document?p_table=INTERPRETATIONS&p_id=24317. Published 2001 Accessed June 6, 2008.
- 69.National Institute of Occupational Safety and Health. Report to congress on workers’ home contamination study conducted under the Workers’ Family Protection Act (29 U.S.C. 671a). http://www.cdc.gov/niosh/docs/95-123/. Published 1995 Accessed February 24, 2015.
- 70.Roscoe RJ, Gittleman JL, Deddens JA, Petersen MR, Halperin WE. Blood lead levels among children of lead-exposed workers: a meta-analysis. Am J Indus Med. 1999;36:475–481. [DOI] [PubMed] [Google Scholar]
- 71.Environmental Protection Agency; CERCLIS (comprehensive environmental response, compensation, and liability information system). Public access database. http://cumulis.epa.gov/supercpad/cursites/srchsites.cfm. Published 2018 Accessed May 28, 2018. [Google Scholar]
- 72.Levin R, Brown MJ, Kashtock ME, et al. Lead exposures in U.S. children, 2008: implications for prevention. Environ Health Perspect. 2008;116:1285–1293. Bibliographic Links [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Maryland Department of the Environment. Facts about Maryland’s lead law. http://www.mde.state.md.us/programs/Land/Documents/LeadFactSheets/LeadfsStandardOfCare.pdf. Published 2015 Accessed May 29, 2018.
- 74.Washington, DC Department of Energy and Environment. Lead Hazard Prevention and Elimination Act of 2008, D.C. Official Code §8-231.01 et seq. https://doee.dc.gov/service/lead-related-regulatory-and-legislative-affairs. Published July 26, 2013 Accessed May 29, 2018. [Google Scholar]
- 75.Gottesfeld P, Pokhrel A. Review: lead exposure in battery manufacturing and recycling in developing countries and among children in nearby communities. J Occup Environ Hygiene. 2011;8:520–532. [DOI] [PubMed] [Google Scholar]
- 76.Dignam TA, Evens A, Eduardo E, et al. High-intensity targeted screening for elevated blood lead levels among children living in 2 inner-city Chicago communities. Am J Public Health. 2004;94:1945–1951. Bibliographic Links [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Plotinsky RN, Straetemans M, Wong LY, et al. Risk factors for elevated blood lead levels among African refugee children in New Hampshire, 2004. Environ Res. 2008;108:404–412. Bibliographic Links [DOI] [PubMed] [Google Scholar]
- 78.Bullard RD, Mohai P, Saha R, Wright B. Toxic wastes and race at twenty: why race still matters after all of these years. Environ Law. 2008;38:371–411. [Google Scholar]
- 79.Basel Convention. Basel convention on the control of transboundary movements of hazardous wastes and their disposal. http://www.basel.int/TheConvention/Overview/TextoftheConvention/tabid/1275/Default.aspx. Published 1989 Accessed February 23, 2015. [PubMed]


