Abstract
Objective
The purpose of this report is to describe a patient with bilateral symptomatic hand osteoarthritis (OA) originally thought to be rheumatoid arthritis (RA) based on clinical and radiographic features.
Clinical Features
A 48-year-old woman presented with bilateral hand pain, stiffness, swelling, and redness in the proximal and distal interphalangeal joints of 1 year’s duration. Laboratory analysis and plain film radiography were equivocal. These findings necessitated the use of diagnostic ultrasound, which revealed no synovitis or erosions in the joints of the hand, so a diagnosis of bilateral symptomatic hand OA was rendered.
Intervention and Outcome
A trial of conservative care consisting of mobilizations, instrument-assisted soft tissue therapy, and laser therapy was given. At 1-month follow-up, the patient regained full pain-free range of motion and strength and returned to complete work activity.
Conclusion
This case report demonstrated that hand OA can present with nonspecific inflammatory-like clinical features. These findings require further testing, in which case ultrasound imaging may be valuable to differentiate OA from RA. Using ultrasound to make this diagnosis may guide management, with rheumatology referral for RA and conservative care for OA.
Key Indexing Terms: Osteoarthritis; Arthritis, Rheumatoid; Diagnosis
Introduction
Hand osteoarthritis (OA) is symptomatic in 20% of the population older than 60, resulting in impaired function and pain.1, 2 The pathophysiology of OA is complex and involves local and systemic chemical inflammation, anatomic derangement, and abnormal mechanical stresses.3 Risk factors for hand OA include advancing age, obesity, female sex, and prior injury.4
Clinical features include pain with activity, morning stiffness, swelling, joint hypertrophy, and functional impairment.5 These features are nonspecific, and when present bilaterally, hand OA may be difficult to differentiate from inflammatory arthritis, especially rheumatoid arthritis (RA). Laboratory analysis and diagnostic imaging may be needed in these scenarios.
Establishing a correct diagnosis is paramount because hand OA may be managed conservatively by a chiropractic physician, whereas RA requires rheumatology comanagement.6 In addition, early recognition and management of RA results in improved outcomes.6 The purpose of this report is to describe the findings in a patient with bilateral symptomatic hand OA that originally was thought to be RA based on clinical and radiographic findings.
Case Report
A 48-year-old Hispanic woman was referred from her primary care provider (PCP) to chiropractic services within a federally qualified health center with a complaint of bilateral hand pain, stiffness, swelling, and weakness. Swelling of the interphalangeal (IP) joints had been present for 1 year, but the pain began insidiously 3 months earlier. The pain was rated at 10 of 10 on the verbal pain scale. Stiffness was described as constant and lasting all day without any relief. The right hand was affected more severely. There was also a complaint of less severe bilateral elbow pain. The hand pain was hindering her ability to work as a house cleaner. She was prescribed naproxen and acetaminophen by her PCP, but discontinued use owing to the development of toxic hepatitis.
Upon visual inspection, the IP joints bilaterally were red and swollen. Physical examination revealed weakness in finger flexion, abduction, and adduction. Palpation demonstrated pain at all proximal IP (PIP) joints and the distal IP (DIP) joints bilaterally.
Laboratory analysis, ordered 1 year earlier by the patient’s PCP, revealed normal erythrocyte sedimentation rate and C-reactive protein, negative rheumatoid factor, and negative anti-nuclear antibodies. Despite old lab values being unremarkable for inflammatory markers, it was determined that diagnostic imaging was needed to evaluate for suspected inflammatory disease. Prior radiographs of the left hand ordered by the PCP were available for review from 3 months earlier, demonstrating normal joint spacing, periarticular osteopenia, and a questionable erosion at the fifth metacarpal base (Fig 1A). Contemporary bilateral hand radiographs were obtained, demonstrating symmetrical findings on the right side and no interval change of the left hand (Figs 1B and C). Targeted ultrasound imaging of the hands using a GE Logiq E9 (GE Healthcare, Wauwatosa, Wisconsin) with a linear transducer operating at 10 MHz was ordered to assess for synovitis and to further evaluate the erosions. These images showed no evidence of synovitis or marginal erosions in the joints of the hands bilaterally (Figs 2A, B, C, and D). A diagnosis of symptomatic hand OA was established.
Fig 1.

Posteroanterior radiograph of the left hand obtained May 12, 2017 (A), demonstrates periarticular osteopenia and a marginal erosion (arrow) at the base of the fifth metacarpal. Repeat posteroanterior radiograph of the left hand obtained August 9, 2017 (B), demonstrates no interval change of the findings. Posteroanterior radiograph of the right hand obtained August 9, 2017 (C), demonstrates symmetrical findings, including apparent erosion (arrow) at the fifth metacarpal.
Fig 2.
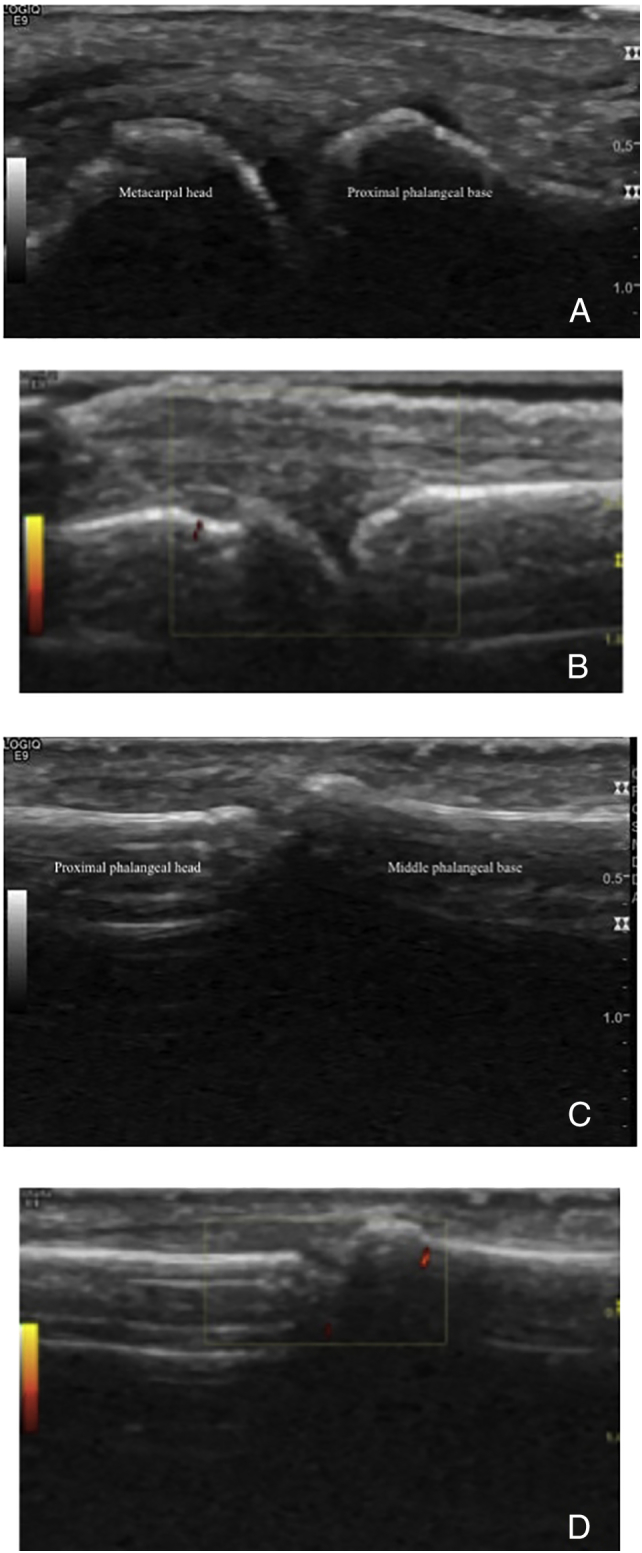
Long-axis B-mode (A) and power Doppler (B) ultrasound images of the right metacarpophalangeal joint are normal, without evidence of bony erosion or synovitis. Long-axis B-mode (C) and power Doppler (D) ultrasound images of the right proximal interphalangeal joint are also normal.
Intervention and Outcome
Manual mobilization in flexion, extension, circumduction, and long-axis traction of the PIP and DIP joints along with instrument-assisted soft tissue therapy to the same joints was performed. Low-level laser therapy using a Chattanooga Vectra Genisys 9 Diode Cluster Laser Applicator (Chattanooga, Hixson, Tennessee) for 1 minute and 30 seconds and 93.6 J at the PIP and DIP joints was used. The patient was given progressive finger extension and flexion exercises to be performed 3× daily in repetitions of 10. At her 1-month re-evaluation, palpatory tenderness persisted at the second through fourth palmar PIP joints bilaterally; however, full, pain-free finger range of motion was regained and strength in the digits was full. The patient self-reported no pain with activities of daily living and no impact on her work. No adverse events were reported throughout care. Informed consent was obtained from the patient to publish this case.
Discussion
Osteoarthritis is the most common rheumatologic disease in the United States, affecting 27 million people, and the hand is the second most common location after the knee.4 Although RA is the most common inflammatory arthritis, its prevalence is lower than OA, affecting only 1.3 million people in the United States.7 Both OA and RA have a predilection for women, but RA commonly presents in the third decade of life, whereas OA typically does not present until 50 years of age.3 Our patient fit the common profile for both diseases, presented with inflammatory-like symptoms, and had equivocal hand radiographs. Therefore, further testing was required to rule out RA before initiating a trial of conservative care.
Osteoarthritis and RA differ in their pathophysiology. Repeated mechanical stress and anatomic derangement contribute to the development of OA. Hand OA also is influenced by local and systemic inflammatory changes.8 Proinflammatory cytokines activate matrix metalloproteinases and aggrecans within the joint that cause chondrocyte death, poor synthesis of extracellular matrix, and subsequent inflammation, cartilage destruction, subchondral bony changes, and low-grade synovitis.8, 9, 10 As this case demonstrates, the consequence of these changes is inflammatory-like pain, stiffness, swelling, and redness that clinically can mimic RA.1, 9 Rheumatoid arthritis is an inflammatory, systemic, autoimmune disease that primarily manifests in the synovial tissue of joints, tendons, and bursae.11 Synovial cell hypertrophy, infiltration of inflammatory cells, and neovascularity to the joint contribute to the soft tissue pannus formation and periarticular osteopenia that ultimately leads to destruction and erosions of cartilage and bone.11 The questionable erosion and periarticular osteopenia noted on the radiographs in this case are more congruent with RA than OA; however, with negative laboratory values the need for diagnostic ultrasound was critical in differentiating OA from RA.
Both OA and RA have similar risk factors, making it difficult to use these in establishing a working diagnosis. Shared risk factors include fourth decade or older, obesity, female sex, and family history.1, 3 The differing risk factors are smoking, which only is associated with RA, and mechanical stressors implicated in the development of OA.11 The patient in this case had several risk factors (48 years old, female, family history of arthritis, and manual labor job) associated with both OA and RA, necessitating laboratory workup and multimodal imaging to solidify a diagnosis.
Hand OA and RA have overlapping presenting features that, as this case demonstrates, are nonspecific. Onset of symptoms can be insidious or abrupt for both types.6, 10 Signs and symptoms of hand OA can be inflammatory-like with morning stiffness lasting more than 1 hour, swelling, and redness.12 Bony enlargement from OA may mimic soft tissue pannus surrounding a joint in RA. Functional deficits in OA, although not as severe as those in RA, can have an impact on work and activities of daily living, especially when grip strength and range of motion are affected. The classic symptoms of RA take time to develop, so the patient presenting with hand pain and mild functional limitations and no deformities could be in the initial stages of RA or have OA.6 Common joints affected by OA include the DIP joints, PIP joints, and first carpometacarpal joints.3 However, OA can present in the metacarpophalangeal joints, especially in isolated instances.13 Sites of RA usually include the PIP and metacarpophalangeal joints, but DIP involvement is seen in up to 37% of cases.14 Simultaneous involvement of other joints is common in RA, so the complaint of bilateral elbow pain along with bilateral PIP and DIP joint pain further warranted additional testing for RA in this case. Ultimately, this elbow pain was considered nonspecific and self-resolved.
Laboratory work is not necessary for the diagnosis of OA, but in this case was done and showed no signs of inflammation (normal erythrocyte sedimentation rate, C-reactive protein, and negative rheumatoid factor). Because rheumatoid factor can be negative in up to 60% of those with RA and inflammatory markers may not be evident in the early stages, imaging was warranted in this patient who demonstrated inflammatory clinical features but negative laboratory findings.6 In this case, radiographs revealed periarticular osteopenia and potential erosions, and because of this RA remained in the differential diagnosis (Figs 1A and B).15 Periarticular osteopenia and the fifth metacarpal base erosions proved to be nonspecific findings in this case. The osteopenia likely is related to disuse, and the erosions without interval change are depressions, or normal variants in anatomy, and not from inflammatory resorption.16, 17 The equivocal radiographic features prompted ultrasound examination (Figs 2A, B, C, and D), which demonstrated no evidence of synovitis or bone erosion. Ultrasound is more sensitive than radiography in the evaluation of synovitis and erosions.15 In addition, ultrasound is widely available and low cost, does not use ionizing radiation, and allows for easy contralateral comparison.15
Management of hand OA targets symptom alleviation because there are no disease-modifying drugs available. In RA, especially if identified early, prompt referral to a rheumatologist to receive disease-modifying antirheumatic drugs results in optimal outcomes.5, 18
Conclusion
This case illuminates the similar presenting clinical features of hand OA and RA. Symptoms classically attributed to inflammatory arthritis are nonspecific and can be present in those with OA. Diagnosing symptomatic hand OA in the setting of inflammatory symptoms should be done cautiously, and both laboratory analysis and diagnostic imaging may be needed. In this case where laboratory analysis was negative and radiographic findings were equivocal, diagnostic ultrasound was definitive in making the diagnosis.
Practical Applications
-
•
This report illuminates the nonspecific clinical features of symptomatic hand OA and those with the features of RA.
-
•
This report demonstrates the most efficient diagnostic strategy using a combination of laboratory analysis and diagnostic imaging to differentiate the 2 conditions.
Alt-text: Unlabelled Box
Funding Sources and Conflicts of Interest
No funding sources or conflicts of interest were reported for this study.
Contributorship Information
Concept development (provided idea for the research): K.L.L., P.J.B.
Design (planned the methods to generate the results): K.L.L., P.J.B.
Supervision (provided oversight, responsible for organization and implementation, writing of the manuscript): K.L.L., P.J.B.
Literature search (performed the literature search): K.L.L., P.J.B.
Writing (responsible for writing a substantive part of the manuscript): K.L.L., P.J.B.
Critical review (revised manuscript for intellectual content, this does not relate to spelling and grammar checking): K.L.L., P.J.B.
References
- 1.Kloppenburg M, Kwok WY. Hand osteoarthritis—a heterogeneous disorder. Nat Rev Rheumatol. 2011;8(1):22–31. doi: 10.1038/nrrheum.2011.170. [DOI] [PubMed] [Google Scholar]
- 2.Zhang Y, Niu J, Kelly-Hayes M, Chaisson CE, Aliabadi P, Felson DT. Prevalence of symptomatic hand osteoarthritis and its impact on functional status among the elderly: the Framingham Study. Am J Epidemiol. 2002;156(11):1021–1027. doi: 10.1093/aje/kwf141. [DOI] [PubMed] [Google Scholar]
- 3.Beasley J. Osteoarthritis and rheumatoid arthritis: conservative therapeutic management. J Hand Ther. 2012;25(2):163–171. doi: 10.1016/j.jht.2011.11.001. quiz 172. [DOI] [PubMed] [Google Scholar]
- 4.Gabay O, Gabay C. Hand osteoarthritis: new insights. Joint Bone Spine. 2013;80(2):130–134. doi: 10.1016/j.jbspin.2012.06.011. [DOI] [PubMed] [Google Scholar]
- 5.Sayyid R, Uthman I. Hand osteoarthritis: an update on therapy. Arch Rheumatol. 2015;30(2):150–158. [Google Scholar]
- 6.Suresh E. Diagnosis of early rheumatoid arthritis: what the non-specialist needs to know. J R Soc Med. 2004;97(9):421–424. doi: 10.1258/jrsm.97.9.421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Singh JA, Furst DE, Bharat A. 2012 update of the 2008 American College of Rheumatology recommendations for the use of disease-modifying antirheumatic drugs and biologic agents in the treatment of rheumatoid arthritis. Arthritis Care Res (Hoboken) 2012;64(5):625–639. doi: 10.1002/acr.21641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen D, Shen J, Zhao W. Osteoarthritis: toward a comprehensive understanding of pathological mechanism. Bone Res. 2017;5 doi: 10.1038/boneres.2016.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bijlsma JW, Berenbaum F, Lafeber FP. Osteoarthritis: an update with relevance for clinical practice. Lancet. 2011;377(9783):2115–2126. doi: 10.1016/S0140-6736(11)60243-2. [DOI] [PubMed] [Google Scholar]
- 10.Leung GJ, Rainsford KD, Kean WF. Osteoarthritis of the hand I: aetiology and pathogenesis, risk factors, investigation and diagnosis. J Pharm Pharmacol. 2014;66(3):339–346. doi: 10.1111/jphp.12196. [DOI] [PubMed] [Google Scholar]
- 11.Wasserman AM. Diagnosis and management of rheumatoid arthritis. Am Fam Physician. 2011;84(11):1245–1252. [PubMed] [Google Scholar]
- 12.Zhang W, Doherty M, Leeb BF. EULAR evidence-based recommendations for the diagnosis of hand osteoarthritis: report of a task force of ESCISIT. Ann Rheum Dis. 2009;68(1):8–17. doi: 10.1136/ard.2007.084772. [DOI] [PubMed] [Google Scholar]
- 13.Haugen IK, Englund M, Aliabadi P. Prevalence, incidence and progression of hand osteoarthritis in the general population: the Framingham Osteoarthritis Study. Ann Rheum Dis. 2011;70(9):1581–1586. doi: 10.1136/ard.2011.150078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jacob J, Sartoris D, Kursunoglu S. Distal interphalangeal joint involvement in rheumatoid arthritis. Arthritis Rheum. 1986;29(1):10–15. doi: 10.1002/art.1780290102. [DOI] [PubMed] [Google Scholar]
- 15.Hayashi D, Roemer FW, Guermazi A. Imaging for osteoarthritis. Ann Phys Rehabil Med. 2016;59(3):161–169. doi: 10.1016/j.rehab.2015.12.003. [DOI] [PubMed] [Google Scholar]
- 16.Avenarius DF, Muller LS, Rosendahl K. Erosion or normal variant? 4-year MRI follow-up of the wrists in healthy children. Pediatr Radiol. 2016;46(3):322–330. doi: 10.1007/s00247-015-3494-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Giannotti S, Bottai V, Dell'osso G. Disuse osteoporosis of the upper limb: assessment of thirty patients. Clin Cases Miner Bone Metab. 2013;10(2):129–132. [PMC free article] [PubMed] [Google Scholar]
- 18.Bukhari MAS, Wiles NJ, Lunt M. Influence of disease-modifying therapy on radiographic outcome in inflammatory polyarthritis at five years: results from a large observational inception study. Arthritis Rheum. 2003;48(1):46–53. doi: 10.1002/art.10727. [DOI] [PubMed] [Google Scholar]


