Abstract
Background
Otitis externa has a lifetime prevalence of 10% and can arise in acute, chronic, and necrotizing forms.
Methods
This review is based on publications retrieved by a selective search of the pertinent literature.
Results
The treatment of acute otitis media consists of analgesia, cleansing of the external auditory canal, and the application of antiseptic and antimicrobial agents. Local antibiotic and corticosteroid preparations have been found useful, but there have been no large-scale randomized controlled trials of their use. Topical antimicrobial treatments lead to a higher cure rate than placebo, and corticosteroid preparations lessen swelling, erythema, and secretions. Oral antibiotics are indicated if the infection has spread beyond the ear canal or in patients with poorly controlled diabetes mellitus or immunosuppression. Chronic otitis externa is often due to an underlying skin disease. Malignant otitis externa, a destructive infection of the external auditory canal in which there is also osteomyelitis of the petrous bone, arises mainly in elderly diabetic or immunosuppressed patients and can be life-threatening.
Conclusion
With correct assessment of the different types of otitis externa, rapidly effective targeted treatment can be initiated, so that complications will be avoided and fewer cases will progress to chronic disease.
Otitis externa is one of the more common diseases in otorhinolaryngological practice and is also frequently encountered in primary and pediatric care. It ranges in severity from a mild infection of the external auditory canal to life-threatening malignant otitis externa. Its correct treatment requires a good understanding of the anatomy, physiology, and microbiology of the ear canal. No German guidelines deal specifically with otitis externa; it is briefly discussed in the AWMF-S2k guidelines on ear pain of the German College of General Practitioners and Family Physicians (Deutsche Gesellschaft für Allgemeinmedizin und Familienmedizin, DEGAM) (1). Here we discuss the epidemiology, etiology, and treatment of otitis externa in the light of the current scientific evidence.
Learning objectives
Readers of this article should
gain an overview of the epidemiology, anatomical setting, and causes of otitis externa,
understand the different forms of the disease, and
become acquainted with their treatment.
Methods
We selectively searched the PubMed database for controlled trials, guidelines, and reviews that appeared up to 30 April 2018 with the key words “otitis externa,” “acute external otitis,” “otitis externa diffusa,” “otitis externa circumscripta,” “chronic external otitis,” “otitis externa maligna,” and “otitis externa necroticans.”
Otitis externa
Definition.
Otitis externa is defined as an infection of the cutis and subcutis of the external auditory canal, possibly involving the tympanic membrane and the pinna as well.
Otitis externa is defined as an infection of the cutis and subcutis of the external auditory canal, possibly involving the tympanic membrane and the pinna as well. Its different forms include acute diffuse otitis externa, circumscribed otitis externa, chronic otitis externa, and malignant (i.e., necrotizing) otitis externa. Its differential diagnoses include perichondritis, erysipelas, otomycosis, herpes zoster oticus, otitis externa bullosa sive hemorrhagica, otitis media (with perforation), and eczema, cholesteatoma, or carcinoma involving the external auditory canal (2).
Anatomy and physiology
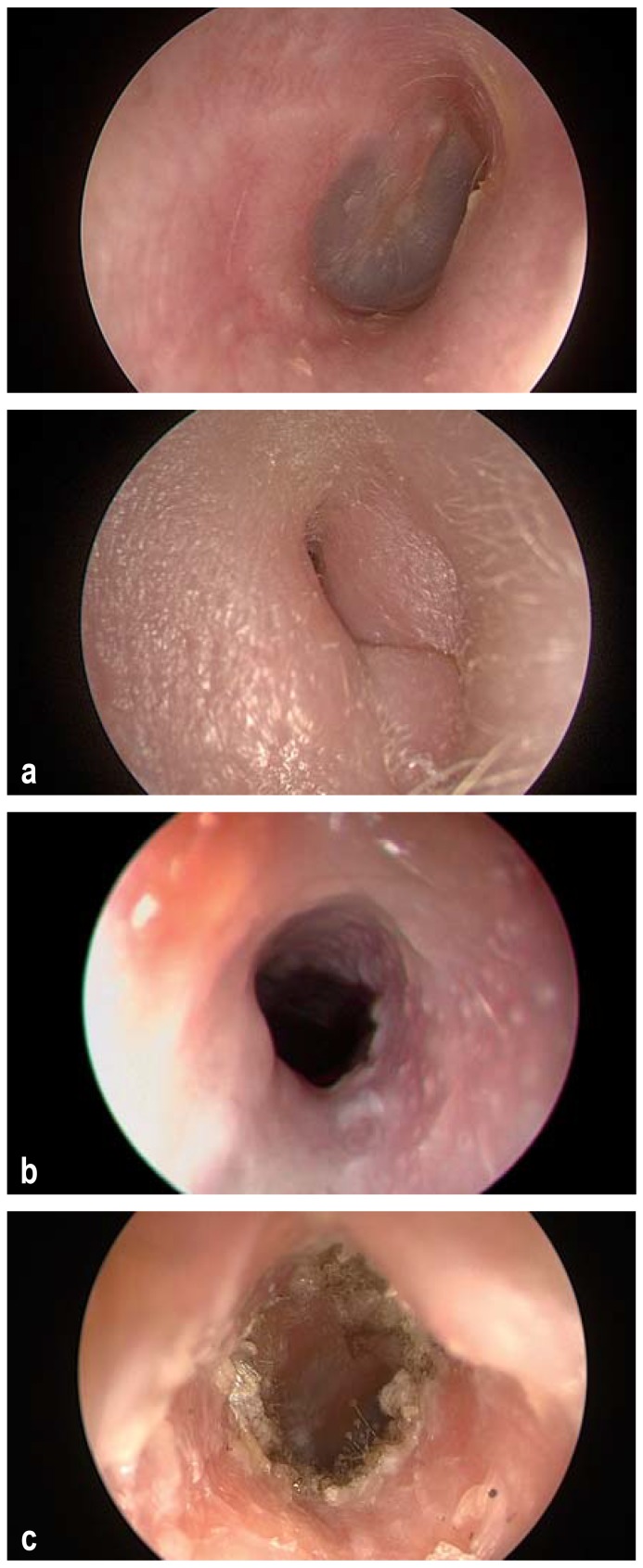
The external auditory canal (ear canal) has lateral cartilaginous and medial bony portions, with an overall length of 2–3.5 cm and a diameter of 5–9 mm (Figure 1a). The skin of the bony ear canal is firmly bound to the periosteum, while the skin of the cartilaginous ear canal lies on a layer of connective tissue and contains hair follicles, sebaceous glands, and apocrine ceruminous glands, whose exudates, combined with desquamated epithelial cells, form cerumen. The cartilaginous ear canal has a roof of connective tissue; its floor contains the connective-tissue clefts of Santorini, along which infections can spread to the parotid gland, infratemporal fossa, and skull base. The sensory innervation of the ear canal is from the auriculotemporal nerve, the auricular branch of the vagus nerve, the greater auricular nerve, and the posterior auricular nerve. The ear canal is normally colonized by bacteria, above all Staphylococcus and Corynebacterium species and streptococci (3). Its pH is normally in the range of 5–5.7; the acid environment and the hydrophobic properties of the cerumen inhibit bacterial growth (2).
Figure 1.
a) Normal right external auditory canal, with view of the eardrum.
b) Swollen introitus of the right external auditory canal in a patient with acute otitis externa.
c) An external auditory canal affected by bacterial otitis externa.
d) Otomycosis
Etiology and epidemiology
Otitis externa is common all over the world, with a higher incidence in tropical than in temperate zones because of the higher temperature and humidity. Its lifetime prevalence is estimated at 10% (4). It affects adults most commonly, and children only rarely (generally aged 7 to 12) (e1). Studies from the Netherlands and the United Kingdom have shown an annual incidence of circa 1% (5, e2). The incidence is increased fivefold in swimmers (6); thus, the condition is also called “swimmer’s ear.” The pathogenesis of otitis externa is multifactorial; a list of predisposing factors is shown in Table 1.
Table 1. Predisposing factors for otitis externa (modified from Schäfer et al. [7]).
| Anatomical factors | Skin diseases | Environmental factors | Trauma | Systemic diseases | Endogenous factors | Other factors |
| Stenosis of the external auditory canal Exostoses of the external auditory canal Heavy coverage of the external auditory canal with hair |
Eczema Psoriasis Seborrhea Neurodermatitis Other inflammatory diseases of the skin |
High humidity of the ambient air High ambient temperature |
Manipulation/ excoriation Cerumen removal Hearing aids Earplugs Foreign bodies |
Metabolic diseases Diabetes mellitus Immunosuppression |
Lack or overproduction of cerumen Sweating |
Water in the ear canal/ swimming Irritants (soap, shampoo, etc.) Radiation Chemotherapy Purulent otitis media Prior surgery of the external ear canal Stress |
More than 90% of cases of otitis externa are due to bacteria (6), most commonly Pseudomonas aeruginosa (22–62%) and Staphylococcus aureus (11–34%). Polymicrobial infection is common (8, e3– e5). Fungi are a rare cause of acute otitis externa (10%) (e6) and a more common cause of chronic otitis externa; typical pathogens are Aspergillus (60–90%) (9) and Candida species (10–40%) (e7). Predisposing factors for fungal otitis externa include long-term antibiotic use, immunosuppression, and diabetes mellitus.
Anatomy and physiology.
The cartilaginous ear canal has a roof of connective tissue; its floor contains the connective-tissue clefts of Santorini, along which infections can spread to the parotid gland, infratemporal fossa, and skull base.
Etiology and epidemiology.
More than 90% of cases of otitis externa are due to bacteria, most commonly Pseudomonas aeruginosa and Staphylococcus aureus. Polymicrobial infection is common. Fungi are a rare cause of acute otitis externa and a more common cause of chronic otitis externa.
The changes in the ear canal that are seen in otitis externa (e.g., hyperkeratosis of the epidermis, chronic granulation tissue, edema, or fibrosis of the dermis) tend to narrow the canal. Epithelial cell migration normally rids the ear canal of cerumen, cellular detritus, and microorganisms. Interference with this process by inflammation or stenosis predisposes to the development and maintenance of otitis externa.
Symptoms
The characteristic symptom of acute otitis externa is severe pain in the ear (otalgia) due to irritation of the periosteum just under the thin dermis of the bony ear canal, which has no subcutis. The pain is typically worsened by pressure on the tragus or tension on the pinna. Further symptoms are otorrhea, itch, erythema, and swelling of the ear canal, potentially leading to conductive hearing loss.
Diagnosis
Symptoms.
The characteristic symptom of acute otitis externa is severe pain in the ear (otalgia) due to irritation of the periosteum just under the thin dermis of the bony ear canal, which has no subcutis.
Otitis externa is diagnosed from the history and physical examination, including, as a minimum, otosopic or otomicroscopic examination of the ear canal and tympanic membrane (if visible), as well as examination of the pinna, the surrounding lymph nodes, and the skin. Especially if the tympanic membrane cannot be seen, screening tests of hearing or an audiological examination should be performed to rule out inner ear involvement. When the ear canal is swollen, the tuning-fork examination and the tone threshold audiogram typically reveal conductive hearing loss. The characteristic findings in acute otitis externa are pain induced by pressure on the tragus and tension on the pinna, along with swelling of the ear canal, perhaps to the point of total obstruction; the skin of the ear canal can be either erythematous or pale because of edema (Figures 1b, c). Secretion is common and can be swabbed for culture and pathogen resistance testing. Rarely, swelling makes the pinna protrude (pseudomastoiditis). Mild fever (up to 39°C) may be present; markedly higher temperatures suggest spread of the infection beyond the ear canal.
Treatment
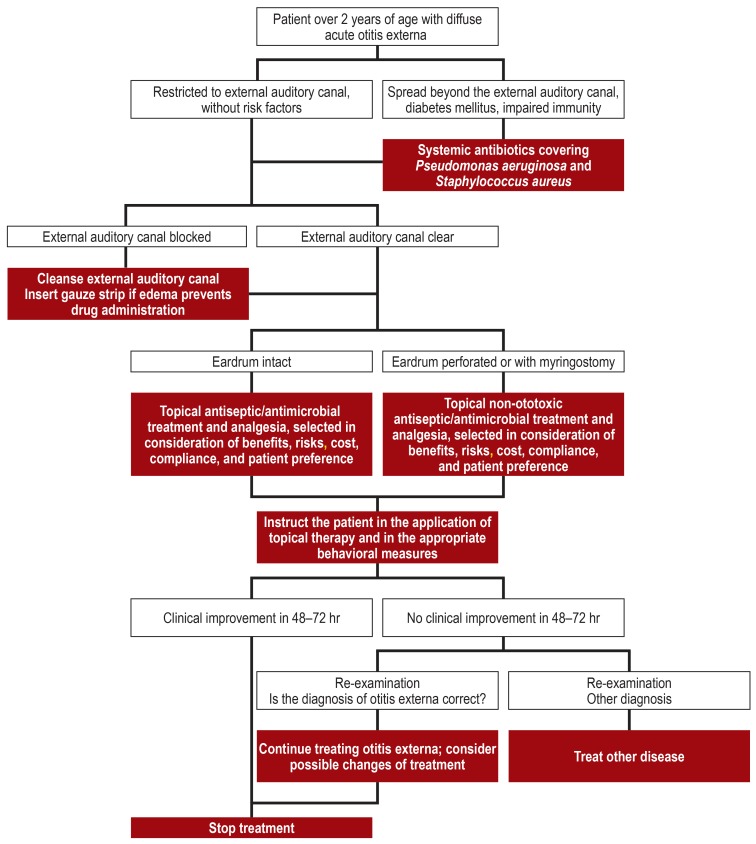
The treatment of uncomplicated acute otitis externa consists of cleansing the ear canal, topical antiseptic and antimicrobial treatment, and adequate analgesia. Primary oral antibiotic treatment should be given only if the infection has spread beyond the ear canal, in the setting of poorly controlled diabetes mellitus or immunosuppression, or if topical treatment is not possible (10) (figure 2). The DEGAM, in its guideline on ear pain, accordingly recommends cleansing the ear canal and using local antibiotics and/or corticosteroids as indicated, in consideration of their availability, costs, and risks. Systemic antibiotic treatment should be considered in individual cases if there are systemic manifestations, or whenever problematic organisms are found (1).
Figure 2.
Treatment algorithm for acute otitis externa (modified from Rosenfeld et al. [8])
Cleansing the ear canal
Treatment.
The treatment of uncomplicated acute otitis externa consists of cleansing the ear canal, topical antiseptic and antimicrobial treatment, and adequate analgesia.
Atraumatic cleansing of the ear canal consists of the removal of cerumen and exudate; the exudate may contain toxins (e.g., Pseudomonas exotoxin A [e8]) that sustain the inflammatory process and limit or prevent the efficacy of topical drugs. Cleansing should be performed by an experienced otorhinolaryngologist under microscopic vision with suction or an aural hook; injury to the ear canal must be avoided. Once a defect of the tympanic membrane has been ruled out, the ear canal can alternatively be cautiously rinsed with distilled water or normal saline. In rural areas without otolaryngology coverage, this can also be done by a general practitioner or pediatrician. Patients should not clean their own ears with cotton swabs, because microtrauma encourages bacterial invasion.
Cleansing of the external auditory canal: rationale.
Atraumatic cleansing of the ear canal consists of the removal of cerumen and exudate; the exudate may contain toxins that sustain the inflammatory process and limit or prevent the efficacy of topical drugs.
Cleansing of the external auditory canal: technique.
Cleansing should be performed by an experienced otorhinolaryngologist under microscopic vision with suction or an aural hook; injury to the ear canal must be avoided.
Topical treatment
Topical treatment.
Topical treatment with antiseptic agents, antibiotics, corticosteroids, and combinations of these is recommended for the treatment of uncomplicated acute otitis externa because of its safety, efficacy compared to placebo, and excellent results in randomized trials and meta-analyses.
Gauze strips.
No randomized trials have been performed on the insertion of a drug-soaked gauze strip into the ear canal as the sole treatment, but this method does seem to improve the local efficacy of topical treatment and to lessen inflammatory edema.
Topical treatment with antiseptic agents, antibiotics, corticosteroids, and combinations of these is recommended for the treatment of uncomplicated acute otitis externa because of its safety, efficacy compared to placebo, and excellent results in randomized trials and meta-analyses (10– 12, e9– e11). Whichever topical agent is used, 65–90% of patients improve clinically in 7–10 days (8). In a Cochrane meta-analysis of randomized controlled trials, antiseptic agents and antibiotics yielded equally good clinical results; no difference was found between single agents and combinations of agents, with or without additional corticosteroids (10). Nonetheless, the additional administration of topical steroids can lessen erythema and secretions. A few trials have shown different results from monotherapy as opposed to combination therapy, but the heterogeneity of the substances used makes it hard to draw any general conclusions (10). In a systematic review, topical antimicrobial drugs were found to increase the clinical cure rate by 46% and the bacteriological cure rate by 61% compared to placebo (11). Ototoxic substances must be avoided if the eardrum is perforated. No randomized trials have been performed on the insertion of a drug-soaked gauze strip into the ear canal as the sole treatment, but this method does seem to improve the local efficacy of topical treatment and to lessen inflammatory edema (10). The decisive factor for optimal topical treatment is patient instruction in how to apply the eardrops. The patient should lie on his or her side with the affected ear up, apply the drops in the ear canal, and keep lying on one side for 3–5 minutes thereafter. Gently moving the ear back and forth helps convey the drops to their site of action (8). The drops should be applied two to five times daily, depending on the preparation (table 2). Topical treatment leads to a cure of acute otitis externa in 65–90% of patients in 7–10 days, whatever agent is chosen (8). In the past, dyes such as gentian violet and acid brilliant green were commonly used for the local antiseptic and desiccating therapy of various ear diseases, but these are toxic and no longer approved for aural use.
Table 2. Eardrops that are approved in Germany for the topical treatment of otitis externa.
| Substance class |
Active agent or combination of active agents |
Approval | Dosage | Use in patients with eardrum perforation (according to manufacturer’s information*1) | Requires prescription? |
| Antibiotic eardrops |
Ciprofloxacin 2 mg/mL | Depending on preparation, from age 1 year or 2 years |
Depending on preparation, 0.25 mL bid for 7 days or 0.5 mL bid for 7 days |
Depending on preparation*2 no (restricted application) or yes |
Yes |
| Ciprofloxacin 3 mg/mL | From age 1 year | 3 drops bid (children) 4 drops bid (adults) |
Yes | Yes | |
| 7500 IU polymyxin B sulfate/mL 3500 IU neomycin sulfate/mL 0.02 mg gramicidin/mL |
No information | 2–3 drops 3–5×/d for 5–7 days | No | Yes | |
| Antibiotic and steroid eardrops | 3 mg ciprofloxacin/mL 1 mg dexamethasone/mL |
From age 1 year | 4 drops bid for 7 days | Yes | Yes |
| 3 mg ciprofloxacin/mL 0.25 mg fluocinolone acetonide/mL |
From age 6 months |
6–8 drops bid for 7 days | Yes | Yes | |
| Steroid eardrops | Fluocinolone acetonide 0.25 mg/mL | From age 18 years | 0.4 mL bid for 7 days | No | Yes |
| Steroid andanalgesic eardrops | Dexamethasone 0.224 mg/mL Cinchocaine 5.08 mg/mL Butane-1,3-diol 539.728 mg/mL |
No information | 2–4 drops tid-qid for a maximum of 10 days |
In case of perforated eardrum, treatment for a short time under an otologist’s supervision | Yes |
| Analgesic eardrops |
Phenazone 50 mg Procaine HCl 10 mg |
From age 3 years; in younger children only under a physician’s supervision | Age 0–2 years: only under a physician’s supervision Age 3–14 years: 2–3 drops tid-qid from age 15 years: 5 drops tid-qid |
No | No |
*1 Red list. The information provided here is taken from the information provided by the manufacturers.
*2 For one preparation containing ciprofloxacin 2 mg/mL, there is a restricted application in case of eardrum perforation, even though other preparations conaining ciprofloxacin in the same dose or a higher dose are permitted in case of eardrum perforation.
Topical antiseptic agents
The treatment of acute otitis externa with various topical antiseptic agents has been described, including acetic acid, chlorhexidine, aluminum acetate, silver nitrate, N-chlorotaurine, fuchsin, and eosin (5, 13, 14, e12– e14). The advantage of topical antiseptic agents is their broad-spectrum efficacy. Many preparations contain alcohol, which is an effective disinfectant and, in high concentration, removes water from tissue and thus lessens edema. pH reduction by acid preparations (e.g., 2% acetic acid) inhibits bacterial growth (3, 14), as most bacteria prefer a pH-neutral environment. Thus, otitis heals more rapidly if treated in this way rather than with placebo. Acetic acid is comparably effective to antibiotic or corticosteroid drops after 7 days of treatment, but significantly less effective if treatment is needed for 2–3 weeks (10).
Topical antibiotics
Acetic acid.
pH reduction by acid preparations (e.g., 2% acetic acid) inhibits bacterial growth, as most bacteria prefer a pH-neutral environment. Acetic acid is comparably effective to antibiotic or corticosteroid drops after 7 days of treatment.
Topical antibiotics should cover the most common pathogens, i.e., Pseudomonas aeruginosa and Staphylococcus aureus, and should be tailored to the drug resistance and sensitivity patterns of the cultured pathogen, if possible. The approved types of antibiotic eardrops in Germany contain quinolones (ciprofloxacin), aminoglycosides (neomycin), or polymyxins (polymyxin B) (table 2). Compared to placebo, these lead to more rapid symptomatic relief and cure, and to lower recurrence rates (11). Quinolones are highly effective and cause no local irritation, but prolonged exposure to them can lead to resistance against this important class of antibiotics. Neomycin is effective but ototoxic and should be given only if the eardrum is intact. It also causes contact dermatitis in 15–30% of patients (9, 15– 17, e15). Polymyxin monotherapy is not effective against? staphylococci and other Gram-positive microorganisms (9). A Cochrane analysis showed no difference in the clinical efficacy of quinolone versus non-quinolone preparations (10). In clinical practice, just as in clinical trials, ophthalmological antibiotic preparations are sometimes used off label to treat otitis externa; the most common active substance is ofloxacin (10, 11). Topical administration results in a high local concentration of drug without the side effects of systemic treatment. Nonetheless, for the reasons just explained, topical antibiotics such as ciprofloxacin or ofloxacin should not be given any longer than necessary. Ototoxic substances must not be used if the eardrum is perforated.
Topical corticosteroids
Topical corticosteroids are used mainly because they lessen edema; antibacterial and antifungal effects have also been described (3). Only individual case reports on topical corticosteroid monotherapy are available (18, 19), so the evidence for this practice is still weak (10). In a few randomized controlled trials, treatment with topical combinations of antibiotics and corticosteroids lessened swelling, erythema, and secretions more effectively than antibiotics alone. The greatest difference was seen during the first few days of treatment (20, 21). High-potency corticosteroids are probably more effective than low-potency corticosteroids against pain, inflammation, and swelling (22) (table 2).
Antifungal treatment
In case of fungal infection (Figure 1d), strips soaked in a solution of antifungal drug (ciclopirox, nystatin, clotrimazole, or miconazole) should be laid in the ear canal. Dye solutions are no longer recommended because of their potential toxicity to the inner ear and their low efficacy (23). If the eardrum is perforated, systemic antifungal treatment should be given according to the resistance and sensitivity pattern (e.g., fluconazole or itraconazole) (23).
Topical antibiotics.
Topical antibiotics should cover the most common pathogens, i.e., Pseudomonas aeruginosa and Staphylococcus aureus, and should be tailored to the drug resistance and sensitivity patterns of the cultured pathogen, if possible.
Analgesia
Pain relief is an essential part of the treatment of acute otitis externa. Severe ear pain arises because the highly sensitive periosteum of the bony ear canal is usually involved in the inflammatory process. Suitable analgesia should, therefore, be provided, e.g., with ibuprofen or acetaminophen. Topical local anesthetics can be used as well (table 2), unless the eardrum is perforated or a myringostomy tube is in place. Local anesthetics, however, can also mask progressive disease; if they are used, the patient should be followed up clinically in 48 hours so that the effect of treatment can be judged (8).
Oral antibiotic treatment
Despite the well-documented safety and efficacy of topical preparations, 20–40% of patients treated for acute otitis externa receive systemic antibiotics as their primary treatment (24, 25). This should be avoided in uncomplicated acute otitis externa because of the side effects and the risk of inducing drug resistance. On the other hand, oral antibiotics are indicated to treat acute otitis externa if the patient suffers from poorly controlled diabetes mellitus or immunosuppression, or if the infection extends beyond the ear canal. Antibiotics should be given that are effective against both Pseudomonas aeruginosa and Staphylococcus aureus (e.g., quinolones). Optimally, antibiotics should be tailored to the findings of bacterial culture and sensitivity testing.
Follow-up and secondary prevention
The response to treatment should be checked in 48–72 hours. If there is no response, the correctness of the diagnosis and the adequacy of treatment should be critically reconsidered, and the causative pathogen should be identified if possible. Known risk factors should be avoided to prevent further episodes of infection. In particular, the ear canal should be kept dry and should be dried with a hair dryer if water enters it (10). If the self-cleansing mechanism of the ear canal is dysfunctional, then the ear canal should be cleansed by a physician whenever the patient intends to spend a considerable amount of time swimming (e.g., a beach holiday).
Circumscribed otitis externa
Analgesia.
Pain relief is an essential part of the treatment of acute otitis externa. Severe ear pain arises because the highly sensitive periosteum of the bony ear canal is usually involved in the inflammatory process.
Circumscribed otitis externa is an abscess-forming infection of a hair follicle (i.e., a furuncle) in the cartilaginous part of the external auditory canal, mostly due to Staphylococcus aureus. If mild, it is treated with topical antibiotic eardrops, salves, or salve strips, along with analgesics. If more severe, it is additionally treated with oral antibiotics and lancing of the furuncle, as needed.
Chronic otitis externa
Manifestations of otitis externa lasting longer than three months, or more than four attacks of otitis externa per year, are designated as chronic otitis externa. This may result from inadequately treated acute otitis externa, although 15% of cases of acute otitis externa heal within 10 days (e16), but the cause usually lies elsewhere. Involvement of the ear canal by a skin disease such as atopic dermatitis or psoriasis is common. An alkaline pH in the ear canal due to the inflammatory process can also predispose to chronic otitis externa (e17). The chronic form of the condition affects both ears in more than half of patients (26). Its typical symptoms are itch and conductive hearing loss due to obstruction, while ear pain is rare. There are two main clinical presentations: the seborrheic form is characterized by a lack of cerumen and by dry, scaly, red, or shiny skin in the ear canal, the eczematous form by moist, erythematous skin (26). Itching can lead the patient to manipulate the ear canal, leading to excoriation and, in turn, to acute inflammation. Chronic inflammation causes progressive fibrosis of the ear canal.
Treatment
The goals of treatment are to return the skin of the ear canal to its original, normal state and to promote the production of cerumen. All potential irritants, such as shampoo or soap, should be kept away from the ear, and the ear canal should be kept dry. The treatment of underlying illnesses, such as skin diseases or autoimmune disorders, is the basis of therapy. Only a few randomized controlled trials on drug therapy for chronic otitis externa have been carried out, generally on a mixture of patients with acute or chronic otitis externa, so that no explicit recommendations can be derived for the treatment of chronic otitis externa as a distinct entity (e18– e20). The goal of topical treatment is to suppress chronic inflammation. Swabbing for culture, to exclude bacterial or fungal infection as the cause, is recommended. The application of strips soaked in alcohol or corticosteroid solution can locally lessen edema. In case of an acute exacerbation, topical antibacterial or antifungal drugs may be needed. Chronic otitis externa often fails to respond to treatment administered for several weeks.
Circumscribed otitis externa.
Circumscribed otitis externa is an abscess-forming infection of a hair follicle (i.e., a furuncle) in the cartilaginous part of the external auditory canal, mostly due to Staphylococcus aureus.
Oral corticosteroids can be effective in cases resistant to other forms of treatment (27). Local treatment with tacrolimus has been described as well (28). Surgical canaloplasty to widen the ear canal is only indicated if the canal is stenotic.
Malignant (necrotizing) otitis externa
Malignant (necrotizing) otitis externa is a destructive infection of the external auditory canal with invasive perichondritis and osteomyelitis of the lateral skull base, arising mainly in elderly men who are either diabetic or immunosuppressed (29). Its incidence is not precisely known. Rare cases have been described in severely immunocompromised children, such as children with acute leukemia or who have undergone bone marrow transplantation (e21, e22). Early diagnosis is essential; intractable otitis externa should always prompt the suspicion that the patient might actually be suffering from the malignant (necrotizing) form of the condition.
Diagnosis and manifestations
Chronic otitis externa.
The typical symptom is itch. There are two main clinical presentations: the seborrheic form is characterized by a lack of cerumen and by dry, scaly, red, or shiny skin in the ear canal, the eczematous form by moist, erythematous skin.
In about 90% of cases, Pseudomonas aeruginosa can be isolated from the exudate in the ear canal (6, e23). Proteases released into the surrounding tissue can cause marked tissue destruction and accompanying vasculitis (30). The infection can spread along the clefts of Santorini to the parotid gland, the periauricular soft tissue, and the temporomandibular joint. Spread of infection along the skull base can lead to inner ear damage, cranial nerve deficits, venous sinus thrombosis, meningitis, and brain abscess. Otalgia is intense, but nonspecific (frequency, 84–100% [29]); along with conductive hearing loss and fetid otorrhea (frequency, 17.6–100% [29]), granulations or polyps are typically found in the floor of the ear canal (frequency, 42.1–100% [29]), sometimes with exposed bone, particularly at the junction of the bony and cartilaginous portions of the canal, due to the underlying osteitis (8) (figure 3). Further manifestations can arise that reflect further complications. Imaging studies typically reveal soft-tissue swelling in the external auditory canal. Petrous osteomyelitis is manifested by bony destruction, usually (80%) spreading toward the temporomandibular joint and the clivus (31). The gold standard for the diagnostic imaging of petrous osteomyelitis is a combination of static and functional imaging (where available), with fluorodeoxyglcose positron-emission tomography and magnetic resonance imaging (FDG-PET/MRI) as well as high-resolution computed tomography (CT). Functional imaging enables the detection of osteitis in an early stage before bone erosion can be seen on CT (31). The advantages and disadvantages of each imaging modality for the evaluation of petrous osteomyelitis are listed in Table 3. A biopsy should always be performed to rule out a malignant tumor or cholesteatoma of the external auditory canal. Malignant otitis media is very rare in children; when it is suspected, MRI is the imaging study of choice.
Figure 3.
Exposed bone in the floor of the external auditory canal in a patient with malignant otitis externa
Table 3. Relative advantages and disadvantages of various imaging modalities for the diagnosis and follow-up of skull-base osteomyelitis (in analogy to van Kroonenburgh et al. [31]).
| Features | Radiological techniques | Nuclear medicine techniques | Hybrid techniques | ||
| CT | MRI | SPECT (Tc99m-MDP) | FDG-PET/CT | FDG-PET/MRI | |
| Bone erosion | ++ | − | − | + | − |
| (Bone) metabolism | − | − | + | + | + |
| Soft tissue | ± | + | − | ± | + |
| Spatial resolution | + | ++ | − | ± | + |
| Radiation exposure | − | + | − | − | ± |
| Follow-up | − | − | − | ± | + |
CT, computed tomography; FDG-PET, fluorodeoxyglucose positron-emission tomography; MRI, magnetic resonance imaging;
SPECT (Tc99m-MDP), single-photon-emission computed tomography (technetium-99m-methylene diphosphonate)
Treatment
Malignant (necrotizing) otitis externa.
Malignant (necrotizing) otitis externa is a destructive infection of the external auditory canal with invasive perichondritis and osteomyelitis of the lateral skull base, arising mainly in elderly men who are either diabetic or immunosuppressed.
High-grade evidence on the treatment of malignant otitis externa is lacking (29). Pathogen-specific parenteral or oral antibiotics, tailored to the findings of sensitivity and resistance testing, are recommended for at least 4–6 weeks (29, 32), as it takes this long for the involved bone to become revascularized (33). If the sensitivity and resistance testing is not yet definitive, empirical antibiotic treatment against Pseudomonas aeruginosa should be begun, depending on the severity of the condition. Topical treatment with antiseptic or antimicrobial strips in the ear canal can be given in addition. If the condition takes a protracted course or fails to respond to medical treatment, necrotic tissue and bone sequestra should be surgically removed, because they impair the penetration of antibiotics and the body’s own defensive substances into the involved tissue (34). Extensive resection in the region of the lateral skull base does not improve the outcome. Optimal blood sugar control is mandatory. Accompanying hyperbaric oxygen therapy may increase the cure rate, but no randomized controlled trials on this topic are available (35). Regular clinical and radiological follow-up examinations are needed to document the response to treatment and to detect any recurrence. The suggested strategies range from imaging only if new symptoms arise to intermittent imaging at 2–6 week intervals until no infectious process can be seen any longer (36). Petrous bone osteomyelitis in malignant otitis externa is associated with a mortality of 10–21% (17, 37– 39, e24). Mortality is elevated if two or more of the following factors are present: age >70, diabetes mellitus, facial nerve palsy, or a positive CT (bone erosion, soft-tissue swelling) (40).
Conclusions for routine clinical practice
Otitis externa is diagnosed from the history and physical examination. Uncomplicated acute otitis externa can be treated to good effect with cleansing of the ear canal, antiseptic or antibiotic eardrops with or without corticosteroids, and preventive measures. Otomycosis should be treated with antifungal agents. For patients with chronic otitis externa, irritating substances should be kept away from the ear, and potential underlying diseases should be treated. Persistent otitis externa, granulation tissue, or freely exposed bone in the external auditory canal may be a sign of malignant (necrotizing) otitis externa. Early diagnosis and the rapid initiation of a 4- to 6-week course of antibiotics help lower the morbidity and mortality of this condition.
Petrous osteomyelitis.
The gold standard for the diagnostic imaging of petrous osteomyelitis is a combination of static and functional imaging (where available), with FDG-PET/MRI as well as high-resolution CT.
Resistance to treatment.
If the condition takes a protracted course or fails to respond to medical treatment, necrotic tissue and bone sequestra should be surgically removed, because they impair the penetration of antibiotics and the body’s own defensive substances into the involved tissue.
Further Information on CME\.
Participation in the CME certification program is possible only over the Internet: cme.aerzteblatt.de. This unit can be accessed until 23 June 2019. Submissions by letter, e-mail, or fax cannot be considered.
-
The following CME units can still be accessed for credit:
Acute Renal Failure of Nosocomial Origin” (issue 9/2019) until 26 May 2019
Determinants of Perioperative Outcome in Frail Older Patients” (issue 5/2019) until 28 April 2019
The Management of Pilonidal Sinus” (issue 1–2/2019) until 31 March 2019
This article has been certified by the North Rhine Academy for Continuing Medical Education. Participants in the CME program can manage their CME points with their 15-digit “uniform CME number” (einheitliche Fortbildungsnummer, EFN), which is found on the CME card (8027XXXXXXXXXXX). The EFN must be stated during registration on www.aerzteblatt.de (“Mein DÄ”) or else entered in “Meine Daten,” and the participant must agree to communication of the results.
CME credit for this unit can be obtained via cme.aerzteblatt.de until 23 June 2019. Only one answer is possible per question. Please select the answer that is most appropriate.
Question 1
What is the estimated lifetime prevalence of otitis externa?
2%
5%
10%
15%
20%
Question 2
What pathogens most commonly cause otitis externa?
Streptococcus viridans and Aspergillus fumigatus
Klebsiella pneumoniae and Escherichia coli
Staphylococcus epidermidis and Candida albicans
Pseudomonas aeruginosa and Staphylococcus aureus
Actinomyces israelii and Streptococcus pyogenes
Question 3
What is a typical symptom of uncomplicated acute otitis externa?
Pain induced by pressure on the tragus
Bloody otorrhea
Dizziness
Tinnitus
Sensorineural hearing loss
Question 4
Which of the following promotes and accelerates healing of acute otitis externa?
The patient’s regular cleansing of the ear canal with a swab
The insertion of a myringostomy tube
Hyperbaric oxygen therapy
The venous administration of anti-inflammatory drugs
Acidic eardrops
Question 5
Which of the following patients with acute otitis externa should be treated with systemic antibiotics?
An 8-year-old girl with an indwelling myringostomy tube
A 25-year-old-man with flu-like symptoms
A 37-year-old woman with diabetes mellitus
A 60-year-old man with conductive hearing loss
A 73-year-old woman with reduced mobility
Question 6
With what disease is malignant otitis externa most commonly associated?
Gout
Type 2 diabetes mellitus
Multiple sclerosis
Wegener disease
Cholesteatoma
Question 7
What is the correct duration of initial antibiotic treatment for culture-proven malignant external otitis?
3–5 days
7–10 days
1–2 weeks
3–4 weeks
4–6 weeks
Question 8
What is the mortality associated with petrous osteomyelitis in malignant external otitis?
10–21%
22–33%
34–45%
46–57%
58–69%
Question 9
Which of the following is a typical sign of malignant external otitis?
Granulations in the floor of the ear canal with exposed bone
Disordered epithelial layering with polymorphic nuclei and areas of squamous epithelium that appear to be inverted
Sensorineural hearing loss of more than 40 dB at 3 kHz
Positive Candida albicans culture from an ear canal swab
Perforation of the eardrum in the anterior inferior quadrant
Question 10
Which of the following predisposes to acute otitis externa?
Status post tympanoplasty
Low temperature in the environment
Low air humidity
Prolonged exposure to water
Little or no coverage of the ear canal with hair
► Participation is possible only via the internet: cme.aerzteblatt.de
Acknowledgments
Translated from the original German by Ethan Taub, M.D.
Footnotes
Conflict of interest statement
The authors state that they have no conflict of interest.
References
- 1.Leitlinie der Deutschen Gesellschaft für Allgemeinmedizin und Familienmedizin (DEGAM) Ohrenschmerzen. www.awmf.org/uploads/tx_szleitlinien/053-009l_S2k_Ohrenschmerzen_2014-12-verlaengert.pdf (last accessed on 25 January 2019) [Google Scholar]
- 2.Neher A, Nagl M, Scholtz AW. Otitis externa. HNO. 2008;56:1067–1080. doi: 10.1007/s00106-008-1830-y. [DOI] [PubMed] [Google Scholar]
- 3.Stroman DW, Roland PS, Dohar J, Burt W. Microbiology of normal external auditory canal. Laryngoscope. 2001;111:2054–2059. doi: 10.1097/00005537-200111000-00035. [DOI] [PubMed] [Google Scholar]
- 4.Raza SA, Denholm SW, Wong JC. An audit of the management of otitis externa in an ENT casualty clinic. J Laryngol Otol. 1995;109:130–133. doi: 10.1017/s0022215100129469. [DOI] [PubMed] [Google Scholar]
- 5.van Balen FA, Smit WM, Zuithoff NP, Verheij TJ. Clinical efficacy of three common treatments in acute otitis externa in primary care: randomised controlled trial. BMJ. 2003;327:1201–1205. doi: 10.1136/bmj.327.7425.1201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Roland PS, Stroman DW. Microbiology of acute otitis externa. Laryngoscope. 2002;112:1166–1177. doi: 10.1097/00005537-200207000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Schaefer P, Baugh RF. Acute otitis externa: an update. Am Fam Physician. 2012;86:1055–1061. [PubMed] [Google Scholar]
- 8.Rosenfeld RM, Schwartz SR, Cannon CR, et al. Clinical practice guideline: acute otitis externa. Otolaryngol Head Neck Surg. 2014;150(1):S1–S24. doi: 10.1177/0194599813517083. [DOI] [PubMed] [Google Scholar]
- 9.Sander R. Otitis externa: A practical guide to treatment and prevention. Am Fam Physician. 2001;63:927–937. [PubMed] [Google Scholar]
- 10.Kaushik V, Malik T, Saeed SR. Interventions for acute otitis externa. Cochrane Database Syst Rev. 2010;1 doi: 10.1002/14651858.CD004740.pub2. CD004740. [DOI] [PubMed] [Google Scholar]
- 11.Rosenfeld RM, Singer M, Wasserman JM, Stinnett SS. Systematic review of topical antimicrobial therapy for acute otitis externa. Otolaryngol Head Neck Surg. 2006 134;(4):24–48. doi: 10.1016/j.otohns.2006.02.013. [DOI] [PubMed] [Google Scholar]
- 12.Mösges R, Nematian-Samani M, Hellmich M, Shah-Hosseini K. A meta-analysis of the efficacy of quinolone containing otics in comparison to antibiotic-steroid combination drugs in the local treatment of otitis externa. Curr Med Res Opin. 2011;27:2053–2060. doi: 10.1185/03007995.2011.616192. [DOI] [PubMed] [Google Scholar]
- 13.van Hasselt P, Gudde H. Randomized controlled trial on the treatment of otitis externa with one per cent silver nitrate gel. J Laryngol Otol. 2004;118:93–6. doi: 10.1258/002221504772784513. [DOI] [PubMed] [Google Scholar]
- 14.Neher A, Nagl M, Appenroth E, et al. Acute otitis externa: efficacy and tolerability of N-chlorotaurine, a novel endogenous antiseptic agent. Laryngoscope. 2004;114:850–854. doi: 10.1097/00005537-200405000-00011. [DOI] [PubMed] [Google Scholar]
- 15.Sood S, Strachan DR, Tsikoudas A, Stables GI. Allergic otitis externa. Clin Otolaryngol Allied Sci. 2002;27:233–236. doi: 10.1046/j.1365-2273.2002.00584.x. [DOI] [PubMed] [Google Scholar]
- 16.Rutka J. Acute otitis externa: treatment perspectives. Ear Nose Throat J. 2004;83(9) 4:20–21. [PubMed] [Google Scholar]
- 17.Fischer M, Dietz A. Die akute Otitis externa und ihre Differentialdiagnosen. Laryngorhinootol. 2015;94:113–125. doi: 10.1055/s-0034-1396837. [DOI] [PubMed] [Google Scholar]
- 18.Emgard P, Hellstrom S. A group III steroid solution without antibiotic components: an effective cure for external otitis. J Laryngol Otol. 2005;119:342–347. doi: 10.1258/0022215053945705. [DOI] [PubMed] [Google Scholar]
- 19.Emgard P, Hellstrom S, Holm S. External otitis caused by infection with pseudomonas aeruginosa or candida albicans cured by use of a topical group III steroid, without any antibiotics. Acta Otolaryngol. 2005;125:346–352. doi: 10.1080/00016480510027529. [DOI] [PubMed] [Google Scholar]
- 20.Mösges R, Domröse CM, Löffler J. Topical treatment of acute otitis externa: clinical comparison of an antibiotics ointment alone or in combination with hydrocortisone acetate. Eur Arch Otorhinolaryngol. 2007;264:1087–1094. doi: 10.1007/s00405-007-0314-0. [DOI] [PubMed] [Google Scholar]
- 21.Mösges R, Schröder T, Baues CM, Sahin K. Dexamethasone phosphate in antibiotic ear drops for the treatment of acute bacterial otitis externa. Curr Med Res Opin. 2008;24:2339–2347. doi: 10.1185/03007990802285086. [DOI] [PubMed] [Google Scholar]
- 22.Roland PS, Younis R, Wall GM. A comparison of ciprofloxacin/dexamethasone with neomycin/polymyxin/hydrocortisone for otitis externa pain. Adv Ther. 2007;24:671–675. doi: 10.1007/BF02848792. [DOI] [PubMed] [Google Scholar]
- 23.Tietz HJ. Pilzbedingte Otitis externa Wie werden Gehörgangsmykosen lege artis behandelt? HNO-Nachrichten. 2014;44 [Google Scholar]
- 24.McCormick AW, Whitney CG, Farley MM, et al. Geographic diversity and temporal trends of antimicrobial resistance in streptococcus pneumoniae in the United States. Nat Med. 2003;9:424–430. doi: 10.1038/nm839. [DOI] [PubMed] [Google Scholar]
- 25.Bhattacharyya N, Kepnes L. Initial impact of the acute otitis externa clinical practice guideline on clinical care. Otolaryngol Head Neck Surg. 2011;145:414–417. doi: 10.1177/0194599811406797. [DOI] [PubMed] [Google Scholar]
- 26.Kesser BW. Assessment and management of chronic otitis externa. Curr Opin Otolaryngol Head Neck Surg. 2011;19:341–347. doi: 10.1097/MOO.0b013e328349a125. [DOI] [PubMed] [Google Scholar]
- 27.Golder J. Oral steroids in the treatment of otitis externa. Aust Fam Physician. 1999;28 [PubMed] [Google Scholar]
- 28.Caffier PP, Harth W, Mayelzadeh B, Haupt H, Scherer H, Sedlmaier B. Topische Immunmodulation Ein Meilenstein in der Behandlung der therapieresistenten nichtinfektiösen chronischen Otitis externa? HNO. 2008;56:530–537. doi: 10.1007/s00106-007-1615-8. [DOI] [PubMed] [Google Scholar]
- 29.Mahdyoun P, Pulcini C, Gahide I, et al. Necrotizing otitis externa: a systematic review. Otol Neurotol. 2013;34:620–629. doi: 10.1097/MAO.0b013e3182804aee. [DOI] [PubMed] [Google Scholar]
- 30.Tisch M, Maier H. Otitis externa necroticans. Laryngorhinootol. 2006;85:763–769. doi: 10.1055/s-2006-925441. [DOI] [PubMed] [Google Scholar]
- 31.van Kroonenburgh AMJL, van der Meer WL, Bothof RJP, van Tilburg M, van Tongeren J, Postma AA. Advanced imaging techniques in skull base osteomyelitis due to malignant otitis externa. Curr Radiol Rep. 2018;6 doi: 10.1007/s40134-018-0263-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Conterno LO, da Silva Filho CR. Antibiotics for treating chronic osteomyelitis in adults. Cochrane Database Syst Rev. 2009;(3) doi: 10.1002/14651858.CD004439.pub2. CD004439. [DOI] [PubMed] [Google Scholar]
- 33.Courson AM, Vikram HR, Barrs DM. What are the criteria for terminating treatment for necrotizing (malignant) otitis externa? Laryngoscope. 2014;124:361–362. doi: 10.1002/lary.24093. [DOI] [PubMed] [Google Scholar]
- 34.Tisch M, Lorenz KJ, Harm M, Lampl L, Maier H. Otitis externa necroticans Kombinierter Einsatz von chirurgischer Therapie, Antibiose, spezifischen Immunglobulinen und hyperbarer Sauerstofftherapie - Ergebnisse des Ulmer Therapiekonzepts. HNO. 2003;51:315–320. doi: 10.1007/s00106-002-0713-x. [DOI] [PubMed] [Google Scholar]
- 35.Phillips JS, Jones SE. Hyperbaric oxygen as an adjuvant treatment for malignant otitis externa. Cochrane Database Syst Rev. 2013;5 doi: 10.1002/14651858.CD004617.pub3. CD004617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Le Clerc N, Verillaud B, Duet M, Guichard JP, Herman P, Kania R. Skull base osteomyelitis: incidence of resistance, morbidity, and treatment strategy. Laryngoscope. 2014;124:2013–2016. doi: 10.1002/lary.24726. [DOI] [PubMed] [Google Scholar]
- 37.Stevens SM, Lambert PR, Baker AB, Meyer TA. Malignant otitis externa: a novel stratification protocol for predicting treatment outcomes. Otol Neurotol. 2015;36:1492–1498. doi: 10.1097/MAO.0000000000000839. [DOI] [PubMed] [Google Scholar]
- 38.Chen CN, Chen YS, Yeh TH, Hsu CJ, Tseng FY. Outcomes of malignant external otitis: survival vs mortality. Acta Otolaryngol. 2010;130:89–94. doi: 10.3109/00016480902971247. [DOI] [PubMed] [Google Scholar]
- 39.Glikson E, Sagiv D, Wolf M, Shapira Y. Necrotizing otitis externa: diagnosis, treatment, and outcome in a case series. Diagn Microbiol Infect Dis. 2017;87:74–78. doi: 10.1016/j.diagmicrobio.2016.10.017. [DOI] [PubMed] [Google Scholar]
- 40.Stern Shavit S, Soudry E, Hamzany Y, Nageris B. Malignant external otitis: factors predicting patient outcomes. Am J Otolaryngol. 2016;37:425–430. doi: 10.1016/j.amjoto.2016.04.005. [DOI] [PubMed] [Google Scholar]
- E1.Hajioff D, MacKeith S. Otitis externa. BMJ Clin Evid. 2015;06 [PMC free article] [PubMed] [Google Scholar]
- E2.Mustafa M, Patawari P, Sien MM, Muniandy RK, Zinatara P. Acute otitis externa: pathophysiology, clinical presentation, and treatment. IOSR. 2015;147:3–8. [Google Scholar]
- E3.Ong YK, Chee G. Infections of the external ear. Ann Acad Med Singapore. 2005;34:330–334. [PubMed] [Google Scholar]
- E4.Musso MF, Crews JD. Infections of the external ear. Inf Dis Ped Otolaryngol. 2016:15–28. [Google Scholar]
- E5.Ijaz T, Anjum AA, Aslam S, Raja SA, Khawaja AR, Ljaz S. Microbial profiling and risk factors assessment for otitis media and otitis externa. Advancements in Life Sciences. 2014:191–196. [Google Scholar]
- E6.Boustred N. Practical guide to otitis externa. Aust Fam Physician. 1999;28:217–221. [PubMed] [Google Scholar]
- E7.Kaur RK, Mittal N, Kakkar M, Aggarwal AK, Mathur MD. Otomycosis: a clinico mycologic study. Ear Nose Throat J. 2000;79:606–609. [PubMed] [Google Scholar]
- E8.Al-zubaidy BJ, Abdulrahman TR, Ahmed WA. Detection of exo a gene in Pseudomonas aeruginosa from human and dogs using polymerase chain reaction. IOSR. 2014;9:38–41. [Google Scholar]
- E9.Connon SJ, Grunwaldt E. Treatment of otitis externa with a tropical steroid-antibiotic combination. Eye Ear Nose Throat Mon. 1967;46:1296–1302. [PubMed] [Google Scholar]
- E10.Cannon S. External otitis: controlled therapeutic trial. Eye Ear Nose Throat Mon. 1970;49:186–189. [PubMed] [Google Scholar]
- E11.Freedman R. Versus placebo in treatment of acute otitis externa. Ear Nose Throat J. 1978;57:198–204. [PubMed] [Google Scholar]
- E12.Kime CE, Ordonez GE, Updegraff WR, Glassman JM, Soyka JP. Effective treatment of acute diffuse otitis externa: II A controlled comparison of hydrocortisone-acetic acid, nonaqueous and hydrocortisone-neomycin-colistin otic solutions. Curr Ther Res Clin Exp. 1978;23(5):3–14. [Google Scholar]
- E13.Clayton MI, Osborne JE, Rutherford D, Rivron RP. A double-blind, randomized, prospective trial of a topical antiseptic versus a topical antibiotic in the treatment of otorrhoea. Clin Otolaryngol Allied Sci. 1990;15:7–10. doi: 10.1111/j.1365-2273.1990.tb00425.x. [DOI] [PubMed] [Google Scholar]
- E14.Lambert IJ. A comparison of the treatment of otitis externa with Otosporin and aluminium acetate: a report from a services practice in Cyprus. J Royal Col Gen Pract. 1981;31:291–294. [PMC free article] [PubMed] [Google Scholar]
- E15.Devos SA, Mulder JJ, van der Valk PG. The relevance of positive patch test reactions in chronic otitis externa. Contact Dermatitis. 2000;42:354–355. [PubMed] [Google Scholar]
- E16.Mösges R, Domröse C. Otitis externa — Ihr Leitfaden zur Therapie. MMW. 2008;150:41–43. doi: 10.1007/BF03365384. [DOI] [PubMed] [Google Scholar]
- E17.Martinez Devesa P, Willis CM, Capper JW. External auditory canal pH in chronic otitis externa. Clin Otolaryngol Allied Sci. 2003;28:320–324. doi: 10.1046/j.1365-2273.2003.00713.x. [DOI] [PubMed] [Google Scholar]
- E18.Cannon SJ, Grunwaldt E. Treatment of otitis externa with a tropical steroid-antibiotic combination. Eye Ear Nose Throat Mon. 1967;46:1296–1302. [PubMed] [Google Scholar]
- E19.Worgan D. Treatment of otitis externa Report of a clinical trial. Practitioner. 1969;202:817–820. [PubMed] [Google Scholar]
- E20.Smith RB, Moodie J. A general practice study to compare the efficacy and toler- ability of a spray (“Otomize”) versus a standard drop formulation (“Sofradex”) in the treatment of patients with otitis externa. Curr Med Res Opin. 1990;12:12–18. doi: 10.1185/03007999009111486. [DOI] [PubMed] [Google Scholar]
- E21.Sobie S, Brodsky L, Stanievich JF. Necrotizing external otitis in children: report of two cases and review of the literature. Laryngoscope. 1987;97:598–601. doi: 10.1288/00005537-198705000-00012. [DOI] [PubMed] [Google Scholar]
- E22.Tezcan I, Tuncer AM, Yenicesu I, et al. Necrotizing otitis externa, otitis media, peripheral facial paralysis, and brain abscess in a thalassemic child after allogeneic BMT. Pediatr Hematol Oncol. 1998;15:459–462. doi: 10.3109/08880019809016578. [DOI] [PubMed] [Google Scholar]
- E23.Bovo R, Benatti A, Ciorba A, Libanore M, Borrelli M, Martini A. Pseudomonas and aspergillus interaction in malignant external otitis: risk of treatment failure. Acta Otorhinolaryngol Ital. 2012;32:416–419. [PMC free article] [PubMed] [Google Scholar]
- E24.Loh S, Loh WS. Malignant otitis externa: an Asian perspective on treatment outcomes and prognostic factors. Otolaryngol Head Neck Surg. 2013;148:991–996. doi: 10.1177/0194599813482107. [DOI] [PubMed] [Google Scholar]