Abstract
Fogging is a deceptive phenomenon that can partially or completely obscure a subacute infarct on noncontrast head CT. We present the appearance of infarct fogging on CT perfusion through 3 cases. At time of fogging, the subacute infarctions demonstrated variable mean transit time with increased cerebral blood volume and cerebral blood flow on CT perfusion. Fogging occurred within 6-10 days, sooner than the previously described 2-3 weeks in classic fogging. At time of fogging, CT perfusion demonstrated a “luxury-like” perfusion pattern and augmented the identification of the true extent of the infarction at time of fogging.
Keywords: Fogging effect, Cerebral infarct/stroke, Vasospasm, CT perfusion, Noncontrast head CT
Introduction
Infarct fogging refers to the transient iso-dense appearance of a previously hypodense infarct on noncontrast head CT (NCCT) [1], [2]. The “fogging effect” generally occurs 2-3 weeks after stroke onset with redemonstration of hypoattenuation on follow-up imaging [1], [2]. Recognition of fogging on NCCT is imperative to avoid underestimation or misdiagnosis of cerebral infarction [1]. This may be especially important to be aware of when assessing a new stroke patient transferred from an outside hospital without available comparison imaging or for junior radiology trainees unfamiliar with infarct confounders.
Comparison to follow-up neurologic imaging can facilitate the identification of infarct fogging [1], [2]. In an ischemic stroke patient, CT perfusion (CTP) can be used to assess blood flow within ischemic parenchyma [3], [4]. We present the appearance of infarct fogging on CTP through 3 cases (Tables 1 and 2).
Table 1.
Patient characteristics and CT perfusion findings at time of infarct fogging.
| Age and gender | Initial presentation | Infarction | Prior intra-arterial Verapamil before fogging (days) | Prior contrast before fogging (days) | Time from infarct to fogging (days) | |
|---|---|---|---|---|---|---|
| Case 1 | 55F | Right ACom aneurysm and SAH | Vasospasm causing right ACA infarction | No | 6 | 6 |
| Case 2 | 47F | Right basal ganglia ICH/IVH | Vasospasm causing right MCA/PCA infarction | 7 | 4 | 7 |
| Case 3 | 52F | Right posterior communicating artery aneurysm and SAH | Vasospasm causing multiple right MCA infarcts | 12 | 7 | 10 |
Table 2.
| Stroke type | MTT | CBV | CBF |
|---|---|---|---|
| Chronic infarction | ↑ | ↓ | ↓ |
| Acute Core | ↑ | ↓ | ↓ |
| Acute Penumbra/Vasospasm | ↑ | ↑↔ | ↓ |
| Luxury Perfusion/Subacute Fogginga | ↓↑ | ↑ | ↑ |
Based on the 3 cases presented.
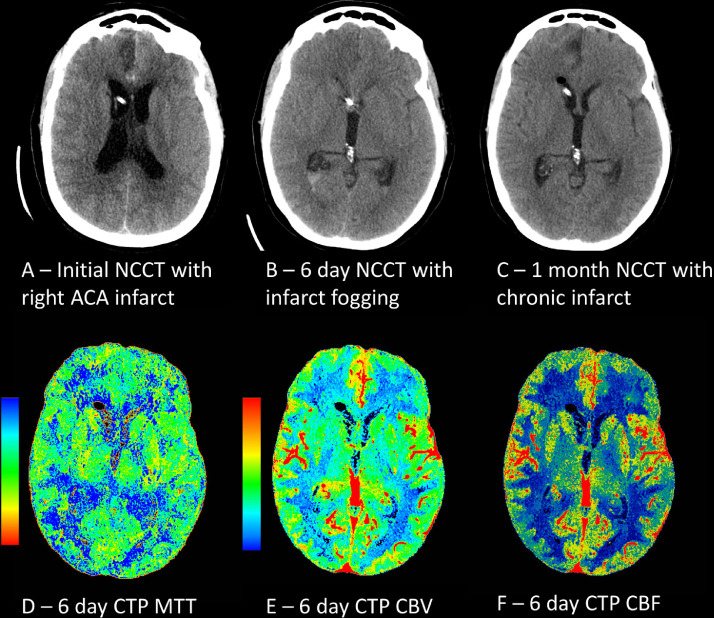
Case 1
A 55-year-old female presented with subarachnoid hemorrahge (SAH) secondary to a ruptured anterior communicating artery aneurysm. The patient developed vasospasm and subsequent small right paramedian frontal anterior cerebral artery infarction 4 days after initial presentation and coil embolization (Fig. 1). Fogging was noted 6 days after initial infarction and last contrast administration with pseudonormalization of right anterior cerebral artery territory hypodensities. On CTP, subtle symmetrical to decreased mean transit time (MTT), and slightly increased cerebral blood volume (CBV) and cerebral blood flow (CBF) were identified in the right anterior cerebral artery territory infarction. The patient's hospital stay required ventricular drain placement, as well as intra-arterial Verapamil 6 days after fogging. One month follow-up NCCT revealed hypodense chronic infarction of the right frontal lobe. Clinically, the patient was discharged with a right visual field defect from concurrent left occipital infarction and personality changes.
Fig. 1.
A 55-year-old female presented with SAH secondary to an anterior communicating aneurysm. The patient developed vasospasm and (A) subsequent right anterior cerebral artery (ACA) infarction. (B) Fogging was noted 6 days after infarction with normalization of hypodensities on NCCT/CTP. (C) One month follow-up NCCT revealed hypodense chronic infarction of the right frontal lobe. Subtle symmetrical to decreased (D) MTT, and increased (E) CBV and (F) CBF were noted at time of fogging.
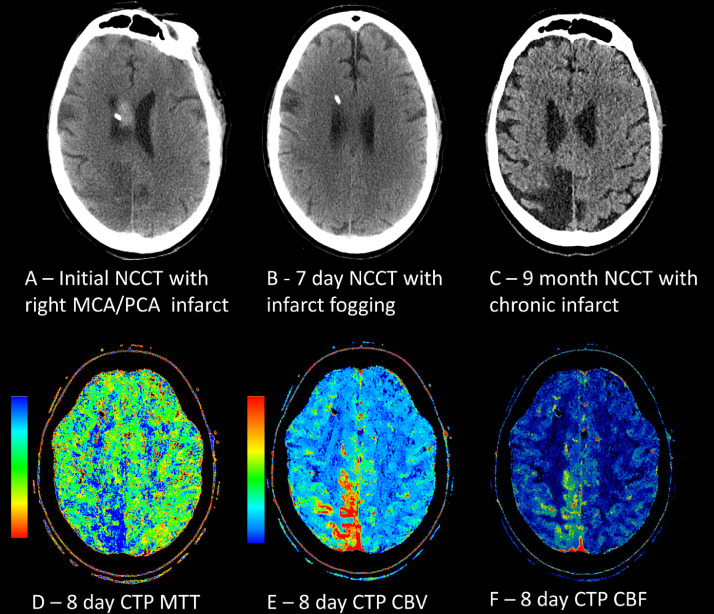
Case 2
A 47-year-old female presented with headache, nausea, and vomiting. Initial head CT angiogram (CTA) demonstrated right basal ganglia intracerebral hemorrhage with intraventricular and subarachnoid extension likely secondary to hypertension. The patient developed vasospasm and subsequent infarction of the right parietal lobe 2 days after initial presentation (Fig. 2). Patient underwent same day cerebral angiogram with balloon angioplasty and intra-arterial Verapamil infusion. Fogging occurred 7 days after initial infarction and 4 days after last contrast administration with areas of isoattenuation on NCCT. Next day NCCT revealed persistent fogging effect with CTP demonstrating increased MTT, CBV, and CBF within the area of infarction. Patient's course was complicated by ventricular drain placement and ventriculitis. Follow-up NCCT 9 months later revealed chronic right parietal infarction. Clinically, the patient's symptoms improved with rehabilitation.
Fig. 2.
A 47-year-old female presented with intracerebral hemorrhage (ICH), intraventricular hemorrhage (IVH), and left ICA dissection secondary to hypertension. The patient developed vasospasm and subsequent (A) right MCA and posterior cerebral artery (PCA) infarction on NCCT. (B) Fogging was noted 7 days later on NCCT/CTP. (C) Follow-up 9-month NCCT demonstrated right parietal chronic infarction. Next day CTP at time of fogging demonstrated (D) prolonged MTT, (E) increased CBV, and (F) increased CBF.
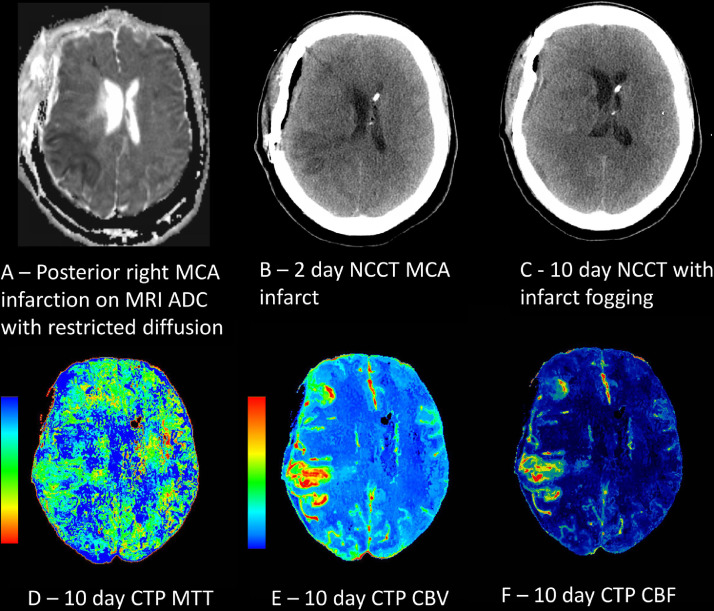
Case 3
A 52-year-old female presented with sudden onset severe headache. Initial CTA and cerebral angiogram revealed SAH secondary to a right posterior communicating artery aneurysm. Patient underwent right frontotemporal craniotomy for surgical aneurysm clipping. Her course was complicated by hydrocephalus requiring a ventricular drain and vasospasm of the right carotid terminus with development of multiple right sided infarctions. Patient underwent balloon angioplasty and intra-arterial Verapamil infusion 8 days after initial presentation. An additional new posterior right middle cerebral artery (MCA) stroke was apparent on MRI obtained 10 days after presentation (Fig. 3). The new infarction was also seen on NCCT 2 days after the MRI. Fogging was noted 10 days after infarction on MRI and 7 days after last contrast administration. At time of fogging, CTP revealed decreased MTT and increased CBF/CBV within areas of the posterior MCA infarction. Patient was discharged to rehabilitation with cognitive defects.
Fig. 3.
A 52-year-old female presented with SAH secondary to a right posterior communicating artery aneurysm. The patient developed vasospasm and subsequent (A) right MCA infarction on MRI with ADC revealing restricted diffusion of the stroke, also seen on (B) 2-day follow-up NCCT. (C) Fogging was noted 10 days after initial infarction. At time of fogging, CTP revealed (D) decreased MTT, (E) increased CBV, and (F) increased CBF.
Discussion
We present the appearance of infarct fogging on CTP through 3 educational cases. In all cases the infarction was secondary to vasospasm from subarachnoid blood. The CTP findings at the time of fogging demonstrated variable MTT but all patients showed elevated CBV and CBF. The presence of iso-dense attenuation of the fogged parenchyma on NCCT and postischemic hyperperfusion on CTP can be misleading findings. Theoretically, hyperperfusion of the infarcted tissue may make the contralateral normal tissue appear as the abnormal hypoperfused side on CTP. Careful evaluation of comparison imaging and familiarity with perfusion patterns on CTP may help avoid this pitfall.
Traditionally, infarct fogging refers to the transient iso-dense appearance of previously hypodense infarction, occurring generally 2-3 weeks after initial infarction [1]. Normal CT imaging within a week of initial stroke symptoms without prior imaging demonstrating a stroke has been previously described [2]. Our cases of iso-dense infarct attenuation developed 6-10 days after initial hypodense infarction, sooner than previously described classic fogging [1]. The decreased conspicuity of infarction at time of traditional fogging on NCCT has been postulated to be secondary to decreased bulk fluid, increased capillary proliferation, and increased influx of macrophages and erythrocytes [1], [2], [5]. However, CTP findings of all 3 of our cases would argue against decreased bulk fluid since each case had consistently elevated CBV and CBF, mimicking a “luxury” like perfusion consistent with a subacute infarction [3], [4]. An explanation for the discrepancies may lie in the etiology for the infarctions, as the 3 presented cases were from vasospasm and not thromboembolic disease [1], [2]. Furthermore, cases 2 and 3 received intra-arterial Verapamil before fogging, which may play a role in augmented vasodilation [6], [7]. Redemonstration of hypodense infarction had been reported to occur within 1-7 weeks after traditional fogging, in concordance with our findings [1].
Infarct fogging is distinct from contrast staining, where the infarction is masked or even mistaken for hemorrhage by recent contrast administration (ie from previous cerebral angiogram) [5], [8], [9], [10]. Both entities can appear similar with pseudonormalization of infarcted parenchyma on NCCT; but, fogging is a subacute process and staining typically happens in the more acute time period [1], [2], [5], [8]. However, infarct contrast staining, and fogging are not mutually exclusive. The infarctions in cases 2 and 3 increased in size and conspicuity on consecutive follow-up exams; poor initial visualization could be partially due to serial contrast enhanced CTAs ordered for the evaluation for vasospasm which is a customary practice at our institution. In cases of contrast staining, repeat CT imaging in 24 hours may be required to show infarction extent in the absence of contrast [8].
In the setting of acute ischemia, CTP can be used to distinguish reversable penumbra from irreversible core infarction [3], [4]. In both situations, MTT is prolonged (Table 2); for penumbra, CBV is preserved and CBF is decreased; whereas for core, both CBV and CBF are decreased [3], [4]. On CTP at time of fogging, the subacute infarctions demonstrated variable MTT with increased CBV and CBF. This perfusion pattern matches postischemia hyperperfusion, or “luxury perfusion,” which generally occurs in subacute infarctions [3], [4]. Luxury perfusion is likely due to increased edema and blood flow in the setting of low oxygen demand secondary to abnormal vascular autoregulation in the infarcted tissue [3], [4]. Even though the infarcts in all 3 cases were due to vasospasm, the CTP pattern at fogging was not similar to vasospasm where MTT is prolonged, CBV is preserved, and CBF is decreased [3], [4]. In all cases, the true extent of the infarction is easily identified on CTP at time of fogging (Fig. 1, Fig. 2, Fig. 3).
Conclusion
Identification of the “fogging effect” on NCCT and CTP is important to avoid underestimation or misdiagnosis of a cerebral infarction. In our case series, infarction fogging occurred 6-10 days after infarction, sooner than the previously described 2-3 weeks in classic fogging [1]. At time of fogging, CTP reflected the chronological stage of the 3 subacute infarctions, with a “luxury-like” perfusion pattern. CTP may augment the identification of this process, as well as outline the true extent of infarction at time of fogging.
References
- 1.Becker H., Desch H., Hacker H., Pencz A. CT fogging effect with ischemic cerebral infarcts. Neuroradiology. 1979;18:185–192. doi: 10.1007/BF00345723. [DOI] [PubMed] [Google Scholar]; Becker H., Desch H., Hacker H., Pencz A.CT fogging effect with ischemic cerebral infarcts. Neuroradiology1979;18:185–192. doi:10.1007/BF00345723. [DOI] [PubMed]
- 2.Skriver E.B., Olsen T.S. Transient disappearance of cerebral infarcts on CT scan, the so-called fogging effect. Neuroradiology. 1981;22:61–65. doi: 10.1007/BF00344775. [DOI] [PubMed] [Google Scholar]; Skriver E.B., Olsen T.S.Transient disappearance of cerebral infarcts on CT scan, the so-called fogging effect. Neuroradiology1981;22:61–65. [DOI] [PubMed]
- 3.Lui Y.W., Tang E.R., Allmendinger A.M., Spektor V. Evaluation of CT perfusion in the setting of cerebral ischemia: patterns and pitfalls. Am J Neuroradiol. 2010;31:1552–1563. doi: 10.3174/ajnr.A2026. [DOI] [PMC free article] [PubMed] [Google Scholar]; Lui Y.W., Tang E.R., Allmendinger A.M., Spektor V.Evaluation of CT perfusion in the setting of cerebral ischemia: patterns and pitfalls. Am J Neuroradiol2010;31:1552–1563. doi:10.3174/ajnr.A2026. [DOI] [PMC free article] [PubMed]
- 4.Keedy A., Soares B., Wintermark M. A pictorial essay of brain perfusion-CT: not every abnormality is a stroke! J Neuroimaging. 2012;22:20–33. doi: 10.1111/j.1552-6569.2012.00716.x. [DOI] [PubMed] [Google Scholar]; Keedy A., Soares B., Wintermark M.A pictorial essay of brain perfusion-CT: not every abnormality is a stroke!J Neuroimaging2012;22:20–33. doi:10.1111/j.1552-6569.2012.00716.x. [DOI] [PubMed]
- 5.Dekeyzer S., Reich A., Othman A.E., Wiesmann M., Nikoubashman O. Infarct fogging on immediate postinterventional CT-a not infrequent occurrence. Neuroradiology. 2017;59:853–859. doi: 10.1007/s00234-017-1894-z. [DOI] [PubMed] [Google Scholar]; Dekeyzer S., Reich A., Othman A.E., Wiesmann M., Nikoubashman O.Infarct fogging on immediate postinterventional CT-a not infrequent occurrence. Neuroradiology2017;59:853–859. doi:10.1007/s00234-017-1894-z. [DOI] [PubMed]
- 6.Joshi S., Young W.L., Pile-Spellman J., Duong D.H., Hacein-Bey L., Vang M.C. Manipulation of cerebrovascular resistance during internal carotid artery occlusion by intraarterial verapamil. Anesth Analg. 1997;85:753–759. doi: 10.1097/00000539-199710000-00008. [DOI] [PubMed] [Google Scholar]; Joshi S., Young W.L., Pile-Spellman J., Duong D.H., Hacein-Bey L., Vang M.C., et al. Manipulation of cerebrovascular resistance during internal carotid artery occlusion by intraarterial verapamil. Anesth Analg1997;85:753–759. [DOI] [PubMed]
- 7.Jun P., Ko N.U., English J.D., Dowd C.F., Halbach V.V., Higashida R.T. Endovascular treatment of medically refractory cerebral vasospasm following aneurysmal subarachnoid hemorrhage. AJNR Am J Neuroradiol. 2010;31:1911–1916. doi: 10.3174/ajnr.A2183. [DOI] [PMC free article] [PubMed] [Google Scholar]; Jun P., Ko N.U., English J.D., Dowd C.F., Halbach V. V., Higashida R.T., et al. Endovascular treatment of medically refractory cerebral vasospasm following aneurysmal subarachnoid hemorrhage. AJNR Am J Neuroradiol2010;31:1911–1916. doi:10.3174/ajnr.A2183. [DOI] [PMC free article] [PubMed]
- 8.Dekeyzer S., Nikoubashman O., Lutin B., De Groote J., Vancaester E., De Blauwe S. Distinction between contrast staining and hemorrhage after endovascular stroke treatment: one CT is not enough. J Neurointerv Surg. 2017;9:394–398. doi: 10.1136/neurintsurg-2016-012290. [DOI] [PubMed] [Google Scholar]; Dekeyzer S., Nikoubashman O., Lutin B., De Groote J., Vancaester E., De Blauwe S., et al. Distinction between contrast staining and hemorrhage after endovascular stroke treatment: one CT is not enough. J Neurointerv Surg2017;9:394–398. doi:10.1136/neurintsurg-2016-012290. [DOI] [PubMed]
- 9.Wing S.D., Norman D., Pollock J.A., Newton T.H. Contrast enhancement of cerebral infarcts in computed tomography. Radiology. 1976;121:89–92. doi: 10.1148/121.1.89. [DOI] [PubMed] [Google Scholar]; Wing S.D., Norman D., Pollock J.A., Newton T.H.Contrast enhancement of cerebral infarcts in computed tomography. Radiology1976;121:89–92. doi:10.1148/121.1.89. [DOI] [PubMed]
- 10.Yock D.H., Marshall W.H. Recent ischemic brain infarcts at computed tomography: appearances pre- and postcontrast infusion. Radiology. 1975;117:599–608. doi: 10.1148/117.3.599. [DOI] [PubMed] [Google Scholar]; Yock D.H., Marshall W.H.Recent ischemic brain infarcts at computed tomography: appearances pre- and postcontrast infusion. Radiology1975;117:599–608. doi:10.1148/117.3.599. [DOI] [PubMed]