Abstract
Purpose
To evaluate final-year pharmacy students’ perceptions toward pharmacogenomics education, their attitudes on its clinical relevance, and their readiness to use such knowledge in practice.
Methods
A 19-question survey was developed and modified from prior studies and was pretested on a small group of pharmacogenomics faculty and pharmacy students. The final survey was administered to 978 final-year pharmacy students in 8 school/colleges of pharmacy in New York and New Jersey between January and May 2017. The survey targeted 3 main themes: perceptions toward pharmacogenomics education, attitudes toward the clinical relevance of this education, and the students’ readiness to use knowledge of pharmacogenomics in practice.
Results
With a 35% response rate, the majority (81%) of the 339 student participants believed that pharmacogenomics was a useful clinical tool for pharmacists, yet only 40% felt that it had been a relevant part of their training. Almost half (46%) received only 1–3 lectures on pharmacogenomics and the majority were not ready to use it in practice. Survey results pointed toward practice-based trainings such as pharmacogenomics rotations as the most helpful in preparing students for practice.
Conclusions
Final-year student pharmacists reported varying exposure to pharmacogenomics content in their pharmacy training and had positive attitudes toward the clinical relevance of the discipline, yet they expressed low confidence in their readiness to use this information in practice.
Keywords: attitudes, clinical adoption, education, pharmacogenomics, readiness, student pharmacists
KEY POINTS.
Final-year student pharmacists had positive attitudes and perceptions toward pharmacogenomics and its clinical relevance even though the majority were not ready to implement related concepts in practice.
Student pharmacists were more likely to feel confident in their ability to use pharmacogenomics in practice after enrolling in advanced pharmacy practice experiential rotations in pharmacogenomics.
Schools of pharmacy should invest in practice-based training opportunities taught by well-trained faculty to increase readiness to implement related concepts in practice.
Pharmacogenomics is the study of how an individual’s genome can influence his or her response to drugs.1 To date, more than 200 Food and Drug Administration (FDA)–approved medications have pharmacogenomics product-label changes and polymorphisms in genes that encode drug-metabolizing enzymes, which make up 80% of these product-label updates.2 However, widespread adoption into clinical practice has been lagging behind the technological advances and research discoveries.
For decades, pharmacists have played pivotal roles in healthcare to optimize drug therapy while minimizing and/or preventing adverse drug events. Pharmacists’ extensive knowledge of pharmacotherapy and their skill sets in therapy optimization uniquely position them to assume key functions and leadership in the clinical implementation of pharmacogenomics.3 The 2015 American Society of Health-System Pharmacists (ASHP) statement on the pharmacist’s role in clinical pharmacogenomics not only affirmed the professional society’s support of pharmacogenomics but also highlighted 5 responsibilities of pharmacists in this specialty. Advocating for the rational and routine use of pharmacogenomics testing, providing test results interpretation, and educating providers and patients on clinical application of pharmacogenomics are a few of the aforementioned roles of pharmacists.4
In a survey of 303 pharmacists, 65% believed that pharmacists need to be knowledgeable about the appropriate use of pharmacogenomics testing; however, nearly the same number of respondents felt inadequately prepared to use the results of pharmacogenomics tests in practice.5 This sentiment has been reported by others as well.6–9 Reports in 2005 demonstrated that only 39% of pharmacy schools included pharmacogenomics content in their curricula.10 In 2010, Murphy et al.11 reported an impressive improvement, with 90% of schools reporting curricular, adoption of pharmacogenomics content. In the Murphy report, the authors also reported varying degrees of content coverage among the schools, and more than half had no plans for faculty development in pharmacogenomics.
The marked increase in the number of pharmacy schools with pharmacogenomics training may be attributed to the efforts of the Accreditation Council for Pharmacy Education (ACPE) and the American Association of Colleges of Pharmacy since the 2005 report. ACPE issued pharmacogenomics content requirements for all pharmacy schools effective July 2007.12 Moreover, the 2008 American Association of Colleges of Pharmacy House of Delegates approved resolutions that called for training and curricular modifications to address implications of personalized medicine and biotechnology as well as tailored faculty training in these disciplines.13
It has been a decade since the initial recommendation to focus on pharmacogenomics training in our schools of pharmacy, and as such, we sought to investigate how the educational strategies and increased training have affected newly graduating pharmacy students. The objective of this study was to assess 2017 final-year pharmacy students’ perceptions and attitudes on pharmacogenomics and their readiness to incorporate it into their practice as pharmacists.
Methods
Survey participants
All 11 schools and colleges of pharmacy in New York, New Jersey, and Connecticut were invited; however, 3 schools did not respond and were therefore excluded from the study. The 8 schools that participated were Albany College of Pharmacy and Health Sciences, Touro College of Pharmacy, St. John Fisher College Wegmans School of Pharmacy, D’Youville College School of Pharmacy, Fairleigh Dickinson University, St. John’s University, Long Island University Arnold & Marie Schwartz College of Pharmacy, and University at Buffalo School of Pharmacy and Pharmaceutical Sciences. The appropriate human subjects protection program institutional review board approvals were granted to all participating schools. In all, 978 final-year students (class of 2017) were eligible to participate in the survey.
Study design
This was a descriptive study that employed a 19-question survey developed and modified from prior studies11,14 to assess participant demographics and 3 main themes1: (1) the students’ attitudes toward pharmacogenomics education,2 (2) their perceptions on the clinical relevance of pharmacogenomics,3 and (3) their readiness to adopt it into their practice. A 5-point Likert scale ranging from “strongly agree” to “strongly disagree” was used to score the responses. A pretest of the survey tool was conducted with 4 academic pharmacists involved in pharmacogenomics research and didactic training as well as 3 pharmacy students undergoing pharmacogenomics advanced pharmacy practice experiential (APPE) rotations. All pretesters provided feedback on content, length, clarity, and utility of the survey tool, which was then used to refine the final set of questions. Additionally, the authors reviewed and approved the questionnaire before it was administered. The survey was administered electronically via www. surveymonkey.com between January and May 2017, and faculty–student champions from each of the participating schools deployed the link to the questionnaire to the graduating class of their respective schools. The participants were given 8 weeks to complete the survey initially. After that, the deadline for completion was extended for an additional 4 weeks. Two reminder emails were sent by the faculty–student champions in 4-week intervals. Moreover, the faculty champions provided additional information on their respective schools and the nature of the pharmacogenomics courses offered.
Statistical analysis
Survey data were collected using SurveyMonkey and interpreted using a range of descriptive statistical methods, such as cross-tabulations, comparisons of means and standard deviations across multinomial variables, and data visualization. Ordinal logistic regression was used to estimate the overall main effects of certain demographic predictors, which were converted to ordered categorical variables, on the survey response outcomes. All statistical analyses were conducted with IBM Corp. Released 2015. IBM SPSS Statistics for Macintosh, Version 23.0. Armonk, NY: IBM Corp.
Results
Student demographics
Of 978 students eligible for the study, 339 (35%) students completed the survey. Table 1 summarizes the relevant demographics. The respondents were mostly females (n = 213, 63%). A majority were between the ages of 21 and 25 (n = 194, 57%) and 26 and 30 years (n = 106, 31%). High school was the most common educational level completed by the respondents prior to matriculating to pharmacy school as reported by 147 (43%) students, and 158 (47%) planned to pursue community pharmacy opportunities postgraduation.
Table 1.
Demographics Information for the Final-Year Pharmacy Student Respondents (n = 339)
| Variable | No. (%) |
|---|---|
| Gender | |
| Female | 213 (62.8) |
| Male | 123 (36.3) |
| Prefer not to disclose | 3 (0.90) |
| Age range | |
| Less than 21 years | 1 (0.30) |
| 21–25 years | 194 (57.2) |
| 26–30 years | 106 (31.3) |
| 31–40 years | 33 (9.70) |
| >40 years | 4 (1.20) |
| No response | 1 (0.30) |
| Highest level of education before pharmacy school | |
| High school diploma | 147 (43.4) |
| Bachelor’s degree | 127 (37.5) |
| Master’s degree | 11 (3.20) |
| Doctorate/J.D. | 31 (9.10) |
| Other | 22 (6.50) |
| No response | 1 (0.30) |
| Postgraduate plans | |
| Residency | 83 (24.5) |
| Fellowship | 19 (5.60) |
| Community | 158 (46.6) |
| Hospital | 32 (9.40) |
| Undecided | 47 (13.9) |
Pharmacogenomics educational opportunities
As shown in Table 2, pharmacogenomics was integrated through other courses at 2 schools, offered as a standalone course in 4 schools, and as both integrated and standalone in the remaining 2 schools of pharmacy. Of those with a standalone course, 4 required it for all their students and 2 offered it as an elective class. Notably, only 2 pharmacogenomics faculty members had been formally trained in pharmacogenomics, while others had undergone varying degrees of training. The learning objectives differed across schools, and an elective pharmacogenomics APPE rotation was available to students from 3 of the participating schools.
Table 2.
Description of Participating Schools of Pharmacy and their Pharmacogenomics Educational Opportunitiesa
| School A | School B | School C | School D | School E | School F | School G | School H | ||
|---|---|---|---|---|---|---|---|---|---|
| Variable | (64.60% Response Rate) | (53.10% Response Rate) | (11.70% Response Rate) | (26.90% Response Rate) | (27.20% Response Rate) | (57% Response Rate) | (16.20% Response Rate) | (39.40% Response Rate) | |
| PGx Faculty | Terminal degree | Ph.D. | Ph.D. | Ph.D. and clinical Pharm.D. | Clinical Pharm.D. | Ph.D. | R.Ph. and Ph.D. | Ph.D. | Ph.D. |
| Formal PGx training | No | No | No | No | No | Yes | Yes | No | |
| Other PGx-related training | PGx coursework as part of a Pharmacology Ph.D. | Applied PGx research as an industry senior scientist position | PGx certificate program | No | Molecular and epigenetics | PGx post-doc fellowship | PGx Ph.D. and post-doc fellowship in PGx | Involved in PGx research in the past | |
| PGx didactic course details | Standalone or integrated? | Standalone | Standalone | Both | Integrated | Integrated | Standalone | Both | Standalone |
| If integrated, what course? | N/A | N/A | Pharmacokinetics (2 lectures) | Pharmacotherapy | Pharmacology | N/A | Several courses | N/A | |
| If standalone, is it required or an elective? | Elective | Required | Elective | N/A | N/A | Required | Required | Required | |
| Average student per year for the elective courses | 35 | N/A | 10–15 | N/A | N/A | N/A | N/A | N/A | |
| When is the course offered? | 1st, 2nd, or 3rd professional year | 2nd professional year | 3rd professional year | 2nd or 3rd professional year | 2nd professional year | 3rd professional year | 3rd professional year | 2nd professional year | |
| Length of course/credits | 1 semester; 2 credit hours | 1 semester; 2 credit hours | 1 semester; 2 credit hours | N/A | N/A | 1 semester; 2 credits | 1 semester; 2 credits | 1 semester; 2 credits | |
| PGx Course Learning Objectives | To identify medications that require or are recommended by FDA to have PGx testing | Yes | Yes | Yes | N/A | Yes | N/A | Yes | Yes |
| To recommend appropriate PGx tests for the medications that require testing | Yes | Yes | Yes | N/A | No | No | Yes | No | |
| To accurately interpret pharmacogenomics tests | Yes | Yes | Yes | N/A | No | No | Yes | No | |
| To recommend alternative therapies or doses when required by a PGx test result | Yes | Yes | Yes | N/A | Yes | Yes | Yes | Yes | |
| Become familiar with how to access, interpret, and use the CPIC guidelines | Yes | No | Yes | N/A | No | N/A | Yes | No | |
| PGx APPEb | PGx APPE opportunity | No | Yes | No | Yes | Yes | No | No | No |
| Length of APPE | N/A | 5 weeks | N/A | 5 weeks | 6 weeks | N/A | N/A | N/A |
bThe PGx APPE training addresses all the learning objectives listed.
Exposure to pharmacogenomics education
The respondents were queried on their exposure to pharmacogenomics content in their pharmacy school curricula. Of the respondents, 156 (46%) were exposed to 1–3 pharmacogenomics lectures, 96 (28%) completed a required pharmacogenomics course, 20 (6%) took an elective pharmacogenomics course, 8 (2%) completed a pharmacogenomics APPE rotation, 39 (12%) did not receive any pharmacogenomics training, and 19 (6%) did not respond to this question.
Perception on the clinical relevance of pharmacogenomics
Four questions were posed to investigate the perceived clinical utility and relevance of pharmacogenomics among the final-year student pharmacists (Table 3). The majority (81%, n = 273) believed that pharmacogenomics was a useful tool that pharmacists and medical professionals could use to optimize medication effectiveness and/or prevent adverse events, and more than half (63%, n = 234) affirmed that it was an integral part of the pharmacy profession. In addition, 61% (n = 205) perceived that pharmacogenomics might be an integral part of their practice as pharmacists, and slightly more (69%, n = 234) predicted that they might encounter pharmacogenomics-related questions during their practice as pharmacists.
Table 3.
Survey Responses from the Final-Year Pharmacy Students
| Survey Questions | Number of Respondents (%) | |||
|---|---|---|---|---|
| Strongly Agree/Agree | Neutral | Strongly Disagree/Disagree | No Response | |
| Perception of the clinical relevance of pharmacogenomics | ||||
| Pharmacogenomics is an integral part of the pharmacy profession. | 214 (63.1) | 67 (19.8) | 28 (8.26) | 30 (8.85) |
| Pharmacogenomics may be an integral part of my practice as a pharmacist. | 205 (60.5) | 62 (18.3) | 42 (12.4) | 30 (8.85) |
| I may encounter pharmacogenomics-related questions during my practice as a pharmacist. | 234 (69.0) | 45 (13.3) | 29 (8.55) | 31 (9.14) |
| Pharmacogenomics is a useful tool that pharmacists and medical professionals can use to optimize medication efficacy and/or prevent adverse events. | 273 (80.5) | 27 (7.96) | 9 (2.65) | 30 (8.85) |
| Attitudes toward pharmacogenomics education | ||||
| Pharmacogenomics has been a relevant part of my doctor of pharmacy curriculum. | 136 (40.1) | 88 (26.0) | 96 (28.3) | 19 (5.60) |
| Pharmacogenomics should be covered in detail for all colleges and schools of pharmacy. | 239 (70.5) | 67 (19.8) | 13 (3.83) | 20 (6.00) |
| Final-year (P4) pharmacy students should be required to have substantial knowledge of pharmacogenomics prior to graduation. | 175 (51.6) | 97 (28.6) | 48 (14.2) | 19 (5.60) |
| Postgraduation, I intend to read up on pharmacogenomics especially on how it influences my practice and/or specialty. | 188 (55.5) | 81 (23.9) | 51 (15.0) | 19 (5.60) |
| Readiness to use pharmacogenomics knowledge in practice | ||||
| I know at least 10 medications that require or are recommended to have pharmacogenomics testing as per the Food and Drug Administration. | 108 (31.9) | 55 (16.2) | 150 (44.2) | 26 (7.67) |
| I am able to recommend the appropriate pharmacogenomics test(s) for the medications that require it. | 72 (21.2) | 79 (23.3) | 161 (47.5) | 27 (7.96) |
| I am able to accurately interpret pharmacogenomics tests. | 91 (26.8) | 75 (22.1) | 147 (43.4) | 26 (7.67) |
| Based on the results of a pharmacogenomics test, I am able to recommend alternative therapies or dose changes when required. | 107 (31.6) | 82 (24.2) | 124 (36.6) | 26 (7.67) |
| I am aware of the Clinical Pharmacogenetics Implementation Consortium’s guidelines on how to use genetic information to guide drug therapy selection/dosing. | 55 (16.2) | 48 (14.2) | 209 (61.7) | 27 (7.96) |
Attitudes toward pharmacogenomics education
Approximately 75% (n = 239) of the respondents believed that pharmacogenomics should be covered in detail in all schools and colleges of pharmacy; however, only 40% (n = 136) felt that it had been a relevant part of their doctor of pharmacy curriculum. Moreover, 51% (n = 175) agreed that final-year pharmacy students should be required to have substantial knowledge of pharmacogenomics prior to graduation, and 56% (n = 188) indicated their intentions of reading pharmacogenomics-related literature after graduation, especially when it pertained to their respective practices and specialties (Table 2).
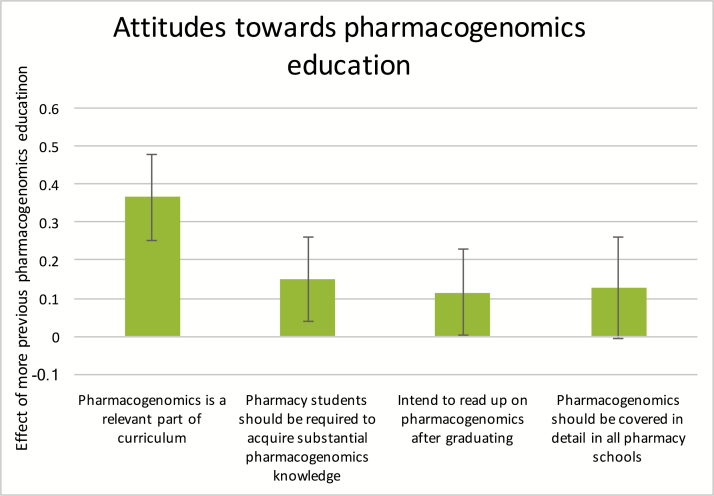
The students’ past exposure to pharmacogenomics training content was significantly associated with their attitudes toward pharmacogenomics education. Pharmacogenomics training was converted into an ordered categorical variable, with the lowest level being no exposure to pharmacogenomics in pharmacy school (n = 39), followed by 1–3 lectures or seminars (n = 156), elective pharmacogenomics course (n = 20), required pharmacogenomics course (n = 96), and finally the highest level being pharmacogenomics APPE rotation (n = 8). This measure of pharmacogenomics training was significantly associated with more agreement to 3 of the 4 questions assessing attitudes toward pharmacogenomics education (Figure 1).
Figure 1.
Attitude toward pharmacogenomics education.
Readiness to use pharmacogenomics knowledge in practice
As proposed by the ASHP,4 pharmacists should know medications with pharmacogenomics implications, the associated tests and their interpretations as well as recommended therapeutic modifications for genetically “high-risk” individuals. To this end, we asked the final-year student pharmacists if they knew at least 10 medications that FDA either requires or recommends pharmacogenomics testing prior to use (Table 3). Only 32% (n = 108) responded affirmatively, whereas 44% (n = 150) did not know at least 10 such medications. Furthermore, when queried on their ability to recommend the appropriate pharmacogenomics tests for the medications that require it, only 21% (n = 72) stated they could and about one-third (27%, n = 91) reported having the ability to accurately interpret pharmacogenomics tests. Again, 32% (n = 107) felt knowledgeable to recommend alternative therapies and/or dose changes based on pharmacogenomic results. Lastly, 62% (n = 209) were not aware of the Clinical Pharmacogenetics Implementation Consortium (CPIC) guidelines, which provide clinical recommendations to clinicians on how to use genetic information to guide medication selection and dosing.15
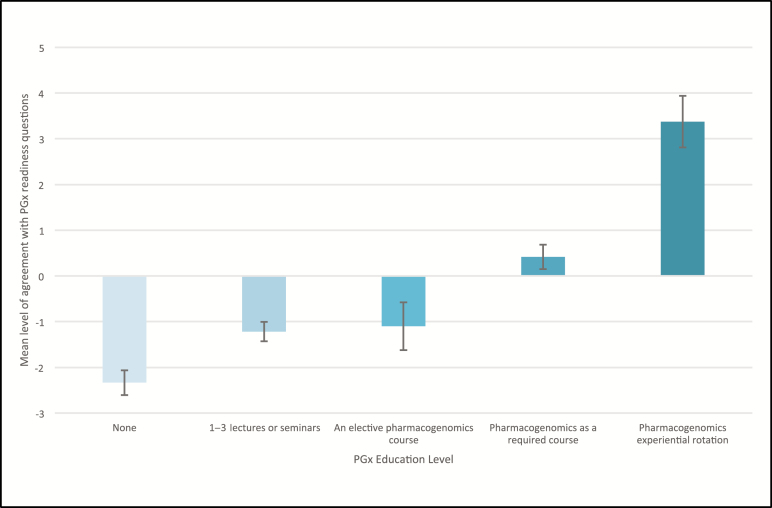
As expected, the students’ past exposure to pharmacogenomics content in their curricula was strongly associated with increased agreement with the statements about readiness to use pharmacogenomics in practice (Figure 2). More exposure to pharmacogenomics was correlated with the students’ knowledge of at least 10 medications needing pharmacogenomic testing (β, 0.349; 95% confidence interval [CI], 0.231–0.468); their ability to recommend appropriate pharmacogenomic tests for such medications (β, 0.251; 95% CI, 0.128–0.375); their ability to accurately interpret these tests (β, 0.363; 95% CI, 0.244–0.482); their knowledge of the appropriate therapeutic recommendations based on the pharmacogenomics test results (β, 0.342; 95% CI, 0.237–0.448); and their awareness of CPIC guidelines (β, 0.313; 95% CI, 0.206–0.420).
Figure 2.
Overall readiness to use pharmacogenomics in practice by exposure to pharmacogenomics education.
Discussion
Clinical applications of pharmacogenomics are increasingly gaining acceptance as evidenced by the National Institutes of Health National Human Genome Research Institute—funded consortia focused on developing tools and clinical implementation strategies16–18—and the availability of databases such as the FDA Table of Biomarkers19 and the Pharmacogenomics Knowledge Base (www.pharmgkb.org).20
Pharmacists are distinctively qualified medical professionals who can lead translational pharmacogenomics and assume essential roles in its education and sustained adoption in professional curricula.3 Of the 339 participants in this study, 82% had been exposed to pharmacogenomics content in varying degrees throughout their pharmacy school program ranging from 1 to 3 lectures to several weeks of pharmacogenomics APPE rotation experience. This finding sadly affirms the 2010 study by Murphy et al.11 in which 67 (89%) colleges/schools of pharmacy reported having pharmacogenomics content in their doctor of pharmacy curricula, albeit the dedicated didactic hours differed greatly from school to school. In that study, 28 schools (41%) dedicated 10 or fewer hours, whereas 29 (42%) reported 11 to 30 didactic hours for pharmacogenomics. A decade later, Murphy et al.’s findings still resonate as demonstrated in the present study. Almost half of the final-year students in our survey (46%) encountered pharmacogenomics content in 1–3 lectures, and approximately 12% received no pharmacogenomics instruction throughout their pharmacy school education. In all, 40% noted that pharmacogenomics had been a relevant part of their pharmacy training. This is almost a 4-fold boost from the 2011 finding by McCullough and colleagues5 in which only 10% of surveyed pharmacists stated that pharmacogenomics had been a relevant component of their pharmacy education.
From this study and others, it is clear pharmacists believe that pharmacogenomics is a relevant tool to optimize patient care; however, the majority are not comfortable in their abilities to use it in their practice.5,6,14,21 The current study and others also confirm that educational opportunities available to student pharmacists in their training may not be sufficient to resolve this issue. Of the students, 71% believed that it should be covered in detail in pharmacy curricula, 52% stated that pharmacists should be required to have substantial knowledge in pharmacogenomics prior to graduation, and 56% intended to continue seeking educational opportunities in this discipline after graduation. Clearly, a great number of the students wanted this information.
There are 2 main reasons for the inadequate training in pharmacogenomics. The first is the lack of well-trained educators to introduce content that addresses core competencies. In our study, 25% of the faculty members were formally trained in pharmacogenomics, whereas the others completed coursework and certificate programs and were exposed through involvement in pharmacogenomics research (Table 2). Although a few were clinical faculty, none were actively practicing in pharmacogenomics.
The University of California San Diego Pharmacogenomics Education Program,22 University of Pittsburgh’s Test2Learn,23 University of Florida Health Personalized Medicine Program graduate and certificate training program,24 and the University of Colorado Pharmacogenomics Certificate Program25 are all excellent opportunities for pharmacy school faculty to receive hands-on training in pharmacogenomics either in person or virtually. Some programs provide a shared curriculum that may be adopted in various schools, and some use the train-the-trainer methods to provide the best results. In all, these avenues were designed for educators and practitioners who are interested in using pharmacogenomic information in their practice to educate the next generation or optimize patient outcomes. The leadership of colleges of pharmacy should invest in their faculty members in participating in these programs, especially those who are in charge of providing the didactic lectures on pharmacogenomics. Moreover, faculty members in this position should be aware of the newly updated pharmacogenomics core competencies in pharmacy practice26 and resources15,20 to better instruct their students in the likely event that they encounter examples that may not have been covered in their courses. Of note, CPIC guidelines were unknown to 62% of the respondents in our study, which highlights the need for CPIC and other pharmacogenomics resource leaders to consider expanding their reach beyond practicing clinicians to trainees. Another proposed strategy for overcoming this challenge is to incorporate pharmacogenomics exposure early in the Pharm.D. curriculum through the foundational courses and into practice-based therapeutic courses, introductory pharmacy practice experiences, and APPEs.27 In addition to the learning objectives in Table 2, other training content to be considered include but are not limited to online resources,28 use of electronic health records in pharmacogenomics, potential implications with over-the-counter medications and herbal therapies, reimbursement, and ethical, legal, and social issues.
The second challenge is the lack of experiential and practice-based opportunities to engage the students in real-life applications of pharmacogenomics. Formea and colleagues29 reported marginal retention of educational objectives among practicing pharmacists after 2 months of providing a fundamental pharmacogenomics education program accredited by ACPE for continuing education. They concluded that education in this topic area will require more effort to increase knowledge and comfort in dealing with its clinical applications as demonstrated by Galvez-Peralta and colleagues30 in the School of Pharmacy at West Virginia University. Our findings support this statement and demonstrate that the extent of pharmacogenomics educational exposure and use of practice-based scenarios for teaching may play an important role in preparing the students for the practice setting.31 Final-year students who were enrolled in pharmacogenomics APPE rotations were more likely to be prepared to apply pharmacogenomics knowledge in practice than those from the other training methods (Figure 2). To the best of our knowledge, there are 2 pharmacogenomics APPE rotation opportunities in the New York/New Jersey region—Mount Sinai32 and Touro College of Pharmacy—and a handful of others across the country with very limited openings for students annually. Mount Sinai offers an elective rotation to final-year student pharmacists from 2 New York schools as well as postgraduate year 1 (PGY1) and postgraduate year 1 (PGY2) pharmacy residents in the Mount Sinai Health System. Of note, it is a required rotation for PGY2 oncology pharmacy residents at the Mount Sinai Hospital. This training is a combination of topic and patient case discussions, development of clinical decision support content and stakeholder educational tools, and personal genotyping. Furthermore, the ASHP Online Residency Directory (https://accred.ashp.org/aps/pages/directory/residencyProgramSearch.aspx) lists 3 accredited PGY2 clinical pharmacogenomics residencies. With approximately 15,000 pharmacy graduates annually,33 the training spots identified here are not nearly enough to accommodate the need. School leaderships should make every effort to hire newly trained pharmacogenomics experts into positions that provide both the didactic and the experiential examples for students. Although establishing a specialty pharmacogenomics residency is not feasible at most institutions, partnering with health systems that are implementing pharmacogenomics32,34,35 and assigning faculty liaisons and/or designing student rotation opportunities may be possible and should be considered. Furthermore, the strength of the relationship observed between the exposure to pharmacogenomics content and perceived readiness to apply in practice may be limited by the subjective nature of the survey. Also, the investigators are not in a position to accurately assess whether the responses provided accurately represented the students’ knowledge. Future studies should focus on objective knowledge-based assessments to address this concern. Moreover, the response rate per school ranged from 16% to 65%, which demonstrates that the results may not be fully representative of all final-year pharmacy students in this region. Also, the findings may not be applicable to all students in the United States, especially for those students who have advanced training options at their institutions.
Conclusion
Final-year student pharmacists reported varying exposure to pharmacogenomics content in their pharmacy training and had positive attitudes toward the clinical relevance of the discipline, yet they expressed low confidence in their readiness to use this information in practice.
Disclosures
Dr. Owusu Obeng was supported by the National Institutes of Health (NIH) National Human Genome Research Institute (NHGRI) and Grant Number 3U01HG008701-02S1 (eMERGE-PGx) and Grant Number 5U01HG007278 (IGNITE) during this project. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH/NHGRI.
All authors have declared no other potential conflicts of interest.
Acknowledgments
The authors gratefully acknowledge all the schools and colleges of pharmacy in New York and New Jersey who graciously allowed their students to participate in this project. The authors thank the class of 2017 students who participated in this project.
References
- 1. Aneesh TP, Sonal Sekhar M, Jose A, Chandran L, Zachariah SM. Pharmacogenomics: the right drug to the right person. J Clin Med Res. 2009;1:191-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Zanger UM. Pharmacogenetics - challenges and opportunities ahead. Front Pharmacol. 2010; 1:112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Owusu-Obeng A, Weitzel KW, Hatton RC et al. . Emerging roles for pharmacists in clinical implementation of pharmacogenomics. Pharmacotherapy. 2014; 34:1102-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Pharmacists ASoH-S. ASHP statement on the pharmacist’s role in clinical pharmacogenomics.Am J Health-Syst Pharm. 2015; 72:579-81. https://www.ashp.org/-/media/assets/policy-guidelines/docs/ statements/pharmacists-role- clinical-pharmacogenomics.ashx?la=en&hash=DED12C9EB9BB5B070CC9FDAA988E4E2DD35280DD. (accessed 2019 March 17).25788513 [Google Scholar]
- 5. McCullough KB, Formea CM, Berg KD et al. . Assessment of the pharmacogenomics educational needs of pharmacists. Am J Pharm Educ. 2011; 75(3):51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Tuteja S, Haynes K, Zayac C et al. . Community pharmacists’ attitudes toward clinical utility and ethical implications of pharmacogenetic testing. Per Med. 2013; 10:793-800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. McMahon T, Tucci J. The perceptions of pharmacists in Victoria, Australia on pharmacogenetics and its implications. Pharm Pract. 2011; 9(3):141-7. [PMC free article] [PubMed] [Google Scholar]
- 8. Wong YM, Quek YN, Tay JC et al. . Efficacy and safety of a pharmacist-managed inpatient anticoagulation service for warfarin initiation and titration. J Clin Pharm Ther. 2011; 36:585-91. [DOI] [PubMed] [Google Scholar]
- 9. Johnson M, Jastrzab R, Tate J et al. . Evaluation of an academic-community partnership to implement MTM services in rural communities to improve pharmaceutical care for patients with diabetes and/or hypertension. J Manag Care Spec Pharm. 2018; 24(2):132-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Latif DA MA. Pharmacogenetics and pharmacogenomics instruction in colleges and schools of pharmacy in the United States. Am J Pharm Educ. 2005;69(2):23. [Google Scholar]
- 11. Murphy JE, Green JS, Adams LA, Squire RB, Kuo GM, McKay A. Pharmacogenomics in the curricula of colleges and schools of pharmacy in the United States. Am J Pharm Educ. 2010;74(1):7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Education ACfP. Accreditation standards and guidelines for the professional program in pharmacy leading to the doctor of pharmacy degree 2006 (updated January 23, 2011). https://www.acpe-accredit.org/pdf/S2007Guidelines2.0_ChangesIdentifiedInRed.pdf (accessed 2019 March 17).
- 13. Final report of the 2007–2008 bylaws and policy development committee. Am J Pharm Edu. 2008;72(suppl):S16. [Google Scholar]
- 14. Muzoriana N, Gavi S, Nembaware V, Dhoro M, Matimba A. Knowledge, attitude, and perceptions of pharmacists and pharmacy students toward pharmacogenomics in Zimbabwe. Pharmacy. 2017;5(3), 36:1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Caudle KE, Klein TE, Hoffman JM et al. . Incorporation of pharmacogenomics into routine clinical practice: the clinical pharmacogenetics implementation consortium (CPIC) guideline development process. Curr Drug Metab. 2014; 15:209-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Rasmussen-Torvik LJ, Stallings SC, Gordon AS et al. . Design and anticipated outcomes of the eMERGE-PGx project: a multicenter pilot for preemptive pharmacogenomics in electronic health record systems. Clin Pharmacol Ther. 2014; 96:482-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Rasmussen LV, Overby CL, Connolly J et al. . Practical considerations for implementing genomic information resources. Experiences from eMERGE and CSER. Appl Clin Inform. 2016; 7:870-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Weitzel KW, Alexander M, Bernhardt BA et al. ; IGNITE Network The IGNITE network: a model for genomic medicine implementation and research. BMC Med Genomics. 2016; 9:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Food and Drug Administration. Table of pharmacogenomic biomarkers in drug labeling (updated February 8, 2018) https://www.fda.gov/Drugs/ScienceResearch/ucm572698.htm. (accessed 2019 March 17).
- 20. Whirl-Carrillo M, McDonagh EM, Hebert JM et al. . Pharmacogenomics knowledge for personalized medicine. Clin Pharmacol Ther. 2012; 92:414-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. de Denus S, Letarte N, Hurlimann T et al. . An evaluation of pharmacists’ expectations toward pharmacogenomics. Pharmacogenomics. 2013; 14:165-75. [DOI] [PubMed] [Google Scholar]
- 22. Kuo GM, Ma JD, Lee KC et al. . Institutional profile: University of California San Diego pharmacogenomics education program (pharmgened™): bridging the gap between science and practice. Pharmacogenomics. 2011; 12(2):149-53. [DOI] [PubMed] [Google Scholar]
- 23. Adams SM, Anderson KB, Coons JC et al. . Advancing pharmacogenomics education in the core PharmD curriculum through student personal genomic testing. Am J Pharm Educ. 2016; 80:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Weitzel KW, McDonough CW, Elsey AR et al. . Effects of using personal genotype data on student learning and attitudes in a pharmacogenomics course. Am J Pharm Educ. 2016; 80(7):122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. University of Colorado Skaggs School of Pharmacy and Pharmaceutical Sciences. Pharmacogenomics Certificate Programhttp://www.ucdenver.edu/academics/colleges/pharmacy/AcademicPrograms/ContinuingEducation/CertificatePrograms/PGXcertificate/Pages/PGXcert.aspx . (accessed 2019 March 17)
- 26. Roederer MW KG, Kisor D, Frye R, Hoffman JM, Jenkins J, Weitzel KW. Pharmacogenomics competencies in pharmacy practice: a blueprint for change. J Am Pharm Assoc. 2017;57(1):120-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Weitzel KW, Aquilante CL, Johnson S et al. . Educational strategies to enable expansion of pharmacogenomics-based care. Am J Health Syst Pharm. 2016; 73:1986-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Caudle KE, Keeling NJ, Klein TE et al. . Standardization can accelerate the adoption of pharmacogenomics: current status and the path forward. Pharmacogenomics. 2018; 19(10):847-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Formea CM, Nicholson WT, McCullough KB et al. . Development and evaluation of a pharmacogenomics educational program for pharmacists. Am J Pharm Educ. 2013; 77(1):10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Gálvez-Peralta M, Szklarz GD, Geldenhuys WJ, Lockman PR. An effective approach to teaching pharmacogenomics in the first year of pharmacy curriculum. Am J Pharm Educ. 2018; 82:6345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Marcinak R, Paris, M, Kinney SRM. Pharmacogenomics Education Improves Pharmacy Student Perceptions of Their Abilities and Roles in Its Use. Am J Pharm Educ. 2018; 82(9):1086-1095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Scott SA, Owusu Obeng A, Botton MR et al. . Institutional profile: translational pharmacogenomics at the Icahn School of Medicine at Mount Sinai. Pharmacogenomics. 2017; 18:1381-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Grabenstein JD. Trends in the numbers of US colleges of pharmacy and their graduates, 1900 to 2014. Am J Pharm Educ. 2016; 80(2):25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Empey PE, Stevenson JM, Tuteja S et al. ; IGNITE Network Multisite investigation of strategies for the implementation of CYP2c19 genotype-guided antiplatelet therapy. Clin Pharmacol Ther. 2018; 104:664-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Owusu Obeng A, Fei K, Levy KD et al. . Physician-reported benefits and barriers to clinical implementation of genomic medicine: a multi-site IGNITE network survey. J Personalized Med. 2018; 8(3), 24:1-13. [DOI] [PMC free article] [PubMed] [Google Scholar]