Abstract
Introduction
Plaque incision and grafting (PIG) is indicated for men with complex or severe penile curvature and, despite a multitude of incision types and grafting materials having been used, no individual technique has proven superiority.
Aim
To assess outcomes following PIG and to understand the operative technique.
Methods
A systematic review was performed to find all relevant studies reporting on use of the PIG technique to correct curvature resulting from Peyronie’s disease. Studies were included if they had >40 participants, were written in the English language, and no penile prosthesis was implanted.
Main Outcome Measures
Primary outcome measures included deformity correction, erectile dysfunction, and degree of penile lengthening/shortening. Secondary outcome measures included satisfaction, reoperation rate, and complications.
Results
Twelve studies were included in the quantitative synthesis, which overall report on the results of 1,025 patients. Careful patient selection was critical, with erectile function requiring assessment with the International Index of Erectile Function (IIEF), subjective patient reports, and consideration of whether erections are pharmacologically aided. There was no evidence of superiority in favor of any particular incision type or grafting material, and absorbable sutures were clearly favored. Postoperatively, 4.6%–67.4% required pharmacologically aided erections and 0–11.8% were completely unable to achieve erections. Successful straightening occurred in 80.0%–96.4%, although there was no consistent definition of success. Penile length was unchanged in 44.2%–95.0%; 88.0%–92.0% of the patients were satisfied, and .7%–4.7% required reoperation. Altered sensation occurred in 2.0%–22.5% of patients, of which 80.0%–100.0% was only a transient loss. All outcomes were heterogeneously reported. There are no clear predictive factors for erectile dysfunction following PIG surgery. No single incision type or grafting material has proven superiority.
Conclusion
PIG is an effective and safe technique for correction of complex or severe penile curvature in terms of satisfaction, length change, straightening, and complications.
Rice PG, Somani BK, Rees RW. Twenty Years of Plaque Incision and Grafting for Peyronie’s Disease: A Review of Literature. Sex Med 2019;7:115–128.
Key Words: Plaque incision, Grafting, Peyronie’s disease, Penile curvature, Review, Andrology
Introduction
Penile curvature was first described 3 centuries ago by the French surgeon Francois de la Peyronie. He described the disease, induratio penis plastica, as a fibrous plaque affecting the corpora cavernosa.1 The curvature results from the development of scar tissue on one side of the tunica albuginea, causing an asymmetrical reduction in elasticity that is pronounced during erection when the layer is stretched. In addition to the curvature, Peyronie’s disease can cause pain, palpable lumps, erectile dysfunction (ED), shortening, and complex deformities, which may culminate in an inability to successfully achieve satisfactory intromission. A prevalence of Peyronie’s disease of up to 9% in the general population has been reported.2 Without treatment, curvature is expected to improve in 3%–13% of patients, stabilize in 47%–67% of patients, and worsen in 30%–50% of patients.3
In addition to the physiological and functional alteration of the penis, there are also substantial psychological effects. Validated mental health questionnaires have shown that 48% of men with Peyronie’s disease have mild or moderate depression sufficient to warrant medical evaluation.4 The severity of penile curvature is the main limiting factor for penetrative intercourse,5 and surgical treatment remains the mainstay for achieving substantial straightening of the penis.
Surgical grafting procedures are indicated for men with good erectile function, complex or severe deformity, and a concern about loss of penile length.6 Initially, it was thought that excision of the diseased tissue and coverage of the defect with a graft was the best approach.7, 8 The assumption was that removal of tissue shown to have an aberrant wound healing mechanism was critical in reducing the risk of disease recurrence. Later, tissue expansion without the excision of plaque was considered; the tunica albuginea could have been expanded by incision through the plaque, followed by graft placement. The reasoning behind this shift was that a fully stabilized plaque has fully calcified; therefore, there is no further risk of recurrence over full excision. Full excisional techniques have demonstrated poorer outcomes9 and have largely been abandoned.
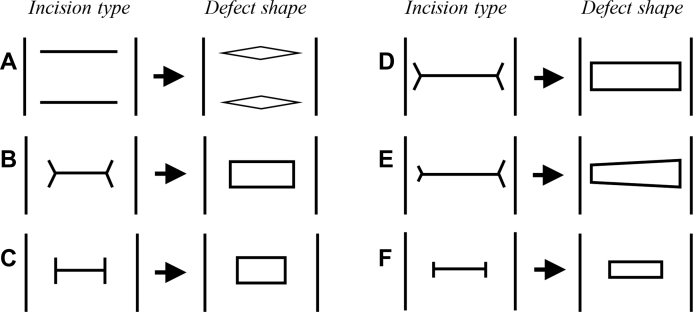
Development of the plaque incision and grafting (PIG) technique has involved numerous different approaches to the incision type itself (Figure 1). The first description of PIG detailed the use of multiple transverse incisions being used to open the corpora,10 resulting in a rhomboid defect. Later, bifurcating “Y”-shaped tails were added to the ends of the transverse incisions, producing the “double-Y” incision type, which aimed to improve diameter reduction.11 In a later technique, these tails were extended to perpendicularly intersect the end of the incision, producing the “H” incision type.12, 13 The transverse incision was then extended almost completely circumferentially, producing the Egydio incision type.14 Although the Egydio incision type has been associated with increased postoperative ED,15 no single incision type has shown overall superiority.
Figure 1.
Types of incision and resultant defects created.
The choice of graft material has also varied substantially throughout the technique’s development, with graft materials frequently investigated in individual and comparative outcome studies. Graft materials are classified as autografts (taken from the individual themselves), allografts (of human origin), xenografts (from a different animal species), or synthetic grafts.16 Owing to the inconsistency of techniques and different outcome measures used in various studies, it is not possible to establish which graft type is associated with the best outcomes. A recent review of all grafting procedures found that although cadaveric allografts and synthetic grafts have been recently abandoned, no graft can be identified as superior, and graft selection remains largely at the discretion of the operating surgeon.17 To date, no review has focused on grafts used specifically for the PIG technique.
Despite the wide selection of grafting materials and incision types available, the technique remains largely unchanged from its original description, because no grafting material or incisional method has proven superior. The aim of the present review was to investigate the study designs, procedure characteristics, patient selection, and outcomes of the PIG technique for patients with Peyronie’s disease in published studies with an adequately large sample size. The primary objective was to evaluate the outcomes of the PIG technique and to determine its overall success. The secondary objective was to investigate the operative technique for the PIG procedure.
Methods
Evidence Acquisition
Inclusion criteria: all studies written in English language, patients of any age, all studies reporting on the PIG technique with any type of incision to correct penile curvature.
Exclusion criteria included studies with <40 participants, animal or laboratory studies, and studies involving complete or partial plaque excision, concomitant penile prosthesis implantation, or congenital penile curvature.
Search Strategy
The systematic review was performed in accordance with the Cochrane Review guidelines and the PRISMA methodology.18 We searched for relevant studies in MEDLINE, Scopus, EMBASE, Cochrane Library, CINAHL, Clinicaltrials.gov, Google Scholar, and individual urologic journals published between January 1990 and June 2018. The search terms included “penile curvature,” “Peyronie's,” “Lue,” “Egydio,” “grafting,” “graft,” “penile bend,” “surgical outcomes,” “incision,” and “plaque incision.” Boolean operators (AND, OR) were used with the above terms to refine the search. Data was extracted for the type of study, country of origin, study period, patient demographics, procedure characteristics, measures of ED, measures of deformity, measures of penile length, complications, and operative success. Any study in which plaque incision and excision techniques were combined for analysis were excluded. Data was collected independently and was extracted on an Excel sheet. No funding was available for this study.
Assessing Outcomes
Primary outcome measures included deformity correction, ED, and degree of penile lengthening/shortening. Secondary outcome measures included satisfaction, reoperation rate, and complications.
Results
Study Characteristics
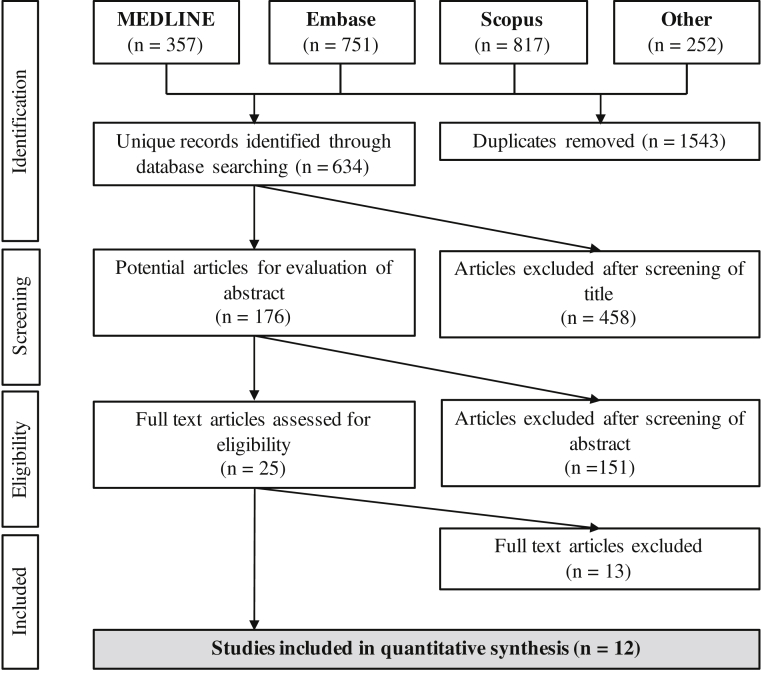
Study characteristics are reported in Table 1. The initial search of 2177 articles identified a total of 12 studies that met our inclusion criteria (Figure 2). These studies were published between 1998 and 2018, covering patients who underwent surgery between 1989 and 2016, a total of 28 years. The studies reported operating on patients in Germany, Spain, Canada, Portugal, Serbia, the United Kingdom, Italy, Turkey, and the United States. A total of 1065 patients underwent the PIG procedure, with 11 studies using retrospective designs and 1 study using a prospective design.
Table 1.
Baseline characteristics for all studies included in the quantitative synthesis
| Type of graft | Lead author | Study characteristics |
Limitations |
Patient demographics |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Year | Number of patients | Follow-up, mo, (SD; range) | Country | Study years | Methodological | Noted by authors | Previous operation | Age, y, mean (SD; range) | Onset duration, mo (SD; range) | Degree of curvature (SD; range) | Complex deformity, % (n/N) | Plaque size, cm | ||
| Xenograft | Sayedahmed19 | 2017 | 43 | 33 (NM; 10–59) | Germany | 2007–2015 | Nonrandomized | No standardized questionnaire for evaluation; no predictive factors for postoperative outcome | NM | 57.4 (NM; 39–82) | sdf 4 | 73.8 (NM; 60–90) | NM | 2.1 (1-4) |
| Cosentino20 | 2016 | 44 | 19.2 (NM; 11–48) | Spain | 2009–2013 | No IIEF, retrospective, no satisfaction measure, no penile length measurement | – | NM | 56.1 (NM; 49–64) | 24 (MM; 9-48) | >60 in 40 patients | NM | NM | |
| Knoll21 | 2007 | 162 | 38 (NM; 6–96) | US | 1998–2006 | No IIEF, retrospective, no satisfaction measurement | – | NM | 52 (NM; 33–69) | 16 (NM; 12–30) | 70 (NM; 60–100)‡ | 0 | 1.5 × 4.0–3.0 × 6.0 | |
| Sansalone22 | 2011 | 157 | 20 (NM; 1224) | Italy/Serbia | 2004–2008 | Retrospective, no penile length measurement | Only 89 patients completed the IIEF. | NM | 55 (±11; 29–70) | sdf 6–12 | NM (NM; NM) | NM | NM | |
| Allograft | Sampaio23 | 2002 | 40 | NM (NM; 16) | Portugal | 1989–1999 | No IIEF, retrospective, no satisfaction measurement | – | NM | 56 (NM; 43–69) | NM (NM; 24–96) | NM (NM; NM) | NM | 1–7 × 2–2.5 |
| Autograft | Kadioglu24 | 2018 | 144 | 51.1 (±39.6; NM) | Turkey | 1997–2016 | No IIEF, retrospective, no satisfaction measurement, no penile length measurement | – | NM | 54.1 (±9.2; NM) | 28.2 (±17.3; NM) | 58.4 (±18.9; NM) | 32.5 (37/114) | NM |
| Kalsi25 | 2005 | 113 | 12 (NM; 8–70) | UK | 1996–2004 | No IIEF, retrospective, no satisfaction measurement | – | 6/113 | 45 (NM; 17–71) | 24 (NM; NM) | 64.5 (NM; 20–180) | 15.9 (18/113)§ | NM | |
| Montorsi26 | 2000 | 50 | 32 (NM; 15–54) | Italy | 1995–1998 | No IIEF, retrospective | – | NM | 44 (NM; 28–62) | sdf 6 | 60 (±4; NM) | NM | NM | |
| Akkus27 | 2001 | 58 | NM | Turkey | 1994–1999 | No IIEF, retrospective, no satisfaction measurement | – | 0/58 | 50 (NM; 39–63) | NM (NM; 12–60) | NM (NM; NM) | NM | NM | |
| El-Sakka13 | 1998 | 112 | NM† | US | 1995–1997 | No IIEF, retrospective | – | NM | 52 (22–73) | sdf 3 | <90 in 82 patients, >90 in 30 patients | 10.7 (12/113) | NM | |
| Multiple | Flores15 | 2011 | 56 | NM | US | 2002–2004 | Retrospective, no satisfaction measurement, no penile length measurement | No recording of pertinent preoperative characteristics, such as mean preoperative curvature, hemodynamics, and erectile function | NM | 57 (±22; NM) | 22 (±9; NM) | 52 (± 23; NM) | 10.7 (6/56) | 4.7 ± 1.2 cm2 |
| Chung28 | 2011 | 86∗ | 98 (NM; 61–120) | Canada | 1995–2005 | Retrospective | Small sample size, patients lost to follow-up, nonrandomized graft material selection, surgery performed across different timelines | 0/86 | 54.6 (NM; 34–73) | 29.1 (NM; 8–60) | 71.7 (NM; 30–160) | NM | NM | |
NM = not mentioned; SD = standard deviation; sdf = stable disease for.
46 contacted for follow-up.
4 had pure hourglass; 4 had concomitant dorsal deformity.
Median.
Waist deformity.
Figure 2.
Flowchart summarizing databases and article selection process.
Patient Demographics
Patient demographic data are reported in Table 1. Only 2 studies reported on whether patients had received previous surgical intervention. The patients ranged in age from 17 to 82 years, and the duration of disease ranged from 16 to 29 months, with all studies reporting at least 3 months of stable disease preoperatively. Average preoperative penile curvature ranged from 52 to 73.8 degrees. A complex deformity (either hourglass or indentation) was present in 10.7%–32.5% of patients. Plaque size was inconsistently reported.
Procedure Characteristics
Characteristics of the procedures are reported in Table 2. A variety of graft materials were reported, with 5 studies using saphenous vein, 5 using small intestinal submucosa, 2 using cadaveric pericardium, 1 using deep dorsal vein, 1 using bovine pericardium collagen matrix, 1 using dermis, and 1 using human dura mater, with some studies reporting the use of multiple grafting materials. Interestingly, 1 study provided histological reports of the graft used (small intestinal submucosa).21 Incision types also varied, with the double-Y (Egydio) incision type more popular in recent years and the H (Lue) incision type more popular in earlier years. Overall, 8 studies used the H type, 4 used the double-Y type, and 2 used the I type. Suture materials used for the attachment of the graft varied greatly, although all studies used a synthetic material. Four studies used absorbable monofilament polydioxanone suture (2 with size 5-0, 1 with size 4-0, and 1 with size 3-0), 2 studies used absorbable braided Vicryl suture (sizes 4-0 and 5-0), 1 study using nonabsorbable monofilament polypropylene suture (size 3-0), 1 study used absorbable monofilament poliglecaprone suture (size 4-0), and 1 study used absorbable braided polyglycolic acid (PGA) suture (size 4-0). Suture types are summarized in Appendix A.
Table 2.
Details of grafting materials and techniques used in the 12 studied reviews
| Type of graft | Lead author | Year | Graft material | Incision | Grafting suture material | NVB dissection | Graft size | Additional grafts | Concurrent convex, % (n/N) |
|---|---|---|---|---|---|---|---|---|---|
| Xenograft | Sayedahmed19 | 2017 | SIS | YY (Egydio) | NM | NM | >20% larger than defect | NM | NM |
| Cosentino20 | 2016 | SIS | H | 4-0 Vicryl | NM | 6.5 cm2; >0.5 cm larger than defect | NM | NM | |
| Knoll21 | 2007 | SIS∗ | H | 4-0 polyglycolic acid | NM | 30% larger than defect | NM | NM | |
| Sansalone22 | 2011 | BPCM | YY (Egydio) | 4-0 poliglecaprone | NM | NM | NM | NM | |
| Allograft | Sampaio23 | 2002 | HDM | I | NM | NM | 0.5 cm wider, 1 cm longer than defect | NM | NM |
| Autograft | Kadioglu24 | 2018 | SV | H/YY (Egydio) | 5-0 PDS | Medial | NM | NM | 33.3 (48/144) |
| Kalsi25 | 2005 | SV | H/I | 3-0 polypropylene/3-0 PDS | Lateral/medial† | NM | (30/113 2x)/(5/113 3x) | 38.1 (43/113) | |
| Montorsi26 | 2000 | SV | H | 5-0 PDS | XXX | NM | (44/50 2x)/(1/50 3x) | 12.0 (6/50) | |
| Akkus27 | 2001 | SV/DDV | H/I | 4-0 Vicryl/5-0 Vicryl | NM | NM | NM | 24.1 (14/58) | |
| El Sakka13 | 1998 | SV | H | NM | NM | NM | 12% >1x | 33.0 (37/112) | |
| Multiple | Flores15 | 2011 | CP (52)/SIS (4) | H/YY (Egydio) | 4-0 PDS | NM | 8 cm2 (SD ±6; range, 4–28) | NM | 0.0 (0/56) |
| Chung28 | 2011 | D (22)/CP (33)/SIS (33) | NM | NM | NM | 20% larger than defect | NM | NM |
BPCM = bovine pericardium collagen matrix; CP = cadaveric pericardium; D = dermal; DDV = deep dorsal vein; HDM = human dura mater; NM = not mentioned; PDS = polydioxanone; SD = standard deviation; SIS = small intestinal submucosa; SV = saphenous vein.
Histological report available.
Medially in patients with ED or arterial risk factors.
ED
ED outcomes are reported in Table 3. Two studies reported improved International Index of Erectile Function (IIEF-5) scores (1 significant at P < .001), and 2 studies reported decreased IIEF scores (both significant at P < .01). None of the studies reporting on IIEF values included both preoperative and postoperative ED status. Notably, Flores et al15 identified preoperative curvature >60°, use of the double-Y incision type, patient age >55 years, and a baseline venous leak (measured by flow-to-maintain and pressure decay) as predictive of a ≥6-point decrease in the erectile function domain of the IIEF.
Table 3.
Preoperative, postoperative and change in erectile function with incision and grafting procedures, where recorded
| Type of graft | Lead author | Year | Preoperative |
Postoperative |
Change | P value | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| IIEF score (SD; range) | Erectile status, % (n/N) |
IIEF score (SD; range) | Erectile status, % (n/N) |
ED change, % (n/N) |
||||||||||
| Unaided | Aided | ED present | Unaided | Aided | Absent | Worsened | Improved | |||||||
| Xenograft | Sayedahmed19 | 2017 | 16 (±3.5; NM) | NM | NM | NM | 20 (±4.2; NM) | 67.4 (29/43) | 20.9 (9/43) | 11.6 (5/43) | 7.0 (3/43) | 69.8 (30/43) | ↑ | <.001 |
| Cosentino20 | 2016 | – | 86.7 (39/44) | NM | 11.4 (5/44) | – | 95.5 (42/44) | 4.6 (2/44) | 0.0 (0/44) | 4.6 (2/44) | NM | ↑ | – | |
| Knoll21 | 2007 | – | NM | NM | 0.0 (0/162) | – | 80.3 (130/162) | 15.4 (25/162) | 4.3 (7/162) | NM | NM | ↓ | – | |
| Sansalone22 | 2011 | 16 (NM; 15–21)† | NM | NM | NM | 22.5 (NM; NM) | 66.9 (105/157) | 33.1 (52/157) | 0.0 (0/157) | NM | NM | ↑ | NM | |
| Allograft | Sampaio23 | 2002 | – | NM | NM | NM | – | NM | NM | NM | 15.0 (6/40) | NM | ↓ | – |
| Autograft | Kadioglu24 | 2018 | – | NM | NM | 25.7 (37/144) | – | 66.7 (96/144) | 21.5 (31/144) | 11.8 (17/144) | NM | NM | ↓ | – |
| Kalsi25 | 2005 | – | 60.2 (68/113) | 39.8 (45/113) | NM | – | 65.5 (74/113) | 11.6 (13/113) | 2.7 (3/113) | 9.7 (11/113) | 3.5 (4/113) | ↓ | – | |
| Montorsi26 | 2000 | – | NM | NM | 0.0 (0/50) | – | NM | NM | NM | 6.0 (3/50) | 0.0 (0/50) | ↓ | – | |
| Akkus27 | 2001 | – | NM | NM | 0.0 (0/58) | – | NM | NM | 0.0 (0/58) | 6.9 (4/58) | 0.0 (0/58) | ↓ | – | |
| El Sakka13 | 1998 | – | NM | NM | 34.8 (39/112) | – | NM | NM | NM | 24.1 (27/112) | 7.1 (8/112) | ↓ | – | |
| Multiple | Flores15 | 2011 | 23 (±4; NM) | 35.7 (20/56) | 64.3 (36/56) | NM | 17 (±9; NM) | NM | NM | NM | NM | NM | ↓ | <.01 |
| Chung28 | 2011 | 15.1 (NM; 6–20) | NM | 14.0 (12/86) | NM | 10.8 (NM; 2–15) | NM | 67.4 (31/46) | NM | NM | NM | ↓ | <.01∗ | |
| Range | – | – | 15.1–23 | 35.7–86.7 | 14.0–64.3 | 0.0–34.8 | 10.8–22.5 | 65.5–95.5 | 4.6–67.4 | 0.0–11.8 | 4.6–24.1 | 0–69.8 | – | – |
Erectile status absent constitutes erectile function insufficient for sexual intercourse; ↑ indicates overall improvement; ↓, overall worsening.
For the penile rigidity domain, sexual desire and intercourse unchanged (P > .05).
Only 89 patients completed the IIEF.
Definitions of ED varied greatly among studies using non-IIEF subjective measures. Therefore, in the present review we categorize erectile function as “unaided,” “aided,” or “present,” with the latter referring to ED noted by studies but with no clear definition given. Preoperatively, 35.7%–86.7% of patients (3 of 12 studies reporting) were able to achieve erections unaided, 14.0%–64.3% (3 of 12 studies reporting) were able to achieve erections aided either pharmacologically or mechanically (ie, by using a vacuum device), and 0–34.8% (6 of 12 studies reporting) had undefined ED. Postoperatively, 65.5%–95.5% of patients (6 of 12 studies reporting) were able to achieve erections unaided, 4.6%–67.4% (7 of 12 studies reporting) were able to achieve erections aided pharmacologically or mechanically, and 0–11.8% (7 of 12 studies reporting) had an absence of erections. Between 4.6% and 24.1% of patients (6 of 12 studies reporting) reported worse erectile function, and 0–69.8% (5 of 12 studies reporting) reported improved erectile function postoperatively. In 3 studies, overall erectile function improved postoperatively, and in 9 studies, overall erectile function worsened postoperatively. Notably, all 3 cases of improved erectile function were reported in studies in which a xenograft was used.
Straightening
Straightening outcomes are reported in Table 4. The definition of successful straightening was not consistent among the reviewed studies, with some studies not reporting the degree of curvature considered successful. One study used a definition of <10°, 2 studies used the definition of <15°, one study used the definition of <20°. Seven studies either did not provide a definition of “straight” or did not report this outcome measure. One study used the definition of a “lack of recurrence.” Between 80.0% and 96.4% of patients (4 of 12 studies reporting) had a “straight” penis postoperatively, with 1.7%–78.3% (8 of 12 studies reporting) developing recurrence. Successful straightening was achieved in 80.0%–96.4% of patients. 3 studies did not report on the percentage of straightening achieved.
Table 4.
Recordings of changes in length and penile straightening following incision and grafting procedures
| Type of graft | Lead author | Year | Length change, % (n/N) |
Straightening, % (n/N) |
|||||
|---|---|---|---|---|---|---|---|---|---|
| Shortening | No change | Lengthening | Straight | Recurrence | Success | Postoperative curvature | |||
| Xenograft | Sayedahmed19 | 2017 | 27.9 (12/43) | 44.2 (19/43) | 27.9 (12/43) | NM | 14.0 (6/43) | 88.4 (38/43) | <15°: 88.4 (38/43); 15°–30°: 7.0 (3/43); >30°: 4.7 (2/43) |
| Cosentino20 | 2016 | NM | NM | NM | NM | NM | NM | NM | |
| Knoll21 | 2007 | 4.9 (8/162) | 46.3 (75/162) | 48.8 (79/162) | NM | 8.6 (14/162) | 91.4 (148/162) | <15°: 91.4 (148/162); >15°: 8.6 (14/162) | |
| Sansalone22 | 2011 | NM | NM | NM† | 87.9 (138/157) | NM | 87.9 (138/157) | <15°: 12.1 (19/157) | |
| Allograft | Sampaio23 | 2002 | NM | 95.0 (38/40) | 5.0 (2/40) | NM | 2.5 (1/40) | NM | NM |
| Autograft | Kadioglu24 | 2018 | NM | NM | NM | NM | 13.9 (20/144) | 87.5 (126/144) | 0°–20°: 87.5 (126/144) |
| Kalsi25 | 2005 | 25.7 (29/113) | NM | NM | NM | NM | 85.8 (97/113) | <10°: 85.8 (97/113); 10°–30°: 10.6 (12/113); >30°: 3.3 (4/113) | |
| Montorsi26 | 2000 | 40.0 (20/50) | 60.0 (30/50)∗ | NM | 80.0 (40/50) | 6.0 (3/50) | 80.0 (40/50) | <30°: 14 (7/50); >30°: 6 (3/50) | |
| Akkus27 | 2001 | 22.4 (13/58) | 77.6 (45/58) | NM | 86.2 (50/58) | 1.7 (1/58) | 86.2 (50/58) | <30°: 12.1 (7/58); >30°: 5.2 (3/58) | |
| El Sakka13 | 1998 | 17.0 (19/112) | 73.2 (82/112) | 9.8 (11/112) | 96.4 (108/112) | 4.5 (5/112) | 96.4 (108/112) | NM | |
| Multiple | Flores15 | 2011 | NM | NM∗ | NM | NM | NM | NM | NM |
| Chung28 | 2011 | 21.7 (10/46) | NM | NM | NM | 78.3 (36/46)‡ | NM | NM | |
| Range | – | – | 4.9–40.0 | 44.2–95.0 | 5.0-48.8 | 80.0–96.4 | 1.7–78.3 | 80.0–96.4 | – |
Straight, defined by the subjective reporting of the penis being straight with no measurement or range of measurements given.
No statistically significant difference in length.
%/N not given, 2.5 cm median gain (range, 1.5–3.5 cm).
Minimal recurrence.
Shortening
Shortening outcomes are reported in Table 4. Between 4.9% and 40.0% of patients (7 of 12 studies reporting) experienced shortening of penile length, 44.2%–95.0% (6 of 12 studies reporting) experienced no change in penile length, and 5.0%–48.8% (4 of 12 studies reporting) experienced penile lengthening. Only 2 studies reported objective measurements of penile length both preoperatively and postoperatively, and both found no statistically significant difference in length. The results from subjective reports are consistent with this, finding that most patients have no change in penile length, with penile lengthening and shortening equally likely following surgery.
Satisfaction, Reoperation, and Complications
Satisfaction, reoperation, and complication rations are reported in Table 5. The satisfaction rates were high in almost all studies that reported this outcome measure, with mean satisfaction ranging between 88.0% and 92.0% (5 of 12 studies reporting). One study was excluded from this range because no absolute number was given, with the authors reporting “more than 65% of patients dissatisfied” and that the “overall satisfaction on a 5-point scale was 2.6.”28 Furthermore, only 46 patients (53.5%) were followed up. Another study was excluded from the range because it measured the partner’s satisfaction with the “cosmetic and functional outcomes of the surgery” rather than the patient’s own satisfaction.22
Table 5.
Complications following incision and grafting procedures, where recorded
| Type of graft | Lead author | Year | Satisfaction, % (n/N) | Reoperation, % (n/N) | Complications, % (n/N) |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| Altered sensation | Recovery from altered sensation | Hematoma | Pain | Edema | Infection | |||||
| Xenograft | Sayedahmed19 | 2017 | 86.0 (37/43) | 4.7 (2/43) | 9.3 (4/43) | NM | NM | 7.0 (3/43) | NM | 0.0 (0/43) |
| Cosentino20 | 2016 | NM | NM | NM | NM | NM | 6.8 (3/44) | 11.4 (5/44) | 2.3 (1/44) | |
| Knoll21 | 2007 | NM | 4.3 (7/162) | 16.7 (27/162) | 100.0 (27/27) | 1.9 (3/162) | 0.0 (0/162) | NM | 0.0 (0/162) | |
| Sansalone22 | 2011 | 97† | NM | 3.2 (5/157) | NM | NM | NM | NM | NM | |
| Allograft | Sampaio23 | 2002 | NM | NM | 22.5 (9/40) | 88.9 (8/9) | 0.0 (0/40) | NM | 20.0 (8/40) | NM |
| Autograft | Kadioglu24 | 2018 | NM∗ | 0.7 (1/144) | NM | NM | NM | NM | NM | NM |
| Kalsi25 | 2005 | NM§ | 0.9 (1/113) | 8.8 (10/113) | 80.0 (8/10) | 0.9 (1/113) | 2.7 (3/113) | NM | NM | |
| Montorsi26 | 2000 | 88.0 (44/50) | NM | 2.0 (1/50) | NM | 4.0 (2/50) | NM | NM | 2.0 (1/50) | |
| Akkus27 | 2001 | NM | NM | NM‖ | 100‖ | NM | NM | NM‖ | NM | |
| El Sakka13 | 1998 | 92.0 (103/112) | NM | 9.8 (11/112) | NM | NM | NM | 2.7 (3/112) | 2.7 (3/112) | |
| Multiple | Flores15 | 2011 | NM | NM | 16.1 (9/56) | 100.0 (9/9) | NM | NM | NM | NM |
| Chung28 | 2011 | <35‡ | NM | 13.0 (6/46) | NM | NM | NM | NM | NM | |
| Range | – | – | 88.0–92.0 | 0.7–4.7 | 2.0–22.5 | 80.0–100.0 | 0.0–4.0 | 0.0–7.0 | 0.0–20.0 | 0.0–2.7 |
Sansalone et al and Chung et al excluded from range.
Success 75.0% (108/144).
Of partners.
>65% dissatisfied.
Success 92.9% (105/113).
No total value given.
The rate of reoperation was between 0.7% and 4.7% (4 of 12 studies reporting), with most reoperations involving implantation of a penile prosthesis indicated for poor postoperative erectile function following PIG surgery. The rates of specific complications varied across the studies, with 2.0%–22.5% of patients (9 of 12 studies reporting) reporting altered sensation and 0–7.0% (4 of 12 studies reporting) reporting pain. Hematoma developed in 0–4.0% (4 of 12 studies reporting), edema developed in 0–20.0% (3 of 12 studies reporting), and infection developed in 0–2.7% (5 of 12 studies reporting). Altered sensation was largely transient, with 80.0%–100.0% of patients (5 of 12 studies reporting) recovering from sensory loss.
Discussion
Peyronie’s disease can have a significant impact on quality of life,29 and surgery remains the mainstay for significantly improving curvature.6 In cases with a larger (>60°) or complex deformity, good erectile function, and concern regarding length loss, PIG techniques are preferred.
Patient Selection
None of the reviewed studies focused on preoperative assessment of ED, and this preoperative assessment was particularly heterogeneously reported. This is critical, because these data are considered in the decision to perform PIG rather than a penile implant.6 The studies reviewed used both subjective and objective assessments of whether PIG was indicated. Subjective factors, such as pain, coital function, duration of disease, erectile function, and distress, may be determined. Validated questionnaires, such as the IIEF30, 31 to assess ED and the Peyronie’s Disease Questionnaire32, 33 to assess general aspects of the disease, are useful tools for standardized assessment. Objective evaluations, including measurement of penile length, degree and direction of curvature, presence of complex deformity, and hemodynamic assessment (using penile duplex ultrasonography with pharmacologic stimulation) also should be included in the preoperative assessment.
Even with the multitude of factors involved in the preoperative assessment of patients with Peyronie’s disease, no consistent predictive factors for de novo ED following PIG surgery have been identified. Using a logistic regression model, Flores et al.15 found that preoperative curvature >60°, use of the Egydio (vs H) incision type, patient age >55 years, and preoperative venous leak (measured by flow-to-maintain and pressure decay) were predictive of a ≤6-point reduction in the erectile function domain score of the IIEF. Although the authors used arterial insufficiency as a hemodynamic assessment factor in their model, they did not describe its impact on the model. However, a later logistic regression model using different factors found that age, deviation, comorbidity, and the number of graft patches were not predictive of postoperative ED, although this was not measured by the IIEF.34 Overall, there are no clear predictive factors for postoperative ED following PIG surgery, and further research is needed to ascertain the most important aspects of preoperative evaluation when considering PIG surgery.
Technique
Neurovascular bundle dissection can be performed with either the lateral or the medial technique. The lateral technique involves incisions of Buck’s fascia above the urethra, at the 5- and 7-o’clock positions. In the medial technique, Buck’s fascia is opened on the dorsal side, and the deep dorsal vein is removed at the most prominent location of the curvature. Five studies described the type of neurovascular bundle dissection technique used, including 3 studies using the medial technique and 2 studies using the lateral technique. Graft size was inconsistently reported. In the studies that reported graft size relative to defect size, it was reported that the graft size should be 20%, or 0.5 cm, greater than the size of the defect. Only earlier studies reported the use of multiple grafts. A concurrent shortening (convex side) procedure was used in 5 studies, which allowed adjustment of an undercorrection or overcorrection after the graft had been applied.
The H incision was the most frequent incision type overall, but the Egydio incision has become equally popular in recent years. The Egydio geometric modifications allow for correction of biplanar defects, reducing the need for additional plications. Although there is no evidence to suggest that additional plications are harmful, their use may lead to complications typically associated with pure plication procedures, such as the presence of palpable knots and length loss.35 The study by Flores et al15 was the sole study that compared incision types, finding an association between the Egydio incision and ED. Although a theoretical comparison of incision types exists,36 no controlled comparison of incision types has been published to date.
An important factor in the correction of penile curvature is the type of suture material used, which may determine the long-term presence of palpable knots, the stability of the graft, and any recurrence of curvature. Absorbable sutures were used in the vast majority of studies, with the majority of studies using absorbable monofilament polydioxanone or poliglecaprone suture material. The second most common sutures used were absorbable braided sutures, including Vicryl and polyglycolic acid. Only 1 study used a nonabsorbable monofilament suture material (polypropylene).22 All sutures were sized between 3-0 and 5-0. The use of larger suture sizes carries a risk of bothersome palpable knots, whereas smaller sutures carry a risk of repair failure. Although no study controlled for differences in suture materials used for securing the graft, the vast majority of studies clearly favored the use of absorbable sutures, and most of the studies used monofilament sutures. The key advantage of absorbable sutures is the avoidance of permanent palpable knots and associated symptoms.
A diverse selection of graft materials has been used, with the autologous vein grafts remaining the most common grafting material. In recent years, small intestinal submucosa has gained popularity. The use of a xenograft over a saphenous vein autograft provides advantages by reducing the operative time and precluding the risk of complications from graft harvesting. Only 1 study presented a comparison of graft materials, including dermis, cadaveric pericardium, and small intestinal submucosa, but this study was unable to identify a superior material.28 Another article presented a histological report of small intestinal submucosa obtained as a biopsy specimen 4 months after surgery, finding that none of the original graft material could be identified, indicating the repopulation of penile connective tissue.21 Owing to the lack of evidence from comparative studies and the inability to determine the best graft material, no clear recommendations for the choice of graft material can be made.
Outcomes
Erectile Function
There was significant variation in how erectile function was recorded and reported in the reviewed studies, presenting challenges to its interpretation. There were inconsistencies within the studies that measured both preoperative and postoperative erectile function using the IIEF, with 2 studies finding improved erectile function and 2 finding worse erectile function.15, 28 In 1 of these studies, poor erectile function outcome may be explained by patient selection.15 Despite the high average preoperative IIEF score, only 35.7% of patients were able to achieve an unaided erection preoperatively, because the erectile function domain of the IIEF-15 does not account for pharmacologic intervention. This study found that the degree of preoperative curvature, use of the Egydio incision, patient age, and a baseline venous leak were all predictive of decreased erectile function. Another study reporting worsened erectile function also had the lowest preoperative erectile function, as defined by the IIEF-5.28 The IIEF-5 is a shortened form of the IIEF-15 that does not account for the full erectile function domain. These results underscore that IIEF scores may be misleading when considering patients for a PIG procedure, and thus establishing whether or not the erections are aided is vital.
All but 1 study using non-IIEF subjective reports described worsening erectile function following PIG, with 4.6%–67.4% of patients requiring pharmacologic intervention, 4.6%–24.1% reporting worse erectile function, and 0.0%–11.8% reporting complete loss of erectile function. Despite this apparent worsening, 65.5%–95.5% of patients were able to achieve unaided erections postoperatively, although this rate may be artificially high owing to the inconsistently reported data. There is disagreement between the studies regarding the extent of ED permitted before PIG surgery is contraindicated. The majority of studies reported on patients with some degree of ED. The 2 studies with low preoperative IIEF scores demonstrated statistically significant improvements in erectile function,22, 28 although it is difficult to ascertain the extent of ED, because the erectile function domain of the IIEF does not account for pharmacologic intervention. Furthermore, a low preoperative IIEF score may reflect an inability to engage in penetrative intercourse owing to penile curvature even with good erectile rigidity. Similarly, a higher postoperative score may reflect an improvement in curvature as opposed to an improvement in erectile rigidity, given that the exclusive use of total IIEF score does not allow for discernment of this difference.
Straightening
Restoration of penile linearity is the principal aim of curvature-correcting surgery; however, there is no standardized format for reporting this variable. As a result, it was the most heterogeneously reported variable, with definitions varying from “straight” to <10°, <15°, <20°, and <30°. This variation hinders interpretation of the anatomic outcomes of this procedure, because it prevents application of standard quantitative synthesis methods. Using the individual studies’ definitions of success, satisfactory straightening was achieved in 80.0%–96.4% of patients, with unsatisfactory straightening thus present in 3.6%–20.0% of patients.
Length Change
Because PIG procedures lengthen the shortened side, they are not associated with the length loss experienced with operations that shorten the longer side. The majority of studies reported either no change or an increase in postoperative penile length. Only 2 studies objectively measured penile length both preoperatively and postoperatively and found no statistically significant change in stretched penile length.15, 26
Complications and Reoperation
Reporting of specific complications varied, with altered sensation, hematoma, pain, oedema and infection being the most commonly reported. Despite the high rate of hypoesthesia, the majority of cases (80.0%–100.0%) involved only a transient loss or reduction of sensation. Although reported in only 3 cases, rates of infection were consistently low. Reoperation rates were also low (0.7%–4.7%), and reoperation was most commonly indicated for poor postoperative erectile function. Implantation of a penile prosthesis was the most common reoperation performed. With overall low rates of complications and reoperation, the PIG technique continues to demonstrate its safety.
Satisfaction
In the studies in which satisfaction was reported, the PIG procedure was consistently associated with high rates of satisfaction ranging from 88.0% to 92.0%. Chung et al28 reported a lower satisfaction rate, which they ascribed to their longer follow-up interval by noting recurrence of curvature, loss of length, and de novo ED as the main causes of dissatisfaction. Although outcomes are naturally important in determining overall satisfaction, sampling problems may influence the results, because only 53.5% of patients were followed up and responded to satisfaction questionnaires. It is also difficult to determine the cause of ED in long-term follow-up, given the natural decline in erectile function with age. Overall, satisfaction rates were very high.
Study Limitations
The sole prospective study used a nonrandomized design,19 only 4 studies used the IIEF as a measure of erectile function,15, 19, 22, 28 7 studies included no measure of patient satisfaction,15, 20, 21, 23, 24, 25, 27 and 4 studies used no measure of penile length.15, 20, 22, 24 Only 4 studies reported limitations.15, 19, 22, 28 Sayedahmed et al19 did not use a standardized questionnaire for evaluation and did not analyze predictive factors for postoperative outcomes. In the study reported by Sansalone et al,22 only 89 of 157 patients completed the IIEF. Flores et al15 described the lack of recording of pertinent preoperative characteristics as a key limitation. Chung et al28 identified their small sample size, large number of patients lost-to-follow-up, nonrandomized graft material selection, and performance of surgeries across different timelines as key limitations.
The inconsistency of data reporting is a key limitation of the present review. The studies themselves provided low-level evidence, with only case series reported. The use of studies from a long time period is a further limitation, because the data might not entirely reflect the modern practice of the technique.
Future Research
Although the use of collagenase Clostridium histolyticum has demonstrated effectiveness at resolving minor curvatures,37, 38 surgery remains the only way to correct large curvatures. Therefore, it is important to continuously assess the effectiveness of techniques, assess the indications for surgery, and innovate new approaches. Randomized controlled trials are needed to assess the variations between techniques. Prospective cohort and case-control studies should be considered to assess the outcomes of individual techniques, particularly those for assessing ED.
Future research should investigate the association between preoperative patient characteristics and postoperative ED, using a model that considers continuous predictors and outcome measures, investigates a greater variety of assessment methods, and uses more sensitive measures of preoperative and postoperative erectile function. Furthermore, future studies should investigate grafting material and incision type using a randomized and controlled methodology.
Conclusion
PIG continues to demonstrate its effectiveness in terms of satisfaction, length change, straightening, and complications. Various techniques are still used, with no single approach proving superior to the others. Inconsistent findings regarding postoperative ED remain. Accurate preoperative assessment and selection are critical.
Statement of authorship
Category 1
-
(a)Conception and Design
- Patrick G. Rice, Bhaskar K. Somani, and Rowland W. Rees
-
(b)Acquisition of Data
- Patrick G. Rice, Bhaskar K. Somani, and Rowland W. Rees
-
(c)Analysis and Interpretation of Data
- Patrick G. Rice and Rowland W. Rees
Category 2
-
(a)Drafting the Article
- Patrick G. Rice, Bhaskar K. Somani, and Rowland W. Rees
-
(b)Revising It for Intellectual Content
- Patrick G. Rice and Rowland W. Rees
Category 3
-
(a)Final Approval of the Completed Article
- Patrick G. Rice, Bhaskar K. Somani, and Rowland W. Rees
Footnotes
Conflicts of Interest: The authors report no conflicts of interest.
Funding: None.
Supplementary data related to this article can be found at https://doi.org/10.1016/j.esxm.2019.01.001.
Supplementary Data
References
- 1.Nesbit R.M. Congenital curvature of the phallus: Report of three cases with description of corrective operation. J Urol. 1965;93:230–232. doi: 10.1016/S0022-5347(17)63751-0. [DOI] [PubMed] [Google Scholar]
- 2.Mulhall J.P., Creech S.D., Boorjian S.A. Subjective and objective analysis of the prevalence of Peyronie’s disease in a population of men presenting for prostate cancer screening. J Urol. 2004;171:2350–2353. doi: 10.1097/01.ju.0000127744.18878.f1. [DOI] [PubMed] [Google Scholar]
- 3.Bekos A., Arvaniti M., Hatzimouratidis K. The natural history of Peyronie's disease: An ultrasonography-based study. Eur Urol. 2008;53:644–651. doi: 10.1016/j.eururo.2007.07.013. [DOI] [PubMed] [Google Scholar]
- 4.Nelson C.J., Diblasio C., Kendirci M. The chronology of depression and distress in men with Peyronie's disease. J Sex Med. 2008;5:1985–1990. doi: 10.1111/j.1743-6109.2008.00895.x. [DOI] [PubMed] [Google Scholar]
- 5.Walsh T., Hotaling J., Lue T. How curved is too curved? The severity of penile deformity may predict sexual disability among men with Peyronie's disease. Int J Impot Res. 2013;25:109–112. doi: 10.1038/ijir.2012.48. [DOI] [PubMed] [Google Scholar]
- 6.Chung E., Ralph D., Kagioglu A. Evidence-based management guidelines on Peyronie's disease. J Sex Med. 2016;13:905–923. doi: 10.1016/j.jsxm.2016.04.062. [DOI] [PubMed] [Google Scholar]
- 7.Devine C.J., Jr., Horton C.E. Surgical treatment of Peyronie's disease with a dermal graff. J Urol. 1974;111:44–49. doi: 10.1016/s0022-5347(17)59886-9. [DOI] [PubMed] [Google Scholar]
- 8.Lowsley O.S., Boyce W.H. Further experiences with an operation for the cure of Peyronie's Disease. J Urol. 1950;63:888–899. doi: 10.1016/S0022-5347(17)68843-8. [DOI] [PubMed] [Google Scholar]
- 9.Dalkin B.L., Carter M.F. Venogenic impotence following dermal graft repair for Peyronie's disease. J Urol. 1991;146:849–851. doi: 10.1016/s0022-5347(17)37941-7. [DOI] [PubMed] [Google Scholar]
- 10.Gelbard M.K., Hayden B. Expanding contractures of the tunica albuginea due to Peyronie's disease with temporalis fascia free grafts. J Urol. 1991;145:772–776. doi: 10.1016/s0022-5347(17)38447-1. [DOI] [PubMed] [Google Scholar]
- 11.Gelbard M.K. Relaxing incisions in correction of penile deformity due to Peyronie's disease. J Urol. 1995;154:1457–1460. [PubMed] [Google Scholar]
- 12.Lue T.F., El-Sakka A.I. Venous patch graft for Peyronie's disease. Part I: Technique. J Urol. 1998;160:2047–2049. doi: 10.1097/00005392-199812010-00029. [DOI] [PubMed] [Google Scholar]
- 13.El-Sakka A.I., Rashwan H.M., Lue T.F. Venous patch graft for Peyronie's disease. Part II: Outcome analysis. J Urol. 1998;160(6 Pt 1):2050–2053. doi: 10.1097/00005392-199812010-00030. [DOI] [PubMed] [Google Scholar]
- 14.Egydio P.H., Lucon A.M., Arap S. Treatment of Peyronie's disease by incomplete circumferential incision of the tunica albuginea and plaque with bovine pericardium graft. Urology. 2002;59:570–574. doi: 10.1016/s0090-4295(01)01651-x. [DOI] [PubMed] [Google Scholar]
- 15.Flores S., Choi J., Alex B. Erectile dysfunction after plaque incision and grafting: Short-term assessment of incidence and predictors. J Sex Med. 2011;8:2031–2037. doi: 10.1111/j.1743-6109.2011.02299.x. [DOI] [PubMed] [Google Scholar]
- 16.Ralph D., Gonzalez-Cadavid N., Mirone V. The management of Peyronie's disease: Evidence-based 2010 guidelines. J Sex Med. 2010;7:2359–2374. doi: 10.1111/j.1743-6109.2010.01850.x. [DOI] [PubMed] [Google Scholar]
- 17.Garcia-Gomez B., Ralph D., Levine L. Grafts for Peyronie's disease: A comprehensive review. Andrology. 2018;6:117–126. doi: 10.1111/andr.12421. [DOI] [PubMed] [Google Scholar]
- 18.Moher D., Liberati A., Tetzlaff J. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sayedahmed K., Rosenhammer B., Spachmann P. Bicentric prospective evaluation of corporoplasty with porcine small intestinal submucosa (SIS) in patients with severe Peyronie’s disease. World J Urol. 2017;35:1119–1124. doi: 10.1007/s00345-016-1973-5. [DOI] [PubMed] [Google Scholar]
- 20.Cosentino M., Kanashiro A., Vives A. Surgical treatment of Peyronie's disease with small intestinal submucosa graft patch. Int J Impot Res. 2016;28:106–109. doi: 10.1038/ijir.2016.10. [DOI] [PubMed] [Google Scholar]
- 21.Knoll L.D. Use of small intestinal submucosa graft for the surgical management of Peyronie’s disease. J Urol. 2007;178:2474–2478. doi: 10.1016/j.juro.2007.08.044. [DOI] [PubMed] [Google Scholar]
- 22.Sansalone S., Garaffa G., Djinovic R. Long-term results of the surgical treatment of Peyronie's disease with Egydio's technique: A European multicentre study. Asian J Androl. 2011;13:842–845. doi: 10.1038/aja.2011.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sampaio J., Fonseca J., Passarinho A. Peyronie’s disease: Surgical correction of 40 patients with relaxing incision and duramater graft. Eur Urol. 2002;41:551–555. doi: 10.1016/s0302-2838(02)00071-4. [DOI] [PubMed] [Google Scholar]
- 24.Kadıoğlu A., Salabaş E., Özmez A. Peyronie’s disease surgery: Surgical outcomes of 268 cases. Turk J Urol. 2018;44:10–15. doi: 10.5152/tud.2018.87405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kalsi J., Minhas S., Christopher N. The results of plaque incision and venous grafting (Lue procedure) to correct the penile deformity of Peyronie's disease. BJU Int. 2005;95:1029–1033. doi: 10.1111/j.1464-410X.2005.05459.x. [DOI] [PubMed] [Google Scholar]
- 26.Montorsi F., Salonia A., Maga T. Evidence based assessment of long-term results of plaque incision and vein grafting for Peyronie's disease. J Urol. 2000;163:1704–1708. [PubMed] [Google Scholar]
- 27.Akkus E., Ozkara H., Alici B. Incision and venous patch graft in the surgical treatment of penile curvature in Peyronie’s disease. Eur Urol. 2001;40:531–537. doi: 10.1159/000049831. [DOI] [PubMed] [Google Scholar]
- 28.Chung E., Clendinning E., Lessard L. Five-year follow-up of Peyronie's graft surgery: Outcomes and patient satisfaction. J Sex Med. 2011;8:594–600. doi: 10.1111/j.1743-6109.2010.02102.x. [DOI] [PubMed] [Google Scholar]
- 29.Nelson C.J., Mulhall J.P. Psychological impact of Peyronie's disease: A review. J Sex Med. 2013;10:653–660. doi: 10.1111/j.1743-6109.2012.02999.x. [DOI] [PubMed] [Google Scholar]
- 30.Rosen R.C., Riley A., Wagner G. The international index of erectile function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology. 1997;49:822–830. doi: 10.1016/s0090-4295(97)00238-0. [DOI] [PubMed] [Google Scholar]
- 31.Rosen R.C., Cappelleri J., Smith M. Development and evaluation of an abridged, 5-item version of the International Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunction. Int J Impot Res. 1999;11:319–326. doi: 10.1038/sj.ijir.3900472. [DOI] [PubMed] [Google Scholar]
- 32.Coyne K.S., Currie B.M., Thompson C.L. Responsiveness of the Peyronie's Disease Questionnaire (PDQ) J Sex Med. 2015;12:1072–1079. doi: 10.1111/jsm.12838. [DOI] [PubMed] [Google Scholar]
- 33.Coyne K.S., Currie B.M., Thompson C.L. The test-retest reliability of the Peyronie's disease questionnaire. J Sex Med. 2015;12:543–548. doi: 10.1111/jsm.12769. [DOI] [PubMed] [Google Scholar]
- 34.Wimpissinger F., Parnham A., Gutjahr G. 10 Years' plaque incision and vein grafting for Peyronie's disease: Does time matter? J Sex Med. 2016;13:120–128. doi: 10.1016/j.jsxm.2015.12.004. [DOI] [PubMed] [Google Scholar]
- 35.Gholami S.S., Lue T.F. Correction of penile curvature using the 16-dot plication technique: A review of 132 patients. J Urol. 2002;167:2066–2069. [PubMed] [Google Scholar]
- 36.Miranda A.F., Sampaio F.J. A geometric model of plaque incision and graft for Peyronie's disease with geometric analyses of different techniques. J Sex Med. 2014;11:1546–1553. doi: 10.1111/jsm.12462. [DOI] [PubMed] [Google Scholar]
- 37.Gelbard M., Goldstein I., Hellstrom W.J. Clinical efficacy, safety and tolerability of collagenase Clostridium histolyticum for the treatment of peyronie disease in 2 large double-blind, randomized, placebo controlled phase 3 studies. J Urol. 2013;190:199–207. doi: 10.1016/j.juro.2013.01.087. [DOI] [PubMed] [Google Scholar]
- 38.Levine L.A., Cuzin B., Mark S. Clinical safety and effectiveness of collagenase Clostridium histolyticum injection in patients with Peyronie's disease: A phase 3 open-label study. J Sex Med. 2015;12:248–258. doi: 10.1111/jsm.12731. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.