Abstract
Parkinson’s disease (PD) is the second most common degenerative disorder. Although the disease was described more than 200 years ago, its pathogenetic mechanisms have not yet been fully described. In recent years, the discovery of the association between mutations of the GBA gene (encoding for the lysosomal enzyme glucocerebrosidase) and PD facilitated a better understating of this disorder. GBA mutations are the most common genetic risk factor of the disease. However, mutations of this gene can be found in different phenotypes, such as Gaucher’s disease (GD), PD, dementia with Lewy bodies (DLB) and rapid eye movements (REM) sleep behavior disorders (RBDs). Understanding the pathogenic role of this mutation and its different manifestations is crucial for geneticists and scientists to guide their research and to select proper cohorts of patients. Moreover, knowing the implications of the GBA mutation in the context of PD and the other associated phenotypes is also important for clinicians to properly counsel their patients and to implement their care. With the present review we aim to describe the genetic, clinical, and therapeutic features related to the mutation of the GBA gene.
Keywords: glucocerebrosidase, Parkinson’s disease, Gaucher’s disease, Lewy Body Dementia, REM sleep behavior disorders
1. Introduction
GBA is a gene located on chromosome 1 (1q21) encoding for the glucocerebrosidase (GCase), a lysosomal enzyme involved in the metabolism of glucosylceramide. The mutation of this gene has been classically associated with Gaucher’s disease, a systemic disorder with a variable degree of involvement of the central nervous system. Surprisingly, about 14 years ago it was observed that mutations in this same gene were associated with an increased incidence of Parkinson’s disease (PD), in both Gaucher’s patients as well as asymptomatic carriers [1,2,3,4]. PD is the second most common neurodegenerative disorder, affecting 2–3% of the world population over the age of 65 [5]. It is caused by the progressive loss of dopaminergic neurons in the substantia nigra. Classically it presents with a combination of bradykinesia, rigidity, resting tremor, and postural instability. However, a list of non-motor features, such as hyposmia, constipation, urinary symptoms, orthostatic hypotension, anxiety, depression, impaired sleep, and cognitive impairment can present as well in various degrees [5]. Since the first observations of GBA and PD, their association has been extensively explored. Different hypotheses have been formulated to explain the causative role of this mutation in PD [6]. First of all, GCase is part of the endolysosomal pathway, which seems to be particularly crucial in the pathogenesis of PD. Indeed, many different monogenic familial forms of PD are caused by genes involved in this pathway [7]. Moreover, mutated GCase is not able to fold properly and thus can accumulate in different cellular compartments of the dopaminergic neurons, causing a cell stress response that can be deleterious of the cells. In addition, impaired GCase activity seems to cause an accumulation of alpha-synuclein (for a comprehensive review see [8]).
Today we know that GBA mutations are the major genetic risk factor for PD. Impaired GCase activity has been identified also in idiopathic cases of PD patients who did not carry a mutation in the gene, suggesting a central role of this enzyme in the pathogenesis of the disease [9,10].
In the present review, we aim to summarize the genetic changes and the characteristic features associated with the mutations of this gene, spanning from Gaucher’s disease to PD and the other described phenotypes. This will aid in a better understanding of the pathogenic role of this mutation. The identification of these phenotypes will allow for clinicians to offer more appropriate counseling to the patients and their families.
2. Pathogenetic Mutations of the GBA Gene
2.1. GBA Mutation and Gaucher’s Disease (GD)
Gaucher’s disease (GD) is a systemic disorder that can present with a various degree of systemic and neurological manifestations. According to the severity of the disease and the neurological involvement, three different types of GD have been identified. GD type 1 has been classically considered only a systemic disorder, with no neurological involvement whatsoever. Anemia, leukopenia, thrombocytopenia with frequent bleeding, osteopenia with bone pain, easy fractures, Erlenmeyer flask deformity, as well as hepatosplenomegaly, failure to grow, and puberty delay can be presenting features of this disease [11,12,13,14]. Monoclonal gammopathy has been reported as well [15]. The disease can manifest early in childhood but it may remain undiagnosed until adulthood when the phenotype is mild. The pathological hallmarks of the disease are the so-called Gaucher cells, macrophages engorged with aberrant lysosomes as a consequence of the GCase-impaired activity. Symptoms are caused by the infiltration of these cells in the reticuloendothelial system of the affected organs [16]. In recent years, the natural history of GD type 1 has dramatically changed since the introduction of target treatments, such as enzyme replacement therapy (ERT) (human recombinant enzyme to be administered intravenously every other week) and oral substrate reduction therapy (SRT) [17]. Treatments with these two approaches are able to address the majority of the systemic symptoms associated with GD type 1 and those in GD type 3. So far, SRT has been approved only for subjects over the age of 18 years. However, in the adult population it represents an important alternative first line treatment. Unfortunately, these therapies are not able to cross the blood-brain barrier and therefore they are not suitable for the treatment of the neurological complications associated with GD type 2 and 3. The two latest forms are also referred to as the acute (type 2) and chronic (type 3) neuronopathic form. Patients affected with GD type 2 start manifesting severe symptoms very early, usually within the first six months of life. They usually present a combination of severe neurological manifestations, with brainstem involvement (i.e., eye movement abnormalities, spasticity, hypotonia) and seizure, as well as life-threatening systemic symptoms, such as respiratory distress and aspiration pneumonia [18,19]. Skin manifestations, like ichthyosis or collodion abnormalities, as well as hydrops fetalis, can be present. Prognosis is very poor and death usually occurs before the age of four [20]. GD type 3 (chronic neuronopathic form) has been further classified as GD type 3a,b,c. GD type 3a presents a milder visceral phenotype, but can be associated with severe and life-threatening myoclonic seizures. GD type 3b, instead, is characterized by a more prominent visceral involvement [21]. Interestingly, one of the features that have been used to try to discriminate between patients with GD type 1 and the milder neuropathic form GD type 3 is the assessment of the eye movements. Indeed, patients with GD type 3, especially type b, present with characteristic eye movement abnormalities. In particular they show loss of horizontal before vertical gaze palsy and slowing of the saccades, suggesting involvement of the brainstem. GD type 3c, instead, is the only subtype of the disease presenting with cardiac mitral and aortic calcification and poor prognosis [21]. A particular cluster of patients with GD type 3 has been identified among the Swedish population. This is also referred as Norrbottnian form, because of its geographical distribution. It is associated with the c.1448T > G mutation and it presents with an early and severe splenomegaly and a combination in the first or second decade of ataxia, spastic paresis, horizontal supranuclear gaze palsy, kyphoscoliosis and other orthopedic abnormalities, cognitive impairment, and seizures [22].
Those different phenotypes are associated with discrete genetic mutations, as detailed below.
Different Pathogenic Mutations of GBA Associated with Gaucher’s Disease (GD) Subtypes
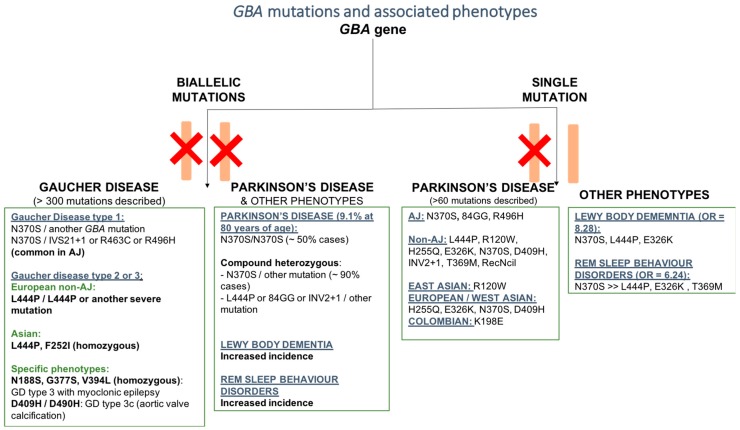
More than 300 variants of the GBA gene have been associated with Gaucher’s disease [23]. GD is an autosomal recessive disorder. In order for the disease to manifest, patients need to carry a pathogenic mutation on both alleles of the GBA gene, either in a homozygous or compound heterozygous fashion. Point mutations, insertion, deletion, missense mutations, splice junctions, and concomitant multiple mutations have been reported [24]. The different variants can be more represented in particular ethnic groups as well as in particular phenotypes. The c.1226A < G (N370S; or N409S according to the new nomenclature) mutation is the most common one among Ashkenazi Jew (AJ) patients, followed by the c.84dupG (84GG) mutation, which is more rare. The c.115 + 1G > A (IVS2 + 1), c.1504C > T (R463C), and c.1604G > A (R496H) are commonly found in AJ patients with GD type 1 [24]. On the contrary, the N370S mutation is rarely found among Chinese and Japanese patients [24] (Hruska et al., 2008). Among Asian ethnic groups, the c.1448T > C (L444P, or L483P according to the new nomenclature) and the c.754T > A (F252I), usually associated with GD type 2 and 3, are more prevalent, also explaining why among these populations the neuropathic forms of GD are more frequent [20]. c.1448T > C (L444P) is also the most frequent mutation among Caucasians with a non-Ashkenazi Jew ancestry [25] (Figure 1).
Figure 1.
Schematic representation of the most common pathogenic mutations of the GBA genes and associated phenotypes. Phenotypes were grouped based on homozygous and heterozygous mutations, ancestry, and specific associated features.
Different mutations can lead to different phenotypes of GD. The c.1226A > G (N370S) mutation is associated only with Gaucher’s disease type 1 and it seems to be protective for the development of the neurological involvement characteristic of GD type 2 and 3. Indeed, patients who present the c.1226A > G (N370S) mutation on at least one allele of the GBA gene will manifest only GD type 1 [24]. Interestingly, subjects who are homozygous for the N370S variant can also remain asymptomatic for the disease. On the other hand, the c.1448T > C (L444P) mutation is usually associated with GD type 2 or 3, even when presenting in a compound heterozygous state [19]. Homozygous c.1448T > C (L444P) mutation [c.1448T > C]1[c.1448T > C] (L444P/L444P) with no recombinant alleles can be associated with very severe but also milder phenotypes [26]. The c.1342G > C (D409H) variant is responsible for GD type 3c which presents with characteristic cardiac valve calcifications [27]. c.680A > G (N188S), c.1246G > A (G377S), and c.1297G > T (V394L) are more likely to be associated with myoclonic epilepsy [28,29,30]. Despite previously reported observations, it is commonly found that members of the same family report variability in the manifestation of symptoms even with an identical genotype, suggesting that a genotype/phenotype correlation is tentative still. Other reported mutations are uniquely rare and oftentimes private among specific families. [12]. Hence, it is difficult to make generalizations about these mutations specific phenotypical profiles.
Another interesting mutation is the c.1093G > A (E326K), which caused a lot of debate in the literature [31]. Indeed, it is not clear whether this mutation is really pathogenic for GD, since it was found also in a significant number of asymptomatic carriers in homozygosity [32,33]. However, when associated with other GBA mutations on the same allele, it can cause severe impairment of the GCase activity [34,35]. Interestingly enough, the same mutation seems to be significantly associated with an increased risk of PD [33].
2.2. GBA Mutation and Parkinson’s Disease (PD)
2.2.1. Pathogenic Mutations of GBA Associated with PD
More than a decade ago, the association between an increased risk of developing PD and the presence of GBA mutations was initially noticed in large Gaucher’s disease clinics. The incidence of PD among GD patients and their relatives, which were supposedly carriers for the mutation, seemed to be higher than the general population. Initially, only single case reports were suggesting this association. Interestingly, PD was noticed in patients with GD type 1, which has always been considered the non-neuropathic form of the disease [36,37,38,39,40,41]. It was only when larger populations of PD patients were screened for mutations of this gene that the important role of GBA in the pathogenesis of PD was assessed worldwide.
So far, more than 50 population studies have screened the GBA gene among PD patients, covering a large number of ancestries (reviewed in [42,43]). Overall, these studies demonstrated that the incidence of GBA mutations is significantly higher among PD patients, compared to non-affected subjects. Compared to GD, a smaller number of GBA mutations have been reported in patients with PD (about 130 GBA mutations) [42]. However, in many of these studies, only the mutations that are most commonly associated with PD were screened. Therefore, less frequent variants still associated with the disease could go undetected. Among all, the c.1226A > G (N370S) and the c.1448T > C (L444P) mutations are the two most common mutations worldwide. Indeed, in some populations they account for the 70–80% of the total number of variants of GBA associated with PD [44]. Among subjects from eastern Europe with an AJ ancestry, the c.1226A > G (N370S) mutation is definitely the most frequent one among PD patients, as already reported for GD (Figure 1). Among the non-AJ European descendants, the c.1448T > C (L444P) mutation is more common. Interestingly, it has been reported that some mutations are able to increase the risk of PD only in the context of specific ancestry [42]. This is the case of the c.84dupG (84GG) and c.1604G > A (R496H) for AJ subjects, the c. 475 C > T (R120W) for East Asian populations, and the c.882T > G (H255Q), c.1093G > A (E326K), c.1342G > C (D409H), and c.1226A < G (N370S), which are only found in subjects of European or West Asian ancestry [42] (Figure 1). A recent study identified an increased incidence of the K198E variant (previously described in GD1 and GD2 patients) in a population of PD patients from Columbia compared to controls [43]. It seems that severe GBA mutations (as classified according to the subtype of GD that they are associated with), such as c.84dupG (84GG), c.115 + 1G >A (IVS2 + 1), c.1297G > T (V394L), c.1342G > C (D409H), c.1448T > C (L444P), and c.1263del + RecTL, are associated with a higher risk of causing PD compared to milder mutations, such as the N370S and c.84dupG (84GG) [45]. Moreover, severe mutations are associated with an earlier age of onset, as well as a more rapid progression and increased involvement of cognitive functions [45,46,47]. In one study, the motor and some of the non-motor symptoms (such as depression, REM sleep behavior disorders, and hyposmia) were significantly worse in PD patients carrying severe GBA mutations compared to subjects carrying mild mutations or with idiopathic PD [48].
Interestingly, GBA represents only a risk factor for PD. This means that not every carrier will develop the disease. The reason for the reduced penetrance of these mutations has not yet been fully elucidated. Based on large population studies, today we know that, among GBA carriers, about 9.1% will develop PD. Some reports suggest that the penetrance of PD in GD patient is 30% at 80 years, but this data needs to be confirmed by further studies [49]. Patients with a homozygous mutation of GBA, thus affected with Gaucher’s disease, have a higher risk of developing PD and usually with an earlier age of onset of symptoms [48]. Having said that, it is worth noticing that the majority of subjects with GD will never develop PD, even in the case of severe mutations. It is still controversial whether PD in patients with GD presents with a more severe phenotype compared to GBA carriers. Carriers of the GBA mutation harbor an increased risk of developing PD by five times in heterozygous carriers and 10–20 times in homozygous carriers [50,51,52,53]. GBA mutations are present in about 2–30% of PD patients [54]. Carrier frequency can be very different across different ancestry. Among AJs, it goes from 10 to 31%, while in Norwegian’s it is only 2.3% [54]. In patients of European non-AJ ancestry, it ranges from 2.9 to 12% [54].
In the last few years, there has been a great effort to try to clarify the pathogenic role of the GBA mutations in PD and many different hypotheses have been formulated, as reported above (for review see [8]). It is important to note that a growing amount of data is suggesting a failure of the endolysosomal and of the autophagic pathways in PD [55]. These scavenger systems are crucial for the degradation of alpha-synuclein, whose accumulation in the dopaminergic neurons is one of the hallmarks of PD. In the lysosome, GCase plays an important contribution for these processes and, in particular, in the interplay with alpha-synuclein [56]. Therefore, it is not totally surprising that a dysfunction of this enzyme is related to PD. How the different mutations of GBA that have been described in PD patients are able to affect the activity of the GCase has not been fully understood. We know that the GCase has three active domains. PD-associated mutations are found in distinctive domains of the protein. The c.1342G > C (D409H) and c.1297G > T (V394L) variants are located in domain I. The c.84dupG (84GG) mutation causes a frameshift that can induce aberrantly shorter or longer proteins that are non-functioning [23]. Other mutations, instead, are not found in the functional domains but do interfere with the final structure of the enzyme, thus making it more unstable or affecting its interaction with other proteins. The c.1226A > G (N370S) and c.1448T > C (L444P) mutations are, for example, located in the proximity of the binding site of the Saposin C, an activator of GCase [57]. More importantly, SapC competes with the binding of alpha-synuclein to GCase, which would cause the inhibition of the enzyme [58,59]. Interestingly, the c.1226A > G (N370S) mutation also seems to affect the ability of the GCase to modify the conformation of one of its loops, loop 3, according to changes in pH [60,61]. Conformational changes in response to the changes of the cellular environment are critical for the proper function of the protein. Despite our knowledge about the structural effects of the different mutations, the exact correlation between the localizations of pathogenetic variants of the gene and the degree of expression of PD has not yet been fully described.
It is also worth noting that GBA presents a pseudogene (GBAP1) that shares a very high degree of homology—96% sequence identity–located in the proximity of the original gene [62,63]. Therefore, genetic analysis will have to take this into account and should be performed in a specialized laboratory in order to obtain reliable results. New technologies, such as the long-read sequencer, are on the horizon for even more in-depth identification of possible GBA mutations [64].
2.2.2. GBA Mutations and Parkinson’s Disease Phenotype
PD patients carrying GBA mutations are not easily recognizable in most cases because they do not present exclusive features that would clearly distinguish them from patients with idiopathic PD (iPD). However, large population studies comparing carriers vs. non-carriers, mild vs. severe mutations, as well as heterozygous manifesting carriers vs. PD–GD patients, allowed the ability to define common traits in these subgroups of patients (for a comprehensive review see [8]). In particular, GBA–PD patients present an overall earlier age of onset compared to non-carriers. Disease manifests about 3–6 years earlier in heterozygous carriers, irrespectively of the severity of the mutation, and about 6–11 years earlier in subjects with homozygous mutations [45,46,48,54,65,66,67,68,69,70]. There are limited reports of GBA mutation carriers having an age of onset in the 20′s. [31,54,71,72,73].
The progression of the disease has been characterized in many different studies by a more pronounced cognitive deficit in a significant percentage of these patients, with a risk of developing dementia up to three times higher compared to iPD, which is even more increased in patients with severe mutations [46,48,74]. Hallucinations and REM sleep behavior disorders (RBD) also are more common among GBA patients in a dose-dependent fashion, being more frequent in subjects with homozygous mutations and in patients carrying severe vs. milder mutations. However, other non-motor symptoms, such as depression and anxiety, constipation, urinary symptoms, orthostatic hypotension, and sexual dysfunctions are over-represented as well in GBA carriers compared to iPD, especially in the presence of severe mutations, but with no increased severity in GD patients [46,48,75,76]. An increased incidence of dysautonomic features has been suggested to be the main driver of the slightly reduced survival reported in these patients [77]. Motor complications, such as dysphagia, dysarthria, and freezing of gait, are more frequent as well in GBA carriers [46,67].
In patients with GBA mutations and PD, the rigid akinetic phenotype seems to be more common. Usually, these patients present a very good response to levodopa, although the progression of the motor symptoms can be slightly faster compared to iPD but without higher rates of motor fluctuations or dyskinesia. Therefore, no specific treatment approaches need to be considered for this subgroup of patients. Interestingly, a recent study evaluated the outcomes of treatment with deep brain stimulation (DBS) in a cohort of PD patients carrying GBA mutations [78]. After a follow up of 7.5 years on average, it was noticed that the het-GBA cohort presented similar outcomes compared to iPD in terms of motor symptoms, while cognitive impairment and non-motor symptoms were definitely more represented among carriers [78]. However, because of the beneficial effect on the motor symptoms, DBS should be considered as a suitable option for these patients.
2.2.3. GBA Mutations and Other Phenotypes
GBA mutations were identified also in cases of REM sleep behavior disorders (RBD) and in cases of dementia with Lewy bodies (DLB) [79].
GBA and Dementia with Lewy Bodies
A relatively low number of studies have been conducted to explore the incidence of the GBA mutation among patients affected with dementia with Lewy bodies (DLB), which was found to be even higher compared to the one in PD patients. In a cohort study of DLB patients, the frequency of GBA mutations was 7.49% with an odd ratio of 8.28 [79]. In another study in Spanish subjects, and in a number of autoptic brain tissues from pathologically proven DLB patients, a GBA mutation was identified in 12–13% of the cases [80]. Recent genome-wide association studies (GWAS) also confirmed the significant association between GBA mutations and DLB (particularly the rs35749011 variant) [81]. Among GBA carriers, the risk of developing DLB is about three times greater than developing PD [82].
As well as in PD patients, GBA mutations are associated with an earlier age of onset in DLB cases compared to non-carriers (of approximately five years) and a higher disease severity score [79,80]. The association between GBA mutations and DLB was found to be higher among male subjects compared to female [80]. These observations were confirmed also in a following study in a cohort of patients with DLB and AJ ancestry [83]. GBA mutation carriers (about 11% of the entire cohort) presented more severe symptoms, particularly in terms of increased hallucinations, worse RBD symptoms, and overall cognitive and motor features [83].
A number of different mutations of the GBA gene have been reported in DLB patients. Other than the two mutations most frequently associated with PD (c.1226A > G (N370S) and c.1448T > C (L444P)), the E326K variant is over-represented in this cohort of patients compared to controls [79,80]. Interestingly, the c.1093G > A (E326K) mutation also is frequently found in patients with PD dementia (PDD) [84].
Neuropathological data does not significantly differ between DLB patients with and without a GBA mutation [79]. However, GBA carriers present a reduced GCase activity as well as a more pronounced alteration of lipid profiles in the brain [85]. GBA expression profiles have been shown to be reduced in DLB and PDD cases in both specific brain regions (temporal cortex and caudate nucleus respectively) and in the peripheral blood [86]. GBA mutations are more significantly associated with Lewy bodies (LB) pathology (especially with a cortical localization) than with Alzheimer’s disease (AD) pathology (i.e., beta-amyloid and neurofibrillary tangles inclusions) [87].
GBA and REM Sleep Behavior Disorders
REM sleep behavior disorders (RBDs) are considered one of the prodromal symptoms of PD and patients affected by this disorder may present with alpha-synuclein accumulation in the brain [88]. According to a recent metanalysis, patients affected with RBDs present an estimated risk of developing a neurodegenerative disorder up to 97% after more than 14 years of follow up [89]. The majority of the cases who present a phenoconversion will develop an alpha-synucleinopathy, represented by PD in the majority of the cases, but also Multiple System Atrophy (MSA), Dementia with Lewy Bodies (DLB), and PD with dementia [90]. In fact, subjects with RBD may present clinical symptoms fulfilling the criteria for prodromal PD in up to 74% of the cases, manifesting worse performances in both motor and non-motor assessments compared to non-affected subjects [91,92]. Notably, many of the studies in this field did not take into consideration the significance of a family history of a neurodegenerative disorder, therefore, it is probable that the percentage of patients that reported a neurodegenerative disease is misrepresented. It would be worth exploring this aspect in future studies.
RBD seems to be more frequent in PD patients with GBA mutations compared with patients without this mutation (OR 3.13) [48,65,67,76]. RBDs are also more frequent in PD patients with concomitant GD than in heterozygous carriers [48]. Based on these observations, a few studies explored the incidence of the GBA mutation among patients affected with RBD [65,91,92,93]. These studies reported that among patients with idiopathic RBDs there is an increased frequency of GBA mutations (2.6–11.6% of RBD patients vs. 0.4–1.8% of the controls) [65,91,93]. A number of different GBA mutations were identified in RBD patients [65,93]. Some of these mutations have already been reported in PD patients, while others still do not have a clear pathogenic role. Among all the reported mutations, the two more commonly found in PD (i.e., c.1226A > G (N370S) and c.1448T > C (L444P), with N370S >> L444P), together with the c.1093G > A (E326K) and the c.1223C > T (T369M), were the most frequently represented in subjects with RBD [65,91,92,93].
Subjects with homozygous GBA mutations, thus affected with GD, and heterozygous carriers with no PD, presented significant worsening of rapid eye movement sleep behavior disorder scores over a period of time of two years compared with non-carrier subjects [92]. Among GBA carriers, the odds ratio (OR) for RBD was 6.24 (95% CI 3.76–10.35, P < 0.0001) [65]. The presence of GBA mutations does not seem to increase the risk among RBD patients of phenoconverting into PD [93]. These observations all together suggest that GBA may play a role in the development of RBDs, but not necessarily in determining more severe phenotypes.
Interestingly, no mutations of the LRRK2 gene, the other common genetic risk factor for PD, have been identified so far in patients with RBDs [91,94].
3. New Targeted Treatments for GBA–PD Patients
Despite the very successful treatments that are now available to address the systemic manifestations of Gaucher’s disease, unfortunately these approaches (i.e., enzyme replacement therapy and substrate reduction therapy) are not able to reach the central nervous system and thus fail to address the neurological symptoms caused by the disease. Different companies have been working for years to try to address this issue, producing very promising results in cellular and animal models. We are now in a very exciting era where some of these experimental approaches are starting to reach the clinical scene. The treatments available so far in clinical trials try to address two main mechanisms that are thought to be detrimental in linking GBA mutations to PD. The first hypothesis is that mutated forms of GBA are not able to fold properly in the endoplasmic reticulum (ER) in the cells, causing the protein to accumulate in this cellular compartment [95]. This would trigger a stress response in the dopaminergic neurons leading to their damage and death [95]. Also, the entrapment of the beta GCase in the ER causes reduced levels of the enzyme in the cells, triggering alpha-synuclein accumulation [95]. In order to target this pathogenic mechanism, different chaperones, which are proteins able to facilitate the refolding of their substrates, were tested [95,96,97,98,99]. In 2016, a clinical study assessing the efficacy of ambroxol, one of these chaperones that showed very exciting preliminary results, was started (NCT02914366 study: https://www.clinicaltrials.gov/ct2/show/NCT02914366?cond=gba+parkinson&rank=7). This is a phase 2 clinical trial to assess the safety and the efficacy of this drug to improve motor and cognitive features of PD patients with a GBA mutation. The study is currently ongoing. Another similar approach has been tested in a phase 1 study by Allergan with LTI-291, a chaperone molecule able to increase the activity of GCase (https://lti-staging.squarespace.com/our-science/#lti-291). Isofagomine is another chaperone protein that has been tested in vitro and in vivo to assess its ability to modulate the phenotype induced by mutations of GBA [97]. This molecule is an inhibitory chaperone whose role would be the stabilization of the GCase. Clinical trials with this molecule are not available at the moment. It is also worth considering that small molecules, such as chaperones, can present different therapeutic profiles in carriers of the different mutations of GBA according to the effect of these variants on the protein [100].
The second mechanism that has been explored to treat GBA–PD patients is the accumulation in the dopaminergic neurons of glucosylceramide (the substrate normally degraded by the GCase) because of the mutation of GBA [101,102,103]. Genzyme recently started a multicenter, randomized, double-blind, placebo-controlled phase 2 study to assess the safety, pharmacokinetics, and pharmacodynamics of an oral compound, ibiglustat (GZ/SAR402671), which is able to reduce the levels of beta-glucocerebrosidase in GBA carriers with early-stage PD (MOVES-PD study: https://www.clinicaltrials.gov/ct2/show/NCT02906020?cond=gba+parkinson&rank=2). It is still a long road for the establishment of an effective treatment, but many paths have been established, giving hope for patients with PD.
Mutated GCase is more unstable compared to the wild-type form. Therefore, modulation of the degradation of GCase could be another suitable strategy to increase the activity of the enzyme and thus tackle alpha-synuclein accumulation and neurodegeneration. Hsp90β, together with other heat shock proteins (HSP), such as Hsp27, parkin, and the endoplasmic reticulum-associated pathway, are responsible for the degradation of misfolded GCase. In particular, histone deacetylase inhibitors (HDACis) and direct inhibitors of specific HSP are able to increase the GCase activity, reducing its degradation [104]. Indeed, HDACis prevent the interaction between Hdp90β and GCase through the hyperactivation of one of its domains [105].
GCase plays an important role in the autophagy-lysosomal pathway (ALP), where other genes that have been associated with PD, such as ATP13A2, scavenger receptor class B member 2 (SCARB2), sphingomyelin phosphodiesterase 1 (SMPD1), and others, are also involved (Moors et al., 2016). Failure of the ALP seems to be responsible for the accumulation of alpha-synuclein in neurons. Therefore, a number of pharmacological approaches directed to the ALP have been attempted in cellular and animal models of PD (for a comprehensive review see [106]). However, the autophagic pathway is broadly represented and active in different cell types and tissues in the organism. Therefore, the identification of approaches with a high selectivity for certain tissues (such as the dopaminergic neurons) or for specific mechanisms within ALP (such as GCase failure) is detrimental for the achievement of effective but also safe treatments for patients.
In order to restore GCase activity, whose failure seems to be responsible for its neuronal pathogenicity, gene therapy approaches are also in the pipeline. Preclinical studies showed that delivery of GBA using adeno-associated virus 1 (AAV1) in A53T–alpha-synuclein mice is able to reduce alpha-synuclein accumulation in the brain [107,108]. The field of gene therapy is now continuously growing in the context of the neurodegenerative disorders [109]. Clinical trials to assess the efficacy of this type of approach may soon be a reality in the context of PD and GBA mutations.
4. Conclusions
The discovery of the association between mutations of the GBA gene and PD allowed important considerations and discoveries that are contributing to a better understating of the pathogenesis of PD. Indeed, after this initial observation, the role of lysosomal impairment has been extensively explored in PD. A growing amount of emerging evidence supports the idea that the endolysosomal trafficking is involved in alpha-synuclein accumulation and dopaminergic neuron degeneration. A number of genes involved in monogenic forms of PD or genetic risk factors for the disease (such as SNCA, ATP13A2, VPS35, DNAJC6, SYNJ1, LRRK2, RAB39B) are part of this pathway (for review see [110]). Mutations of genes involved in the endolysosomal pathways are responsible for a group of disorders designated as Lysosomal Storage Disorders (LSD). These are typically rare autosomal recessive diseases which cause systemic involvements with variable degrees of severity and neurological involvement, usually presenting during childhood (reviewed in [111]). It is interesting to note that an increased burden of LSD-associated mutations has been identified in the screening of large PD populations compared to controls [112]. At the same time, among the 39 new gene loci associated with PD reported in the largest genome wide association study (GWAS) performed in PD patients so far, a number of these variants were found in LSD-associated genes (i.e., NAGLU, GUSB, NEU1, and GRN) [113].
The case of autosomal recessive conditions causing severe and rare disorders during childhood, which in turn present as genetic risk factors for common adult neurodegenerative disorders when in a heterozygous state, appears to be more and more frequent, usually presenting an incomplete penetrance. This is the case for a number of LSD in the context of PD or of a parkinsonian degeneration, such as SMPD1 (sphingomyelin phosphodiesterase, Niemann–Pick disease), ATP13A2 (P5-type ATPase, Kufor–Rakeb disease), GALC (galactosylceramidase, Krabbe disease), NPC1 (Niemann–Pick type C), NAGLU (α-N-acetylglucosminidase, Sanfilippo syndrome B, or mucopoly-saccharidosis III disease B (MPS-IIIB)), HEXB (β-hexosaminidase B, Sandhoff disease (GM2 gangliosidosis)) (summarized in [114]). The association between GBA mutations, GD, and PD must be just the tip of the iceberg of a larger phenomenon, where the association between genes initially considered responsible only for autosomal recessive disorders turned out to be risk factors for common neurodegenerative conditions. This association may have been recognized first in GD patients because of the higher frequency of this disease compared with other LSD.
Interestingly, this is also the case for the TREM2 gene (encoding for Triggering Receptor Expressed on Myeloid cells 2), which seems to be the most frequent genetic risk factor of another common neurodegenerative disorder, Alzheimer’s disease (AD) [115]. Autosomal recessive mutations of TREM2 are responsible for the rare, juvenile condition known as Polycystic lipomembranous osteodysplasia with sclerosing leukoencephalopathy. Of note, TREM2 plays a crucial role in microglia cells as part of the phagocytic scavenger pathway [116].
The phenomena of one gene presenting with different phenotypes is becoming more common in the context of neurological disorders and in respect to common diseases, such as PD and AD. It is important for clinicians to be familiar with these concepts in order to be able to properly counsel their patients and their family members. Also, the identification of such patients will hopefully offer more effective treatments, once available.
These new insights into the understanding of neurodegenerative diseases and, in particular, PD open new scenarios that only a few years ago were still totally obscure. Hopefully, these discoveries will be important for a real discernment of these severe conditions and for the discovery of more effective therapeutic approaches.
Acknowledgments
We sincerely thank Brooklyn Henderson, Registered Nurse for her significant contribution in the editing of the manuscript.
Author Contributions
Conceptualization, G.M.R. and A.B.D.F.; writing—original draft preparation, G.M.R. and A.B.D.F.; writing—review and editing, G.M.R. and A.B.D.F.
Funding
Marlene and Paolo Fresco Institute Clinical Fellowship program; American Parkinson Disease Association.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Goker-Alpan O., Schiffmann R., LaMarca M.E., Nussbaum R.L., McInerney-Leo A., Sidransky E. Parkinsonism among Gaucher disease carriers. J. Med. Genet. 2004;41:937–940. doi: 10.1136/jmg.2004.024455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lwin A., Orvisky E., Goker-Alpan O., LaMarca M.E., Sidransky E. Glucocerebrosidase mutations in subjects with parkinsonism. Mol. Genet. Metab. 2004;81:70–73. doi: 10.1016/j.ymgme.2003.11.004. [DOI] [PubMed] [Google Scholar]
- 3.Eblan M.J., Walker J.M., Sidransky E. The glucocerebrosidase gene and Parkinson’s disease in Ashkenazi Jews. N. Engl. J. Med. 2005;352:728–731. doi: 10.1056/nejm200502173520719. [DOI] [PubMed] [Google Scholar]
- 4.Sidransky E. Heterozygosity for a Mendelian disorder as a risk factor for complex disease. Clin. Genet. 2006;70:275–282. doi: 10.1111/j.1399-0004.2006.00688.x. [DOI] [PubMed] [Google Scholar]
- 5.Poewe W., Seppi K., Tanner C.M., Halliday G.M., Brundin P., Volkmann J., Schrag A.E., Lang A.E. Parkinson disease. Nat. Rev. Dis Primers. 2017;3:17013. doi: 10.1038/nrdp.2017.13. [DOI] [PubMed] [Google Scholar]
- 6.Gegg M.E., Schapira A.H.V. The role of glucocerebrosidase in Parkinson disease pathogenesis. FEBS J. 2018;285:3591–3603. doi: 10.1111/febs.14393. [DOI] [PubMed] [Google Scholar]
- 7.Klein A.D., Mazzulli J.R. Is Parkinson’s disease a lysosomal disorder? Brain. 2018;141:2255–2262. doi: 10.1093/brain/awy147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Blandini F., Cilia R., Cerri S., Pezzoli G., Schapira A.H.V., Mullin S., Lanciego J.L. Glucocerebrosidase mutations and synucleinopathies: Toward a model of precision medicine. Mov. Disord. Off. J. Mov. Disord. Soc. 2019;34:9–21. doi: 10.1002/mds.27583. [DOI] [PubMed] [Google Scholar]
- 9.Chiasserini D., Paciotti S., Eusebi P., Persichetti E., Tasegian A., Kurzawa-Akanbi M., Chinnery P.F., Morris C.M., Calabresi P., Parnetti L., et al. Selective loss of glucocerebrosidase activity in sporadic Parkinson’s disease and dementia with Lewy bodies. Mol. Neurodegener. 2015;10:15. doi: 10.1186/s13024-015-0010-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Parnetti L., Paciotti S., Eusebi P., Dardis A., Zampieri S., Chiasserini D., Tasegian A., Tambasco N., Bembi B., Calabresi P., et al. Cerebrospinal fluid beta-glucocerebrosidase activity is reduced in parkinson’s disease patients. Mov. Disord. Off. J. Mov. Disord. Soc. 2017;32:1423–1431. doi: 10.1002/mds.27136. [DOI] [PubMed] [Google Scholar]
- 11.Wenstrup R.J., Roca-Espiau M., Weinreb N.J., Bembi B. Skeletal aspects of Gaucher disease: A review. Br. J. Radiol. 2002;75(Suppl. 1):A2–A12. doi: 10.1259/bjr.75.suppl_1.750002. [DOI] [PubMed] [Google Scholar]
- 12.Elstein D., Abrahamov A., Dweck A., Hadas-Halpern I., Zimran A. Gaucher disease: Pediatric concerns. Paediatr. Drugs. 2002;4:417–426. doi: 10.2165/00128072-200204070-00001. [DOI] [PubMed] [Google Scholar]
- 13.Andersson H., Kaplan P., Kacena K., Yee J. Eight-year clinical outcomes of long-term enzyme replacement therapy for 884 children with Gaucher disease type 1. Pediatrics. 2008;122:1182–1190. doi: 10.1542/peds.2007-2144. [DOI] [PubMed] [Google Scholar]
- 14.Kauli R., Zaizov R., Lazar L., Pertzelan A., Laron Z., Galatzer A., Phillip M., Yaniv Y., Cohen I.J. Delayed growth and puberty in patients with Gaucher disease type 1: Natural history and effect of splenectomy and/or enzyme replacement therapy. ISR Med. Assoc. J. 2000;2:158–163. [PubMed] [Google Scholar]
- 15.Arends M., van Dussen L., Biegstraaten M., Hollak C.E. Malignancies and monoclonal gammopathy in Gaucher disease; a systematic review of the literature. Br. J. Haematol. 2013;161:832–842. doi: 10.1111/bjh.12335. [DOI] [PubMed] [Google Scholar]
- 16.Zimran A., Elstein D. Gaucher disease and related Lysosomal Storage Diseases. In: Lichtman M.A., Kaushansky K., Prchal J.T., Levi M., Burns L.J., Press O.W., Caligiuri M.A., editors. Williams’ Hematology. Volume 72. McGraw-Hill; New York, NY, USA: 2016. p. 1121. [Google Scholar]
- 17.Gupta P., Pastores G. Pharmacological treatment of pediatric Gaucher disease. Expert Rev. Clin. Pharm. 2018;11:1183–1194. doi: 10.1080/17512433.2018.1549486. [DOI] [PubMed] [Google Scholar]
- 18.Beutler E., Grabowski G. Gaucher disease. In: Beaudet A.L., Scriver C.R., Sly W.S., Valle D., Childs B., Kinzler K.W., Vogelstein B., editors. The Metabolic and Molecular Basis of Inherited Disease. 8th ed. McGraw-Hill International Book Co.; New York, NY, USA: 2001. pp. 3635–3668. [Google Scholar]
- 19.Stirnemann J., Belmatoug N., Camou F., Serratrice C., Froissart R., Caillaud C., Levade T., Astudillo L., Serratrice J., Brassier A., et al. A Review of Gaucher Disease Pathophysiology, Clinical Presentation and Treatments. Int. J. Mol. Sci. 2017;18:441. doi: 10.3390/ijms18020441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pastores G., Hughes D. Gaucher Disease. In: Ardinger H.H., Adam M.P., Pagon R.A., Wallace S.E., Bean L.J.H., Stephens K., Amemiya A., editors. GeneReviews® [Internet] University of Washington; Seattle, WA, USA: 2000. (updated 2018 June 21) [PubMed] [Google Scholar]
- 21.Bennett L.L., Mohan D. Gaucher disease and its treatment options. Ann. Pharm. 2013;47:1182–1193. doi: 10.1177/1060028013500469. [DOI] [PubMed] [Google Scholar]
- 22.Dreborg S., Erikson A., Hagberg B. Gaucher disease—Norrbottnian type. I. General clinical description. Eur. J. Pediatrics. 1980;133:107–118. doi: 10.1007/BF00441578. [DOI] [PubMed] [Google Scholar]
- 23.Smith L., Mullin S., Schapira A.H.V. Insights into the structural biology of Gaucher disease. Exp. Neurol. 2017;298:180–190. doi: 10.1016/j.expneurol.2017.09.010. [DOI] [PubMed] [Google Scholar]
- 24.Hruska K.S., LaMarca M.E., Scott C.R., Sidransky E. Gaucher disease: Mutation and polymorphism spectrum in the glucocerebrosidase gene (GBA) Hum. Mutat. 2008;29:567–583. doi: 10.1002/humu.20676. [DOI] [PubMed] [Google Scholar]
- 25.Grabowski G.A., Horowitz M. Gaucher’s disease: Molecular, genetic and enzymological aspects. Baillieres Clin. Haematol. 1997;10:635–656. doi: 10.1016/S0950-3536(97)80032-7. [DOI] [PubMed] [Google Scholar]
- 26.Goker-Alpan O., Hruska K.S., Orvisky E., Kishnani P.S., Stubblefield B.K., Schiffmann R., Sidransky E. Divergent phenotypes in Gaucher disease implicate the role of modifiers. J. Med. Genet. 2005;42:e37. doi: 10.1136/jmg.2004.028019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cindik N., Ozcay F., Suren D., Akkoyun I., Gokdemir M., Varan B., Alehan F., Ozbek N., Tokel K. Gaucher disease with communicating hydrocephalus and cardiac involvement. Clin. Cardiol. 2010;33:E26–E30. doi: 10.1002/clc.20348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Koprivica V., Stone D.L., Park J.K., Callahan M., Frisch A., Cohen I.J., Tayebi N., Sidransky E. Analysis and classification of 304 mutant alleles in patients with type 1 and type 3 Gaucher disease. Am. J. Hum. Genet. 2000;66:1777–1786. doi: 10.1086/302925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kowarz L., Goker-Alpan O., Banerjee-Basu S., LaMarca M.E., Kinlaw L., Schiffmann R., Baxevanis A.D., Sidransky E. Gaucher mutation N188S is associated with myoclonic epilepsy. Hum. Mutat. 2005;26:271–273. doi: 10.1002/humu.20217. [DOI] [PubMed] [Google Scholar]
- 30.Park J.K., Orvisky E., Tayebi N., Kaneski C., Lamarca M.E., Stubblefield B.K., Martin B.M., Schiffmann R., Sidransky E. Myoclonic epilepsy in Gaucher disease: Genotype-phenotype insights from a rare patient subgroup. Pediatr. Res. 2003;53:387–395. doi: 10.1203/01.PDR.0000049515.79882.94. [DOI] [PubMed] [Google Scholar]
- 31.Duran R., Mencacci N.E., Angeli A.V., Shoai M., Deas E., Houlden H., Mehta A., Hughes D., Cox T.M., Deegan P., et al. The glucocerobrosidase E326K variant predisposes to Parkinson’s disease, but does not cause Gaucher’s disease. Mov. Disord. Off. J. Mov. Disord. Soc. 2013;28:232–236. doi: 10.1002/mds.25248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Park J.K., Tayebi N., Stubblefield B.K., LaMarca M.E., MacKenzie J.J., Stone D.L., Sidransky E. The E326K mutation and Gaucher disease: Mutation or polymorphism? Clin. Genet. 2002;61:32–34. doi: 10.1034/j.1399-0004.2002.610106.x. [DOI] [PubMed] [Google Scholar]
- 33.Horowitz M., Pasmanik-Chor M., Ron I., Kolodny E.H. The enigma of the E326K mutation in acid beta-glucocerebrosidase. Mol. Genet. Metab. 2011;104:35–38. doi: 10.1016/j.ymgme.2011.07.002. [DOI] [PubMed] [Google Scholar]
- 34.Chabas A., Gort L., Diaz-Font A., Montfort M., Santamaria R., Cidras M., Grinberg D., Vilageliu L. Perinatal lethal phenotype with generalized ichthyosis in a type 2 Gaucher disease patient with the [L444P;E326K]/P182L genotype: Effect of the E326K change in neonatal and classic forms of the disease. Blood Cells Mol. Dis. 2005;35:253–258. doi: 10.1016/j.bcmd.2005.04.007. [DOI] [PubMed] [Google Scholar]
- 35.Liou B., Grabowski G.A. Is E326K glucocerebrosidase a polymorphic or pathological variant? Mol. Genet. Metab. 2012;105:528–529. doi: 10.1016/j.ymgme.2011.12.002. [DOI] [PubMed] [Google Scholar]
- 36.Neudorfer O., Giladi N., Elstein D., Abrahamov A., Turezkite T., Aghai E., Reches A., Bembi B., Zimran A. Occurrence of Parkinson’s syndrome in type I Gaucher disease. QJM. 1996;89:691–694. doi: 10.1093/qjmed/89.9.691. [DOI] [PubMed] [Google Scholar]
- 37.Machaczka M., Rucinska M., Skotnicki A.B., Jurczak W. Parkinson’s syndrome preceding clinical manifestation of Gaucher’s disease. Am. J. Hematol. 1999;61:216–217. doi: 10.1002/(SICI)1096-8652(199907)61:3<216::AID-AJH12>3.0.CO;2-B. [DOI] [PubMed] [Google Scholar]
- 38.Perez-Calvo J., Bernal M., Giraldo P., Torralba M.A., Civeira F., Giralt M., Pocovi M. Co-morbidity in Gaucher’s disease results of a nationwide enquiry in Spain. Eur. J. Med. Res. 2000;5:231–235. [PubMed] [Google Scholar]
- 39.Varkonyi J., Simon Z., Soos K., Poros A. Gaucher disease type I complicated with Parkinson’s syndrome. Haematologia. 2002;32:271–275. doi: 10.1163/15685590260461084. [DOI] [PubMed] [Google Scholar]
- 40.Tayebi N., Walker J., Stubblefield B., Orvisky E., LaMarca M.E., Wong K., Rosenbaum H., Schiffmann R., Bembi B., Sidransky E. Gaucher disease with parkinsonian manifestations: Does glucocerebrosidase deficiency contribute to a vulnerability to parkinsonism? Mol. Genet. Metab. 2003;79:104–109. doi: 10.1016/S1096-7192(03)00071-4. [DOI] [PubMed] [Google Scholar]
- 41.Bembi B., Zambito Marsala S., Sidransky E., Ciana G., Carrozzi M., Zorzon M., Martini C., Gioulis M., Pittis M.G., Capus L. Gaucher’s disease with Parkinson’s disease: Clinical and pathological aspects. Neurology. 2003;61:99–101. doi: 10.1212/01.WNL.0000072482.70963.D7. [DOI] [PubMed] [Google Scholar]
- 42.Zhang Y., Shu L., Zhou X., Pan H., Xu Q., Guo J., Tang B., Sun Q. A Meta-Analysis of GBA-Related Clinical Symptoms in Parkinson’s Disease. Parkinsons Dis. 2018;2018:3136415. doi: 10.1155/2018/3136415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Velez-Pardo C., Lorenzo-Betancor O., Jimenez-Del-Rio M., Moreno S., Lopera F., Cornejo-Olivas M., Torres L., Inca-Martinez M., Mazzetti P., Cosentino C., et al. The distribution and risk effect of GBA variants in a large cohort of PD patients from Colombia and Peru. Parkinsonism Relat. Disord. 2019 doi: 10.1016/j.parkreldis.2019.01.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lesage S., Anheim M., Condroyer C., Pollak P., Durif F., Dupuits C., Viallet F., Lohmann E., Corvol J.C., Honore A., et al. Large-scale screening of the Gaucher’s disease-related glucocerebrosidase gene in Europeans with Parkinson’s disease. Hum. Mol. Genet. 2011;20:202–210. doi: 10.1093/hmg/ddq454. [DOI] [PubMed] [Google Scholar]
- 45.Gan-Or Z., Giladi N., Rozovski U., Shifrin C., Rosner S., Gurevich T., Bar-Shira A., Orr-Urtreger A. Genotype-phenotype correlations between GBA mutations and Parkinson disease risk and onset. Neurology. 2008;70:2277–2283. doi: 10.1212/01.wnl.0000304039.11891.29. [DOI] [PubMed] [Google Scholar]
- 46.Cilia R., Tunesi S., Marotta G., Cereda E., Siri C., Tesei S., Zecchinelli A.L., Canesi M., Mariani C.B., Meucci N., et al. Survival and dementia in GBA-associated Parkinson’s disease: The mutation matters. Ann. Neurol. 2016;80:662–673. doi: 10.1002/ana.24777. [DOI] [PubMed] [Google Scholar]
- 47.Liu G., Boot B., Locascio J.J., Jansen I.E., Winder-Rhodes S., Eberly S., Elbaz A., Brice A., Ravina B., van Hilten J.J., et al. Specifically neuropathic Gaucher’s mutations accelerate cognitive decline in Parkinson’s. Ann. Neurol. 2016;80:674–685. doi: 10.1002/ana.24781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Thaler A., Gurevich T., Bar Shira A., Gana Weisz M., Ash E., Shiner T., Orr-Urtreger A., Giladi N., Mirelman A. A “dose” effect of mutations in the GBA gene on Parkinson’s disease phenotype. Parkinsonism Relat. Disord. 2017;36:47–51. doi: 10.1016/j.parkreldis.2016.12.014. [DOI] [PubMed] [Google Scholar]
- 49.Anheim M., Elbaz A., Lesage S., Durr A., Condroyer C., Viallet F., Pollak P., Bonaiti B., Bonaiti-Pellie C., Brice A. Penetrance of Parkinson disease in glucocerebrosidase gene mutation carriers. Neurology. 2012;78:417–420. doi: 10.1212/WNL.0b013e318245f476. [DOI] [PubMed] [Google Scholar]
- 50.Sidransky E., Nalls M.A., Aasly J.O., Aharon-Peretz J., Annesi G., Barbosa E.R., Bar-Shira A., Berg D., Bras J., Brice A., et al. Multicenter analysis of glucocerebrosidase mutations in Parkinson’s disease. N. Engl. J. Med. 2009;361:1651–1661. doi: 10.1056/NEJMoa0901281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bultron G., Kacena K., Pearson D., Boxer M., Yang R., Sathe S., Pastores G., Mistry P.K. The risk of Parkinson’s disease in type 1 Gaucher disease. J. Inherit. Metab. Dis. 2010;33:167–173. doi: 10.1007/s10545-010-9055-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.McNeill A., Duran R., Hughes D.A., Mehta A., Schapira A.H. A clinical and family history study of Parkinson’s disease in heterozygous glucocerebrosidase mutation carriers. J. Neurol. Neurosurg. Psychiatry. 2012;83:853–854. doi: 10.1136/jnnp-2012-302402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.McNeill A., Duran R., Proukakis C., Bras J., Hughes D., Mehta A., Hardy J., Wood N.W., Schapira A.H. Hyposmia and cognitive impairment in Gaucher disease patients and carriers. Mov. Disord. Off. J. Mov. Disord. Soc. 2012;27:526–532. doi: 10.1002/mds.24945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Neumann J., Bras J., Deas E., O’Sullivan S.S., Parkkinen L., Lachmann R.H., Li A., Holton J., Guerreiro R., Paudel R., et al. Glucocerebrosidase mutations in clinical and pathologically proven Parkinson’s disease. Brain. 2009;132:1783–1794. doi: 10.1093/brain/awp044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Moors T., Paciotti S., Chiasserini D., Calabresi P., Parnetti L., Beccari T., van de Berg W.D. Lysosomal Dysfunction and alpha-Synuclein Aggregation in Parkinson’s Disease: Diagnostic Links. Mov. Disord. Off. J. Mov. Disord. Soc. 2016;31:791–801. doi: 10.1002/mds.26562. [DOI] [PubMed] [Google Scholar]
- 56.Mazzulli J.R., Xu Y.H., Sun Y., Knight A.L., McLean P.J., Caldwell G.A., Sidransky E., Grabowski G.A., Krainc D. Gaucher disease glucocerebrosidase and alpha-synuclein form a bidirectional pathogenic loop in synucleinopathies. Cell. 2011;146:37–52. doi: 10.1016/j.cell.2011.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lieberman R.L., Wustman B.A., Huertas P., Powe A.C., Jr., Pine C.W., Khanna R., Schlossmacher M.G., Ringe D., Petsko G.A. Structure of acid beta-glucosidase with pharmacological chaperone provides insight into Gaucher disease. Nat. Chem. Biol. 2007;3:101–107. doi: 10.1038/nchembio850. [DOI] [PubMed] [Google Scholar]
- 58.Yap T.L., Gruschus J.M., Velayati A., Sidransky E., Lee J.C. Saposin C protects glucocerebrosidase against alpha-synuclein inhibition. Biochemistry. 2013;52:7161–7163. doi: 10.1021/bi401191v. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ouled Amar Bencheikh B., Leveille E., Ruskey J.A., Spiegelman D., Liong C., Fon E.A., Rouleau G.A., Dauvilliers Y., Dupre N., Alcalay R.N., et al. Sequencing of the GBA coactivator, Saposin C, in Parkinson disease. Neurobiol. Aging. 2018;72:187.e1–187.e3. doi: 10.1016/j.neurobiolaging.2018.06.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Offman M.N., Krol M., Silman I., Sussman J.L., Futerman A.H. Molecular basis of reduced glucosylceramidase activity in the most common Gaucher disease mutant, N370S. J. Biol. Chem. 2010;285:42105–42114. doi: 10.1074/jbc.M110.172098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wei R.R., Hughes H., Boucher S., Bird J.J., Guziewicz N., Van Patten S.M., Qiu H., Pan C.Q., Edmunds T. X-ray and biochemical analysis of N370S mutant human acid beta-glucosidase. J. Biol. Chem. 2011;286:299–308. doi: 10.1074/jbc.M110.150433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Horowitz M., Wilder S., Horowitz Z., Reiner O., Gelbart T., Beutler E. The human glucocerebrosidase gene and pseudogene: Structure and evolution. Genomics. 1989;4:87–96. doi: 10.1016/0888-7543(89)90319-4. [DOI] [PubMed] [Google Scholar]
- 63.Imai K., Nakamura M., Yamada M., Asano A., Yokoyama S., Tsuji S., Ginns E.I. A novel transcript from a pseudogene for human glucocerebrosidase in non-Gaucher disease cells. Gene. 1993;136:365–368. doi: 10.1016/0378-1119(93)90497-q. [DOI] [PubMed] [Google Scholar]
- 64.Leija-Salazar M., Sedlazeck F.J., Toffoli M., Mullin S., Mokretar K., Athanasopoulou M., Donald A., Sharma R., Hughes D., Schapira A.H.V., et al. Evaluation of the detection of GBA missense mutations and other variants using the Oxford Nanopore MinION. Mol. Genet. Genom. Med. 2019:e564. doi: 10.1002/mgg3.564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Gan-Or Z., Amshalom I., Kilarski L.L., Bar-Shira A., Gana-Weisz M., Mirelman A., Marder K., Bressman S., Giladi N., Orr-Urtreger A. Differential effects of severe vs. mild GBA mutations on Parkinson disease. Neurology. 2015;84:880–887. doi: 10.1212/WNL.0000000000001315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Alcalay R.N., Dinur T., Quinn T., Sakanaka K., Levy O., Waters C., Fahn S., Dorovski T., Chung W.K., Pauciulo M., et al. Comparison of Parkinson risk in Ashkenazi Jewish patients with Gaucher disease and GBA heterozygotes. JAMA Neurol. 2014;71:752–757. doi: 10.1001/jamaneurol.2014.313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Jesus S., Huertas I., Bernal-Bernal I., Bonilla-Toribio M., Caceres-Redondo M.T., Vargas-Gonzalez L., Gomez-Llamas M., Carrillo F., Calderon E., Carballo M., et al. GBA Variants Influence Motor and Non-Motor Features of Parkinson’s Disease. PLoS ONE. 2016;11:e0167749. doi: 10.1371/journal.pone.0167749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Malek N., Weil R.S., Bresner C., Lawton M.A., Grosset K.A., Tan M., Bajaj N., Barker R.A., Burn D.J., Foltynie T., et al. Features of GBA-associated Parkinson’s disease at presentation in the UK Tracking Parkinson’s study. J. Neurol. Neurosurg. Psychiatry. 2018;89:702–709. doi: 10.1136/jnnp-2017-317348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Rosenbloom B., Balwani M., Bronstein J.M., Kolodny E., Sathe S., Gwosdow A.R., Taylor J.S., Cole J.A., Zimran A., Weinreb N.J. The incidence of Parkinsonism in patients with type 1 Gaucher disease: Data from the ICGG Gaucher Registry. Blood Cells Mol. Dis. 2011;46:95–102. doi: 10.1016/j.bcmd.2010.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Lopez G., Kim J., Wiggs E., Cintron D., Groden C., Tayebi N., Mistry P.K., Pastores G.M., Zimran A., Goker-Alpan O., et al. Clinical course and prognosis in patients with Gaucher disease and parkinsonism. Neurol Genet. 2016;2:e57. doi: 10.1212/NXG.0000000000000057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Tan E.K., Tong J., Fook-Chong S., Yih Y., Wong M.C., Pavanni R., Zhao Y. Glucocerebrosidase mutations and risk of Parkinson disease in Chinese patients. Arch. Neurol. 2007;64:1056–1058. doi: 10.1001/archneur.64.7.1056. [DOI] [PubMed] [Google Scholar]
- 72.Eblan M.J., Nguyen J., Ziegler S.G., Lwin A., Hanson M., Gallardo M., Weiser R., De Lucca M., Singleton A., Sidransky E. Glucocerebrosidase mutations are also found in subjects with early-onset parkinsonism from Venezuela. Mov. Disord. Off. J. Mov. Disord. Soc. 2006;21:282–283. doi: 10.1002/mds.20766. [DOI] [PubMed] [Google Scholar]
- 73.Wu Y.R., Chen C.M., Chao C.Y., Ro L.S., Lyu R.K., Chang K.H., Lee-Chen G.J. Glucocerebrosidase gene mutation is a risk factor for early onset of Parkinson disease among Taiwanese. J. Neurol. Neurosurg. Psychiatry. 2007;78:977–979. doi: 10.1136/jnnp.2006.105940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Davis M.Y., Johnson C.O., Leverenz J.B., Weintraub D., Trojanowski J.Q., Chen-Plotkin A., Van Deerlin V.M., Quinn J.F., Chung K.A., Peterson-Hiller A.L., et al. Association of GBA Mutations and the E326K Polymorphism With Motor and Cognitive Progression in Parkinson Disease. JAMA Neurol. 2016;73:1217–1224. doi: 10.1001/jamaneurol.2016.2245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Li Y., Sekine T., Funayama M., Li L., Yoshino H., Nishioka K., Tomiyama H., Hattori N. Clinicogenetic study of GBA mutations in patients with familial Parkinson’s disease. Neurobiol. Aging. 2014;35 doi: 10.1016/j.neurobiolaging.2013.09.019. [DOI] [PubMed] [Google Scholar]
- 76.Brockmann K., Srulijes K., Hauser A.K., Schulte C., Csoti I., Gasser T., Berg D. GBA-associated PD presents with nonmotor characteristics. Neurology. 2011;77:276–280. doi: 10.1212/WNL.0b013e318225ab77. [DOI] [PubMed] [Google Scholar]
- 77.Brockmann K., Srulijes K., Pflederer S., Hauser A.K., Schulte C., Maetzler W., Gasser T., Berg D. GBA-associated Parkinson’s disease: Reduced survival and more rapid progression in a prospective longitudinal study. Mov. Disord. Off. J. Mov. Disord. Soc. 2015;30:407–411. doi: 10.1002/mds.26071. [DOI] [PubMed] [Google Scholar]
- 78.Lythe V., Athauda D., Foley J., Mencacci N.E., Jahanshahi M., Cipolotti L., Hyam J., Zrinzo L., Hariz M., Hardy J., et al. GBA-Associated Parkinson’s Disease: Progression in a Deep Brain Stimulation Cohort. J. Parkinsons Dis. 2017;7:635–644. doi: 10.3233/JPD-171172. [DOI] [PubMed] [Google Scholar]
- 79.Nalls M.A., Duran R., Lopez G., Kurzawa-Akanbi M., McKeith I.G., Chinnery P.F., Morris C.M., Theuns J., Crosiers D., Cras P., et al. A multicenter study of glucocerebrosidase mutations in dementia with Lewy bodies. JAMA Neurol. 2013;70:727–735. doi: 10.1001/jamaneurol.2013.1925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Gamez-Valero A., Prada-Dacasa P., Santos C., Adame-Castillo C., Campdelacreu J., Rene R., Gascon-Bayarri J., Ispierto L., Alvarez R., Ariza A., et al. GBA Mutations Are Associated With Earlier Onset and Male Sex in Dementia With Lewy Bodies. Mov. Disord. Off. J. Mov. Disord. Soc. 2016;31:1066–1070. doi: 10.1002/mds.26593. [DOI] [PubMed] [Google Scholar]
- 81.Guerreiro R., Ross O.A., Kun-Rodrigues C., Hernandez D.G., Orme T., Eicher J.D., Shepherd C.E., Parkkinen L., Darwent L., Heckman M.G., et al. Investigating the genetic architecture of dementia with Lewy bodies: A two-stage genome-wide association study. Lancet Neurol. 2018;17:64–74. doi: 10.1016/S1474-4422(17)30400-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Asselta R., Rimoldi V., Siri C., Cilia R., Guella I., Tesei S., Solda G., Pezzoli G., Duga S., Goldwurm S. Glucocerebrosidase mutations in primary parkinsonism. Parkinsonism Relat. Disord. 2014;20:1215–1220. doi: 10.1016/j.parkreldis.2014.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Shiner T., Mirelman A., Gana Weisz M., Bar-Shira A., Ash E., Cialic R., Nevler N., Gurevich T., Bregman N., Orr-Urtreger A., et al. High Frequency of GBA Gene Mutations in Dementia With Lewy Bodies Among Ashkenazi Jews. JAMA Neurol. 2016;73:1448–1453. doi: 10.1001/jamaneurol.2016.1593. [DOI] [PubMed] [Google Scholar]
- 84.Mata I.F., Leverenz J.B., Weintraub D., Trojanowski J.Q., Chen-Plotkin A., Van Deerlin V.M., Ritz B., Rausch R., Factor S.A., Wood-Siverio C., et al. GBA Variants are associated with a distinct pattern of cognitive deficits in Parkinson’s disease. Mov. Disord. Off. J. Mov. Disord. Soc. 2016;31:95–102. doi: 10.1002/mds.26359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Clark L.N., Chan R., Cheng R., Liu X., Park N., Parmalee N., Kisselev S., Cortes E., Torres P.A., Pastores G.M., et al. Gene-wise association of variants in four lysosomal storage disorder genes in neuropathologically confirmed Lewy body disease. PLoS ONE. 2015;10:e0125204. doi: 10.1371/journal.pone.0125204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Perez-Roca L., Adame-Castillo C., Campdelacreu J., Ispierto L., Vilas D., Rene R., Alvarez R., Gascon-Bayarri J., Serrano-Munoz M.A., Ariza A., et al. Glucocerebrosidase mRNA is Diminished in Brain of Lewy Body Diseases and Changes with Disease Progression in Blood. Aging Dis. 2018;9:208–219. doi: 10.14336/AD.2017.0505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Clark L.N., Kartsaklis L.A., Wolf Gilbert R., Dorado B., Ross B.M., Kisselev S., Verbitsky M., Mejia-Santana H., Cote L.J., Andrews H., et al. Association of glucocerebrosidase mutations with dementia with lewy bodies. Arch. Neurol. 2009;66:578–583. doi: 10.1001/archneurol.2009.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Boeve B.F., Silber M.H., Ferman T.J., Lin S.C., Benarroch E.E., Schmeichel A.M., Ahlskog J.E., Caselli R.J., Jacobson S., Sabbagh M., et al. Clinicopathologic correlations in 172 cases of rapid eye movement sleep behavior disorder with or without a coexisting neurologic disorder. Sleep Med. 2013;14:754–762. doi: 10.1016/j.sleep.2012.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Galbiati A., Verga L., Giora E., Zucconi M., Ferini-Strambi L. The risk of neurodegeneration in REM sleep behavior disorder: A systematic review and meta-analysis of longitudinal studies. Sleep Med. Rev. 2019;43:37–46. doi: 10.1016/j.smrv.2018.09.008. [DOI] [PubMed] [Google Scholar]
- 90.Ferini-Strambi L., Marelli S., Galbiati A., Rinaldi F., Giora E. REM Sleep Behavior Disorder (RBD) as a marker of neurodegenerative disorders. Arch. Ital. Biol. 2014;152:129–146. doi: 10.12871/000298292014238. [DOI] [PubMed] [Google Scholar]
- 91.Barber T.R., Lawton M., Rolinski M., Evetts S., Baig F., Ruffmann C., Gornall A., Klein J.C., Lo C., Dennis G., et al. Prodromal Parkinsonism and Neurodegenerative Risk Stratification in REM Sleep Behavior Disorder. Sleep. 2017;40 doi: 10.1093/sleep/zsx071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Beavan M., McNeill A., Proukakis C., Hughes D.A., Mehta A., Schapira A.H. Evolution of prodromal clinical markers of Parkinson disease in a GBA mutation-positive cohort. JAMA Neurol. 2015;72:201–208. doi: 10.1001/jamaneurol.2014.2950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Gamez-Valero A., Iranzo A., Serradell M., Vilas D., Santamaria J., Gaig C., Alvarez R., Ariza A., Tolosa E., Beyer K. Glucocerebrosidase gene variants are accumulated in idiopathic REM sleep behavior disorder. Parkinsonism Relat. Disord. 2018;50:94–98. doi: 10.1016/j.parkreldis.2018.02.034. [DOI] [PubMed] [Google Scholar]
- 94.Fernandez-Santiago R., Iranzo A., Gaig C., Serradell M., Fernandez M., Tolosa E., Santamaria J., Ezquerra M. Absence of LRRK2 mutations in a cohort of patients with idiopathic REM sleep behavior disorder. Neurology. 2016;86:1072–1073. doi: 10.1212/WNL.0000000000002304. [DOI] [PubMed] [Google Scholar]
- 95.McNeill A., Magalhaes J., Shen C., Chau K.Y., Hughes D., Mehta A., Foltynie T., Cooper J.M., Abramov A.Y., Gegg M., et al. Ambroxol improves lysosomal biochemistry in glucocerebrosidase mutation-linked Parkinson disease cells. Brain. 2014;137:1481–1495. doi: 10.1093/brain/awu020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Ambrosi G., Ghezzi C., Zangaglia R., Levandis G., Pacchetti C., Blandini F. Ambroxol-induced rescue of defective glucocerebrosidase is associated with increased LIMP-2 and saposin C levels in GBA1 mutant Parkinson’s disease cells. Neurobiol. Dis. 2015;82:235–242. doi: 10.1016/j.nbd.2015.06.008. [DOI] [PubMed] [Google Scholar]
- 97.Sanchez-Martinez A., Beavan M., Gegg M.E., Chau K.Y., Whitworth A.J., Schapira A.H. Parkinson disease-linked GBA mutation effects reversed by molecular chaperones in human cell and fly models. Sci. Rep. 2016;6:31380. doi: 10.1038/srep31380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Migdalska-Richards A., Daly L., Bezard E., Schapira A.H. Ambroxol effects in glucocerebrosidase and alpha-synuclein transgenic mice. Ann. Neurol. 2016;80:766–775. doi: 10.1002/ana.24790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Migdalska-Richards A., Ko W.K.D., Li Q., Bezard E., Schapira A.H.V. Oral ambroxol increases brain glucocerebrosidase activity in a nonhuman primate. Synapse. 2017;71 doi: 10.1002/syn.21967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Barkhuizen M., Anderson D.G., Grobler A.F. Advances in GBA-associated Parkinson’s disease--Pathology, presentation and therapies. Neurochem. Int. 2016;93:6–25. doi: 10.1016/j.neuint.2015.12.004. [DOI] [PubMed] [Google Scholar]
- 101.Fernandes H.J., Hartfield E.M., Christian H.C., Emmanoulidou E., Zheng Y., Booth H., Bogetofte H., Lang C., Ryan B.J., Sardi S.P., et al. ER Stress and Autophagic Perturbations Lead to Elevated Extracellular alpha-Synuclein in GBA-N370S Parkinson’s iPSC-Derived Dopamine Neurons. Stem Cell Rep. 2016;6:342–356. doi: 10.1016/j.stemcr.2016.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Bae E.J., Yang N.Y., Song M., Lee C.S., Lee J.S., Jung B.C., Lee H.J., Kim S., Masliah E., Sardi S.P., et al. Glucocerebrosidase depletion enhances cell-to-cell transmission of alpha-synuclein. Nat. Commun. 2014;5:4755. doi: 10.1038/ncomms5755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Sardi S.P., Clarke J., Kinnecom C., Tamsett T.J., Li L., Stanek L.M., Passini M.A., Grabowski G.A., Schlossmacher M.G., Sidman R.L., et al. CNS expression of glucocerebrosidase corrects alpha-synuclein pathology and memory in a mouse model of Gaucher-related synucleinopathy. Proc. Natl. Acad. Sci. USA. 2011;108:12101–12106. doi: 10.1073/pnas.1108197108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Yang C., Swallows C.L., Zhang C., Lu J., Xiao H., Brady R.O., Zhuang Z. Celastrol increases glucocerebrosidase activity in Gaucher disease by modulating molecular chaperones. Proc. Natl. Acad. Sci. USA. 2014;111:249–254. doi: 10.1073/pnas.1321341111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Yang C., Rahimpour S., Lu J., Pacak K., Ikejiri B., Brady R.O., Zhuang Z. Histone deacetylase inhibitors increase glucocerebrosidase activity in Gaucher disease by modulation of molecular chaperones. Proc. Natl. Acad. Sci. USA. 2013;110:966–971. doi: 10.1073/pnas.1221046110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Moors T.E., Hoozemans J.J., Ingrassia A., Beccari T., Parnetti L., Chartier-Harlin M.C., van de Berg W.D. Therapeutic potential of autophagy-enhancing agents in Parkinson’s disease. Mol. Neurodegener. 2017;12:11. doi: 10.1186/s13024-017-0154-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Sardi S.P., Clarke J., Viel C., Chan M., Tamsett T.J., Treleaven C.M., Bu J., Sweet L., Passini M.A., Dodge J.C., et al. Augmenting CNS glucocerebrosidase activity as a therapeutic strategy for parkinsonism and other Gaucher-related synucleinopathies. Proc. Natl. Acad. Sci. USA. 2013;110:3537–3542. doi: 10.1073/pnas.1220464110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Rocha E.M., Smith G.A., Park E., Cao H., Brown E., Hayes M.A., Beagan J., McLean J.R., Izen S.C., Perez-Torres E., et al. Glucocerebrosidase gene therapy prevents alpha-synucleinopathy of midbrain dopamine neurons. Neurobiol. Dis. 2015;82:495–503. doi: 10.1016/j.nbd.2015.09.009. [DOI] [PubMed] [Google Scholar]
- 109.Sudhakar V., Richardson R.M. Gene Therapy for Neurodegenerative Diseases. Neurother. J. Am. Soc. Exp. Neurother. 2019;16:166–175. doi: 10.1007/s13311-018-00694-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Abeliovich A., Gitler A.D. Defects in trafficking bridge Parkinson’s disease pathology and genetics. Nature. 2016;539:207–216. doi: 10.1038/nature20414. [DOI] [PubMed] [Google Scholar]
- 111.Sun A. Lysosomal storage disease overview. Ann. Transl. Med. 2018;6:476. doi: 10.21037/atm.2018.11.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Robak L.A., Jansen I.E., van Rooij J., Uitterlinden A.G., Kraaij R., Jankovic J., Heutink P., Shulman J.M. Excessive burden of lysosomal storage disorder gene variants in Parkinson’s disease. Brain. 2017;140:3191–3203. doi: 10.1093/brain/awx285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Nalls M.A., Blauwendraat C., Vallerga C.L., Heilbron K., Bandres-Ciga S., Chang D., Tan M., Kia D.A., Noyce A.J., Xue A., et al. Parkinson’s disease genetics: Identifying novel risk loci, providing causal insights and improving estimates of heritable risk. BioRxiv. 2018 doi: 10.1101/388165. [DOI] [Google Scholar]
- 114.Ysselstein D., Shulman J.M., Krainc D. Emerging links between pediatric lysosomal storage diseases and adult parkinsonism. Mov. Disord. Off. J. Mov. Disord. Soc. 2019 doi: 10.1002/mds.27631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Jonsson T., Stefansson H., Steinberg S., Jonsdottir I., Jonsson P.V., Snaedal J., Bjornsson S., Huttenlocher J., Levey A.I., Lah J.J., et al. Variant of TREM2 associated with the risk of Alzheimer’s disease. N. Engl. J. Med. 2013;368:107–116. doi: 10.1056/NEJMoa1211103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Carmona S., Zahs K., Wu E., Dakin K., Bras J., Guerreiro R. The role of TREM2 in Alzheimer’s disease and other neurodegenerative disorders. Lancet Neurol. 2018;17:721–730. doi: 10.1016/S1474-4422(18)30232-1. [DOI] [PubMed] [Google Scholar]