Abstract
Background and Objectives
Persons with dementia (PWDs) often place greater importance on their care values (i.e., maintaining autonomy and social relations, choosing caregivers, avoiding being a burden) than family caregivers (CGs) perceive, which can detract from dementia care planning (e.g., care arrangements or surrogate decisions). Notable variability has been found across family care dyads (PWD and CG) in their perceptions of care values, suggesting that there may be multiple patterns of perception. The purpose of this study was to characterize distinct patterns of perception of care values in family care dyads.
Design and Methods
Using cross-sectional data from 228 community-dwelling family care dyads, we quantified dyads’ average perceptions and incongruence in perceptions of the importance of everyday care values using multilevel modeling. These scores were then used in a latent class analysis to identify distinct patterns of perception, with the dyad as the unit of analysis.
Results
Two distinct patterns of care value perception were identified. 25% of dyads were labeled as “CG underestimating” due to lower average estimations of the importance of PWDs’ care values, and a significant amount of dyadic incongruence. Underestimating dyads were characterized by a confirmed diagnosis of dementia, lower cognitive function, and younger age in PWDs, and higher relationship strain in the dyad.
Implications
Care dyads that fall into an underestimating pattern may be at greater risk for inadequate dementia care planning. Interventions to improve care planning in this higher-risk group may include care values identification with the PWD, strategies for alleviating relationship strain, early-stage planning, and disease education.
Keywords: Caregiving – Informal, Dementia, Family issues, Care Values, dyadic analysis
The process of care planning reflects a culmination of, and often a tension between, an individual’s values and resources. In the context of dementia, family caregivers (CGs) are both a critical resource for supportive care of the person with dementia (PWD), and often the main spokesperson for representing and honoring the PWD’s care values. Family CGs (typically adult children or spouses/partners) provide most of the supportive care to PWDs in the United States (National Alliance for Caregiving, 2017). Family CGs are also instrumental in helping make care decisions that are based upon the PWD’s values, such as the value of autonomy (Whitlatch, Feinberg, & Tucke, 2005b). These dual roles make CGs essential to the dementia care-planning process. For decades, researchers have examined the many facets of CGs’ experiences of providing regular supportive care to PWDs. Equally challenging is the other role of a dementia CG: knowing the PWD’s care values (i.e., the importance of autonomy, avoiding being a burden, who helps out with care, social activities, and safety) and making decisions in accordance with those values. This study addresses perceptions within family care dyads (PWD and CG) regarding the importance of care values to the PWD, with the goal of informing future research, theory, and practice regarding the dementia care planning process.
It is important for CGs to know the PWD’s care values in order to be active participants in dementia care planning, and eventually to make effective surrogate decisions. Decisions reflect values, since we arrive at a decision by actively supporting a value through choice (Koppelman, 2002). In early to mid-stage dementia, PWDs can reliably report on their own care values and preferences (Carpenter, Kissel, & Lee, 2007; Feinberg & Whitlatch, 2001; Whitlatch, Feinberg, & Tucke, 2005a). Yet, even early in the disease process, CGs often take a more dominant role in decision making on the PWD’s behalf (Karlawish, Casarett, Propert, James, & Clark, 2002; Samsi & Manthorpe, 2013; Smebye, Kirkevold, & Engedal, 2012). In order for CGs to be effective as surrogate decision makers–especially if they are to follow the recommended substituted judgement standard (making a decision based upon what the patient would choose)—they need adequate knowledge of the PWD’s care values (Hirschman, Kapo, & Karlawish, 2006). Formal documentation of specific care values, such as those found in advanced directives, is useful for physicians who must make treatment decisions, but broader knowledge of the importance of care values to the PWD is necessary for CGs, who must make decisions about a wider range of everyday issues (Elliott, Gessert, & Peden-McAlpine, 2009; Hirschman et al., 2006; Jox et al., 2012; Robins-Browne, Hegarty, Guillmen, Komesaroff, & Palmer, 2017).
Despite the centrality of CGs to PWDs’ lives and the importance of knowing PWDs’ care values, there is evidence from dyadic studies that many CGs have perceptions of the PWD’s care values and preferences that are incongruent with PWDs’ perceptions (Carpenter et al., 2007; Heid, Bangerter, Abbott, & Van Haitsma, 2017; Miller, Whitlatch, Lee, & Lyons, 2017; Reamy, Kim, Zarit, & Whitlatch, 2011). One study found that CGs perceive a decline in the importance of care values to the PWD over time (Reamy, Kim, Zarit, & Whitlatch, 2013), but according to the PWD in other studies, values and preferences remain fairly stable over time (Carpenter et al., 2007; Feinberg & Whitlatch, 2001). There is also consistency across studies in the direction of incongruence in perceptions of care values (CGs’ underestimating the importance to the PWD), which suggests that incongruence is a product of the family member’s negative appraisals, and not just the result of poor communication or a lack of awareness (Heid et al., 2017; Miller et al., 2017; Reamy et al., 2011).
Previous studies examining perceptions of PWDs’ care values have noted significant variability across family care dyads in the amount of incongruence (Carpenter et al., 2007; Miller et al., 2017; Reamy et al., 2011), indicating that some CGs share appraisals of care values with PWDs (i.e., limited incongruence) while others underestimate the importance of care values to the PWD (i.e., significant incongruence). Lower magnitudes of incongruence have been predicted in previous studies (albeit cross-sectional) when dyads were African American (Reamy et al., 2011; Schmid, Allen, Haley, & Decoster, 2010), had lower levels of cognitive impairment among PWDs (Buckley et al., 2012; Reamy et al., 2011), less care-related strain among CGs, and lower levels of relationship strain in the dyad (Lyons, Zarit, Sayer, & Whitlatch, 2002; Sands, Ferreira, Stewart, Brod, & Yaffe, 2004). There is also some evidence that when CGs share more similar appraisals of the PWD’s care values with the PWD, both CGs and PWDs have better quality of life (Moon, Townsend, Whitlatch, & Dilworth-Anderson, 2016).
Distinguishing which dyads belong to a pattern of perception that is at higher risk for poor care planning outcomes could help to target at-risk dyads and tailor care planning interventions to their needs. There are a number of stressors and strains upon CGs that likely impact their perceptions of the PWD’s care values. The stress process model (Pearlin, Mullan, Semple, & Skaff, 1990) (SPM) provided a theoretical framework for this study, as well as the original research from which the data for this study were derived. According to the SPM, under certain conditions, the provision of support or assistance to a family member (i.e., caregiving) becomes the dominant and overly stressful dimension of a relationship that was once multi-dimensional and reciprocal. The prolonged and progressive impairment associated with dementia is one such circumstance. The direct effects of dementia (e.g., cognitive impairment, dependence on others) are known as primary stressors in the SPM. A dynamic process involving secondary stressors and strains—manifesting in the dyad’s relationship as much as it does within the CG’s psyche—unfolds from there (Aneshensel, Pearlin, Mullan, Zarit, & Whitlatch, 1995). The extent and nature of the impact of the stress process on CGs is highly variable, with both positive and negative impacts on the care dyad’s relationship (Pinquart & Sorensen, 2003), which can lead to a variety of outcomes, including incongruence in the family care dyad (Miller et al., 2017).
Given the importance of the CG’s understanding of the PWD’s care values for care planning, and the relatedness of incongruence to the dyad’s relationship quality and individual well-being, the ability to characterize a more incongruent sub-group of family care dyads, and distinguish dyads that are at higher risk for belonging to it, would help focus efforts around improving dementia care planning in clinical settings. Several qualitative studies have identified typologies or archetypes in family care dyads, which helps organize and advance the science of dementia care both theoretically and clinically (Bangerter, Griffin, Zarit, & Havyer, 2017; Clemmensen, Busted, Soborg, & Bruun, 2016; Esandi, Nolan, Alfaro, & Canga-Armayor, 2017). The purpose of this study was to characterize distinct patterns (i.e. sub-groups) of perception among family care dyads regarding the importance of care values to the PWD, and to identify factors that differentiate which dyads belonged to each pattern. Our hypotheses were as follows:
1. There would be at least two patterns of perception among PWD-CG dyads, with one pattern characterized by greater levels of incongruence in perceptions of the PWD’s care values and lower dyadic averages for rating of the importance of care values to the PWD.
2. Predictors of patterns of perception in PWD-CG dyads would include contextual factors (e.g., type of kin relationship), objective stressors (e.g., level of cognitive impairment in the PWD) and subjective stressors (e.g., dyadic relationship strain) from the SPM.
Design and Methods
This study is a secondary analysis of cross-sectional baseline data from three dyadic care planning trials, each of which have been described in detail elsewhere: “Early Diagnosis Dyadic Intervention” (EDDI: n = 49 dyads) (Whitlatch, Judge, Zarit, & Femia, 2006); “Enhancing Cognitive Health Outcomes” (ECHO: n = 50 dyads) (Orsulic-Jeras, Whitlatch, Szabo, Shelton, & Johnson, 2016); and “Support, Health, Activities, Resources, and Education” (SHARE: n = 128 dyads) (Whitlatch et al., 2017). Data were merged for a combined sample of 228 dyads.
Inclusion Criteria
Dyads were eligible for participation if both dyad members were living in the community setting and had a close kin-type relationship with each other (i.e., spouses/partners, adult child (or child-in-law)-parent dyads). CGs needed to have assumed primary responsibility for providing day-to-day assistance or care to the PWD. Additional criteria for inclusion of PWDs were age 50 years or older (ECHO), age 55 years of age or older (SHARE), a confirmed diagnosis of or symptoms consistent with an early-stage dementia, and scores on the Mini-mental State Exam (MMSE) between 23 and 26 for ECHO; 20 and 26 for SHARE; and for EDDI scores between 16 and 24, or if higher, a confirmed diagnosis of dementia or mild cognitive impairment.
Exclusion Criteria
Dyads were not eligible for participation if non-English speaking, or if either dyad member had a severe untreated mental health diagnosis (e.g. bipolar or depression).
Ethical Approval
The primary study approvals for the three trials were obtained from the IRBs of Benjamin Rose Institute on Aging (EDDI, ECHO, and SHARE), Pennsylvania State University (EDDI), and University Hospitals Cleveland (ECHO). Informed consent was obtained from all participants for the original studies. Approval for the current secondary analysis of de-identified data was obtained by the IRB of the University of Utah after being determined as exempt for human subjects review.
Outcome Measures
Care Values were measured among PWDs and CGs using the Care Values Scale (Orsulic-Jeras et al., 2016; Whitlatch, Piiparinen, & Feinberg, 2009), which asks participants to rate their perceptions of how important 24 different values for everyday care are to the PWD. The measure consists of five subscales, scored on a three-point scale from 1 (not important), to 3 (very important). The subscales used in this study included the value of autonomy (five items: PWD α = 0.71; CG α = 0.71), the value of avoiding being a burden (five items: PWD α = 0.72; CG α = 0.82), the value of who helps out with care (four items: PWD α = 0.63; CG α = 0.65), and the value of social activities (five items: PWD α = 0.69; CG α = 0.75). The subscale for the value of safety (five items) was not used in this analysis due to changes to the items between studies that resulted in missing data on over half the merged sample. Missing data on all other subscales were less than 5% and handled using full information maximum likelihood during dyadic data analysis.
Independent Variables
A survey of background characteristics of the dyad was designed by the researchers of the original studies and administered over the course of screening and baseline interviews with PWDs and CGs. The characteristics that were available across all three original studies, and used in the current study, were: age, race/ethnicity, education level, kinship type of dyad (spouse dyads or non-spouse dyads), income level, employment status of the CG (paid employment yes/no), marital status, and dementia diagnosis (yes/no).
Cognitive status of PWDs was measured using the original version of the Mini-Mental State Examination (MMSE) (Folstein, Folstein, & McHugh, 1975). The MMSE assesses 11 cognitive domains (30 items) including aspects of orientation, working memory, language, delayed recall, attention, and comprehension. The scale range is 0–30, with higher scores indicating higher cognitive function. It is used widely in research, has good reliability and diagnostic accuracy in the community setting (Mitchell, 2009).
Relationship strain in the dyad was measured using the five-item Dyadic Strain subscale of the Dyadic Relationship Scale (Sebern & Whitlatch, 2007). Each item is a statement of a potential source of strain in the dyad’s relationship, for which CGs rated their level of agreement from 1 (strongly disagree) to 4 (strongly agree). An example item is: “Because of helping my family member, I felt resentful toward her/him.” Items were averaged for a scale range of 1 to 4, with higher scores indicating more perceived relationship strain. The reliability in this sample was strong (α = 0.89).
Positive interactions in the dyad were measured using the Positive Dyadic Interactions subscale of the Dyadic Relationship Scale (Sebern & Whitlatch, 2007). Each item is a statement of a potential source of positive interaction in the dyad’s relationship, for which CGs rated their level of agreement from 1 (strongly disagree) to 4 (strongly agree). An example item is “Because of helping my family member, I felt closer to him/her than I have in awhile.” Items were averaged for a scale range of 1–4, with higher scores indicating more perceived positive interactions. The reliability in this sample was good (α = 0.87).
Analytic Approach
Multilevel Modeling
Analysis of the dyadic data was conducted using multilevel modeling (MLM) and the software program HLM, version 7 (Raudenbush, Bryk, & Congdon, 2011). The procedures for applying the univariate-outcomes model for dyads, and the advantages of this analytic approach for modeling dyadic incongruence, have been described in detail previously, including in a previous study of dyadic incongruence using the Care Values Scale (Miller et al., 2017; Sayer & Klute, 2005). Four separate MLM analyses were conducted, one for each of the four care values subscales (autonomy, avoiding burden, choosing who helps with care, and maintaining social relations), as indicated in the following equation:
Care value Y is estimated through fixed effects (empirical Bayes estimates), including the intercept (β0j), which is the dyadic average, and the slope (β1j), which represents the average magnitude and direction of incongruence in perceptions for the given care value. Measurement error is also estimated (r). By coding PWDs’ scores as −0.5 and CGs’ scores as 0.5 in Dyadij, the direction of incongruence can be interpreted from the slope (β1j). If the importance of the PWD’s value is underestimated on average by CGs, the resulting β1 coefficient will be negative.
Each MLM analysis resulted in two outcome variables: the dyadic average (the intercept), and the dyadic incongruence (the slope, representing both the direction and magnitude of the difference between the PWD’s and CG’s perceptions). Thus, this phase of analysis resulted in eight variables (empirical Bayes estimates of four incongruence slopes, and four dyadic averages) characterizing dyads’ perceptions of the importance of care values to the PWD.
Latent Class Mixture Modeling
We sought to further characterize care values by identifying distinct patterns of perceptions using latent class mixture modeling and the software program Mplus v 7.11 (Los Angeles, CA). After extracting scores (empirical Bayes estimates) from the dyadic analyses described above, we included dyadic incongruence and the dyadic average for perceptions of care values as indicator variables in a latent class mixture model. The integration of dyadic/family-level analysis with robust clustering techniques has been previously performed in a latent class mixture modeling analysis of data form heart failure patients and their CGs regarding heart failure self-care (Lee et al., 2017), and in a latent profile analysis of data from parents of multiple adult children regarding family support (Kim, Fingerman, Birditt, & Zarit, 2016). One advantage of performing this additional analysis is the ability to examine heterogeneous data for underlying subgroups that fit into distinct patterns. If more than one pattern is observed, then subgroups who belong to those patterns can be described and interventions tailored to their unique characteristics and needs.
Our selection of the most appropriate model was guided by the following indicators of model performance and fit: model convergence (entropy near 1.0), the size of the observed patterns (pattern sizes over 5% of sample), average posterior probabilities for most likely pattern near 1.0, a significant (p < .05) Vuong–Lo–Mendell–Rubin adjusted likelihood ratio test, the Parametric Bootstrap Likelihood Ratio Test (p-value NS), and by comparing the sample-size adjusted Bayesian Information Criterion between models.
After determining the most appropriate number of observed patterns, we differentiated patterns and also distinguished between dyads that were more likely to belong to each pattern of perception of care values using Stata, version 15 (Statacorp, 2017). We compared observed patterns using t-tests and χ2, and calculated effect sizes for comparisons using Cohen’s d. Multivariate logistic regression analyses were conducted to identify factors associated with the incongruent pattern. Covariates for the logistic regression were selected based upon the SPM, but were limited to those variables that were measured across all three datasets.
Results
Participants with dementia were, on average, 74 ± 9 years of age, of predominantly non-Hispanic white ethnicity/race (81%), had an average MMSE score of 24 ± 3, and a slight majority (54%) were female. Family CG participants were, on average, 65 ± 13 years of age, of predominantly non-Hispanic white ethnicity/race (82%), majority female (73%), and most were spouses/partners (65%), or adult children/children-in-law (24%) of the participants with dementia. See Table 1 for additional sample characteristics.
Table 1.
Overall Sample Characteristics (N = 228 Dyads)
| PWD mean ± SD or % | CG mean (SD) or % | |
|---|---|---|
| Age in yearsa | 74.32 ± 9.06 | 64.93 ± 12.85 |
| Gender (% female) | 53.5% | 73.3% |
| Education (>high school diploma) | 63.4% | 76.2% |
| Employment (% paid, part-time or more) | — | 49.6% |
| Race/ethnicity | ||
| White (Non-Hispanic) | 80% | 82% |
| Black/African-American | 17.0% | 17.0% |
| Native American/Pacific Islander | 0.5% | 0% |
| Asian | 1.0% | 0.5% |
| Hispanic/Latino | 1.0% | 1.0% |
| Marital status (married/partnered) | 70.0% | 80.0% |
| Relationship to PWD | ||
| Wife | — | 40.4% |
| Husband | — | 24.6% |
| Daughter/daughter-in-law | — | 21.5% |
| Son/son-in-law | — | 3.0% |
| Other relative | — | 8.5% |
| Non-relative | — | 2.0% |
| Cognitive function (MMSE, range 12–27) | 24.40 ± 3.48 | — |
| Relationship strain (scale 1–4) | 1.78 ± 0.60 | 1.83 ± 0.60 |
| Positive dyadic interactions (scale 1–4) | 2.88 ± 0.59 | 2.85 ± 0.60 |
CG = family caregiver; MMSE = Mini-mental state examination; PWD = person with dementia.
aAges 90 years or older were all recorded as 90 to protect identity.
MLM Results
Overall in this sample of 228 family care dyads, there was a significant amount of incongruence for perceptions of the importance to the PWD of avoiding being a burden (β = −0.15, p < .001), who helps with care (β = −0.15, p < .001), and engaging in social activities (β = −0.11, p < .001), but not a significant amount of incongruence for the importance to the PWD of the value of maintaining autonomy (β = −0.01, p = .613). The direction of incongruence was such that the CG perceived the PWD’s care value as being less important than the PWD rated the care value. The tau correlations (from HLM) between PWD and CG ratings of the PWD’s values were small to moderate: maintaining autonomy τ = 0.38; avoiding burden τ = 0.24; help with care τ = 0.11; social activities τ = 0.49. There was a significant amount of variability around the average dyadic incongruence scores on all four of the care values subscales, and a significant amount of variability around all average dyadic perceptions of the importance of care values. Thus, the MLM analysis confirmed that the data were heterogeneous and could potentially be better understood though examining whether subgroups of dyads belonged to distinct patterns of perception of care values.
Latent Class Mixture Modeling Results
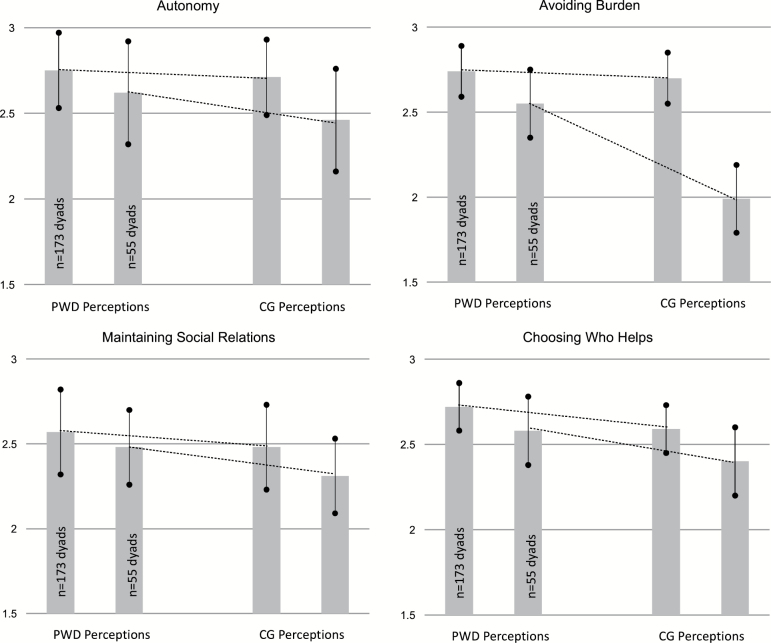
Two distinct patterns of perception of care values were identified (Vuong–Lo–Mendell–Rubin adjusted likelihood ratio test = 194.82, p = .012; entropy = 0.86; posterior probabilities > 0.90). Table 2 reports how the two patterns differ by indicator variables, which is also depicted in Figure 1. 25% of dyads were observed as belonging to the “CG underestimating” group due to: (a) significantly lower average perceptions from dyads regarding the importance of PWDs’ care values; (b) significantly greater incongruence for two of the four care values (autonomy and burden) for this pattern over the alternative pattern of perception; (c) the direction of incongruence indicated that CGs underestimated the importance of all four care values to the PWDs.
Table 2.
Differentiation of Dyadic Patterns of Perception Regarding the Importance of Care Values to the PWD
| Pattern 1: shared understanding (n = 173 dyads) ± SD | Pattern 2: CG underestimating (n = 55 dyads) ± SD | p-value (t-tests) | Effect size (Cohen’s d) | |
|---|---|---|---|---|
| Autonomy | ||||
| Dyadic average | 2.73 ± 0.22 | 2.54 ± 0.29 | <.0001 | 0.80 |
| Incongruence | 0.03 ± 0.26 | –0.14 ± 0.37 | <.001 | 0.54 |
| Avoiding burden | ||||
| Dyadic average | 2.72 ± 0.15 | 2.27 ± 0.20 | <.001 | 2.66 |
| Incongruence | –0.02 ± 0.23 | –0.57 ± 0.44 | <.001 | 1.86 |
| Choosing who helps | ||||
| Dyadic average | 2.65 ± 0.14 | 2.49 ± 0.20 | <.001 | 0.93 |
| Incongruence | –0.14 ± 0.32 | –0.17 ± 0.42 | .539 | 0.10 |
| Maintaining social relations | ||||
| Dyadic average | 2.52 ± 0.25 | 2.40 ± 0.30 | .004 | 0.37 |
| Incongruence | –0.10 ± 0.25 | –0.15 ± 0.22 | .273 | 0.15 |
All scores reported for patterns are empirical Bayes estimates derived from multi-level modelling analysis, which takes into account the interdependence of data and corrects scores for measurement error (i.e., not the raw average or raw difference scores). Negative incongruence scores indicate that CGs rate the value as less important than PWDs; positive incongruence scores indicate that CGs rate the value as more important than PWDs.
CG = family caregiver; PWD = person with dementia.
Figure 1.
Distinct dyadic patterns of perception of the importance of care values to the PWD. PWD = person with dementia; CG = family caregiver; Dashed lines represent average amount of incongruence between perceptions of the PWD’s care values for each pattern: the “Shared Understanding” pattern (n = 173 dyads) and the “CG Underestimating” pattern (n = 55 dyads).
In the dominant pattern of perception, 75% of dyads were labeled as having “shared understanding” of care values due to: (a) no incongruence for the value of avoiding burden, (b) less incongruence than in the “CG underestimating” pattern for all three of the other care values. Dyadic averages for perceptions of the importance of care values to the PWD were significantly different between the two patterns for all four of the care values (see Table 2). The two patterns of perception were most divergent over the value of avoiding being a burden on others, with very large effect sizes for both the dyadic average (Cohen’s d = 2.66) and incongruence (d = 1.86). There were also large effect sizes for the dyadic averages corresponding to the values of choosing who helps with care (d = 0.93) and maintaining autonomy (d = 0.80), and moderate effect sizes for difference between patterns in the amount of incongruence corresponding to the values of autonomy (d = 0.53) and maintaining social relations (d = 0.37).
Table 3 reports unadjusted differences in characteristics between the two patterns, according to t-tests. In the “CG underestimating” pattern, dyads were characterized by a significantly higher rate of dementia diagnosis and significantly more strain in the dyad’s relationship. In the multivariate logistic regression analysis (see Table 4), higher relationship strain remained significantly associated (OR = 3.21, p < .001) with a higher likelihood of being in the “CG underestimating” group, controlling for positive dyadic interactions (NS), level of cognitive function in PWDs (OR = 0.87, p = .007), dementia diagnosis (OR = 3.55, p = .001), employment status of the CG (NS), kin relationship type (NS), CG gender (NS), race/ethnicity of CG (NS), and age of PWD (OR = 0.95, p = .013).
Table 3.
Unadjusted Differences in Sample Characteristics Between Patterns of Perception (t-tests or χ2)
| Pattern 1: shared understanding (n = 173 dyads) | Pattern 2: CG underestimating (n = 55 dyads) | p-value | |
|---|---|---|---|
| Factors | |||
| Age in years | 74.95 ± 9.28 | 72.36 ± 8.13 | .065 |
| Gender (% female) | 94 (54%) | 28 (51%) | .659 |
| Race/ethnicity (% non-Hispanic white) | 136 (79%) | 46 (84%) | .421 |
| MMSE score | 24.63 ± 3.42 | 23.69 ± 3.59 | .081 |
| Dementia diagnosis (% yes) | 99 (58%) | 43 (76%) | .005 |
| Education level (% some college or more) | 111 (65%) | 34 (63%) | .756 |
| CG factors | |||
| Age in years | 65.31 ± 12.98 | 63.76 ± 12.49 | .440 |
| Gender (% female) | 127 (73%) | 40 (73%) | .921 |
| Race/ethnicity (% non-Hispanic white) | 141 (81%) | 46 (84%) | .721 |
| Paid employment (% yes) | 91 (53%) | 22 (40%) | .104 |
| Education level (% some college or more) | 131 (77%) | 43 (80%) | .694 |
| Dyadic factors | |||
| Dyad co-residing (% yes) | 137 (79%) | 44 (80%) | .900 |
| Kinship type (% spouses/partners) | 111 (64%) | 37 (67%) | .675 |
| Relationship strain (PWD perception) | 1.76 ± 0.62 | 1.86 ± 0.54 | .244 |
| Relationship strain (CG perception) | 1.78 ± 0.58 | 2.01 ± 0.63 | .013 |
| Positive dyadic interactions (PWD perception) | 2.87 ± 0.62 | 2.89 ± 0.49 | .870 |
| Positive dyadic interactions (CG perception) | 2.83 ± 0.63 | 2.93 ± 0.48 | .297 |
CG = family caregiver; MMSE = Mini-Mental State Examination; PWD = person with dementia.
Table 4.
Multivariate Logistic Regression Predicting “CG Underestimating” Pattern
| Predictor (scale: sample range) | Odds ratio, p-value, 95% Confidence Interval |
|---|---|
| PWD factors | |
| Age (years: 43–90) | OR= 0.954, p = .013, CI [0.92, 0.99] |
| Cognitive impairment (MMSE: 15–30) | OR= 0.867, p = .007, CI [0.78, 0.96] |
| Dementia diagnosis (1 = yes, 0 = no) | OR= 3.547, p = .001, CI [1.65, 7.62] |
| CG factors | |
| Race/ethnicity (1 = all, except non-Hispanic white = 0) | OR= 0.730, p = .532, CI [0.27, 1.96] |
| Paid employment (1 = yes, 0 = no) | OR= 0.564, p = .145, CI [0.26, 1.22] |
| Gender (1 = female, 0 = male) | OR= 1.168, p = .696, CI [0.54, 2.54] |
| Dyadic factors | |
| Kinship type (spouses/partners) | OR= 0.983, p = .967, CI [0.45, 2.17] |
| Relationship strain: CG’s perception (DRS, 1–4) | OR= 3.208, p = .000, CI [1.68, 6.12] |
| Positive dyadic interactions: CG’s perception (DRS, 1–4) | OR= 1.998, p = .065, CI [0.96, 4.17] |
Model results: Likelihood ratio χ2 = 35.18, p < .001, pseudo-R2 = 0.14; Post-estimation procedures indicated that the overall fit of the multivariate model was good: the Hosmer–Lemeshow goodness-of-fit test was non-significant (p = .65), the correct classification rate was 77%, and the area under the curve was 75%.
CG = Family caregiver; DRS = Dyadic Relationship Scale (Sebern & Whitlatch, 2007); MMSE = Mini-Mental State Examination (Folstein et al., 1975); PWD = person with dementia.
Discussion
This study examined family care dyads’ perceptions of care values in dementia. Two distinct dyadic patterns of perception were observed: (a) 25% of dyads were observed as belonging to the “CG underestimating” pattern, exhibiting lower dyadic averages for perceptions of the importance of the PWD’s care values, more incongruence in perceptions of care values, and CGs underestimating the importance of the PWD’s care values to the PWD; and (b) 75% of dyads were observed as belonging to a pattern of shared understanding, exhibiting less/no incongruence in perceptions of care values, and a higher dyadic average for rating the importance of care values highly. The “CG underestimating” pattern was characterized by dyads with more instances of dementia diagnosis, more cognitive impairment among PWDs, younger age in PWDs, and greater relationship strain in the dyad. Our hypotheses for this study were supported, but there are several notable findings deserving further discussion.
The CG needs knowledge and understanding of the PWD’s care values in order to be an active participant in dementia care planning, and eventually to make surrogate decisions that support the PWD’s values (Hirschman et al., 2006; Robins-Browne et al., 2017). It is important to note that the majority of dyads in this study (75%) belonged to the lower-risk pattern of “shared understanding.” This sub-group of dyads still exhibited some incongruence, however a complete absence of incongruence is not likely a feasible goal, and the dyads that fell into the “CG underestimating” pattern clearly represent the target population for future interventions to improve knowledge and understanding of the PWD’s care values. This has important implications for conserving scarce resources and creating interventions that are more effective for the higher-risk minority of dyads that need the most help with care planning.
In this study, and in previous research, CGs were more likely to underestimate than overestimate the importance of everyday care values to the PWD (Miller et al., 2017; Reamy et al., 2011). The interesting and novel aspect of this study was the examination of incongruence across multiple care values in latent patterns of perception. The current study revealed that the values of “autonomy” and “avoiding being a burden” were most influential in distinguishing between patterns. For example, a CG’s underestimation of the importance to the PWD of maintaining autonomy may lead the CG to support more rapid dependence. However, the highest amount of incongruence observed in this study corresponded with the value of “avoiding being a burden” (i.e. CGs highly underestimated how important it was for the PWD to avoid being a burden on others). For CGs in dyads that belong to the underestimating pattern, incongruence over the importance of the value of “avoiding being a burden” implies that CGs may take on more care responsibilities than the PWD desires. The main clinical implication is that it is not only necessary to solicit information about care values from the PWD, it is also important to subsequently address and realign the CG’s expectations for providing care.
Dementia diagnosis as a risk factor for belonging to the “CG underestimating” pattern was an unexpected finding. In this study of PWDs with early-stage dementia, a confirmed (rather than probable or presumed) diagnosis significantly increased the likelihood of being in the “CG underestimating” pattern, above and beyond the level of cognitive impairment. The level of cognitive impairment (according to MMSE scores) was also significant, which is consistent with previous studies (Buckley et al., 2012; Reamy et al., 2011). Whereas the severity of cognitive impairment has implications for the PWD’s ability to communicate their values and be involved in care planning (Sörensen, Mak, & Pinquart, 2011), being diagnosed with dementia is an opportunity to come together with family members to plan for future care. Several researchers have noted the potential for detrimental effects of a diagnosis of dementia, such as stigma (Werner, 2014), losing decisional capacity (Sabat, 2005), and loss of quality of life (Stites, Karlawish, Harkins, Rubright, & Wolk, 2017; Whitehouse, 2009). It is likely that even in the face of noticeable cognitive impairment, CGs’ perceptions of the PWD’s values are affected negatively by this confirmation of the irreversible decline to come. Future research should focus on how information and education about the disease shapes CGs’ perceptions of the PWD, and study longitudinally how incongruence changes as dementia progresses and its effects on dementia care planning.
Greater strain in the dyad’s relationship, when perceived by CGs, also helped identify which dyads belonged to the “CG underestimating” pattern. This finding is consistent with previous studies that have also found an association between relationship strain and incongruence (Lyons et al., 2002; Miller et al., 2017; Moon et al., 2016). The concept of stress proliferation explains that secondary strains–such as relationship strain–are manifestations of the primary dementia-related stressors (e.g. cognitive impairment), and can rapidly proliferate depending on the individuals’ circumstances (Aneshensel et al., 1995). A perception of higher relationship strain could be a reflection of how the CG has internalized the damaging effects that the disease can have on the dyad’s relationship (Pearlin et al., 1990). This type of negative appraisal among CGs also helps explain why their perceptions of the importance of the PWD’s care values would be lower despite minimal differences in any other characteristics of CGs or PWDs belonging to the incongruent subgroup. The stress process may have proliferated more extensively among CGs in the underestimating subgroup, as evidenced by more their negative perceptions of the dyad’s relationship and underestimation of the importance of care values to the PWD. Future research examining the mechanisms of the SPM would help pinpoint at which juncture stress is likely to proliferate for dyads in this distinct subgroup.
Limitations
Although this study was possible because of the large number of dyads obtained by merging datasets, there were some limitations that resulted from our approach, most prominently the lack of measures available in across merged/secondary datasets and the inability to achieve a higher proportion of explained variance for factors associated with our observed patterns of perception. In future studies, it will be important to consider other potential stressors and strains (e.g., service use, CG role overload, social isolation) that may be influential on perceptions of the importance of care values to the PWD, and on care planning more broadly. The integrated MLM and LCMM approach was a strength of the study, but a caveat is that the residual terms capturing measurement error in the MLM analyses were not included in the LCMM phase of analysis, and thus only fixed effects (i.e., not random effects) were modeled in LCMM. Lastly, we were not able to include the value of safety in our analysis, which is often at odds with the value of autonomy and will be important to include in future research.
Strengths
The large and diverse sample of family care dyads included in this study was a great strength that allows for better generalizability. Another strength of this study was the inclusion of the PWD’s perspective, which is necessary when examining incongruence in family care dyads, but it also reflects the dyadic process inherent within caregiving (Lyons et al., 2002). Furthermore, this study was novel in the integration of MLM and LCMM, which allowed for the data to preserved as dyadic while identifying patterns of perception. This integrated analysis adds clinical usefulness to the study in terms of identifying a risk profile and differentiating which dyads are most likely to be in the higher risk group. Dementia care planning could be substantially improved by tailoring efforts to the needs of more high-risk dyads, thereby helping those who need the most help.
Although care planning ideally occurs proactively in an older adult’s life, it is most often initiated or revisited in reaction to an event, such as a decline in health or physical function (Aspinwall, 2005; Sörensen et al., 2011). A diagnosis of dementia requires extensive care planning, since the illness leads to progressive dependence upon others to maintain one’s daily life. In addition to the areas for future research and theory that have already been discussed above, a goal of this study was to inform practice. For practitioners involved in care planning or case management for PWDs and their CGs, this study suggests that, in a distinct subset of dyads, relying solely upon a family proxy for dementia care planning could yield care decisions that fall short of representing the PWD’s values. Interventions to improve care planning in this higher-risk group may include working with the dyad to identify and communicate about the PWD’s views on the importance of care values, strategies for alleviating relationship strain, early-stage planning, and disease education.
Funding
None reported
Conflict of Interest
None reported.
Acknowledgements
This work was supported in part by grants from the National Institute of Nursing Research and National Institute of Mental Health, of the National Institutes of Health (T32NR013456; R01MH070629); and the U.S. Administration for Community Living (90AI0040; 90AI0004; 90CG256). The content is solely the responsibilities of the authors and does not necessarily represent the views of the funding agencies.
References
- Aneshensel C. S., Pearlin L. I., Mullan J. T., Zarit S. H., & Whitlatch C. J (1995). Profiles in caregiving: The unexpected career. San Diego, CA: Academic Press. [Google Scholar]
- Aspinwall L. G. (2005). The pscyhology of future-oriented thinking: From achievement to proactive coping, adaptation, and aging. Motivation and Emotion, 29, 203–235. doi:10.1007/s11031-006-9013-1 [Google Scholar]
- Bangerter L. R., Griffin J. M., Zarit S. H., & Havyer R (2017). Measuring the needs of family caregivers of people with dementia: An assessment of current methodological strategies and key recommendations. Journal of Applied Gerontology, 1–15. doi:10.1177/0733464817705959 [DOI] [PubMed] [Google Scholar]
- Buckley T., Fauth E. B., Morrison A., Tschanz J., Rabins P. V., Piercy K. W., …Lyketsos C. G (2012). Predictors of quality of life ratings for persons with dementia simultaneously reported by patients and their caregivers: the Cache County (Utah) Study. International Psychogeriatrics, 24, 1094–1102. doi:10.1017/S1041610212000063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpenter B. D., Kissel E. C., & Lee M. M (2007). Preferences and life evaluations of older adults with and without dementia: Reliability, stability, and proxy knowledge. Psychology and Aging, 22, 650–655. doi:10.1037/0882-7974.22.3.650 [DOI] [PubMed] [Google Scholar]
- Clemmensen T. H., Busted L. M., Soborg J., & Bruun P (2016). The family’s experience and perception of phases and roles in the progression of dementia: An explorative, interview-based study. Dementia (London). doi:10.1177/1471301216682602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliott B. A., Gessert C. E. & Peden-McAlpine C (2009). Family decision-making in advanced dementia: Narrative and ethics. Scandinavian Journal of Caring Sciences, 23, 251–258. doi:10.1111/j.1471-6712.2008.00613.x [DOI] [PubMed] [Google Scholar]
- Esandi N., Nolan M., Alfaro C., & Canga-Armayor A (2017). Keeping things in balance: Family experiences of living with Alzheimer’s disease. The Gerontologist. doi:10.1093/geront/gnx084 [DOI] [PubMed] [Google Scholar]
- Feinberg L. F. & Whitlatch C. J (2001). Are persons with cognitive impairment able to state consistent choices?The Gerontologist, 41, 374–382. doi:10.1093/geront/41.3.374 [DOI] [PubMed] [Google Scholar]
- Folstein M. F., Folstein S. E. & McHugh P. R (1975). “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research, 12, 189–198. doi:10.1016/0022-3956(75)90026-6 [DOI] [PubMed] [Google Scholar]
- Heid A. R., Bangerter L. R., Abbott K. M. & Van Haitsma K (2017). Do family proxies get it right? Concordance in reports of nursing home residents’ everyday preferences. Journal of Applied Gerontology, 36, 667–691. doi:10.1177/0733464815581485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirschman K. B., Kapo J. M., & Karlawish J (2006). Why doesn’t a family member of a person with advanced dementia use a substituted judgment when making a decision for that person?American Journal of Geriatric Psychiatry, 14, 659–667. doi:10.1097/01.JGP.0000203179.94036.69 [DOI] [PubMed] [Google Scholar]
- Jox R. J., Denke E., Hamann J., Mendel R., Förstl H. & Borasio G. D (2012). Surrogate decision making for patients with end-stage dementia. International Journal of Geriatric Psychiatry, 27, 1045–1052. doi:10.1002/gps.2820 [DOI] [PubMed] [Google Scholar]
- Karlawish J. H., Casarett D., Propert K. J., James B. D. & Clark C. M (2002). Relationship between Alzheimer’s disease severity and patient participation in decisions about their medical care. Journal of Geriatric Psychiatry and Neurology, 15, 68–72. doi:10.1177/089198870201500203 [DOI] [PubMed] [Google Scholar]
- Kim K., Fingerman K. L., Birditt K. S. & Zarit S. H (2016). Capturing between- and within-family differences in parental support to adult children: A typology approach. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 71, 1034–1045. doi:10.1093/geronb/gbv029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koppelman E. R. (2002). Dementia and dignity: Towards a new method of surrogate decision making. The Journal of Medicine and Philosophy, 27, 65–85. doi:10.1076/jmep.27.1.65.2971 [DOI] [PubMed] [Google Scholar]
- Lee C. S., Mudd J. O., Auld J., Gelow J. M., Hiatt S. O., Chien C. V., …Lyons K. S (2017). Patterns, relevance and predictors of heart failure dyadic symptom appraisal. European Journal of Cardiovascular Nursing, 16, 595–604. doi:10.1177/1474515117700760 [DOI] [PubMed] [Google Scholar]
- Lyons K. S., Zarit S. H., Sayer A. G. & Whitlatch C. J (2002). Caregiving as a dyadic process: Perspectives from caregiver and receiver. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 57, P195–P204. doi:10.1093/geronb/57.3.P195 [DOI] [PubMed] [Google Scholar]
- Miller L. M., Whitlatch C. J., Lee C. S., & Lyons K. S (2017). Incongruent perceptions of the care values of hospitalized persons with dementia: A pilot study of patient-family caregiver dyads. Aging & Mental Health, 1–8. doi:10.1080/13607863.2017.1280766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell A. J. (2009). A meta-analysis of the accuracy of the mini-mental state examination in the detection of dementia and mild cognitive impairment. Journal of Psychiatric Research, 43, 411–431. doi:10.1016/j.jpsychires.2008.04.014 [DOI] [PubMed] [Google Scholar]
- Moon H., Townsend A., Whitlatch C. J., & Dilworth-Anderson P (2016). Quality of life for dementia caregiving dyads: Effects of incongruent perceptions of everyday care and values. Gerontologist, 57, 657–666. doi:10.1093/geront/gnw055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moon H., Townsend A. L., Dilworth-Anderson P. & Whitlatch C. J (2016). Predictors of discrepancy between care recipients with mild-to-moderate dementia and their caregivers on perceptions of the care recipients’ quality of life. American Journal of Alzheimer’s Disease and Other Dementias, 31, 508–515. doi:10.1177/1533317516653819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Alliance for Caregiving (2017). Dementia caregiving in the U.S. Retrieved from http://www.caregiving.org/wp-content/uploads/2014/01/Dementia-Caregiving-in-the-US_February-2017.pdf [Google Scholar]
- Orsulic-Jeras S., Whitlatch C. J., Szabo S. M., Shelton E. G., & Johnson J (2016). The SHARE program for dementia: Implementation of an early-stage dyadic care-planning intervention. Dementia (London). doi:10.1177/1471301216673455 [DOI] [PubMed] [Google Scholar]
- Pearlin L. I., Mullan J. T., Semple S. J. & Skaff M. M (1990). Caregiving and the stress process: An overview of concepts and their measures. The Gerontologist, 30, 583–594. doi:10.1093/geront/30.5.583 [DOI] [PubMed] [Google Scholar]
- Pinquart M. & Sörensen S (2003). Associations of stressors and uplifts of caregiving with caregiver burden and depressive mood: A meta-analysis. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 58, P112–P128. [DOI] [PubMed] [Google Scholar]
- Raudenbush S. W., Bryk A. S., & Congdon R (2011). HLM for Windows (Version 7). Skokie, IL: Scientific Software International, Inc. [Google Scholar]
- Reamy A. M., Kim K., Zarit S. H. & Whitlatch C. J (2011). Understanding discrepancy in perceptions of values: Individuals with mild to moderate dementia and their family caregivers. The Gerontologist, 51, 473–483. doi:10.1093/geront/gnr010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reamy A. M., Kim K., Zarit S. H. & Whitlatch C. J (2013). Values and preferences of individuals with dementia: Perceptions of family caregivers over time. The Gerontologist, 53, 293–302. doi:10.1093/geront/gns078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robins-Browne K., Hegarty K., Guillmen M., Komesaroff P. & Palmer V (2017). The role of relational knowing in advance care planning. The Journal of Clinical Ethics, 28, 122–134. [PubMed] [Google Scholar]
- Sabat S. R. (2005). Capacity for decision-making in Alzheimer’s disease: Selfhood, positioning and semiotic people. The Australian and New Zealand Journal of Psychiatry, 39, 1030–1035. doi:10.1080/j.1440-1614.2005.01722.x [DOI] [PubMed] [Google Scholar]
- Samsi K. & Manthorpe J (2013). Everyday decision-making in dementia: Findings from a longitudinal interview study of people with dementia and family carers. International Psychogeriatrics, 25, 949–961. doi:10.1017/S1041610213000306 [DOI] [PubMed] [Google Scholar]
- Sands L. P., Ferreira P., Stewart A. L., Brod M. & Yaffe K (2004). What explains differences between dementia patients’ and their caregivers’ ratings of patients’ quality of life?The American Journal of Geriatric Psychiatry, 12, 272–280. doi:10.1097/00019442-200405000-00006 [PubMed] [Google Scholar]
- Sayer A. G., & Klute M. M (2005). Analyzing couples and families: Multilevel methods. In Bengtson V. L., Acock A. C., Allen K. R., Dilworth-Anderson P., & Klein D. M (Eds.), Sourcebook of family theory and research (pp. 289–313). Thousand Oaks, CA: Sage Publications. [Google Scholar]
- Schmid B., Allen R. S., Haley P. P. & Decoster J (2010). Family matters: Dyadic agreement in end-of-life medical decision making. The Gerontologist, 50, 226–237. doi:10.1093/geront/gnp166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sebern M. D. & Whitlatch C. J (2007). Dyadic relationship scale: A measure of the impact of the provision and receipt of family care. The Gerontologist, 47, 741–751. doi:10.1093/geront/47.6.741 [DOI] [PubMed] [Google Scholar]
- Smebye K. L., Kirkevold M. & Engedal K (2012). How do persons with dementia participate in decision making related to health and daily care? A multi-case study. BMC Health Services Research, 12, 241. doi:10.1186/1472-6963-12-241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sörensen S., Mak W. & Pinquart M (2011). Planning and decision making for care transitions. Annual Review of Gerontology & Geriatrics, 31, 111–142. doi:10.1891/0198-8794.31.111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Statacorp (2017). Stata statistical software: Release 15 (Version 14). College Station, TX: StataCorp LP. [Google Scholar]
- Stites S. D., Karlawish J., Harkins K., Rubright J. D. & Wolk D (2017). Awareness of mild cognitive impairment and mild Alzheimer’s disease dementia diagnoses associated with lower self-ratings of quality of life in older adults. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 72, 974–985. doi:10.1093/geronb/gbx100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Werner P. (2014). Stigma and Alzheimer's disease: A systematic review of evidence, theory, and methods. In Corrigan P. W. (Ed.), The stigma of disease and disability: Understanding causes and overcoming injustices (pp. 223–244). Retrieved from 10.1037/14297-012 [DOI] [Google Scholar]
- Whitehouse P. J. (2009). Can we fix this with a pill? Qualities of life and the aging brain. In Ballenger J. F., Whitehouse P. J., Lyketsos C. G., Rabins P. V., & Karlawish J(Eds.), Treating dementia: Do we have a pill for it? (pp. 168–182). Baltimore, MD: The Johns Hopkins University Press. [Google Scholar]
- Whitlatch C. J., Feinberg L. F., & Tucke S. S (2005a). Accuracy and consistency of responses from persons with cognitive impairment. Dementia, 4, 171–183. doi:10.1177/1471301205051091 [Google Scholar]
- Whitlatch C. J., Feinberg L. F. & Tucke S. S (2005b). Measuring the values and preferences for everyday care of persons with cognitive impairment and their family caregivers. The Gerontologist, 45, 370–380. doi:10.1093/geront/45.3.370 [DOI] [PubMed] [Google Scholar]
- Whitlatch C. J., Heid A. R., Femia E. E., Orsulic-Jeras S., Szabo S. M., & Zarit S. H (2017). The support, health, activities, resources, and education program for early stage dementia: Results from a randomized controlled trial. Dementia (London). doi:10.1177/1471301217743033 [DOI] [PubMed] [Google Scholar]
- Whitlatch C. J., Judge K., Zarit S. H. & Femia E (2006). Dyadic intervention for family caregivers and care receivers in early-stage dementia. The Gerontologist, 46, 688–694. doi:10.1093/geront/46.5.688 [DOI] [PubMed] [Google Scholar]
- Whitlatch C. J., Piiparinen R., & Feinberg L. F (2009). How well do family caregivers know their relatives’ care values and preferences?Dementia, 8, 223–243. doi:10.1177/1471301209103259 [Google Scholar]