Abstract
Primary immunodeficiencies affecting the function of neutrophils and other phagocytic leukocytes are notable for an increased susceptibility to bacterial and fungal infections as a result of impaired leukocyte recruitment, ingestion, and/or killing of microbes. The underlying molecular defects can also impact other innate immune responses to infectious and inflammatory stimuli, leading to inflammatory and autoimmune complications that are not always directly related to infection. This review will provide an update on congenital disorders affecting neutrophil function in which a combination of host defense and inflammatory complications are prominent, including nicotinamide dinucleotide phosphate oxidase defects in chronic granulomatous disease and β2 integrin defects in leukocyte adhesion deficiency.
Introduction
Immune dysregulation is a feature of many primary immunodeficiency (PID) disorders,1-3 including those affecting neutrophil function. Neutrophils and other phagocytes are essential effectors of innate immunity and rapidly respond to the presence of invading bacteria, fungi, and parasites. Inflammatory signals activate adhesion, chemotaxis, phagocytosis, and release of oxidants, proteases, and other molecules aimed at microbial killing. These same processes are important for appropriate responses to wounds or sterile inflammation. Phagocytic leukocytes also synthesize and secrete multiple inflammatory mediators, including leukotrienes, chemokines, and other cytokines to amplify and regulate the inflammatory response and initiate cross talk with adaptive immune cells. Hence, PID with functional phagocyte defects can display recurrent severe bacterial and fungal infections and aberrant inflammation that is not always related to infection.
This review will cover the current understanding of the clinical features and underlying mechanisms driving dysregulated inflammation in 2 inherited defects affecting neutrophil function. A major focus will be on chronic granulomatous disease (CGD), which results from genetic defects in the leukocyte nicotinamide dinucleotide phosphate (NADPH) oxidase. Clinical manifestations in CGD include recurrent bacterial and fungal infections, as well as acute and chronic inflammatory conditions, which reflect the broad impact of reactive oxygen species (ROS) generated from the NADPH oxidase on immune responses. In addition, new insights into the severe periodontal disease associated with leukocyte adhesion deficiency type 1 (LAD-1) will be summarized. This manifestation illuminates another facet of neutrophil biology, in which clearance of senescent neutrophils in tissues is linked to an interleukin-23 (IL-23)–IL-17–granulocyte colony-stimulating factor (G-CSF) cytokine axis that is dysregulated in LAD-1.
CGD
CGD is caused by inactivating X-linked or autosomal-recessive mutations in the leukocyte NADPH oxidase (also referred to as the respiratory burst oxidase) (Figure 1).4,5 Superoxide generated by this enzyme is rapidly converted into other ROS, including H2O2 and myeloperoxidase-catalyzed formation of hypochlorous acid. These oxidants have important microbicidal activity, because their absence leads to susceptibility to a distinctive set of bacterial and fungal pathogens. A second hallmark of CGD is the frequent development of granulomas and other inflammatory disorders. These symptoms reflect the importance of NADPH oxidase–derived ROS for microbial killing, as well as for their pleiotropic impact on other cellular processes.6-10
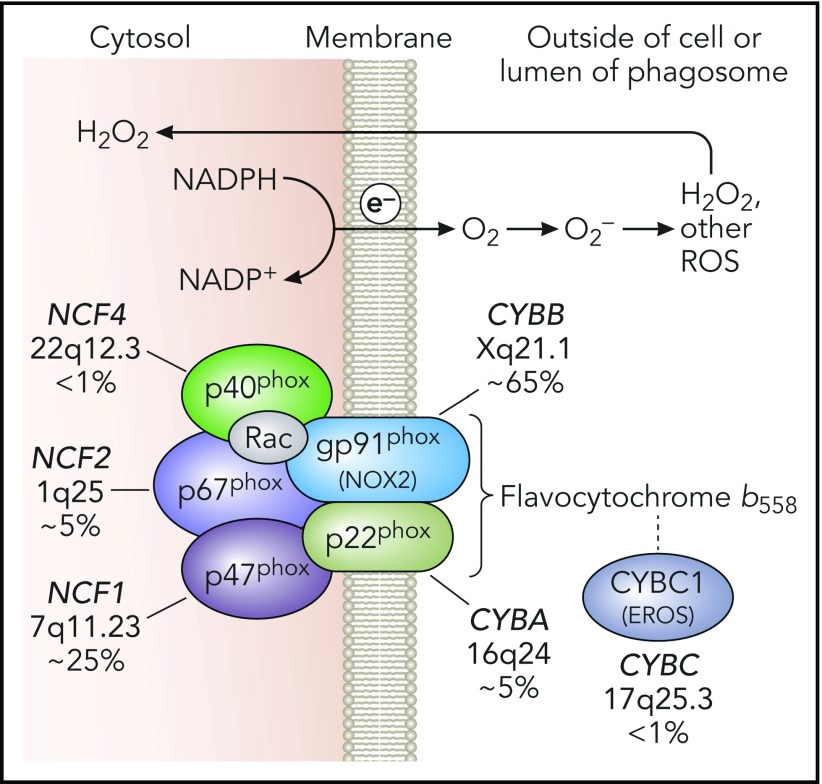
Figure 1.
NADPH oxidase and genetic defects in CGD. The leukocyte NADPH oxidase enzyme complex is composed of membrane and cytosolic subunits that are referred to by their molecular mass (kDa) and the designation “phox,” for phagocyte oxidase. CYBB and CYBA refer to cytochrome b-245 β chain and cytochrome b-245 α chain, respectively, the large and small subunits of flavocytochrome b558, whereas NCF refers to neutrophil cytosolic factor, used to designate the cytosolic regulatory subunits of the oxidase. Flavocytochrome b558 is the electron transferase and is located in plasma, specific granules (in neutrophils), and phagosome and some endosome membranes. This heterodimer is composed of gp91phox and p22phox. The gp91phox subunit is sometimes referred to as NOX2. CYBC1 (also known as EROS) is an endoplasmic reticulum protein important for expression of the flavocytochrome b558 heterodimer. The soluble regulatory proteins p47phox, p67phox, and p40phox form a complex in the cytosol; upon leukocyte activation, phosphorylation-induced conformational changes lead to their binding to flavocytochrome b558. The small GTPase Rac is also essential for NADPH oxidase enzymatic activity, which, in its active GTP-bound state, becomes membrane bound and activates p67phox. Together, these regulatory proteins activate the flavocytochrome b558–mediated transfer of electrons from cytosolic NADPH across the membrane via FAD and heme redox centers to molecular oxygen, thereby forming superoxide in the extracellular space or within phagosomes or endosomes. Superoxide is converted into H2O2, which can diffuse across membranes, and other ROS. CGD results from inactivating recessive mutations in any 1 of the 5 phox subunits or CYBC1, as indicated with the approximate incidence, gene, and chromosomal location. Professional illustration by Patrick Lane, ScEYEnce Studios.
The concept that the respiratory burst plays a broad role in immune responses was solidified by 2 key experimental observations. In 1 study, administration of sterile Aspergillus hyphae into the lungs of CGD mice induced an excessive acute neutrophilic response and subsequent chronic granulomatous inflammation.11 This finding established the importance of the NADPH oxidase for limiting inflammation, independent of its antimicrobial effects. A second important study made the link between NADPH oxidase deficiency and autoimmunity. Here, positional cloning identified a gene conferring increased severity of experimental arthritis in rats, which unexpectedly proved to be a hypomorphic mutation in an NADPH oxidase subunit, p47phox (NCF1).12
NADPH oxidase and molecular genetics of CGD
The NADPH oxidase is a multi-subunit phagosome and plasma membrane-associated enzyme (see Figure 1 for details) expressed in neutrophils, monocytes and macrophages, dendritic cells, and eosinophils.13 The enzyme is also present in B, and perhaps T, lymphocytes, although here its function is not well understood. The flavocytochrome b558 is composed of 2 integral membrane proteins: gp91phox (also known as NADPH oxidase 2 [NOX2]) and p22phox. The gp91phox subunit contains flavoprotein and heme-binding domains, and p22phox harbors a key docking site for p47phox. Heterodimer formation is mediated, in part, by the endoplasmic reticulum–resident protein essential for ROS (EROS), also known as CYBC1.14 A complex of 3 regulatory subunits, p47phox, p67phox, and p40phox, translocate from the cytoplasm to flavocytochrome b558, along with guanosine triphosphate (GTP)-bound Rac, upon cellular activation with inflammatory or phagocytic stimuli to initiate electron transfer from NADPH to molecular oxygen. Defects in the leukocyte-specific Rac2 isoform lead to only mild impairments in the NADPH oxidase, probably because of redundancy with Rac1, and are not associated with a CGD phenotype.4
CGD occurs in ≈1 in 200 000 live births.15 Approximately two thirds of patients have defects in X-linked CYBB.4 Autosomal-recessive mutations in NCF1 account for ≈25% of CGD. Rarer autosomal-recessive forms of CGD involve mutations in CYBA, NCF2, or NCF4 genes. The incidence of autosomal-recessive CGD is higher in countries with high rates of consanguineous marriage.16,17
Autosomal-recessive null mutations in NCF4 or CYBC1 have only recently been described.18-21 In contrast to the “classic” forms of CGD that lack or have profoundly reduced NADPH oxidase activity, the respiratory burst defects are more nuanced. NCF4 (p40phox) is a specialized subunit that stimulates phagosome oxidase activity via a regulatory domain that binds to phosphatidylinositol 3-phosphate, a membrane lipid present in high concentrations on phagosome and other intracellular membranes.13 As a result, intracellular NADPH oxidase activity is substantially reduced, especially to phagocytic stimuli, and macrophages also display a partial reduction in plasma membrane activity.18,19,22 Thus far, 24 patients with NCF4 defects are described worldwide.18,19 EROS (CYBC1) defects were originally identified in a mouse mutagenesis screen and associated with a profound reduction in macrophage flavocytochrome b558; neutrophils appeared less affected.14 Nine patients are reported, including 8 from Iceland homozygous for the same founder mutation and 1 patient from Saudi Arabia.20,21 Detailed studies are still limited but suggest that defects in human monocyte and macrophage flavocytochrome b558 expression and NADPH oxidase activity are more substantial that those in neutrophils. Of note, phorbol ester–induced dihydrorhodamine-1,2,3 oxidation in neutrophils, a widely used diagnostic test for CGD, may not be abnormal in NCF4 or CYBC1 deficiency.
Clinical features of CGD
Infections
Manifestations of CGD typically begin in infancy or early childhood, although they can be delayed until adolescence or even adulthood.4,15-17,23-27 CGD patients are particularly susceptible to Staphylococcus aureus, Burkholderia cepacia, Nocardia spp., and certain gram-negative enteric bacilli, including Serratia marcescens and Salmonella spp.28 CGD patients have increased risk from Mycobacterium tuberculosis in endemic areas and can develop severe local or systemic disease with bacillus Calmette-Guérin (BCG), an attenuated strain of Mycobacterium bovis, following BCG vaccination.17,24 Invasive fungal infections are a major threat in CGD, most commonly with Aspergillus fumigatus and Aspergillus nidulans.29,30 Frequent sites of infection include the lungs, lymph nodes, skin and soft tissues, the gastrointestinal (GI) tract, including staphylococcal liver abscesses, and osteomyelitis.4,15
Inflammatory complications
Inflammatory manifestations are common in CGD and are often associated with neutrophilic and/or granulomatous inflammation.4-10,31 These symptoms can reflect a dysregulated inflammatory response in the absence of respiratory burst–derived ROS. Excessive acute or persistent inflammation can be seen in the setting of active infection or as a sequelae. However, in other cases, abnormal inflammation develops in the absence of antecedent infection.
Recurrent or chronic inflammatory conditions can involve the skin, GI tract, lung, and liver. A retrospective study of 98 CGD patients from a single institution found that almost 70% had symptoms associated with inflammatory manifestations,32 similar to prior multi-institution registry data.15,25-27 GI symptoms, including abdominal pain, diarrhea, and oral aphthous ulcers, were present in 60 patients. Forty-four patients underwent biopsy, and chronic GI inflammatory lesions were identified in 22 patients. Pulmonary findings, including dyspnea, were reported in 18 patients and were associated with pleural thickening, interstitial lung disease, and/or fibrosis. Twelve patients had episodes of bladder wall granulomas or other inflammation involving the urogenital tract. Chorioretinitis and ocular granulomata were reported in 6 patients, and 7 patients had discoid lupus, leukocytoclastic vasculitis, arthritis, or dermatomyositis. Liver disease with noncirrhotic portal hypertension can also occur and may be an independent risk factor for mortality in CGD.33
The most frequent inflammatory disease of significance is GI disease that is somewhat reminiscent of Crohn’s disease. This can occur in all genetic subgroups of CGD and does not correlate with a higher risk for severe bacterial and fungal infections.28 Although involvement of the anus and rectum is most common, upper GI tract disease is also common.34-36 Microgranulomas pigmented macrophages and tissue eosinophilia are common biopsy findings.35 Granulomatous obstruction of the gastric outlet or urinary tract also occur. X-linked carriers of CGD are also at risk for developing Crohn’s disease, which affected 5 of 93 women in a recent study.37
Macrophage activation syndrome and hemophagocytic lymphohistiocytosis (HLH) can be another complication of CGD. In 63 patients with PIDs that met criteria for HLH but did not have cytotoxicity defects or X-linked lymphoproliferative disorders, 22 had CGD.38 These episodes were triggered by fungi, bacteria (especially B cepacia), or Leishmania in endemic areas. In another new study, only 19 of 101 children with HLH who received genetic testing had biallelic mutations in recognized familial HLH genes. Of the remaining children, 47 underwent whole-exome sequencing, and 14 patients proved to have PID, including 2 with underlying CGD.39
Aberrant inflammation with autoimmune features can also occur in CGD. Up to ≈10% of patients with X-linked CGD develop discoid lupus-like lesions or aphthous ulcers.16,17,23-27 Discoid lupus, photosensitivity, and aphthous ulcers also occur in carrier females, with an incidence of 20% to 50%.37,40,41 Less commonly, CGD patients and X-linked CGD carriers develop systemic autoimmune disease, including lupus, juvenile idiopathic arthritis, antiphospholipid syndrome, idiopathic thrombocytopenic purpura, and immunoglobulin A nephropathy.16,17,23-27,37
Several studies demonstrated skewed immune response parameters in CGD patients studied at times when they were in otherwise good health. Analysis of global gene expression in CGD neutrophils showed constitutively increased expression of inflammation-associated genes, including chemokines and immune receptors.42 Analysis of whole blood in a different study showed increased expression of type 1 interferon–regulated genes in CGD.43 Another group identified increased IL-1β and tumor necrosis factor-α (TNF-α) content in CGD monocytes and a T helper 17 cell bias of CD4+ T cells.44 Human CGD monocytes produced higher levels of IL-1β when stimulated in vitro with particulate and soluble activators of caspase-1 and NLRP3 inflammasome, and 1 study also found increased IL-1α release upon lipopolysaccharide stimulation.45-47 Increased IL-8 release by CGD neutrophils following formyl-methionyl-leucyl phenylalanine stimulation is also reported.48 Finally, many CGD patients, even without colitis, have elevated levels of antimicrobial and other antibodies associated with inflammatory bowel disease (IBD), suggesting an abnormal response to chronic antigen stimulation.49,50
Clinical features in different subgroups of CGD and in X-linked CGD carriers
Patients with X-linked CGD and those with CYBA and NCF2 mutations tend to have a more severe clinical course compared with patients with NCF1 defects.4,15,51 This may reflect, in part, the observation that fungal infections occur slightly less frequently with NCF1 defects and are associated with lower mortality.28 p47phox−/− neutrophils have a small amount (≤2%) of residual enzyme activity, because this subunit functions as an adaptor protein rather than mediating electron transfer. Some X-linked CGD patients with a partially functional gp91phox also have a milder clinical course. These observations suggest that even a small amount of NADPH oxidase activity can partially mitigate the defects in host defense. In contrast, GI disease was not correlated with the degree of residual superoxide production.51
The spectrum of disease with defects in NCF4 or CYBC1, both of which have more superoxide production compared with the 4 original CGD subgroups,18-21 resembles an atypical form of CGD. To date, reported patients have not had invasive bacterial and fungal infections with typical CGD pathogens, including A fumigatus. However, 1 patient with CYBC1 deficiency developed a localized abscess following BCG vaccination20 and a second had miliary tuberculosis,21 perhaps due to a greater impairment in flavocytochrome b biosynthesis in CYBC1-deficient macrophages. More prominent in CYCB1 and NCF4 subgroups are inflammatory manifestations, including granulomatous GI disease; patients with NCF4 defects also frequently exhibited discoid lupus-like skin lesions.19-21
Female carriers of X-linked CGD, as already noted, can develop CGD-associated inflammatory conditions.37,40,41 X-linked inactivation of the chromosome harboring the mutant CYBB allele appears to be random, with a median ≈50% of neutrophils lacking NADPH oxidase activity.4,37 Carriers with ≤10% NADPH oxidase–positive neutrophils can develop infections characteristic of CGD.4,37,40 However, the occurrence of inflammatory and autoimmune complications appears to be independent of the frequency of NADPH oxidase–positive neutrophils. This suggests that even the absence of NADPH oxidase ROS in some leukocytes can promote aberrant inflammation.
Finally, there is a surprising clinical heterogeneity among the >90% of CGD patients who lack or are profoundly deficient in NADPH oxidase activity.4,15 Some develop symptoms beginning during infancy, whereas, at the other end of the spectrum, patients can be well for many years and then develop a serious infection or inflammatory complication. Coexisting genetic variants in other antimicrobial systems and components of innate immunity likely play important roles in modifying disease severity. Variants in the myeloperoxidase, mannose binding lectin, and FcγRIIa genes were associated with a higher risk for granulomatous or autoimmune complications in CGD.52 Each of 2 patients with HLH and X-linked CYBB or NCF1 CGD studied by whole-exome sequencing had a variant in a second gene (DOCK11 or NLRP12) that could impact inflammatory responses. Another study found an increased frequency of single nucleotide polymorphisms associated with IBD risk in 40 unrelated children with CGD who had IBD compared with CGD children without GI inflammation.53 Notably, the number of IBD risk variants in CGD IBD patients was much lower than in other pediatric IBD patients without underlying immunologic defects, supporting the concept that a defective NADPH oxidase is an independent and major risk factor for GI inflammation. Finally, although not yet systematically studied, there is some experimental support for the importance of environmental factors in CGD-associated inflammation. The severity of experimental colitis in NCF1-deficient CGD mice was similar to wild-type littermates, but it became more severe in CGD if the composition of gut microbiota was altered.54
Hypomorphic variants in NADPH oxidase genes are associated with inflammatory and autoimmune diseases
Multiple recent studies identified variant alleles of NADPH oxidase genes as risk factors for autoimmune diseases and inflammatory bowel disease, including lupus (NCF2), rheumatoid arthritis (NCF1, NCF4), Sjögren syndrome (NCF1), Crohn disease (NCF2, NCF4, RAC2), and early-onset IBD (NCF1, NCF2, NCF4, CYBB, RAC2).55-61 These include missense polymorphisms, whereas others are intronic, in promoters, or affect copy number. These variants are not associated with microbial infections. Many of the missense variants reside in important functional domains, but those characterized have only a modest effect on NADPH oxidase activity.55,56,62 These findings illustrate how loci involved as causes of PID overlap with those identified in polygenic disorders of autoimmunity and inflammation.1,63 In PID, rare monogenic mutations with a strong effect cause disease. For more common inflammatory/autoimmune disorders, multiple genes harboring common variants contribute to these conditions. Of note, the most frequent and major genetic associations with lupus are common missense polymorphisms in NCF1 and NCF2,58 and lupus is more severe in NADPH oxidase–deficient mice, including X-linked CGD carriers and mice heterozygous for an NCF2 deletion, in several models of murine lupus.64-66
Mechanisms underlying NADPH oxidase regulation of immune cell functions
ROS are generated by multiple sources and have beneficial and deleterious effects. Mitochondria may be the largest contributor of intracellular ROS, but the NADPH oxidase family,67 which includes the NOX2-containing leukocyte NADPH oxidase, is another important source. ROS can promote harmful oxidative damage to proteins, DNA, and lipids.9,68 On the other hand, H2O2 can oxidize cysteines and methionines to physiologically regulate protein function, including protein kinases and phosphatases. In effect, these modifications use ROS as a signaling mechanism and are reversible by thiol-disulfide and glutathione reductases.9,68 Electron transfer across the membrane by the leukocyte oxidase also has electrogenic effects that can increase neutrophil intracellular calcium levels,69 as well as alter the pH within phagosomes and the activity of digestive proteases.13,70
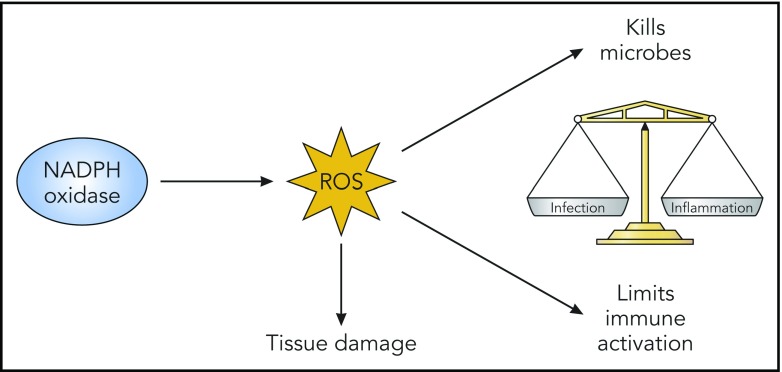
Thus, NADPH oxidase ROS can have multiple effects (Figure 2), including damaging oxidation that aids microbial killing, but it can be injurious to host tissue if oxidant production is not appropriately regulated or confined. Triggering of NOX2 ROS production has coevolved with activation of other immune responses, and it exerts immunoregulatory effects that balance immune activation (Figure 3). Although specific molecular targets are incompletely understood, a general theme is that deficiency of NOX2-derived ROS increases acute inflammatory responses and can also predispose to autoimmunity. Examples and current insights are summarized below.
Figure 2.
NADPH oxidase–derived ROS have beneficial and deleterious effects. NADPH oxidase–derived ROS have damaging oxidative effects that are important for microbial killing but can damage host tissues. In addition, derivative ROS have immunoregulatory effects, which act to balance immune responses that otherwise promote inflammation and even autoimmunity. Likely factors contributing to abnormal inflammation in the absence of NADPH oxidase ROS include impaired digestion of microbes or debris, increased proinflammatory cytokine production reflecting changes in redox-regulated signals, delayed clearance of inflammatory neutrophils, and altered antigen presentation. Professional illustration by Patrick Lane, ScEYEnce Studios.
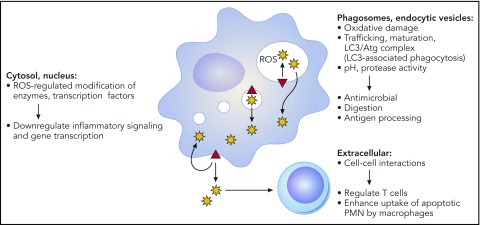
Figure 3.
NADPH oxidase–derived oxidants can influence multiple aspects of innate and adaptive immune responses. The phagocyte NADPH oxidase (red triangle) is assembled on the plasma membrane, phagosomes, and endocytic compartments. Superoxide is released inside membrane compartments or the extracellular space and is rapidly converted into derivative ROS. This includes dismutation to H2O2, which is membrane permeant and, thus, can diffuse into the cytosol. Oxidase-generated ROS can have many effects, depending on the site of ROS production, and, thus, can impact multiple pathways important for innate and adaptive immunity. See text for additional details. Professional illustration by Patrick Lane, ScEYEnce Studios.
Loss of NADPH oxidase ROS can alter redox modifications that otherwise regulate signaling and transcription factors. Proinflammatory NF-κB activity was increased in lipopolysaccharide- or zymosan-stimulated CGD macrophages, reflecting reduced oxidation of nuclear redox factor 1.71,72 CGD mouse neutrophils stimulated with fungal cell walls also exhibited increased phosphorylation of MAPKs and NF-κB activity.73 In both cell types, increased production of proinflammatory chemokines and other cytokines was observed. Activation of the transcription factor nuclear factory erythroid 2–related factor 2, which regulates protective oxidative stress–response genes following oxidation of its inhibitor Keap1, was reduced in zymosan-stimulated CGD mouse macrophages and human monocytes.71 CGD Epstein-Barr virus B-cell lines showed increased p38 mitogen–activated protein kinase activation and cytokine production upon stimulation with Toll-like receptor 7 or 9 agonists.74
NADPH oxidase deficiency is associated with an intrinsically enhanced IL-1 response to various agonists, including necrotic cell lysates, other damage associated molecular patterns (DAMPs), and uric acid crystals. IL-1 induces expression of many proinflammatory genes. Activated human CGD monocytes display increased production of IL-1α and IL-1β,45-47 with similar findings in mouse macrophages and bone marrow–derived dendritic cells.70,75 The underlying mechanism is not understood. One proposal is that enhanced IL-1 production and/or release in CGD reflects reduced activity of autophagy pathways,45 but this is unresolved.
Accumulation of microtubule-associated protein light chain 3 (LC3) on phagosomes, a form of noncanonical autophagy referred to as LC3-associated phagocytosis (LAP), is stimulated by NADPH oxidase ROS.76-78 Triggers of LAP in myeloid cells include microbial cell wall components, immunoglobulin-opsonized particles, and apoptotic cells. The autophagy proteins involved in LAP can accelerate or delay phagosome maturation and impact digestion, depending on the cell type and cargo.70,79 For example, binding and ingestion of apoptotic neutrophils (efferocytosis) activated the respiratory burst in inflammatory murine macrophages, which promoted acquisition of LC3 and rapid acquisition of vacuolar-type H+ ATPases mediating acidification.70 In turn, acidification facilitated efficient proteolysis of efferosome contents. These were impaired in CGD inflammatory macrophages. Defective macrophage LAP following efferocytosis was also associated with increased proinflammatory cytokine production by bone marrow–derived macrophages80 but not by inflammatory macrophages.70
Although LAP is also impaired in CGD neutrophils,76 whether this impacts events within neutrophil phagosomes is uncertain. Proteases and other compounds are delivered to neutrophil phagosomes by fusion with neutrophil granules, rather than the progressive remodeling by sequential fusion of different endocytic compartments as occurs in macrophages. Regulation of luminal pH also differs in neutrophils compared with macrophages.13 Neutrophil phagosomes initially maintain a neutral or even slightly alkaline pH because of their higher levels of NADPH oxidase activity, which consume luminal protons as superoxide dismutates to H2O2; ROS also inhibit V-ATPase accumulation on neutrophil phagosomes.81 Thus, in the absence of the NADPH oxidase, CGD neutrophil phagosomes acidify very rapidly,82,83 although the consequences are not well understood.
The NADPH oxidase can influence antigen presentation, a process that requires controlled degradation to preserve peptides for T-cell recognition. Proteolysis of antigens delivered on small particles was accelerated in mouse and human CGD dendritic cells and macrophages to reduce MHC-1 cross-presentation, which involves enhanced acidification and/or a more reductive environment that maintains cysteine protease activity.84-88 The impact of NADPH oxidase ROS also depends on the cargo. Delayed vacuolar-type H+ ATPase-mediated acidification of CGD macrophage efferosomes slowed digestion and increased cross-presentation of associated antigens.70 The NADPH oxidase also modulates class II processing and antigen repertoire in mouse macrophages and human Epstein-Barr virus B cells.89,90
Neutrophilic inflammation is prominent in CGD. In part, this reflects increased production of proinflammatory mediators by oxidase-deficient myeloid cells, which increases neutrophil recruitment. In addition, spontaneous apoptosis is delayed in oxidase-deficient neutrophils.91,92 Moreover, apoptotic CGD neutrophils generate reduced levels of cell surface lyso-phosphotidylserine,93,94 which otherwise enhances macrophage efferocytosis94 to remove dying cells prior to necrosis and release of DAMPs. An intrinsic impairment in CGD mouse macrophage efferocytosis was also reported in some,95 but not other,70 investigations.
Transcriptional changes driven by hypoxia-inducible factor (HIF) play important roles in regulating the inflammatory response.96 HIF expression triggered by tissue hypoxia at inflamed sites can be impacted by NADPH oxidase–deficient neutrophils as a result of their reduced consumption of oxygen in the absence of a respiratory burst. In an induced colitis model, an excessive infiltration of neutrophil inflammation in CGD mice could be abrogated by pharmacological stabilization of HIF within intestinal epithelial cells.97
The generation of neutrophil extracellular traps (NETs) is a form of neutrophil cell death associated with the release of DNA coated with various proteins into the extracellular environment.98 NETosis may contribute to host defense by trapping microbes, but it also can have deleterious proinflammatory effects. Whether alterations in NETosis contribute to dysregulated inflammation in CGD is unknown. NETosis can be regulated by the NADPH oxidase, particularly in response to microbial stimuli. However, human and mouse CGD neutrophils are capable of generating NETs in response to immune complexes and even spontaneously.64,99 Release of NETS in these settings may be mediated by increased neutrophil mitochondrial ROS, which were detected in lupus patients and some CGD patients.99 This is intriguing, because NETs are postulated to induce autoantibody formation, as well as activate production of type 1 interferon by dendritic cells.100 Hence, there could be a link between aberrant increased NETosis and discoid lupus, systemic lupus, and other autoimmune disease in NADPH oxidase deficiency.
Deficient NADPH oxidase ROS can affect T-cell–dependent inflammation and autoimmunity, although the mechanisms are incompletely understood. Many studies point to a role for NADPH oxidase–derived ROS in limiting T-cell activation in induced arthritis models. This may involve altered oxidation of the T-cell surface, antigen processing, or oxidation of presented autoantigens.101-103 Interestingly, mice with an NCF4 phosphatidylinositol 3-phosphate–binding mutation show enhanced susceptibility to collagen-induced arthritis but not to mannose-induced psoriatic arthritis, whereas NCF1-deficient mice are susceptible to both.104 This suggests that the effects of NADPH oxidase ROS can depend on the level and/or compartment in which they are generated. Other studies in mice support a role for macrophage and dendritic cell NADPH oxidase ROS to induce regulatory T-cell lymphocytes102,105 and suppress the production of interferon-γ, IL-12, and IL-17 by T cells.75,106 NADPH oxidase ROS are also reported to be important for myeloid-derived suppressor cell suppression of T-cell responses in tumor models.107
Given the many processes affected by NADPH oxidase, the etiology of the dysregulated inflammation and autoimmunity associated with NADPH oxidase deficiency is complex, influenced by the inciting agent, and often involves cross talk between different leukocytes. Altered responses by CGD monocytes and macrophages, including increased proinflammatory mediator production, likely play a central role. Restoring oxidase activity to macrophages and monocytes in NCF1-null mice using a CD68 transgene protected against fungal cell wall–induced inflammation and against increased susceptibility to induced arthritis, although the specific pathways responsible are not known.102,108,109 In peritoneal inflammation induced by endogenous DAMPs, increased IL-1α released by CGD sentinel peritoneal macrophages enhanced G-CSF expression, which rapidly mobilized greater numbers of marrow neutrophils for recruitment to the inflamed peritoneal cavity.70 This led to increased acute and prolonged peritoneal inflammation, which could be ameliorated by blocking IL-1α or G-CSF. Interestingly, prolonged peritoneal inflammation in CGD was also associated with impaired activation of invariant natural killer T lymphocytes by efferocytic macrophages, leading to reduced invariant natural killer T production of the proresolution cytokine IL-4.110 NADPH oxidase–deficient neutrophils themselves may also promote excessive inflammation by their increased production of inflammatory mediators, a prolonged lifespan at inflamed sites, and delayed clearance, as discussed earlier.
Management of infections and inflammatory complications in CGD
Management of patients with CGD includes the use of antimicrobials, as well as drugs targeting immune responses.4,5 Prophylactic trimethoprim/sulfamethoxazole (or, in sulfa-allergic patients, dicloxacillin or trimethoprim) and itraconazole, coupled with interferon-γ and aggressive treatment of acute infections and prolonged courses of antimicrobial treatment, have markedly reduced the frequency and severity of infections in CGD.4,111-114 X-linked CGD carriers with a low frequency of NADPH oxidase–positive cells may also benefit from antibiotic prophylaxis.37 Corticosteroids are used to treat clinically significant granulomatous or other inflammatory complications, including CGD-associated GI disease, although with caution because this may increase the risk of fungal infections.4,111 Fulminant pneumonia due to the inhalation of a large number of Aspergillus spores (“mulch pneumonitis”) is also managed with steroids, in addition to antifungal agents, to control the excessive inflammatory response.115 Corticosteroids have also emerged as an important component of treating staphylococcal liver abscesses in CGD, with improved outcomes and oftentimes the avoidance of invasive procedures for abscess drainage.116 TNF-α inhibitors can improve symptoms in CGD IBD but should be avoided because of their predisposing risk of infections.111 Treatment with anakinra, an IL-1 receptor antagonist, relieved symptoms in several CGD patients with colitis,45 but responses were poor or were not sustained in other patients.117 Hydroxychloroquine has been used to treat discoid lupus skin lesions.41 Macrophage activation syndrome and HLH in CGD have been treated with steroids and IV immunoglobulin.38 Because of its immunomodulatory and anti–TNF-α effects, thalidomide has been tried in a few patients with CGD-associated inflammation.118 Intriguingly, pioglitazone, a peroxisome proliferator-activated receptor γ agonist that is approved for type 2 diabetes increased mitochondrial oxidant production and bactericidal function in activated human and mouse CGD phagocytes.119 The increased generation of ROS by an alternative source could potentially benefit both defects in host defense and inflammation in CGD.
Allogeneic hematopoietic stem cell transplantation is curative for CGD, and reduced-intensity conditioning for allogeneic transplantation has emerged as an effective approach.120,121 Gene therapy targeted at autologous hematopoietic stem cells is also under active development.122,123 Currently, selection of patients for these approaches is based on the severity and frequency of infectious or inflammatory complications. Of note, refractory GI disease has been effectively treated with hematopoietic stem cell transplantation, including patients with NCF4 defects and a patient with CYBC1 deficiency.19,20
LAD
Adhesion of neutrophils to the endothelium, tissue matrix, and microbes is essential for their ability to emigrate into sites of infection and eliminate pathogens. Many of these interactions are mediated by integrin and selectin glycoproteins. LAD is a group of autosomal-recessive immunodeficiencies resulting from defects impacting integrin or selectin functions, leading to severe bacterial infections. The most common and first-described LAD subtype is LAD-1, caused by genetic defects in CD18, the common chain of the β2 integrin family, with several hundred patients reported.4,5,124 Patients present with recurrent severe infections, including deep tissue abscesses caused by S aureus or Gram-negative enteric organisms, and also have neutrophilia, but impaired formation of pus, as a result of adhesion and motility defects.
LAD-1 is associated with severe periodontitis, which had been attributed to impaired neutrophil surveillance of periodontal tissue. However, new studies in LAD-1 patients and mice identified a dysregulated IL-23/IL-17 inflammatory axis as the critical mediator of periodontal destruction, rather than bacterial load.125 This appears to reflect disruption of the “neutrostat,” a homeostatic mechanism for linking neutrophil production to disposal of senescent neutrophils in tissues.126,127 In this feedback loop, ingestion of apoptotic neutrophils by phagocytes suppresses their release of IL-23, which controls downstream production of IL-17 by lymphocytes and, in turn, G-CSF by fibroblasts and other cells.127 Because neutrophil emigration is impaired in LAD-1, these cytokines are all markedly increased in LAD-1, leading to the neutrophilia characteristic of LAD-1,127 and, in periodontal tissue, to pathologic IL-17 elevation and inflammatory periodontal bone loss.125 Moreover, compared with healthy individuals and those with aggressive periodontitis not associated with LAD-1, the subgingival microbiome of LAD-1 patients is altered, harboring microbial products that trigger IL-23–related inflammation.128 Taking advantage of these observations, an LAD-1 patient with severe periodontitis and a chronic sacral wound was recently treated with an antibody that blocks the activity of IL-23 and IL-12 and the downstream production of IL-17, which led to resolution of both complications.129
Concluding remarks
Inherited disorders affecting neutrophil function have illuminated cellular pathways that are important for effective control of bacterial and fungal pathogens, as well as for homeostasis, resolution of inflammation, and suppression of autoimmunity. The careful study of affected patients and animal models is leading to new insights into the underlying mechanisms of immune dysregulation and could improve therapeutic approaches for their management.
Acknowledgments
The author thanks Tina McGrath for assistance with manuscript preparation and apologizes to colleagues whose primary work was not cited because of space limitations.
This work was supported by grants from the National Institutes of Health, National Heart, Lung, and Blood Institute (R01HL045635) and the National Institutes of Health, National Institute of Arthritis and Musculoskeletal and Skin Diseases (R01AR072212) and by the Children’s Discovery Institute of Washington University and St. Louis Children’s Hospital.
Authorship
Contribution: M.C.D. reviewed the literature and wrote the manuscript.
Conflict-of-interest disclosure: The author declares no competing financial interests.
Correspondence: Mary C. Dinauer, Department of Pediatrics, Washington University School of Medicine in St. Louis, 660 S. Euclid Ave, Campus Box 8208, St. Louis, MO 63110; e-mail: mdinauer@wustl.edu.
REFERENCES
- 1.Schmidt RE, Grimbacher B, Witte T. Autoimmunity and primary immunodeficiency: two sides of the same coin? Nat Rev Rheumatol. 2017;14(1):7-18. [DOI] [PubMed] [Google Scholar]
- 2.Walter JE, Farmer JR, Foldvari Z, Torgerson TR, Cooper MA. Mechanism-based strategies for the management of autoimmunity and immune dysregulation in primary immunodeficiencies. J Allergy Clin Immunol Pract. 2016;4(6):1089-1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fischer A, Provot J, Jais JP, Alcais A, Mahlaoui N; members of the CEREDIH French PID study group. Autoimmune and inflammatory manifestations occur frequently in patients with primary immunodeficiencies. J Allergy Clin Immunol 2017;140(5):1388-1393.e8. [DOI] [PubMed]
- 4.Dinauer M, Newburger P, Borregaard N. Phagocyte system and disorders of granulopoiesis and granulocyte function. In: Orkin SH, Fisher DE, Ginsburg D, Look AT, Lux SE, Nathan DG, eds. Nathan and Oski’s Hematology of Infancy and Childhood. Philadelphia, PA: Elsevier/Saunders; 2015:773-847. [Google Scholar]
- 5.Dinauer MC. Primary immune deficiencies with defects in neutrophil function. Hematology Am Soc Hematol Educ Program. 2016;2016:43-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rieber N, Hector A, Kuijpers T, Roos D, Hartl D. Current concepts of hyperinflammation in chronic granulomatous disease. Clin Dev Immunol. 2012;2012:252460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Holmdahl R, Sareila O, Olsson LM, Bäckdahl L, Wing K. Ncf1 polymorphism reveals oxidative regulation of autoimmune chronic inflammation. Immunol Rev. 2016;269(1):228-247. [DOI] [PubMed] [Google Scholar]
- 8.Cachat J, Deffert C, Hugues S, Krause KH. Phagocyte NADPH oxidase and specific immunity. Clin Sci (Lond). 2015;128(10):635-648. [DOI] [PubMed] [Google Scholar]
- 9.Holmström KM, Finkel T. Cellular mechanisms and physiological consequences of redox-dependent signalling. Nat Rev Mol Cell Biol. 2014;15(6):411-421. [DOI] [PubMed] [Google Scholar]
- 10.Singel KL, Segal BH. NOX2-dependent regulation of inflammation. Clin Sci (Lond). 2016;130(7):479-490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Morgenstern DE, Gifford MA, Li LL, Doerschuk CM, Dinauer MC. Absence of respiratory burst in X-linked chronic granulomatous disease mice leads to abnormalities in both host defense and inflammatory response to Aspergillus fumigatus. J Exp Med. 1997;185(2):207-218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Olofsson P, Holmberg J, Tordsson J, Lu S, Akerström B, Holmdahl R. Positional identification of Ncf1 as a gene that regulates arthritis severity in rats. Nat Genet. 2003;33(1):25-32. [DOI] [PubMed] [Google Scholar]
- 13.Nunes P, Demaurex N, Dinauer MC. Regulation of the NADPH oxidase and associated ion fluxes during phagocytosis. Traffic. 2013;14(11):1118-1131. [DOI] [PubMed] [Google Scholar]
- 14.Thomas DC, Clare S, Sowerby JM, et al. Eros is a novel transmembrane protein that controls the phagocyte respiratory burst and is essential for innate immunity. J Exp Med. 2017;214(4):1111-1128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Winkelstein JA, Marino MC, Johnston RB Jr, et al. Chronic granulomatous disease. Report on a national registry of 368 patients. Medicine (Baltimore). 2000;79(3):155-169. [DOI] [PubMed] [Google Scholar]
- 16.Wolach B, Gavrieli R, de Boer M, et al. Chronic granulomatous disease in Israel: clinical, functional and molecular studies of 38 patients. Clin Immunol. 2008;129(1):103-114. [DOI] [PubMed] [Google Scholar]
- 17.Koker MY, Camcioglu Y, van Leeuwen K, et al. Clinical, functional, and genetic characterization of chronic granulomatous disease in 89 Turkish patients. J Allergy Clin Immunol 2013;132(5):1156-1163.e5. [DOI] [PubMed]
- 18.Matute JD, Arias AA, Wright NA, et al. A new genetic subgroup of chronic granulomatous disease with autosomal recessive mutations in p40 phox and selective defects in neutrophil NADPH oxidase activity. Blood. 2009;114(15):3309-3315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.van de Geer A, Nieto-Patlán A, Kuhns DB, et al. Inherited p40phox deficiency differs from classic chronic granulomatous disease. J Clin Invest. 2018;128(9):3957-3975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thomas DC, Charbonnier LM, Schejtman A, et al. EROS/CYBC1 mutations: decreased NADPH oxidase function and chronic granulomatous disease. J Allergy Clin Immunol. 2019;143(2):782-785.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Arnadottir GA, Norddahl GL, Gudmundsdottir S, et al. A homozygous loss-of-function mutation leading to CYBC1 deficiency causes chronic granulomatous disease. Nat Commun. 2018;9(1):4447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bagaitkar J, Barbu EA, Perez-Zapata LJ, et al. PI(3)P-p40phox binding regulates NADPH oxidase activation in mouse macrophages and magnitude of inflammatory responses in vivo. J Leukoc Biol. 2017;101(2):449-457. [DOI] [PubMed] [Google Scholar]
- 23.Raptaki M, Varela I, Spanou K, et al. Chronic granulomatous disease: a 25-year patient registry based on a multistep diagnostic procedure, from the referral center for primary immunodeficiencies in Greece [published correction appears in J Clin Immunol. 2014;34(8):1018]. J Clin Immunol. 2013;33(8):1302-1309. [DOI] [PubMed] [Google Scholar]
- 24.de Oliveira-Junior EB, Zurro NB, Prando C, et al. Clinical and genotypic spectrum of chronic granulomatous disease in 71 Latin American patients: first report from the LASID Registry. Pediatr Blood Cancer. 2015;62(12):2101-2107. [DOI] [PubMed] [Google Scholar]
- 25.Jones LB, McGrogan P, Flood TJ, et al. Special article: chronic granulomatous disease in the United Kingdom and Ireland: a comprehensive national patient-based registry. Clin Exp Immunol. 2008;152(2):211-218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Martire B, Rondelli R, Soresina A, et al. ; IPINET . Clinical features, long-term follow-up and outcome of a large cohort of patients with chronic granulomatous disease: an Italian multicenter study. Clin Immunol. 2008;126(2):155-164. [DOI] [PubMed] [Google Scholar]
- 27.van den Berg JM, van Koppen E, Ahlin A, et al. Chronic granulomatous disease: the European experience. PLoS One. 2009;4(4):e5234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Marciano BE, Spalding C, Fitzgerald A, et al. Common severe infections in chronic granulomatous disease. Clin Infect Dis. 2015;60(8):1176-1183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Henriet S, Verweij PE, Holland SM, Warris A. Invasive fungal infections in patients with chronic granulomatous disease. Adv Exp Med Biol. 2013;764:27-55. [DOI] [PubMed] [Google Scholar]
- 30.Dotis J, Pana ZD, Roilides E. Non-Aspergillus fungal infections in chronic granulomatous disease. Mycoses. 2013;56(4):449-462. [DOI] [PubMed] [Google Scholar]
- 31.Henrickson SE, Jongco AM, Thomsen KF, Garabedian EK, Thomsen IP. Noninfectious manifestations and complications of chronic granulomatous disease. J Pediatric Infect Dis Soc 2018;7(suppl 1):S18-S24. [DOI] [PMC free article] [PubMed]
- 32.Magnani A, Brosselin P, Beaute J, et al. Inflammatory manifestations in a single-center cohort of patients with chronic granulomatous disease. J Allergy Clin Immunol 2014;134(3):655-662.e8. [DOI] [PubMed]
- 33.Feld JJ, Hussain N, Wright EC, et al. Hepatic involvement and portal hypertension predict mortality in chronic granulomatous disease. Gastroenterology. 2008;134(7):1917-1926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Khangura SK, Kamal N, Ho N, et al. Gastrointestinal features of chronic granulomatous disease found during endoscopy. Clin Gastroenterol Hepatol 2016;14(3):395-402.e5. [DOI] [PMC free article] [PubMed]
- 35.Alimchandani M, Lai JP, Aung PP, et al. Gastrointestinal histopathology in chronic granulomatous disease: a study of 87 patients. Am J Surg Pathol. 2013;37(9):1365-1372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Marciano BE, Rosenzweig SD, Kleiner DE, et al. Gastrointestinal involvement in chronic granulomatous disease. Pediatrics. 2004;114(2):462-468. [DOI] [PubMed] [Google Scholar]
- 37.Marciano BE, Zerbe CS, Falcone EL, et al. X-linked carriers of chronic granulomatous disease: Illness, lyonization, and stability. J Allergy Clin Immunol. 2018;141(1):365-371. [DOI] [PubMed] [Google Scholar]
- 38.Bode SF, Ammann S, Al-Herz W, et al. ; Inborn Errors Working Party of the EBMT . The syndrome of hemophagocytic lymphohistiocytosis in primary immunodeficiencies: implications for differential diagnosis and pathogenesis. Haematologica. 2015;100(7):978-988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chinn IK, Eckstein OS, Peckham-Gregory EC, et al. Genetic and mechanistic diversity in pediatric hemophagocytic lymphohistiocytosis. Blood. 2018;132(1):89-100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Battersby AC, Cale AM, Goldblatt D, Gennery AR. Clinical manifestations of disease in X-linked carriers of chronic granulomatous disease. J Clin Immunol. 2013;33(8):1276-1284. [DOI] [PubMed] [Google Scholar]
- 41.Cale CM, Morton L, Goldblatt D. Cutaneous and other lupus-like symptoms in carriers of X-linked chronic granulomatous disease: incidence and autoimmune serology. Clin Exp Immunol. 2007;148(1):79-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kobayashi SD, Voyich JM, Braughton KR, et al. Gene expression profiling provides insight into the pathophysiology of chronic granulomatous disease. J Immunol. 2004;172(1):636-643. [DOI] [PubMed] [Google Scholar]
- 43.Kelkka T, Kienhöfer D, Hoffmann M, et al. Reactive oxygen species deficiency induces autoimmunity with type 1 interferon signature. Antioxid Redox Signal. 2014;21(16):2231-2245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gabrion A, Hmitou I, Moshous D, et al. Mammalian target of rapamycin inhibition counterbalances the inflammatory status of immune cells in patients with chronic granulomatous disease. J Allergy Clin Immunol. 2017;139(5):1641-1649.e6. [DOI] [PubMed] [Google Scholar]
- 45.de Luca A, Smeekens SP, Casagrande A, et al. IL-1 receptor blockade restores autophagy and reduces inflammation in chronic granulomatous disease in mice and in humans. Proc Natl Acad Sci USA. 2014;111(9):3526-3531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.van de Veerdonk FL, Smeekens SP, Joosten LA, et al. Reactive oxygen species-independent activation of the IL-1beta inflammasome in cells from patients with chronic granulomatous disease. Proc Natl Acad Sci USA. 2010;107(7):3030-3033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Meissner F, Seger RA, Moshous D, Fischer A, Reichenbach J, Zychlinsky A. Inflammasome activation in NADPH oxidase defective mononuclear phagocytes from patients with chronic granulomatous disease. Blood. 2010;116(9):1570-1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lekstrom-Himes JA, Kuhns DB, Alvord WG, Gallin JI. Inhibition of human neutrophil IL-8 production by hydrogen peroxide and dysregulation in chronic granulomatous disease. J Immunol. 2005;174(1):411-417. [DOI] [PubMed] [Google Scholar]
- 49.Yu JE, De Ravin SS, Uzel G, et al. High levels of Crohn’s disease-associated anti-microbial antibodies are present and independent of colitis in chronic granulomatous disease. Clin Immunol. 2011;138(1):14-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Baghdasraian E, Coates TD, Harb R, Church, JA. Serologic assessment for inflammatory bowel disease in patients with chronic granulomatous disease. Pediatr Allergy Immunol Pulmonol. 2010;23(4):261-263. [Google Scholar]
- 51.Kuhns DB, Alvord WG, Heller T, et al. Residual NADPH oxidase and survival in chronic granulomatous disease. N Engl J Med. 2010;363(27):2600-2610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Foster CB, Lehrnbecher T, Mol F, et al. Host defense molecule polymorphisms influence the risk for immune-mediated complications in chronic granulomatous disease. J Clin Invest. 1998;102(12):2146-2155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Huang C, De Ravin SS, Paul AR, et al. ; NIDDK IBD Genetics Consortium . Genetic risk for inflammatory bowel disease is a determinant of Crohn’s disease development in chronic granulomatous disease. Inflamm Bowel Dis. 2016;22(12):2794-2801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Falcone EL, Abusleme L, Swamydas M, et al. Colitis susceptibility in p47(phox−/−) mice is mediated by the microbiome. Microbiome. 2016;4(1):13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jacob CO, Eisenstein M, Dinauer MC, et al. Lupus-associated causal mutation in neutrophil cytosolic factor 2 (NCF2) brings unique insights to the structure and function of NADPH oxidase. Proc Natl Acad Sci USA. 2012;109(2):E59-E67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Dhillon SS, Fattouh R, Elkadri A, et al. Variants in nicotinamide adenine dinucleotide phosphate oxidase complex components determine susceptibility to very early onset inflammatory bowel disease. Gastroenterology 2014;147(3):680-689.e2. [DOI] [PubMed]
- 57.Muise AM, Xu W, Guo C-H, et al. ; NEOPICS . NADPH oxidase complex and IBD candidate gene studies: identification of a rare variant in NCF2 that results in reduced binding to RAC2 [published correction appears in Gut. 2013;62(10):1432]. Gut. 2012;61(7):1028-1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Zhong J, Olsson LM, Urbonaviciute V, Yang M, Bäckdahl L, Holmdahl R. Association of NOX2 subunits genetic variants with autoimmune diseases. Free Radic Biol Med. 2018;125:72-80. [DOI] [PubMed] [Google Scholar]
- 59.Olsson LM, Johansson AC, Gullstrand B, et al. A single nucleotide polymorphism in the NCF1 gene leading to reduced oxidative burst is associated with systemic lupus erythematosus. Ann Rheum Dis. 2017;76(9):1607-1613. [DOI] [PubMed] [Google Scholar]
- 60.Zhao J, Ma J, Deng Y, et al. A missense variant in NCF1 is associated with susceptibility to multiple autoimmune diseases. Nat Genet. 2017;49(3):433-437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Armstrong DL, Eisenstein M, Zidovetzki R, Jacob CO. Systemic lupus erythematosus-associated neutrophil cytosolic factor 2 mutation affects the structure of NADPH oxidase complex. J Biol Chem. 2015;290(20):12595-12602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Li XJ, Marchal CC, Stull ND, Stahelin RV, Dinauer MC. p47phox Phox homology domain regulates plasma membrane but not phagosome neutrophil NADPH oxidase activation. J Biol Chem. 2010;285(45):35169-35179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Fodil N, Langlais D, Gros P. Primary immunodeficiencies and inflammatory disease: a growing genetic intersection. Trends Immunol. 2016;37(2):126-140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Jacob CO, Yu N, Yoo DG, et al. Haploinsufficiency of NADPH oxidase subunit neutrophil cytosolic factor 2 is sufficient to accelerate full-blown lupus in NZM 2328 mice. Arthritis Rheumatol. 2017;69(8):1647-1660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kienhöfer D, Hahn J, Stoof J, et al. Experimental lupus is aggravated in mouse strains with impaired induction of neutrophil extracellular traps. JCI Insight. 2017;2(10):92920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Campbell AM, Kashgarian M, Shlomchik MJ. NADPH oxidase inhibits the pathogenesis of systemic lupus erythematosus. Science Transl Med 2012;4(157):157ra141. [DOI] [PMC free article] [PubMed]
- 67.Al Ghouleh I, Khoo NK, Knaus UG, et al. Oxidases and peroxidases in cardiovascular and lung disease: new concepts in reactive oxygen species signaling. Free Radic Biol Med. 2011;51(7):1271-1288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hoffmann MH, Griffiths HR. The dual role of reactive oxygen species in autoimmune and inflammatory diseases: evidence from preclinical models. Free Radic Biol Med. 2018;125:62-71. [DOI] [PubMed] [Google Scholar]
- 69.Geiszt M, Kapus A, Német K, Farkas L, Ligeti E. Regulation of capacitative Ca2+ influx in human neutrophil granulocytes. Alterations in chronic granulomatous disease. J Biol Chem. 1997;272(42):26471-26478. [DOI] [PubMed] [Google Scholar]
- 70.Bagaitkar J, Huang J, Zeng MY, et al. NADPH oxidase activation regulates apoptotic neutrophil clearance by murine macrophages. Blood. 2018;131(21):2367-2378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Segal BH, Han W, Bushey JJ, et al. NADPH oxidase limits innate immune responses in the lungs in mice. PLoS One. 2010;5(3):e9631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Han W, Li H, Cai J, et al. NADPH oxidase limits lipopolysaccharide-induced lung inflammation and injury in mice through reduction-oxidation regulation of NF-κB activity. J Immunol. 2013;190(9):4786-4794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Endo D, Fujimoto K, Hirose R, et al. Genetic phagocyte NADPH oxidase deficiency enhances nonviable Candida albicans-induced inflammation in mouse lungs. Inflammation. 2017;40(1):123-135. [DOI] [PubMed] [Google Scholar]
- 74.McLetchie S, Volpp BD, Dinauer MC, Blum JS. Hyper-responsive Toll-like receptor 7 and 9 activation in NADPH oxidase-deficient B lymphoblasts. Immunology. 2015;146(4):595-606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Cachat J, Deffert C, Alessandrini M, et al. Altered humoral immune responses and IgG subtypes in NOX2-deficient mice and patients: a key role for NOX2 in antigen-presenting cells. Front Immunol. 2018;9:1555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Huang J, Canadien V, Lam GY, et al. Activation of antibacterial autophagy by NADPH oxidases. Proc Natl Acad Sci USA. 2009;106(15):6226-6231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ma J, Becker C, Lowell CA, Underhill DM. Dectin-1-triggered recruitment of light chain 3 protein to phagosomes facilitates major histocompatibility complex class II presentation of fungal-derived antigens. J Biol Chem. 2012;287(41):34149-34156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Martinez J, Malireddi RK, Lu Q, et al. Molecular characterization of LC3-associated phagocytosis reveals distinct roles for Rubicon, NOX2 and autophagy proteins. Nat Cell Biol. 2015;17(7):893-906. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 79.Cemma M, Grinstein S, Brumell JH. Autophagy proteins are not universally required for phagosome maturation. Autophagy 2016;12(9):1440-1446. [DOI] [PMC free article] [PubMed]
- 80.Martinez J, Cunha LD, Park S, et al. Noncanonical autophagy inhibits the autoinflammatory, lupus-like response to dying cells [published correction appears in Nature. 2016;539(7627):124] Nature. 2016;533(7601):115-119. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 81.Jankowski A, Scott CC, Grinstein S. Determinants of the phagosomal pH in neutrophils. J Biol Chem. 2002;277(8):6059-6066. [DOI] [PubMed] [Google Scholar]
- 82.Jankowski A, Grinstein S. Modulation of the cytosolic and phagosomal pH by the NADPH oxidase. Antioxid Redox Signal. 2002;4(1):61-68. [DOI] [PubMed] [Google Scholar]
- 83.Segal AW, Geisow M, Garcia R, Harper A, Miller R. The respiratory burst of phagocytic cells is associated with a rise in vacuolar pH. Nature. 1981;290(5805):406-409. [DOI] [PubMed] [Google Scholar]
- 84.Gardiner GJ, Deffit SN, McLetchie S, Pérez L, Walline CC, Blum JS. A role for NADPH oxidase in antigen presentation. Front Immunol. 2013;4:295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Rybicka JM, Balce DR, Chaudhuri S, Allan ER, Yates RM. Phagosomal proteolysis in dendritic cells is modulated by NADPH oxidase in a pH-independent manner. EMBO J. 2012;31(4):932-944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Rybicka JM, Balce DR, Khan MF, Krohn RM, Yates RM. NADPH oxidase activity controls phagosomal proteolysis in macrophages through modulation of the lumenal redox environment of phagosomes. Proc Natl Acad Sci USA. 2010;107(23):10496-10501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Mantegazza AR, Savina A, Vermeulen M, et al. NADPH oxidase controls phagosomal pH and antigen cross-presentation in human dendritic cells. Blood. 2008;112(12):4712-4722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Savina A, Jancic C, Hugues S, et al. NOX2 controls phagosomal pH to regulate antigen processing during crosspresentation by dendritic cells. Cell. 2006;126(1):205-218. [DOI] [PubMed] [Google Scholar]
- 89.Crotzer VL, Matute JD, Arias AA, et al. Cutting edge: NADPH oxidase modulates MHC class II antigen presentation by B cells. J Immunol. 2012;189(8):3800-3804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Allan ERO, Tailor P, Balce DR, et al. NADPH oxidase modifies patterns of MHC class II-restricted epitopic repertoires through redox control of antigen processing. J Immunol. 2014;192(11):4989-5001. [DOI] [PubMed] [Google Scholar]
- 91.Fadeel B, Ahlin A, Henter JI, Orrenius S, Hampton MB. Involvement of caspases in neutrophil apoptosis: regulation by reactive oxygen species. Blood. 1998;92(12):4808-4818. [PubMed] [Google Scholar]
- 92.Kasahara Y, Iwai K, Yachie A, et al. Involvement of reactive oxygen intermediates in spontaneous and CD95 (Fas/APO-1)-mediated apoptosis of neutrophils. Blood. 1997;89(5):1748-1753. [PubMed] [Google Scholar]
- 93.Frasch SC, Berry KZ, Fernandez-Boyanapalli R, et al. NADPH oxidase-dependent generation of lysophosphatidylserine enhances clearance of activated and dying neutrophils via G2A. J Biol Chem. 2008;283(48):33736-33749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Frasch SC, Fernandez-Boyanapalli RF, Berry KZ, et al. Signaling via macrophage G2A enhances efferocytosis of dying neutrophils by augmentation of Rac activity. J Biol Chem. 2011;286(14):12108-12122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Fernandez-Boyanapalli RF, Frasch SC, McPhillips K, et al. Impaired apoptotic cell clearance in CGD due to altered macrophage programming is reversed by phosphatidylserine-dependent production of IL-4. Blood. 2009;113(9):2047-2055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Taylor CT, Colgan SP. Regulation of immunity and inflammation by hypoxia in immunological niches. Nat Rev Immunol. 2017;17(12):774-785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Campbell EL, Bruyninckx WJ, Kelly CJ, et al. Transmigrating neutrophils shape the mucosal microenvironment through localized oxygen depletion to influence resolution of inflammation. Immunity. 2014;40(1):66-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Nauseef WM, Kubes P. Pondering neutrophil extracellular traps with healthy skepticism. Cell Microbiol. 2016;18(10):1349-1357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Lood C, Blanco LP, Purmalek MM, et al. Neutrophil extracellular traps enriched in oxidized mitochondrial DNA are interferogenic and contribute to lupus-like disease. Nat Med. 2016;22(2):146-153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Jorch SK, Kubes P. An emerging role for neutrophil extracellular traps in noninfectious disease. Nat Med. 2017;23(3):279-287. [DOI] [PubMed] [Google Scholar]
- 101.Yang M, Haase C, Viljanen J, et al. Cutting edge: processing of oxidized peptides in macrophages regulates T cell activation and development of autoimmune arthritis. J Immunol. 2017;199(12):3937-3942. [DOI] [PubMed] [Google Scholar]
- 102.Gelderman KA, Hultqvist M, Pizzolla A, et al. Macrophages suppress T cell responses and arthritis development in mice by producing reactive oxygen species. J Clin Invest. 2007;117(10):3020-3028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Gelderman KA, Hultqvist M, Holmberg J, Olofsson P, Holmdahl R. T cell surface redox levels determine T cell reactivity and arthritis susceptibility. Proc Natl Acad Sci USA. 2006;103(34):12831-12836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Winter S, Hultqvist Hopkins M, Laulund F, Holmdahl R. A reduction in intracellular reactive oxygen species due to a mutation in NCF4 promotes autoimmune arthritis in mice. Antioxid Redox Signal. 2016;25(18):983-996. [DOI] [PubMed] [Google Scholar]
- 105.Kraaij MD, Savage ND, van der Kooij SW, et al. Induction of regulatory T cells by macrophages is dependent on production of reactive oxygen species. Proc Natl Acad Sci USA. 2010;107(41):17686-17691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.George-Chandy A, Nordström I, Nygren E, et al. Th17 development and autoimmune arthritis in the absence of reactive oxygen species. Eur J Immunol. 2008;38(4):1118-1126. [DOI] [PubMed] [Google Scholar]
- 107.Corzo CA, Cotter MJ, Cheng P, et al. Mechanism regulating reactive oxygen species in tumor-induced myeloid-derived suppressor cells. J Immunol. 2009;182(9):5693-5701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Grimm MJ, Vethanayagam RR, Almyroudis NG, et al. Monocyte- and macrophage-targeted NADPH oxidase mediates antifungal host defense and regulation of acute inflammation in mice. J Immunol. 2013;190(8):4175-4184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Deffert C, Carnesecchi S, Yuan H, et al. Hyperinflammation of chronic granulomatous disease is abolished by NOX2 reconstitution in macrophages and dendritic cells. J Pathol. 2012;228(3):341-350. [DOI] [PubMed] [Google Scholar]
- 110.Zeng MY, Pham D, Bagaitkar J, et al. An efferocytosis-induced, IL-4-dependent macrophage-iNKT cell circuit suppresses sterile inflammation and is defective in murine CGD. Blood. 2013;121(17):3473-3483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Thomsen IP, Smith MA, Holland SM, Creech CB. A Comprehensive approach to the management of children and adults with chronic granulomatous disease. J Allergy Clin Immunol Pract. 2016;4(6):1082-1088. [DOI] [PubMed] [Google Scholar]
- 112.A controlled trial of interferon gamma to prevent infection in chronic granulomatous disease. The International Chronic Granulomatous Disease Cooperative Study Group. N Engl J Med 1991;324(8):509-516. [DOI] [PubMed]
- 113.Marciano BE, Wesley R, De Carlo ES, et al. Long-term interferon-gamma therapy for patients with chronic granulomatous disease. Clin Infect Dis. 2004;39(5):692-699. [DOI] [PubMed] [Google Scholar]
- 114.Gallin JI, Alling DW, Malech HL, et al. Itraconazole to prevent fungal infections in chronic granulomatous disease. N Engl J Med. 2003;348(24):2416-2422. [DOI] [PubMed] [Google Scholar]
- 115.Siddiqui S, Anderson VL, Hilligoss DM, et al. Fulminant mulch pneumonitis: an emergency presentation of chronic granulomatous disease. Clin Infect Dis. 2007;45(6):673-681. [DOI] [PubMed] [Google Scholar]
- 116.Straughan DM, McLoughlin KC, Mullinax JE, et al. The changing paradigm of management of liver abscesses in chronic granulomatous disease. Clin Infect Dis. 2018;66(9):1427-1434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Hahn KJ, Ho N, Yockey L, et al. Treatment with anakinra, a recombinant IL-1 receptor antagonist, unlikely to induce lasting remission in patients with CGD colitis. Am J Gastroenterol. 2015;110(6):938-939. [DOI] [PubMed] [Google Scholar]
- 118.Yang CS, Kim C, Antaya RJ. Review of thalidomide use in the pediatric population. J Am Acad Dermatol. 2015;72(4):703-711. [DOI] [PubMed] [Google Scholar]
- 119.Fernandez-Boyanapalli RF, Frasch SC, Thomas SM, et al. Pioglitazone restores phagocyte mitochondrial oxidants and bactericidal capacity in chronic granulomatous disease. J Allergy Clin Immunol 2015;135(2):517-527.e2. [DOI] [PMC free article] [PubMed]
- 120.Güngör T, Teira P, Slatter M, et al. ; Inborn Errors Working Party of the European Society for Blood and Marrow Transplantation . Reduced-intensity conditioning and HLA-matched haemopoietic stem-cell transplantation in patients with chronic granulomatous disease: a prospective multicentre study. Lancet. 2014;383(9915):436-448. [DOI] [PubMed] [Google Scholar]
- 121.Morillo-Gutierrez B, Beier R, Rao K, et al. Treosulfan-based conditioning for allogeneic HSCT in children with chronic granulomatous disease: a multicenter experience. Blood. 2016;128(3):440-448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Kuo CY, Kohn DB. Gene therapy for the treatment of primary immune deficiencies. Curr Allergy Asthma Rep. 2016;16(5):39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Booth C, Gaspar HB, Thrasher AJ. Treating immunodeficiency through HSC gene therapy. Trends Mol Med. 2016;22(4):317-327. [DOI] [PubMed] [Google Scholar]
- 124.van de Vijver E, van den Berg TK, Kuijpers TW. Leukocyte adhesion deficiencies. Hematol Oncol Clin North Am. 2013;27(1):101-116, viii. [DOI] [PubMed] [Google Scholar]
- 125.Moutsopoulos NM, Konkel J, Sarmadi M, et al. Defective neutrophil recruitment in leukocyte adhesion deficiency type I disease causes local IL-17-driven inflammatory bone loss. Sci Transl Med. 2014;6(229):229ra40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Christopher MJ, Link DC. Regulation of neutrophil homeostasis. Curr Opin Hematol. 2007;14(1):3-8. [DOI] [PubMed] [Google Scholar]
- 127.Stark MA, Huo Y, Burcin TL, Morris MA, Olson TS, Ley K. Phagocytosis of apoptotic neutrophils regulates granulopoiesis via IL-23 and IL-17. Immunity. 2005;22(3):285-294. [DOI] [PubMed] [Google Scholar]
- 128.Moutsopoulos NM, Chalmers NI, Barb JJ, et al. Subgingival microbial communities in leukocyte adhesion deficiency and their relationship with local immunopathology [published correction appears in PLoS Pathog. 2015;11(4):e1004860]. PLoS Pathog. 2015;11(3):e1004698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Moutsopoulos NM, Zerbe CS, Wild T, et al. Interleukin-12 and interleukin-23 blockade in leukocyte adhesion deficiency type 1. N Engl J Med. 2017;376(12):1141-1146. [DOI] [PMC free article] [PubMed] [Google Scholar]