Abstract
Background The efficacy and safety of the direct oral anticoagulants (DOACs) in fragile patients (age ≥ 75 years and/or creatinine clearance levels ≤ 50 mL/min and/or body weight ≤ 50kg) with venous thromboembolism (VTE) has not been evaluated.
Methods We used the RIETE database to compare the rates of the composite of VTE recurrences or major bleeding during anticoagulation in fragile patients with VTE, according to the use of DOACs or standard anticoagulant therapy.
Results From January 2013 to April 2018, 24,701 patients were recruited. Of these, 10,054 (41%) were fragile. Initially, 473 fragile patients (4.7%) received DOACs and 8,577 (85%) low-molecular-weight heparin (LMWH). For long-term therapy, 1,298 patients (13%) received DOACs and 5,038 (50%) vitamin K antagonists (VKAs). Overall, 95 patients developed VTE recurrences and 262 had major bleeding. Patients initially receiving DOACs had a lower rate of the composite outcome (hazard ratio [HR]: 0.32; 95% confidence interval [CI]: 0.08–0.88) than those on LMWH. Patients receiving DOACs for long-term therapy had a nonsignificantly lower rate of the composite outcome (HR: 0.70; 95% CI: 0.46–1.03) than those on VKAs. On multivariable analysis, patients initially receiving DOACs had a nonsignificantly lower risk for the composite outcome (HR: 0.36; 95% CI: 0.11–1.15) than those on LMWH, while those receiving DOACs for long-term therapy had a significantly lower risk (HR: 0.61; 95% CI: 0.41–0.92) than those on VKAs.
Conclusions Our data suggest that the use of DOACs may be more effective and safe than standard therapy in fragile patients with VTE, a subgroup of patients where the risk for bleeding is particularly high.
Keywords: venous thromboembolism, fragile patients, direct oral anticoagulants
Introduction
Subgroup analyses from randomized clinical trials suggested that the direct oral anticoagulants (DOACs) may have some advantages over standard therapy in fragile patients with venous thromboembolism (VTE). In the EINSTEIN trials, the rate of major bleeding was much lower in fragile patients receiving rivaroxaban than in those on standard therapy. 1 This difference was not seen in nonfragile patients. Besides, the HOKUSAI trial found a higher efficacy using edoxaban than warfarin in fragile patients, without any safety concern. 2 Fragile patients are underrepresented in clinical trials, and these favorable results have not been validated yet in real life. In a recent study, we found that 42% of VTE patients in real life are fragile, 3 and that during anticoagulation they had fewer VTE recurrences and more major bleeding events than the nonfragile.
The RIETE (Registro Informatizado de Enfermedad TromboEmbólica) registry is an ongoing, multicenter registry of consecutive patients with acute VTE with 223 collaborating centers in the Americas, Asia, and Europe (ClinicalTrials.gov identifier: NCT02832245). Since its inception in 2001, the aim of RIETE was to record data including the clinical characteristics, treatment patterns, and outcomes in patients diagnosed with VTE. 4 5 6 7 Using the RIETE database, the current study aimed to compare the outcomes during anticoagulation in fragile patients with VTE, according to the use of DOACs or standard anticoagulant therapy.
Patients and Methods
Consecutive patients presenting with symptomatic, acute deep vein thrombosis (DVT) or pulmonary embolism (PE) confirmed by objective tests (compression ultrasonography or contrast venography for DVT; helical computed tomography [CT] scan, ventilation-perfusion lung scintigraphy, or angiography for PE) were enrolled in RIETE. Patients were excluded if they were currently participating in a therapeutic clinical trial with a blinded therapy. The rationale, design, and methodology of RIETE have been reported elsewhere. 8
Study Design
We conducted a retrospective study of prospectively collected data from consecutive patients with acute VTE enrolled in the RIETE registry. Data were collected from January 2013 to April 2018, corresponding to the time when the prescription of DOACs was allowed. The major outcome was the composite of VTE recurrences or major bleeding events appearing during therapy. Comparisons were made separately for initial (DOACs vs. low-molecular-weight heparin [LMWH]) and for long-term therapy (DOACs vs. vitamin K antagonists [VKAs]).
For initial therapy, patients receiving DOACs were considered to receive the recommended therapy if they started within the first 48 hours after VTE diagnosis and were prescribed rivaroxaban 15 mg twice daily for 21 ± 2 days or apixaban 10 mg twice daily for 7 ± 2 days. For long-term therapy, patients were considered to receive the recommended doses if they were prescribed rivaroxaban 20 mg once daily; apixaban 5 mg twice daily; dabigatran 150 mg twice daily or edoxaban 60 mg once daily.
Definitions
Fragile patients were defined as those having age ≥75 years, creatinine clearance (CrCl) levels ≤50 mL/min, or body weight ≤50 kg, as previously reported. Immobilized patients were defined as nonsurgical patients who had been immobilized (i.e., total bed rest with bathroom privileges) for ≥4 days in the 2-month period prior to VTE. Surgical patients were defined as those who underwent a surgical intervention in the 2 months prior to VTE. Active cancer was defined as newly diagnosed cancer, metastatic cancer, or cancer that was being treated (i.e., surgery, chemotherapy, radiotherapy, support therapy). Recent bleeding was defined as any major bleeding episode <30 days prior to VTE. Initial therapy was defined as any therapy administered during the first week in the case of LMWH or apixaban, and during the first 3 weeks in the case of rivaroxaban. Long-term therapy was defined as any therapy administered after the end of initial therapy. Bleeding events were classified as “major” if they were overt and required a transfusion of two units or more of blood, or were retroperitoneal, spinal or intracranial, or when they were fatal. Fatal bleeding was defined as any death occurring within 10 days of a major bleeding episode, in the absence of an alternative cause of death. Fatal PE, in the absence of autopsy, was defined as any death appearing within 10 days after symptomatic PE diagnosis, in the absence of any alternative cause of death.
Treatment and Follow-up
Patients were managed according to each participating hospital's clinical practice, and there were no standardized or recommended duration of therapy or follow-up. All patients had to be followed up for at least 3 months in the outpatient clinic or physician's office. During each visit, any signs or symptoms suggesting VTE recurrences or bleeding complications were noted. Each episode of clinically suspected recurrent VTE was investigated by repeat compression ultrasonography, lung scanning, helical CT scan, or pulmonary angiography, as appropriate. Most outcomes were classified as reported by the clinical centers. However, if staff at the coordinating center were uncertain how to classify a reported outcome, that event was reviewed by a central adjudicating committee (less than 10% of events).
Statistical Analysis
Categorical variables were compared using the chi-square test (two-sided) and Fisher's exact test (two-sided). Continuous variables were compared using Student t -test. Hazard ratios (HRs) and corresponding 95% confidence intervals (CIs) were calculated. Incidence rates were calculated as cumulative incidence (events/100 patient-years) and compared using the HRs and 95% CI. Cox proportional hazard models were used to compare the rates of the composite outcome of VTE recurrences or major bleeding occurring during initial and long-term therapy, separately. Crude and adjusted HRs as well as their 95% CIs were estimated. Covariates included in the adjusted model were those for which a statistically significant difference (a threshold p -value of 0.1 was set to assess significance of differences) was found between the different drugs, and a backward selection was used for the covariate selection in the multivariable model. Statistical analyses were conducted with SPSS for Windows Release 20.0 (SPSS Inc., Chicago, Illinois, United States).
Role of the Funding Source
The sponsors of the RIETE registry (Sanofi and Bayer) had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
From January 2013 to April 2018, 24,701 patients with acute VTE were recruited in RIETE. Of these, 10,054 (41%) were fragile ( Fig. 1 ). Initially, 473 fragile patients (4.7%) received DOACs (rivaroxaban 382, apixaban 91) and 8,577 (85%) were prescribed LMWH. Then, 1,298 patients (13%) switched to DOACs for long-term therapy (rivaroxaban 844, apixaban 344, dabigatran 69, edoxaban 41) and 5,038 (50%) to VKAs.
Fig. 1.
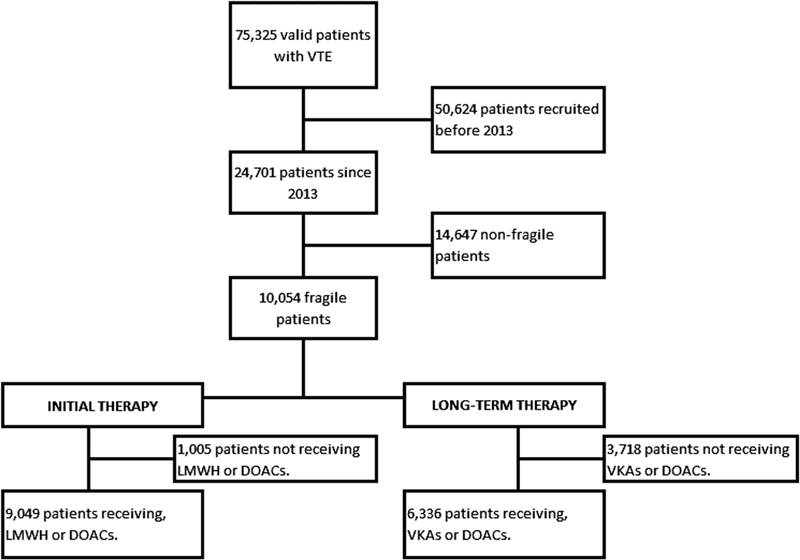
Flowchart of the patients.
For initial therapy, patients receiving DOACs were 2 years younger than those treated with LMWH, less likely presented with PE (as compared with DVT), and were less likely to have cancer, anemia, or renal insufficiency, but were more likely to have unprovoked VTE, prior VTE, chronic heart failure, or to receive corticosteroids at baseline ( Table 1 ). Median duration of initial therapy with rivaroxaban, apixaban, or LMWH was 23, 9, and 10 days, respectively ( Table 2 ). Most patients received the recommended doses of DOACs (rivaroxaban 91%, apixaban 74%). Many patients receiving nonrecommended doses had recent major bleeding, severe renal insufficiency, liver failure, or thrombocytopenia. For long-term therapy, patients receiving DOACs were less likely to have renal insufficiency and more likely to have prior VTE, chronic heart failure, or recent major bleeding than those on long-term VKAs ( Table 1 ). Median duration of therapy with DOACs was half that of VKAs (96 vs. 172 days, respectively) and the proportion of patients receiving the recommended doses of DOACs was: rivaroxaban 65%, apixaban 68%, dabigatran 55%, and edoxaban 61%. Again, many patients receiving nonrecommended doses had recent major bleeding, severe renal insufficiency, liver failure, or thrombocytopenia.
Table 1. Clinical characteristics of the patients, according to initial therapy with LMWH or DOACs.
| Initial therapy | Long-term therapy | |||
|---|---|---|---|---|
| DOACs | LMWH | DOACs | VKAs | |
| Patients, N | 473 | 8,577 | 1,298 | 5,038 |
| Clinical characteristics | ||||
| Male gender | 176 (37%) | 3,291 (38%) | 481 (37%) | 1,917 (38%) |
| Mean age (years ± SD) | 78 ± 11 a | 80 ± 10 | 79 ± 9.9 | 80 ± 9.6 |
| Age ≥ 75 y | 417 (88%) | 7,539 (88%) | 1,170 (90%) | 4,497 (89%) |
| Body weight (kg ± SD) | 72 ± 14 | 71 ± 14 | 72 ± 15 | 72 ± 14 |
| Body weight ≤ 50 kg | 36 (7.6%) | 780 (9.1%) | 103 (7.9%) | 324 (6.4%) |
| Initial VTE presentation | ||||
| Pulmonary embolism | 242 (51%) a | 4,932 (58%) | 795 (61%) | 3,156 (63%) |
| Risk factors for VTE | ||||
| Immobilization ≥ 4 d | 133 (28%) | 2,229 (26%) | 307 (24%) | 1,162 (23%) |
| Surgery | 40 (8.5%) | 661 (7.7%) | 103 (7.9%) | 361 (7.2%) |
| Cancer | 66 (14%) b | 2,168 (25%) | 157 (12%) | 626 (12%) |
| Estrogen use | 12 (2.5%) | 292 (3.4%) | 41 (3.2%) | 129 (2.6%) |
| Pregnancy/postpartum | 0 | 14 (0.16%) | 1 (0.08%) | 6 (0.12%) |
| None of the above | 251 (53%) c | 4,060 (47%) | 755 (58%) | 3,011 (60%) |
| Prior VTE | 83 (18%) c | 1,143 (13%) | 232 (18%) a | 739 (15%) |
| Underlying diseases | ||||
| Chronic heart failure | 79 (17%) b | 932 (11%) | 184 (14%) b | 543 (11%) |
| Chronic lung disease | 77 (16%) | 1,288 (15%) | 183 (14%) | 786 (16%) |
| Recent major bleeding | 9 (1.9%) | 215 (2.5%) | 38 (2.9%) b | 56 (1.1%) |
| Blood tests at baseline | ||||
| Anemia | 144 (31%) b | 3,488 (41%) | 420 (32%) | 1,649 (33%) |
| Platelet count < 100,000/µL | 5 (1.1%) c | 238 (2.8%) | 17 (1.3%) | 109 (2.2%) |
| CrCl levels (mL/min ± SD) | 60 ± 21 b | 55 ± 24 | 59 ± 21 b | 54 ± 23 |
| CrCl levels ≤50 mL/min | 169 (36%) b | 4,185 (49%) | 496 (38%) b | 2,479 (49%) |
| Concomitant drugs | ||||
| Corticosteroids | 74 (16%) a | 977 (11%) | 135 (10%) | 512 (10%) |
| Antiplatelets | 134 (28%) | 2,300 (27%) | 340 (26%) | 1,362 (27%) |
| NSAIDs | 38 (8.1%) | 665 (7.8%) | 98 (7.6%) | 390 (7.7%) |
Abbreviations: CrCl, creatinine clearance; DOACs, direct oral anticoagulants; LMWH, low-molecular-weight heparin; NSAIDs, nonsteroidal anti-inflammatory drugs; SD, standard deviation; VKAs, vitamin K antagonists; VTE, venous thromboembolism.
Comparisons between DOACs versus standard therapy:
p < 0.01;
p < 0.001;
p < 0.05.
Table 2. Treatment strategies for initial and for long-term therapy.
| Initial therapy | Long-term therapy | |||
|---|---|---|---|---|
| DOACs | LMWH | DOACs | VKAs | |
| Initial therapy with LMWH, N | 473 | 8,577 | 1,298 | 5,038 |
| Mean days of therapy ( ± SD) | 20 ± 16 a | 13 ± 16 | 149 ± 156 | 251 ± 248 |
| Median days of therapy (IQR) | 23 (12–24) a | 10 (7–13) | 96 (65–183) | 172 (99–313) |
| Mean LMWH doses (IU/kg/d) | – | 170 ± 46 | – | – |
| Rivaroxaban, N | 382 | 844 | ||
| Mean days of therapy ( ± SD) | 21 ± 17 | – | 144 ± 163 | – |
| Median days of therapy (IQR) | 23 (14–24) | – | 94 (42–172) | – |
| 30 mg daily | 346 (91%) | – | 204 (24%) | – |
| 20 mg daily | 10 (2.6%) | – | 547 (65%) | – |
| 15 mg daily | 25 (6.5%) | – | 87 (10%) | – |
| Apixaban, N | 91 | 344 | ||
| Mean days of therapy ( ± SD) | 10 ± 11 | – | 162 ± 147 | – |
| Median days of therapy (IQR) | 9 (9–10) | – | 114 (85–191) | – |
| 20 mg daily | 67 (74%) | – | 44 (13%) | – |
| 10 mg daily | 13 (14%) | – | 233 (68%) | – |
| 5 mg daily | 11 (12%) | – | 64 (19%) | – |
| Dabigatran, N | 69 | |||
| Mean days of therapy ( ± SD) | – | – | 173 ± 137 | – |
| Median days of therapy (IQR) | – | – | 134 (93–203) | – |
| 220 mg daily | – | – | 38 (55%) | – |
| Other doses/not reported | – | – | 31 (45%) | – |
| Edoxaban, N | 41 | |||
| Mean days of therapy ( ± SD) | – | – | 125 ± 78 | – |
| Median days of therapy (IQR) | – | – | 98 (88–170) | – |
| 60 mg daily | – | – | 25 (61%) | – |
| 30 mg daily | – | – | 16 (39%) | – |
Abbreviations: DOACs, direct oral anticoagulants; IQR, interquartile range; LMWH, low-molecular-weight heparin; SD, standard deviation; VKAs, vitamin K antagonists.
Comparisons between DOACs versus standard therapy: a p < 0.001.
During the course of anticoagulation, 95 patients developed VTE recurrences (LMWH 85, DOACs 10), 262 had major bleeding (VKAs 241, DOACs 21), and 595 died (standard therapy 536, DOACs 59). Patients receiving DOACs for initial therapy had a significantly lower rate of the composite outcome (HR: 0.32; 95% CI: 0.08–0.88) and a lower mortality rate (HR: 0.29; 95% CI: 0.12–0.62) than those receiving LMWH ( Table 3 ). No patient receiving DOACs initially developed VTE recurrences, and the rate of major bleeding was nonsignificantly lower (HR: 0.37; 95% CI: 0.09–1.04) than in those on LMWH. All three major bleeding events occurring in patients initially receiving DOACs appeared in patients aged ≥75 years, with CrCl levels >50 mL/min. None of the 169 patients with CrCl levels ≤50 mL/min developed major bleeding during initial therapy with DOACs. No patients initially receiving DOACs died of PE or bleeding. On multivariable analysis, patients initially receiving DOACs had a nonsignificantly lower risk for the composite outcome (HR: 0.36; 95% CI: 0.11–1.15) than those on LMWH. During long-term therapy, patients receiving DOACs had a nonsignificantly lower rate of the composite outcome (HR: 0.70; 95% CI: 0.46–1.03), VTE recurrences (HR: 0.77; 95% CI: 0.38–1.45), or major bleeding (HR: 0.68; 95% CI: 0.41–1.10) than those on VKAs, and a similar mortality rate (HR: 1.03; 95% CI: 0.76–1.39) ( Fig. 2 and Tables 3 and 4 ). Most patients (17 of 18, 94%) presenting with major bleeding during long-term therapy with DOACs were aged ≥75 years. Of these, eight patients had CrCl levels >50 mL/min and nine had levels ≤50 mL/min. On multivariable analysis, patients receiving DOACs had a significantly lower risk for the composite outcome (HR: 0.61; 95% CI: 0.41–0.92) than those on VKAs ( Table 5 ).
Table 3. Outcomes in fragile patients with VTE, according to initial therapy with LMWH or DOACs.
| N |
N
per 100
patient-years |
N |
N
per 100
patient-years |
Hazard ratio (95% CI) |
|
|---|---|---|---|---|---|
| Initial therapy | DOACs | LMWH | |||
| Patients, N | 473 | 8,577 | |||
| Recurrent DVT | 0 | – | 8 | 2.29 (1.07–4.36) | – |
| Recurrent PE | 0 | – | 12 | 3.44 (1.86–5.84) | – |
| Recurrent VTE | 0 | – | 20 | 5.74 (3.60–8.71) | – |
| Major bleeding | 3 | 11.7 (2.98–31.9) | 109 | 31.4 (25.9–37.7) | 0.37 (0.09–1.04) |
| Gastrointestinal | 1 | 3.90 (0.20–19.2) | 30 | 8.60 (5.91–12.1) | 0.45 (0.02–2.38) |
| Intracranial | 1 | 3.90 (0.19–19.2) | 9 | 2.58 (1.26–4.73) | 1.52 (0.07–9.09) |
| Composite outcome | 3 | 11.7 (2.98–31.9) | 128 | 36.9 (30.9–43.8) | 0.32 (0.08–0.88) |
| Death | 6 | 23.4 (9.49–48.7) | 277 | 79.7 (70.8–89.6) | 0.29 (0.12–0.62) |
| Causes of death | |||||
| Pulmonary embolism | 0 | – | 54 | 15.5 (11.7–20.0) | – |
| Bleeding | 0 | – | 16 | 4.58 (2.71–7.28) | – |
| Long-term therapy | DOACs | VKAs | |||
| Patients, N | 1,298 | 5,038 | |||
| Recurrent DVT | 3 | 0.40 (0.10–1.09) | 31 | 0.82 (0.57–1.16) | 0.49 (0.12–1.43) |
| Recurrent PE | 7 | 0.94 (0.41–1.85) | 35 | 0.93 (0.66–1.28) | 1.01 (0.41–2.17) |
| Recurrent VTE | 10 | 1.34 (0.68–2.39) | 65 | 1.74 (1.35–2.20) | 0.77 (0.38–1.45) |
| Major bleeding | 18 | 2.41 (1.47–3.74) | 132 | 3.52 (2.95–4.16) | 0.68 (0.41–1.10) |
| Gastrointestinal | 12 | 1.61 (0.87–2.73) | 54 | 1.43 (1.09–1.86) | 1.12 (0.57–2.04) |
| Intracranial | 2 | 0.27 (0.04–0.88) | 20 | 0.53 (0.33–0.80) | 0.51 (0.08–1.85) |
| Composite outcome | 27 | 3.63 (2.44–5.21) | 193 | 5.19 (4.50–5.96) | 0.70 (0.46–1.03) |
| Death | 53 | 7.09 (5.36–9.20) | 259 | 6.86 (6.06–7.73) | 1.03 (0.76–1.39) |
| Causes of death | |||||
| Recurrent PE | 3 | 0.40 (0.10–1.09) | 2 | 0.05 (0.01–0.17) | 7.69 (1.12–50.0) |
| Bleeding | 1 | 0.13 (0.01–0.66) | 19 | 0.50 (0.31–0.77) | 0.27 (0.01–1.45) |
| Fatal PE or bleeding | 4 | 0.53 (0.17–1.29) | 21 | 0.56 (0.35–0.84) | 0.96 (0.28–2.63) |
Abbreviations: DOACs, direct oral anticoagulants; DVT, deep vein thrombosis; LMWH, low-molecular-weight heparin; PE, pulmonary embolism; VKAs, vitamin K antagonists; VTE, venous thromboembolism.
Fig. 2.
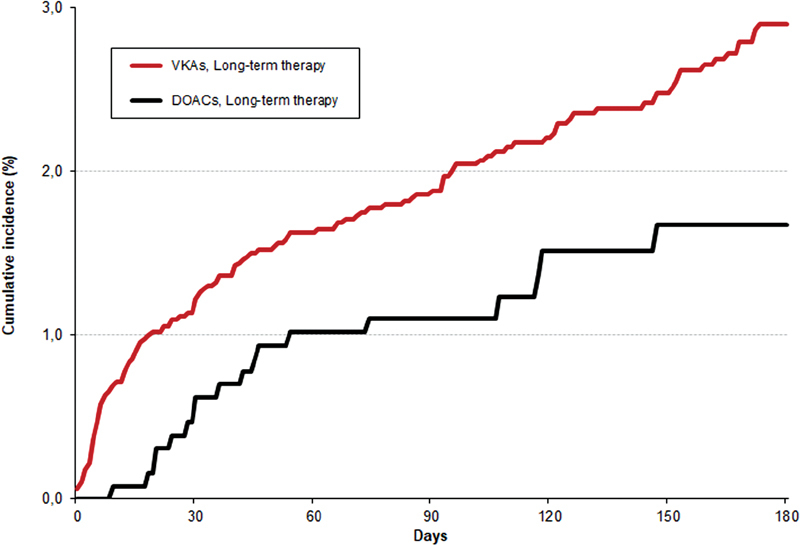
Cumulative rates of the composite outcome during the first 6 months of therapy.
Table 4. Cumulative rates of the composite of VTE recurrences or major bleeding during the first 6 months of therapy.
| Days | 30 | 60 | 90 | 120 | 150 | 180 | |
|---|---|---|---|---|---|---|---|
| VKAs | Patients at risk | 4,988 | 4,827 | 4,616 | 3,935 | 3,176 | 2,767 |
| Events | 61 (1.22%) | 81 (1.63%) | 93 (1.88%) | 106 (2.21%) | 115 (2.48%) | 127 (2.9%) | |
| DOACs | Patients at risk | 1,288 | 1,250 | 1,118 | 857 | 653 | 544 |
| Events | 8 (0.62%) | 13 (1.02%) | 14 (1.11%) | 17 (1.51%) | 18 (1.67%) | 18 (1.67%) | |
Table 5. Uni- and multivariable analyses for the composite outcome of VTE recurrences plus major bleeding.
| Initial therapy | Long-term therapy | |||
|---|---|---|---|---|
| Univariable | Multivariable | Univariable | Multivariable | |
| Events, N | 131 | |||
| Clinical characteristics | ||||
| Male gender | 0.73 (0.51–1.06) | 0.70 (0.48–1.02) | 1.03 (0.78–1.35) | – |
| Age > 80 y | 1.16 (0.82–1.64) | – | 1.43 (1.09–1.87) a | 1.31 (0.99–1.73) |
| Body weight ≤ 70 kg | 0.90 (0.64–1.27) | – | 1.32 (1.01–1.72) b | 1.25 (0.95–1.65) |
| Initial VTE presentation | ||||
| Pulmonary embolism | 1.34 (0.94–1.92) | – | 1.13 (0.85–1.50) | – |
| Risk factors for VTE | ||||
| Unprovoked | Ref. c | Ref. b | Ref. c | Ref. b |
| Cancer | 1.90 (1.23–2.95) a | 1.71 (1.09–2.69) b | 1.67 (1.15–2.44) a | 1.52 (1.04–2.23) b |
| Transient risk factors | 2.17 (1.43–3.28) c | 1.80 (1.18–2.76) a | 1.65 (1.22–2.21) c | 1.36 (1.01–1.85) b |
| Prior VTE | 1.11 (0.69–1.79) | – | 1.12 (0.80–1.58) | – |
| Underlying diseases | ||||
| Chronic heart failure | 1.21 (0.73–2.01) | – | 1.56 (1.08–2.23) b | 1.37 (0.94–1.98) |
| Chronic lung disease | 1.33 (0.86–2.06) | – | 1.26 (0.89–1.78) | – |
| Recent major bleeding | 4.51 (2.59–7.86) c | 3.69 (2.09–6.54) c | 3.28 (1.62–6.65) a | 2.37 (1.15–4.88) b |
| Blood tests | ||||
| Anemia | 1.52 (1.08–2.14) b | 1.23 (0.86–1.76) | 1.96 (1.50–2.55) c | 1.69 (1.28–2.23) c |
| Platelet count < 100,000/µL | 1.52 (0.62–3.72) | – | 1.52 (0.72–3.23) | – |
| CrCl levels ≤50 mL/min | 1.12 (0.79–1.58) | – | 1.26 (0.97–1.64) | 1.02 (0.77–1.35) |
| Concomitant drugs | ||||
| Corticosteroids | 1.28 (0.79–2.08) | – | 1.47 (1.00–2.18) | 1.26 (0.85–1.87) |
| Antiplatelets | 1.45 (1.01–2.09) b | 1.48 (1.03–2.13) b | 1.32 (0.99–1.75) | 1.18 (0.88–1.57) |
| NSAIDs | 1.30 (0.73–2.30) | – | 1.78 (1.21–2.63) a | 1.70 (1.15–2.53) a |
| DOACs | ||||
| Yes | 0.34 (0.11–1.06) | 0.36 (0.11–1.15) | 0.65 (0.43–0.97) b | 0.61 (0.41–0.92) b |
Abbreviations: CrCl, creatinine clearance; DOACs, direct oral anticoagulants; NSAIDs, nonsteroidal anti-inflammatory drugs; Ref., reference; VTE, venous thromboembolism.
Comparisons: a p < 0.01; b p < 0.05; c p < 0.001.
During initial therapy, the rate of major bleeding in patients receiving DOACs at recommended doses was lower than in those receiving LMWH (HR: 0.14; 95% CI: 0.007–0.71), as shown in Table 6 . The rate in patients receiving nonrecommended doses of DOACs was higher. During long-term therapy, patients receiving DOACs at recommended doses (but not those on nonrecommended doses) had half the rate of the composite outcome (HR: 0.45; 95% CI: 0.23–0.80) compared to those on VKAs. The rates of the composite outcome during long-term therapy with rivaroxaban, apixaban, or dabigatran were similar.
Table 6. Rates of VTE recurrences, major bleeding, and the composite outcome, according to prescribed drugs and doses. Results expressed as number of events per 100 patient-years and 95% confidence intervals.
| Initial therapy | Long-term therapy | |||
|---|---|---|---|---|
| N | Events per 100 patient-years |
N | Events per 100 patient-years |
|
| Standard therapy, N | 8,577 | 5,038 | ||
| VTE recurrences | 20 | 5.74 (3.60–8.71) | 65 | 1.74 (1.35–2.20) |
| Major bleeding | 109 | 31.4 (25.9–37.7) | 132 | 3.52 (2.85–4.16) |
| Composite outcome | 128 | 36.9 (30.9–43.8) | 193 | 5.19 (4.50–5.96) |
| DOACs, recommended doses, N | 413 | 843 | ||
| VTE recurrences | 0 | – | 4 | 0.85 (0.27–2.06) |
| Major bleeding | 1 | 4.44 (0.22–21.9) | 7 | 1.49 (0.65–2.95) |
| Composite outcome | 1 | 4.44 (0.22–21.9) | 11 | 2.35 (1.23–4.08) |
| DOACs, nonrecommended doses, N | 60 | 455 | ||
| VTE recurrences | 0 | – | 6 | 2.19 (0.89–4.56) |
| Major bleeding | 2 | 65.4 (11.0–216.1) | 11 | 4.02 (2.12–6.99) |
| Composite outcome | 2 | 65.4 (11.0–216.1) | 16 | 5.88 (3.48–9.35) |
| Rivaroxaban, N | 382 | 844 | ||
| VTE recurrences | 0 | – | 9 | 1.85 (0.90–3.39) |
| Major bleeding | 3 | 13.2 (3.37–36.1) | 10 | 2.05 (1.04–3.65) |
| Composite outcome | 3 | 13.2 (3.37–36.1) | 18 | 3.71 (2.27–5.74) |
| Apixaban, N | 91 | 344 | ||
| VTE recurrences | 0 | – | 1 | 0.51 (0.03–2.50) |
| Major bleeding | 0 | – | 6 | 3.05 (1.24–6.34) |
| Composite outcome | 0 | – | 7 | 3.56 (1.56–7.04) |
| Dabigatran, N | 0 | 69 | ||
| VTE recurrences | 0 | – | 0 | – |
| Major bleeding | 0 | – | 2 | 4.84 (0.81–16.0) |
| Composite outcome | 0 | – | 2 | 4.84 (0.81–16.0) |
| Edoxaban, N | 0 | 41 | ||
| VTE recurrences | 0 | – | 0 | – |
| Major bleeding | 0 | – | 0 | – |
| Composite outcome | 0 | – | 0 | |
Abbreviations: DOACs, direct oral anticoagulants; VTE, venous thromboembolism.
Discussion
Our data, obtained from a series of fragile patients with VTE in real life, suggest that the use of DOACs may be more effective and safe than standard therapy in this patient population. No patient receiving DOACs for initial therapy in our cohort developed VTE recurrences, and their rate of major bleeding was one-third the rate in patients on LMWH. On multivariable analysis, the risk for the composite outcome was not significantly lower, most likely since fragile patients on DOACs were younger and less likely to have cancer, anemia, or renal insufficiency than those on LMWH. During long-term therapy however, the clinical characteristics of patients receiving DOACs or VKAs were similar, and the use of DOACs was associated with a lower risk for the composite outcome after adjusting for potential confounders.
In a previous study using the RIETE database, we found that fragile patients with VTE had a twofold higher rate of major bleeding and half the rate of VTE recurrences compared to the nonfragile. 3 Thus, there are reasons to suggest that when choosing an anticoagulant drug for fragile patients with VTE, safety is an important issue. The current findings confirm that the rate of major bleeding during the course of anticoagulation clearly outweighed the rate of VTE recurrences (262 vs. 95 events, respectively). Unexpectedly however, only one in every 20 fragile patients was prescribed DOACS initially, and only one in every eight for long-term therapy. Data from the PREFER in VTE registry also showed that the use of DOACs was less likely in elderly patients or in those with renal insufficiency. 1 9 10 11 12 13 14 It would seem to be more cost effective to prescribe safer drugs in patients at increased risk for bleeding, as fragile patients are. As far as we know, no studies have compared yet the efficacy and safety of the DOACs versus standard therapy in fragile patients with VTE. In a recent study, Coleman et al compared rivaroxaban versus VKAs in a cohort of frail patients with VTE. 15 However, the term “fragile” has been recently incorporated into the literature to include VTE patients who are elderly, renally impaired, or with low body weight. 1 This term should not be confused with “frail,” which usually refers to elderly people with reduced physiologic reserve associated with increased susceptibility to disability. 16 17 18 19 20
During long-term therapy, only two in every three patients (65%) on DOACs received the recommended doses. This is important since the use of DOACs at nonrecommended doses has been associated with a much higher rate of VTE recurrences and a similar rate of major bleeding compared to those on recommended doses. 21 One in every six patients (496 of 2,975, 17%) with CrCl levels <50 mL/min in our series was prescribed DOACs, a subgroup of patients at increased risk for bleeding. 4 22 23 However, only six of these patients had major bleeding, thus suggesting that the DOACs might be at least as safe as VKAs in patients with CrCl levels <50 mL/min. Unfortunately, randomized clinical trials to compare the DOACs versus standard therapy are not allowed in patients with CrCl levels <50 mL/min.
The present study has several potential limitations. First, since RIETE is an observational registry (and not a randomized trial) our data are hypothesis-generating. They might be a useful basis for future controlled clinical trials comparing different therapeutic strategies, but we should be extremely cautious in suggesting changes in treatment strategies just because of uncontrolled registry data. Second, for long-term therapy we compared DOACs versus VKAs, but one in every eight such patients (12%) had active cancer, and they should have been compared rather with LMWH. Third, treatment varied with local practice, and is likely to have been influenced by a physician's assessment of a patient's risk of bleeding. Fourth, patients in the RIETE database were selected from several different countries. The variability of practices in different countries could potentially affect the study outcomes. Fifth, a variety of practitioners entered data into the registry, which may lend itself to potential inaccuracies in the data being reported. Finally, lack of central adjudication of the events is another limitation that is impossible for us to overcome. The main strengths of our observation are the high number of included patients, the strict diagnostic criteria, and the reporting of objectively established outcomes (major bleeding and recurrent VTE). Additionally, the population-based sample we used describes the effects of anticoagulant therapy in “real-world” clinical care, as opposed to that in a protocol driven randomized trial, and enhances the generalizability of our findings.
In summary, in real life 41% of VTE patients were fragile, a subgroup of patients where the risk for bleeding is particularly high. Our findings suggest that the use of DOACs may be more effective and safe than standard therapy in this patient population. Intervention studies specifically designed to confirm our findings and the potential role of the DOACs in fragile patients receiving anticoagulant therapy for VTE are warranted.
Acknowledgments
We express our gratitude to Sanofi Spain for supporting this registry with an unrestricted educational grant. We also express our gratitude to Bayer Pharma AG for supporting this registry. Bayer Pharma AG's support was limited to the part of RIETE outside Spain, which accounts for a 25.20% of the total patients included in the RIETE Registry. We also thank the RIETE Registry Coordinating Center, S&H Medical Science Service, for their quality control data, logistic and administrative support, and Prof. Salvador Ortiz, Universidad Autónoma Madrid, and Silvia Galindo, both Statistical Advisors in S&H Medical Science Service, for the statistical analysis of the data presented in this article.
Conflict of Interest None declared.
Authors' Contributions
All the authors introduced patients in the database, performed the research, analyzed results, and reviewed the article. J. J. López-Núñez and M. Monreal designed the research and wrote the article.
A full list of RIETE investigators is given in Appendix A .
Appendix A.
Coordinator of the RIETE Registry: Manuel Monreal.
RIETE Steering Committee Members: Paolo Prandoni, Benjamin Brenner, and Dominique Farge-Bancel.
RIETE National Coordinators: Raquel Barba (Spain), Pierpaolo Di Micco (Italy), Laurent Bertoletti (France), Sebastian Schellong (Germany), Inna Tzoran (Israel), Abilio Reis (Portugal), Marijan Bosevski (R. Macedonia), Henri Bounameaux (Switzerland), Radovan Malý (Czech Republic), Peter Verhamme (Belgium), Joseph A. Caprini (United States), Hanh My Bui (Vietnam).
RIETE Registry Coordinating Center: S&H Medical Science Service.
Members of the RIETE Group: SPAIN: Adarraga MD, Agud M, Aibar MA, Aibar J, Alcalde-Manero M, Amado C, Arcelus JI, Ballaz A, Barba R, Barrón M, Barrón-Andrés B, Bascuñana J, Blanco-Molina A, Camon AM, Cañas I, Carrasco C, Castro J, de Ancos C, del Toro J, Demelo P, Díaz-Pedroche C, Díaz-Peromingo JA, Falgá C, Farfán AI, Fernández-Capitán C, Fernández-Criado MC, Fidalgo MA, Font C, Font L, Furest I, García MA, García-Bragado F, García-Morillo M, García-Raso A, García-Ródenas M, Gavín O, Gaya-Manso I, Gayol MC, Gil-Díaz A, Gómez V, Gómez-Cuervo C, González-Martínez J, Grau E, Gutiérrez J, Hernández-Blasco LM, Iglesias M, Jara-Palomares L, Jaras MJ, Jiménez D, Jou I, Joya MD, Lima J, Llamas P, Lobo JL, López-Jiménez L, López-Miguel P, López-Núñez JJ, López-Reyes R, López-Sáez JB, Lorente MA, Lorenzo A, Loring M, Madridano O, Maestre A, Marchena PJ, Martín del Pozo M, Martín-Fortea MP, Martín-Guerra JM, Martínez-González L, Mella C, Mellado M, Monreal M, Montesa C, Morales MV, Nieto MA, Nieto JA, Núñez MJ, Olivares MC, Otero R, Pedrajas JM, Pellejero G, Pérez-Ductor C, Pérez-Jacoiste A, Pérez-Rus G, Peris ML, Porras JA, Rivas A, Rodríguez-Hernández A, Rubio CM, Ruiz-Artacho P, Ruiz-Ruiz J, Ruiz-Sada P, Sahuquillo JC, Sala-Sainz MC, Salazar V, Salgueiro G, Sampériz A, Sánchez-Muñoz-Torrero JF, Sancho T, Soler S, Suriñach JM, Tolosa C, Torres MI, Trujillo-Santos J, Uresandi F, Valle R, Vidal G, Villares P. ARGENTINA: Gutiérrez P, Vázquez FJ, Vilaseca A. BELGIUM: Vanassche T, Vandenbriele C, Verhamme P. CZECH REPUBLIC: Hirmerova J, Malý R. ECUADOR: Salgado E. FRANCE: Benzidia I, Bertoletti L, Bura-Riviere A, Debourdeau P, Farge-Bancel D, Hij A, Mahé I, Merah A, Moustafa F. GERMANY: Schellong S. ISRAEL: Braester A, Brenner B, Ellis M, Tzoran I. IRAN: Sharif-Kashani B. ITALY: Barillari G, Bilora F, Bortoluzzi C, Brandolin B, Ceccanti G, Ciammaichella M, Dentali F, Di Micco P, Grandone E, Maida R, Mastroiacovo D, Pallotti G, Pace F, Parisi R, Pesavento R, Prandoni P, Quintavalla R, Rocci A, Siniscalchi C, Tufano A, Visonà A, Vo Hong N, Zalunardo B. LATVIA: Gibietis V, Kigitovica D, Skride A. REPUBLIC OF MACEDONIA: Bosevski M. SWITZERLAND: Bounameaux H, Mazzolai L. USA: Caprini J. VIETNAM: Bui HM, Pham KQ.
References
- 1.Bauersachs R, Berkowitz S D, Brenner B et al. Oral rivaroxaban for symptomatic venous thromboembolism. N Engl J Med. 2010;363(26):2499–2510. doi: 10.1056/NEJMoa1007903. [DOI] [PubMed] [Google Scholar]
- 2.Büller H R, Décousus H, Grosso M A et al. Edoxaban versus warfarin for the treatment of symptomatic venous thromboembolism. N Engl J Med. 2013;369(15):1406–1415. doi: 10.1056/NEJMoa1306638. [DOI] [PubMed] [Google Scholar]
- 3.Moustafa F, Pierfranceschi M G, Di Micco P et al. Clinical outcomes during anticoagulant therapy in fragile patients with venous thromboembolism. Res Pract Thromb Haemost. 2017;1(02):172–179. doi: 10.1002/rth2.12036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ruíz-Giménez N, Suárez C, González R et al. Predictive variables for major bleeding events in patients presenting with documented acute venous thromboembolism. Findings from the RIETE Registry. Thromb Haemost. 2008;100(01):26–31. doi: 10.1160/TH08-03-0193. [DOI] [PubMed] [Google Scholar]
- 5.Muñoz-Torrero J F, Bounameaux H, Pedrajas J Met al. Effects of age on the risk of dying from pulmonary embolism or bleeding during treatment of deep vein thrombosis J Vasc Surg 20115406, Suppl):26S–32S. [DOI] [PubMed] [Google Scholar]
- 6.Jiménez D, de Miguel-Díez J, Guijarro R et al. Trends in the management and outcomes of acute pulmonary embolism: Analysis from the RIETE Registry. J Am Coll Cardiol. 2016;67(02):162–170. doi: 10.1016/j.jacc.2015.10.060. [DOI] [PubMed] [Google Scholar]
- 7.Muriel A, Jiménez D, Aujesky D et al. Survival effects of inferior vena cava filter in patients with acute symptomatic venous thromboembolism and a significant bleeding risk. J Am Coll Cardiol. 2014;63(16):1675–1683. doi: 10.1016/j.jacc.2014.01.058. [DOI] [PubMed] [Google Scholar]
- 8.Bikdeli B, Jimenez D, Hawkins M et al. Rationale, design and methodology of the computerized registry of patients with venous thromboembolism (RIETE) Thromb Haemost. 2018;118(01):214–224. doi: 10.1160/TH17-07-0511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bauersachs R, Agnelli G, Gitt A K et al. The role of heparin lead-in in the real-world management of acute venous thromboembolism: the PREFER in VTE registry. Thromb Res. 2017;157:181–188. doi: 10.1016/j.thromres.2017.07.029. [DOI] [PubMed] [Google Scholar]
- 10.Cohen A T, Gitt A K, Bauersachs R et al. The management of acute venous thromboembolism in clinical practice. Results from the European PREFER in VTE Registry. Thromb Haemost. 2017;117(07):1326–1337. doi: 10.1160/TH16-10-0793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schulman S, Kearon C, Kakkar A K et al. Dabigatran versus warfarin in the treatment of acute venous thromboembolism. N Engl J Med. 2009;361(24):2342–2352. doi: 10.1056/NEJMoa0906598. [DOI] [PubMed] [Google Scholar]
- 12.Büller H R, Prins M H, Lensin A W et al. Oral rivaroxaban for the treatment of symptomatic pulmonary embolism. N Engl J Med. 2012;366(14):1287–1297. doi: 10.1056/NEJMoa1113572. [DOI] [PubMed] [Google Scholar]
- 13.Agnelli G, Buller H R, Cohen A et al. Oral apixaban for the treatment of acute venous thromboembolism. N Engl J Med. 2013;369(09):799–808. doi: 10.1056/NEJMoa1302507. [DOI] [PubMed] [Google Scholar]
- 14.Becattini C, Agnelli G. Treatment of venous thromboembolism with new anticoagulant agents. J Am Coll Cardiol. 2016;67(16):1941–1955. doi: 10.1016/j.jacc.2016.01.072. [DOI] [PubMed] [Google Scholar]
- 15.Coleman C I, Turpie A GG, Bunz T J, Beyer-Westendorf J. Effectiveness and safety of rivaroxaban versus warfarin in frail patients with venous thromboembolism. Am J Med. 2018;131(08):9330–9380. doi: 10.1016/j.amjmed.2018.02.015. [DOI] [PubMed] [Google Scholar]
- 16.Buchner D M, Wagner E H. Preventing frail health. Clin Geriatr Med. 1992;8(01):1–17. [PubMed] [Google Scholar]
- 17.Rockwood K, Song X, MacKnight C et al. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005;173(05):489–495. doi: 10.1503/cmaj.050051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Robinson T N, Eiseman B, Wallace J I et al. Redefining geriatric preoperative assessment using frailty, disability and co-morbidity. Ann Surg. 2009;250(03):449–455. doi: 10.1097/SLA.0b013e3181b45598. [DOI] [PubMed] [Google Scholar]
- 19.Robinson T N, Wu D S, Pointer L, Dunn C L, Cleveland J C, Jr, Moss M. Simple frailty score predicts postoperative complications across surgical specialties. Am J Surg. 2013;206(04):544–550. doi: 10.1016/j.amjsurg.2013.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Perera V, Bajorek B V, Matthews S, Hilmer S N. The impact of frailty on the utilisation of antithrombotic therapy in older patients with atrial fibrillation. Age Ageing. 2009;38(02):156–162. doi: 10.1093/ageing/afn293. [DOI] [PubMed] [Google Scholar]
- 21.Trujillo-Santos J, Di Micco P, Dentali F et al. Real-life treatment of venous thromboembolism with direct oral anticoagulants: the influence of recommended dosing and regimens. Thromb Haemost. 2017;117(02):382–389. doi: 10.1160/TH16-07-0494. [DOI] [PubMed] [Google Scholar]
- 22.Monreal M, Falgá C, Valle R et al. Venous thromboembolism in patients with renal insufficiency: findings from the RIETE Registry. Am J Med. 2006;119(12):1073–1079. doi: 10.1016/j.amjmed.2006.04.028. [DOI] [PubMed] [Google Scholar]
- 23.Moustafa F, Stehouwer A, Kamphuisen P et al. Management and outcome of major bleeding in patients receiving vitamin K antagonists for venous thromboembolism. Thromb Res. 2018;171:74–80. doi: 10.1016/j.thromres.2018.09.049. [DOI] [PubMed] [Google Scholar]


