Abstract
Objective
The objective of the present study was to use retrospective data to test the hypothesis that cannabis dependence would be associated with an increased rate of post-deployment suicide attempts.
Methods
Participants included 319 veterans who had deployed to either Iraq or Afghanistan. Study procedures involved completion of a structured clinical interview and a battery of self-report questionnaires.
Results
As expected, lifetime cannabis dependence was significantly associated with post-deployment suicide attempts, AOR = 7.963, p = .014, even after controlling for the effects of pre-deployment suicide attempts, posttraumatic stress disorder, depression, pain, non-cannabis substance use disorder, and gender.
Conclusions
While preliminary, our findings provide the first evidence to date that heavy cannabis use may be a unique risk factor for post-deployment suicide attempts among veterans.
Keywords: cannabis, marijuana, suicide attempts, veterans
Introduction
Military personnel deployed to warzones frequently encounter an array of combat experiences that increase their risk for mental health problems, including posttraumatic stress disorder (PTSD), depression, and anxiety disorders (Keane et al., 1989; Kimbrel et al., 2015; Kimbrel et al., 2014b). In turn, the presence of mental health problems appears to significantly increase veterans’ risk for both suicide attempts (Jakupcak et al., 2009; Kimbrel et al., 2014a; Kimbrel et al., 2016; Ramsawh et al., 2014) and death by suicide (Bullman and Kang, 1994; Ilgen et al., 2012). Substance use disorders (SUDs) are also associated with risk for suicide attempts and death by suicide (Borges et al., 2016; Poorolajal et al., 2015). Moreover, emerging research suggests that cannabis use disorders (CUD), in particular, may be associated with increased risk for suicide attempts among veterans (Kimbrel et al., 2017a; Kimbrel et al., 2017b).
The potential association between CUD and suicidal behavior is particularly relevant to Iraq/Afghanistan-era veterans, as CUD diagnoses rose among veterans by more than 50% from 2002 to 2009 (Bonn-Miller et al., 2012). There is also evidence that younger veterans who served in Iraq and Afghanistan are more likely to use cannabis than other substances or alcohol (Bonn-Miller et al., 2012). Veterans report using cannabis to deal with post-deployment physical and mental health symptoms, such as chronic pain, depression, and anxiety (Elliott et al., 2015); however, CUD has also been associated with a range of mental and physical health problems among civilians, including suicide attempts (Bellivier et al., 2011; Borges et al., 2016; Goldman et al., 2010; Joshi et al., 2014). For example, a recent meta-analysis found that heavy cannabis use was associated with significantly increased risk for suicide attempts in the general population (OR = 3.20, 95% CI: 1.72-5.94; (Borges et al., 2016)). In addition, a second meta-analysis has demonstrated that lifetime cannabis use disorders are associated with increased risk for suicide attempts among adult civilians with bipolar disorder (N = 3,439 individuals; Carrà et al., 2014), which is another population at high risk for suicide. While none of the studies included in these two meta-analyses were comprised of Iraq/Afghanistan-era veterans, Kimbrel et al. (2017a) and Kimbrel et al. (2017b) have recently reported a significant association between lifetime history of CUD and lifetime history of suicide attempts in Iraq/Afghanistan-era veterans, even after adjusting for gender, depression, and non-cannabis substance-use disorders; however, two limitations of the latter studies were that they: (a) did not examine whether severity of CUD was differentially associated with suicidal behavior; and (b) were unable to determine if CUD was specifically associated with post-deployment suicide attempts (i.e., suicide attempts that occurred after veterans had returned from their military deployments).
Study Objective
There is a significant need for additional studies aimed at evaluating the association between cannabis abuse, cannabis dependence, and suicide attempts (Borges et al., 2016). There is also a pressing need to identify predictors of suicidal behavior among veterans (US Department of Veterans Affairs, 2016). Accordingly, the objective of the present study was to overcome previous limitations by examining if cannabis dependence, a more severe form of CUD, was differentially associated with risk for suicide attempts as well as whether cannabis dependence would be specifically associated with post-deployment suicide attempts. Based upon prior work by Borges et al. (2016) indicating that heavy cannabis use is most strongly associated with suicidal behavior, we hypothesized that: (a) cannabis dependence would be more strongly associated with suicide attempts than cannabis abuse, and that (b) cannabis dependence would be associated with post-deployment suicide attempts, even after accounting for the influence of other known risk factors for suicide attempts, including gender, major depressive disorder, PTSD, non-cannabis substance use disorders, pain, and history of pre-deployment suicide attempts.
Methods
Participants
Participants included 319 Iraq/Afghanistan-era veterans who served in the military after September 11, 2001. Participants were recruited through mailings, advertisements, and clinician- referrals. Participants’ ages ranged from 21 to 67 (M = 39.6, SD = 10.6) years of age. The majority of participants were male (n = 261, 81.8%) and Black/African American (n = 161, 50.5%) or White (n = 122, 38.2%). Approximately 5% (n = 16) of the sample identified as Hispanic/Latino.
Procedures
All procedures were approved by the local Institutional Review Board, and written informed consent was obtained from all participants before any study procedures were completed. Participation consisted of completion of a structured clinical interview and a battery of self-report questionnaires.
Measures
Lifetime major depressive disorder (MDD), non-cannabis substance use disorder (SUD), and cannabis use disorder (CUD) were assessed using the Structured Clinical Interview for DSM-IV-TR Axis I Disorders (SCID; First et al., 1996). PTSD was assessed with the Clinician Administered PTSD Scale for DSM-IV (Blake et al., 1995). Diagnostic interviews were administered by licensed clinical psychologists or staff working under the supervision of a licensed clinical psychologist. Reliability among the interviewers was excellent (Fleiss’ kappa = 0.92 for lifetime psychiatric disorders on fidelity training videos). To reduce the number of covariates included in the model, a dichotomous non-cannabis lifetime SUD variable was created by combining lifetime abuse and dependence diagnoses together for all alcohol and non-cannabis illicit substances, with the exception of nicotine. Using this methodology, 6% (n = 20) met lifetime criteria for one or more non-cannabis SUDs.
A composite lifetime PTSD-depression variable (“0” = no lifetime history of PTSD or depression; “1” = a lifetime history of PTSD or depression; “2” = a lifetime history of PTSD and depression) was also included as a covariate in the logistic regression analyses due to recent findings indicating that cannabis use is associated with both PTSD and depression among veterans (Gentes et al., 2016) and that co-occurring PTSD-depression may be a particularly strong risk factor for suicide attempts in Iraq/Afghanistan-era veterans (Kimbrel et al., 2016). In the present study, 23% (n = 72) of the sample met lifetime criteria for PTSD, 36% (n = 115) met lifetime criteria for depression, and 13% (n = 42) met lifetime criteria for both PTSD and depression.
High levels of self-reported pain were assessed using the methodology of Naylor and colleagues (2017). Specifically, any participants who self-reported high levels of pain [i.e., a score of 3 or 4 on a 5-point scale that ranges from 0 (not at all) to 4 (extremely)] due to headaches, low back pain, or muscle soreness on the Symptom Checklist 90-R (Derogatis & Savitz, 1999) were categorized as having significant levels of pain (i.e., 0 = no/low levels of pain; 1 = high levels of pain present). Using this methodology, 40% (n = 129) of the present sample met criteria for high levels of pain.
History of suicide attempts was assessed retrospectively with a series of questions that inquired whether participants had made a suicide attempt before, during, between, or after any of their previous deployments. Specifically, participants were asked to indicate if the statement “I attempted suicide” applied to them during each of these four time periods. A total of 38 (11.9%) separate lifetime suicide attempts were reported on this scale, including 10 (3%) pre-deployment suicide attempts, 4 (1.3%) suicide attempts that occurred during deployment, 5 (1.6%) suicide attempts that occurred between deployments, and 19 (6.0%) post-deployment suicide attempts. In addition, three participants reported having made attempts during two separate time periods. Thus, a total of 35 (10.9%) veterans who participated in the present study reported having made one or more suicide attempts during their lifetime.
Data Analysis Plan
Chi-square tests were used to assess the bivariate association between cannabis abuse, cannabis dependence, and pre-deployment suicide attempts, post-deployment suicide attempts, and lifetime suicide attempts. Suicide attempts occurring during (n=4) and between deployments (n=5) were not examined separately in any of the analyses due to low base rates; however, note that suicide attempts occurring during and between deployments were included in the calculation of the lifetime suicide attempts variable (n=35). Logistic regression was used to test the association between cannabis abuse, cannabis dependence, and lifetime suicide attempts, pre-deployment suicide attempts, and post-deployment suicide attempts after controlling for gender, PTSD-MDD, pain, and non-cannabis SUD (including alcohol). An additional model predicting post-deployment suicide attempts was also run in which pre-deployment suicide attempt history was included as an additional covariate.
Results
Cannabis abuse (9.4%) and cannabis dependence (3.8%) were examined separately in order to test our first hypothesis. As expected, veterans with a lifetime history of cannabis dependence reported the highest overall rates of pre-deployment suicide attempts, χ2 (2) = 8.083, p = .018, post-deployment suicide attempts, χ2 (2) = 9.567, p = .008, and lifetime suicide attempts, χ2 (2) = 7.716, p = .021 (Figure 1). Follow-up chi-square tests revealed that rates of suicide attempts did not differ significantly between veterans with a history of cannabis abuse and veterans with no history of CUD (all p’s ≥ .34). In contrast, veterans with a history of cannabis dependence reported significantly higher rates of pre-deployment suicide attempts, χ2 (1) = 6.341, p = .012, post-deployment suicide attempts, χ2 (1) = 9.689, p = .002, and lifetime suicide attempts, χ2 (1) = 7.723, p = .005, than veterans with no history of CUD.
Figure 1.
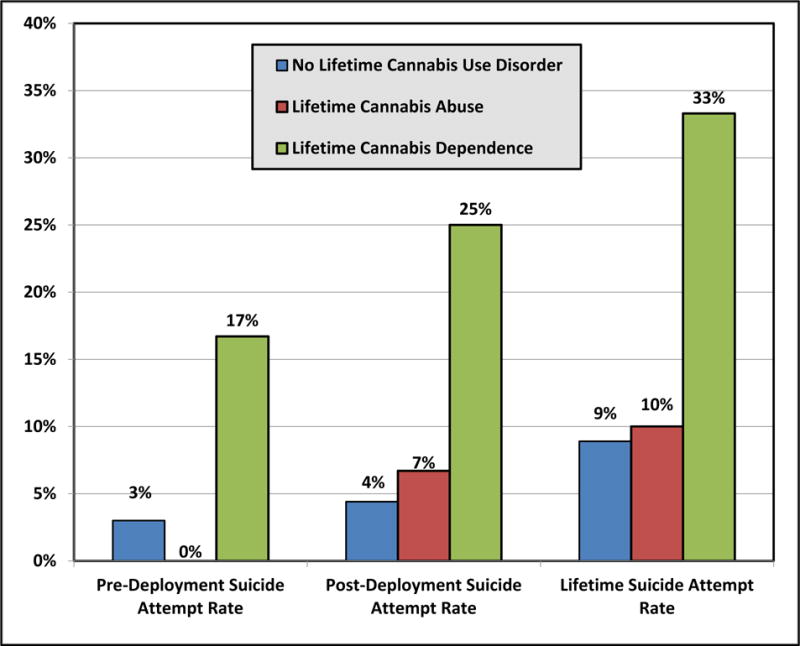
Association between Cannabis Abuse, Cannabis Dependence, and Suicide Attempts among Iraq/Afghanistan-era Veterans
Given the lack of bivariate associations observed between lifetime cannabis abuse and suicide attempts, the logistic regression analyses were limited to models examining lifetime cannabis dependence as a predictor. Consistent with our second hypothesis, lifetime cannabis dependence was associated with lifetime history of suicide attempts, adjusted odds ratio (AOR) = 5.135, p = 0.018, pre-deployment suicide attempts, AOR = 8.527, p= .022, and post-deployment suicide attempts, AOR = 7.746, p = .011, after adjusting for the effects of gender, PTSD-MDD, pain, and non-cannabis SUD (see Table 1). An additional model was also run in which post-deployment suicide attempts served as the dependent variable, and pre-deployment suicide attempt history was included as a covariate along with gender, PTSD-MDD, pain, and non-cannabis SUD. As expected, lifetime cannabis dependence continued to be associated with post-deployment suicide attempts in this model as well, AOR = 7.963, p = .014 (see Table 1).
Table 1.
Summary of the Logistic Regression Models Predicting Suicide Attempts among Iraq/Afghanistan-era Veterans
| Adjusted Odds Ratios | ||||
|---|---|---|---|---|
| Variable Name | Lifetime Suicide Attempts | Pre-Deployment Suicide Attempts | Post-Deployment Suicide Attempts | Post-Deployment Suicide Attempts |
| Gender (0 = Female; 1 = Male) | 1.661 | 0.742 | 2.726 | 2.722 |
| PTSD-Depression | 1.018 | 0.523 | 1.135 | 1.135 |
| Pain | 2.675* | 1.863 | 3.254* | 3.285* |
| Non-Cannabis Substance Use Disorder | 2.385* | 1.872 | 3.561* | 3.557* |
| Cannabis Dependence | 5.135* | 8.527* | 7.746* | 7.963* |
| Pre-Deployment Suicide Attempts | – | – | – | 0.862 |
Note:
p < .05.
Discussion
The rate of death by suicide is three times higher among U.S. veterans compared with the general population rate for U.S. adults (39.0/100,000 vs. 13.0/100,000; US Department of Veterans Affairs, 2016). Indeed, the most recent data available suggest that, on average, 20 veterans die by suicide in the U.S. each day (US Department of Veterans Affairs, 2016). Thus, there is a pressing need to identify novel risk factors that may potentially increase risk for suicidal behavior within this important subset of the population. The findings from the present study provide additional evidence that heavy lifetime cannabis use is positively associated with suicide attempts among veterans. Notably, the present research expands on prior research conducted among veterans in two important ways. First, the current findings indicate that veterans with lifetime cannabis dependence (using DSM-IV parlance) or moderate to severe CUD (using DSM-5 parlance) appear to be at the greatest risk for suicide attempts, as no association was observed between lifetime cannabis abuse and any of the suicide attempt history variables. In contrast, lifetime cannabis dependence was reliably associated with all of the suicide attempt history variables examined. Second, the present findings demonstrate for the first time that lifetime cannabis dependence is specifically associated with post-deployment suicide attempts among Iraq/Afghanistan-era veterans, even after accounting for the effects of gender, PTSD-depression, pain, non-cannabis SUD, and pre-deployment suicide attempts.
As noted above, the potential association between lifetime CUD and suicidal behavior is particularly relevant to Iraq/Afghanistan-era veterans, as rates of CUD diagnoses have risen by more than 50% within this population from 2002 to 2009 (Bonn-Miller et al., 2012). Many veterans report using cannabis to deal with post-deployment mental health issues; however, the findings from the present research suggest that cannabis dependence may have the paradoxical effect of increasing veterans’ risk for suicidal behavior (Kimbrel et al., 2017b). Accordingly, in addition to conducting a thorough safety assessment, we recommend that clinicians working with veterans also carefully assess patients for cannabis dependence and other substance use disorders and proactively treat these conditions when it is feasible to do so (Kimbrel et al., 2017a).
Study Limitations
The present findings should be interpreted within the context of several limitations. For example, due to its retrospective design, causal relationships cannot be inferred from the current study. In addition, because of our interest in determining when suicide attempts occurred in relation to deployment status, a novel assessment of suicide attempts was used in the present study which asked whether participants had attempted suicide before, during, between, or after their deployments; however, our findings should be interpreted cautiously, given that this methodology has not been independently validated. In particular, it is possible that our use of a single item could have resulted in other suicidal behaviors (e.g., aborted suicide attempts) being mistakenly included in the suicide attempt variable. Thus, future research studies on this topic might consider using clinical interviews that could provide a more nuanced assessment of lifetime history of suicide attempts in relation to veterans’ history of deployments. Another limitation of our assessment approach was that CUD was not chronologically-anchored to deployment status or military service. Thus, it is impossible for us to determine whether CUD preceded suicide attempts or vice versa. While the finding that lifetime cannabis dependence was associated with both pre-deployment and post-deployment suicide attempts mitigates this concern to some degree, prospective research is still needed to determine if cannabis dependence is prospectively associated with suicide attempts in Iraq/Afghanistan-era veterans. An addition limitation concerns the relatively low rates of CUD and suicide attempts observed in this sample, which likely limited statistical power. Thus, replication of these findings in larger samples of veterans is needed to provide more stable estimates of the observed effects.
Despite these limitations, the present study provides important insights into the potential influence of cannabis dependence on suicide risk among veterans. Many returning veterans face multiple, potentially compounding suicide risk factors, such as comorbid psychiatric and substance use disorders and low levels of social support (e.g., Debeer et al., 2014; Ilgen et al., 2012; Kimbrel et al., 2014b; Kimbrel et al., 2016; US Department of Veterans Affairs, 2016). As a result, rates of CUD diagnoses have steadily risen within this population (Bonn-Miller et al., 2012), as many veterans with mental health problems, such as PTSD, chronic pain, depression, and anxiety report using cannabis to deal with post-deployment physical and mental health symptoms (e.g., Elliott et al., 2015; Gentes et al., 2016). In contrast with the growing public sentiment that cannabis is harmless (Hasin, 2018), the findings from the present research suggest that cannabis dependence may be an important, independent risk factor for suicide attempts among veterans, and that additional research aimed at prospectively examining the influence of cannabis dependence on suicide risk among this at-risk population is needed.
Acknowledgments
This work was supported by the National Institute of Mental Health (#R01MH080988), the Rehabilitation Research & Development Service of Department of Veterans Affairs Office of Research and Development, the Department of Veterans Affairs Mid-Atlantic Mental Illness Research, Education, and Clinical Center, and the Research and Development and Mental Health Services of the Durham VA Medical Center. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the VA or the US government.
References
- Bonn-Miller MO, Harris AHS, Trafton JA. Prevalence of cannabis use disorder diagnoses among veterans in 2002, 2008, and 2009. Psychol Serv. 2012;9:404–416. doi: 10.1037/a0027622. [DOI] [PubMed] [Google Scholar]
- Borges G, Bagge CL, Orozco R. A literature review and meta-analyses of cannabis use and suicidality. J Affect Disord. 2016;195:63–74. doi: 10.1016/j.jad.2016.02.007. [DOI] [PubMed] [Google Scholar]
- Bullman TA, Kang HK. Posttraumatic stress disorder and the risk of traumatic deaths among Vietnam veterans. J Nerv Ment Dis. 1994;182:604–610. doi: 10.1097/00005053-199411000-00002. [DOI] [PubMed] [Google Scholar]
- Carrà G, Bartoli F, Crocamo C, Brady KT, Clerici M. Attempted suicide in people with co-occurring bipolar and substance use disorders: Systematic review and meta-analysis. Journal of Affective Disorders. 2014;167:125–135. doi: 10.1016/j.jad.2014.05.066. [DOI] [PubMed] [Google Scholar]
- Debeer BB, Kimbrel NA, Meyer EC, Gulliver SB, Morissette SB. Combined PTSD and depressive symptoms interact with post-deployment social support to predict suicidal ideation in Operation Enduring Freedom and Operation Iraqi Freedom veterans. Psychiatr Res. 2014;216:357–362. doi: 10.1016/j.psychres.2014.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis LR, Savitz KL. The SCL-90-R, Brief Symptom Inventory, and Matching Clinical Rating Scales. In: Maruish ME, editor. The use of psychological testing for treatment planning and outcomes assessment. Mahwah, NJ, US: Lawrence Erlbaum Associates Publishers; 1999. pp. 679–724. [Google Scholar]
- Elliott L, Golub A, Bennett A, Guarino H. PTSD and cannabis-related coping among recent veterans in New York City. Contemporary Drug Problems. 2015;42:60. doi: 10.1177/0091450915570309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for the DSM-IV Axis I Disorders. Biometrics Research, New York State Psychiatric Institute; New York, NY: 1996. [Google Scholar]
- Gentes EL, Schry AR, Hicks TA, Clancy CP, Collie CF, Kirby AC, Calhoun PS. Prevalence and correlates of cannabis use in an outpatient VA posttraumatic stress disorder clinic. Psychology of Addictive Behaviors. 2016;30(3):415. doi: 10.1037/adb0000154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldman M, Suh JJ, Lynch KG, Szucs R, Ross J, Ju X, O’Brien CP, Oslin DW. Identifying risk factors for marijuana use among veterans affairs patients. Journal of Addiction Medicine. 2010;4:47–51. doi: 10.1097/ADM.0b013e3181b18782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS. US epidemiology of cannabis use and associated problems. Neuropsychopharmacology Reviews. 2018;43:195–212. doi: 10.1038/npp.2017.198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ilgen MA, McCarthy JF, Ignacio RV, Bohnert AS, Valenstein M, Blow FC, Katz IR. Psychopathology, Iraq and Afghanistan service, and suicide among Veterans Health Administration patients. J Consult Clin Psychol. 2012;80:323–330. doi: 10.1037/a0028266. [DOI] [PubMed] [Google Scholar]
- Jakupcak M, Cook J, Imel Z, Fontana A, Rosenheck R, McFall M. Posttraumatic stress disorder as a risk factor for suicidal ideation in Iraq and Afghanistan War veterans. J Trauma Stress. 2009;22:303–306. doi: 10.1002/jts.20423. [DOI] [PubMed] [Google Scholar]
- Joshi M, Joshi A, Bartter T. Marijuana and lung diseases. Current Opinion in Pulmonary Medicine. 2014;20:173–179. doi: 10.1097/MCP.0000000000000026. [DOI] [PubMed] [Google Scholar]
- Keane TM, Fairbank JA, Caddell JM, Zimering RT, Taylor KL, Mora CA. Clinical evaluation of a measure to assess combat exposure. Psychological Assessment: A Journal of Consulting and Clinical Psychology. 1989;1:53–55. [Google Scholar]
- Kimbrel NA, Calhoun PS, Elbogen EB, Brancu M, V. A. Mid-Atlantic MIRECC Registry Workgroup. Beckham JC. The factor structure of psychiatric comorbidity among Iraq/Afghanistan-era veterans and its relationship to violence, incarceration, suicide attempts, and suicidality. Psychiatr Res. 2014a;220:397–403. doi: 10.1016/j.psychres.2014.07.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimbrel NA, DeBeer BB, Meyer EC, Silvia PJ, Beckham JC, Young KA, Morissette SB. An examination of the broader effects of warzone experiences on returning Iraq/Afghanistan veterans׳ psychiatric health. Psychiatr Res. 2015;226:78–83. doi: 10.1016/j.psychres.2014.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimbrel NA, Evans LD, Patel AB, Wilson LC, Meyer EC, Gulliver SB, Morissette SB. The critical warzone experiences (CWE) scale: Initial psychometric properties and association with PTSD, anxiety, and depression. Psychiatr Res. 2014b;220:1118–1124. doi: 10.1016/j.psychres.2014.08.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimbrel NA, Meyer EC, DeBeer BB, Gulliver SB, Morissette SB. A 12-Month prospective study of the effects of PTSD-depression comorbidity on suicidal behavior in Iraq/Afghanistan-era veterans. Psychiatr Res. 2016;243:97–99. doi: 10.1016/j.psychres.2016.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimbrel NA, Meyer EC, DeBeer BB, Gulliver SB, Morissette SB. The impact of cannabis use disorder on suicidal and nonsuicidal self-injury in Iraq/Afghanistan-era veterans with and without mental health disorders. Suicide and life-threatening behavior. 2017a doi: 10.1111/sltb.12345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimbrel NA, Newins AR, Dedert EA, van Voorhees EE, Elbogen EB, Naylor JC, Wagner HR, Brancu M, Wokgroup VMAM, Beckham JC, Calhoun PS. Cannabis use disorder and suicide attempts in Iraq/Afghanistan-era veterans. J Psychiatr Res. 2017b;89:1–5. doi: 10.1016/j.jpsychires.2017.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poorolajal J, Haghtalab T, Farhadi M, Darvishi N. Substance use disorder and risk of suicidal ideation, suicide attempt, suicide death: A meta-analysis. Journal of Public Health. 2015:1–10. doi: 10.1093/pubmed/fdv148. [DOI] [PubMed] [Google Scholar]
- Ramsawh HJ, Fullerton CS, Mash HB, Ng TH, Kessler RC, Stein MB, Ursano RJ. Risk for suicidal behaviors associated with PTSD, depression, and their comorbidity in the U.S. Army. J Affect Disord. 2014;161:116–122. doi: 10.1016/j.jad.2014.03.016. [DOI] [PubMed] [Google Scholar]
- US Department of Veterans Affairs. VA Suicide Prevention Program Factos about Veteran Suicide. :2016. https://www.va.gov/opa/publications/factsheets/Suicide_Prevention_FactSheet_New_VA_Stats_070616_1400.pdf.


