Abstract
Depression as well as other psychosocial factors remain largely unaddressed among people living with HIV (PLHIV) in low and middle-income countries (LMIC). Depression is a common occurrence among PLHIV and is elevated in those who consume alcohol. This paper will document the presence of depressive symptoms in alcohol-consuming male PLHIV receiving antiretroviral treatment (ART) in India. It examines the correlates of depressive symptoms and uses the data from in-depth interviews to explain the nature of the statistical relationships obtained from an NIH-funded a multilevel, multicentric intervention study. A cross-sectional, baseline survey was administered to 940 alcohol consuming, male PLHIV in five hospital-based ART Centers in urban Maharashtra, India via face to face interviews from October 2015 to April 2016. An additional 55 men were recruited independently to engage in in-depth interviews on alcohol use and other factors related to adherence. The results of the survey showed that approximately 38% of PLHIV reported having moderate to severe depressive symptoms. Depressive symptoms were positively associated with higher levels of family-related concerns (OR=1.18; 95%CI=1.12–1.23), work difficulties (OR=2.04; 95%CI=1.69–2.69) and HIV-related self-stigma (OR=1.05; 95%CI=1.03–1.07) and a lower level of ART service satisfaction (OR=0.58 95% CI:0.44–0.77). The results of in-depth interviews showed that PLHIV’s tenshun (a Hindi term most closely corresponding to depressive symptoms) resulted from feelings of guilt and concerns about how family, friends, and neighbors might react to their HIV status and the potential for loss of job as a result of disclosure of their HIV status at work. The level of depressive symptoms among male PLHIV involved in ART treatment points to the need to strengthen the psychological component of PLHIV treatment in India.
Keywords: HIV, depressive symptoms, tenshun, self-stigma, family-related concerns, VIH, síntomas depresivos, tenshun, auto-estima, preocupaciones familiares
Resumen
La depresión y otros factores psicosociales siguen sin abordarse en gran medida entre las personas que viven con el VIH (PVVIH) en los países de ingresos bajos y medianos (PIBM). La depresión es una ocurrencia común entre las personas que viven con el VIH y es elevada en aquellos que consumen alcohol. Este documento documentará la presencia de síntomas depresivos en las PVVIH, masculinos, consumidores de alcohol que reciben tratamiento antirretroviral (TAR) en la India. Examina las correlaciones de los síntomas depresivos y utiliza los datos de las entrevistas en profundidad para explicar la naturaleza de las relaciones estadísticas obtenidas de un estudio de intervención multicéntrico de multinivel financiado por el NIH. Una encuesta transversal, encuesta inicial, se administró a 940 personas que consumen alcohol y viven con el VIH en cinco centros de terapia antirretroviral en el área rural de Maharashtra, en la India. Estas entrevistas fueron hechas en persona de octubre de 2015 a abril de 2016. Se reclutaron 55 hombres adicionales para participar en entrevistas en profundidad y captar sobre el consumo de alcohol y otros factores relacionados con la adherencia. Los resultados de la encuesta mostraron que aproximadamente el 38% de las PVVIH informaron tener síntomas depresivos moderados a severos. Los síntomas depresivos se asociaron positivamente con mayores niveles de preocupaciones familiares (OR = 1.18, IC 95% = 1.12–1.23), dificultades con el trabajo (OR = 2.04, IC 95% = 1.69–2.69) y la auto-estima relacionado con el VIH ( OR = 1.05, IC 95% = 1.03–1.07), pero un nivel más bajo de satisfacción con el servicio de ART (OR = 0.58 IC 95%: 0.44–0.77). Los resultados de las entrevistas en profundidad mostraron que el tenshun de PVVS (el término para la depresión) se debió a sentimientos de culpa y preocupaciones sobre cómo la familia, los amigos y los vecinos podrían reaccionar a su estado de VIH y la posible pérdida de trabajo como resultado de la divulgación de su estado de VIH en el trabajo. El nivel significativamente más alto de síntomas depresivos entre las PVVIH masculinos en tratamiento de ART indica la necesidad de fortalecer el componente psicológico del tratamiento de PVVIH en la India.
Introduction
Depression is a common mental health problem with symptoms that include sadness, loss of interest or pleasure, feelings of guilt or low self-worth, disturbed sleep or appetite, feelings of tiredness, and poor concentration [1]. It has become a leading contributor to the global burden of disease [2] with an estimated 350 million people suffering from depression globally [3]. The absence of mental health services, especially in low and middle-income countries (LMICs), means that few people receive the treatment they need for depression [4].
Depressive symptoms are highly prevalent among persons living with HIV (PLHIV) especially in LMICs [5–7]. A recent review found that the worldwide prevalence of depression among PLHIV varied widely from 7.2% to 71.9% [8]. In a meta-analysis, depressive disorder in PLHIV was found to be nearly twice that of HIV-negative men and women [9].
A number of factors have been associated with or found to be predictive of depression among PLHIV. The need for lifelong medication, the potential for co-morbidities, the threat of early mortality and widespread experience of social stigma have all been associated with depression [5–7]. PLHIV who are stigmatized feel anxiety, alienation, guilt, worthlessness and helplessness, which contribute to increased depression [10–12]. Internalized stigma, characterized by feelings of worthlessness, self-blame (“I did it to myself”) [13,14] has been shown to result in alienation from family and friends and the breakdown of social support systems, both of which further contribute to depression among PLHIV [15]. For example, a study among PLHIV in Botswana found that men with a higher level of HIV-related self (internalized) stigma were two times more likely to experience depression [16].
Depression is associated with alcohol use. A systematic review in LMICs revealed that alcohol problems are more common in people with depression than those in the general population [17]. Among PLHIV, higher levels of alcohol consumption are associated with increased depressive symptoms [18]. Alcohol and depression interact in PLHIV; drinking acts as a coping mechanism for depression and in turn, contributes to increased depression. A study among Hispanic men living with HIV in the US found that those with higher levels of depression were more likely to report alcohol use during the last three months than those with lower levels of depression [19].
Patient satisfaction with services has been used to predict the short- and long-term effectiveness of substance abuse programs [20,21]. Patient satisfaction has been defined as the extent to which health care experiences in general and antiretroviral treatment in particular match PLHIV expectations [22]. Among PLHIV, higher levels of patient satisfaction are positively associated with better ART adherence [23] and more patient-provider interaction [24]. One study in Norway has found that satisfied patients were more likely to adhere to their treatment, resulting in better clinical outcomes [25].
Previous work among PLHIV has shown an association between family income, family financial supports, the quality of intra-family relationships and depression. A study among PLHIV in Kampala, Uganda demonstrated a significant relationship between depression and concerns about maintaining support for the family, particularly the ability to sustain children’s education [26]. Other studies show that those who were unemployed are more likely to have more depressive symptoms than those employed [27,28]. PLHIV who had a poor relationship with their spouse and belonged to joint families (where conflict can be elevated) were more likely to have higher levels of depression [29]. Among HIV infected caregivers, financial concerns were significantly associated with greater depression [30].
Western and culturally-based concepts of depression
In many parts of the Western world, the term “depression” is well-established both as a diagnosis (e.g. DSM-5) and as a lay term for self- description of transient and chronic mood and mental health status. There are numerous instruments for measuring and diagnosis of both depression and depressive symptoms. The Center for Epidemiologic Studies Depression Scale (CES-D) has been used as a measure of depressive symptoms in culturally diverse populations, including PLHIV, in developed countries and LMICs (the 10-item short form, and a longer 20-item form) [31–36].The short form has been demonstrated to have strong psychometric properties, including predictive accuracy and high correlations with the original 20-item CES-D version in several cross-national settings [37–40].
In India, the English term “depression” (translated into Hindi as udas) has for the most part, not been integrated into national and local languages. Instead, over the last decade the term tenshun, in Hindi, adapted from the English “tension.” has come into common usage (41). The word is used as a verb, “I am tensed,” in relation to a disturbing event, as a noun, as in “I have tenshun because…” and “I always have tenshun since…” indicating chronicity. Tenshun scales developed and tested in South Asian communities [42,43] have been shown to have a high degree of overlap with Western derived and adapted depression scales [42]. As a result, the culturally-based concept of tenshun is related to depressive symptoms. The perceived etiology, symptoms and consequences of depression and depressive symptoms can be easily be explored by structuring qualitative and quantitative questions with reference to tenshun. In this paper, we measure “tenshun” with the CES-D. We use “sources of tenshun”, a culturally specific scale with two subscales developed in India, as a culturally specific means of examining aspects of the lives of PLHIV that contribute to depression.
The purpose of this paper is to describe the frequency and risk of depressive symptoms among alcohol consuming male PLHIV in greater Mumbai using the 10-item CES-D short form and examine the correlates of depressive symptoms and use in-depth interview data to explain the correlations.
Methods
The data for this paper were collected as a part of the NIAAA-funded, Indo-US research and intervention project entitled, “Alcohol and ART Adherence: Assessment, Intervention and Modeling in India. The study is currently in its fifth year and is being conducted in five ART centers in greater Mumbai randomly selected from a total of 13 centers in the study areas. The study design calls for screening for eligibility, enrollment, and collection of baseline data followed by multiple interventions and follow-up data collection points. This paper utilizes data from the baseline survey collected from enrolled participants in all five centers (n=940), along with qualitative data collected through in-depth interviews with 55 alcohol-consuming PLHIV who were separately recruited. The study was approved by the Institutional Review Board of the University of Connecticut Health Center, the India Council for Medical Research, the Health Ministry Screening Committee, the National AIDS Control Organization and Institutional Review Boards of all collaborating agencies and hospitals. Written informed consent in Hindi or Marathi was obtained from all participants in the study.
Eligibility and Screening
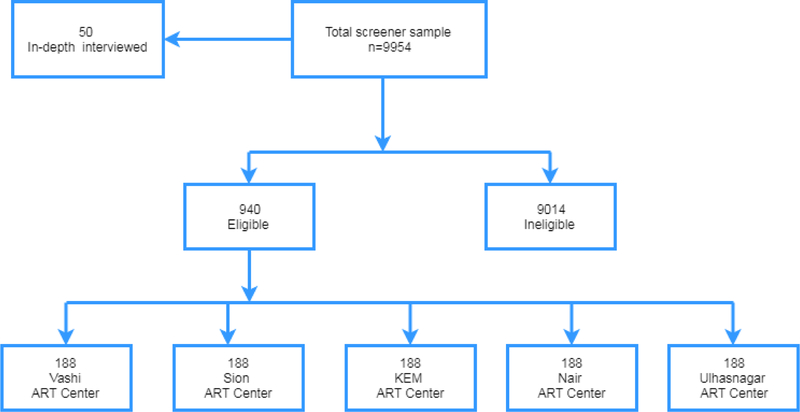
A screening instrument was administered to male PLHIV awaiting treatment to assess eligibility. Eligibility criteria for study enrollment were: (1) on ART treatment for over 6 months; (2) had consumed alcohol during the last 30 days; and (3) 18 years of age and above. Women were not included in the study because female PLHIV alcohol consumers constituted less than 1% of the patients in Maharashtra ART centers [44]. Trained research investigators approached men as they waited for treatment and administered the screening instrument to determine eligibility. A total of 9,954 male PLHIV were screened. Of those screened, 940 PLHIV were eligible, available and consented to join the study, and provided permission to access participants’ medical records. After consenting, participants were administered a baseline survey instrument and a viral load test. Recruitment, enrollment and retention are summarized in Figure 1.
Figure 1:
Flowchart showing the selection of the participants in the study
Baseline Survey Instrument
All registered ART center patients are required to pick up their monthly medication every 30 days, scheduled in advance. The baseline survey instrument was administered after medication pick-up to all eligible and consented PLHIV during the period from October 2015 to April 2016 in all five centers.
Measures
Demographic variables.
Age, educational level, marital status, employment, migration status, monthly household income, time since diagnosis and time on medication. Data on these variables were used as covariates in the analysis.
Depressive symptoms.
Depressive symptoms are measured using the 10-item Center for Epidemiologic Studies-Depression (CES-D) scale which covers depressed mood, feelings of guilt, worthlessness, and helplessness, loss of appetite, and sleep disturbance [45,46], and has been validated in India [47]. The total score ranges from 0–30 (Chronbach’s alpha =.70). The resulting scale was skewed, so it was transformed to a categorized variable by using the standardized cut off of 10 to distinguish none/mild (0–9) from moderate (10–14) and severe (15 or higher) depressive symptoms [46,48].
Family-related concerns are measured using a 7-item scale which was developed and validated based on prior studies in India and formative work in this study [49]. The scale identifies and assesses sources of family-related tenshun including spousal/partner relations, transmission risk, children, extended family relationships and finances. Responses were “To a great extent,” (1) “To some extent,” (2) or “Not at all” (3). The total score ranged from 0–24 with higher scores indicating higher levels of family-related sources of tenshun (The Cronbach’s alpha =.85).
Work difficulties are measured using a 3-item scale with yes/no responses. Participants were asked about their job difficulty, how they were treated at their worksite and whether their HIV status resulted in losing their job or business. The total score ranged from 3–6 with higher scores indicating greater levels of work concerns (Cronbach’s alpha =.60.).
HIV-related self-stigma is assessed using a 16-item scale derived from Berger’s HIV stigma scale [50] validated in India [51] that covers three domains: fears related to disclosure (6 items); negative self-image (5 items); and concerns with public attitudes about people with HIV (5 items). Participants responded to each question using a four-item Likert scale (strongly disagree=1, disagree=2, agree=3 and strongly agree=4). The total score ranged from 16–64 with higher scores indicating greater perception of HIV related self-stigma. (Cronbach alpha = .88).
ART Center service satisfaction is measured using a 5-item scale derived from ethnographic observation and key informant interviewing covering five domains: doctor services, counselor services, medication availability and disbursement, other medication department services and lab testing-related services. Responses were: 1) Not at all satisfied, 2) Somewhat satisfied, 3) Satisfied, 4) Very satisfied. The total score ranges from 4 to 20 with higher scores indicating higher levels of satisfaction (Cronbach alpha = .86).
Alcohol problem drinking is measured using the 10-item Alcohol Use Disorders Identification (AUDIT) questionnaire developed by WHO [52] and validated in India [53] (Cronbach’s alpha = .76). The responses for each item were scored from 0 to 4 with higher scores indicating a high level of alcohol use. The total scores were categorized as low risk (0–7), moderate risk (8–15), high risk (≥16) [54].
ART adherence is measured using the AIDS Clinical Trials Group (ACTG) instrument [55] based on self-reported number of missed doses of ART medication for the 4-day period prior to administration of the baseline survey. The ART non-adherence rate was calculated by dividing the number of missed doses by doses prescribed over a 4-day period. Poor adherence was categorized as <.90 and good adherence as .90 and above [56].
Quantitative Data analysis
Descriptive analyses illustrate the distribution of depressive symptom patterns, socio-demographic characteristics and other relevant variables. The associations between depressive symptoms and socio-demographic characteristics were examined using Chi-square. Univariate and multivariate logistic regression analysis were used to explore the relationship between depression and a series of hypothesized independent variables including family-related concerns, work difficulties, ART Center service satisfaction, HIV self-stigma, 4-day ART adherence and alcohol use (AUDIT) adjusting for demographic and socioeconomic factors (age, education, marriage and employment). Those variables significant at p <0.25 in the univariate models were included in the multivariable regression model. A p value of <.05 is used as an indication of statistical significance.
In-depth Interviews (IDIs) and Qualitative Data Analysis
Fifty-five men, approximately 11 from each of the five ART Centers, constituting a purposive sample who met the study eligibility criteria, were recruited for in-depth interviews lasting one to one and a half hours, conducted by trained research investigators. These interviews explored their perceptions of how they contracted HIV, the impact of HIV on their lives and their families, the process of referral to the ART Center, services received at the ART Center, social support, co-morbidities, alcohol use, their experience with ART use and adherence, their perception of their disease status and their emotional status with special emphasis on depression. Interviews were transcribed, translated into English and entered into Atlas.ti [57]. Code categories were developed based on both the project research model and new issues that emerged from the interview text, creating complementarity, allowing for qualitative explanation of quantitative associations [58]. Multiple project staff coded the text and checked for reliability.
Results
Demographic characteristics
The mean age of the 940 male PLHIV who enrolled in the study and completed the baseline survey was 41.5 years. The number of months since diagnosis of HIV ranged from 7 to 244 with a mean of 68. The number of months since starting ART treatment ranged from 7 to 156 with a mean of 54.
Depressive symptoms
Among alcohol-consuming male PLHIV on ART in the five centers in urban Maharashtra, 38.3% reported moderate to severe depressive symptoms on the 10-item C-ESD short form.
Socio-demographic factors and depressive symptoms
Table 2 presents the results of socio-demographic characteristics of the participants in relation to depressive symptoms. Participants with lower income reported more depressive symptoms than participants who had higher income (p=0.015). Participants who are single were more likely to report depressive symptoms than those who were married (p=0.04). Participants who were employed tended to report more depressive symptoms than those who were unemployed (p=0.08).
Table 2-.
Presence of depressive symptoms by demographic characteristics
| Depression* | |||
|---|---|---|---|
| n | percent | p value | |
| Age | |||
| 19–29 | 19 | 43.2 | 0.69 |
| 30 to 39 | 93 | 36.5 | |
| 40–49 | 178 | 40.2 | |
| 50–59 | 59 | 35.5 | |
| 60 + | 11 | 34.4 | |
| Education | |||
| Illiterate | 41 | 47.1 | 0.06 |
| Primary school | 81 | 38.8 | |
| Secondary school | 92 | 32.5 | |
| High school | 133 | 41.6 | |
| College and above | 13 | 31.7 | |
| Marriage | |||
| Single/divorced/separated/widowed | 91 | 43.8 | 0.04 |
| Married | 269 | 36.7 | |
| Religion | |||
| Hindu | 43 | 36.1 | 0.60 |
| Other | 317 | 38.6 | |
| Migration | |||
| Born in Mumbai | 140 | 38.4 | 0.97 |
| Born outside Mumbai | 220 | 38.3 | |
| Working | |||
| Currently working | 34 | 47.9 | 0.08 |
| No working | 326 | 37.5 | |
| Household income per month | |||
| <12000 INR** | 229 | 41.9 | 0.015 |
| 12000–20000 INR | 99 | 35.1 | |
| >20000 INR | 32 | 28.8 | |
Depression= CES-D score ≥10.
INR: India rupee
The frequencies of all independent variables are shown in Table 3.
Table 3.
Frequencies of independent variables
| Median | IQR* | |
|---|---|---|
| Family-related concerns | 7.4 | 4.1–10.8 |
| Work difficulties | 2.7 | 2.1–3.4 |
| ART service satisfaction | 3.1 | 2.9–3.4 |
| HIV-related self stigma | 40.0 | 36.0–45.0 |
| n | Percent | |
| Audit score | ||
| Low risk | 649 | 69.0 |
| Moderate risk | 245 | 26.1 |
| High risk | 46 | 4.9 |
| 4 day adherence | ||
| < 90 percent | 152 | 16.2 |
| ≥ 90 percent | 778 | 83.8 |
IQR: inter-quartile ranges
Factors associated with depressive symptoms
Table 4 presents the results of univariate and multivariate logistic regression analysis of factors associated with risk of depressive symptoms. The results of multivariate logistic regression model show that each one unit increase in family-related concerns resulted in a 1.18 fold increase in the odds of having depressive symptoms (OR=1.18; 95%CI=1.12–1.23); each one unit increase in work difficulties was associated with a 2.04 fold increase in the odds of having depressive symptoms (OR=2.04; 95%CI=1.69–2.69); each one unit decrease in ART service satisfaction was associated with a 1.4% increase in the odds of having depressive symptoms (OR=0.58 95% CI:0.44–0.77); and each one unit increase in HIV-related self stigma was associated with a 1.05 fold increase in the odds of having depressive symptoms (OR=1.05; 95%CI=1.03–1.07). Neither 4-day ART adherence or alcohol use were associated with depressive symptoms.
Table 4-.
Logistic regression of factors associated with depressive symptoms
| Characteristics | uOR (95%CI) | P Value | aOR (95%CI) | P Value |
|---|---|---|---|---|
| Family-related concerns | 1.16 (1.12–1.20) | <0.001 | 1.18 (1.12–1.23) | <0.001 |
| Work difficulties | 2.88 (2.32–3.57) | <0.001 | 2.04 (1.69–2.69) | <0.001 |
| ART service satisfaction | 0.85 (0.81–0.90) | <0.001 | 0.58 (0.44–0.77) | <0.001 |
| HIV-related self-stigma | 1.09 (1.06–1.11) | <0.001 | 1.05 (1.03–1.07) | <0.001 |
| Audit score | ||||
| Low risk (0–7) | 1 | 1 | ||
| Moderate risk (8–15) | 1.43 (1.06–1.92) | 0.02 | 0.85 (0.59–1.21) | 0.53 |
| High risk (≥16) | 1.52 (0.83–2.77) | 0.17 | 1.00 (0.51–1.91) | 0.95 |
| 4 day adherence | ||||
| < 90 percent | 1 | 1 | ||
| ≥ 90 percent | 0.68 (0.48–0.96) | 0.03 | 1.10 (0.73–1.16) | 0.63 |
The final model was adjusted for age; education, marital status, employment, household income and time on ART medication; uOR: unadjusted Odds Ratio; aOR: adjusted Odds Ratio; CI: confidence interval.
Explaining associations: the Qualitative IDI data
The results of the regression identify the independent variables associated with depressive symptoms and include family-related concerns, work difficulties, ART service satisfaction, and HIV-related self-stigma. In this section, we go beyond the associations and utilize the unique advantages of the qualitative data to examine the ways in which participants explain the interaction of the independent variables with depressive symptoms using the culturally relevant term of tenshun.
Family-related concerns as a source of tenshun
Examples of family concerns included negative relationships with wives, children, and extended family members, household finances, disclosure of HIV status, support for HIV treatment, and planning for the future. Families act both as sources of tenshun for men and as a positive force in reducing tenshun. When the family was at the center of a supportive social environment, concerns about managing HIV treatment and household income were mitigated, and respondents described having less concern about the future of the family. When the relationship with family was negative and communication was difficult, financial, and treatment management concerns were perceived by PLHIV as resting solely on their shoulders, thus resulting in significant tenshun.
I don’t like having tension and stress. Now I only think that to take care for family, my mother and father, and to educate my son for his good future, to keep my family happy. HIV positive people taking tenshun, I don’t like that. Patient should not take tenshun of having HIV illness, “Tension mansala marun takte” (tenshun kills the patient!). He should think about his future life and family. (31 years old, 9 years education, married 9 years, 1 Child)
Work difficulties as a source of tenshun
Male PLHIV also described reactions they faced at work as sources of tenshun. Some described how disclosure of their HIV status at work led to job termination, while others feared the loss of a job or stigmatization resulting from co-worker gossip and shunning.
The place where I work there is one fellow who is aware about my status; he often visits my paan shop [place for purchasing betelquid with tobacco). Yesterday he was come in the evening and he had drunk alcohol, so he was using abusive language and using my name. Hence, I was feeling sad, and felt hurt. I used to blame on myself for that. Because of that big mistake, people are behaving with me badly. (Age 35, Married, 2 Children)
ART Service Satisfaction as a source of tenshun
Men describe ART services as a source of tenshun:
Every time we have to stand in the queue for long time. We have to meet the counselor, doctor and pharmacist to collect medicine. ART center opens at 9 am, but doctor comes at 10 am. We have to wait for 3–4 hours in the ART center…Sometimes I think I should stop the medicine because of irritability. (47 years old, 12 years of education, married for 22 years)
A subset of men described how the counselling they had received at the ART centers had reduced their tenshun by giving them new coping techniques or providing health and nutrition information.
The counseling which I was provided from the doctor helped me to develop my confidence and it helped me reduce my tenshun and worries. Then doctor told me about food habits so I followed that, I used to drink milk every day and also eat egg. Now I am staying alone, so I make my food own. I take my medicine regular and on time, I did not skip a single dose of medicine. I think because of this my CD4 count was increased. (33 years old, 10 years of education, never married)
HIV-related self stigma as a source of tenshun
Men described feelings of guilt and internal stigma as sources of tenshun. For a subset of men, their tenshun caused them extreme mental anguish and suicide ideation. Many men reported greater internalized stigma associated with tenshun in the first few months after their diagnosis, which decreased as they learned to manage their illness.
Some time I got angry on myself. I always ask the question to myself, what I did. And how you will face to the society? But I knew this is happened because of me. I have guilt also. And sometime I feel to finish myself. (36 years old, 12 years of education, never married)
Some men who described having no shame or guilt associated with their HIV status reported experiencing little or no tenshun.
No, I do not feel myself guilt and I do not blame me or others. I am taking my medicine regular and on time, so I follow this timetable regularly. I always carry the medicine along with me (he took out one pouch from packet in which medicine were kept, and showed it), these are tablets. Otherwise I do not think negative or do not have tenshun for taking medicine. I am a very careful man. (31 years old, 9 years of education, married for 9 years)
Discussion
The results of this study provide an estimate of the level of depression in alcohol consuming male PLHIV on ART in urban Maharashtra, India and identify some of the main factors associated with higher or lower levels of depressive symptoms. In the baseline sample of 940, nearly 40% of PLHIV reported scores of 10 or above on the C-ESD, indicating the need for further screening and referral for clinical assessment. These results are consistent with earlier studies confirming the high level of depressive symptoms among PLHIV in India, ranging from 29% to 58.1% [59,60]. The level of depressive symptoms in this study population was higher than the level of depression among PLHIV in Vietnam (15%) [61] and Botswana (31.4%) [16] and lower than the level of depression among Hispanic PLHIV in the US (65%) [19].
Higher levels of HIV-related internalized stigma were significantly associated with higher levels of depressive symptoms, a pattern consistent with previous studies in India and other developing countries [16,62–64]. The qualitative data illustrate how HIV (internalized) stigma contributed to tenshun for the men in our study. Men’s tenshun resulted from feelings of guilt and concerns about how family, friends, and neighbors might react to their HIV status and shame that their behaviors had caused their illness. A small subset of men described how tenshun caused them extreme mental anguish and suicidal ideation.
PLHIV vary in their assessment of whether the services at ART Centers that include meetings with the HIV counselor, the medical staff and the pharmacy meet their needs. All urban Centers in Maharashtra now exceed their planned capacity resulting in longer wait times, without a concomitant expansion of services. PLHIV who were less satisfied with ART services were more likely to report having depressive symptoms. This result is comparable to of PLHIV in Ethiopia in which having mild to moderate depression was associated with a lower level of satisfaction with HIV treatment services [65].
This study has shown that family-related concerns play an important role in relation to depressive symptoms among PLHIV. Financial burdens and worries about the ability to support children were associated with higher levels of depressive symptoms in among this population. These results are consistent with a previous study in India in which PLHIV with low incomes were more likely to experience more depressive symptoms [60].
Limitations need to be considered when interpreting the finds of this study. First, this was not a random sample; all eligible people were approached and participants were free to consent or not. Second, the study did not include men who have sex with men (MSM) who are a major risk group for HIV in India [66]. Only three participants out of 940 PLHIV in this study reported their MSM status, which may be undercount given the stigma and discrimination associated with MSM in India [67]. Third, this is a sample of alcohol consuming PLHIV in only five ART centers. The results may not be generalizable to PLHIV who do not consume alcohol. India is an extremely diverse country so that these results should be the basis for studies in rural areas and other States. Depressive symptoms, alcohol use problems and ART adherence was based on self-report, which may be subject to social desirability and recall bias and as such may under-estimate frequency. Given the cross-sectional nature of this study, a causal relationship among the study variables cannot be established.
In summary, those male PLHIV that consume alcohol and are being treated at an ART Center who reported greater internalized stigma, had a more negative view of ART Center services, more work-related difficulties and a greater number of family-related concerns had a greater degree of moderate or severe depressive symptoms. Those PLHIV with less internalized stigma, a more positive view of ART Center services, less difficulties at work, and fewer family-related concerns reported an absence of or only mild depressive symptoms. These results have direct implications for counseling PLHIV at ART centers.
The concept of tenshun in Indian society provides an appropriate, salient and culturally based pathway for discussing depressive symptoms. It is also useful in identifying the elements in the lives of male PLHIV that contribute to their psychological concerns. The use of the concept of tenshun by counselors and medical staff to initiate dialogue about mental health issues avoids the stigma associated with mental illness while gaining insights into PLHIV psychosocial concerns.
The parent study used these formative results to implement a multilevel intervention that included individual counseling, group intervention, PLHIV collective advocacy and an integrated package of all three interventions for positive impact on the independent variables that contribute to depressive symptoms. While ART has had a dramatic effect on the physical quality of life for PLHIV, it is important to recognize that the psychosocial aspects of HIV infection have remained largely unaddressed in low and middle-income countries for both men and women and should be included in on-going treatment approaches.
Table 1:
Participant’s characteristics
| n | Percent | |
|---|---|---|
| Age | ||
| 19–29 | 44 | 4.7 |
| 30 to 39 | 255 | 27.1 |
| 40–49 | 443 | 47.1 |
| 50–59 | 166 | 17.7 |
| 60 + | 32 | 3.4 |
| Education | ||
| Illiterate | 87 | 9.3 |
| Primary school | 209 | 22.2 |
| Secondary school | 283 | 30.1 |
| High school | 320 | 34.0 |
| College and above | 41 | 4.4 |
| Months since diagnosis of HIV (Mean, SD*) | 68 | 42 |
| Months since starting ART treatment (Mean, SD) | 54 | 31 |
| Currently married | 298 | 82.5 |
| Religion | ||
| Hindu | 320 | 88.6 |
| Other | 41 | 11.4 |
| Migration | ||
| Born in Mumbai | 136 | 37.7 |
| Born outside Mumbai | 225 | 62.3 |
| Currently working | 334 | 92.5 |
SD: standard deviation.
Acknowledgments
This project is a collaboration of the India offices of the International Center for Research on Women, the Population Council, the Network of Maharashtran Positive People (NMP+), the University of Connecticut School of Medicine, and the Institute for Community Research in Hartford, CT. We would like to acknowledge the project team with special thanks to the research investigators who so diligently and effectively collected the interview and survey data for this article and project.
Funding: This study was funded by National Institute on Alcohol Abuse and Alcoholism Grant No. U01AA021990-01.
Footnotes
Compliance with Ethical Standards:
Ethical approval: All procedures performed in the study involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards
Informed consent: Informed consent was obtained from all individual participants included in the study.
Conflict of Interest: Toan Ha declares that he has no conflict of interest. Stephen L. Schensul declares that he has no conflict of interest. Mitchell Irving declares that he has no conflict of interest. Marie A. Brault declares that she has no conflict of interest. Jean J. Schensul declares that she has no conflict of interest. Priti Prabhughate declares that she has no conflict of interest. Melita Vaz declares that she has no conflict of interest
References
- 1).American Psychiatric Association. Diagnostic and statistical manual of mental disorders 5th ed. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- 2).World Health Organization. Depression Available at: http://www.who.int/mediacentre/factsheets/fs369/en/. Accessed December, 2017.
- 3).Marcus M, Yasamy T, Ommeren M, Chisholm D, Shekhar S. Depression A Global Public Health Concern Available at: http://www.who.int/mental_health/management/depression/who_paper_depression_wfmh_2012.pdf. Accessed December, 2017.
- 4).Rathod S, Pinninti N, Irfan M, Gorczynski P, Rathod P, Gega L, et al. Mental Health Service Provision in Low-and Middle-Income Countries. Health Services Insights 2017;10:1178632917694350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5).Nakimuli-Mpungu E, Bass JK, Alexandre P, et al. Depression, Alcohol Use and Adherence to Antiretroviral Therapy in Sub-Saharan Africa: A Systematic Review. AIDS Behav 2012;16(8):2101–2118. [DOI] [PubMed] [Google Scholar]
- 6).Mayston R, Kinyanda E, Chishinga N, Prince M, Patel V. Mental disorder and the outcome of HIV/AIDS in low-income and middle-income countries: a systematic review. AIDS 2012;26(S117–35). [DOI] [PubMed] [Google Scholar]
- 7).Valente SM. Depression and HIV disease. Journal of the Association of Nurses in AIDS Care 2003;14(2):41–51. [DOI] [PubMed] [Google Scholar]
- 8).Chaudhury S, Bakhla AK, Saini R. Prevalence, impact, and management of depression and anxiety in patients with HIV: a review. Neurobehavioral HIV Medicine 2016;7:15–30. [Google Scholar]
- 9).Ciesla JA, Roberts JE. Meta-Analysis of the relationship between HIV infection and risk for depressive disorders. Am J Psychiatry 2001;158:725. [DOI] [PubMed] [Google Scholar]
- 10).Crandall CS, Coleman R. AIDS related stigmatization and the disruption of social relationships. J Soc Personal Relationship 1992;9:163–177. [Google Scholar]
- 11).University of California, San Francisco. Comprehensive, up-to-date information on HIV/AIDS treatment and prevention from the University of California San Francisco.Coping with HIV/AIDS: Mental Health 2016; Available at: http://hivinsite.ucsf.edu/hiv?page=pb-daily-mental#S2X. Accessed December, 23, 2017.
- 12).Shanthi AG, Damodharan J, Priya G. Depression and coping: a study on HIV positive men and women. Sri Ramachandra Journal of Medicine 2007; 15–19.
- 13).Yi S, Chhoun P, Suong S, Thin K, Brody C, Tuot S. AIDS-Related Stigma and Mental Disorders among People Living with HIV: A Cross-Sectional Study in Cambodia. PLoS ONE 2015; 10(3):e0121461 10.1371/journal.pone.0121461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14).Rao D, Chen WT, Person CR, et al. Social Support Mediates the Relationship between HIV Stigma and Depression/Quality of Life among People Living with HIV in Beijing, China. Int J STD AIDS 2012. July; 23(7): 481–484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15).Gerbi GB, Habtemariam T, Robnett V, Nganwa D, Tameru B. Psychosocial factors as predictors of HIV/AIDS risky behaviors among people living with HIV/AIDS. Journal of AIDS and HIV Research 2012;4(1):8–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16).Gupta R, Dandu M, Packel L, et al. Depression and HIV in Botswana: a population-based study on gender-specific socioeconomic and behavioral correlates. PLoS One 2010;5(12):e14252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17).Sullivan EL, Fiellin DA, O’Connor PG. The prevalence and impact of alcohol problems in major depression: A systematic review. The American Journal of Medicine 2005;118:330–341. [DOI] [PubMed] [Google Scholar]
- 18).Sullivan LE, Saitz R, Cheng DM, Libman H, Nunes D, Samet JH. The impact of alcohol use on depressive symptoms in HIV-infected patients. Addiction 2008; 103(9) :1461–1467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19).De Santis J, Gonzalez-Guarda RM, Provencio-Vasquez E. Psychosocial and Cultural Correlates of Depression among Hispanic Men with HIV Infection: A Pilot Study. Journal of Psychiatric and Mental Health Nursing 2012;19(10):860–869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20).Carlson MJ, Gabriel RM. Patient satisfaction, use of services, and one-year outcomes in publicly funded substance abuse treatment. Psychiatr Serv 2001. September;52(9):1230–6. [DOI] [PubMed] [Google Scholar]
- 21).Zhang Z, Gerstein DR, Friedmann DP. Patient Satisfaction and Sustained Outcomes of Drug Abuse Treatment. J Health Psychol 2008;13(3):338–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22).Pascoe GC. Patient satisfaction in primary health care: a literature review and analysis. Eval Program Plann 1983;6:185–210. [DOI] [PubMed] [Google Scholar]
- 23).Roberts KJ. Physician-Patient Relationships, Patient Satisfaction, and Antiretroviral Medication Adherence Among HIV-Infected Adults Attending a Public Health Clinic. AIDS Patient Care and STDs 2002;16(1):43–50. [DOI] [PubMed] [Google Scholar]
- 24).Devnani M, Gupta AK, Wanchu A, Sharma RK. Factors associated with health service satisfaction among people living with HIV/AIDS: a cross sectional study at ART center in Chandigarh, India. AIDS Care 2012;24(1):100–107. [DOI] [PubMed] [Google Scholar]
- 25).Guldvog B Can patient satisfaction improve health among patients with angina pectoris. Int J Qual Health Care 1999;11:233–240. [DOI] [PubMed] [Google Scholar]
- 26).Wagner GJ, Ghosh-Dastidar B, Dickens A, et al. Depression and its Relationship to Work Status and Income Among HIV Clients in Uganda. World J AIDS 2012;2(3):126–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27).Ngum PA, Fon PN, Ngu RC, Verla VS, Luma HN. Depression among HIV/AIDS Patients on Highly Active Antiretroviral Therapy in the Southwest Regional Hospitals of Cameroon: A Cross-Sectional Study. Neurology and Therapy 2017;6(1):103–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28).Ong JY, Lee JS, Seo YB, et al. Depression Among HIV-infected Patients in Korea: Assessment of Clinical Significance and Risk Factors. Infection & Chemotherapy 2013;45:211–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29).Bhatia MS, Munjal S. Prevalence of Depression in People Living with HIV/AIDS Undergoing ART and Factors Associated with it. Journal of Clinical and Diagnostic Research 2014;8(10):WC01–WC04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30).Land H, Hudson SM, Stiefel B. Stress and Depression among HIV-Positive and HIV-Negative Gay and Bisexual AIDS Caregivers. AIDS and Behavior 2003;7:41–53. [DOI] [PubMed] [Google Scholar]
- 31).Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Measure 1977;1:385–401. [Google Scholar]
- 32).Bernard C, Dabis F, de Rekeneire N. Prevalence and factors associated with depression in people living with HIV in sub-Saharan Africa: A systematic review and meta-analysis. PLoS One 2017;12(8):e0181960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33).Vilagut G, Carlos G, Forero CG, Barbaglia G, Alonso J. Screening for Depression in the General Population with the Center for Epidemiologic Studies Depression (CES-D): A Systematic Review with Meta-Analysis. PLoS ONE 2016;11(5 (e0155431)). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34).Schrag A, Barone P, Brown RG, et al. Depression rating scales in Parkinson’s disease: critique and recommendations. Mov Disord 2007;22(8):1077–1092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35).Seth P, Kidder D, Pals S, et al. Psychosocial Functioning and Depressive Symptoms Among HIV-Positive Persons Receiving Care and Treatment in Kenya, Namibia, and Tanzania. Prevention Science : The Official Journal of the Society for Prevention Research 2014;15(3):318–328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36).Ickovics J, Hamburger M, Vlahov D, et al. Mortality, CD4 count decline and depressive symptoms among HIV-seropositive women. Longitudinal analysis from the HIV Epidemiology Research Study. JAMA 2001;285:1466–1474. [DOI] [PubMed] [Google Scholar]
- 37).Zhang W, O’Brien N, Forrest JI, et al. Validating a Shortened Depression Scale (10 Item CES-D) among HIV-Positive People in British Columbia, Canada. PLoS ONE 2012;7(7):e40793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38).Chen H, Mui AC. Factorial validity of the Center for Epidemiologic Studies Depression Scale short form in older population in China. Int Psychogeriatr 2014;26(1):49–57. [DOI] [PubMed] [Google Scholar]
- 39).Baron EC, Davies T, Lund C. Validation of the 10-item Centre for Epidemiological Studies Depression Scale (CES-D-10) in Zulu, Xhosa and Afrikaans populations in South Africa. MC Psychiatry 2017;17(1):6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40).Mohebbi M, Nguyen V, McNeil JJ, et al. Psychometric properties of a short form of the Center for Epidemiologic Studies Depression (CES-D-10) scale for screening depressive symptoms in healthy community dwelling older adults. General hospital psychiatry 2018;51:118–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41).Maitra S, Brault MA, Schensul SL, et al. An Approach to Mental Health in Low- and Middle-Income Countries: A Case Example from Urban India. International Journal of Mental Health 2015;44(3):215–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42).Weaver LJ. Tension Among Women in North India: An Idiom of Distress and a Cultural Syndrome. Cult Med Psychiatry 2017. March;41(1):33–35. [DOI] [PubMed] [Google Scholar]
- 43).Karasz A, Patel V, Kabita M, Shimu P. “Tension” in South Asian women: developing a measure of common mental disorder using participatory methods. Prog Community Health Partnersh 2013;7(4):429–441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44).Schensul SL, Ha T, Schensul JJ, et al. The Role of Alcohol on Antiretroviral Therapy Adherence Among Persons Living With HIV in Urban India. J Stud Alcohol Drugs 2017;78(5):716–724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45).Radloff LS. The CES-D scale. Applied Psychological Measurement 1977;1(3):385–401. [Google Scholar]
- 46).Björgvinsson T, Kertz SJ, Bigda-Peyton JS, McCoy KL, Aderka IM. Psychometric properties of the CES-D-10 in a psychiatric sample. Assessment 2013;20(4):429–436. [DOI] [PubMed] [Google Scholar]
- 47).Chokkanathan S, Mohanty J. Factor structure of the CES-D scale among older adults in Chennai, India. Ageing and Mental Health 2013;17(4):517–525. [DOI] [PubMed] [Google Scholar]
- 48).Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). Am J Prev Med 1994;10(2):77–84. [PubMed] [Google Scholar]
- 49).Schensul SL, Saggurti N, Singh R, Verma RK, Nastasi BK, Mazumder PG. Multilevel perspectives on community intervention: An example from an Indo-U.S. HIV prevention project in Mumbai, India. American Journal of Community Psychology 2009;43(3):277–291. [DOI] [PubMed] [Google Scholar]
- 50).Berger BE, Ferrans C, Lashley F. Measuring stigma in people with HIV: Psychometric assessment of the HIV stigma scale. Research in Nursing and Health 2001;24:518–529. [DOI] [PubMed] [Google Scholar]
- 51).Steward WT, Herek GM, Ramakrishna J, et al. HIV-related stigma: Adapting a theoretical framework for use in india. Soc Sci Med 2008;67(8):1225–1235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52).Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of The Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption-II. Addiction 1993;88(6):791–804. [DOI] [PubMed] [Google Scholar]
- 53).Pal HR, Jena R, Yadav D. Validation of the Alcohol Use Disorders Identification Test (AUDIT) in urban community outreach and de-addiction center samples in north India J Stud Alcohol 2004. November;65(6):794–800. [DOI] [PubMed] [Google Scholar]
- 54).Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. AUDIT-The Alcohol Use Disorders Identification Test Guidelines for Use in Primary Care Second ed.: World Health Organization; 2001. [Google Scholar]
- 55).Chesney MA, Ickovics JR, Chambers DBea. Self-reported adherence to antiretroviral medications among participants in HIV clinical trials: The AACTG adherence instruments. Patient care committee & adherence working group of the outcomes committee of the adult AIDS clinical trials group (AACTG). AIDS Care 2000;12(3):255–266. [DOI] [PubMed] [Google Scholar]
- 56).Pahari S, Roy S, Mandal A, Kuila S, Panda S. Adherence to anti-retroviral therapy & factors associated with it: a community based cross-sectional study from West Bengal, India. The Indian Journal of Medical Research 2015;14(2):301–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57).Friese S. User’s manual for ATLAS.ti 6.0, ATLAS.ti Scientific Software Development. Berlin: GmbH.: 2013. 2013. [Google Scholar]
- 58).Schensul S Using ethnograph to build a survey instrument. Cultural Anthropology Methods 1993;5(2):9–9. [Google Scholar]
- 59).Sivasubramanian M, Mimiaga MJ, Mayer KH, et al. Suicidality, clinical depression, and anxiety disorders are highly prevalent in men who have sex with men in Mumbai, India: findings from a community-recruited sample. Psychol Health Med 2011;16(4):450–460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60).Bhatia MS, Munjal S. Prevalence of Depression in People Living with HIV/AIDS Undergoing ART and Factors Associated with it. Journal of Clinical and Diagnostic Research 2014;8(10):WC01–WC04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61).Esposito CA, Steel Z, Gioi TM, Huyen TTN, Tarantola D. The Prevalence of Depression among Men Living With HIV Infection in Vietnam. American Journal of Public Health 2009;99(Suppl 2):S439–S444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62).Kumarasamy N, Safren SA, Raminani SR, et al. Barriers and facilitators to antiretroviral medication adherence among patients with HIV in Chennai, India: a qualitative study. AIDS Patient Care STDS 2005;19:526–537. [DOI] [PubMed] [Google Scholar]
- 63).Li L, Lee S, Thammawijaya P, Jiraphongsa C, Rotheram-Borus MJ. Stigma, social support, and depression among people living with HIV in Thailand. AIDS Care 2009;21(8):1007–1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64).Tesfaw G, Ayano G, Awoke T, et al. Prevalence and correlates of depression and anxiety among patients with HIV on-follow up at Alert Hospital, Addis Ababa, Ethiopia. BMC Psychiatry 2016;16(1):368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65).Yakoba B, Ncamaa PB. Client satisfaction: correlates and implications for improving HIV/AIDS treatment and care services in southern Ethiopia. Int Health 2016;8(292):298. [DOI] [PubMed] [Google Scholar]
- 66).Solomon SS, Mehta SH, Srikrishnan AK, et al. High HIV prevalence and incidence among MSM across 12 cities in India. AIDS 2015; 29(6): 723–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67).Chakrapani V, Newman PA, Shunmugam M, McLuckie A, Melwin F. Structural violence against Kothi-identified men who have sex with men in Chennai, India: a qualitative investigation. AIDS Educ Prev 2007. August;19(4):346–64. [DOI] [PubMed] [Google Scholar]