Abstract
Heart attacks kill more Americans than all cancers combined. Fatal heart attack victims have no symptoms until minutes before they die, hence early detection of high-risk asymptomatic individuals is needed. Even though heart attacks kill and cost more than cancers, as a nation we spend over 20 times more on screening for asymptomatic cancer than for asymptomatic atherosclerotic cardiovascular disease (ASCVD), the underlying cause of heart attacks. Currently, payers only cover screening for risk factors of ASCVD such as blood pressure and blood cholesterol. This approach tends to miss high-risk and over-treat low-risk individuals. Although treadmill stress testing with ECG is not indicated for ASCVD detection in asymptomatic individuals, it is done often, and frequently leads to misleading conclusions or unnecessary downstream diagnostic procedures. For example, former President Clinton had passed his treadmill stress tests for several years during his presidential annual checkup but had a heart attack shortly after his presidency. This common practice is a waste of our limited resources. Instead, a more accurate risk assessment using coronary artery calcium (CAC) testing is available; and has just been adopted by ACC/AHA guidelines, however payers do not cover it. CAC is measured non-invasively with a 5-minute CT-scan of the heart, and costs less than $200, whereas cancer screening with colonoscopy and mammography costs over $3000. There is an opportunity to save lives and dollars if CAC testing is covered for appropriately selected individuals. Texas has already passed HB1290 to mandate CAC coverage. Other states must step up and take actions.
Keywords: Cardiovascular disease (CVD), Atherosclerotic cardiovascular disease (ASCVD); Coronary artery calcium (CAC), Atherosclerosis, Vulnerable patient, Computed tomography (CT) scan
1. Introduction
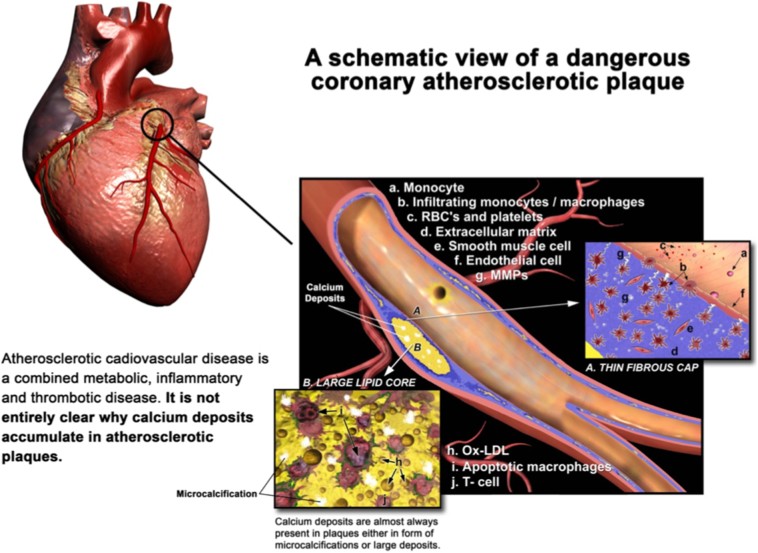
Cardiovascular disease (CVD) is the leading cause of death in America. On average, every 38 s one person dies of CVD in the U.S.(Benjamin et al., 2017) Unlike cancers for which numerous underlying pathologies exist, in CVD the majority of deaths and disabilities result from one underlying pathology: atherosclerosis. Heart attack and stroke are the two most common manifestations of atherosclerotic cardiovascular disease (ASCVD). Atherosclerosis is a combined metabolic, inflammatory, and thrombotic disorder that is chronic and silent until very late stages. It starts from a gradual deposit of lipids under the endothelial layer of certain arteries that instigates both cellular and humoral responses from the body's immune system. Over time this process leads to the formation of atherosclerotic plaques inside the arterial wall (Fig. 1).
Fig. 1.
A schematic view of a dangerous coronary atherosclerotic plaque. This figure illustrates various molecular and cellular players in the development of a high-risk atherosclerotic plaque inside the wall of a coronary artery. Permission obtained from Society for Heart Attack Prevention and Eradication.
Such plaques can be found in multiple locations throughout the arterial tree; however, they are most dangerous in the coronary and carotid arteries. Due to mechanisms yet to be completely understood, the vast majority of these plaques become calcified.(Schurgers et al., 2018) Atherosclerotic plaques may progressively narrow the arterial lumen without causing symptoms. Certain plaques may become inflamed and vulnerable to rupture or erode, resulting in a blood clot that cuts off flow downstream. The thrombotic complications of vulnerable plaques in the coronary arteries results in sudden interruption of blood flow to myocardium causing a heart attack or sudden death. Similarly, such complications in the carotid arteries can lead to stroke. Individuals with vulnerable plaques usually have other characteristics, such as vulnerable blood and vulnerable myocardium, that contribute to the total vulnerability to acute events. Early detection and treatment of such vulnerable patients have been the focus of research in preventive cardiology for a long time; unfortunately not much progress has been made..(Naghavi et al., 2003a; Naghavi et al., 2003b) Heart attack and stroke cause far more deaths in the US than all cancers combined.(Benjamin et al., 2017) Despite this sobering fact, screening for asymptomatic cancer is widely accepted, but screening for asymptomatic ASCVD is not. Sadly, most patients who die from a heart attack have no symptoms until about an hour before they die. Since the 1980s, standards of preventive cardiovascular testing have been limited to testing for high cholesterol, high blood pressure and other risk factors of atherosclerosis which were discovered in 1959 by the Framingham Heart Study.(Dawber et al., 1959) Noninvasive detection of atherosclerosis itself by imaging was not possible then, but it is now, and costs less than a mammography or colonoscopy. Despite a mountain of evidence suggesting that early detection and treatment of ASCVD can save lives and money, there is no initiative from healthcare policymakers to change the outdated status quo. Furthermore, there is no financial incentive for the medical industry to invest in the primary prevention of ASCVD. Instead, every year the medical industry introduces expensive new products (catheters, stents, surgical instruments, and pharmaceutical drugs) for treatment of patients during and after a heart attack. The latter is called secondary prevention, i.e., preventing recurrent heart attacks. Ironically, the financial incentive for prevention of the second heart attack is far greater than the financial incentive for prevention of the first heart attack.(Naghavi, 2010) In this paper we review evidence that indicates that noninvasive detection of atherosclerosis is superior to the status quo, both for early detection and treatment of high-risk patients, and for reducing unnecessary therapy in low-risk individuals. We urge healthcare policymakers to examine the evidence and take actions similar to that taken in the state of Texas (HB1290, 2006).
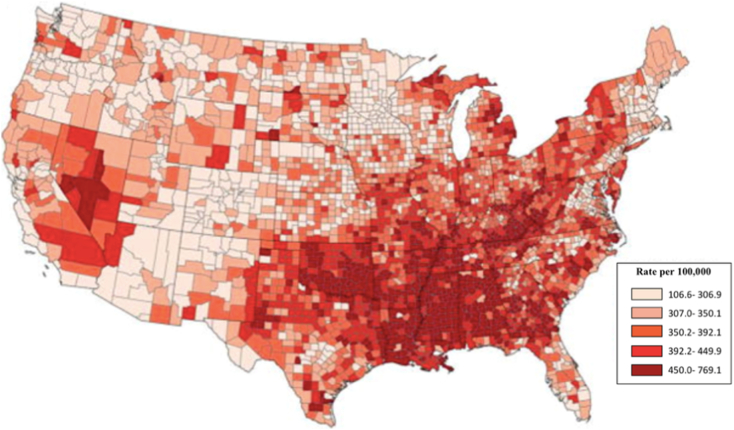
2. Cardiovascular disease map
The prevalence of CVD and its most common component, ASCVD, is increasing across the United States and is expected to double by 2050. (Casper et al., 2016; Heidenreich et al., 2011) In particular the Southern and Western regions of the U.S. have the highest prevalence and incidence (Fig. 2).
Fig. 2.
Heart disease death map: South and West have the highest rates. Age-adjusted heart disease death rates in ≥35 years old by county and quintile ranking (8).
In the West, Nevada has the highest rate of heart disease followed by California. In the Southeast, Mississippi has the highest rate of heart disease followed by Oklahoma. Despite decades of public education about behavioral risk factors for CVD such as unhealthy diet, the American Heart Association reported that the prevalence of an ideal diet score between 2002 and 2012 increased from only 0.7% to 1.5% in adults, meaning 98.5% of adults are still not following an ideal healthy diet. The need for new strategies for prevention could not be clearer.(Writing Group, 2016)
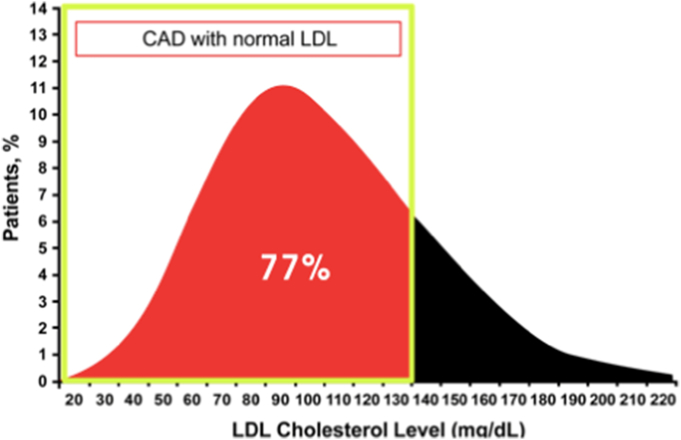
3. What is wrong with the status quo?
Measuring CVD risk factors such as age, smoking, hypertension, diabetes, and dyslipidemia has been the status quo for estimating the risk of future ASCVD events. These risk factors are drawn from population-based studies and do not translate to personal, specific risk in an individual. Many individuals with these risk factors will not experience an ASCVD event in their lifetime; conversely many patients who actually experience an ASCVD event do not have a high risk according to risk calculators. For example, in a study based on American Heart Association's Get with the Guidelines database, 77% of 136,000 patients who were diagnosed with coronary artery disease in the emergency room had normal LDL cholesterol levels (Fig. 3).(Sachdeva et al., 2009)
Fig. 3.
Of 136,905 patients hospitalized with CAC, 77% had normal LDL levels below 130 mg/dl. Red shows percentage of patients with a normal LDL cholesterol level but experienced a heart disease event (11).
Sir Winston Churchill was 91 when he died in his sleep. He was overweight and a smoker. In contrast, the famous marathoner, Jim Fixx, was 53 when he died of a heart attack. He was very fit and did not smoke. Based on apparent risk factors, Fixx's heart attack risk was fairly low, and Churchill's was very high. Fixx is not the only marathon runner who was found to have atherosclerosis. A study was done examining 49 marathon runners who had participated in over 22 marathons.(Burgstahler et al., 2017) Atherosclerosis was diagnosed in 56% of the runners.(Casper et al., 2016) None of them smoked, had high cholesterol, or any other risk factors that stood out. Therefore, the known ASCVD risk factors do not always tell the full story regarding who is going to have an ASCVD event. If Jim Fixx had an imaging study for atherosclerosis, his outcome may have been much different.
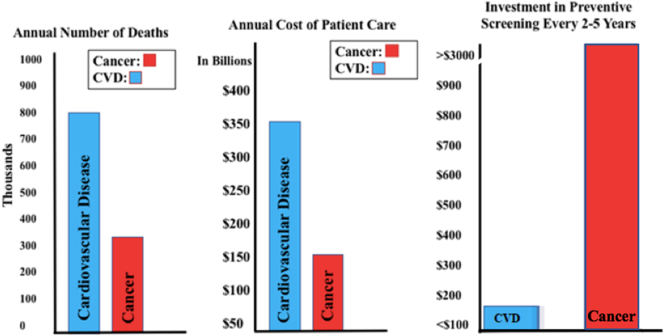
Another problem with the status quo is that ASCVD kills and costs more than all cancers combined; nonetheless, investment in screening for prevention and treatment of asymptomatic ASCVD is far less than that of cancers. While two types of cancer screening (mammography for breast cancer and colonoscopy for colorectal cancer) cost over $3000 and are paid for by insurance companies, ASCVD screening is still limited to less than $100 covered for measuring risk factors (Fig. 4). Unfortunately, because of lack of insurance coverage, physicians today are not testing for atherosclerosis.
Fig. 4.
Disparity between the burden of the disease (cardiovascular and cancer) versus the investment made in related preventive screening. Screening test coverage for primary prevention of cardiovascular disease is <10% of the coverage for screening for primary prevention of cancer.
Based on data from the National Center for Health and Statistics.
In summary, the main problem with the status quo is that we as a nation put more money to fix a heart attack during and after it happens rather than to prevent it in the first place. Furthermore, we use a population-based statistical tool for risk assessment in an individual to decide who needs preventive intervention. We need to advance to personalized risk assessment using noninvasive detection of atherosclerosis with a coronary artery calcium (CAC) score, the most studied and evidence-based test that goes beyond conventional risk assessment.
4. What are the advantages of the CAC score over the status quo?
The proof of the benefits of the CAC test lies in the hundreds of scientific studies published so far. Budoff et al. followed over 25,000 asymptomatic patients over 12 years who were referred for coronary artery calcium scoring. (Budoff et al., 2007) Out of 1000 patients who had a CAC score of 0, over 99% lived. On the contrary, only 73% of patients who had a high CAC score over 1000 survived.(Budoff et al., 2007) Another study of >85,000 patients showed that those with high CAC score were 8 times more likely to experience a cardiac event than those without. (Sarwar et al., 2009) Both studies show us the clear correlation of a high CAC score to a high risk of an ASCVD event, and low CAC score to low a risk. Perhaps the strongest evidence favoring CAC over traditional risk factors came from MESA (Multi-Ethnic Study of Atherosclerosis), a large NIH (National Institutes of Health) funded study on ASCVD, that compared noninvasive tests to detect ASCVD in 6800 asymptomatic individuals and followed them for over 10 years. CAC was the most powerful predictor of ASCVD risk.(Yeboah et al., 2012) Data from 6 studies of 27,622 asymptomatic patients were summarized in an ACCF/AHA clinical expert consensus document that examined predictors of ASCVD events.(Greenland et al., 2007) The 11,815 subjects who had CAC scores of 0 had a low rate of events over the subsequent 3 to 5 years (0.4%, based on 49 events). CAC scores between 100 and 400 increased the risk to 4.3% (95% CI 3.5 to 5.2; p < 0.0001); and scores from 400 to 1000 had a 7.2% risk (95% CI 5.2 to 9.9; p < 0.0001). Any score above 1000 indicated a risk of 10.8% events over 3–5 years (95% CI 4.2 to 27.7; p < 0.0001). No conventional risk factor has shown such a predictive power. These studies demonstrate that the relationships between CAC and outcomes are similar in men and women and different ethnic groups. Each of these studies showed that the accuracy to predict coronary artery events is significantly higher with CAC than traditional risk factor-based risk stratification alone. More recently Greenland et al. shed further light on the clinical implications of CAC for ASCVD risk assessment, proposing that CAC could be used to guide decisions about statin therapy when 10-year ASCVD risk is 5–20%.(Greenland et al., 2018)
It is noteworthy that a low-hanging fruit in the adoption of CAC can be found in over 20 million CT scans done annually in the US to screen for lung cancer (Fig. 5).
Fig. 5.
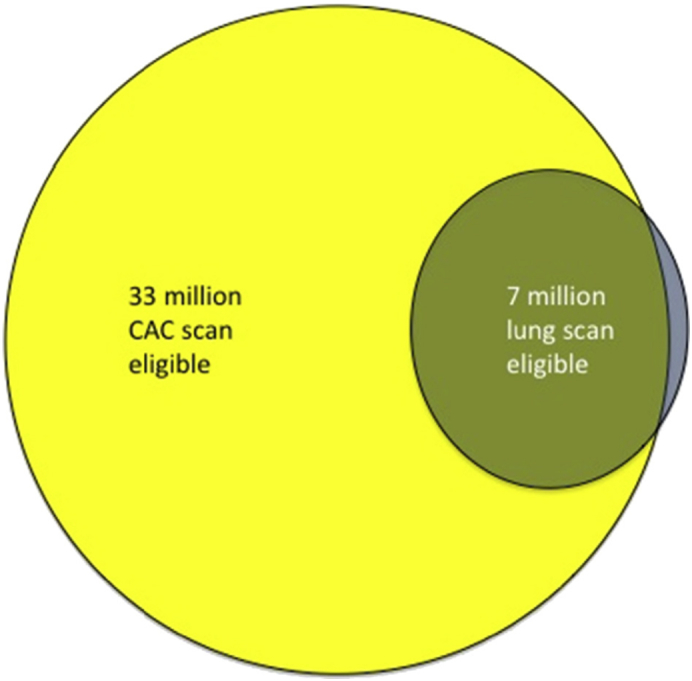
United States Estimates and Overlap of CAC and Lung Scan Eligible Patients
The number of eligible patients in the United States is estimated at 33 million for CAC scanning (yellow) and 7 million for lung scanning in green. Excluding lung scan eligible patients who have established coronary disease (5.3%, unpublished data from the I-ELCAP database) yields an overlap of 6.6 million lung scan patients who would be expected to benefit from CAC scanning. Adapted with permission from: (Hecht HS. Coronary artery calcium scanning: past, present, and future. JACC Cardiovasc Imaging.)
Patients can be informed about the presence of CAC on these scans. Patients with higher levels of calcium in their coronary arteries incidentally detected in these lung scans are more than twice as likely to die.(Hecht et al., 2014) While there needs to be more research done on the subject of using CAC for mass screening to improve ASCVD outcomes, we could improve the status quo if CAC is adopted in a selected population at intermediate risk. Furthermore, a zero CAC score comes with a 5-year “warranty” of very low risk suggesting the patient may not need treatment with a statin. (Min et al., 2010) Even if a patient has high cholesterol, if their CAC score is zero they will be at low risk for ASCVD for the next 5 years. Some even argue that they have a low risk of ASCVD for the next 15 years.(Valenti et al., 2015) These studies convincingly show that a zero CAC score downgrades risk more than any other biomarker.(Blaha et al., 2016; Valenti et al., 2015) In the EISNER trial (Early Identification of Subclinical Atherosclerosis by Noninvasive Imaging Research) investigators studied 2137 patients in primary prevention clinics.(Rozanski et al., 2011) Half underwent general clinical and risk factor evaluations, while the other half underwent the same risk factor evaluations plus a coronary calcium scan. The half that received the scan showed a greater reduction in waist size and Framingham risk score (e.g., lower blood pressure and cholesterol levels). The CAC test is also expected to increase patient adherence to treatment. The phrase “seeing is believing” can apply to CAC. Seeing calcium in their arteries helps patients visualize their risk and motivates them to take action.(Maron, 2017)
5. New guidelines based on CAC testing
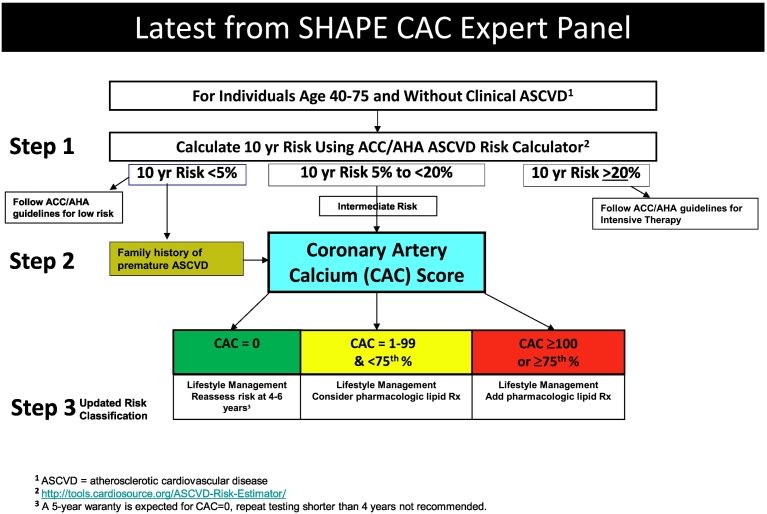
Over the past decade, a number of the coauthors of this paper have volunteered with the non-profit SHAPE (Society for Heart Attack Prevention and Eradication) organization to create a new set of guidelines that utilizes noninvasive imaging of atherosclerosis, more specifically CAC testing.(Naghavi et al., 2006) Our main focus has been on identification of the vulnerable patient.(Naghavi et al., 2006) The journey to find the vulnerable patients began almost two decades ago with the rise of interest in vulnerable plaques thanks to pioneering work by Davies et al. (Davies, 1990), Falk et al. (Falk, 1989), Willerson et al. (Casscells et al., 1996), and Fuster et al. (Fuster et al., 1985) After years of research and discoveries it became obvious that for primary prevention of ASCVD events we must broaden our scope from vulnerable plaques to vulnerable patient.(Naghavi et al., 2003a; Naghavi et al., 2003b)The SHAPE Guidelines were created as the first step on the path toward identifying the vulnerable patient as an increasing mountain of evidence emerged to indicate that asymptomatic individuals with the highest level of CAC score had the highest risk and were most vulnerable to ASCVD events..(Maron, 2017) More recently, we updated the SHAPE flow-chart in light of the ACC/AHA recommendations (Goff Jr. et al., 2013). See Fig. 6.
Fig. 6.
In 2006 the SHAPE Task Force proposed the SHAPE Guideline(Naghavi et al., 2006) which is based on noninvasive detection of atherosclerosis using coronary artery calcium scoring. The higher the burden of atherosclerosis the higher the risk, and the more intensive therapy needed. The “Intermediate Risk” category is the focus of SHAPE Guideline and results in the majority of ASCVD events.
The SHAPE approach has been analyzed by healthcare economy experts and found to be cost-effective if the CAC test is priced below $200.(Shaw & Blankstein, 2010) Although the cost of a CAC test used to be >$400, today it ranges from $100–$200.(Pletcher, 2016) This cost is insignificant compared to the cost of stress electrocardiography, stress echocardiography and nuclear stress tests which are often performed on asymptomatic individuals and cost our healthcare system millions of dollars. Cost-effectiveness analysis by Shaw et al. indicates that the US healthcare system could save $21.5 billion dollars annually if the SHAPE guidelines were adopted.(Shaw et al., 2018) (Table 1).
Table 1.
Cost Effectiveness of SHAPE Guidelines. Cost effectiveness modeling predicts ~ $21.5 billion can be saved annually in the U.S. if SHAPE Guidelines are adopted. (44).
| Estimated impact of SHAPE | Estimated change in cost: USA | |
|---|---|---|
| CVD deaths | ↓ 10% (5%–25%) | ↓ $1.2 B |
| MI (Prevalence) | ↓ 25% (5%–35%) | ↓ $18.0 B |
| Chest pain symptoms (ER Visits) | ↓ 5% (2.5%–25%) | ↓ $4.1 B |
| Hospital discharge for primary diagnosis of CVD | ↑ 10% (5%–25%) | ↑ $3.8 B |
| Hospital discharge for primary diagnosis of CHD | ↓ 10% (5%–25%) | ↓ $9.9 B |
| Cholesterol lowering therapy | ↑ 50% (50%–65%) | ↑ $8 B |
| CV imaging | ↑ 10% (5%–25%) | ↑ $358 M |
| Angiography | ↑ 15%-CTA (2.5%–25%) | ↑ $600 M |
| PCI (Percutaneous coronary interventions per year) | ↓ 10% (5%–50%) | ↓ $580 M |
| CABS (Coronary artery bypass surgeries per year) | ↓ 5% (2.5%–50%) | ↓ $672 M |
| Total Δ in cost | $21.5 B |
6. 2018 ACC/AHA cholesterol guideline adopted CAC
The 2018 update to the American College of Cardiology/American Heart Association guidelines for the management of cholesterol recommend CAC measurement when the decision about starting statin therapy is uncertain from the patient or provider perspective. According to the new guidelines, withholding or deferring statin initiation is reasonable if CAC = 0 and the patient lacks other high-risk features. If CAC score is ≥100, statin therapy should be started, including individuals whose risk estimate falls between 5% and 7.5%.(Grundy et al., 2018) This is a major change compared to previous guidelines and acknowledges the abundant evidence that individuals with CAC ≥100 warrant more intensive preventive therapy and that individuals with zero coronary calcium are very low risk. Lack of coverage for CAC testing deprives patients from personalized preventive care and results in undertreatment when therapy is indicated and unnecessary drug therapy when CAC = 0.
7. Texas Heart Attack Eradication Bill and similar initiatives
In 2010, SHAPE helped Texas Representative Rene Oliveira to pass the HB1290 bill, which requires reimbursement of up to $200 for a CAC test in men ages 45–75, and women ages 55–75 who fall in the intermediate risk category.(HB1290, 2006; Naghavi, n.d.) This initiative brought to light the importance of early detection and treatment of CVD patients without symptoms. Data suggests a possible association between passing HB1290 and decline in incidence of reported heart disease in Texas.(Rankings, 2016) (Fig. 7).
Fig. 7.
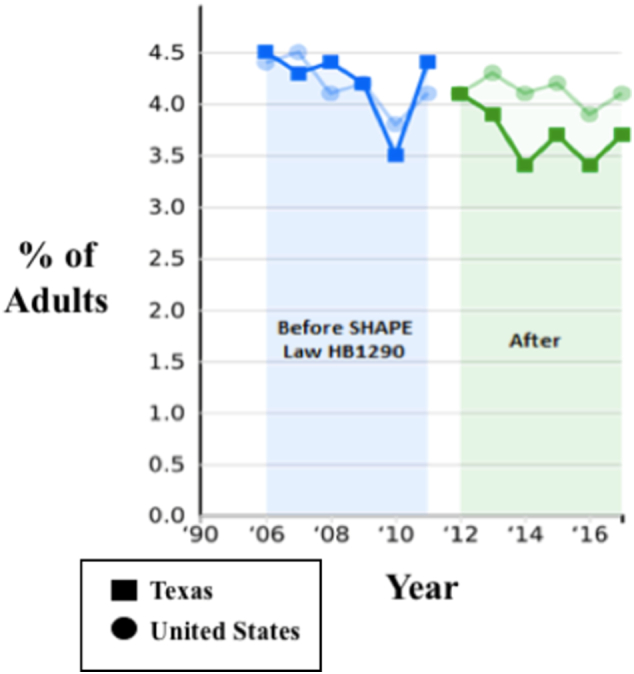
Trend: Heart Disease, Texas vs U.S. This figure shows reported CVD* in Texas vs. U.S. before and after passing Texas SHAPE Law HB1290. It is unclear whether this figure demonstrates a causal relationship or a random association. (48)
*Percentage of adults who reported being told by a health professional that they have angina or coronary heart disease.
Other states are beginning to realize the opportunity to pass similar bills. The Florida state legislature introduced a bill in 2011 offering coverage for cardiovascular screening for males over 45 and females over 55 with low-intermediate risk of CVD. This bill follows SHAPE guidelines. A similar bill is also under consideration in South Carolina, to provide reimbursement for CT scans to specifically test for coronary calcium in males over 45 and females over 55 with low-intermediate risk of CVD.(H. 4839, 2017–2018) Now it is time for other states to take action and make a change for the better.
8. Conclusion
Preventable heart attacks are killing Americans who are not adequately aware of their risk. The current standard of care not only fails to alert high-risk individuals but also results in potentially unnecessary drug therapy for low-risk individuals. A more accurate test, CAC score, is now available; however, insurance companies do not cover it. By covering CAC score, many will be able to find out if they have coronary plaques. If so, they can be prompted to take preventive actions before a heart attack occurs. This initiative has the potential to save lives and money. Texas has already passed HB1290 to mandate CAC coverage. Other states and other countries can take this cause even further. They can set the goal to be the first to eradicate heart attacks. Although eradicating heart attacks requires a multipronged long-term approach, it is now well within our reach; and early detection of high-risk asymptomatic individuals with CAC testing presents as a low-hanging fruit. We must strive for a heart attack-free future for the next generation, the same way that the previous generation gifted us a polio- and smallpox-free life.
References
- Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, et al. Heart disease and stroke statistics-2017 update: a report from the American Heart Association. Circulation. 2017;135(10):e146-e603. Epub 2017/01/27. doi: 10.1161/CIR.0000000000000485. PubMed PMID: 28122885; PubMed Central PMCID: PMCPMC5408160. [DOI] [PMC free article] [PubMed]
- Blaha MJ, Cainzos-Achirica M, Greenland P, McEvoy JW, Blankstein R, Budoff MJ, et al. Role of coronary artery calcium score of zero and other negative risk markers for cardiovascular disease: the Multi-Ethnic Study of Atherosclerosis (MESA). Circulation. 2016;133(9):849–58. Epub 2016/01/24. doi: 10.1161/CIRCULATIONAHA.115.018524. PubMed PMID: 26801055; PubMed Central PMCID: PMCPMC4775391. [DOI] [PMC free article] [PubMed]
- Budoff MJ, Shaw LJ, Liu ST, Weinstein SR, Mosler TP, Tseng PH, et al. Long-term prognosis associated with coronary calcification: observations from a registry of 25,253 patients. J Am Coll Cardiol. 2007;49(18):1860–70. Epub 2007/05/08. doi: 10.1016/j.jacc.2006.10.079. PubMed PMID: 17481445. [DOI] [PubMed]
- Burgstahler C, Cipowicz H, Thomas C, Schabel C, Mangold S, Ketelsen D, et al. Coronary and carotid atherosclerosis in asymptomatic male marathon runners. Scand J Med Sci Sports. 2017. Epub 2017/12/15. doi: 10.1111/sms.13035. PubMed PMID: 29239051. [DOI] [PubMed]
- Casper M, Kramer MR, Quick H, Schieb LJ, Vaughan AS, Greer S. Changes in the geographic patterns of heart disease mortality in the United States: 1973 to 2010. Circulation. 2016;133(12):1171–80. Epub 2016/03/24. doi: 10.1161/CIRCULATIONAHA.115.018663. PubMed PMID: 27002081; PubMed Central PMCID: PMCPMC4836838. [DOI] [PMC free article] [PubMed]
- Casscells W, Hathorn B, David M, Krabach T, Vaughn WK, McAllister HA, et al. Thermal detection of cellular infiltrates in living atherosclerotic plaques: possible implications for plaque rupture and thrombosis. Lancet. 1996;347(9013):1447–51. Epub 1996/05/25. PubMed PMID: 8676628. [DOI] [PubMed]
- Davies MJ. A macro and micro view of coronary vascular insult in ischemic heart disease. Circulation. 1990;82(3 Suppl):II38–46. Epub 1990/09/01. PubMed PMID: (2203563). [PubMed]
- Dawber TR, Kannel WB, Revotskie N, Stokes J, 3rd, Kagan A, Gordon T. Some factors associated with the development of coronary heart disease: six years' follow-up experience in the Framingham study. Am J Public Health Nations Health. 1959;49:1349–56. Epub 1959/10/01. PubMed PMID: 13814552; PubMed Central PMCID: PMCPMC1372949. [DOI] [PMC free article] [PubMed]
- Falk E. Morphologic features of unstable atherothrombotic plaques underlying acute coronary syndromes. Am. J. Cardiol. 1989;63(10):114E-20E. Epub 1989/03/07. PubMed PMID: (2646888). [DOI] [PubMed]
- Fuster V, Steele PM, Chesebro JH. Role of platelets and thrombosis in coronary atherosclerotic disease and sudden death. J. Am. Coll. Cardiol. 1985;5(6 Suppl):175B-84B. Epub 1985/06/01. PubMed PMID: (3889109). [DOI] [PubMed]
- Goff DC, Jr., Lloyd-Jones DM, Bennett G, Coady S, D'Agostino RB, Gibbons R, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25 Suppl 2):S49–73. Epub 2013/11/14. doi: 10.1161/01.cir.0000437741.48606.98. PubMed PMID: 24222018. [DOI] [PubMed]
- Greenland P, Bonow RO, Brundage BH, Budoff MJ, Eisenberg MJ, Grundy SM, et al. ACCF/AHA 2007 clinical expert consensus document on coronary artery calcium scoring by computed tomography in global cardiovascular risk assessment and in evaluation of patients with chest pain: a report of the American College of Cardiology Foundation Clinical Expert Consensus Task Force (ACCF/AHA Writing Committee to Update the 2000 Expert Consensus Document on Electron Beam Computed Tomography) developed in collaboration with the Society of Atherosclerosis Imaging and Prevention and the Society of Cardiovascular Computed Tomography. J Am Coll Cardiol. 2007;49(3):378–402. Epub 2007/01/24. doi: 10.1016/j.jacc.2006.10.001. PubMed PMID: 17239724. [DOI] [PubMed]
- Greenland P, Blaha MJ, Budoff MJ, Erbel R, Watson KE. Coronary calcium score and cardiovascular risk. J. Am. Coll. Cardiol. 2018;72(4):434–47. Epub 2018/07/22. doi: 10.1016/j.jacc.2018.05.027. PubMed PMID: (30025580). [DOI] [PMC free article] [PubMed]
- Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, Braun LT, de Ferranti S, Faiella-Tommasino J, Forman DE, Goldberg R, Heidenreich PA, Hlatky MA, Jones DW, Lloyd-Jones D, Lopez-Pajares N, Ndumele CE, Orringer CE, Peralta CA, Saseen JJ, Smith SC Jr, Sperling L, Virani SS, Yeboah J. J Am Coll Cardiol. 2018 Nov 8.
- H. 4839, (2017–2018).
- HB1290, (2006)
- Hecht HS, Henschke C, Yankelevitz D, Fuster V, Narula J. Combined detection of coronary artery disease and lung cancer. Eur. Heart J. 2014;35(40):2792–6. Epub 2014/08/13. doi: 10.1093/eurheartj/ehu296. PubMed PMID: (25112665). [DOI] [PubMed]
- Heidenreich PA, Trogdon JG, Khavjou OA, Butler J, Dracup K, Ezekowitz MD, et al. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation. 2011;123(8):933–44. Epub 2011/01/26. doi: 10.1161/CIR.0b013e31820a55f5. PubMed PMID: 21262990. [DOI] [PubMed]
- Maron DJ. Preventive interventions after coronary artery calcium scanning: seeing is believing. JACC Cardiovasc. Imaging 2017;10(8):843–4. Epub 2017/08/12. doi: 10.1016/j.jcmg.2017.02.025. PubMed PMID: (28797403). [DOI] [PubMed]
- Min JK, Lin FY, Gidseg DS, Weinsaft JW, Berman DS, Shaw LJ, et al. Determinants of coronary calcium conversion among patients with a normal coronary calcium scan: what is the "warranty period" for remaining normal? J Am Coll Cardiol. 2010;55(11):1110–7. Epub 2010/03/13. doi: 10.1016/j.jacc.2009.08.088. PubMed PMID: 20223365. [DOI] [PubMed]
- Naghavi M. Asymptomatic atherosclerosis: pathophysiology, detection, and treatment. New York: Humana Press; 2010. xxii, 737 p. p.
- Naghavi M. The First Heart Attack Preventive Screening Bill Becomes Law in Texas www.shapesociety.org2015. Available from: http://shapesociety.org/the-first-heart-attack-preventive-screening-bill-becomes-law-in-texas/.
- Naghavi M, Libby P, Falk E, Casscells SW, Litovsky S, Rumberger J, et al. From vulnerable plaque to vulnerable patient: a call for new definitions and risk assessment strategies: Part I. Circulation. 2003a;108(14):1664–72. Epub 2003/10/08. doi: 10.1161/01.CIR.0000087480.94275.97. PubMed PMID: 14530185. [DOI] [PubMed]
- Naghavi M, Libby P, Falk E, Casscells SW, Litovsky S, Rumberger J, et al. From vulnerable plaque to vulnerable patient: a call for new definitions and risk assessment strategies: Part II. Circulation. 2003b;108(15):1772–8. Epub 2003/10/15. doi: 10.1161/01.CIR.0000087481.55887.C9. PubMed PMID: 14557340. [DOI] [PubMed]
- Naghavi M, Falk E, Hecht HS, Jamieson MJ, Kaul S, Berman D, et al. From vulnerable plaque to vulnerable patient--Part III: Executive summary of the Screening for Heart Attack Prevention and Education (SHAPE) Task Force report. Am J Cardiol. 2006;98(2A):2H-15H. Epub 2006/07/18. doi: 10.1016/j.amjcard.2006.03.002. PubMed PMID: 16843744. [DOI] [PubMed]
- Pletcher M. When is measuring a coronary artery calcium score cost effective? Am. Coll. Cardiol. June 14, 2016 https://www.acc.org/latest-in-cardiology/articles/2016/06/14/09/17/when-is-measuring-a-coronary-artery-calcium-score-cost-effective. [Google Scholar]
- Rankings AsH. Texas; United States: 2016. Trend: Heart Disease.https://www.americashealthrankings.org/explore/2016-annual-report/measure/CHD/state/TX Available from: [Google Scholar]
- Rozanski A, Gransar H, Shaw LJ, Kim J, Miranda-Peats L, Wong ND, et al. Impact of coronary artery calcium scanning on coronary risk factors and downstream testing the EISNER (Early Identification of Subclinical Atherosclerosis by Noninvasive Imaging Research) prospective randomized trial. J Am Coll Cardiol. 2011;57(15):1622–32. Epub 2011/03/29. doi: 10.1016/j.jacc.2011.01.019. PubMed PMID: 21439754; PubMed Central PMCID: PMCPMC3104928. [DOI] [PMC free article] [PubMed]
- Sachdeva A, Cannon CP, Deedwania PC, Labresh KA, Smith SC, Jr., Dai D, et al. Lipid levels in patients hospitalized with coronary artery disease: an analysis of 136,905 hospitalizations in Get With The Guidelines. Am Heart J. 2009;157(1):111–7 e2. Epub 2008/12/17. doi: 10.1016/j.ahj.2008.08.010. PubMed PMID: 19081406. [DOI] [PubMed]
- Sarwar A, Shaw LJ, Shapiro MD, Blankstein R, Hoffmann U, Cury RC, et al. Diagnostic and prognostic value of absence of coronary artery calcification. JACC Cardiovasc Imaging. 2009;2(6):675–88. Epub 2009/06/13. doi: 10.1016/j.jcmg.2008.12.031. PubMed PMID: 19520336. [DOI] [PubMed]
- Schurgers LJ, Akbulut AC, Kaczor DM, Halder M, Koenen RR, Kramann R. Initiation and Propagation of Vascular Calcification Is Regulated by a Concert of Platelet- and Smooth Muscle Cell-Derived Extracellular Vesicles. Front Cardiovasc Med. 2018;5:36. Epub 2018/04/24. doi: 10.3389/fcvm.2018.00036. PubMed PMID: 29682509; PubMed Central PMCID: PMCPMC5897433. [DOI] [PMC free article] [PubMed]
- Shaw L.J., Blankstein R. Humana Press; New York: 2010. Asymptomatic Atherosclerosis: Pathophysiology, Detection, and Treatment. (737 p) [Google Scholar]
- Shaw LJ, Goyal A, Mehta C, Xie J, Phillips L, Kelkar A, et al. 10-year resource utilization and costs for cardiovascular care. J Am Coll Cardiol. 2018;71(10):1078–89. Epub 2018/03/10. doi: 10.1016/j.jacc.2017.12.064. PubMed PMID: 29519347; PubMed Central PMCID: PMCPMC5846485. [DOI] [PMC free article] [PubMed]
- Valenti V, B OH, Heo R, Cho I, Schulman-Marcus J, Gransar H, et al. A 15-year warranty period for asymptomatic individuals without coronary artery calcium: a prospective follow-up of 9,715 individuals. JACC Cardiovasc Imaging. 2015;8(8):900–9. Epub 2015/07/21. doi: 10.1016/j.jcmg.2015.01.025. PubMed PMID: 26189116; PubMed Central PMCID: PMCPMC4537357. [DOI] [PMC free article] [PubMed]
- Writing Group M, Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, et al. Heart disease and stroke statistics-2016 update: a report from the American Heart Association. Circulation. 2016;133(4):e38–360. Epub 2015/12/18. doi: 10.1161/CIR.0000000000000350. PubMed PMID: 26673558. [DOI] [PubMed]
- Yeboah J, McClelland RL, Polonsky TS, Burke GL, Sibley CT, O'Leary D, et al. Comparison of novel risk markers for improvement in cardiovascular risk assessment in intermediate-risk individuals. JAMA. 2012;308(8):788–95. Epub 2012/08/23. doi: 10.1001/jama.2012.9624. PubMed PMID: 22910756; PubMed Central PMCID: PMCPMC4141475. [DOI] [PMC free article] [PubMed]