Abstract
Background
Behavioral interventions based on Social Cognitive Theory (SCT) are efficacious for increasing both objectively-measured and self-reported physical activity in people with multiple sclerosis (MS).
Purpose
This study involved a secondary analysis of data focused on SCT constructs as correlates of individual-level changes (i.e., response heterogeneity) following a behavioral intervention.
Method
Twenty-two persons with MS who completed a 6-month SCT-based behavioral intervention for increasing physical activity were included in analyses. The intervention consisted of two primary components, namely a dedicated Internet website and one-on-one video chats with a behavioral coach. Outcomes included objectively-measured moderate-vigorous physical activity (MVPA) using Actigraph model GT3X+ accelerometers and self-reported physical activity using the Godin Leisure-Time Exercise Questionnaire (GLTEQ) as well as SCT variables of exercise self-efficacy, barriers self-efficacy, outcome expectations, goal setting and planning and facilitators/impediments.
Results
There was individual variability in physical activity change following the intervention. For example, 4/22 participants demonstrated a reduction in MVPA, 1/22 participants had no change, 9/22 participants had less than 0.5 standard deviation (SD) increase in MVPA, and 8/22 participants had an increase in MVPA of more than 0.5 SD. Baseline SCT variables, particularly outcome expectations, goal setting, planning, and barriers self-efficacy, correlated with increased physical activity.
Conclusions
This study indicates that SCT variables correlate with the response heterogeneity associated with physical activity behavioral interventions, and this might inform the delivery of interventions consistent with Bandura's stepwise implementation model for optimizing the “fit” of an intervention based on SCT for maximizing treatment efficacy in MS.
Keywords: Behavior, Health, Multiple sclerosis, Exercise
Abbreviations: MS, Multiple Sclerosis; SCT, Social Cognitive Theory; RCT, Randomized Controlled Trial; MVPA, Moderate-Vigorous Physical Activity; BIPAMS, Behavioral Intervention for Physical Activity in Multiple Sclerosis
1. Introduction
There is consistent evidence that physical activity levels are lower among persons with multiple sclerosis (MS) than the general population of adults in the United States [1]. Such an observation is concerning given (a) the exceedingly low rate of physical activity in the general population of adults [2], (b) evidence that physical activity levels decline over time in MS [3], and (c) observation that physical activity benefits might be greater in MS than the general population [4]. To address the problem of physical inactivity in MS, researchers have proposed focusing on behavioral interventions that target lifestyle physical activity (i.e., accumulation of physical activity through planned or unplanned leisure, occupation, or household activities as part of everyday life) rather than exercise training [5]. Such behavioral interventions focus on teaching people the skills, techniques, and strategies for changing physical activity, typically based on a health behavior theory. Researchers have developed, and repeatedly tested and refined, behavioral interventions based on Social Cognitive Theory (SCT) [6] and delivered such interventions through an Internet website for changing physical activity in MS [[7], [8], [9], [10]]. The most recent study involved a phase-II, randomized controlled trial (RCT) that examined the efficacy of a newly developed Internet website that delivered a SCT-based behavioral intervention using e-learning approaches for increasing physical activity over a 6-month period in a sample of 47 persons with MS [11]. The analysis of data from that study identified behavioral intervention effects on self-reported and objectively-measured moderate-to-vigorous physical activity (MVPA), but did not focus on heterogeneity of changes in physical activity nor the possibility that SCT variables might correlate with individual variability in physical activity changes over time. Such an examination is necessary for identifying the characteristics of participants who benefit the most from this behavioral intervention (i.e., precision or targeted medicine) and relevant considering Bandura's notion that the efficacy of interventions based on SCT might depend on initial differences in SCT variables consistent with a stepwise implementation process [6].
The present study involved an exploratory analysis of data [11] and examined (a) the presence of heterogeneity in changes for both objective and self-report measures of physical activity and (b) SCT variables as correlates of heterogeneity in physical activity behavior change among the persons with MS who completed the behavioral intervention condition of the RCT. We expected heterogeneity in physical activity behavior change [9] and that baseline levels of self-efficacy, goal setting, planning, outcome expectations, and facilitators/impediments would correlate with changes in physical activity behavior.
2. Materials and methods
2.1. Participants
This paper involves a secondary analysis of data and the full details on participant recruitment were reported previously [11]. The inclusion criteria were: (a) 18–64 years of age, (b) diagnosis of MS, (c) relapse free for the past 30 days, (d) Internet access, (e) willingness to complete study procedures (i.e. complete questionnaires, wear accelerometer, and undergo randomization), (f) non-active during the previous six months, and (g) ability to ambulate with or without assistance. There were 47 persons who were enrolled in the study and randomized into conditions, and this study includes the 22 participants who completed the behavioral intervention condition.
2.2. Outcomes
Physical activity. The primary study outcome was objective physical activity measured using Actigraph model GT3X+ accelerometers (Actigraph Corporation, FL). The accelerometer was placed in a pouch on an elastic belt and worn around the waist over the non-dominant hip during the waking hours of a seven-day period. Data from the accelerometers were downloaded at 60 s epochs, processed using the low frequency extension and scored for wear time and minutes/day of MVPA based on activity count cut-points for MS [12]. Days with 600 or more minutes of wear time were considered valid and included in the analyses of average min/day of MVPA over a seven-day period.
We further measured physical activity using the Godin Leisure-Time Exercise Questionnaire (GLTEQ) [13]. The GLTEQ includes three items that measure the frequency of engagement in 15 or more minutes of mild, moderate, or strenuous physical activity in the previous week. The GLTEQ total score was computed by multiplying frequency of strenuous, moderate, and light activity by nine, five, and three metabolic equivalents, respectively, and then summing weighted scores. The GLTEQ health contribution score (HCS) was computed by multiplying frequency of strenuous and moderate activity by nine and five metabolic equivalents, respectively, and then summing weighted scores [14].
SCT Variables. The SCT predictor variables included outcome expectations, goal setting/planning, self-efficacy, and facilitators/impediments. Outcome expectations about the benefits of regular exercise and physical activity were measured using the 19-item Multidimensional Outcome Expectations for Exercise Scale (MOEES) [15]. Goal setting for exercise and physical activity was measured using the 10-item Exercise Goal setting Scale (EGS) [16]. Exercise planning was measured using the 10-item Exercise Plans Scale [16]. Self-efficacy was measured using the six-item Exercise Self-Efficacy (EXSE) scale [17] and the 13-item Barriers for Self-Efficacy (BARSE) scale [18]. Functional limitations as impediments for physical activity were assessed using the 15-item Functional Limitations component of the abbreviated Late-Life Function and Disability Instrument (LL-FDI) [19].
Demographics/clinical characteristics. Participants self-reported sex and current age as well as disease duration and clinical course. Neurological disability was measured using both the clinician-administered Expanded Disability Status Scale (EDSS) [20] and Patient Determined Disease Steps (PDDS) scale [21].
2.3. Intervention
As described previously [11], the Behavioral Intervention for Physical Activity in Multiple Sclerosis (BIPAMS) was developed based on a series of pilot RCTs [[7], [8], [9], [10]] and consisted of two primary components, namely a dedicated Internet website and one-on-one video chats with a behavioral coach. The Internet website primarily included interactive video courses developed using Articulate Storyline 360 that provided engaging and immersive experiences for learning about the skills, resources, and strategies of behavioral change based on SCT. The one-on-one video chats were based on principles of supportive accountability, and targeted intervention compliance (i.e., visiting and using the Internet website) and discussion of behavior change principles and practices based on SCT.
2.4. Procedures
All study procedures were approved by a university institutional review board. Interested participants contacted the research team and were screened for eligibility criteria. The screening process involved inclusion criteria and completion of the Physical Activity Readiness Questionnaire [22], medical clearance from a physician, and signed informed consent. Once medical clearance and consent were received, participants completed a baseline testing session including questionnaires and assessment of disability status. Participants further received instructions on wearing the accelerometer and following receipt of accelerometer the project coordinator randomized participants into the intervention or control conditions and provided instructions regarding the assignment via mail and email. Participants completed the same assessments after the 6-month intervention.
2.5. Data analysis
All analyses were performed using SPSS Statistics 24 (IBM, Inc., Armonk, NY). Baseline descriptive characteristics are reported as mean ± standard deviation, unless otherwise noted (e.g., median). We examined group-level change in physical activity outcomes using "non-parametric" pair-samples t-tests "(i.e., Wilcoxon test). We then examined individual-level absolute changes in physical activity (follow-up minus baseline such that positive score indicates an increase and negative score indicates a decrease) using bar graphs and boxplots. We further expressed the pattern of individual-level change based on “categories” of change wherein participants were grouped based on decline (i.e., negative change), no change, small increase (i.e., less than 0.5 SD), or large increase (i.e., more than 0.5 SD) in physical activity; the SD was based on mean SD of change score for each measure. We lastly performed Spearman rank-order correlations (ρ) for examining whether baseline SCT constructs (i.e., outcome expectations, goal setting, exercise planning, self-efficacy, barriers to self-efficacy, and functional limitations mobility) were associated with absolute changes in physical activity outcomes.
3. Results
3.1. Participants
The sample was middle-aged (52.2 ± 10.5 years old), primarily female (n = 20), with moderate MS-related mobility disability based on a median (IQR) PDDS score of 1.5 ± 4.0 and EDSS score of 3.5 ± 2.0. The majority of participants had relapsing remitting course of disease (n = 19) with a disease duration of 13.9 ± 10.3 years.
3.2. Physical activity change: group and individual level analyses
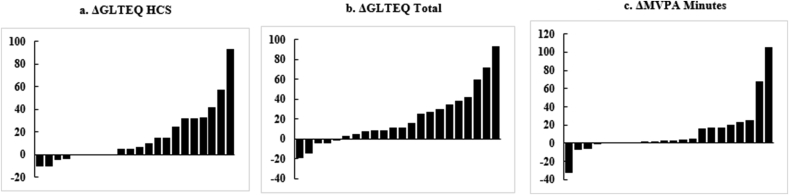
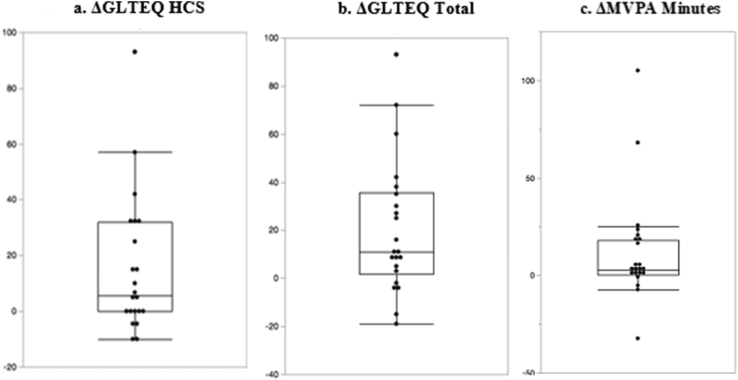
The individual-level absolute change in physical activity outcomes (i.e. GLTEQ total, GLTEQ HCS, MVPA min/day) is illustrated as bar graphs in Fig. 1 and boxplots with whiskers in Fig. 2.
Fig. 1.
Bar graphs of individual-level change in measures of physical activity.
Fig. 2.
Box and whisker plots of individual-level change in measures of physical activity.
GLTEQ HCS (Fig. 1, Fig. 2a). The mean change in the GLTEQ HCS was 15.5 ± 24.9 arbitrary units and this was statistically significant (Z = 2.77, p < .006). There was response heterogeneity such that 4/22 participants demonstrated a decrease in physical activity, 5/22 participants had no change in physical activity, 4/22 participants had less than a 0.5 SD increase in physical activity, and 9/22 participants had more than a 0.5 SD increase in physical activity.
GLTEQ Total (Fig. 1, Fig. 2b). The mean change in GLTEQ Total was 20.4 ± 27.9 arbitrary units and statistically significant (Z = 3.07, p < .002). There was evidence of response heterogeneity whereby 5/22 participants demonstrated a decrease in physical activity, 3/22 participants had less than a 0.5 SD increase in physical activity, and 14/22 participants had more than 0.5 SD increase in physical activity.
Minutes MVPA (Fig. 1, Fig. 2c). The effect of the intervention on objectively measured MVPA was 12.2 ± 27.7 min/day and statistically significant (Z = 2.52, p = .012). Regarding individual-level change, 4/22 participants demonstrated a decline in min/day of MVPA, 1/22 participant had no change, 9/22 participants had less than 0.5 SD increase in min/day of MVPA, and 8/22 participants had more than 0.5 SD increase in min/day of MVPA.
3.3. SCT correlates of response heterogeneity
Baseline SCT variables were examined as correlates of change in physical activity within the behavioral intervention condition (Table 1). MOEES (overall outcome expectations) correlated with change in GLTEQ HCS (ρ = 0.46, p < .05) and GLTEQ total (ρ = 0.47, p < .05). EGS (goal setting) correlated with change in GLTEQ HCS (ρ = 0.51, p < .05) and GLTEQ total (ρ = 0.49, p < .05). BARSE (barriers self-efficacy) correlated with change in GLTEQ HPS (ρ = 0.46, p < .05) and GLTEQ total (ρ = 0.43, p < .05). EPS (exercise planning) correlated with change in objectively measured MVPA (ρ = 0.46, p < .05). Of note, baseline EDSS or PDDS scores did not correlate with changes in the physical activity outcomes (all ρ < 0.27, and p > .23), and these data are not reported in Table 1.
Table 1.
Bivariate correlations among baseline social cognitive theory variables and changes in physical activity.
| ΔGLTEQ HCS | ΔGLTEQ Total | ΔMVPA Minutes/day | |
|---|---|---|---|
| MOEES | .46* | .47* | .37 |
| EGS | .51* | .49* | .28 |
| EPS | .31 | .30 | .46* |
| EXES | -.02 | -.05 | .27 |
| BARSE | .46* | .43* | .32 |
| LLFDI | -.12 | -.01 | .29 |
*p < .05.
4. Discussion
The BIPAMS intervention resulted in statistically significant group-level change in physical activity, but there was further evidence of individual-level variability regarding change in both self-reported and objectively-measured physical activity following the six-month intervention. The majority of participants had increases in physical activity, yet 22% of participants reduced or did not change physical activity levels with the behavioral intervention. Outcome expectations, goal setting, planning, and self-efficacy at baseline were positively associated with changes in physical activity. This is the first known examination of SCT variables as correlates of treatment response heterogeneity with a behavioral intervention for increasing physical activity in persons with MS, and our results may have practical and theoretical implications for the future design and delivery of such approaches for changing physical activity in this population.
The current study focused, in part, on documenting the possibility of response heterogeneity regarding physical activity change with the 6-month BIPAMS behavioral intervention. We observed an overall increase in physical activity and positive changes in physical activity for the majority of participants who completed the behavioral intervention, yet some participants had a decline or no change in physical activity. This is consistent with previous research using an Internet-delivered, SCT-based behavioral intervention for increasing physical activity in MS [11,23]. For example, the first pilot study of the Internet-delivered behavioral intervention reported statistically significant improvements in physical activity, but graphically illustrated a pattern of heterogeneous changes within the intervention condition [9]. We later did a Phase-I RCT and reported improvements in objective and self-reported physical activity as well as positive effects on fatigue, disability status, and walking impairment [10]. Collectively, our results combined with previous research indicate that the behavioral intervention based on SCT is efficacious for increasing physical activity behavior in MS on the group-level, but there is heterogeneity such that a portion of participants demonstrate improvements in physical activity, whereas others do not change or even decrease physical activity thereby indicating an individual-level pattern of change. This is an important observation, as most research only reports on group-level changes in physical activity and other outcomes with such behavioral interventions, and we report and further confirm the presence of individual-level change as a sign-post for future trials in MS and beyond.
The BIPAMS intervention centered on SCT as the backbone of both website content and one-on-one coaching strategies, and therefore SCT variables represent obvious choices for examination as correlates of response heterogeneity in physical activity. We observed that those with higher baseline levels of outcome expectations, self-efficacy, planning and goal setting had the largest changes in physical activity after the 6-month behavioral intervention. This is consistent with Bandura's theory of health promotion by social cognitive means that posits knowledge, perceived self-efficacy, outcome expectations, perceived facilitators and impediments as core determinants of health behavior change, including physical activity [6]. This is further consistent with notion of a stepwise implementation approach wherein individuals with higher levels of SCT constructs (self-efficacy, goal setting, planning, and outcome expectations) might have the easiest path toward behavior change, and only need a distance-based, Internet platform focusing on behavior change techniques that align with SCT-principles for successfully increasing physical activity. By comparison, those with lower levels of SCT constructs may require a different approach for initiating behavioral change such as face-to-face interaction or group-based social contact as a more intense intervention for behavioral change.
We are aware of one previous study that identified disability status as a primary correlate of physical activity behavior change with an earlier version of the Internet-delivered behavioral intervention [23]. The current study did not replicate such results, as neither EDSS nor PDDS scores were correlated with change in physical activity. Perhaps SCT variables are more potent correlates of behavioral intervention changes, as this program was designed based on that theory, or SCT variables might be highly associated with disability status and explain why persons with higher levels of disability would have less change in physical activity, as reported in previous research [23]. Nevertheless, the samples were relatively small in the current and previous research, and the studies were not designed for identifying sources of response heterogeneity per se. We believe that future studies, such as the ongoing Phase-III trial of BIPAMS, will clearly identify and articulate the possible range of variables that explain response heterogeneity with SCT-based, internet-delivered behavioral interventions for MS [24].
This study includes two primary limitations. This study involved an exploratory analysis of data from a relatively small Phase-II RCT in ambulatory persons with MS and the trial was not designed for examining sources of response heterogeneity in physical activity per se. This further prevented a multivariate analysis such as linear regression for examining the independent contribution of the SCT variables as correlates of change in physical activity. The current study primarily focused on a relatively narrow set of SCT variables, and there are a range of other variables that might operate independently and interactively with SCT variables for explaining response heterogeneity in physical activity with the BIPAMS behavioral intervention.
5. Conclusions
Overall, the BIPAMS intervention was efficacious for improving both objectively-measured and self-reported physical activity in persons with MS, yet there was variability in the pattern of change that correlated with baseline SCT variables. Such a pattern of results reaffirms our notions of variability in the efficacy of behavioral interventions and the importance of explaining this variability for optimizing the precision of interventions in MS and likely other populations with neurological diseases that result in physical disability. The continuation of research on response heterogeneity will represent another major step forward in our understanding of the optimal, tailored approaches for changing physical activity in MS, and possibly open a new agenda for changing other health behavior in this population.
Funding
This study was supported by the National Multiple Sclerosis Society [RG 5144A6/1 & MB 0029].
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.conctc.2019.100366.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Kinnett-Hopkins D., Adamson B., Rougeau K., Motl R. People with MS are less physically active than healthy controls but as active as those with other chronic diseases: an updated meta-analysis. Mult. Scler Relat. Disord. 2017;13:38–43. doi: 10.1016/j.msard.2017.01.016. [DOI] [PubMed] [Google Scholar]
- 2.Ham S., Yore M., Fulton J., Kohl H.W., III Prevalence of no leisure-time physical activity-35 states and the District of Columbia, 1988-2002. MMWR Morb. Mortal. Wkly. Rep. 2004;53(4):82–86. [PubMed] [Google Scholar]
- 3.Motl R.W., McAuley E., Sandroff B.M. Longitudinal change in physical activity and its correlates in relapsing-remitting multiple sclerosis. Phys. Ther. 2013;93(8):1037–1048. doi: 10.2522/ptj.20120479. [DOI] [PubMed] [Google Scholar]
- 4.Motl R.W., Sandroff B.M. Benefits of exercise training in multiple sclerosis. Curr. Neurol. Neurosci. Rep. 2015;15(9):62. doi: 10.1007/s11910-015-0585-6. [DOI] [PubMed] [Google Scholar]
- 5.Ellis T., Motl R.W. Physical activity behavior change in persons with neurologic disorders: overview and examples from Parkinson disease and multiple sclerosis. J. Neurol. Phys. Ther. 2013;37(2):85–90. doi: 10.1097/NPT.0b013e31829157c0. [DOI] [PubMed] [Google Scholar]
- 6.Bandura A. Health promotion by social cognitive means. Health Educ. Behav. 2004;31(2):143–164. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- 7.Dlugonski D., Motl R.W., McAuley E. Increasing physical activity in multiple sclerosis: replicating Internet intervention effects using objective and self-report outcomes. J. Rehabil. Res. Dev. 2011;48(9):1129–1136. doi: 10.1682/jrrd.2010.09.0192. [DOI] [PubMed] [Google Scholar]
- 8.Dlugonski D., Motl R.W., Mohr D.C., Sandroff B.M. Internet-delivered behavioral intervention to increase physical activity in persons with multiple sclerosis: sustainability and secondary outcomes. Psychol. Health Med. 2012;17(6):636–651. doi: 10.1080/13548506.2011.652640. [DOI] [PubMed] [Google Scholar]
- 9.Motl R.W., Dlugonski D., Wojcicki T.R., McAuley E., Mohr D.C. Internet intervention for increasing physical activity in persons with multiple sclerosis. Mult. Scler. 2011;17(1):116–128. doi: 10.1177/1352458510383148. [DOI] [PubMed] [Google Scholar]
- 10.Pilutti L.A., Dlugonski D., Sandroff B.M., Klaren R., Motl R.W. Randomized controlled trial of a behavioral intervention targeting symptoms and physical activity in multiple sclerosis. Mult. Scler. 2014;20(5):594–601. doi: 10.1177/1352458513503391. [DOI] [PubMed] [Google Scholar]
- 11.Motl R.W., Hubbard E.A., Bollaert R.E. Randomized controlled trial of an e-learning designed behavioral intervention for increasing physical activity behavior in multiple sclerosis. Mult. Scler J. Exp. Transl. Clin. 2017;3(4) doi: 10.1177/2055217317734886. 2055217317734886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sandroff B.M., Motl R.W., Suh Y. Accelerometer output and its association with energy expenditure in persons with multiple sclerosis. J. Rehabil. Res. Dev. 2012;49(3):467–475. doi: 10.1682/jrrd.2011.03.0063. [DOI] [PubMed] [Google Scholar]
- 13.Godin G., Shephard R. A simple method to assess exercise behavior in the community. Can. J. Appl. Sport Sci. 1985;10(3):141–146. [PubMed] [Google Scholar]
- 14.Motl R.W., Bollaert R.E., Sandroff B.M. Validation of the Godin Leisure-Time Exercise Questionnaire classification coding system using accelerometry in multiple sclerosis. Rehabil. Psychol. 2018;63(1):77–82. doi: 10.1037/rep0000162. [DOI] [PubMed] [Google Scholar]
- 15.McAuley E., Motl R.W., White S.M., Wójcicki T.R. Validation of the multidimensional outcome expectations for exercise scale in ambulatory, symptom-free persons with multiple sclerosis. Arch. Phys. Med. Rehabil. 2010;91(1):100–105. doi: 10.1016/j.apmr.2009.09.011. [DOI] [PubMed] [Google Scholar]
- 16.Rovniak L.S., Anderson E.S., Winett R.A., Stephens R.S. Social cognitive determinants of physical activity in young adults: a prospective structural equation analysis. Ann. Behav. Med. 2002;24(2):149–156. doi: 10.1207/S15324796ABM2402_12. [DOI] [PubMed] [Google Scholar]
- 17.McAuley E. The role of efficacy cognitions in the prediction of exercise behavior in middle-aged adults. J. Behav. Med. 1992;15(1):65–88. doi: 10.1007/BF00848378. [DOI] [PubMed] [Google Scholar]
- 18.McAuley E. Self-efficacy and the maintenance of exercise participation in older adults. J. Behav. Med. 1993;16(1):103–113. doi: 10.1007/BF00844757. [DOI] [PubMed] [Google Scholar]
- 19.McAuley E., Konopack J.F., Motl R.W., Rosengren K., Morris K.S. Measuring disability and function in older women: psychometric properties of the late-life function and disability instrument. J. Gerontol. A Biol. Sci. Med. Sci. 2005;60(7):901–909. doi: 10.1093/gerona/60.7.901. [DOI] [PubMed] [Google Scholar]
- 20.Kurtzke J.F. Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS) Neurology. 1983;33(11):1444–1452. doi: 10.1212/wnl.33.11.1444. [DOI] [PubMed] [Google Scholar]
- 21.Hadjimichael O., Kerns R.D., Rizzo M.A., Cutter G., Vollmer T. Persistent pain and uncomfortable sensations in persons with multiple sclerosis. Pain. 2007;127(1–2):35–41. doi: 10.1016/j.pain.2006.07.015. [DOI] [PubMed] [Google Scholar]
- 22.Thomas S., Reading J., Shephard R.J. Revision of the physical activity readiness questionnaire (PAR-Q) Can. J. Sport Sci. 1992;17(4):338–345. [PubMed] [Google Scholar]
- 23.Motl R.W., Dlugonski D., Pilutti L.A., Klaren R.E. Does the effect of a physical activity behavioral intervention vary by characteristics of people with multiple sclerosis? Int. J. MS Care. 2015;17(2):65–72. doi: 10.7224/1537-2073.2014-016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Motl R.W., Sandroff B.M., Wingo B.C. Phase-III, randomized controlled trial of the behavioral intervention for increasing physical activity in multiple sclerosis: project BIPAMS. Contemp. Clin. Trials. 2018;71:154–161. doi: 10.1016/j.cct.2018.06.017. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.