Abstract
Objective:
We performed an integrated cross-sectional analysis of relationships between long-term care work environments, employee and resident satisfaction, and quality of patient care.
Methods:
Facility-level data came from a network of 203 skilled nursing facilities in 13 states in the eastern United States owned or managed by one company. K-means cluster analysis was applied to investigate clustered associations between safe resident handling program (SRHP) performance, resident care outcomes, employee satisfaction, rates of workers’ compensation claims, and resident satisfaction.
Results:
Facilities in the better-performing cluster were found to have better patient care outcomes and resident satisfaction; lower rates of workers compensation claims; better SRHP performance; higher employee retention; and greater worker job satisfaction and engagement.
Conclusion:
The observed clustered relationships support the utility of integrated performance assessment in long-term care facilities.
Nursing homes function as both work and residential settings. As such, the organizational characteristics of these facilities have the potential to impact experiences for residents and workers and for these experiences to overlap and interact.1 Health care service quality is influenced by work organization factors such as staffing levels and retention rates, among other characteristics.2–6 In addition, health care worker self-reported experiences are associated with differences in objective measures of patient care quality; in a national study of Veterans Administration hospitals, employee perceptions of organizational factors were found to be associated with a number of performance quality measures, including quality of chronic disease management, preventive care, postsurgical mortality, patient satisfaction, and cost per patient.7 The United States National Institute for Occupational Safety and Health (NIOSH) has highlighted the potential links between health care occupational safety and quality of care and has called for further investigations into the relationships between patient and worker safety, work practices, and service quality.8
Among the many occupational hazards in health care work, physically demanding and repetitive tasks are known risk factors for work-related injuries, contributing to high rates of low back injuries and other acute and degenerative work-related musculoskeletal disorders.9–14 Employees of long-term care facilities are at particularly high risk for work-related musculoskeletal disorders; nationally, among all private sector job titles, workers with the position of ‘‘nursing assistant’’ have the highest rates of lost-time injuries and illnesses and the highest rates of musculoskeletal disorders.15 Specific tasks and work features that contribute to increased injury risk include performing frequent manual patient handling, mobility assistance, and care tasks and the potential for physical assaults by residents with impaired cognition. Furthermore, the effects of stress and physical workload on musculoskeletal injury risk may be multiplied by working extended schedules, such as extended shifts or mandatory overtime, which are common in direct patient care work.16 These work factors not only may increase the risk of work-related injury in long-term care occupations but also may have other adverse effects on work satisfaction and general physical and mental health, including burnout, depression, reduced sleep quality and quantity, somatic distress, and intention for turnover.9,12,17–27
Unsurprisingly, given the demands and hazards of long-term care work, low levels of job satisfaction are reported by workers in this industry, and high rates of absenteeism and employee turnover present ongoing challenges for long-term care employers.8 In the United States in 2012, median employee turnover in skilled nursing facilities (SNFs) was 43.9%.28 Using data from the 2004 National Nursing Home Survey, Donoghue previously reported annualized turnover rates as high as 74.5% for certified nursing assistants (CNAs), with rates for registered nurses (RNs) and licensed practical nurses (LPNs) at over 50%.29 Difficulty retaining and/or recruiting long-term care workers can contribute to further organizational challenges, including staff shortages, poor teamwork, poor relationships with supervisors, limited decision-making opportunities, and feeling a lack of respect or appreciation.25,30–33
This study was undertaken as an integrated cross-sectional analysis of the relationships between long-term care work environments, employee and resident satisfaction, workplace safety, and quality of patient care. Facility-level data came from a network of 203 SNFs in 13 states in the eastern United States that were owned or jointly managed by a single company. We obtained facility Centers for Medicare and Medicaid facility ratings, workers’ compensation claims (WCCs) data, human resources records for staffing levels and annual retention rates, employee and resident satisfaction survey responses, and facility-reported annual rates of resident adverse events: pressure ulcers, falls, and unexplained weight loss.
In addition, the company managing these facilities had introduced a mandatory safe resident handling program (SRHP) in all of its owned or managed facilities beginning in 2004.34,35 Introduction of this SRHP was intended to, and succeeded in, reducing worker exposures to lifting hazards and lowering WCCs and costs.34–38
However, even though the SHRP was implemented by a single vendor across all 203 facilities, benefits from these programs were found to vary among facilities.35,38 The observed heterogeneity in program effectiveness was another motivating factor for conducting this integrated, systematic examination of differences between centers across multiple domains of long-term care work and care service delivery. Identifying the underlying factors contributing to the variation among the SNFs could inform facility managers and policy-makers. Using a cluster analysis method to explore relationships underlying the identified heterogeneity, we examined patterns in the study measures for a network of 203 SNFs. This exploratory analysis sought to investigate whether facilities demonstrated clustered associations reflecting relationships between SRHP performance, resident care outcomes, employee work satisfaction, rates of WCCs, and resident satisfaction.
METHODS
Institutional Review Board (IRB) approval was obtained before data collection for this study from the University of Massachusetts Lowell IRB (IRB approval number 12-056). This study included 203 SNFs located in 13 states in the eastern United States that were owned or jointly managed by one skilled nursing and rehabilitation therapy company during the year 2012.
Facility Characteristics
Facilities included in the analysis operated either exclusively as SNFs or as SNFs in combination with Independent and/or Assisted Living Facilities. For each facility, information was recorded for location, number of beds, and whether the facility was owned or jointly managed by the participating company. The proportion of short-term placement beds in each facility, such as beds for postsurgical rehabilitation, was recorded. Union representation of workers at each facility was coded as yes/no (any versus none). Administrators for each facility were asked to report the number of wellness activities underway at their centers during 2012; these responses were coded as “few” (0–4) or “many” (5+) activities.
Centers for Medicare & Medicaid Services (CMS) generate publicly available ratings for facilities serving Medicare and Medicaid beneficiaries. For each facility included in the study, we obtained the CMS Survey Ratings, Quality Ratings, and Staffing Ratings reports for the year 2012. The facility Survey Rating is determined on the basis of health inspection performance, with rankings assigned according to state-specific distributions due to state differences in inspection protocols. The Quality Rating is determined on the basis of facility performance on nine patient care outcome measures. The Staffing Rating is based on the clinical staff hours per resident as reported quarterly to CMS (CMS, 2015). In post-hoc comparisons between cluster groups, the CMS Staffing Ratings and CMS Quality Ratings were found to demonstrate collinearity with the CMS Survey Ratings but offered less certain validity. Therefore, the primary metric selected for quality comparison among facilities was the Survey Rating.
Staff Characteristics
De-identified workforce rosters were used to calculate the number of clinical hours worked in each facility per year, in units of full-time equivalents (FTE), where one FTE was defined as the work performed by one employee working 40 hours per week for 1 year. For each facility, counts of WCCs and the number of employee sick hours reported during the year 2012 were then divided by the number of clinical FTEs worked to obtain rates of worker’s compensation claims per clinical FTE and sick hours taken per clinical FTE.
Clinical staff hours per resident-day were calculated as the sum of clinical FTEs worked by CNAs, certified medical assistants (CMAs), LPNs, and RNs, divided by the number of resident-days of care provided at each facility in 2012. Clinical employee retention rates for the year 2012 were recorded as the percentage of employees remaining at each facility in the following positions compared with the previous year: certified nursing or medical aides (CNAs/CMAs), LPNs, and RNs. Retention of upper level management during the 2012 study period was coded as a binary variable [any/none] to reflect personnel changes in the following positions: Administrator, Director of Nursing (DON), or Assistant DON.
A unique feature of the company facilities included in this study was the existence of a nonprofit foundation that had been created to provide financial assistance to employees in need. As the foundation provides assistance only to current employees, the percentage of workers contributing to this foundation was taken as an indicator of overall employee engagement and intention to continue employment in the facility.
Resident Characteristics
The CMS Minimum Data Set (MDS) is a federally required clinical assessment recorded for each nursing home resident at the time of admission, annually, and at discharge. All nursing home facilities are required to submit MDS reports to CMS annually. Summary CMS MDS reports from each facility through December 2011 (marking the end of MDS version 2.0) were used in this analysis. From these reports, we extracted rates of pressure ulcers; rates of falls; rates of unexplained weight loss; and mean resident Activities of Daily Living (ADL) transfer scores.
The proportion of Medicare and Medicaid patients in each facility were abstracted from facility records for the year 2011. Facility discharge rates were calculated as the number of discharge satisfaction surveys distributed per number of facility beds per year.
Resident and Employee Satisfaction Survey Data
“My InnerView” (MIV) is an annual survey tool created by the National Research Corporation (a private entity) to survey employee and resident experiences during nursing home care.39 Data from two sets of surveys were included in this analysis: (1) job satisfaction survey responses from individual employees and (2) resident experience satisfaction surveys completed by residents themselves and/or by residents’ family members or friends.
Facility-level MIV survey data were provided by the partnering company for this study. To permit comparisons, among facilities, we computed center-wide average values for the employee and resident satisfaction surveys. We also calculated employee and resident response percentages. For residents, we averaged the center-level response percentages from the residents themselves and from family or friends; these two sets of scores were moderately correlated (Spearman r = 0.43, P < 0.0001), thus we used the average response in the further analysis.
Safe Resident Handling Program Performance
Beginning in 2004, the partnering company had initiated a SRHP that was mandatory in all of the company’s owned or managed SNFs. As measures of SRHP effectiveness at the site level, we had previously computed two measures of program effectiveness: (1) facility-level annual rate of return on investment (ROI) of the SRHP over the first 3 years38 and (2) percentage change in total WCC rates for 3 years before SRHP implementation compared with the second 3-year period after SRHP implementation (approximately 2010 to 2013).37
Data Management and Preliminary Analysis
Center characteristics were extracted from the data sets for each center. All data used in this study were collected for the year 2012, except where this information was not available (Table 1). Information from 2011 was used for Employee Satisfaction Survey Ratings, Percent of Employee Satisfaction Surveys returned, Resident Satisfaction Survey Ratings, Percent of Resident Satisfaction Surveys returned, proportion of residents on Medicaid and Medicare, and average resident ADL transfer scores. SRHP ROI was computed for the time interval 2003 to 2012 and relative changes in worker’s compensation claims rates were calculated using data through April 2013. Data sets containing the characteristics of interest were cross-walked and merged using unique center identification numbers to produce a single data set for further analysis.
TABLE 1.
Descriptive Statistics for Included Skilled Nursing Facilities
| Domain | Cluster Variable (Y/N) | Variable [units] | n | Mean (±SD) | Range | Coefficient of Variation |
|---|---|---|---|---|---|---|
| Employees | Y | Sick hours [hours per FTE] | 193 | 39.91 (±8.37) | 3.98–70.29 | 20.97 |
| Y | Employee Foundation [% participation] | 202 | 0.42 (±0.29) | 0.00–1.00 | 68.84 | |
| Y | MIV Employee Satisfaction [Average rating 0–3] (2011) | 195 | 1.86 (±0.18) | 1.38–2.52 | 9.46 | |
| N | MIV Employee Response Rate [% survey returns] (2011) | 195 | 0.85 (±0.14) | 0.36–1.01 | 16.10 | |
| N | Workers Compensation Claims [Claims/FTE] | 182 | 0.13 (±0.07) | 0.01–0.41 | 51.82 | |
| N | RN retention [Proportion/Year] | 198 | 0.64 (±0.16) | 0.20–1.00 | 25.20 | |
| Y | CNA retention [Proportion/Year] | 198 | 0.72 (±0.11) | 0.38–0.95 | 15.87 | |
| N | LPN Retention [Proportion/Year] | 198 | 0.79 (±0.17) | 0.00–1.00 | 21.59 | |
| Y | Staffing ratio [Care staff hours/resident-day] | 197 | 4.34 (±1.25) | 1.42–7.15 | 28.91 | |
| N | Nurse Administrator Turnover [Yes = 1/No = 0] | 203 | 40/203 (19.4%) | |||
| N | Worker Unionization [Any = 1/None = 0] | 196 | 38/196 (19.7%) | |||
| Residents | Y | Rate of pressure ulcers [Annual total incidents/average daily census] | 202 | 0.03 (±0.02) | 0.00–0.13 | 69.35 |
| Y | Rate of falls [Annual total incidents/average daily census] | 202 | 0.19 (±0.07) | 0.05–0.46 | 38.54 | |
| Y | Rate of unexplained weight loss [Annual total incidents/average daily census] | 202 | 0.03 (±0.01) | 0.00–0.09 | 47.49 | |
| N | Percent Medicaid and Medicare [Proportion of residents funded by Medicare or Medicaid] (2011) | 203 | 0.83 (±0.08) | 0.56–0.98 | 9.48 | |
| Y | Resident, Family, or Friend MIV Satisfaction [Average rating 0–3] (2011) | 203 | 2.28 (±0.16) | 1.71–2.62 | 7.19 | |
| N | MIV Resident Response Rate [% survey returns] (2011) | 189 | 0.83 (±0.18) | 0.21–1.04 | 21.13 | |
| N | Resident ADL Transfer Score [Average score 0–4] (2011) | 203 | 2.27 (±0.20) | 1.81–2.83 | 8.66 | |
| N | Discharge rate [Number of discharge surveys sent out/number of beds] (2011) | 203 | 0.36 (±0.18) | 0.07–1.14 | 50.05 | |
| N | Proportion of short-term beds [Number short-term beds/total skilled beds] | 198 | 0.14 (±0.20) | 0.00–1.00 | 144.10 | |
| N | Any short-term units [Yes = 1/No = 0] | 198 | 90/198 (45.5%) | |||
| Centers for Medicare and Medicaid Services (CMS) Ratings | Y | Survey Rating [Scale Range 1–5] | 203 | 2.74 (±1.30) | 1.00–5.00 | 47.59 |
| N | Quality rating [Scale range 1–5] | 203 | 3.80 (±0.96) | 1.00–5.00 | 25.18 | |
| N | Staffing rating [Scale range 1–5] | 202 | 3.07 (±1.00) | 1.00–5.00 | 32.60 | |
| Safe Resident Handling Program (SHRP) Performance | N | SHRP Return on Investment (ROI) [Calculated ROI (Lahiri et al, 2013)] | 119 | 0.58 (±1.15–2.18 to 5.60 | 198.46 | |
| N | Change in Workers’ Compensation Claims Rates [Pre-SRHP rate/3-6 years Post-SRHP rate] (rate ratio through April 2013) | 135 | 0.95 (± 0.95) | 0.23–10.61 | 100.20 | |
Variables used for clustering are highlighted in grey. All data were from 2012 except as noted.
Cluster Analysis Variable Selection
Data management and statistical analyses were conducted in SAS 9.4 (SAS Institute, Cary, NC). Spearman correlation coefficients were computed for all pairs of key ordinal and scale indicators. Of the 23 continuous facility variables, 10 were selected for use in the cluster analysis (Fig. 1; Table 1). As each variable was measured in different units, these were standardized to a mean of zero and standard deviation of one for comparable scaling.40
FIGURE 1.
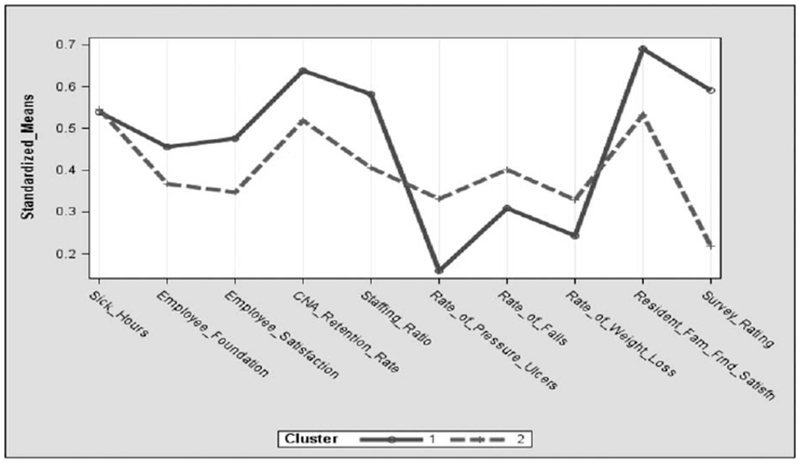
Cluster profiles showing the means of the 10 standardized variables used to fit the two clusters; standardizations are centered on distribution means.
The variables not used to determine the clusters were compared post-hoc between the cluster groups. These included the CMS staffing and quality ratings (due to collinearity with the CMS Survey Ratings but less certain validity) and the MIV residents’ response rates, because overlap between residents and their proxy respondents could not be identified. WCC rates, ROI, and reduction in the WCCs rates were excluded from the cluster analysis due to missing values (21, 84, and 68 missing data points, respectively) (Table 1).
Resident care aides (CNA/CMA) represented the largest single job group in the nursing home workforce in this study and were assumed to provide most of the direct care to residents. The retention rate for this group was the most stably estimated and was found to be moderately well correlated with retention rates for RNs (Spearman correlation coefficient r = 0.44, P < 0.0001) and LPNs (r = 0.41, P < 0.0001). Therefore, CNA/CMA retention rates were used as summary measures of employee retention in the cluster analysis.
Cluster Analysis
Cluster Analysis41 was used to identify homogeneous and unobserved distinct subgroups among the 203 SNFs; to examine heterogeneity among study sites; and to determine whether site characteristics together could be used to partition the centers into relatively homogenous groups. Non-hierarchical clustering (k-means) divides the observations into two or more mutually exclusive subgroups by minimizing the distance among observations within each group and maximizing the distance between groups.
The analytic algorithm used was SAS PROC FASTCLUS that handles observations with missing data points by scaling the distance measure of all variables with no missing data.42 Observations were allocated to the respective cluster membership with nearest centroid.43 A random order was assigned. The k-means approach is a heuristic method that uses a pre-specified value, k, to partition the observations into subgroups. Preliminary analysis was performed with several values for k (k = 2, 3, 4). The most widely used heuristic index for selecting the number of clusters is the pseudo F-statistic, which gives a larger value for better partitions.43,44 The value of in cluster analysis indicates the extent to which the variable contributes to cluster separation.44 PROC CAN-DISC in SAS was employed to generate a canonical scatter plot of the 10 variables used to partition the groups. This procedure excluded those SNFs with one or more missing data point(s).
Post-hoc Subgroup Analysis
After cluster solutions were obtained, the distributions of the remaining variables between the two clusters were examined by comparing mean values for continuous variables and prevalence for dichotomous variables. Dichotomous measures not incorporated in the cluster solution were the following: occurrence of nurse administrator turnover in the prior year, presence or absence of short-term care units, and presence or absence of any union representation. We then stratified data by each of the binary variables to examine whether any of these variables affected the cluster solutions.
RESULTS
Administrative data files from the participating company were used to identify 258 facilities for potential inclusion. Among these, 228 sites offered skilled nursing services, exclusively or in part, and were owned or jointly managed by the participating company. Twenty-three of these facilities were affiliated but not owned by the company, and they had too many missing data points to be included in the analysis. Two other sites were excluded because they had closed before 2012. The study population therefore included 203 SNFs. Of these, WCCs data were not available from centers located in West Virginia (n = 27), which has a state-insured system.
Study facilities were found to vary substantially (high coefficients of variation) across most of the characteristics examined, with the exception of MIV survey responses for overall employee satisfaction and overall resident satisfaction (Table 1). As examples of the ranges of variations, employee sick hours ranged from 3.98 to 70.29 per full time equivalent (FTE); CNA/CMA retention rates ranged from 38% to 95%; and rates of resident falls ranged from 0.05 to 0.46 per resident-day.
In the cluster analysis, a two-cluster solution achieved the largest pseudo F-statistic (F = 32.40), compared with values for three- (F = 28.16) or four- (24.86) cluster solutions. Each cluster solution is characterized by patterns of study measures used to achieve the separation. In the two-cluster solution, Cluster 1 contained 118 (58%) of the SNFs and had more favorable characteristics for all 10 of the variables utilized, compared with Cluster 2, which contained 85 centers (Fig. 1).
The variables that exercised the most influence on the separation between the two clusters (higher values), in descending order, were CMS Survey Rating, resident pressure ulcer rate, average employee and resident satisfaction, and clinical staffing ratio (Table 2). Negative average values (all in Cluster 2) indicate a value below the overall group mean. In Cluster 1, 87 SNFs (74%) rated at least three stars on the CMS Survey Rating, while only 19 out of 85 SNFs (22%) in Cluster 2 were rated at least three stars. Twenty centers in Cluster 1 had achieved a CMS five-star rating, while no center in Cluster 2 had achieved five stars.
TABLE 2.
Center-Level Variable Descriptive Statistics by Cluster Membership
| Cluster 1 (n = 118) | Cluster 2 (n = 85) | ||||
|---|---|---|---|---|---|
| Domain | Variable | Mean (SD) | Mean (SD) | R2 | P |
| Employees | Sick hours | 39.74 (9.44) | 40.17 (6.63) | 0% | |
| Employee Foundation | 0.46 (0.30) | 0.37 (0.26) | 2% | ||
| MIV Employee Satisfaction | 1.93 (0.17) | 1.78 (0.15) | 18% | ||
| MIV Employees’ response rate* | 0.85 (0.14) | 0.85 (0.13) | 0.821 | ||
| Workers Compensation Claim Rate* | 0.13 (0.06) | 0.14 (0.08) | 0.597 | ||
| CNA retention rate | 0.75 (0.11) | 0.68 (0.11) | 9% | ||
| RN retention rate* | 0.69 (0.15) | 0.57 (0.16) | <0.0001 | ||
| LPN retention rate* | 0.82 (0.17) | 0.74 (0.16) | <0.0001 | ||
| Clinical staffing ratio | 4.76 (1.00) | 3.75 (1.34) | 16% | ||
| Administrator/Director of Nursing Turnover (Y/N)* | 22.0% (26) | 16.5% (14) | 0.326† | ||
| Unionization (Y/N)* | 23.7% (27) | 13.4% (11) | 0.073† | ||
| Residents and Services | Rate of pressure ulcers | 0.02 (0.01) | 0.04 (0.02) | 28% | |
| Rate of falls | 0.17 (0.07) | 0.21 (0.07) | 6% | ||
| Rate of unexplained weight loss | 0.02 (0.01) | 0.03 (0.01) | 9% | ||
| Percent Medicaid and Medicare (2011)* | 0.82 (0.08) | 0.85 (0.07) | 0.0004 | ||
| MIV Satisfaction: Resident, Family or Friend | 2.34 (0.14) | 2.19 (0.16) | 18% | ||
| MIV Residents response rate* | 0.84 (0.18) | 0.81 (0.18) | 0.107 | ||
| Residents’ ADL transfer score* | 2.27 (0.21) | 2.26 (0.17) | 0.855 | ||
| Discharge rate* | 0.38 (0.18) | 0.32 (0.17) | 0.0058 | ||
| Proportion of short-term beds* | 0.15 (0.21) | 0.12 (0.19) | 0.344 | ||
| Short-term units (Y/N) * | 47.0% (54) | 43.4% (36) | 0.617† | ||
| CMS | Survey rating | 3.36 (1.16) | 1.87 (0.95) | 32% | |
| Quality rating* | 4.00 (0.90) | 3.52 (0.97) | 0.0002 | ||
| Staffing rating* | 3.05 (1.02) | 3.11 (0.99) | 0.849 | ||
| SRHP | Return on investment* | 0.81 (1.24) | 0.06 (0.72) | 0.0009 | |
| Relative change in WC claim rate* | 0.85 (0.43) | 1.13 (1.45) | 0.159 | ||
Percentage of variability explained by each variable or for variables not used for clusters, test of difference in distributions.
ADL, activities of daily living; CNA, Certified Nursing Aide; LPN, Licensed Practical Nurse; RN, Registered Nurse; ROI, return on investment; WCC, Workers’ Compensation Claim.
Variables not used in the cluster analysis.
P value from Wilcoxon nonparametric test, except (†) from Chi-squared statistic.
In the pairwise canonical scatterplot of the two-cluster solution, 19 SNFs were excluded due to missing data point(s) (Fig. 2). The two clusters were found to be moderately well-separated; there were about 15 centers in an overlapping region the center of the continuum defined by canonical variable 1, even though the three-cluster solution did not fit the data as well. Among the center characteristics compared post-hoc between the two clusters, there was not a single variable for which the centers in Cluster 2 achieved a better average value (Table 2). Centers in Cluster 1 were marginally more likely to have union representation. The clusters did not differ in having ‘‘many’’ or ‘‘few’’ wellness activities for their staff members. Most notably, Cluster 1 had higher retention rates for both RNs and LPNs, higher CMS Quality Ratings, and a higher ROI from the SRHP.
FIGURE 2.
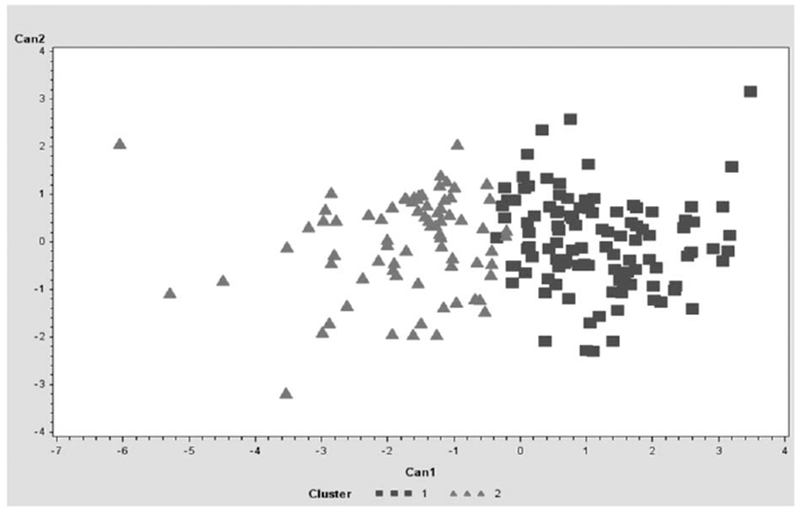
Canonical scatterplot depicting cluster pattern for nursing facilities in the two clusters.
The majority of pairwise Spearman correlation coefficients were low. Some exceptions included significant associations between nursing staff retention rates and a number of facility variables (Table 3). Among these, higher RN, CNA, and LPN retention rates were found to be significantly correlated with greater sick hour utilization. In addition, higher RN, CNA, and LPN retention rates were found to be significantly correlated with lower rates of resident falls. Higher RN retention rates were also significantly correlated with lower rates of resident pressure ulcers (Table 3). A positive correlation was found between MIV Employee Satisfaction and Resident/Family/Friends Satisfaction responses (r = 0.37, P < 0.05). At the facility level, higher rates of sick hour utilization per FTE were correlated with lower rates of resident falls (r = −0.17, P < 0.05), and greater reductions in workers compensation claims rates following SRHP introduction (r = 0.18, P < 0.05). CMS Survey Ratings were positively associated with worker job satisfaction, contributions to the employee foundation, clinical staffing ratio, RN and LPN retention, and resident and family satisfaction.
TABLE 3.
Significant Correlations Between Nursing Staff Retention Rates and Facility Variables
| Significant Association (P < 0.05) | Spearman Coefficient (r) | |
|---|---|---|
| RN retention rate | Sick hours | 0.16 |
| CNA retention | 0.44 | |
| LPN retention | 0.29 | |
| Rate of pressure ulcers | −0.32 | |
| Rate of falls | −0.15 | |
| Resident/Family/Friends satisfaction | 0.20 | |
| Discharge rate | −0.16 | |
| Survey rating | 0.24 | |
| CNA retention rate | Sick hours | 0.30 |
| Employee foundation | −0.18 | |
| WCC rate | −0.21 | |
| RN retention | 0.44 | |
| LPN retention | 0.41 | |
| Rate of falls | −0.38 | |
| Resident ADL transfer score | −0.18 | |
| Discharge rate | −0.21 | |
| Quality rating | 0.18 | |
| LPN retention rate | Sick hours | 0.23 |
| RN retention | 0.29 | |
| CNA retention | 0.41 | |
| Rate of falls | −0.28 | |
| Discharge rate | −0.19 | |
| Survey rating | 0.21 | |
| SPHM ROI | 0.27 |
ADL, activities of daily living; CNA, Certified Nursing Aide; LPN, Licensed Practical Nurse; RN, Registered Nurse; ROI, return on investment; WCC, Workers’ Compensation Claim.
In stratified analyses, the two-cluster solution was found to be quite stable. The 40 centers where there had been a change in nursing administration in the past year retained more favorable characteristics in Cluster 1, with the exception of employee foundation participation and employee survey response rates, which were slightly better in Cluster 2. In the 163 centers with no administration-level turnover, Cluster 1 centers consistently had better values for every variable. Stratification on the presence or absence of short-term beds (90 vs 108 facilities, respectively) and on the presence or absence of any union representation (22 vs 158 facilities, respectively) did not significantly change outcomes of the comparisons between the two clusters.
DISCUSSION
In this analysis of integrated data from a network of 203 SNFs, we found that that facilities with better patient care outcomes and greater resident satisfaction were also those with lower rates of workers compensation claims, better SRHP performance, higher employee retention rates, and higher rates of worker job satisfaction and engagement. Despite the fact that all facilities included in this analysis were owned or managed by a single company, two distinct groups of facilities could be differentiated using the study measures, with fewer than 10% in the central region of cluster overlap. These findings demonstrate that even under the management of a single corporate entity, there may exist notable differences in workers’ and residents’ experiences, with associated differences in facility performance. Higher-performing facilities identified in this analysis achieved consistently better performance across all of the domains studied: lower rates of resident adverse outcomes, higher clinical staff retention rates, higher staffing ratios, better employee and resident satisfaction, higher CMS survey ratings, and greater employee participation in the nonprofit foundation designed to offer employees temporary financial assistance. These findings support the value of integrated analyses of work and patient measures for evaluating nursing home care environments and for assessing the impacts of work organization on healthcare quality.
Interestingly, in this analysis, rate of employee sick hours was the only clustering variable that did not differ between the two clusters. However, we did find that at the facility level, higher rates of sick hour utilization per FTE were correlated with higher rates of personnel retention, lower rates of resident falls, and greater reductions in workers compensation claims rates following SRHP introduction. Although these positive associations with the utilization of more sick hours might initially seem counterintuitive, these findings may reflect supportive management practices and work environments that encourage appropriate use of sick hours when needed. Rather than serving as a direct measure of workforce morbidity, absenteeism is likely a more complex measure of workforce dynamics. The use of sick hours has been proposed to serve a positive function for workers in demanding jobs, permitting self-determined respite as needed from physical overload or psychological strain.45
One limitation of this study is that it is cross-sectional and therefore exploratory. The analysis method used in this study, k-means cluster analysis, is a multivariate statistical technique. In this approach, study subjects are separated into unique clusters based on unlabeled data, meaning that predictor and outcome relationships are not assumed to exist between quantitative facility measures and there is no method for validating these results. Thus, this method explores and identifies patterns of the interrelationships, but causal relationships between nursing home working conditions, worker satisfaction and safety, and patient satisfaction and care quality cannot be inferred from our results.
Nonetheless, the results of this study do provide some intriguing hypotheses for future investigations into how improvements in patient care worker retention and safety may be leveraged to positively impact resident care outcomes and quality of life. When workers feel safe and are more satisfied with their working conditions, they are less likely to look for other employment and may be more engaged in their daily activities and work interactions. The existence of relationships between occupational health and safety programming, staffing, and patient care staff turnover have been also been recently confirmed by Mohr et al,46 in their 2016 study of registered nurse staff retention and absenteeism relative to indicators of integrated employee occupational health services and health promotion in the Veterans Administration health system.46 Going further, retaining a higher proportion of experienced clinical staff supports care delivery and consistency, by maintaining facility staffing levels and ensuring that care providers are familiar with the residents in the facility. A central importance of staffing for maintaining care quality has been further demonstrated by the results of the CMS Staffing Study, which found a clear associations between nurse staffing ratios and nursing home quality of care.47 Although associations between staffing levels and health care quality have been demonstrated, however, how staffing, workforce retention, and work organization interact to impact health care quality remains to be further understood.
One limitation of the present study is the use of facility as the units of observation. How the present findings relate to the work or living experiences of individual workers or residents is not clear. Nonetheless, employee gender ratios and average age varied little across centers, suggesting that these demographic differences were unlikely to have confounded or moderated the results.37 In contrast, a strength of this study design was that our access to data from multiple sources and multiple facilities permitted comparisons of factors that are inherently collective, including staffing ratios, CMS ratings, SRHP impacts on WCC rates, and de-identified, aggregated resident and worker survey responses.
In this study, we used a cluster analysis approach to examine patterns between objective measures covering multiple long-term care work and productivity domains. Cluster analysis methods may be applied to explore relationships between analysis variables without the need to specifically identify independent versus outcome variables. There are a number of different techniques available for cluster analysis,41,48 but there is no single standard approach and no established objective criteria for selecting the number of clusters.44 Although results may differ depending on the specific method and starting assumptions, the k-means approach has been widely used for exploratory data analysis in complex systems. This method is highly sensitive to distance metrics, missing data points, and the sorting of observations. Nonetheless, we believe that the application of a cluster analysis approach to explore work satisfaction, work safety, resident satisfaction, and health care quality in long-term care represents a useful extension of these methods for health care systems evaluation. This exploratory study is among initial studies that have focused on cluster analysis to examine the unobserved variation among SNFs. Future studies should focus on analytical techniques that can incorporate both continuous and categorical study measures, as well as variables measured on different scales, to provide better understanding on the complex interrelationship between workers and residents in nursing home facilities.
In conclusion, the results of this study provide evidence to support the inter-relatedness of long-term care work organization, work safety, patient safety, and quality of care. Although clinical and human resource data are routinely collected, the complexity of these data streams and their separate management pathways have resulted in their infrequently being examined in relation to each other. Nonetheless, the linkages between health care safety and quality found in this study suggest that integrated assessment and management of these domains may offer opportunities for ongoing work safety and care quality improvement. Given the projected increases in the aging population and the expanding demand for long-term care services, integrated performance evaluation methods offer promise for understanding how investments in workplace safety, higher staffing levels, and employee engagement programs may yield further benefits in the form of improved employee retention, improved resident satisfaction, and better quality of care.
ACKNOWLEDGMENT
We thank our corporate partner for the many data and documentation files.
The work is supported by Grant No. U19-OH008857 from the U.S. NIOSH (NIOSH/CDC). This work is solely the responsibility of the authors and does not necessarily represent the official views of NIOSH.
Footnotes
The authors have no conflicts of interest to declare.
Contributor Information
Ernest Boakye-Dankwa, College of Health Sciences, University of Massachusetts Lowell, Lowell, Massachusetts; Institute for Health and Ageing, Australian Catholic University, Melbourne, Victoria, Australia.
Erin Teeple, College of Health Sciences, University of Massachusetts Lowell, Lowell, Massachusetts.
Rebecca Gore, College of Health Sciences, University of Massachusetts Lowell, Lowell, Massachusetts.
Laura Punnett, College of Health Sciences, University of Massachusetts Lowell, Lowell, Massachusetts.
REFERENCES
- 1.Pekkarinen L, Sinervo T, Perala ML, Elovainio M. Work stressors and the quality of life in long-term care units. Gerontologist. 2004;44:633–643. [DOI] [PubMed] [Google Scholar]
- 2.Castle NG, Engberg J. The influence of staffing characteristics on quality of care in nursing homes. Health Serv Res 2007;42:1822–1847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Collier E, Harrington C. Staffing characteristics, turnover rates, and quality of resident care in nursing facilities. Res Gerontol Nurs 2008;1:157–170. [DOI] [PubMed] [Google Scholar]
- 4.Institute of Medicine. Keeping Patients Safe: Transforming the Work Environment of Nurses . Washington, DC: The National Academies Press; 2004, 23–52. [Google Scholar]
- 5.Shin JH, Hyun TK. Nurse staffing and quality of care of nursing home residents in Korea. J Nurs Scholarsh 2015;47:555–564. [DOI] [PubMed] [Google Scholar]
- 6.Spilsbury K, Hewitt C, Stirk L, Bowman C. The relationship between nurse staffing and quality of care in nursing homes: a systematic review. Int J Nurs Stud 2011;48:732–750. [DOI] [PubMed] [Google Scholar]
- 7.Warren N, Hodgson M, Craig T, et al. Employee working conditions and healthcare system performance: the Veterans Health Administration experience. J Occup Environ Med 2007;49:417–429. [DOI] [PubMed] [Google Scholar]
- 8.The National Institute for Occupational Safety and Health. State of the Sector: Healthcare and Social Assistance: Identification of Research Opportunities for the Next Decade of NORA. US Department of Health and Human Services; 2009. Available at: https://www.cdc.gov/niosh/docs/2009-139/pdfs/2009-139.pdf. [Google Scholar]
- 9.Engels JA, van der Beek AJ, van der Gulden JW. A LISREL analysis of work-related risk factors and health complaints in the nursing profession. Int Arch Occup Environ Health. 1998;71:537–542. [DOI] [PubMed] [Google Scholar]
- 10.Galinsky T, Waters T, Malit B. Overexertion injuries in home healthcare workers and the need for ergonomics. Home Health Care Serv Q. 2001;20:57–73. [DOI] [PubMed] [Google Scholar]
- 11.Kurowski A, Boyer J, Punnett L. The health hazards of healthcare In:Duffy M, Armenia A, Stacey CL, editors. Caring on the Clock: The Complexities and Contradictions of Paid Care Work. New Brunswick, NJ: Rutgers University Press; 2015. p. 83–93. [Google Scholar]
- 12.Jakobsen LM, Jorgensen AF, Thomsen BL, Greiner BA, Rugulies R. A multilevel study on the association of observer-assessed working conditions with depressive symptoms among female eldercare workers from 56 work units in 10 care homes in Denmark. BMJ Open. 2015;5:e008713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Holtermann A, Clausen T, Jørgensen MB, Burdorf A, Andersen LL. Patient handling and risk for developing persistent low-back pain among female healthcare workers. Scand J Work Environ Health. 2013;39:164–169. [DOI] [PubMed] [Google Scholar]
- 14.Yassi A, Lockhart K. Work-relatedness of low back pain in nursing personnel: a systematic review. Int J Occup Environ Health. 2013;19: 223–244. [DOI] [PubMed] [Google Scholar]
- 15.US Bureau of Labor Statistics. Nonfatal Occupational Injuries and Illnesses Requiring Days Away from Work, 2014. US Department of Labor; 2015. Available at: https://www.bls.gov/news.release/archives/osh2_11192015.pdf. Accessed September 27, 2017. [Google Scholar]
- 16.Trinkoff AM, Le R, Geiger-Brown J, Lipscomb J, Lang G. Longitudinal relationship of work hours, mandatory overtime, and on-call to musculoskeletal problems in nurses. Am J Ind Med 2006;49:964–971. [DOI] [PubMed] [Google Scholar]
- 17.de Jonge J, Le Blanc PM, Peeters MC, Noordam H. Emotional job demands and the role of matching job resources: a cross-sectional survey study among health care workers. Int J Nurs Stud 2008;45:1460–1469. [DOI] [PubMed] [Google Scholar]
- 18.Eriksen W, Tambs K, Knardahl S. Work factors and psychological distress in nurses’ aides: a prospective cohort study. BMC Public Health. 2006;6:290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Geiger-Brown J, Muntaner C, Lipscomb J, Trinkoff A. Demanding work schedules and mental health in nursing assistants working in nursing homes. Work Stress. 2004;18:292–304. [Google Scholar]
- 20.Miranda H, Punnett L, Gore RJ, Team PR. Musculoskeletal pain and reported workplace assault: a prospective study of clinical staff in nursing homes. Hum Factors. 2014;56:215–227. [DOI] [PubMed] [Google Scholar]
- 21.Muntaner C, Li Y, Xue X, O’Campo P, Chung HJ, Eaton WW. Work organization, area labor-market characteristics, and depression among U.S. nursing home workers: a cross-classified multilevel analysis. Int J Occup Environ Health. 2004;10:392–400. [DOI] [PubMed] [Google Scholar]
- 22.Myers D, Silverstein B, Nelson NA. Predictors of shoulder and back injuries in nursing home workers: a prospective study. Am J Ind Med 2002;41:466–476. [DOI] [PubMed] [Google Scholar]
- 23.van den Tooren M, de Jonge J. Managing job stress in nursing: what kind of resources do we need? J Adv Nurs 2008;63:75–84. [DOI] [PubMed] [Google Scholar]
- 24.Miranda H, Punnett L, Gore R, Boyer J. Violence at the workplace increases the risk of musculoskeletal pain among nursing home workers. Occup Environ Med 2011;68:52–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhang Y, Punnett L, Gore R, Team C-NR. Relationships among employees’ working conditions, mental health, and intention to leave in nursing homes. J Appl Gerontol 2014;33:6–23. [DOI] [PubMed] [Google Scholar]
- 26.Zhang Y, Punnett L, McEnany GP, Gore R. Contributing influences of work environment on sleep quantity and quality of nursing assistants in long-term care facilities: a cross-sectional study. Geriatr Nurs 2016;37:13–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Miranda H, Gore RJ, Boyer J, Nobrega S, Punnett L. Health behaviors and overweight in nursing home employees: contribution of workplace stressors and implications for worksite health promotion. Sci World J 2015;2015: 915359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.American Health Care Association. 2012. Staffing Report 2014. Available at: http://www.ahcancal.org/research_data/staffing/Documents/2012_Staffing_Report.pdf.
- 29.Donoghue C Nursing home turnover and retention: an analysis of national level data. J Appl Gerontol 2010;29:89–106. [Google Scholar]
- 30.Alsaraireh F, Quinn Griffin MT, Ziehm SR, Fitzpatrick JJ. Job satisfaction and turnover intention among Jordanian nurses in psychiatric units. Int J Ment Health Nurs 2014;23:460–467. [DOI] [PubMed] [Google Scholar]
- 31.Bowers BJ, Esmond S, Jacobson N. Turnover reinterpreted CNAs talk about why they leave. J Gerontol Nurs 2003;29:36–43. [DOI] [PubMed] [Google Scholar]
- 32.Castle NG, Engberg J. Organizational characteristics associated with staff turnover in nursing homes. Gerontologist. 2006;46:62–73. [DOI] [PubMed] [Google Scholar]
- 33.Kemper P, Heier B, Barry T, et al. What do direct care workers say would improve their jobs? Differences across settings. Gerontologist. 2008;48(Spec No 1):17–25. [DOI] [PubMed] [Google Scholar]
- 34.Kurowski A, Boyer J, Fulmer S, Gore R, Punnett L. Changes in ergonomic exposures of nursing assistants after the introduction of a no-lift program in nursing homes. Int J Ind Ergon 2012;42:525–532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kurowski A, Gore R, Buchholz B, Punnett L. Differences among nursing homes in outcomes of a safe resident handling program. J Healthc Risk Manag 2012;32:35–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kurowski A, Buchholz B, Punnett L, Team PR. A physical workload index to evaluate a safe resident handling program for nursing home personnel. Hum Factors. 2014;56:669–683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kurowski A, Gore R, Roberts Y, Kincaid K, Punnett L. Injury rates before and after the implementation of a safe resident handling program in the long-term care sector. Safety Sci 2017;92:217–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lahiri S, Latif S, Punnett L, ProCare Research Team. An economic analysis of a safe resident handling program in nursing homes. Am J Ind Med 2013;56:469–478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Health NRC. My InnerView. 2015. Available at: https://www.myinnerview.com/index.php.
- 40.Fisher L, Van Ness J. Admissible clustering procedures. Biometrika. 1971;58: 91–104. [Google Scholar]
- 41.Saunders J Cluster analysis. J Market Manag 1994;194:13–28. [Google Scholar]
- 42.Fu P Tip: K-means Clustering in SAS: Comparing PROC FASTCLUS and PROC HPCLUS. SAS Communities Library; 2014. Available at: https://communities.sas.com/t5/SAS-Communities-Library/Tip-K-means-clustering-in-SAS-comparing-PROC-FASTCLUS-and-PROC/ta-p/221369. [Google Scholar]
- 43.Lattin J, Carroll J, Green P. Analyzing Multivariate Data. Pacific Grove, CA: Thomson Brooks Cole Publishing; 2003. [Google Scholar]
- 44.Koehly L, Arabie P, Bradlow E, Hutchinson W. How do I choose the optimal number of clusters in cluster analysis? J Consum Psychol 2001;10: 102–104. [Google Scholar]
- 45.Kristensen TS. Sickness absence and work strain among Danish slaughterhouse workers: an analysis of absence from work regarded as coping behaviour. Soc Sci Med 1991;32:15–27. [DOI] [PubMed] [Google Scholar]
- 46.Mohr DC, Schult T, Eaton JL, Awosika E, McPhaul KM. Integrated employee occupational health and organizational-level registered nurse outcomes. J Occup Environ Med 2016;58:466–470. [DOI] [PubMed] [Google Scholar]
- 47.Kramer AM, Fish R. The relationship between nursing staffing levels and the quality of nursing home care Phase II final report to the Centers for Medicare & Medicaid Services. Washington, DC: Department of Health and Human Services; 2001:1–26. [Google Scholar]
- 48.Dolnicar S A review of unquestioned standards in using cluster analysis for data-driven market segmentation. CD Conference Proceedings of Australian and New Zealand Marketing Academy Conference 2002 (ANZMAC 2002); 2002. Available at: http://ro.uow.edu.au/cgi/viewcontent.cgi?article=1286&-context=commpapers. [Google Scholar]


