Abstract
Objectives
Glucocorticoids have anti-inflammatory, transrepression-mediated effects, although adverse events (AEs; transactivation-mediated effects) limit long-term use in patients with rheumatoid arthritis (RA). We evaluated the efficacy and safety of fosdagrocorat (PF-04171327), a dissociated agonist of the glucocorticoid receptor, versus prednisone or placebo.
Methods
In this 12-week, phase II, randomised controlled trial, 323 patients with moderate to severe RA were randomised 1:1:1:1:1:1:1 to fosdagrocorat (1 mg, 5 mg, 10 mg or 15 mg), prednisone (5 mg or 10 mg) or placebo, once daily. The primary endpoints (week 8) were American College of Rheumatology 20% improvement criteria (ACR20) responses, and percentage changes from baseline in biomarkers of bone formation (procollagen type 1 N-terminal peptide [P1NP]) and resorption (urinary N-telopeptide to urinary creatinine ratio [uNTx:uCr]). Safety was assessed.
Results
ACR20 responses with fosdagrocorat 10 mg and 15 mg were superior to placebo, and fosdagrocorat 15 mg was non-inferior to prednisone 10 mg (week 8 model-predicted ACR20 responses: 47%, 61%, 69% and 73% vs 51%, 71% and 37% with fosdagrocorat 1 mg, 5 mg, 10 mg and 15 mg vs prednisone 5 mg, 10 mg and placebo, respectively). Percentage changes from baseline in P1NP with fosdagrocorat 1 mg, 5 mg and 10 mg met non-inferiority criteria to prednisone 5 mg. Corresponding changes in uNTx:uCr varied considerably. All fosdagrocorat doses reduced glycosylated haemoglobin levels. AEs were similar between groups; 63 (19.5%) patients reported treatment-related AEs; 9 (2.8%) patients reported serious AEs. No patients had adrenal insufficiency, treatment-related significant infections or laboratory abnormalities. No deaths were reported.
Conclusion
In patients with RA, fosdagrocorat 10 mg and 15 mg demonstrated efficacy similar to prednisone 10 mg and safety similar to prednisone 5 mg.
Trial registration number
Keywords: disease activity, rheumatoid arthritis, treatment
Key messages.
What is already known about this subject?
Glucocorticoids (GCs) are widely used to treat patients with rheumatoid arthritis (RA).
However, they are associated with adverse effects, and efforts to improve efficacy and reduce adverse consequences of GCs include the development of dissociated agonists of the GC receptors (DAGRs).
Phase I studies of the DAGR, fosdagrocorat (10–25 mg), showed equivalent anti-inflammatory effects and bone formation biomarker reductions to prednisone (5–20 mg); and in a short phase IIa study in patients with RA on stable background methotrexate (MTX), fosdagrocorat (10 and 25 mg) improved the symptoms of active disease compared with prednisone (5 mg once daily).
What does this study add?
In patients with RA receiving background MTX, we have demonstrated the similar efficacy of fosdagrocorat (10 mg and 15 mg) to prednisone (10 mg), and the similar safety profile of these doses of fosdagrocorat to prednisone (5 mg).
How might this impact on clinical practice?
Larger-scale, and longer-term, evaluations of fosdagrocorat in patient populations with active RA who are naïve to GC will help clarify the bone and glucose metabolism effects of fosdagrocorat and assist in determining its future role in the treatment of RA.
Introduction
Two-thirds of patients with rheumatoid arthritis (RA) receive glucocorticoids (GCs) during treatment to reduce signs and symptoms of active disease and inhibit progression of joint structural damage.1–3 Unfortunately, GCs are associated with adverse effects, especially at doses >7.5 mg/day and over longer treatment duration,4–7 which cause considerable morbidity.8 Although guidelines and recommendations exist for managing patients receiving GC therapy,9–12 GC use presents a clinical challenge in balancing benefits and risks. Developments to improve the efficacy and/or reduce adverse consequences include evaluation of selective GC receptor agonists (SEGRAs), dissociated agonists of the GC receptor (DAGRs) and liposomal GCs. Here, we report the findings of a phase II trial of fosdagrocorat (PF-04171327), a first-in-class, oral, selective, high-affinity DAGR under investigation for the treatment of RA.
GCs are estimated to regulate transcription of ~1% of the genome, including suppression of proinflammatory genes (transrepression) and upregulated protein synthesis (transactivation). It is considered that transrepression predominantly produces anti-inflammatory effects, while transactivation (affecting glucose metabolism) or a combination of both (affecting bone metabolism) are responsible for their adverse effects.13 14 An agent that shifts the transrepression/transactivation ratio towards transrepression may provide an improved GC benefit to risk ratio.
Fosdagrocorat demonstrated similar anti-inflammatory activity to standard GC receptor agonists while avoiding some associated adverse events (AEs) in preclinical studies. Phase I studies show single oral doses of fosdagrocorat 10–25 mg were associated with equivalent anti-inflammatory effects and similar reductions in bone formation biomarkers to single doses of prednisone 5–20 mg.15 16 In a 2-week, phase IIa study in patients with active RA on stable background methotrexate (MTX), fosdagrocorat 10 mg and 25 mg once daily were well tolerated and demonstrated rapid and robust onset of improved signs and symptoms of active disease versus placebo and prednisone 5 mg once daily.17
Fosdagrocorat is believed to bind to the cytosolic GC receptor with the resulting fosdagrocorat–GC receptor complex conformation enabling transrepression while prohibiting, or reducing, transactivation activities.18 19 The transcription factor binding site may function like GC–GC receptor complexes, enabling suppression of proinflammatory gene expression, but the DNA-binding site is thought to be non-functional or dysfunctional, thereby reducing or preventing unwanted transactivation activities (online supplementary figure S1). Preclinical studies of other SEGRA/DAGR agents support this theory of a shift in the transrepression/transactivation ratio.20–22 Thus, fosdagrocorat is expected to reduce inflammation with fewer of the AEs typically associated with the transactivation activities of GC use.18 19
rmdopen-2018-000889supp001.docx (3.6MB, docx)
We evaluated the clinical efficacy of fosdagrocorat in patients with RA and its effects on safety, measured by bone biomarkers, glucose metabolism and the hypothalamic-pituitary-adrenal (HPA) axis, versus prednisone or placebo. The underlying transrepression/transactivation hypothesis was also investigated in a clinical setting.
Methods
Study design and patients
This was a 12-week, phase II, multicentre, double-blind, parallel-group, active-controlled and placebo-controlled trial in patients with active RA. Using an interactive voice response system, patients with stable background MTX were randomised 1:1:1:1:1:1:1 to receive fosdagrocorat 1 mg, 5 mg, 10 mg or 15 mg, prednisone 5 mg or 10 mg, or matched placebo for 8 weeks, followed by 4-week blinded taper and 1-week washout (online supplementary figure S2). The randomisation procedure used blocks of 14, and there were four strata based on geographical randomisation. All study treatments were administered once daily. During taper, patients received the study drug (fosdagrocorat 1 mg, prednisone 5 mg or placebo, according to randomisation) and placebo on alternate days over weeks 9 and 10, every 3 days over weeks 11 and 12, and no study medication during week 13 (online supplementary figure S2).
Patients (aged >18 years) with active RA defined as ≥6 tender and ≥6 swollen joints (of 28-joint count) plus C reactive protein (CRP) ≥7 mg/L at screening had received MTX for ≥3 months, with a stable dose (≤25 mg per week) for ≥8 weeks. Key exclusion criteria included GC use within 6 weeks of screening, active or latent tuberculosis, and clinically significant infection within 6 months of screening (online supplementary section S1).
Patients were recruited at 73 centres globally (online supplementary section S2; table S1).
Outcomes and procedures
The primary objectives were to compare the efficacy and safety of fosdagrocorat 1 mg, 5 mg, 10 mg and 15 mg with prednisone 5 mg and 10 mg, and placebo, and to identify fosdagrocorat dose(s) with American College of Rheumatology 20% improvement criteria (ACR20) response(s) similar to prednisone 10 mg and bone biomarker changes similar to prednisone 5 mg. The primary efficacy endpoint was ACR20/50/70 responses at week 8; coprimary bone biomarker endpoints were percentage changes from baseline at week 8 in serum procollagen type 1 N-terminal propeptide (P1NP; bone formation) and urinary N-telopeptide to urinary creatinine ratio (uNTx:uCr; bone resorption).
Efficacy assessments
Efficacy endpoints were assessed at weeks 2, 4, 6, 8 and 12, and included ACR20/50/70 responses; individual ACR component scores; Disease Activity Score in 28 joints with CRP (DAS28-4[CRP] and DAS28-3[CRP]: tender and swollen joint counts, CRP, patient global assessment of arthritis [DAS28-4(CRP) only]); Health Assessment Questionnaire-Disability Index (HAQ-DI)23 24; and Short-Form 36 Health Survey (SF-36, V.2, acute version)25 at weeks 4, 8 and 12.
Pharmacodynamic evaluations
Serum levels of bone biomarkers P1NP, uNTx:uCr and osteocalcin (OC; bone formation) were measured at baseline and at weeks 2, 4, 6, 8, 10, 12 and 13, and C-terminal telopeptide (CTx [a by-product biomarker of bone resorption]) at baseline and at weeks 4, 8 and 12.
Safety
Safety endpoints included plasma levels of active fosdagrocorat (PF-00251802) and its metabolite (PF-04015475); glycosylated haemoglobin (HbA1c) concentration (screening, weeks 8 and 12); fasting plasma glucose (baseline, weeks 4, 8, 12 and 13); lymphocyte, neutrophil and eosinophil cell counts (weeks 4, 8 and 12); and HPA axis suppression measured by serum cortisol levels following adrenocorticotropic hormone (ACTH) stimulation test at week 13 (online supplementary section S3). AEs and laboratory values were assessed throughout the study.
Sample size rationale and statistical analysis methods
Sample size calculations were based on the ability to estimate the dose–response curve for an ACR20 response at week 8 with an acceptable degree of precision and to select a minimally effective dose (MED) that had a true effect within an acceptable range with a reasonably good probability. In order to estimate the probability of finding a dose with an acceptable effect for sample size, study design and analysis methods in the study, 250 trials were simulated, with the following assumptions: (1) maximum difference over placebo is ~50% for ACR20 response; (2) dose resulting in 50% of maximum effect (ED50) is 5 mg; (3) n=45 per group; and (4) an acceptable range for an MED for the placebo-corrected ACR20 response is 20%–35%. The lowest dose that met the criteria of: the 80% lower confidence bound for the placebo-corrected difference, obtained from an Emax model using Bayesian methods, of >20%; would identify a dose in the acceptable range with an estimated probability of 0.68.
All analyses used the full analysis set (all randomised patients receiving ≥1 dose of study drug). The primary efficacy analysis used a four-parameter Emax model to characterise the week 8 ACR20 dose response. Bayesian methods with moderately informative prior distributions for the four parameters were used to fit the model. The prior distributions were empirically based on a previous proof-of-concept study for this compound and distributions obtained from the referenced meta-analysis.26 27 Model-based estimates determined fosdagrocorat superiority of ≥20% versus placebo, with ≥80% confidence (ie, lower bound of 60% credible interval ≥20%) and fosdagrocorat non-inferiority to prednisone 10 mg by a ≥5% margin with ≥80% confidence (ie, lower bound of 60% credible interval ≥5%). For binary endpoints, missing values due to patient dropout from the trial were handled using non-responder imputation.
Coprimary bone biomarkers (P1NP and uNTx:uCr) were analysed as percentage change from baseline in the week 8 (0 hour) measurement with a mixed-effects repeated measure model (MMRM) that included fixed effects of treatment, visit and treatment-by-visit interaction, and baseline value. An unstructured variance-covariance matrix was used. The primary treatment comparison was based on the week 8 contrast between fosdagrocorat dose groups and prednisone 5 mg. MMRM model-based estimates of treatment differences in mean percentage changes from baseline and corresponding CIs were used to assess non-inferiority of the bone biomarkers to prednisone 5 mg by a margin of 20% with 90% confidence (ie, for P1NP, lower bound of 80% CI for treatment difference must be ≥20%; for uNTX:uCR, upper bound of 80% CI for treatment difference must be <20%).
Secondary bone biomarkers (OC and serum CTx) and other longitudinal continuous endpoints in the trial were similarly analysed (including DAS28-3[CRP], DAS-28-4[CRP], fasting plasma glucose and SF-36).
Dose–response modelling for DAS28-4(CRP) at week 8 was performed using an Emax model similar to that used for ACR20, with last observation carried forward to handle missing data.
Other binary endpoints were analysed using the normal approximation for differences in binomial proportions, with binomial proportions, treatment differences (and CIs) reported by week. HbA1c was analysed as change from screening at week 8 using analysis of covariance with treatment and baseline values as covariates. SAS, R and OpenBUGS software (R version 3.4.4 [2018-03-15]) were used to complete the statistical analyses.
Results
In total, 649 patients were screened (online supplementary figure S3), with 323 randomised and treated between September 2011 and June 2014: fosdagrocorat 1 mg (n=45), 5 mg (n=47), 10 mg (n=45) and 15 mg (n=48); prednisone 5 mg (n=45) and 10 mg (n=46); and placebo (n=47). Overall, 91.6% (n=296) of randomised and treated patients completed the trial (online supplementary figure S3). Baseline demographics and disease characteristics were generally balanced between groups (table 1).
Table 1.
Baseline demographics and characteristics
| Fosdagrocorat | Prednisone | Placebo | |||||
| 1 mg (n=45) |
5 mg (n=47) |
10 mg (n=45) |
15 mg (n=48) |
5 mg (n=45) |
10 mg (n=46) |
(n=47) | |
| Age (years), mean (range) | 50 (18–78) | 55 (29–77) | 55 (25–80) | 54 (27–84) | 53 (20–78) | 57 (34–75) | 55 (23–79) |
| Race (white), n (%) | 38 (84.4) | 41 (87.2) | 43 (95.6) | 42 (87.5) | 39 (86.7) | 38 (82.6) | 41 (87.2) |
| Gender (female), n (%) | 33 (73.3) | 38 (80.9) | 34 (75.6) | 37 (77.1) | 39 (86.7) | 41 (89.1) | 37 (78.7) |
| Disease duration (years), mean (range) | 7.9 (0.3–33.0) | 8.1 (0.3–42.0) | 6.6 (0.3–27.0) | 8.2 (0.3–35.0) | 7.4 (0.3–34.9) | 5.2 (0.3–17.0) | 6.7 (0.3–33.0) |
| Postmenopausal, n (%)* | 15 (33.3) | 17 (36.2) | 22 (48.9) | 17 (35.4) | 18 (40.0) | 26 (56.5) | 23 (48.9) |
| DAS28-4(CRP), mean (SD)† | 5.82 (0.85) | 5.96 (0.80) | 5.98 (0.73) | 5.92 (0.70) | 5.95 (0.84) | 5.99 (0.67) | 6.00 (0.84) |
| SJC, mean (SD) | 13.7 (5.9) | 15.7 (5.4) | 14.6 (5.8) | 14.5 (5.6) | 14.9 (6.4) | 14.9 (4.5) | 15.9 (5.5) |
| TJC, mean (SD) | 11.6 (5.2) | 11.6 (4.6) | 11.0 (4.9) | 10.9 (4.8) | 11.6 (4.5) | 11.3 (3.8) | 12.1 (3.8) |
| CRP (mg/L), mean (SD)† | 23.2 (21.9) | 25.5 (23.7) | 26.9 (20.7) | 26.3 (26.1) | 24.6 (23.8) | 27.0 (38.1) | 22.4 (24.0) |
| IGT, n (%) | 1 (2.2) | 0 | 1 (2.2) | 0 | 0 | 0 | 0 |
| DM, n (%) | 3 (6.7) | 0 | 1 (2.2) | 1 (2.1) | 1 (2.2) | 1 (2.2) | 0 |
| P1NP (ng/mL), mean (SD)‡ | 58.4 (28.4) | 51.3 (25.6) | 50.5 (28.5) | 50.1 (25.2) | 52.9 (28.6) | 48.7 (18.4) | 58.0 (30.9) |
| Median (Q1–Q3) | 57.2 (37.0–66.3) | 46.2 (32.7–63.2) | 43.1 (30.3–64.4) | 46.2 (34.0–62.4) | 47.8 (34.9–59.9) | 49.2 (31.9–60.5) | 52.2 (33.4–79.5) |
| uNTx:uCr (nM BCE/mM), mean (SD)§ | 58.5 (38.6) | 60.5 (39.3) | 54.6 (35.7) | 48.7 (22.4) | 67.0 (51.6) | 53.0 (25.0) | 64.9 (30.8) |
| Median (Q1–Q3) | 53.1 (34.3–63.7) | 49.1 (30.1–80.6) | 47.9 (30.8–65.3) | 44.3 (33.0–59.1) | 50.7 (38.2–73.9) | 46.1 (33.7–72.0) | 60.0 (44.7–86.3) |
| OC (ng/mL), mean (SD)‡ | 27.6 (13.9) | 26.4 (13.8) | 24.2 (12.6) | 21.3 (8.5) | 24.5 (11.9) | 22.9 (7.5) | 26.1 (12.3) |
| Median (Q1–Q3) | 26.6 (18.7–31.4) | 22.4 (14.5–36.5) | 21.1 (14.3–32.8) | 20.1 (15.8–25.2) | 23.3 (15.2–30.7) | 21.2 (18.3–28.6) | 25.3 (17.6–32.7) |
| CTx (ng/mL), mean (SD)‡ | 0.50 (0.25) | 0.49 (0.30) | 0.43 (0.26) | 0.43 (0.24) | 0.50 (0.27) | 0.43 (0.21) | 0.49 (0.25) |
| Median (Q1–Q3) | 0.48 (0.37–0.60) | 0.48 (0.25–0.60) | 0.43 (0.21–0.57) | 0.37 (0.23–0.65) | 0.45 (0.33–0.58) | 0.38 (0.27–0.60) | 0.48 (0.27–0.65) |
| Cortisol (ng/mL), mean (SD)¶ | 104.4 (53.4) | 117.9 (57.2) | 108.6 (48.9) | 109.4 (58.1) | 115.3 (48.5) | 120.1 (54.5) | 113.7 (60.1) |
| HAQ-DI, mean (SD) | 1.40 (0.71) | 1.60 (0.64) | 1.47 (0.60) | 1.61 (0.63) | 1.62 (0.55) | 1.63 (0.58) | 1.65 (0.56) |
| SF-36 PCS, mean (SD) | 33.24 (7.29) | 31.49 (6.21) | 30.44 (6.53) | 31.87 (7.41) | 31.86 (6.46) | 30.52 (7.18) | 31.68 (6.08) |
| SF-36 MCS, mean (SD) | 38.28 (10.34) | 38.08 (10.62) | 42.41 (12.08) | 37.61 (10.79) | 40.05 (11.55) | 37.30 (10.07) | 38.74 (9.56) |
All study treatments were administered once daily.
*Menopause was assessed by study investigator at week 2.
†n=45 for prednisone 10 mg.
‡n=45, 47, 45, 47, 44, 45 and 47 for fosdagrocorat 1 mg, 5 mg, 10 mg and 15 mg, prednisone 5 mg and 10 mg, and placebo, respectively.
§n=45, 47, 44, 48, 44, 45 and 47 for fosdagrocorat 1 mg, 5 mg, 10 mg, and 15 mg, prednisone 5 mg and 10 mg, and placebo, respectively.
¶n=45, 47, 43, 48, 43, 43 and 45 for fosdagrocorat 1 mg, 5 mg, 10 mg, and 15 mg, prednisone 5 mg and 10 mg, and placebo, respectively.
BCE, bone collagen equivalent;CRP, C reactive protein;CTx, C-terminal telopeptide;DAS28-4(CRP), Disease Activity Score in 28 joints (CRP);DM, diabetes mellitus;HAQ-DI, Health Assessment Questionnaire-Disability Index;IGT, impaired glucose tolerance;MCS, mental component summary;n, number of patients with observations;OC, osteocalcin;PCS, physical component summary;P1NP, procollagen type 1 N-terminal propeptide;Q, quartile;SF-36, Short-Form 36 Health Survey;SJC, swollen joint count;TJC, tender joint count;uNTx:uCr, urinary N-telopeptide to urinary creatinine ratio.
Efficacy assessments
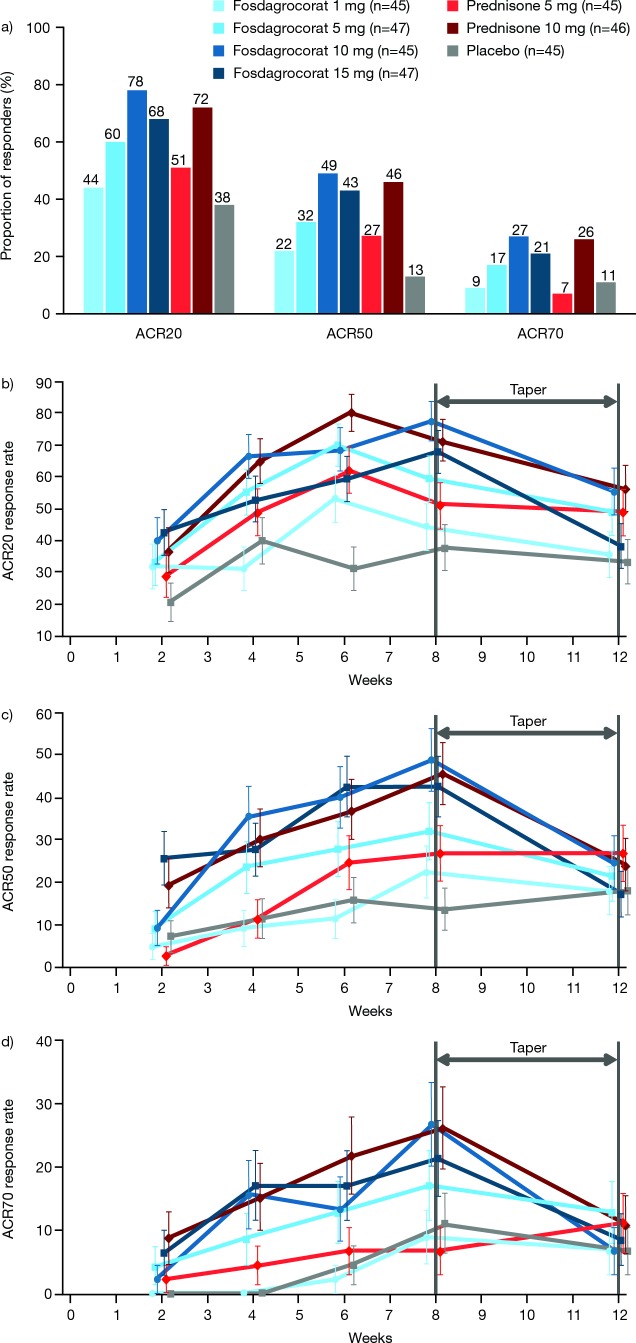
Week 8 ACR20 responses demonstrated efficacy: fosdagrocorat 10 mg and 15 mg were superior to placebo; fosdagrocorat 15 mg non-inferior to prednisone 10 mg; and fosdagrocorat 10 mg numerically similar to prednisone 10 mg (figure 1). Model-based estimates of ACR20 responses at week 8 were 47%, 61%, 69% and 73% for fosdagrocorat 1 mg, 5 mg, 10 mg and 15 mg, respectively, and 51%, 71% and 37% for prednisone 5 mg and 10 mg, and placebo, respectively (online supplementary figure S4).
Figure 1.
(A) ACR20, ACR50 and ACR70 sample proportions at week 8, and (B) ACR20, (C) ACR50 and (D) ACR70 responses over time (Fas, NRI). All study treatments were administered once daily. ACR20/50/70, American College of Rheumatology response criteria; Fas, full analysis set; NRI, non-responder imputation.
ACR20/50/70 responses demonstrated similar trends with fosdagrocorat 10 mg across all time points; fosdagrocorat 10 mg and 15 mg were comparable with prednisone 10 mg at week 8 (figure 1). ACR component scores followed similar trends (online supplementary figure S5).
Week 8 DAS28-4(CRP) mean changes from baseline (online supplementary figures S6A,B) were numerically greater for fosdagrocorat (all doses) than placebo. DAS28-3(CRP) results demonstrated numerical similarity between fosdagrocorat 15 mg and prednisone 10 mg, and all active treatments had numerically greater changes from baseline than placebo (online supplementary figure S6C,D). Fosdagrocorat 10 mg showed numerically greater reductions from baseline in DAS28-4(CRP) versus prednisone 10 mg: –0.09 (–0.61, 0.42). Emax dose–response modelling analysis demonstrated efficacy for fosdagrocorat 10 mg and 15 mg at week 8 and a dose–response relationship for all fosdagrocorat doses (online supplementary figure S7). The results for DAS28-4(CRP) at week 8 were generally consistent with the ACR primary efficacy endpoint.
Across all active treatments, patients reported clinically meaningful improvements (reductions ≥0.22) from baseline in HAQ-DI at week 8 (online supplementary table S2). Week 8 mean changes from baseline in SF-36 physical component summary scores trended towards improvement with fosdagrocorat 5 mg, 10 mg and 15 mg versus placebo. There were numerical improvements in week 8 mean changes from baseline in mental component summary scores with fosdagrocorat versus placebo (online supplementary table S2).
Pharmacodynamic evaluations
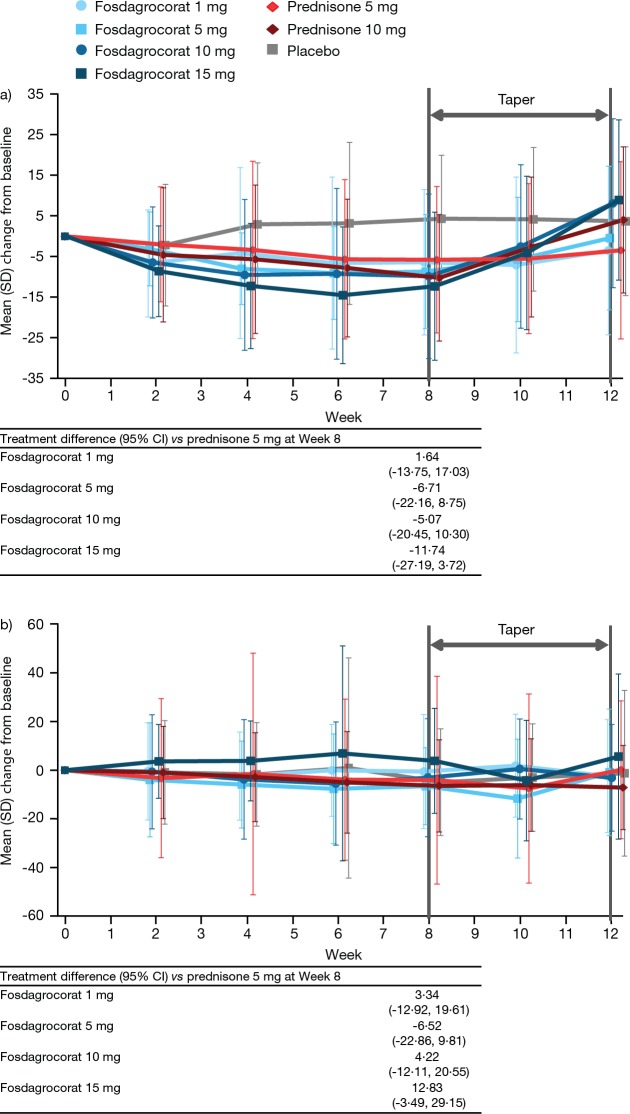
At week 8, all doses of fosdagrocorat inhibited P1NP versus placebo (figure 2A). Fosdagrocorat 1 mg, 5 mg and 10 mg met the criteria for non-inferiority to prednisone 5 mg at week 8.
Figure 2.
Mean change from baseline in (A) P1NP and (B)uNTx:uCr over time (active treatment and taper periods). All study treatments were administered once daily. All statistical values are derived from a repeated measures mixed model with fixed effects for treatment and visit, treatment-by-visit interaction and baseline value. P1NP, procollagen type 1 N-terminal telopeptide; uNTx:uCr, urinary N-terminal telopeptide to urinary creatinine ratio.
Week 8 uNTx:uCr levels increased with fosdagrocorat 1 mg, 10 mg and 15 mg versus placebo (figure 2B); fosdagrocorat 1 mg, 5 mg and 10 mg met the criteria for non-inferiority to prednisone 5 mg. The greatest increase occurred with fosdagrocorat 15 mg. A clear dose–response relationship was not observed; variability and presence of outliers made interpretations inconclusive. Mean changes from baseline in OC and CTx were consistent with the coprimary bone biomarkers (online supplementary table S3).
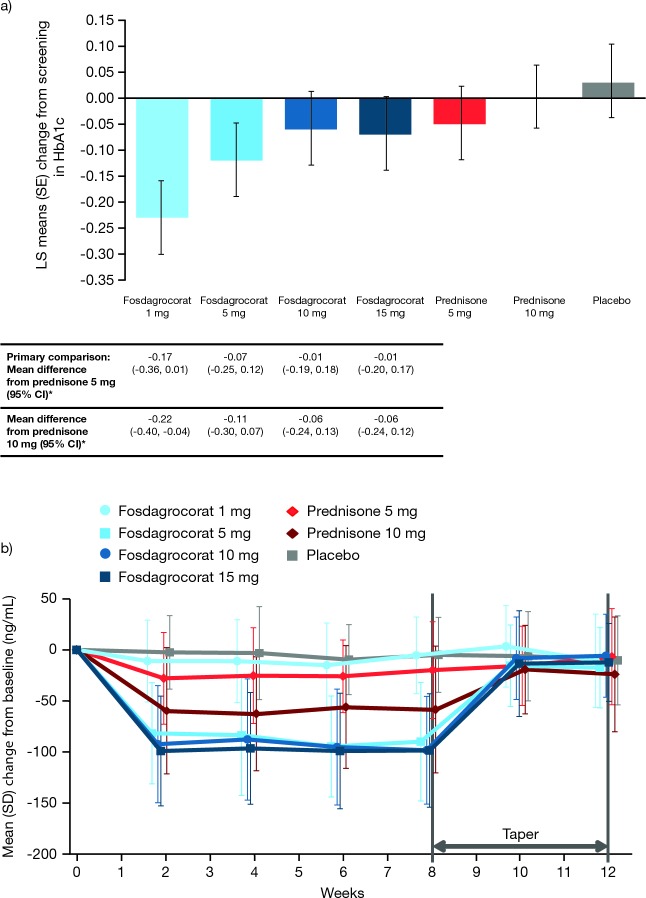
Safety
At week 8, fosdagrocorat reduced HbA1c from baseline in this predominantly non-diabetic population at low risk for glucose metabolism changes (figure 3A). All doses of fosdagrocorat reduced fasting plasma glucose levels (online supplementary figure S8). Fosdagrocorat 1 mg and 10 mg demonstrated numerically similar changes from baseline to week 8 in fasting plasma glucose levels. Fosdagrocorat 5 mg and 15 mg were numerically similar to prednisone 5 mg and 10 mg, respectively. Fasting plasma glucose returned to near baseline levels in all groups by week 12.
Figure 3.
(A) Change from screening in glucose metabolism biomarker HbA1c at week 8. (B) Change from baseline in cortisol over time (active treatment and taper periods). *Estimates are from an ANCOVA model with baseline as a covariate. All study treatments were administered once daily. ANCOVA, analysis of covariance; HbA1c, glycosylated haemoglobin; LS, least squares.
Rapid HPA axis suppression occurred with all active treatments except fosdagrocorat 1 mg (figure 3B). During taper, cortisol normalised to baseline levels in the fosdagrocorat groups versus prednisone 10 mg. All groups demonstrated prompt HPA axis recovery at week 13, although eight patients did not have normal ACTH stimulation test responses: fosdagrocorat 1 mg (n=2), 5 mg (n=1), 10 mg (n=2), 15 mg (n=2), prednisone 5 mg (n=1). Responses normalised within 2–4 weeks in all patients except two (prednisone 5 mg and fosdagrocorat 15 mg) who did not complete the follow-up ACTH stimulation test. No clinical symptoms of adrenal insufficiency were reported.
A summary of AEs and discontinuations is presented in table 2.
Table 2.
Summary of safety results
| Fosdagrocorat | Prednisone | Placebo | |||||
| 1 mg (n=45) |
5 mg (n=47) |
10 mg (n=45) |
15 mg (n=48) |
5 mg (n=45) |
10 mg (n=46) |
(n=47) | |
| TEAEs, n (%) | 20 (44.4) | 19 (40.4) | 22 (48.9) | 18 (37.5) | 16 (35.6) | 19 (41.3) | 17 (36.2) |
| Mild | 21 (46.7) | 20 (42.6) | 32 (71.1) | 18 (37.5) | 21 (46.7) | 30 (65.2) | 15 (31.9) |
| Moderate | 6 (13.3) | 7 (14.9) | 16 (35.6) | 14 (29.2) | 10 (22.2) | 14 (30.4) | 10 (21.3) |
| Severe | 0 | 3 (6.4) | 0 | 0 | 0 | 5 (10.9) | 3 (6.4) |
| Treatment-related, n (%) | 12 (26.7) | 8 (17.0) | 9 (20.0) | 7 (14.6) | 7 (15.6) | 10 (21.7) | 10 (21.3) |
| SAEs, n (%) | 0 | 1 (2.1) | 2 (4.4) | 2 (4.2) | 0 | 2 (4.3) | 2 (4.3) |
| Treatment-related, n (%) | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| AEs of special interest | 2* | 3† | 0 | 1‡ | 3§ | 1¶ | 2** |
| D/C | 3 (6.7) | 7 (14.9) | 1 (2.2) | 5 (10.4) | 1 (2.2) | 2 (4.3) | 8 (17.0) |
| D/C due to AEs, n (%) | 2 (4.4) | 4 (8.5) | 1 (2.2) | 2 (4.2) | 0 | 2 (4.3) | 3 (6.4) |
| Treatment-related, n (%) | 2 (4.4) | 4 (8.5) | 0 | 1 (2.1) | 0 | 1 (2.2) | 1 (2.1) |
All study treatments were administered once daily.
Six patients had dose reduction or were temporarily discontinued due to an AE (1 [2.2%] with fosdagrocorat 1 mg, 1 [2.1%] with fosdagrocorat 5 mg, 1 [2.2%] with fosdagrocorat 10 mg and 3 [6.4%] with placebo); three were considered treatment-related (1 [2.2%] with fosdagrocorat 1 mg and 2 [4.3%] with placebo).
*Fatigue (n=1) and neutropaenia (n=1): neutropaenia was mild to moderate and related to study drug; no action was taken with regard to study drug and both events resolved.
†Hypertension (n=3).
‡Hypertension (n=1): treatment-related leading to discontinuation after one dose of study drug.
§Insomnia (n=1) and hypertension (1 patient; 2 events).
¶Dyslipidaemia (n=1).
**Dyslipidaemia (n=1) and neutropaenia (n=1): neutropaenia was mild and related to study drug; no action was taken with regard to study drug and both events resolved.
AE, adverse event;D/C, discontinuation;n, number of patients;SAE, serious adverse event;TEAE, treatment-emergent adverse event.
In total, 27 (8.4%) patients discontinued; 9 (2.8%) due to treatment-related AEs. Overall, 63 (19.5%) patients experienced treatment-related AEs (TEAEs). Most TEAEs were mild (table 2); the most frequently reported were alanine aminotransferase elevations and nasopharyngitis (online supplementary table S4). Infection AEs were more frequently reported in the fosdagrocorat versus prednisone groups. Six cases of hypertension were considered of special interest; one led to treatment discontinuation (fosdagrocorat 15 mg). Eighteen patients were treated (with parenteral antibiotics) for significant infections; two were serious (placebo group). No trends or dose responses were observed in TEAEs, AEs of special interest, discontinuations due to AEs or treatment-related AEs with fosdagrocorat, but were with prednisone. No significant laboratory abnormalities (online supplementary figures S9 and S10) or changes in vital signs were observed. No deaths occurred during the study; one death (judged unrelated to study medication) was reported post-treatment (online supplementary section S4).
Discussion
Our results demonstrated that, in patients with RA receiving background MTX, fosdagrocorat 10 mg and 15 mg provided superior efficacy to placebo, by ACR20 and DAS28-4(CRP) responses, and fosdagrocorat 15 mg was non-inferior to prednisone 10 mg. Suppression of bone formation biomarkers with fosdagrocorat 1 mg, 5 mg and 10 mg met the criteria for non-inferiority to prednisone 5 mg once daily. Both P1NP and OC bone formation biomarkers showed a dose–response consistent with expected effects of low-dose GCs28 29 and with previous phase I fosdagrocorat bone biomarker analyses.15 16 Efficacy results were similar to an earlier phase II study, in which fosdagrocorat 10 mg and 25 mg once daily demonstrated numerically greater DAS improvements than prednisone.17 It should be noted that prednisone 10 mg appeared to have greater HAQ-DI improvements versus fosdagrocorat 15 mg; however, numbers are too small to exclude a type 2 error.
Prolonged GC use can increase the likelihood of developing glucose intolerance and diabetes.4 Glucose metabolism is mediated by transactivation13; therefore, we would expect fosdagrocorat to favourably affect glucose metabolism versus prednisone—in other words, a decrease in HbA1c or a diminished increase than would be expected with prednisone. Only a few patients with diabetes and impaired glucose tolerance were enrolled in this trial. Nonetheless, all fosdagrocorat doses reduced HbA1c levels from screening to week 8 versus no change with prednisone 10 mg and an increase with placebo. The fasting plasma glucose results demonstrated numerical similarity between fosdagrocorat and prednisone 5 mg, suggesting similar or marginally improved effects with fosdagrocorat versus prednisone, supporting expectations of the transrepression/transactivation theory.
Suppression of the HPA axis is a common, transrepression-mediated, adverse effect of GC therapy, particularly for doses >5 mg.30 31 Consistent with the underlying theory, and data from GC studies in patients with RA30 32 and phase I fosdagrocorat studies,15 16 fosdagrocorat 5 mg, 10 mg and 15 mg demonstrated substantial, rapid suppression of cortisol versus a partial reduction with prednisone 5 mg and 10 mg. Despite initial differences between fosdagrocorat and prednisone groups, all groups fully recovered HPA axis function after taper, and >95% of patients had normal ACTH stimulation test responses at week 13. HPA axis suppression risk is considered to be manageable long term, provided patients follow precautions (eg, carrying details of their medication).
Long-term use of prednisone >10 mg once daily is generally not acceptable for most patients with RA,3 but there is evidence that fosdagrocorat 10 mg or 25 mg per day may provide clinical efficacy17 without affecting OC, P1NP or HbA1c levels to the same extent as prednisone. The observed lack of a dose–response relationship for bone resorption biomarkers requires further investigation. Reported efficacy, bone metabolism, glucose metabolism and cortisol results support the underlying transactivation/transrepression hypothesis; observed efficacy is consistent with fosdagrocorat retaining desirable anti-inflammatory transrepression activity; observed HPA axis suppression suggests this effect is mediated by transrepression.13 Bone biomarker and glucose metabolism biomarker results support the theory that fosdagrocorat has reduced or impaired transactivation activities compared with prednisone.
Fosdagrocorat was generally well tolerated with an acceptable safety profile in this trial. It should be noted that this study was not powered to allow for inferences on statistical significance in terms of safety endpoints. Overall TEAE rates were similar across treatment groups and comparable with AE reports from a previous phase II trial.17 Fosdagrocorat was not associated with an AE dose–response, while prednisone was. No significant safety laboratory abnormalities or changes in vital signs were observed.
A potential limitation of this study includes enrolment of patients with a history of GC use. Although GCs were not permitted ≤6 weeks before screening, physiological effects of GC treatment can potentially persist up to 1 year following discontinuation.33 Of note, all patients had normal fasting morning cortisol levels and no signs of adrenal insufficiency at baseline. In addition, prior GC use had occurred in patients across all treatment groups, and other GC studies have used similar cut-off periods of ≤6 weeks.34–36 It may be useful for future studies to assess the efficacy and safety of fosdagrocorat in patients who are naïve to GC therapy. The 12-week duration may limit the evaluation of fosdagrocorat on bone and glucose metabolism; longer term trials will provide clarification of this. Patients in this trial also had active disease and high systemic inflammation at baseline, and were predominantly non-diabetic—factors that could limit the evaluation of bone and glucose effects. It is important to note that the simplification of transrepression versus transactivation theory has been a controversial topic37; nevertheless, our results generally support that increasing transrepression while decreasing transactivation with DAGRs could increase or maintain efficacy while reducing AEs, compared with traditional GC therapy.
Fosdagrocorat 10 mg and 15 mg had similar efficacy to prednisone 10 mg and similar safety profiles to prednisone 5 mg. Some of the results presented here—especially those regarding glucose metabolism, bone resorption and overall benefit to risk ratio—indicate that a larger trial of longer duration (>1 year) in other populations of patients with RA populations, such as GC-naïve patients, is warranted.
Acknowledgments
This study was sponsored by Pfizer Inc. Employees of the sponsor were involved in study conception, design and conduct, and in data collection and analysis. Medical writing support under the guidance of the authors was provided by Amanda Pedder, MSc, at CMC Connect, a division of Complete Medical Communications, Macclesfield, UK, and was funded by Pfizer, New York, New York, USA, in accordance with Good Publication Practice (GPP3) guidelines (Ann Intern Med 2015;163:461–4). The authors would like to thank Sheela Kolluri of Pfizer Inc and Paul Healey, formerly of Pfizer Inc, for their contribution to this study.
Footnotes
Contributors: All authors fulfil all criteria for authorship.
Funding: This study was sponsored by Pfizer Inc.
Competing interests: FB has received consultancy fees, honoraria and travel expenses from Pfizer Inc. VS is a consultant for Pfizer Inc. EBL has acted as a consultant for Pfizer Inc. BT, RR, AG and JH-H are employees of Pfizer Inc. DM was an employee of Pfizer Inc at the time the trial was conducted.
Patient consent for publication: Not required.
Ethics approval: Conduct was in accordance with applicable legal and regulatory requirements, the International Ethical Guidelines for Biomedical Research Involving Human Subjects, the International Conference on Harmonisation Guidelines for Good Clinical Practice, and the Declaration of Helsinki. The institutional review boards or independent ethics committees at each investigational centre approved the study. All patients provided written, informed consent.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: All data relevant to the study are included in the article or uploaded as online supplementary information.
References
- 1.Caplan L, Wolfe F, Russell AS, et al. Corticosteroid use in rheumatoid arthritis: prevalence, predictors, correlates, and outcomes. J Rheumatol 2007;34:696–705. [PubMed] [Google Scholar]
- 2.Criswell LA, Saag KG, Sems KM, et al. Moderate-term, low-dose corticosteroids for rheumatoid arthritis. Cochrane Database Syst Rev 2000;2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gaujoux-Viala C, Nam J, Ramiro S, et al. Efficacy of conventional synthetic disease-modifying antirheumatic drugs, glucocorticoids and tofacitinib: a systematic literature review informing the 2013 update of the EULAR recommendations for management of rheumatoid arthritis. Ann Rheum Dis 2014;73:510–5. 10.1136/annrheumdis-2013-204588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Da Silva JAP, Jacobs JWG, Kirwan JR, et al. Safety of low dose glucocorticoid treatment in rheumatoid arthritis: published evidence and prospective trial data. Ann Rheum Dis 2006;65:285–93. 10.1136/ard.2005.038638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fardet L, Flahault A, Kettaneh A, et al. Corticosteroid-induced clinical adverse events: frequency, risk factors and patient's opinion. Br J Dermatol 2007;157:142–8. 10.1111/j.1365-2133.2007.07950.x [DOI] [PubMed] [Google Scholar]
- 6.Ethgen O, de Lemos Esteves F, Bruyere O, et al. What do we know about the safety of corticosteroids in rheumatoid arthritis? Curr Med Res Opin 2013;29:1147–60. 10.1185/03007995.2013.818531 [DOI] [PubMed] [Google Scholar]
- 7.Ferreira JF, Ahmed Mohamed AA, Emery P. Glucocorticoids and rheumatoid arthritis. Rheum Dis Clin North Am 2016;42:33–46. 10.1016/j.rdc.2015.08.006 [DOI] [PubMed] [Google Scholar]
- 8.Listing J, Kekow J, Manger B, et al. Mortality in rheumatoid arthritis: the impact of disease activity, treatment with glucocorticoids, TNFα inhibitors and rituximab. Ann Rheum Dis 2015;74:415–21. 10.1136/annrheumdis-2013-204021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Duru N, van der Goes MC, Jacobs JWG, et al. EULAR evidence-based and consensus-based recommendations on the management of medium to high-dose glucocorticoid therapy in rheumatic diseases. Ann Rheum Dis 2013;72:1905–13. 10.1136/annrheumdis-2013-203249 [DOI] [PubMed] [Google Scholar]
- 10.Strehl C, Bijlsma JWJ, de Wit M, et al. Defining conditions where long-term glucocorticoid treatment has an acceptably low level of harm to facilitate implementation of existing recommendations: viewpoints from an EULAR Task Force. Ann Rheum Dis 2016;75:952–7. 10.1136/annrheumdis-2015-208916 [DOI] [PubMed] [Google Scholar]
- 11.Palmowski Y, Buttgereit T, Dejaco C, et al. "Official View" on Glucocorticoids in Rheumatoid Arthritis: A Systematic Review of International Guidelines and Consensus Statements. Arthritis Care Res 2017;69:1134–41. 10.1002/acr.23185 [DOI] [PubMed] [Google Scholar]
- 12.van der Goes MC, Jacobs JWG, Boers M, et al. Monitoring adverse events of low-dose glucocorticoid therapy: EULAR recommendations for clinical trials and daily practice. Ann Rheum Dis 2010;69:1913–9. 10.1136/ard.2009.124958 [DOI] [PubMed] [Google Scholar]
- 13.Buttgereit F, Burmester G, Lipworth B. Optimised glucocorticoid therapy: the sharpening of an old spear. The Lancet 2005;365:801–3. 10.1016/S0140-6736(05)71005-9 [DOI] [PubMed] [Google Scholar]
- 14.Sedwick C. Wanted: a new model for glucocorticoid receptor transactivation and transrepression. PLoS Biol 2014;12:e1001814 10.1371/journal.pbio.1001814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stock T, Fleishaker D, Mukherjee A, et al. Evaluation of the safety, pharmacokinetics (PK), and pharmacodynamics (PD) of a dissociated agonist of the glucocorticoid receptor (DAGR), in healthy volunteers. Ann Rheum Dis 2010;69(Suppl. 3). [Google Scholar]
- 16.Stock T, Fleishaker D, Mukherjee A, et al. Evaluation of safety, pharmacokinetics and pharmacodynamics of a selective glucocorticoid receptor modulator (SGRM) in healthy volunteers. Arthritis Rheum 2009;60(Suppl.10). [Google Scholar]
- 17.Stock T, Fleishaker D, Wang X, et al. Phase 2 evaluation of PF-04171327, a dissociated agonist of the glucocorticoid receptor, for the treatment of rheumatoid arthritis in patients with an inadequate response to methotrexate. Arthritis Rheum 2013;65(Suppl.10). [Google Scholar]
- 18.Buttgereit F, Burmester GR, Straub RH, et al. Exogenous and endogenous glucocorticoids in rheumatic diseases. Arthritis Rheum 2011;63:1–9. 10.1002/art.30070 [DOI] [PubMed] [Google Scholar]
- 19.Strehl C, Buttgereit F. Optimized glucocorticoid therapy: teaching old drugs new tricks. Mol Cell Endocrinol 2013;380:32–40. 10.1016/j.mce.2013.01.026 [DOI] [PubMed] [Google Scholar]
- 20.Harcken C, Riether D, Kuzmich D, et al. Identification of highly efficacious glucocorticoid receptor agonists with a potential for reduced clinical bone side effects. J Med Chem 2014;57:1583–98. 10.1021/jm4019178 [DOI] [PubMed] [Google Scholar]
- 21.Baiula M, Bedini A, Baldi J, et al. Mapracorat, a selective glucocorticoid receptor agonist, causes apoptosis of eosinophils infiltrating the conjunctiva in late-phase experimental ocular allergy. Drug Des Devel Ther 2014;8:745–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Klopot A, Baida G, Bhalla P, et al. Selective activator of the glucocorticoid receptor Compound A dissociates therapeutic and atrophogenic effects of glucocorticoid receptor signaling in skin. J Cancer Prev 2015;20:250–9. 10.15430/JCP.2015.20.4.250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fries JF, Spitz PW, Young DY. The dimensions of health outcomes: the health assessment questionnaire, disability and pain scales. J Rheumatol 1982;9:789–93. [PubMed] [Google Scholar]
- 24.Hochberg MC, Chang RW, Dwosh I, et al. The American College of rheumatology 1991 revised criteria for the classification of global functional status in rheumatoid arthritis. Arthritis Rheum 1992;35:498–502. 10.1002/art.1780350502 [DOI] [PubMed] [Google Scholar]
- 25.Ware JE, Kosinski M, Dewey JE. How to score version two of the SF-36 health survey. QualityMetric Incorporated: Lincoln, RI, 2000. [Google Scholar]
- 26.Thomas N, Roy D. Analysis of clinical dose–response in small-molecule drug development: 2009–2014. Stat Biopharm Res 2017;9:137–46. 10.1080/19466315.2016.1256229 [DOI] [Google Scholar]
- 27.Thomas N, Sweeney K, Somayaji V. Meta-analysis of clinical dose–response in a large drug development Portfolio. Stat Biopharm Res 2014;6:302–17. 10.1080/19466315.2014.924876 [DOI] [Google Scholar]
- 28.Lems WF, Van Veen GJ, Gerrits MI, et al. Effect of low-dose prednisone (with calcium and calcitriol supplementation) on calcium and bone metabolism in healthy volunteers. Br J Rheumatol 1998;37:27–33. 10.1093/rheumatology/37.1.27 [DOI] [PubMed] [Google Scholar]
- 29.Engvall I-L, Svensson B, Tengstrand B, et al. Impact of low-dose prednisolone on bone synthesis and resorption in early rheumatoid arthritis - experiences from a two-year randomized study. Arthritis Res Ther 2008;10 10.1186/ar2542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.LaRochelle GE Jr, LaRochelle AG, Ratner RE, et al. Recovery of the hypothalamic-pituitary-adrenal (HPA) axis in patients with rheumatic diseases receiving low-dose prednisone. Am J Med 1993;95:258–64. 10.1016/0002-9343(93)90277-V [DOI] [PubMed] [Google Scholar]
- 31.Alten R, Wiebe E. Hypothalamic-pituitary-adrenal axis function in patients with rheumatoid arthritis treated with different glucocorticoid approaches. Neuroimmunomodulation 2015;22:83–8. 10.1159/000362731 [DOI] [PubMed] [Google Scholar]
- 32.Henzen C, Suter A, Lerch E, et al. Suppression and recovery of adrenal response after short-term, high-dose glucocorticoid treatment. The Lancet 2000;355:542–5. 10.1016/S0140-6736(99)06290-X [DOI] [PubMed] [Google Scholar]
- 33.Livanou T, Ferriman D, James VHT. Recovery of hypothalamo-pituitary-adrenal function after corticosteroid therapy. The Lancet 1967;290:856–9. 10.1016/S0140-6736(67)92592-5 [DOI] [PubMed] [Google Scholar]
- 34.Buttgereit F, Mehta D, Kirwan J, et al. Low-dose prednisone chronotherapy for rheumatoid arthritis: a randomised clinical trial (CAPRA-2). Ann Rheum Dis 2013;72:204–10. 10.1136/annrheumdis-2011-201067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Verschueren P, De Cock D, Corluy L, et al. Patients lacking classical poor prognostic markers might also benefit from a step-down glucocorticoid bridging scheme in early rheumatoid arthritis: week 16 results from the randomized multicenter CareRA trial. Arthritis Res Ther 2015;17 10.1186/s13075-015-0611-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nam JL, Villeneuve E, Hensor EMA, et al. Remission induction comparing infliximab and high-dose intravenous steroid, followed by treat-to-target: a double-blind, randomised, controlled trial in new-onset, treatment-naive, rheumatoid arthritis (the IDEA study). Ann Rheum Dis 2014;73:75–85. 10.1136/annrheumdis-2013-203440 [DOI] [PubMed] [Google Scholar]
- 37.Strehl C, van der Goes MC, Bijlsma JWJ, et al. Glucocorticoid-targeted therapies for the treatment of rheumatoid arthritis. Expert Opin Investig Drugs 2017;26:187–95. 10.1080/13543784.2017.1276562 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
rmdopen-2018-000889supp001.docx (3.6MB, docx)