Abstract
Objective:
Unexplained medical terminology impedes clinician/parent communication. We describe jargon use in a pediatric surgical setting.
Methods:
We evaluated encounters between parents of children with sleep-disordered breathing (SDB; n=64) and otolaryngologists (n=8). Participants completed questionnaires evaluating demographics, clinical features, and parental role in decision-making via a 4-point categorical item. Two coders reviewed consultations for occurrence of clinician and parent utterance of medical jargon. Descriptive statistics established a profile of jargon use, and logistic regression evaluated associations between communication factors with jargon use.
Results:
Unexplained medical jargon was common (mean total utterances per visit=28.9,SD=19.5,Range=5–100), including SDB-specific jargon (M=8.3,SD=8.8), other medical terminology (M=13.9,SD=12) and contextual terms (M=3.8,SD=4). Parents used jargon a mean of 4.3 times (SD=4.6). Clinicians used more jargon in consults where they perceived parents as having greater involvement in decision-making (OR=3.4,p<0.05) and when parents used more jargon (OR=1.2,p<0.05).
Conclusions:
Jargon use in pediatric surgical consultations is common and could serve as a barrier to informed or shared parent decision-making. This study provides a foundation for further research into patterns of jargon use across surgical populations.
Practice Implications:
Results will be integrated into communication training to enhance clinician communication, foster self-awareness in language use, and create strategies to evaluate parental understanding.
Keywords: jargon, communication, physician/patient relationship, decision-making, pediatrics, otolaryngology, tonsillectomy
1. Introduction
Effective communication between clinicians and parents is essential for provision of quality pediatric healthcare. The manner in which clinicians use language, including medical jargon with which parents may be unfamiliar, has significant impact on parental understanding and, consequently, decision-making regarding treatment. Elective surgery in children poses a unique scenario for parental decision-making: often there is clinical equipoise, or uncertainty as to whether or not surgical intervention results in superior outcomes compared to observation without surgery.[1] Clear communication may improve parental knowledge and decision quality concerning surgical intervention.
Tonsillectomy is the most common major pediatric surgical procedure in the United States, with more than 600,000 cases performed each year. [2, 3] These surgeries are frequently performed by pediatric otolaryngologists, who are surgeons treating disorders related to the ear, nose, throat, and related structures of the head and neck.[4] Tonsillectomy is the primary treatment for obstructive sleep-disordered breathing (SDB), a spectrum of sleep-related breathing conditions ranging from snoring to obstructive sleep apnea.[2, 5] Although tonsillectomy is an effective treatment for sleep-disordered breathing, it comes with notable risks, including postoperative pain, hemorrhage, and respiratory risks related to anesthesia.[6, 7] A multi-institutional randomized-controlled Childhood Adenotonsillectomy Trial (CHAT) showed that one third to one half of children with mild-moderate sleep apnea had resolution of symptoms without surgical intervention when assessed 7 months following baseline.[8, 9] As such, there is clinical equipoise as to treatment alternatives for surgery or observation, and parents harbor decision conflict for this surgery due to the lack of a definitive treatment recommendation.[10] Clear communication may improve parental knowledge and enable truly informed decision-making for all medical interventions.
Jargon use has not been extensively evaluated in research and to our knowledge has not been studied in pediatric otolaryngology. This oversight is a significant shortcoming, as extensive use of medical jargon has the potential to create meaningful barriers to conversation. Patients who are not fluent in the English language often suffer communication barriers and poorer quality of healthcare.[11] Similarly, jargon use has the potential to confound parents not proficient in the language of medical terminology. Parents may experience a language barrier when addressed with a multitude of words they do not comprehend.[12–14] As such, it is important to consider the presence and impact of medical jargon in the clinical context. Although not broadly studied, presence of jargon in the clinical context has been evaluated in adult populations to a limited extent, including jargon relating to chief complaint,[12, 15] complex medical terminology,[16–19] use of statistics,[20] contextual jargon (lay terms with specific meaning in the clinical context),[19] and provision of explanations.[17, 18, 21, 22] All play a role in creating communication barriers between clinicians and families. For example, a randomized crossover trial found that adult patients with chronic illnesses had better understanding of their conditions when medical terminology was translated in clinical correspondence.[22] Similarly, studies evaluating parents of children with diabetes and chronic illnesses indicated that parents may misunderstand and resent medical jargon, and endorsed clearer language and communication techniques to allow for parent understanding.[23] [21] Additionally, clinician use of jargon created barriers for the clinician/parent relationship, when parents considered use of language they could not comprehend as an avoidance of direct conversation.[21] Jargon use persists despite findings in research showing evidence of parents’ negative and emotional reactions to clinician jargon,[12, 24] parental lack of understanding of complex language,[20–23, 25, 26] and parental difficulty recalling and understanding complex medical dialogue.[27] [16–19, 24, 25] [13, 28–30] A greater understanding of the factors associated with surgeon jargon use might facilitate better parent-clinician communication[31] and optimize surgical decision-making. This study seeks to describe the extent of medical jargon used by a sample of pediatric otolaryngologists when speaking to parents. We aim to foster a greater understanding of the factors associated with surgeon use of jargon to facilitate a movement towards improved parent-clinician communication and optimize shared decision-making.
2. Methods
Johns Hopkins School of Medicine Institutional Review Board approved all study procedures (IRB:54662).
2.1. Data Collection.
Parents were eligible for participation if their child was between the ages of 2–17, undergoing first evaluation for sleep-disordered breathing, and had not previously undergone surgery. Patients were identified via clinic scheduling records and parents were subsequently contacted by telephone. Parents and clinicians completed informed consent for the study prior to their appointment.
Consults between otolaryngologists and parents were audio-recorded and transcribed. Parents and clinicians completed questionnaires evaluating demographic characteristics (education, insurance) and extent of parental involvement in decision-making, via a previously used 4-point scale ranging from low involvement (“clinician made all decisions”) to high involvement (“parent made all decisions”).[32, 33] Clinicians completed the Ottawa Treatment Opinion Scale, which asked clinicians to rate their treatment opinion for or against surgery on a 10-point scale.[34] Greater ratings suggested use of tonsillectomy, and ratings 4–6 indicated equipoise. As the majority of children examined were below the age of assent and too young to engage in medical dialogue [n=51 (80%)≤7 years; M=5.8, SD=2.5], only parental communication and outcomes were measured. Data was collected as part of a larger parent study on outcomes of communication and decision-making with parents of children undergoing tonsillectomy evaluation.[35]
2.2. Identification of jargon.
Transcripts were comprehensively reviewed prior to coding, and a scheme of jargon classification was developed based on previous research which incorporated both contextual and medical jargon into communication evaluations,[19] and results from the collected transcripts (Figure 1). Researchers developed a detailed dictionary containing every identified jargon term, classified via the coding scheme. As researchers reviewed transcripts, new terms were discussed and added to the dictionary. Two independent coders coded, categorized, and quantified jargon per the developed scheme and dictionary.
Figure 1:
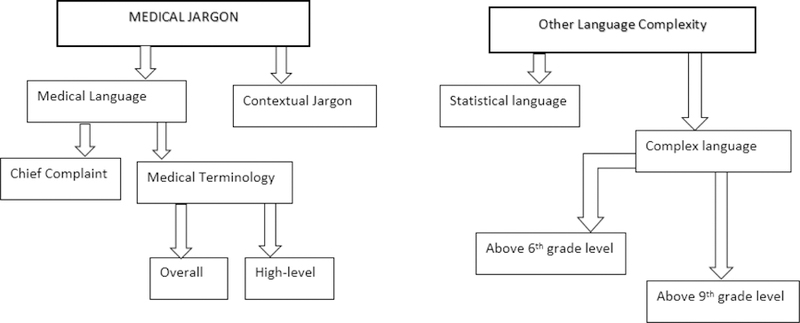
Coding scheme for clinician use of jargon
Definitions.
Our main focus was use of medical jargon, which was classified into three categories: jargon related to the chief complaint (SDB), other complex medical jargon, and contextual jargon. “Other complex jargon” (turbinate) is considered synonymous with the phrase “medical terminology.” We also evaluated complex language (advanced vocabulary) and 3 additional aspects of language use: statistical language, clinician provision of explanations with jargon terms, and parent jargon use (Table 1). If a parent introduced a jargon term without solicitation, the term was not considered to be “unexplained jargon” for the duration of the consult, and therefore not coded. If a medical term was explained by a clinician (“carbon dioxide, the gas we breathe out”), it was not considered to be jargon. When considering the 15 consults that included multiple caregivers, all parental utterances were accounted for.
Table 1:
Definitions of jargon categorization
| Category | Definition | Examples |
|---|---|---|
| Medical Jargon, chief- complaint | Jargon relating to chief complaint | tonsils, tonsillectomy, sleep apnea |
| Medical Terminology | ||
| Jargon relating to medical terms other than SDB/AT | High level: IGG subclass, laryngomalacia, medial meniscus | |
| Low level: steroid spray, carbon dioxide | ||
| Explained jargon | Jargon terms explained by clinician | “carbon dioxide, which is the gas we breath out” |
| “CPAP, which is a breathing machine at nighttime” | ||
| Contextual Jargon | Laymen terms which take on a different meaning in the clinical context | significant, candidate, quality of life |
| Complex language1 | Words that may be outside of the vocabulary of a lower- literate parent | Intermediate: prone, symmetric labile |
| Advanced: cusp, copious, caveat | ||
| Statistical language | Use of statistical results | “Getting tonsils and adenoids out will cure 80%” |
| “risk of post-op bleeding, in 2–5% of kids” | ||
Intermediate complex language was defined as words > 6th grade vocabulary. It was determined subjectively by two independent coders and confirmed via the GSL/AWL (General Service List/Academic Word List). Advanced (high-level) complex language was defined as words > 9th grade comprehension. These terms were classified as advanced vocabulary if they were > 7th level of the BNC- COCA (British National Corpus and Corpus of Contemporary American English) word frequency list.
Medical jargon.
Medical jargon was defined as any medical terminology which may be unfamiliar to persons without clinical experience, including:
Chief complaint jargon, defined as any term identifying sleep-disordered breathing or tonsils,
Medical terminology, medical terms which did not fall under the definition of “chief complaint” (e.g. thalassemia).
Contextual jargon, layman terms which took on specific meanings in the clinical context (e.g. episode).
We also identified higher-level medical terminology, which included clinician-introduced terms considered to be more advanced (“IGG subclass”), and excluded more simple terms (“congested”) or medication labels (“Albuterol”). Higher-level terminology applied exclusively to clinician dialogue.
Complex language represented advanced vocabulary outside of the typical comprehension of either <6th grade education (intermediate) or < 9th grade education (advanced). These grade levels were determined by health literacy recommendations and previous research determining average reading comprehension.[36, 37] Complex words were identified by two independent coders and compared to vocabulary frequency corpuses (Advanced: 7th level BNC-COCA; Intermediate: GSL/AWL) to ensure they were not frequently used in the English language.[38, 39], [40, 41] Based on previous research, complex terms were classified as “intermediate” or “advanced” based on where they fell on the BNC-COCA frequency corpus (Advanced:> level 7).[38]
Statistical language was defined as clinician presentation of any statistical information (“2–5% risk”). Statistical discourse was included as an element of language complexity because it relies on mathematical terminology and understanding. This represents a language barrier synonymous to that experienced with medical terminology, when information is not provided in a manner parents can understand. In previous research, adult patients have indicated a lack of understanding when provided with disease risk-based statistics during medical encounters.[20] Provision of explanations included any explanation following a jargon term, from minimal (“adenoids, block the nose”) to detailed (“the adenoids...the same type of tissue as the tonsils, located up in the back of the nose”). Although the isolated category of jargon with explanations is evaluated less frequently than overall jargon use, previous research has shown that once jargon terms are explained, patient understanding increases.[22] As such, once a jargon term was defined, it was no longer considered to be “unexplained jargon,” and therefore further instances were not coded. Statistical language and provision of explanations were coded exclusively for clinician dialogue.
Coding.
Two coders (AL, CW) independently and systematically reviewed transcribed consults for each identified jargon and complex language classification. Each transcript was coded identically; researchers made no assumptions about parents’ understanding of medical jargon based on socioeconomic elements. All unexplained jargon terms were coded qualitatively and confirmed by both coders and 3 clinical researchers. Coders met regularly to confirm agreement and resolve disputes. Prior to analysis, a team of 5 researchers (3 clinical, 2 non-clinical) met to reach final consensus on the jargon dictionary and all coded terms. Final coding was completed via the MaxDictio qualitative software,[19, 42] which allowed coders to 1) systematically build the jargon dictionary, 2) create categorical coding schemes for each jargon classification, 3) quantify jargon use, and 4) identify questionable jargon terms for discussion. Quantitative analysis was conducted via Stata Statistical Software.[43]
2.3. Quantitative analysis of jargon use.
To determine the extent of jargon use, we obtained descriptive statistics for the extent to which jargon was used overall, and between clinicians. Kruskal-Wallis tests evaluated variation between clinicians. Extent of jargon use reflected the number of jargon terms uttered per consult. Medical terminology phrases (cardiac hypertension) were coded as single utterances of jargon.
Extent of jargon use.
Primary analysis centered on descriptive statistics of the overall extent of medical jargon use. Descriptive statistics present enumeration of the number of jargon terms uttered by clinicians or parents, regardless of consult length. Means, standard deviations, medians, and ranges for medical jargon overall, and within each classification were obtained. Because “tonsils” may be familiar to parents with prior experience, we obtained descriptions of overall medical jargon use including and excluding chief complaint jargon.
We also obtained descriptive summaries for other aspects contributing to complexity of clinicians’ dialogue. This included provision of explanations, complex language, and use of statistics. Clinician presentation of statistics was included due to applicability to complex mathematical language, and previous research illustrating patients’ lack of comprehension of statistical dialogue.[20]
Associations with parent behavior.
We evaluated the extent to which parental characteristics (insurance) and behavior (perceived involvement in decision-making) predicted degree to which clinicians used jargon during encounters. Distribution of jargon use fit neither a normal nor Poisson distribution. Ordered logistic regression was performed using an ordinal classification of jargon, to approximate a normal distribution.[44] Logistic regression accounted for possible confounding factors (identity of clinician, parent education, patient insurance) and evaluated prediction of parent involvement (parent use of jargon and decision-making role). Patients had low decision complexity if they had no sleep apnea, or had severe sleep apnea.
3. Results
3.1. Participant characteristics
Participants consisted of 64 parents of children with sleep-disordered breathing or enlarged tonsils and 8 surgical otolaryngologists. Of the 149 eligible families who were approached for participation, 64 (43%) agreed to participate. All 8 otolaryngologists approached agreed to participate. Clinician participants consisted of 4 pediatric otolaryngologists, 2 pediatric otolaryngology fellows, 1 pediatric otolaryngology nurse practitioner, and 1 general otolaryngologist (Table 2). Consults were conducted at 3 outpatient clinical sites affiliated with the medical institution (Primary Campus Urban-based Outpatient Center, n=35; Suburban Offsite Pediatric Otolaryngology clinic, n=18, Community Medical Center, n=11). The majority of parent participants were mothers (59/64, 91%) and had public insurance (39/64, 61%). A small proportion (14/64; 23%) had low annual income (<20,000) and had not attended college (15/64, 24%). Race of parents was largely white (39/64, 62%) and African-American (25/64, 39%). While 10 (16%) had elected to consult with otolaryngologists on their own, 54 (84%) were referred to the clinics by their pediatrician. Clinicians reported equipoise in 11 (18%) consults, but leaned towards tonsillectomy in 35 (58%), and watchful waiting in 14 (23%).
Table 2:
Clinician characteristics (N = 8)
| Characteristic | Clinician, N = 8 [n (%)] |
|---|---|
| Age [M (SD)] | 42.9 (9.2) |
| Race/Ethnicity | |
| White | 7 (87.5) |
| African-American | -- |
| Asian/Japanese-American | 1 (12.5) |
| Hispanic/Latino | -- |
| Gender | |
| Female | 3 (37.5) |
| Clinical specialty | |
| Pediatric otolaryngologist | 4 (50) |
| Otolaryngologist | 1 (12.5) |
| Otolaryngology fellow | 2 (25) |
| Otolaryngology nurse practitioner | 1 (12.5) |
| Years of experience in practice | |
| < 5 years | 3 (37.5) |
| 5–10 years | 2 (25) |
| 10–20 years | 2 (25) |
| >20 years | 1 (12.5) |
| Percent of pediatric patients in practice | |
| < 25% | -- |
| 25–50% | 1 (12.5) |
| 50–75% | -- |
| <75% | 7 (87.5) |
| Percent of pediatric SDB patients in practice | |
| < 25% | 1 (12.5) |
| 25–50% | 5 (62.5) |
| 50–75% | 2 (25) |
| >75% | -- |
3.2. Use of jargon and complex language
Medical jargon.
Preliminary inter-rater agreement for jargon occurrence was 74.3%, and final consensus of coded jargon met 100% agreement. Medical jargon was used consistently and varied by clinician (Figure 2), as Kruskal-Wallis tests for all medical jargon (ꭓ=13.9, p=.016), and jargon excluding chief complaint (ꭓ=16.2, p=.006) confirmed. The clinician with greatest jargon use uttered a mean of 40.2 (SD=26.7) terms per consult; the clinician with lowest use uttered 17.9 (SD=10.1).
Figure 2: Use of medical jargon: Between-clinician variation.
Overall medical jargon use, and jargon use by category
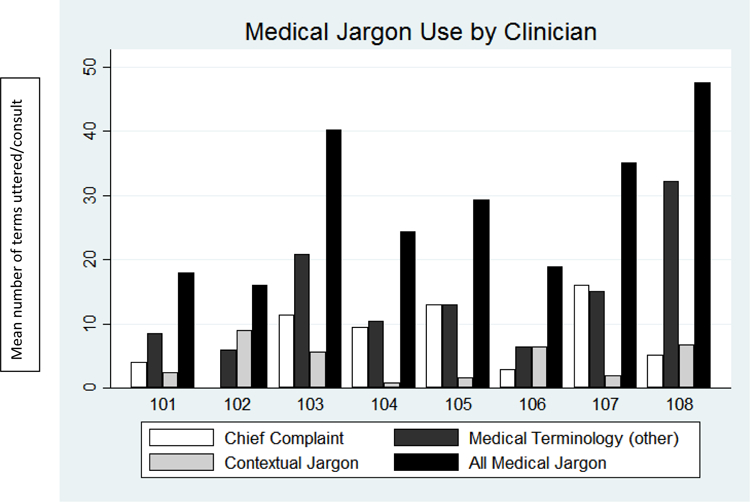
Numbers 101 – 108 represent de-identified consulting clinicians.
Overall, clinicians uttered a mean of 28.9 medical jargon terms per consult (SD=19.5, Med=25.5, R=5–100), or 17.6 (SD=14.5, Med=13, R=1–72) excluding chief complaint. Chief complaint jargon (apnea, tonsils) accounted for a mean of 8.3 terms per consult (SD=8.8, Med=6, R=0–38), medical terminology (thalassemia) accounted for 13.9(SD=12, Med=10, R=1–56), and contextual jargon (episode) accounted for 3.75 (SD=4, Med=2, R=0–16). 55 (85.9%) clinicians explained at least one medical jargon term, offering a mean of 2.9 explanations per consult (SD=2.3). Higher-level medical terminology (IGG subclass, ciliary) were identified less often (M=5.1, SD=5.1, R=0–26) than less complex terms (e.g., steroid; M=8.8, SD=8.4, R=0–42).
Complex language.
Intermediate complex language (> 6th grade level) (hospitalize, elevate) was used consistently, with a mean of 5.1 (SD=5) per consult. Advanced complex language (cusp, caveat) was used sparingly (M=0.4, SD=.8); clinicians did not use any advanced terms during 46 encounters (71.9%). Clinicians introduced statistics at least once in 34 (53.1%) of the 64 consults (“a 2–5% risk of bleeding”), and used statistics multiple times when discussing treatment in 15 consults (23.4%). Cumulative use of statistics did not significantly vary by clinicians (χ = 6.6, p = .08).
Parent use of jargon.
A minority of parents (n=13; 20.3%) introduced one jargon term during consultation with clinician, and 30 (46.8%) introduced at least two terms (e.g., tonsils, Albuterol). Parents introduced a mean of 2.4 (SD=2.8) terms per consult, and repeated terms clinicians had introduced 1.8 (SD=2.5) times. Overall use was infrequent: Across 64 consults, parents uttered a total of 250 terms, as compared to 1,912 clinician frequency.
3.3. Associations with clinician use of medical jargon
Parent involvement.
Clinician participants mainly believed that parents either wanted them to make most treatment decisions (n=23 consults, 37.7%), or share decision-making (n=31, 51.8%). Clinicians believed parents desired them to make all decisions in 6 consults (9.8%). Clinicians believed parents wished to make all decisions in only 1 consult (1.6%).
Associations with clinician jargon use.
Ordered logistic regression of medical jargon revealed that clinicians were more likely to use jargon when they perceived parents as having greater involvement in final decision-making (OR=3.5, p=.019) and when parents used more jargon (OR=1.2, p=.023). Full regression results predicting use of jargon categories (e.g., medical terminology, contextual jargon) are presented in Table 4.
Table 4:
Predictors of clinician use of medical jargon: Results from ordered logistic regressions
| Predictor | All jargon (OR, p-value) | Without SDB/AT (OR, p-value) | Medical terms (OR, p-value) | Contextual (OR, p-value) |
|---|---|---|---|---|
| Parent College-Educated | 1.2, p = .8 | 1.1, p = .8 | 1.1, p = .8 | .4, p = .14 |
| Child Public Insurance | .67, p = .43 | .56, p = .26 | .65, p = .4 | .89, p = .8 |
| Parent Jargon Use | 1.2, p = .023 | 1.1, p = .046 | 1.2, p = .01 | 1.2, p = .008 |
| Parent Involvement | 3.5, p = .019 | 1.3, p = .5 | 1.7, p = .2 | 3.4, p = .023 |
Parental involvement refers to the extent to which parents were involved in decision-making, dichotomized as greater involvement (parent as equal partner or parent as sole decision-maker) or lesser involvement (little to no involvement in final decision making)
4. Discussion and Conclusions
This study is the first to describe common use of jargon and complex language in a pediatric otolaryngology or surgical setting. Our results reflect those of prior studies emphasizing jargon in other adult medical fields, including osteoarthritic[45], rheumatologic,[45, 46] diabetic,[16, 25] gynecologic,[26] and oncologic[17, 20] clinical settings. Similar to previous research, chief complaint jargon and other medical terminology are used across consults in pediatric otolaryngology, regardless of parental characteristics.[17, 18] Clinicians used more jargon when they believed that parents were more involved in decision-making. This finding presents implications for parental understanding and satisfaction, particularly as clinicians have been shown to overestimate parents’ ability to recall medical terminology.[47]
4.1. Discussion
Previous studies have consistently demonstrated the adverse effects of clinicians using jargon with parents. These effects include parental or patient difficulty comprehending the information relayed,[12, 23] patients perceiving clinicians as avoidant,[12, 21] and patients feeling excluded from care decisions.[48] For example, in one study, in regards to clinician explanation of pulmonary nodules, adult patients articulated negative effects of jargon use on their comprehension (“Don’t hide nothing...tell me the truth, tell me in my language, so I understand what you’re saying”).[12] In another study, lower-literate parents undergoing diabetes education were confused by jargon, desired simple language, and often used terms incorrectly, indicating a lack of comprehension.[23] In a pediatric study, parents perceived pediatricians’ use of medical jargon as avoidance of directly providing parents with information, when clinicians used more complicated language that parents may be unable to question directly. They also indicated that use of more simple language would increase their understanding (“Often the parents have to guess what they mean. They often avoid the answer...by using very specialist words”).[21] Parents considered jargon use as intentional use of incomprehensible language in order to avoid discussing difficult information,[21] or addressing the patient’s concerns.[12] Not only do parents have negative reactions to jargon, many demonstrate lack of comprehension of clinician language.[21, 23, 45] Furthermore, when multiple clinicians examine a patient concurrently in the same encounter (e.g., medical doctor and nurse practitioner), they have a tendency to use exclusionary jargon terms with each other when discussing clinical status in front of the patient,[48] impacting the opportunity for shared decision-making. Given evidence of negative parental reactions to jargon, and dissonance between clinicians’ perception and patients’ experience, our findings have implications for practice. Clarification of medical terminology may improve parent satisfaction, informed consent, and decision-making. It may alleviate parental anxiety, dissatisfaction, and suboptimal clinical outcomes occurring when parents are unclear about pre- and post-surgical care recommendations.
While there is great emphasis in research and practice on application of shared decision-making in pediatric care, specific lexical content of clinician discourse has been of minimal focus.[49, 50] Findings from our logistic regression indicate that clinician jargon use may be prompted by perception of parent understanding rather than parental demographic characteristics. These data present an opportunity for clinicians to improve communication by recognizing their own potential bias in perceptions of parents’ level of comprehension and maintaining awareness of language use.
The importance of this opportunity for improvement is supported by the possibility that clinicians may overestimate parents’ understanding.[47] For example, within our sample, parent use of jargon such as “tonsil” may originate from experience with specific terms based on pediatric visits, as opposed to overall medical knowledge. The relatively small number of parent-uttered terms compared to clinician-uttered terms (250 v 1,912) is also notable, as perceptions may be drawn from a small sample of dialogue. If clinicians misinterpret parental dialogue and adapt their language to use more terminology, parents may experience negative care experiences including unfavorable views of the clinician[12] and improper comprehension of medical information.[21, 23] Conversely, when clinicians explain jargon terms, patients experience better outcomes and greater understanding.[22] Despite the less extensive distribution of parental jargon use, clinicians were more likely to increase medical jargon use when consulting with parents who used jargon themselves. Therefore, even a small amount of parental jargon use has the potential to influence clinician communication. By maintaining awareness of the pitfalls of relying on subjective perceptions of parental involvement and ability, clinicians may improve communication with parents and foster an environment of shared decision-making.
We found that the degree of clinician jargon use was predicted by degree of parental jargon use consistently, both overall and within isolated categories. However, the same cannot be said for clinician perception of parental involvement, which predicted degree of clinician jargon use only when examining the full distribution of terms (anesthesiologist, IGG subclass; n=1912), and the less-commonly used contextual jargon (e.g., episode, candidate; n=272). Specific results of these differentiations are presented in Table 4. This distinction bears further examination with a larger and more diverse sample, and could be accounted for by a variety of factors. The isolation of different jargon categories necessarily limits range of data (e.g., chief complaint: M=8.8, R=0–38; overall: M=28.9, R=5–100). Furthermore, differences between contextual and medical terminology may also originate from the foundation of language use: Clinicians may consider medical jargon to be concrete and necessary (there is one word for “adenoids”). Contextual jargon terms are more nebulous and easier to rephrase. For example, the sentence “the tonsils are part of the immune system, but taking them out doesn’t compromise you,” could potentially be rephrased “even though the tonsils are part of the immune system, taking them out won’t harm you.” While “tonsils” and “immune system” are definitive names, the contextual term “compromise” is more flexible. Therefore, contextual jargon may be more likely to be used when clinicians perceive parents as involved in the discussion and subsequently relax their dialogue style to be more peer-associated. Unfortunately research on effects of contextual jargon use is sparse. Further research may investigate different properties of contextual and explicit medical language and how clinician usage of this language impacts parent experience of care and child health outcomes.
Limitations.
There was opportunity for coder bias (over or under interpretation) in the subjective identification of jargon. This limitation was accounted for by systematically double-coding each consult and confirming the jargon dictionary via a team of five researchers. Nevertheless, particular terms (e.g., adenoid) were disputed and discussed. We note that our sample is small (N=64 parents, 8 clinicians) and lacks demographic variation within each clinician’s practice. For example, of 8 practices, 2 included 100% public insurance while 1 included 100% private; 4 practices were over 80% white and 2 were 100% African-American). Additionally, we experienced significant collinearity between characteristics such as race and insurance (Black: 95.8% public insurance; White: 39.3% public insurance). Future research with larger samples of clinicians and a widespread demographic distribution is needed to determine the true prevalence of jargon in pediatric surgical care. A larger sample of contributing clinicians may increase the power of logistic regression, particularly considering the wide variation in jargon use between clinicians. Future research should also evaluate parental satisfaction with the manner in which clinicians used language, distinguishing objective jargon use from parental perception of jargon use. For example, despite wide use of medical jargon in our sample, many parents indicated that clinicians used medical terminology infrequently. Parental perceptions were based on a one-item survey measure administered in conjunction with our parent study[35], and could be accounted for by social desirability or recall factors.[16, 51] However, it may also represent subjective differences not accounted for in present literature. An extensive methodology measuring parental experience and satisfaction would add insight to complement results of this study. Additionally, because clinicians and parents were aware that their consults were audio-recorded, there is a potential for observer and social desirability effect.[51, 52] There was not a pre-encounter measure of parent knowledge about their child’s referral or condition. Preemptive knowledge by parents may have an impact on their degree of jargon introduction into consults. The object of this study was to ascertain overall extent of jargon use, or the cumulative number of terms to which parents were exposed. Future complementary research might also compare these results to the proportion of jargon terms based on consult length.
4.2. Conclusions
Jargon and complex language were used consistently across pediatric otolaryngology consults, but varied between clinicians. Further, clinicians use more jargon when they perceive parents as being more engaged in the healthcare process. Future research should address parental satisfaction and aim to understand what causes clinicians to amplify use of different jargon types, including perception of parental engagement or parent demographics.
4.3. Practice implications
These findings may help clinicians foster an awareness of their communication style and language use, and its potential consequences for parents and patients. This includes the extent to which they use difficult-to-understand terms, how they address the comprehension of parents and patients, and their self-awareness when making assumptions about parental understanding based on their involvement in decision-making.
Results from this study will be integrated into communication training. This training will seek to enhance clinician communication and interactions with parents, foster clinician self-awareness in language choice and use, and create strategies to systematically evaluate parental understanding of clinical communication.
Supplementary Material
Table 3:
Parent characteristics (N = 64)
| Characteristic | Parent, N = 64 [n (%)] |
|---|---|
| Age [M (SD)] | 33.4 (6.4) |
| Race/Ethnicity | |
| White | 30 (46.9) |
| African-American | 25 (39.1) |
| Hispanic | 5 (7.8) |
| Other | 4 (6.3) |
| Gender | |
| Female | 58 (90.6) |
| Male | 6 (9.4) |
| Insurance | |
| Private | 22 (34.4) |
| Public | 39 (60.9) |
| Other/Prefer not to say | 3 (4.7) |
| Income | |
| < 20,000 | 14 (22.9) |
| 20,000 – 79,999 | 27 (44.23) |
| >80,000 | 20 (32.8) |
| Education | |
| < high school | 3 (4.7) |
| High school degree | 35 (54.7) |
| Bachelor’s degree | 16 (25) |
| Graduate/Professional degree | 9 (14.1) |
| Other/Prefer not to say | 1 (1.6) |
| Clinical Equipoise | |
| Equipoise | 14 (23.3) |
| Towards watchful waiting | 11 (18.3) |
| Towards tonsillectomy | 35 (58.3) |
Acknowledgments
Funding: Dr. Boss was supported by the Agency for Healthcare Research and Quality (AHRQ K08HS022932). In addition, Dr. Beach was supported by K24 DA037804. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agency. Dr. Boss is also supported by the American Society of Pediatric Otolaryngology Career Development Award.
Footnotes
Declarations of interest: None
All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work
REFERENCES
- [1].Boss EF, et al. , Shared Decision Making and Choice for Elective Surgical Care: A Systematic Review, Otolaryngology -- Head and Neck Surgery(2015). 10.1177/0194599815620558. [DOI] [PMC free article] [PubMed]
- [2].Alexander NS and Schroeder JW Jr., Pediatric obstructive sleep apnea syndrome, Pediatr Clin North Am 60(2013): p. 827–40. 10.1016/j.pcl.2013.04.009. [DOI] [PubMed] [Google Scholar]
- [3].Ingram DG and Friedman NR, Toward Adenotonsillectomy in Children: A Review for the General Pediatrician, JAMA Pediatr(2015): p. 1–8. 10.1001/jamapediatrics.2015.2016. [DOI] [PubMed]
- [4].What’s an ENT? 2018. [cited 2018 11/28/2018]; Available from: https://www.enthealth.org/whats-an-ent/.
- [5].Grime C and Tan HL, Sleep Disordered Breathing in Children, Indian J Pediatr 82(2015): p. 945–55. 10.1007/s12098-015-1857-5. [DOI] [PubMed] [Google Scholar]
- [6].Collins CE and Everett LL, Challenges in pediatric ambulatory anesthesia: kids are different, Anesthesiol Clin 28(2010): p. 315–28. 10.1016/j.anclin.2010.02.005. [DOI] [PubMed] [Google Scholar]
- [7].Byars SG, Stearns SC, and Boomsma JJ, Association of Long-Term Risk of Respiratory, Allergic, and Infectious Diseases With Removal of Adenoids and Tonsils in Childhood, JAMA Otolaryngol Head Neck Surg 144(2018): p. 594–603. 10.1001/jamaoto.2018.0614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Marcus CL, et al. , A randomized trial of adenotonsillectomy for childhood sleep apnea, N Engl J Med 368(2013): p. 2366–76. 10.1056/NEJMoa1215881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Redline S, et al. , The Childhood Adenotonsillectomy Trial (CHAT): rationale, design, and challenges of a randomized controlled trial evaluating a standard surgical procedure in a pediatric population, Sleep 34(2011): p. 1509–17. 10.5665/sleep.1388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Hong P, et al. , Parental decision making in pediatric otoplasty: The role of shared decision making in parental decisional conflict and decisional regret, Laryngoscope 126 Suppl 5(2016): p. S5–s13. 10.1002/lary.26071. [DOI] [PubMed] [Google Scholar]
- [11].Flores G, The impact of medical interpreter services on the quality of health care: a systematic review, Med Care Res Rev 62(2005): p. 255–99. 10.1177/1077558705275416. [DOI] [PubMed] [Google Scholar]
- [12].Wiener RS, et al. , What do you mean, a spot?: A qualitative analysis of patients’ reactions to discussions with their physicians about pulmonary nodules, Chest 143(2013): p. 672–677. 10.1378/chest.12-1095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Rancher CE, et al. , Disclosing neuroimaging incidental findings: a qualitative thematic analysis of health literacy challenges, BMC Med Ethics 17(2016): p. 58 10.1186/s12910-016-0141-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Sadeghi S, Brooks D, and Goldstein RS, Patients’ and providers’ perceptions of the impact of health literacy on communication in pulmonary rehabilitation, Chron Respir Dis 10(2013): p. 65–76. 10.1177/1479972312471548. [DOI] [PubMed] [Google Scholar]
- [15].Hoang JK, Avoid Jargon Terms for Normal, J Am Coll Radiol 12(2015): p. 546 10.1016/j.jacr.2015.03.018. [DOI] [PubMed] [Google Scholar]
- [16].Al Sayah F, et al. , Health literacy and nurses’ communication with type 2 diabetes patients in primary care settings, Nurs Res 63(2014): p. 408–17. 10.1097/nnr.0000000000000055. [DOI] [PubMed] [Google Scholar]
- [17].Deuster L, et al. , A method to quantify residents’ jargon use during counseling of standardized patients about cancer screening, J Gen Intern Med 23(2008): p. 1947–52. 10.1007/s11606-008-0729-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Farrell M, et al. , Pediatric residents’ use of jargon during counseling about newborn genetic screening results, Pediatrics 122(2008): p. 243–9. 10.1542/peds.2007-2160. [DOI] [PubMed] [Google Scholar]
- [19].Schnitzler L, et al. , Communication during radiation therapy education sessions: The role of medical jargon and emotional support in clarifying patient confusion, Patient Educ Couns 100(2017): p. 112–120. 10.1016/j.pec.2016.08.006. [DOI] [PubMed] [Google Scholar]
- [20].Han PK, et al. , Conceptual problems in laypersons’ understanding of individualized cancer risk: a qualitative study, Health Expect 12(2009): p. 4–17. 10.1111/j.1369-7625.2008.00524.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Konstantynowicz J, et al. , What Do Children with Chronic Diseases and Their Parents Think About Pediatricians? A Qualitative Interview Study, Matern Child Health J 20(2016): p. 1745–52. 10.1007/s10995-016-1978-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Wernick M, et al. , A randomised crossover trial of minimising medical terminology in secondary care correspondence in patients with chronic health conditions: impact on understanding and patient reported outcomes, Intern Med J 46(2016): p. 596–601. 10.1111/imj.13062. [DOI] [PubMed] [Google Scholar]
- [23].Howe CJ, et al. , Parent Health Literacy and Communication With Diabetes Educators in a Pediatric Diabetes Clinic: A Mixed Methods Approach, J Health Commun 20 Suppl 2(2015): p. 50–9. 10.1080/10810730.2015.1083636. [DOI] [PubMed] [Google Scholar]
- [24].McCrary S and Christensen RC, Slang ‘on board’. A moral analysis of medical jargon, Arch Fam Med 2(1993): p. 101–5. [DOI] [PubMed] [Google Scholar]
- [25].Castro CM, et al. , Babel babble: physicians’ use of unclarified medical jargon with patients, Am J Health Behav 31 Suppl 1(2007): p. S85–95. 10.5555/ajhb.2007.31.supp.S85. [DOI] [PubMed] [Google Scholar]
- [26].Senekjian L, et al. , Do Women Understand Urogynecologic Terminology?, Female Pelvic Med Reconstr Surg 17(2011): p. 215–217. 10.1097/SPV.0b013e31822dcffe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Kessels RPC, Patients’ memory for medical information, Journal of the Royal Society of Medicine 96(2003): p. 219–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Kountz DS, Strategies for improving low health literacy, Postgrad Med 121(2009): p. 171–7. 10.3810/pgm.2009.09.2065. [DOI] [PubMed] [Google Scholar]
- [29].Hersh L, Salzman B, and Snyderman D, Health Literacy in Primary Care Practice, Am Fam Physician 92(2015): p. 118–24. [PubMed] [Google Scholar]
- [30].Hironaka LK and Paasche-Orlow MK, The implications of health literacy on patient-provider communication, Arch Dis Child 93(2008): p. 428–32. 10.1136/adc.2007.131516. [DOI] [PubMed] [Google Scholar]
- [31].Ventres W and Gordon P, Communication strategies in caring for the underserved, J Health Care Poor Underserved 1(1990): p. 305–14. [DOI] [PubMed] [Google Scholar]
- [32].Brody DS, et al. , Patient perception of involvement in medical care: relationship to illness attitudes and outcomes, J Gen Intern Med 4(1989): p. 506–11. [DOI] [PubMed] [Google Scholar]
- [33].Beach MC, Duggan PS, and Moore RD, Is patients’ preferred involvement in health decisions related to outcomes for patients with HIV?, J Gen Intern Med 22(2007): p. 1119–24. 10.1007/s11606-007-0241-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].O’Connor A. User Manuel--Measure of Decision/Choice Predisposition 1996. [cited 2018; Available from: http://decisionaid.ohri.ca/docs/develop/User_Manuals/UM_ChoicePredisposition_Decision.pdf.
- [35].Callon W, et al. , An expanded framework to define and measure shared decision-making in dialogue: A ‘top-down’ and ‘bottom-up’ approach, Patient Education and Counseling 10.1016/j.pec.2018.03.014. [DOI] [PMC free article] [PubMed]
- [36].Ryan L, et al. , Evaluation of printed health education materials for use by low-education families, J Nurs Scholarsh 46(2014): p. 218–28. 10.1111/jnu.12076. [DOI] [PubMed] [Google Scholar]
- [37].Wang LW, et al. , Assessing readability formula differences with written health information materials: application, results, and recommendations, Res Social Adm Pharm 9(2013): p. 503–16. 10.1016/j.sapharm.2012.05.009. [DOI] [PubMed] [Google Scholar]
- [38].Chujo K and Oghigian K, Examining corpus-based L2 vocabulary lists for grade level and semantic field distribution, (2015): p. 11–18.
- [39].Davies M. The Corpus of Contemporary American English (COCA): 560 million words, 1990-present . 2008; Available from: https://corpus.byu.edu/coca/.
- [40].Smith S. The Academic Word List (AWL) 2018. [cited 2018 3–22-18]; Available from: http://www.eapfoundation.com/vocab/academic/awllists/.
- [41].Smith S. The General Service List (GSL) 2018. [cited 2018 3–22-18]; Available from: http://www.eapfoundation.com/vocab/general/gsl/.
- [42].V. GbmH, MaxQDA Plus 2018, Verbi Software GbmH: Berlin, Germany. [Google Scholar]
- [43].StataCorp, Stata Statistical Software 2015, StataCorp: College Town, TX. [Google Scholar]
- [44].George MR, et al. , Using regression mixture models with non-normal data: Examining an ordered polytomous approach, J Stat Comput Simul 83(2013): p. 757–770. 10.1080/00949655.2011.636363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Barker KL, Reid M, and Minns Lowe CJ, What does the language we use about arthritis mean to people who have osteoarthritis? A qualitative study, Disabil Rehabil 36(2014): p. 367–72. 10.3109/09638288.2013.793409. [DOI] [PubMed] [Google Scholar]
- [46].Berman JR, et al. , Fellow use of medical jargon correlates inversely with patient and observer perceptions of professionalism: results of a rheumatology OSCE (ROSCE) using challenging patient scenarios, Clin Rheumatol 35(2016): p. 2093–9. 10.1007/s10067-015-3113-9. [DOI] [PubMed] [Google Scholar]
- [47].LeBlanc TW, et al. , Patient understanding of medical jargon: a survey study of U.S. medical students, Patient Educ Couns 95(2014): p. 238–42. 10.1016/j.pec.2014.01.014. [DOI] [PubMed] [Google Scholar]
- [48].Hamilton HE, et al. , Physicians, nonphysician healthcare providers, and patients communicating in hepatitis C: an in-office sociolinguistic study, Gastroenterol Nurs 29(2006): p. 364–70. [DOI] [PubMed] [Google Scholar]
- [49].Boss EF, et al. , Parent experience of care and decision-making for children who snore, JAMA Otolaryngology–Head & Neck Surgery(2016). 10.1001/jamaoto.2016.2400. [DOI] [PMC free article] [PubMed]
- [50].Chorney J, et al. , Understanding shared decision making in pediatric otolaryngology, Otolaryngol Head Neck Surg 152(2015): p. 941–7. 10.1177/0194599815574998. [DOI] [PubMed] [Google Scholar]
- [51].Crowne DP and Marlowe D, A new scale of social desirability independent of psychopathology, Journal of Consulting Psychology 24(1960): p. 349–354. 10.1037/h0047358. [DOI] [PubMed] [Google Scholar]
- [52].Laughlin PR and Wong-McCarthy WJ, Social inhibition as a function of observation and recording of performance, Journal of Experimental Social Psychology 11(1975): p. 560–571. 10.1016/0022-1031(75)90007-4. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


