Abstract
Objectives.
To examine whether exposure to family member deaths throughout the life course is associated with subjective life expectancy – a person’s assessment of their own mortality risk – at age 65, with attention to differences by race.
Methods.
We analyzed 11 waves of data from a study of men and women over age 50 (Health and Retirement Study; n=13,973).
Results.
Experiencing the deaths of multiple family members before the respondent is 50 years old is negatively associated with subjective life expectancy at age 65.
Discussion.
Understanding the life-course predictors of older adults’ subjective life expectancy is particularly important because survival expectations influence long-term planning, health, and longevity. Moreover, black Americans are exposed to more family member deaths earlier in their life compared to white Americans, with implications for long-term health and well-being.
Keywords: Subjective life expectancy, Race, Bereavement, Families, Aging
The United States has experienced dramatic gains in life expectancy as mortality has become concentrated at older ages (Arias, Heron, & Xu, 2017). Because of these gains, adults expect to live longer lives. However, subjective life expectancy – a person’s certainty that they will survive to a specific age – is influenced by a number of factors. A potentially significant but overlooked predictor of subjective life expectancy among older adults is exposure to the death of multiple family members throughout the life course. Prior studies have examined parental longevity as a biomedical or genetic predictor of subjective life expectancy (Griffin, Loh, & Hesketh, 2013; Hurd & McGarry, 1995; van Doorn & Kasl, 1998; van Solinge & Henkens, 2017), but family member deaths, especially multiple deaths, are stressful life events that may further reduce subjective life expectancy through multiple pathways (e.g., biological, social, psychological, behavioral). Specifically, family member deaths likely contribute to feelings of existential threat and fatalism, lowering expectations for survival. We shift thinking about the predictors of subjective life expectancy by suggesting that multiple family member deaths throughout the life course will be associated with lower levels of subjective life expectancy among older adults.
An important consideration is that, compared to whites, black Americans are exposed to earlier and more frequent family member deaths (Umberson et al., 2017), especially for current cohorts of older black adults who came of age in the Jim Crow era and experienced considerable discrimination throughout their lives. Because multiple family member deaths lead to an accumulation of stress and risk factors across the life course (Umberson, 2017), we expect that the consequences of multiple family member deaths for subjective life expectancy will be more significant for black than for white Americans. Understanding how family member deaths contribute to expectations for survival among older adults is essential because subjective life expectancy is a significant predictor of long-term planning, health, and well-being (e.g., Hurd & McGarry, 2002; Mirowsky, 1997; Perozek, 2008; van Solinge & Henkens, 2017). Older adults who do not expect to live a long life have fewer reasons to do things to promote longevity (e.g., accumulate wealth, plan for retirement, engage in health-promoting behavior). Indeed, lower expectations of survival are associated with a range of risky behaviors and poor health outcomes (e.g., Hurd, Smith, & Zissimopoulos, 2004; Scott-Sheldon et al., 2010; Mirowsky, 1997). As such, experiencing family member deaths has implications for long-term health and well-being.
The current study explores how exposure to the death of multiple close family members (i.e., mother, father, child, spouse, sibling) from childhood through adulthood is associated with subjective life expectancy at age 65 using the Health and Retirement Study (HRS), a nationally representative, longitudinal study of older Americans. We embed this study within a life course framework by focusing on the implications of family member deaths that occurred before the respondent is 50 years old. This study builds on prior work by merging a stress and life course perspective to examine the implications of stressful events (i.e., family loss) for midlife adults.
Background
Subjective Life Expectancy
Why Subjective Life Expectancy?
Subjective life expectancy – sometimes referred to as future certainty, subjective survival expectations, or subjective probabilities of survival – has implications for health across the life course, especially in mid- and later-life. Many studies on subjective life expectancy in adulthood have focused on the ability to predict behaviors that are important for older adults’ quality of life, such as planning and saving for retirement (Hamermesh, 1985; Hurd et al., 2004). Older adults’ survival expectations also have implications for health and longevity. For example, adults’ subjective life expectancy is positively associated with personal control or mastery (Mirowsky, 1997), which is protective against depression, distrust, health-compromising behaviors, and mortality (e.g., Pearlin et al., 1981; Seeman & Lewis, 1995). Although pessimistic expectations for survival may encourage people to live more carefully (e.g., Lang & Carstensen, 2002) and unrealistic optimism may prompt recklessness and risk-seeking (e.g., Chipperfield et al., 2016), the vast majority of studies of subjective life expectancy find that higher expectations promote longevity. Indeed, one of the most significant characteristics of subjective life expectancy is its association with mortality (Hurd & McGarry, 2002; Jylhä, 2011; Perozek, 2008; Smith, Taylor, & Sloan, 2001; van Solinge & Henkens, 2017). Subjective life expectancy in midlife warrants greater research attention, including attention to heterogeneity (e.g., race) in, and new predictors of, subjective life expectancy.
Race Differences in Subjective Life Expectancy
Race differences in subjective life expectancy are not fully understood. Prior research on subjective life expectancy of adults shows a race paradox, such that black individuals expect to live longer than whites, despite their shorter life expectancy (Bulanda & Zhang, 2009; Irby-Shasanmi, 2012; Mirowsky, 1999). The reasons for this paradox remain unclear. However, these findings align with prior studies finding over-optimism among black individuals in other domains. For example, compared to whites, black high school students have higher occupational and educational expectations than their socioeconomic status would predict (Ainsworth-Darnell & Downey, 1998; Kao & Tienda, 1998). One explanation for the racial paradox in subjective life expectancy is methodological, which can be attributed to race differences in reporting heterogeneity (Lee & Smith, 2016). For example, white adults are more likely to say they have a 50% chance of surviving to age 75, whereas black adults are more likely to say they have 100% chance. This race difference in focal values could contribute to a race difference in survival expectations. However, despite some heterogeneity in reporting subjective life expectancy by race, subjective life expectancy is an accurate indicator of subsequent health for white and black respondents (Lee & Smith, 2016).
Another explanation is selection. Because of unequal selection by socioeconomic status across the life course (Pudrovska, 2014), an older sample may be a robust group of adults, especially black respondents. Indeed, the considerably higher mortality rates for blacks compared to whites at younger ages (Rogers, Lawrence, Hummer, & Tilstra, 2017) could mean that “blacks who survive past the early life course are more hopeful about surviving to older ages because they feel they are a select group” (Bulanda & Zhang, 2009, p. 691). Thus, because the present study assesses subjective life expectancy when respondents are age 65, the sample may consist of a group of robust survivors who lived to age 65 despite their disadvantaged backgrounds. For example, the majority of black adults in our sample were born in the 1930s and 1940s and experienced considerable discrimination and segregation throughout their lives. In line with prior research, we expect black older adults to report higher/more optimistic subjective life expectancy than whites. As a first step, we confirm race differences in subjective life expectancy at midlife before testing our main research hypotheses.
Family Member Death and Subjective Life Expectancy
A substantial literature finds that the death of a family member undermines health and mortality (e.g., Marks, Jun, & Song, 2007; Stroebe, Schut, & Stroebe, 2007). Losing a family member is one of the most stressful events over a person’s life course and such losses can trigger a cascade of biopsychosocial and behavioral responses that undermine health for years to come (e.g., Maier & Lachman, 2000; Marks et al., 2007; Stroebe et al., 2007). For example, exposure to death can increase engagement in risky behaviors (alcohol, smoking), vigilance and anxiety, and strain in existing relationships (Marks et al., 2007; Umberson, Liu, & Reczek, 2008; Utz et al., 2002). Moreover, losing a family member often leads to new financial strains, especially when the family member is a primary wage earner, such as a parent or spouse. Lower income, especially earlier in life, has considerable consequences for future health and well-being (e.g., Elo, 2009; Pudrovska, 2014). Thus, death exposures can lead to an accumulation of risk factors over the life course.
Notably, many of these responses to the loss of a loved one (e.g., socioeconomic status, relationship quality, health behaviors) are predictive of subjective life expectancy (e.g., Griffin et al., 2013; Hurd & McGarry, 1995; Irby-Shasanmi, 2012; Mirowsky & Ross, 2000; Ross & Mirowsky, 2002). However, prior work has largely neglected to consider how family member deaths shape subjective life expectancy. The few studies that include a family member death typically focus solely on parental longevity as a genetic indicator of survival (Griffin et al., 2013; Hurd & McGarry, 1995; van Doorn & Kasl, 1998; van Solinge & Henkens, 2017). Indeed, individuals may use family member longevity as information in assessing their own likelihood of surviving. The death of genetically-similar family members (e.g., parents) may signal shared risks that contribute to individuals’ more realistic and/or pessimistic subjective life expectancy. This is supported by evidence suggesting that individuals are more optimistic about their survival prospects if their parent has survived to old age (Griffin et al., 2013; Hurd & McGarry, 1995; van Doorn & Kasl, 1998; van Solinge & Henkens, 2017). Thus, if a family member’s death is earlier than anticipated, it may have greater consequences for a person’s subjective life expectancy than if the family member death occurs “on-time”. This may be because subjective life expectancy is a fairly accurate reflection of a person’s health, and both genetics and family member death contribute to poor health.
However, we suggest that exposure to family losses will also reduce an individual’s subjective life expectancy in midlife because experiencing family member deaths, especially earlier than anticipated, can change a person’s outlook on life. Indeed, this idea was documented as early as the 1600s when John Donne stated “Any man’s death diminishes me, because I am involved in mankind; and therefore never send to know for whom the bell tolls; it tolls for thee.” Donne was likely indicating that the death of others is a loss to mankind, of which we are a part, and is also a reminder of the inevitability of one’s own death. Thus, the death of family members can force individuals to acknowledge their own mortality. This can contribute to feelings of existential threat or fatalism, especially when people are confronted with repeated family losses. For example, one qualitative study found that experiencing the murder of close friends and relatives significantly altered young men’s worldviews and perceptions of the length of their own lives (Smith, 2015). Moreover, the death of a parent often marks a rite of passage to adulthood as the child becomes the next generation in line for death (Umberson, 2003). However, when these transitional events are non-normative and involuntary (e.g., the death of a parent in young adulthood), reactions tend to be more harmful (Pearlin et al., 2005) and may contribute to pessimistic expectations for survival. Moreover, experiencing multiple family deaths likely has cumulative effects for survival expectations. Although prior work has not examined whether the accumulation of family deaths has cumulative effects on health and well-being, Umberson (2017) identifies this as an avenue for future research. Thus, we investigate whether experiencing family member deaths, especially before midlife, will reduce expectations for survival. This is important because subjective life expectancy has real consequences for later life planning and health.
A stress and life course perspective emphasizes that consideration of the timing of significant stressors is essential to understanding the implications of stress, especially among older adults (Pearlin & Skaff, 1996). Indeed, deaths occurring earlier than anticipated, or “off-time,” are more likely to activate a range of short- and long-term responses (e.g., Maier & Lachman, 2000; Shonkoff et al., 2012). These off-time deaths may occur during or after childhood (e.g., death of a spouse in midlife), and deaths in midlife likely compound earlier losses. Indeed, traumatic events experienced before age 65, including the death of family members, have the strongest relationship with current health in older adults (Krause, Shaw, & Cairney, 2004). Therefore, we test the following hypothesis:
Hypothesis 1: Exposure to family member deaths, especially multiple deaths, before age 50 will be associated with lower subjective life expectancy at age 65.
Race, Family Member Death, and Subjective Life Expectancy
The stress process model emphasizes that disadvantaged groups are exposed to more stressors and have fewer resources to cope with these stressful experiences (Pearlin et al., 2005). Race differences in exposure to the death of close family members reflect this socially-patterned variation in stress. Indeed, black Americans experience family member death earlier and more frequently in life compared to white Americans (Umberson et al., 2017). For example, recent research shows that black individuals are two to three times more likely than whites to lose a parent by age 20 (Umberson et al., 2017). This racial inequality in exposure to family member deaths reflects the destructive effects of historical race differences in mortality risk across the life course (e.g., Arias et al., 2017).
Guided by theories of cumulative disadvantage and resilience, we examine whether black and white respondents have differential reactions to family member deaths. In line with the cumulative disadvantage perspective, we may expect that black respondents will report worse survival expectations than whites in response to family member deaths. This is because family member deaths launch a cascade of adversity that reduces resources, increases risks, and increases stress over time. Moreover, earlier stressors are exacerbated by later-life stressors and lead to accumulating disadvantage over the life course. Thus, because black Americans experience earlier and more frequent family member deaths throughout their lives (Umberson et al., 2017), and this leads to a longer period of accumulating disadvantage, each additional death may have a larger impact on subjective life expectancy for black compared to white older adults.
An alternative possibility is that the association between family member death and survival expectations may be weaker for blacks compared to whites as a reflection of resilience among black adults. Theories of resilience emphasize heterogeneity in the effects of disadvantage, and indeed, studies have found that the consequences of adverse events can unfold in unexpected ways. For example, research on cancer survivors suggests that, for some, cancer can increase mastery (Pudrovska, 2010a) and slow the rate of decline in personal growth that accompanies age (Pudrovska, 2010b). In the present study, the sample of older black Americans in the HRS is more likely than older white Americans to be both physically and psychologically robust as a result of overcoming the repeated trauma of losing close family members. Moreover, recent research finds that older black adults are less likely to be upset by exposure to stressors compared to white adults (Brown, Mitchell, & Ailshire, Forthcoming). These theories align with prior work findings that black adults expect to live longer than whites, despite their greater socioeconomic disadvantage (Bulanda & Zhang, 2009; Irby-Shasanmi, 2012; Mirowsky, 1999). Taken together, we test the following hypothesis:
Hypothesis 2: The association between family member deaths and subjective life expectancy at age 65 will be weaker for black compared to white older adults.
Data and Methods
Data
For the present study, we analyze 11 waves of longitudinal data from the Health and Retirement Study (HRS), a nationally representative sample of the United States population over age 50. The HRS has been administered every two years since 1992 and has added new cohorts every six years with younger cohorts not previously represented. Cohorts in the HRS include the original HRS cohort (born 1931–1941), the AHEAD cohort (born 1890–1923), the Children of the Depression cohort (born 1924–1930), the War Babies cohort (born 1942–1947), the Early Baby Boomers (born 1948–1953), and the Mid Baby Boomers (born 1954–1959). The HRS oversamples African-American and Hispanic households. The analytic sample for this study includes respondents who identify as non-Hispanic white or non-Hispanic black and who reported their subjective life expectancy at age 65 during the study period (n=13,973). Thus, the analytic sample includes respondents from four cohorts: the original HRS cohort, the Children of the Depression cohort, the War Babies cohort, and the Early Baby Boomers cohort.
Measures
The outcome of interest is subjective life expectancy measured at age 65. Because the HRS is administered every two years, we use the measure of subjective life expectancy when the respondent is closest to 65 years old but at least 61 years old. This approach essentially organizes the HRS data by age instead of survey year. For example, the older respondents were age 65 in the 2nd and 3rd waves, whereas the younger respondents, especially those from replenishing cohorts (e.g., Early Baby Boomers), were age 65 in the 11th wave. Respondents 65 years old and under were asked: “What is the percent chance that you will live to be 75 or more.” Responses ranged from 0 to 100, which we convert to a proportion for analytic purposes described below (range 0 to 1). There is some evidence of heaping on this measure, particularly at 50 percent chance (25% of sample) and 100 percent chance (19% of sample). We examine subjective life expectancy at age 65 to record the percent chance that respondents think they will live ten additional years. Although subjective assessments of mortality may be less accurate than objective predictions based on life tables (Elder, 2013), subjective assessments have internal consistency, predictive validity, and covary with other variables in a way that is similar to objective assessments (Hurd & McGarry, 1995; Hurd & McGarry, 2002).
For the measure of cumulative family member death, we consider the death of mothers, fathers, siblings, spouses, and children. To take into account variability in the risk of exposure to family deaths, we limit analyses of deaths to respondents who report having the family relationship. For example, in recording whether or not a respondent has experienced the death of a spouse, we only include respondents who were ever married. Measures of parental death were considered missing if the respondent did not know whether their parent was alive. We further consider the age of the respondent when a family member died. Respondents reported the year in which mother, father, and spouse death occurred. Respondents did not report the year when children or siblings died. We include deaths of children or siblings that occurred between the 2 year survey waves by coding these deaths at the midpoint of the time between surveys. Other sibling deaths that occurred before the baseline survey are not included in the analysis, which likely reflects an underestimation of the total number of deaths. The limited information about siblings also prevents us from including a control for childhood family size. For child deaths, respondents report the number of children they have had and the number of children currently living during their baseline interview. Thus, if respondents report fewer living children than the number of children ever born, this is coded as experiencing a child’s death before age 50. We subtract the respondent’s birth year from the year of death to get the respondent’s age at each family member death. If respondents experienced the death of multiple siblings, spouses, or children, we use the respondent’s age at the time of the first death exposure (e.g., age when first sibling died). This approach aligns with previous work by Umberson and colleagues (2017).
We focus on cumulative death exposure before age 50 by summing binary indicators of each family member death (1=yes). We also control for family member deaths occurring between age 51 and 65. For both of these measures, response categories include no deaths, 1 death, 2 deaths, or 3 or more deaths. The measure of the number of family deaths before age 50 includes parents, spouses, and children, whereas the measure of family deaths between age 50 and 65 also includes the death of a sibling.
We include control variables that are likely associated with family death exposure and subjective life expectancy, including race (1=black), gender (1=female), HRS birth cohort, mean parent education (in years), life course residence (born in south, live in south (reference); born in south, live outside south; born outside south, live in south; born outside south, live outside south), household size at baseline interview, number of children ever born to respondent, the number of chronic conditions at age 65, self-rated health at age 65 (excellent (ref), very good, good, fair, poor), and dementia status (cognitively intact (ref), cognitive impairment without dementia (CIND), dementia). Self-rated health is included to tap into psychosocial factors contributing to the assessment of subjective life expectancy. Moreover, the measure of chronic conditions requires a diagnosis from a doctor and, thus, access to health care, which varies across sociodemographic groups. Dementia status is included to account for cognitive functioning that might impact a person’s ability to assess probabilities. For parent’s education, we considered the average of the number of years of schooling completed by each parent. Missing data on control variables were accounted for with multiple imputation, which estimated missing values for all respondents based on simulated versions of the sample.
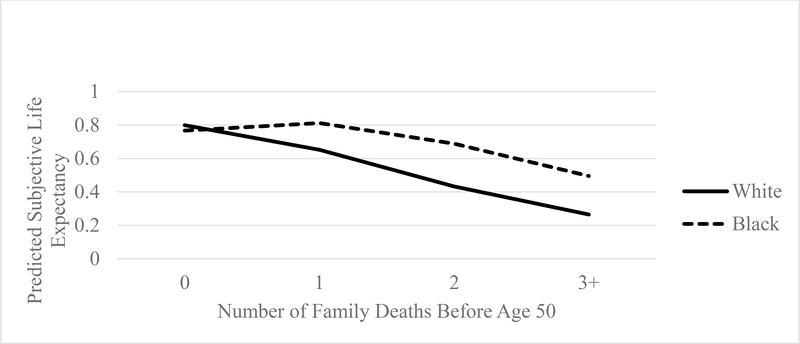
Analytic Strategy
To examine whether cumulative family member deaths across the life course are associated with subjective life expectancy at age 65, we use generalized linear models with a logit link and the binomial family. This type of model, which employs a maximum likelihood estimator, is appropriate when the dependent variable has values between zero and one. Table 2 examines the association of cumulative family member death exposure before age 50 with subjective life expectancy at age 65 and whether this association differs for black and white respondents. We estimate predicted values to illustrate the pattern of results in Figure 1. Finally, Table 3 examines whether the death of specific family members before age 50 is associated with survival expectations at age 65. We model the most common combinations of family member death before age 50 (mother only, father only, both parents, a parent and a spouse, a parent and a child) in comparison to respondents who experienced no family member death by age 50. As a robustness check, we replicated all results using a regression model for heaped data (Cummings et al., 2015), and the pattern of results was the same. In all analyses, we include controls for covariates and account for the complex survey design of the HRS.
Table 2.
Generalized Linear Model Results of Subjective Life Expectancy at Age 65 Regressed on Cumulative Family Death Exposure (n=13,973)
| 1 | (SE) | 2 | (SE) | |
|---|---|---|---|---|
| Number of Family Deaths Age 0–50 (ref: 1 Death) | ||||
| 0 Deaths | 0.11** | (0.03) | 0 14*** | (0.03) |
| 2 Deaths | −0.17*** | (0.03) | −0 19*** | (0.04) |
| 3+ Deaths | −0.24*** | (0.06) | −0.24*** | (0.06) |
| Number of Family Deaths Age 51–65 (ref: 1 Death) | ||||
| 0 Deaths | −0.02 | (0.02) | −0.02 | (0.02) |
| 2 Deaths | −0.02 | (0.03) | −0.03 | (0.03) |
| 3+ Deaths | −0.07 | (0.06) | −0.07 | (0.06) |
| Black | 0.36*** | (0.04) | 0.37*** | (0.05) |
| Female | 0 17*** | (0.03) | 0 17*** | (0.03) |
| Birth Cohort (ref: Born 1931–1941) | ||||
| Born 1924–1930 | 0.04 | (0.05) | 0.04 | (0.05) |
| Born 1942–1947 | −0.04 | (0.03) | −0.04+ | (0.03) |
| Born 1948–1953 | −0.22*** | (0.04) | −0.22*** | (0.04) |
| Parent Education | 0.03*** | (0.05) | 0.03*** | (0.01) |
| Life Course Residence (ref: Born south, live south) | ||||
| Born south, live outside south | 0.07 | (0.05) | 0.07 | (0.05) |
| Born outside south, live outside south | 0.03 | (0.03) | 0.03 | (0.03) |
| Born outside south, live in south | 0.05 | (0.05) | 0.05 | (0.05) |
| Baseline Household Size | 0.01 | (0.01) | 0.01 | (0.01) |
| Number of Kids Ever Born | 0.01 | (0.01) | 0.01 | (0.01) |
| Chronic Conditions at 65 | −0.07*** | (0.01) | −0 07*** | (0.01) |
| Self-Rated Health at 65 (ref: Excellent Health) | ||||
| Very Good | −0.27*** | (0.04) | −0.27*** | (0.04) |
| Good | −0.54*** | (0.04) | −0.54*** | (0.04) |
| Fair | −0 89*** | (0.04) | −0.89*** | (0.04) |
| Poor | −1.30*** | (0.06) | −1.30*** | (0.06) |
| Dementia Status at 65 (ref: No Dementia/CIND) | ||||
| Dementia | −0.27** | (0.10) | −0.26** | (0.10) |
| Cognitive Impairment - No Dementia (CIND) | −0.12** | (0.04) | −0.12** | (0.04) |
| Black*0 Deaths from Age 0–50 | −0.16* | (0.08) | ||
| Black*2 Deaths from Age 0–50 | 0.10 | (0.07) | ||
| Black*3+ Death from Age 0–50 | −0.01 | (0.14) | ||
| Constant | 0.91*** | (0.08) | 0.91*** | (0.08) |
p<0.001
p<0.01
p<0.05
p<0.10
Figure 1.
Predicted Subjective Life Expectancy by Number of Family Deaths Before Age 50 for Black and White Americans
Table 3.
Generalized Linear Model Results of Subjective Life Expectancy at Age 65 Regressed on Specific Family Deaths Before Age 50 (n=10,056)
| 1 | (SE) | |
|---|---|---|
| Type of Family Death Age 0–50 (ref: No Deaths 0–50) | ||
| Only Mother Died | −0.12* | (0.06) |
| Only Father Died | −0.13** | (0.05) |
| Both Mother & Father Died | −0.34*** | (0.05) |
| A Parent & A Spouse Died | −0.32*** | (0.08) |
| A Parent & A Child Died | −0 29*** | (0.06) |
| Number of Family Deaths Age 51–65 (ref: 1 Death) | ||
| 0 Deaths | −0.02 | (0.03) |
| 2 Deaths | −0.04 | (0.04) |
| 3+ Deaths | −0.14+ | (0.07) |
| Black | 0 44*** | (0.06) |
| Female | 0.14*** | (0.03) |
| Birth Cohort (ref: Born 1931–1941) | ||
| Born 1924–1930 | 0.04 | (0.05) |
| Born 1942–1947 | 0.01 | (0.03) |
| Born 1948–1953 | −0 19*** | (0.04) |
| Parent Education | 0.03*** | (0.01) |
| Life Course Residence (ref: Born south, live south) | ||
| Born south, live outside south | 0.01 | (0.06) |
| Born outside south, live outside south | 0.04 | (0.04) |
| Born outside south, live in south | 0.08+ | (0.05) |
| Baseline Household Size | 0.02+ | (0.01) |
| Number of Kids Ever Born | −0.01 | (0.01) |
| Chronic Conditions at 65 | −0.07*** | (0.01) |
| Self-Rated Health at 65 (ref: Excellent Health) | ||
| Very Good | −0 27*** | (0.05) |
| Good | −0.56*** | (0.05) |
| Fair | −0 90*** | (0.05) |
| Poor | −1.35*** | (0.06) |
| Dementia Status at 65 (ref: No Dementia/CIND) | ||
| Dementia | −0.23+ | (0.12) |
| Cognitive Impairment - No Dementia (CIND) | −0.11* | (0.05) |
| Constant | 1.03*** | (0.11) |
p<0.001
p<0.01
p<0.05
p<0.10
Results
Descriptive Results
Descriptive results in Table 1 show that, on average, black adults report a somewhat greater percent chance that they will live to age 75 (67%) compared to white adults (64%) when they are 65 years old. Descriptive results also show that a greater percent of black respondents report two family member deaths or three or more family member deaths before age 50. The black sample is also more female, has lower mean parent education, is much more likely to have been born in the south, has more children on average, has been diagnosed with more chronic conditions at age 65, reports worse self-rated health at age 65, and has higher rates of dementia at age 65 compared to the white sample of adults.
Table 1.
Descriptive data for sample
| Total (n=13,973) | White (n=11,434) | Black (n=2,539) | |
|---|---|---|---|
| Subjective Life Expectancy at Age 65 (Mean) | 0.65 | 0.64 | 0.67a |
| Number of Family Deaths Age 0–50 (%) | |||
| 0 Deaths | 25.86 | 26.71 | 22.02 a |
| 1 Death | 40.39 | 40.98 | 37.69 a |
| 2 Deaths | 28.81 | 28.28 | 31.23 a |
| 3+ Deaths | 4.95 | 4.03 | 9.06 a |
| Number of Family Deaths Age 0–50 (Mean) | 1.13 | 1.09 | 1.27a |
| Specific Family Deaths Age 0–50 (%) | |||
| Mother Death | 41.35 | 39.95 | 47.45 a |
| Father Death | 69.26 | 69.28 | 69.17 |
| Spouse Death | 5.97 | 5.16 | 9.87 a |
| Child Death | 10.13 | 8.73 | 16.50 a |
| Number of Family Deaths Age 50–65 (%) | |||
| 0 Deaths | 37.67 | 38.18 | 35.37 a |
| 1 Death | 41.87 | 42.18 | 40.45 |
| 2 Deaths | 17.20 | 16.75 | 19.26 a |
| 3+ Deaths | 3.26 | 2.89 | 4.92 a |
| Black (%) | 18.17 | ||
| Female (%) | 54.98 | 53.69 | 60.81 a |
| Birth Cohort (%) | |||
| Born 1924–1930 | 5.25 | 5.71 | 3.19 a |
| Born 1931–1941 | 57.27 | 58.23 | 52.97 a |
| Born 1942–1947 | 18.91 | 19.46 | 16.42 a |
| Born 1948–1953 | 18.56 | 16.60 | 27.41 a |
| Parent Education (Mean) | 9.48 | 9.72 | 8.40 a |
| Life Course Residence (%) | |||
| Born south, live south | 28.74 | 24.36 | 48.48 a |
| Born south, live outside south | 8.09 | 4.51 | 24.22 a |
| Born outside south, live outside south | 50.78 | 57.27 | 21.54 a |
| Born outside south, live in south | 12.39 | 13.86 | 5.75 a |
| Baseline Household Size (Mean) | 2.66 | 2.63 | 2.83 a |
| Number of Kids Ever Born (Mean) | 2.81 | 2.70 | 3.35 a |
| Chronic Conditions at 65 (Mean) | 1.74 | 1.68 | 1.97 a |
| Self-Rated Health at 65 (%) | |||
| Excellent | 13.57 | 14.83 | 7.92 a |
| Very Good | 30.59 | 32.31 | 22.89 a |
| Good | 30.83 | 30.33 | 33.09 a |
| Fair | 17.57 | 15.80 | 25.57 a |
| Poor | 7.43 | 6.73 | 10.56 a |
| Dementia Status at 65 (%) | |||
| Dementia | 1.90 | 1.20 | 5.09 a |
| Cognitive Impairment - No Dementia (CIND) | 11.37 | 8.70 | 23.42 a |
| No Dementia/CIND | 86.72 | 90.11 | 71.49 a |
Note:
significantly different from white respondents
Family Member Death and Subjective Life Expectancy
We first examine the association of the number of family deaths experienced before age 50 with subjective life expectancy at age 65, accounting for the previously mentioned covariates (Table 2). Model 1 in Table 2 shows that the accumulation of family member deaths before age 50 is strongly associated with subjective life expectancy at age 65, net of covariates. For example, compared to respondents who experience one family member death before age 50, those who experience two deaths before age 50 or three or more family deaths before age 50 report lower odds of surviving to age 75 in midlife (p<.001). Notably, experiencing the death of family members between age 50 and 65 is not significantly associated with subjective life expectancy at age 65 after accounting for deaths experienced before age 50, even though those deaths are most recent. Overall, results indicate that exposure to multiple family member deaths is harmful for subjective life expectancy at age 65, but only for deaths experienced before age 50.
We also examine whether the association between family member death before age 50 and subjective life expectancy at age 65 is being driven by a few key deaths (e.g., parent deaths). In Table 3, we focus on the most common combinations of death before age 50 and thus use a smaller subsample (n=10,056). We find that, compared to respondents who experience no family member death before age 50, respondents who are exposed to the death of a mother (p<.05), a father (p<.01), both parents (p<.001), at least one parent and a spouse (p<.001), or at least one parent a child (p<.001) before age 50 report a lower chance of surviving 10 additional years at age 65. These findings suggest two things. First, the association between family member death and survival expectations is not being driven solely by the death of respondents’ parents, even though respondents may see their parents as genetic indicators of their own chances of survival. Second, the coefficients are largest for multiple family member deaths (i.e., losing both parents, a parent and a spouse, or a parent and a child), providing evidence that the accumulation of family member deaths has cumulative consequences for survival expectations.
Race, Family Death, and Subjective Life Expectancy
We next examine whether the association between family member deaths and subjective life expectancy at 65 differs for black and white respondents. Although black respondents report higher subjective life expectancy at 65, there is no difference between black and white respondents in the association between family loss and subjective life expectancy for the most part. However, the negative and significant interaction of race and no family member deaths before age 50 in Model 2 of Table 2 (p<.05) indicates race differences in the consequences of the first family loss before age 50. The interactions between race and 2 deaths or 3+ deaths are not significant, suggesting that the negative consequences of more than one family member deaths before age 50 may be similar for black and white respondents. This is illustrated in Figure 1, which shows the predicted subjective life expectancy of black and white adults by the number of family member deaths experienced by age 50. Figure 1 shows that black and white adults have similar reports of subjective life expectancy when they have not experienced a family member death. However, whereas the line in Figure 1 slopes down at a relatively consistent rate for white adults, it does not begin sloping downward until after one family loss for white adults. Thus, one family member death before age 50 has greater consequences for the survival expectations of white respondents at age 65, but the accumulation of multiple family member deaths before age 50 has similar consequences for black and white respondents.
Discussion
The death of a family member, especially an off-time death, is a highly stressful event that has a range of consequences for the bereaved individual. However, prior work has not examined whether the death of multiple family members throughout life contributes to subjective life expectancy in later midlife. Understanding the life course factors that contribute to subjective assessments of survival is particularly important in light of evidence that higher expectations for survival promote long-term planning, health, and longevity (e.g., Hurd & McGarry, 2002; Mirowsky, 1997; Perozek, 2008; van Solinge & Henkens, 2017). The current study examined whether exposure to family member deaths before age 50 is associated with subjective life expectancy at age 65 and whether this association differs for black and white Americans. We hypothesized that family member deaths, especially multiple deaths, would reduce subjective life expectancy in midlife. We highlight two major themes that emerged from the findings.
First, in support of Hypothesis 1, we found that the accumulation of family member deaths by age 50 has adverse consequences for survival assessments at age 65, accounting for more recent deaths that occur after age 50. We expand on prior work finding that parental longevity improves expectations for survival (Griffin et al., 2013; Hurd & McGarry, 1995; van Doorn & Kasl, 1998; van Solinge & Henkens, 2017) by suggesting that any family member deaths before midlife are significant stressors that shape subjective life expectancy. We note that these findings are not driven by specific key deaths, such as the death of parents early in life. Although parental longevity is undoubtedly a genetic indicator of survival that respondents consider when assessing their own chances of survival, we suggest that multiple family member deaths before midlife can have cumulative effects on subjective life expectancy. One explanation is that any death of a loved one can change a person’s outlook on life (Smith, 2015) and can lead to feelings of existential threat or fatalism that can lower expectations for survival. Indeed, a stress and life course perspective indicates that traumatic and non-normative events (e.g., the death of a child in midlife) can have particularly harmful consequences (Pearlin & Skaff, 1996; Pearlin et al., 2005) and can lead to an accumulation of risk factors for poor health over the life course. Because survival expectations predict health and well-being (e.g., Hurd & McGarry, 2002; Hurd et al., 2004; Jylhä, 2011; Perozek, 2008; Smith, Taylor, & Sloan, 2001; van Solinge & Henkens, 2017), low subjective life expectancy at age 65 is certainly a risk factor for aging adults.
The second major theme concerns race differences in survival expectations and the association between family member death and survival expectations. First, we found that black respondents reported higher subjective life expectancy than whites at age 65. Although this finding does not align with well-documented objective mortality data, wherein black Americans have a lower life expectancy than white Americans, this finding aligns with other studies documenting a more general optimism of subjective life expectancy and other positive outcomes among black respondents (Ainsworth-Darnell & Downey, 1998; Bulanda & Zhang, 2009; Irby-Shasanmi, 2012; Kao & Tienda, 1998; Mirowsky, 1999) and well-documented race differences in survival expectations (Bulanda & Zhang, 2009; Irby-Shasanmi, 2012; Mirowsky, 1999).
We also found only modest differences in the consequences of multiple family member losses for black and white adults (partial support for Hypothesis 2). Indeed, one family member death before age 50 is associated with a greater reduction in survival expectations for white respondents than black respondents at age 65, but each additional loss is associated with a similar reduction for black and white adults. One explanation for this finding is that because black Americans experience family member deaths earlier and more frequently in life compared to white Americans (Umberson et al., 2017), experiencing only one family member death by age 50 could be less normative and thus change one’s outlook on life more dramatically for white compared to black adults. Another explanation, drawing on theories of resilience, is that the current sample of 65 year old black respondents in the HRS is more physically and psychologically robust than the sample of white respondents due to selection processes across the life course (Pudrovska, 2014). Older black adults who have been exposed to the repeated trauma of losing close family members and have survived a prejudicial social and political landscape may be particularly resilient and realistically optimistic about their survival prospects. Indeed, Bulanda and Zhang (2009) note that black adults surviving into midlife may be hopeful about future survival because they feel they are a select group. Moreover, older black adults are less reactive to stressors compared to white adults (Brown et al., Forthcoming), suggesting greater resilience in the face of stress. Thus, the trauma of a family member death by age 50 may have less of an impact on the survival expectations for this cohort of older black adults.
The present study advances our understanding of how exposure to the death of multiple family members is associated with lower expectations for survival in later midlife. However, limitations should be noted. First, we do not have information about the cause of death for family members. The reasons why family members are dying may have different effects on subjective life expectancy (e.g., genetic health-related death versus an accident) or may differ by race. This is an important avenue for future research. Second, we measure subjective life expectancy at age 65, excluding respondents who may have died before 65; thus, the analytic sample, especially the black sample, is likely a select group. For example, black respondents report higher subjective life expectancy than white respondents in Table 1, which may exist due to the absence of higher mortality black Americans from these survey data (Mirowsky, 1999). Future studies should continue to explore the causes and consequences of this well-documented race paradox in subjective life expectancy (Bulanda & Zhang, 2009; Irby-Shasanmi, 2012; Mirowsky, 1999). Similarly, interviews in the HRS can be conducted with proxies when respondents are unable to be interviewed; however, proxies are not asked the subjective life expectancy question. Thus, many unhealthy respondents are excluded from the analytic sample. Finally, the HRS did not ask respondents about the deaths of other close relatives (e.g., grandparents, cousins) or close non-kin relationships (e.g., neighbors, friends), which likely differ by race. For example, prior work has documented that the violent death of black young men’s close friends and extended kin has deleterious consequences for well-being (Smith, 2015).
Overall, this study represents an essential first step in establishing the association between multiple family member deaths across the life course and subjective life expectancy among older adults. Our findings suggest that the accumulation of multiple family member deaths before age 50 is detrimental for subjective life expectancy. Future studies should document specific biopsychosocial and behavioral pathways through which family member deaths contribute to subjective life expectancy. Understanding the life-course predictors of subjective life expectancy is particularly important in light of the robust and persistent association between survival expectations and mortality (Hurd & McGarry, 2002; Jylhä, 2011; Perozek, 2008; Smith et al., 2001; van Solinge & Henkens, 2017). The findings from the present study highlight the need for public health interventions to target individuals experiencing family losses, especially off-time losses. These interventions could reduce the adverse consequences of family member death for older adults’ survival expectations and future health outcomes, a key consideration for an aging population.
Acknowledgments
This research was supported, in part, by grant P2CHD042849, Population Research Center, awarded to the Population Research Center at The University of Texas at Austin by the Eunice Kennedy Shriver National Institute of Child Health and Human Development; grant T32HD007081, Training Program in Population Studies, awarded to the Population Research Center at The University of Texas at Austin by the Eunice Kennedy Shriver National Institute of Child Health and Human Development; and grant R01AG17455 from the National Institute on Aging (PI, Debra Umberson).
Contributor Information
Rachel Donnelly, The University of Texas at Austin.
Debra Umberson, The University of Texas at Austin.
Tetyana Pudrovska, The University of Texas at Austin.
REFERENCES
- Ainsworth-Darnell James W. and Downey Douglas B.. 1998. “Assessing the Oppositional Culture Explanation for Racial/Ethnic Differences in School Performance.” American Sociological Review 63(4):536–553. [Google Scholar]
- Arias Elizabeth, Heron Melonie, and Xu Jiaquan. 2017. “United States Life Tables, 2014” National Vital Statistics Report 66(4). Hyattsville, MD: National Center for Health Statistics. [PubMed] [Google Scholar]
- Bulanda Jennifer Roebuck and Zhang Zhenmei. 2009. “Racial-Ethnic Differences in Subjective Survival Expectations for the Retirement Years.” Research on Aging 31(6):688–709 [Google Scholar]
- Chipperfield Judith G., Perry Raymond P., Pekrun Reinhard, Barchfeld Petra, Lang Frieder R., and Hamm Jeremy M.. 2016. “The Paradoxical Role of Perceived Control in Late Life Health Behavior.” PLoS ONE 11(3): e0148921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummings Tammy H., Hardin James W., Alexander C McLain James R. Hussey, Bennet Kevin J., Wingood Gina M.. 2015. “Modeling Heaped Count Data.” The Stata Journal 15(2):457–479. [Google Scholar]
- Elder Todd E. 2013. “The Predictive Validity of Subjective Mortality Expectations: Evidence from the HRS.” Demography 50:569–589. [DOI] [PubMed] [Google Scholar]
- Elo Irma T. 2009. “Social Class Differentials in Health and Mortality: Patterns and Explanations in Comparative Perspective.” Annual Review of Sociology 35:553–572. [Google Scholar]
- Griffin Barbara, Loh Vanessa, and Hesketh Beryl. 2013. “A Mental Model of Factors Associated with Subjective Life Expectancy.” Social Science & Medicine 82:79–86. [DOI] [PubMed] [Google Scholar]
- Hamermesh Daniel S. 1985. “Expectations, Life Expectancy, and Economic Behavior.” The Quarterly Journal of Economics 100(2):389–408. [Google Scholar]
- Hurd Michael D. and Kathleen McGarry. 1995. “Evaluation of the Subjective Probabilities of Survival in the HRS.” The Journal of Human Resources 30:S268–S292. [Google Scholar]
- Hurd Michael D. and Kathleen McGarry. 2002. “The Predictive Validity of Subjective Probabilities of Survival.” The Economic Journal 112(482):966–985. [Google Scholar]
- Hurd Michael D., Smith James P., and Zissimopoulos Julie M.. 2004. “The Effects of Subjective Survival on Retirement and Social Security Claiming.” Journal of Applied Econometrics 19(6):761–775. [Google Scholar]
- Irby-Shasanmi Amy. 2012. “Predictors of Subjective Life Expectancy Among African Americans.” Research on Aging 35(3):322–347. [Google Scholar]
- Jylhä Marja. 2011. “Self-Rated Health and Subjective Survival Probabilities as Predictors of Mortality” In: Rogers R, Crimmins E (eds). International Handbook of Adult Mortality. International Handbooks of Population (vol 2). Springer, Dordrecht. [Google Scholar]
- Kao Grace and Tienda Marta. 1998. “Educational Aspirations of Minority Youth.” American Journal of Education 106(3):349–384. [Google Scholar]
- Krause Neal, Shaw Benjamin A., and Cairney John. 2004. “A Descriptive Epidemiology of Lifetime Trauma and the Physical Health Status of Older Adults.” Psychology and Aging 19(4):637–648. [DOI] [PubMed] [Google Scholar]
- Lang Frieder R., and Carstensen Laura L.. 2002. “Time Counts: Future Time Perspective, Goals, and Social Relationships.” Psychology and Aging, 17(1):125–139. [DOI] [PubMed] [Google Scholar]
- Lee Sunghee and Smith Jacqui. 2016. “Methodological Aspects of Subjective Life Expectancy: Effects of Culture-Specific Reporting Heterogeneity Among Older Adults in the United States.” Journals of Gerontology: Social Sciences 71(3):558–568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maier E. Hailey and Lachman Margie E. 2000. “Consequences of Early Parental Loss and Separation for Health and Well-Being in Midlife.” International Journal of Behavioral Development 24:183–189. [Google Scholar]
- Marks Nadine F., Jun Heyjung, and Song Jieun. 2007. “Death of Parents and Adult Psychological and Physical Well-Being: A Prospective U.S. National Study.” Journal of Family Issues 28(12):1611–1638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mirowsky John. 1997. “Age, Subjective Life Expectancy, and the Sense of Control: The Horizon Hypothesis.” Journal of Gerontology: Social Sciences 52B(3):S125–S134. [DOI] [PubMed] [Google Scholar]
- Mirowsky John. 1999. “Subjective Life Expectancy in the US: Correspondence to Actuarial Estimates by Age, Sex, and Race.” Social Science & Medicine 49:967–979. [DOI] [PubMed] [Google Scholar]
- Mirowsky John and Ross Catherine E.. 2000. “Socioeconomic Status and Subjective Life Expectancy.” Social Psychology Quarterly 63(2):133–151. [Google Scholar]
- Pearlin Leonard I., Lieberman Morton, Menaghan Elizabeth, and Mullan J 1981. “The Stress Process.” Journal of Health and Social Behavior 22(4):337–356. [PubMed] [Google Scholar]
- Pearlin Leonard I., Schieman Scott, Fazio Elena M., and Meersman Stephen C.. 2005. “Stress, Health, and the Life Course: Some Conceptual Perspectives.” Journal of Health and Social Behavior 46:205–219. [DOI] [PubMed] [Google Scholar]
- Pearlin Leonard I. and Skaff Marilyn McKean 1996. “Stress and the Life Course: A Paradigmatic Alliance.” The Gerontologist 36(2):239–247. [DOI] [PubMed] [Google Scholar]
- Perozek Maria. 2008. “Using Subjective Expectations to Forecast Longevity: Do Survey Respondents Know Something We Don’t Know?” Demography 45(1):95–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pudrovska Tetyana. 2010a. “Cancer and Mastery: Do Age and Cohort Matter?” Social Science & Medicine 71(7):1285–1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pudrovska Tetyana. 2010b. “What Makes You Stronger: Age and Cohort Differences in Personal Growth After Cancer.” Journal of Health and Social Behavior 51(3):260–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pudrovska Tetyana. 2014. “Early-Life Socioeconomic Status and Mortality at Three Life Course Stages: An Increasing Within-Cohort Inequality.” Journal of Health and Social Behavior 55(2):181–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers Richard G., Lawrence Elizabeth M., Hummer Robert A., and Tilstra Andrea M.. 2017. “Racial/Ethnic Differences in Early-Life Mortality in the United States.” Biodemography and Social Biology 63(3):189–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross Catherine E. and Mirowsky John. 2002. “Family Relationships, Social Support, and Subjective Life Expectancy.” Journal of Health and Social Behavior 43(4):469–489. [PubMed] [Google Scholar]
- Scott-Sheldon Lori A., Carey Michael P., Vanable Peter A, and Senn Theresa E.. 2010. “Subjective Life Expectancy and Health Behaviors among STD Clinic Patients.” American Journal of Health Behaviors 34(3):349–361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seeman Melvin & Lewis Susan. 1995. “Powerlessness, Health, and Mortality: A Longitudinal Study of Older Men and Mature Women.” Social Science & Medicine 41(4):517–526. [DOI] [PubMed] [Google Scholar]
- Shonkoff Jack P., Garner Andrew S., The Committee on Psychosocial Aspects of Child and Family Health, Committee on Early Childhood, Adoption, and Dependent Care, Section on Developmental and Behavioral Pediatrics, Siegel Benjamin S., Dobbins Mary I., Earls Marian F., Garner Andrew S., McGuinn Laura, Pascoe John, and Wood David L.. 2012. “The Lifelong Effects of Early Childhood Adversity and Toxic Stress.” Pediatrics 129(1):232–246. [DOI] [PubMed] [Google Scholar]
- Smith Jocelyn R. 2015. “Unequal Burdens of Loss: Examining the Frequency and Timing of Homicide Deaths Experienced by Young Black Men across the Life Course.” American Journal of Public Health 105:S483–S490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith V.Kerry, Taylor Donald H. Jr., and Sloan Frank A. 2001. “Longevity Expectations and Death: Can People Predict Their Own Demise?” The American Economic Review 91(4):1126–1134. [Google Scholar]
- Stroebe Margaret, Schut Henk, and Stroebe Wolfgang. 2007. “Health Outcomes of Bereavement.” Lancet 370(9603):1960–73. [DOI] [PubMed] [Google Scholar]
- Umberson Debra. 2003. Death of a Parent: Transition to a New Adult Identity. New York: Cambridge University Press. [Google Scholar]
- Umberson Debra. 2017. “Black Deaths Matter: Race, Relationship Loss, and Effects on Survivors.” Journal of Health and Social Behavior 58(4):405–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umberson Debra, Liu Hui, and Reczek Corinne. 2008. “Stress and Health Behavior Over the Life Course.” Advances in Life Course Research 13:19–44. [Google Scholar]
- Umberson Debra, Julie Skalamera Olson Robert Crosnoe, Liu Hui, Pudrovska Tetyana, and Donnelly Rachel. 2017. “Death of Family Members as an Overlooked Source of Racial Disadvantage in the United States.” Proceedings of the National Academy of Sciences 114(5):915–920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Utz Rebecca L., Carr Deborah, Nesse Randolph, and Wortman Camille B.. 2002. “The Effect of Widowhood on Older Adults’ Social Participation: An Evaluation of Activity, Disengagement, and Continuity Theories.” The Gerontologist 42(4):522–533. [DOI] [PubMed] [Google Scholar]
- van Doorn Carol and Kasl Stanislav V.. 1998. “Can Parental Longevity and Self-Rated Life Expectancy Predict Mortality Among Older Persons? Results from an Australian Cohort.” Journals of Gerontology: Social Sciences 53B(1):S28–S34. [DOI] [PubMed] [Google Scholar]
- van Solinge Hanna and Henkens Kène. 2017. “Subjective Life Expectancy and Actual Mortality: Results of a 10-year Panel Study among Older Workers.” European Journal of Ageing. Online First. DOI 10.1007/s10433-017-0442-3 [DOI] [PMC free article] [PubMed] [Google Scholar]