Abstract
Background:
Many patients with type 2 diabetes are uncontrolled on maximum oral treatment. The early introduction of insulin can lower diabetes-related complications. This study aimed to evaluate type 2 diabetes patients’ demographic characteristics, clinical factors, and attitude toward insulin therapy initiation.
Methods:
In the present cross-sectional study, 457 patients were selected from 12 diabetes clinics in the southern Iranian city of Shiraz in 2017. Adult patients (>30 y) with type 2 diabetes indicated to use insulin for the first time (insulin-naive) were asked to complete a researcher-designed questionnaire. The data were analyzed using SPSS 19. The relationships between insulin and the tendency to use insulin, demographic characteristics, and clinical data were evaluated using the χ2 or t test and logistic regression. The significance level was considered at 0.05.
Results:
The mean age of the participants was 55.16±8.76 years and 67.4% were female. Despite physician recommendations, 60.2% of the patients were disinclined to use insulin. Those unwilling to initiate insulin therapy had more misconceptions. In the multivariate analysis, the chances of insulin noncompliance were increased by 4.63-fold among the patients without supplementary insurance (P<0.001), by 2.38-fold among those with a nondiabetic diet (P=0.002), and by 6.75-fold among the illiterate ones (P<0.001).
Conclusion:
Based on the results, the factors affecting insulin noncompliance in our insulin-naive patients with type 2 diabetes included insurance coverage, illiteracy, and nondiabetic regimens as well as misconceptions about and irrational fear of insulin injection. Overall, our results indicate the need for further education and financial support for patients and health staff.
Keywords: Diabetes mellitus, Type 2 ; Injections ; Insulin ; Compliance ; Fear
What’s Known
Insulin therapy is the best treatment choice for patients with advanced type 2 diabetes mellitus and suggested for early diabetes. However, patients commonly postpone insulin initiation for several reasons.
What’s New
This study investigated the possible factors influencing patient compliance with insulin therapy vis-à-vis their perspectives, demographic characteristics, disease-related factors, and financial issues in a large sample population. The results can offer researchers and physicians a broad perspective on factors influencing insulin compliance in the target population.
Introduction
Diabetes is the most common and serious chronic disease worldwide with increasing prevalence in the recent decades,1 especially in developing countries.2 Diabetes is associated with several comorbidities and causes several anatomical, structural, and functional changes that lead to multi-organ dysfunction.3 By 2030, diabetes is estimated to be the seventh leading cause of death.4
The most prominent causes of diabetes-related mortality and morbidities include micro- and macrovascular complications,5 commonly found at the time of diagnosis in patients from developing countries.6 Most patients (>90%) suffer from type 2 diabetes,7 and the commonly used treatment for these patients is oral antidiabetic agents. However, fewer than 40% of patients are controlled with oral antidiabetic agents and complications continue to diminish patients’ quality of life and life expectancy.8 In addition, some oral antidiabetic agents are contraindicated in some cases and some may be poorly tolerated.9
Considering the role of insulin resistance and inadequate insulin secretion as the underlying mechanism of the development of type 2 diabetes,10 insulin is prescribed in patients with type 2 diabetes as the most effective antihyperglycemic agent. It improves insulin sensitivity and the metabolic abnormality of diabetes and decreases or eliminates the toxic effects of hyperglycemia.11 Given the favorable effects of insulin, early insulin therapy initiation is suggested as the best treatment method in theory;12 in clinical practice, nonetheless, it is still controversial because its costs outweigh its benefits13 and there is low patient compliance.14
Therapeutic adherence encompasses patient compliance with medication, diet, exercise, and lifestyle alterations.14,15 In patients with type 2 diabetes, patient adherence to oral medication seems to be satisfactory,16,17 while compliance with insulin is poor.18 Thus, it is mandatory to study the factors affecting nonadherence to insulin, not least among patients with type 2 diabetes, with a greater chance of insulin noncompliance than patients with type 1 diabetes.19 The major factors for insulin rejection include patient-perceived barriers, type of the delivery device (pen devices are associated with better compliance), and cost of medication/insurance coverage.20
Noncompliance with insulin initiation is principally due to psychological perceptions among insulin-naive patients with type 2 diabetes: 48% of insulin-naive patients perceived that insulin initiation was in consequence of inadequate response to previous treatment21 and the low efficacy and the probable adverse effects of insulin.22 As a result, it is crucial to identify patients with poor compliance and design strategies to resolve the underlying reasons for noncompliance. Although it is determined that patient perspective is the main factor underlying noncompliance with insulin, it can vary based on financial factors, sociocultural and emotional beliefs, and demographic differences.23 It is, therefore, vitally important that this issue be subjected to rigorous scrutiny in each community.
The present study aimed to evaluate insulin-naive type 2 diabetes patients’ demographic characteristics, clinical factors, and attitude with respect to nonadherence to insulin injection with a view to emphasizing the fundamental role of insulin in the treatment of type 2 diabetes and the factors affecting insulin compliance in this group of patients.
Patients and Methods
In the present cross-sectional study, all patients who referred to 12 diabetes clinics in the southern Iranian city of Shiraz in 2017 were evaluated. The study design was approved by the Ethics Committee of Shiraz University of Medical Sciences (code: IR.SUMS.REC.1395.S1084). Before recruitment in the study, the participants received a thorough explanation of the design and objectives of the study and those willing to participate provided written informed consent.
Among 8376 diabetic patients referring to the center during the study period, 457 patients were selected according to the sample size calculated based on studies considering a rejection rate of insulin of 25%, 95% confidence interval, error of 0.05, and design effect of 1.7.
The inclusion criteria for assessing eligible patients included in the study consisted of a minimum age of 30 years; diagnosis of type 2 diabetes; consumption of oral drugs to control diabetes on maximum doses according to the guidelines of the National and American Diabetes Association (ADA);24 not having ever received any form of insulin (being insulin-naive); having the indication to use insulin for having HbA1c levels equal to or greater than 7.5% (58 mmol/mol); experiencing a diabetes-induced complication such as nephropathy, cardiovascular event, retinopathy, and diabetic foot; and physician recommendation to use insulin. Pregnant or lactating women were not included in the study, and patients who became pregnant during the study period were excluded. In addition, after initial assessment by the physician, patients with dementia or severe mental illnesses such as depression were excluded from the study.
Patients who met the inclusion criteria were selected via the convenient sampling method and were informed about the instrument used in this study, which was a questionnaire. The questionnaire was designed by the researchers based on the expert opinion of clinical specialists and epidemiologists, and after a thorough literature review. It was completed by a trained nurse through face-to-face interviews with the patients. After completing the questions, the nurse would read them to the patient to check whether it was correctly and completely completed.
The questionnaire was comprised of 2 parts. The first part encompassed demographic information such as gender, age, place of residence, educational level, marital status, and insurance coverage as well as the patients’ height, weight, waist circumference measured according to the standard protocols, body mass index calculated and categorized based on the guidelines of the World Health Organization,25 and clinical information on the duration of diabetes, level of HbA1c (% and mmol/mol) in the past 6 months, any diabetes-associated complication, recommended duration of insulin use, diet status, daily physical activities (recorded as high, low, or moderate),26 visiting nutrition consultants, and desire to start insulin therapy. The second part of the questionnaire contained 28 questions on the reasons for insulin noncompliance, which was designed in 2 dimensions. The first dimension comprised factors other than insulin (sociocultural factors) and the second dimension covered factors related to insulin, which were scored based on a 5-point Likert scale as follows: (1) strongly disagree, (2) disagree, (3) undecided, (4) agree, and (5) strongly agree.
The validity of this questionnaire at the beginning and after the initial design was determined through a review by 5 professors, epidemiologists, and experts on diabetes at Shiraz University of Medical Sciences and their comments were applied in the questionnaire. All of the experts approved the questionnaire after the application of the recommended changes.
The reliability and the internal consistency of the questionnaire were evaluated using test-retest and Cronbach’s alpha. First, the reliability was estimated via the test-retest method. In other words, the questionnaire was completed by 20 patients with type 2 diabetes who referred to the Diabetes Center of Motahhari Clinic, Shiraz, and was subsequently completed by the same patients after 2 weeks. The reliability of the questionnaire was estimated at 0.91 and the Cronbach’s alpha was calculated at 0.92.
The relationships between insulin and the tendency to use insulin, demographic characteristics, and clinical data were evaluated using the χ2 or the t test. A logistic regression model was employed to evaluate the effects of the demographic characteristics and the clinical variables on the tendency to use insulin. Analysis was conducted in this model via the forward Wald method. Following data collection, statistical software SPSS, version 19, was used (IBM SPSS Statistics for Windows, Armonk, NY: IBM Corp.). The significance level was considered at 0.05.
Results
Among the 457 adult patients with diabetes recruited into the current study, 67.4% (n=308) were female and the mean age of the participants was 55.16±8.76 years. The mean duration of diabetes was 10.43±5.79 years, and the mean HbA1c level was 8.92% (74 mmol/mol).
The medications used for diabetes control, as well as the anthropometric and demographic characteristics, are shown in table 1.
Table 1.
Demographic and clinical characteristics of the participants
| Qualitative Characteristics | No. (%) | Quantitative Characteristics | Mean±SD |
|---|---|---|---|
| Gender | Age (y) | 55.16±8.76 | |
| Woman | 308 (67.4) | Range (min-max) | 49.00 (34.00-83.00) |
| Man | 149 (32.6) | ||
| Marital status | Duration diabetes (y) | 10.43±5.79 | |
| Unmarried | 107 (23.4) | Range (min-max) | 30.00 (2.00-32.00) |
| Married | 350 (76.6) | ||
| Educational level | Duration of insulin, as suggested by the physician (mon) | 3.40±2.50 | |
| Illiterate | 136 (29.8) | ||
| Non-academic | 244 (53.4) | ||
| Academic | 77 (16.8) | Range (min-max) | 23.00 (1.00-24.00) |
| Place of residence | Height (cm) | 166.42±8.35 | |
| Rural | 73 (16.0) | Range (min-max) | 49.00 (140.00-189.00) |
| Urban | 384 (84.0) | ||
| Supplementary insurance | Weight (kg) | 73.47±11.02 | |
| No | 349 (76.4) | Range (min-max) | 77.00 (48.00-125.00) |
| Yes | 108 (23.6) | ||
| Consulting nutritionist | BMI (kg/M2) | 26.46±2.93 | |
| No | 281 (61.5) | Range (min-max) | 22.3 (18.5-40.4) |
| Yes | 176 (38.5) | ||
| Diet | Waist/hip ratio: | ||
| Normal family diet | 362 (79.2) | Men | 1.12±0.07 |
| Diabetic regimen | 95 (20.8) | Women | 0.88±0.03 |
| Physical activities | HbA1c (%) | 8.92±1.01 | |
| Irregular | 364 (79.6) | Range (min-max) | 6.30 (7.50-13.80) |
| Regular (>50 min/d) | 93 (20.4) | ||
| BMI (kg/M2) | HbA1c (mmol/mmol) | 74 | |
| Normal | 129 (28.2) | Median (range) | 45 (69) |
| Overweight | 283 (61.9) | ||
| Class 1 obesity | 36 (7.9) | ||
| Class 2 obesity | 9.0 (2.0) | ||
| Medications | |||
| Metformin | 457 (100) | ||
| Glibenclamide | 295 (64.6) | ||
| Acarbose | 148 (32.4) | ||
| Aspirin | 114 (24.9) | ||
| Complications | |||
| Nephropathy | 142 (31.1) | ||
| Cardiovascular events | 104 (22.8) | ||
| High blood pressure | 286 (62.6) | ||
| Retinopathy | 148 (32.4) | ||
| Diabetic foot | 54 (11.8) | ||
| Just 1 complication | 246 (53.8) | ||
| 2 complications | 147 (32.2) | ||
| 3 or more complications | 64 (14.0) | ||
BMI: Body mass index
The most common complication was hypertension (62.6%), followed by nephropathy in 31.1% of the study population, cardiovascular events in 22.8%, and retinopathy in 32.4%. Diabetic foot was present only in 11.8% of the patients. Only 53.8% of the study population had 1 complication, while 2 simultaneous complications and more than 3 concurrent complications were observed in 32.2% and 14% of the patients.
Apropos of insulin compliance, 60.2% of the patients were disinclined to use insulin, despite the recommendation of their treating physician. A variety of variables were significantly associated with patient compliance with insulin use such as age, gender, marital status, educational level, place of residence, supplementary insurance, consulting nutritionists, diet, and physical activities (P<0.001), as well as the duration of diabetes (P=0.025). Among these factors, only the duration of insulin use as suggested by the treating physician did not have a statistically significant association with patient compliance with insulin use (P=0.306) (table 2).
Table 2.
Univariate analysis and multivariate logistic regression analysis predicting hypothetical noncompliance with insulin injection
| Variable | Univariate Analysis* | Multivariate Analysis** | ||||
|---|---|---|---|---|---|---|
| OR‡ | 95% CI | P | OR‡ | 95% CI | P | |
| Gender | 0.049a | 0.887 | ||||
| Man | ||||||
| Woman | 1.48 | (1.23-2.05) | 1.09 | (0.51-1.50) | ||
| Marital status | <0.001a | 0.125 | ||||
| Married | ||||||
| Unmarried | 2.66 | (1.89-4.36) | 1.32 | (0.75-2.33) | ||
| Educational level | <0.001a | |||||
| Academic | ||||||
| Non-academic | 6.25 | (4.28-7.78) | 1.79 | (1.08-2.95) | 0.022 | |
| Illiterate | 12.06 | (9.18-16.25) | 6.75 | (3.08-14.76) | <0.001 | |
| Place of residence | 0.002a | 0.703 | ||||
| Urban | ||||||
| Rural | 2.48 | (1.98-3.42) | 1.08 | (0.56-2.09) | ||
| Supplementary insurance | <0.001a | |||||
| Yes | ||||||
| No | 8.96 | (6.50-15.22) | 4.63 | (2.60-8.25) | <0.001 | |
| Consulting nutritionist | <0.001a | 0.174 | ||||
| Yes | ||||||
| No | 2.83 | (1.46-3.58) | 1.28 | (0.68-2.18) | ||
| Diet | <0.001a | |||||
| Diabetic regimen | ||||||
| Normal family diet | 3.57 | (2.18-6.48) | 2.38 | (1.38-4.09) | 0.002 | |
| Physical activities | <0.001a | 0.102 | ||||
| Regular (>50 min/d) | ||||||
| Irregular | 3.20 | (2.36-6.88) | 1.79 | (1.23-3.05) | ||
| Quantitative characteristics | Group 1 | Group 2 | P | |||
| Age (y), mean ± SD| | 53.92±8.94 | 55.98±8.55 | 0.014b | 0.99 | (0.97-1.01) | 0.232 |
| Duration of diabetes (y), mean ± SD| | 9.69±5.58 | 10.93±5.89 | 0.025b | 1.02 | (0.96-1.06) | 0.395 |
| Duration of insulin use (mon), suggested by the physician, mean ± SD | 3.54±3.41 | 3.30±1.65 | 0.306b | - | - | - |
P value based on the χ2 and t test;
P value based on logistic regression;
Results of the χ2 test;
Results of the t test;
Group 1: The group willing to start insulin; Group 2: The group unwilling to start insulin
As is demonstrated in table 2, the female patients, unmarried patients, and those living in rural areas were more reluctant to use insulin. Additionally, the likelihood of nonadherence to insulin use was significantly higher among the patients who did not consult a nutritionist and did not keep the diabetic diet, as well as among those without regular physical activities (P<0.001).
Our multivariate logistic regression demonstrated not having supplementary insurance, being illiterate, and having a routine family diet (nondiabetic) increased the chance of noncompliance (table 2).
Considering the scores of the second part of the questionnaire, as is demonstrated in table 3, the participants who were reluctant to use insulin scored all the questions higher in both dimensions (insulin-related and sociocultural factors) with a mean score of higher than 3.5 in almost all the questions (P<0.001). After comparing the mean scores of the items in the questionnaire, we compared the total mean score between the unwilling and willing patients with respect to insulin therapy initiation (figure 1).
Table 3.
Comparison of the responses to the items in the questionnaire on insulin compliance in patients with type 2 diabetes between the willing and unwilling patients
| Dimensions and Factors Affecting Insulin Rejection | Group Willing to Start Insulin* Mean±SD (n=182) | Group Unwilling to Start Insulin* Mean±SD (n=275) | P | |
|---|---|---|---|---|
| First dimension: Non-insulin (sociocultural) factors | Experiences of others regarding insulin | 2.02±0.67 | 3.97±0.83 | <0.001 |
| I hear that insulin can hurt family members because of needle use. | 2.04±0.66 | 3.93±0.90 | <0.001 | |
| Dependence on others due to insulin use | 2.03±0.84 | 4.17±0.83 | <0.001 | |
| Others’ expressed regrets about taking insulin | 1.88±0.79 | 3.89±0.90 | <0.001 | |
| Believing that insulin is addictive | 2.02±0.96 | 3.83±0.80 | <0.001 | |
| Some people believe that insulin is less efficient than oral medication | 1.62±0.74 | 3.74±0.86 | <0.001 | |
| Threatening behavior of physicians | 2.42±1.01 | 3.49±1.09 | <0.001 | |
| Preferring complementary medicine (e.g., acupuncture and herbal medicines) | 2.18±0.86 | 4.22±0.87 | <0.001 | |
| Waiting for a new treatment method | 2.31±0.85 | 3.43±0.80 | <0.001 | |
| Believing that it is not necessary to start insulin treatment | 1.68±0.91 | 3.94±0.74 | <0.001 | |
| Difficulty in injection due to aging and disability | 1.95±0.87 | 3.53±0.96 | <0.001 | |
| Being alone | 1.81±0.80 | 3.25±0.90 | <0.001 | |
| Embarrassment, especially in public, because of the use of insulin | 1.59±0.71 | 3.09±1.03 | <0.001 | |
| Social stigma attached to insulin use and abhorrence thereof | 1.51±0.70 | 3.01±1.05 | <0.001 | |
| Believing that there is no more hope of recovery after insulin use | 1.47±0.59 | 3.32±0.96 | <0.001 | |
| Believing that insulin impairs children’s future | 1.44±0.58 | 3.00±0.94 | <0.001 | |
| first dimension (16 items)‡ | 29.95±6.49 | 57.81±6.43 | <0.001 | |
| .sulin-related factors | Additional costs caused by taking insulin | 2.47±1.08 | 3.82±0.79 | <0.001 |
| Difficulty of keeping insulin | 2.17±0.86 | 4.00±0.69 | <0.001 | |
| Inconveniency of carrying needles and syringes and keeping insulin cool, especially on trips | 2.16±0.89 | 4.10±0.70 | <0.001 | |
| Variability of insulin types and forgetting insulin injections | 2.13±0.69 | 4.04±0.70 | <0.001 | |
| Pain, injuries, and bruises at the injection site | 2.23±0.94 | 3.98±0.63 | <0.001 | |
| Believing that insulin injection leads to renal failure | 2.23±0.82 | 3.38±0.82 | <0.001 | |
| Infection or other complications after injection | 2.09±0.64 | 3.73±0.73 | <0.001 | |
| Coma due to an unbalanced use of insulin and severe drop in blood sugar | 2.12±0.70 | 3.73±0.76 | <0.001 | |
| Sudden death caused by taking insulin | 2.01±0.71 | 3.56±0.88 | <0.001 | |
| Difficulty of learning the correct method of injection | 2.08±0.82 | 4.23±0.82 | <0.001 | |
| Fear of correct injection method and dosage | 2.08±0.87 | 4.29±0.82 | <0.001 | |
| Fear of needles | 2.02±0.94 | 4.19±1.06 | <0.001 | |
| Total second dimension (12 items)§ | 25.78±5.82 | 47.05±5.92 | <0.001 | |
| Total of both dimensions (28 items)|| | 55.73±11.08 | 104.86±11.47 | <0.001 |
Scores from 1 to 5;
Range of 16 to 80;
Range of 12 to 60;
Range of 28 to 140
Figure1.
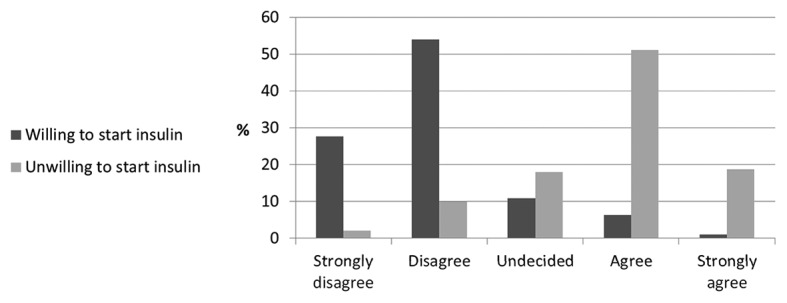
Overall spectrum of agreement (%) with the factors that can foster reluctance to commence insulin therapy.
Discussion
We studied 457 patients, mainly consisting of women (67.4%), with type 2 diabetes who were eligible to receive insulin for the first time (after taking oral drugs for several years) due to uncontrolled glycemic state (HbA1c levels ≥7.5%) and diabetes-induced complications, despite taking oral drugs for several years (mean duration=10.43±5.79 y). The mean age of the study population was 55.16±8.76 years, and the mean HbA1c level was 8.92% (74 mmol/mol). The results showed a high prevalence of insulin therapy refusal in our study patients (60.2%), despite the recommendation of their treating physician.
The percentage of nonadherence to insulin therapy in patients with type 2 diabetes varies among the studies in the existing literature. A study on 1400 insulin-naive type 2 diabetes patients in a western country found that 17.2% were unwilling to start insulin and 34.7% were ambivalent (i.e., 48% of the patients were willing to start insulin),27 while in the present study, fewer than 40% of the patients were willing to commence insulin therapy. The disparities in the results may be due to sociocultural and financial differences among nations as well as demographic dissimilarities among the samples recruited in different studies (e.g. male-to-female ratio of the included population and duration of diabetes).
A review study previously reported that the rate of patient compliance differed between the insulin-naive and insulin-experienced patients and that the patients with prior insulin experience had fewer injection-related concerns about the burden of insulin progression than their insulin-naive counterparts.28 Another investigation revealed that the insulin-experienced patients had greater fear of the adverse effects of insulin and weight gain, whereas the insulin-naive patients had greater fear of needles and injection-related difficulties,29 which is concordant with the results of the present study, revealing that the most important insulin-related factors in the insulin-naive patients were fear of needles and difficulty in learning the correct method of injection. Similarly, another study suggested that fewer injections and more user-friendly devices such as insulin pens could augment the chance of insulin compliance among insulin-naive patients.30
The results of the present study also revealed that among sociocultural factors affecting patients’ unwillingness to start insulin, the belief that it is not necessary to commence insulin treatment played an important role besides the fear of social rejection. Therefore, involving patients in their treatment process, considering their concerns, and explaining the progressive nature of diabetes and the value of insulin can be effective education strategies.31 Also deemed an effectual educational method for the improvement of patient compliance is the education of insulin-naive patients with type 2 diabetes about the disease and its complications, benefits of insulin, correct insulin injection method, and user-friendly insulin injection devices.28,31,32 In view of the favorable perspective of patients with type 2 diabetes with the experience of insulin injection28,29 and the efficacy of peer-group education in diabetes self-care,33 it can be argued that the peer education of insulin-naive patients by insulin-experienced patients can be an effective measure to increase their adherence to insulin therapy. Nevertheless, even effective educational methods cannot completely eliminate the rate of patient noncompliance with insulin.28 According to the results of the present study, the main issues vis-à-vis insulin therapy refusal were false beliefs, irrational fears, and misconceptions, known as needle/injection phobia.34-36 Consequently, it is essential to determine the fundamental factors underlying such perspectives in patients.
In the present study, aside from the patient-related factors and sociocultural factors affecting the patients’ perspective on insulin initiation, we investigated the demographic, financial, and disease-related factors and found that the patients without supplementary insurance had a 4.63-fold increased chance of being reluctant to use insulin. This finding is consistent with previous research, indicating income and health insurance as effective factors in the compliance of patients with the treatment for type 2 diabetes.14,37 Hence, patient-friendly insulin devices and insulin types with fewer injections that are under insurance coverage can enhance patient compliance in the target population.
In addition, studies have revealed that attachment to lifestyle modification plays an important role in diabetes control and nonadherence to lifestyle recommendations in patients with type 2 diabetes can affect the treatment outcome,15 which chimes in with the results of the present study inasmuch as the patients with a nondiabetic diet had a 2.38-fold increase in the likelihood of reluctance to use insulin. Such findings highlight the significant role of education of type 2 diabetes patients in relation to diet and other lifestyle changes. Moreover, we found a 6.75-fold increased chance of insulin initiation refusal among our illiterate patients, which emphasizes the need for designing simple and easy-to-understand educational materials for the illiterate diabetic population.38 As previous investigations have reported poor glycemic control among diabetic patients, it is necessary that physicians pay greater attention to illiterate patients and bring to bear more patience in their education with a view to attaining favorable treatment results. 39,40
As evidence suggests, patients with type 2 diabetes have lower insulin compliance than patients with type 1 diabetes,19 and among patients with type 2 diabetes, insulin-naive patients tend to exhibit less willingness to initiate insulin therapy than patients with the experience of insulin injection.28,29 Accordingly, this target group (insulin-naive patients with type 2 diabetes) requires great attention.
First and foremost among the limitations of the present study is that the data were obtained only from public, and not private, diabetes centers. Needless to say, this limits the generalizability of the results to the whole Iranian population, although the selected diabetes clinics were referral centers. Moreover, the fact that the study design was cross-sectional precluded the extrapolation of causative relations and the results were presented as mere associations. It is critical that the origin of patient misconceptions in regard to insulin therapy be fully explored in order that guidelines can be devised on how to prevent fear of insulin among diabetic patients. Indeed, as some patients in the current study stated, sometimes treating physicians tend to discourage their patients from insulin use in favor of oral therapy. One salient omission in the list of reasons for insulin rejection was insulin-induced obesity, which is absent in table 3. We recommend that this omission be addressed in future studies.
Conclusion
In light of the findings of the present study, we conclude that factors responsible for insulin noncompliance among insulin-naive patients with type 2 diabetes include insurance coverage, illiteracy, nondiabetic diet regimens, and fear of insulin injection or insulin-phobia, all of which indicate the need for patient education and financial support.
Acknowledgement
The present study is partially obtained from the results of Hamed Delam’s dissertation at Shiraz University of Medical Sciences (Code: 95/12448). Many thanks are due to Dr. Hamid Zare as well as the managers and medical staff of the studied clinics for their assistance in data collection in the present project. We also hereby express our gratitude to Shiraz University of Medical Sciences for its financial support.
Conflict of Interest:None declared.
References
- 1.Danaei G, Finucane MM, Lu Y, Singh GM, Cowan MJ, Paciorek CJ, et al. National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2.7 million participants. Lancet. 2011;378:31–40. doi: 10.1016/S0140-6736(11)60679-X. [DOI] [PubMed] [Google Scholar]
- 2.Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010;87:4–14. doi: 10.1016/j.diabres.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 3.Rahman S, Rahman T, Ismail AA, Rashid AR. Diabetes-associated macrovasculopathy: pathophysiology and pathogenesis. Diabetes Obes Metab. 2007;9:767–80. doi: 10.1111/j.1463-1326.2006.00655.x. [DOI] [PubMed] [Google Scholar]
- 4.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3:e442. doi: 10.1371/journal.pmed.0030442. [ PMC Free Article] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cade WT. Diabetes-related microvascular and macrovascular diseases in the physical therapy setting. Phys Ther. 2008;88:1322–35. doi: 10.2522/ptj.20080008. [ PMC Free Article] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chowdhury TA, Lasker SS. Complications and cardiovascular risk factors in South Asians and Europeans with early-onset type 2 diabetes. QJM. 2002;95:241–6. doi: 10.1093/qjmed/95.4.241. [DOI] [PubMed] [Google Scholar]
- 7.Tripathi BK, Srivastava AK. Diabetes mellitus: complications and therapeutics. Med Sci Monit. 2006;12:RA130–47. [PubMed] [Google Scholar]
- 8.Koro CE, Bowlin SJ, Bourgeois N, Fedder DO. Glycemic control from 1988 to 2000 among U. S. adults diagnosed with type 2 diabetes: a preliminary report Diabetes Care 2004;27:17–20. doi: 10.2337/diacare.27.1.17. [DOI] [PubMed] [Google Scholar]
- 9.Pfeiffer AF, Klein HH. The treatment of type 2 diabetes. Dtsch Arztebl Int. 2014;111:69–81. doi: 10.3238/arztebl.2014.0069. [ PMC Free Article] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. American Diabetes Association. Diagnosis and Classification of Diabetes Mellitus. Diabetes Care. 2010;33(Suppl 1):S62–S69. doi: 10.2337/dc10-S062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wu Y, Ding Y, Tanaka Y, Zhang W. Risk factors contributing to type 2 diabetes and recent advances in the treatment and prevention. Int J Med Sci. 2014;11:1185–200. doi: 10.7150/ijms.10001. [ PMC Free Article] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Meneghini LF. Early insulin treatment in type 2 diabetes: what are the pros? Diabetes Care. 2009;32:S266–9. doi: 10.2337/dc09-S320. [ PMC Free Article] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Davidson MB. Early insulin therapy for type 2 diabetic patients: more cost than benefit. Diabetes Care. 2005;28:222–4. doi: 10.2337/diacare.28.1.222. [DOI] [PubMed] [Google Scholar]
- 14.Jin J, Sklar GE, Min Sen Oh, V Chuen, Li S. Factors affecting therapeutic compliance: A review from the patient’s perspective. Ther Clin Risk Manag. 2008;4:269–86. doi: 10.2147/tcrm.s1458. [ PMC Free Article] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mumu SJ, Saleh F, Ara F, Afnan F, Ali L. Non-adherence to life-style modification and its factors among type 2 diabetic patients. Indian J Public Health. 2014;58:40–4. doi: 10.4103/0019-557X.128165. [DOI] [PubMed] [Google Scholar]
- 16.Grant RW, Devita NG, Singer DE, Meigs JB. Polypharmacy and medication adherence in patients with type 2 diabetes. Diabetes Care. 2003;26:1408–12. doi: 10.2337/diacare.26.5.1408. [DOI] [PubMed] [Google Scholar]
- 17.Donnan PT, MacDonald TM, Morris AD. Adherence to prescribed oral hypoglycaemic medication in a population of patients with Type 2 diabetes: a retrospective cohort study. Diabet Med. 2002;19:279–84. doi: 10.1046/j.1464-5491.2002.00689.x. [DOI] [PubMed] [Google Scholar]
- 18.Rubin RR. Adherence to pharmacologic therapy in patients with type 2 diabetes mellitus. Am J Med. 2005;118:27S–34S. doi: 10.1016/j.amjmed.2005.04.012. [DOI] [PubMed] [Google Scholar]
- 19.Farsaei S, Radfar M, Heydari Z, Abbasi F, Qorbani M. Insulin adherence in patients with diabetes: risk factors for injection omission. Prim Care Diabetes. 2014;8:338–45. doi: 10.1016/j.pcd.2014.03.001. [DOI] [PubMed] [Google Scholar]
- 20.Davies MJ, Gagliardino JJ, Gray LJ, Khunti K, Mohan V, Hughes R. Real-world factors affecting adherence to insulin therapy in patients with Type 1 or Type 2 diabetes mellitus: a systematic review. Diabet Med. 2013;30:512–24. doi: 10.1111/dme.12128. [DOI] [PubMed] [Google Scholar]
- 21.Peyrot M, Rubin RR, Khunti K. Addressing barriers to initiation of insulin in patients with type 2 diabetes. Prim Care Diabetes. 2010;4:S11–8. doi: 10.1016/S1751-9918(10)60004-6. [DOI] [PubMed] [Google Scholar]
- 22.Woudenberg YJ, Lucas C, Latour C, Scholte op Reimer WJ. Acceptance of insulin therapy: a long shot? Psychological insulin resistance in primary care. Diabet Med. 2012;29:796–802. doi: 10.1111/j.1464-5491.2011.03552.x. [DOI] [PubMed] [Google Scholar]
- 23.Brundisini F, Vanstone M, Hulan D, DeJean D, Giacomini M. Type 2 diabetes patients’ and providers’ differing perspectives on medication nonadherence: a qualitative meta-synthesis. BMC Health Serv Res. 2015;15:516. doi: 10.1186/s12913-015-1174-8. [ PMC Free Article] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. American Diabetes A. 8. Pharmacologic Approaches to Glycemic Treatment. Diabetes Care. 2017;40:S64–S74. doi: 10.2337/dc17-S011. [DOI] [PubMed] [Google Scholar]
- 25. Global Database on Body Mass Index: BMI classification [Internet] . Geneva: World Health Organization. c2006- [cited 2016 June 24] . Available from: [http://www.assessmentpsychology.com/icbmi.htm. ] [Google Scholar]
- 26.Aune D, Norat T, Leitzmann M, Tonstad S, Vatten LJ. Physical activity and the risk of type 2 diabetes: a systematic review and dose-response meta-analysis. Eur J Epidemiol. 2015;30:529–42. doi: 10.1007/s10654-015-0056-z. [DOI] [PubMed] [Google Scholar]
- 27.Polonsky WH, Hajos TR, Dain MP, Snoek FJ. Are patients with type 2 diabetes reluctant to start insulin therapy? An examination of the scope and underpinnings of psychological insulin resistance in a large, international population. Curr Med Res Opin. 2011;27:1169–74. doi: 10.1185/03007995.2011.573623. [DOI] [PubMed] [Google Scholar]
- 28.Polinski JM, Smith BF, Curtis BH, Seeger JD, Choudhry NK, Connolly JG, et al. Barriers to insulin progression among patients with type 2 diabetes: a systematic review. Diabetes Educ. 2013;39:53–65. doi: 10.1177/0145721712467696. [DOI] [PubMed] [Google Scholar]
- 29.Casciano R, Malangone E, Ramachandran A, Gagliardino JJ. A quantitative assessment of patient barriers to insulin. Int J Clin Pract. 2011;65:408–14. doi: 10.1111/j.1742-1241.2010.02590.x. [DOI] [PubMed] [Google Scholar]
- 30.Ratanawongsa N, Crosson JC, Schillinger D, Karter AJ, Saha CK, Marrero DG. Getting under the skin of clinical inertia in insulin initiation: the Translating Research Into Action for Diabetes (TRIAD) Insulin Starts Project. Diabetes Educ. 2012;38:94–100. doi: 10.1177/0145721711432649. [ PMC Free Article] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Petznick AM. Identifying and addressing barriers to insulin acceptance and adherence in patients with type 2 diabetes mellitus. J Am Osteopath Assoc. 2013;113:S6–16. [PubMed] [Google Scholar]
- 32.Cani CG, Lopes Lda S, Queiroz M, Nery M. Improvement in medication adherence and self-management of diabetes with a clinical pharmacy program: a randomized controlled trial in patients with type 2 diabetes undergoing insulin therapy at a teaching hospital. Clinics (Sao Paulo) 2015;70:102–6. doi: 10.6061/clinics/2015(02)06. [ PMC Free Article] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Qi L, Liu Q, Qi X, Wu N, Tang W, Xiong H. Effectiveness of peer support for improving glycaemic control in patients with type 2 diabetes: a meta-analysis of randomized controlled trials. BMC Public Health. 2015;15:471. doi: 10.1186/s12889-015-1798-y. [ PMC Free Article] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Karter AJ, Subramanian U, Saha C, Crosson JC, Parker MM, Swain BE, et al. Barriers to insulin initiation: the translating research into action for diabetes insulin starts project. Diabetes Care. 2010;33:733–5. doi: 10.2337/dc09-1184. [ PMC Free Article] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shahid M, Sarfraz A, Shaikh S, Mahar SA, Alam M, Shahid N. Perception of Diabetic Patients Regarding Basal Bolus Insulin Injections and Outcome of its Use. J Coll Physicians Surg Pak. 2016;26:177–81. [PubMed] [Google Scholar]
- 36.Fu SN, Wong CK, Chin WY, Luk W. Association of more negative attitude towards commencing insulin with lower glycosylated hemoglobin (HbA1c) level: a survey on insulin-naive type 2 diabetes mellitus Chinese patients. J Diabetes Metab Disord. 2015;15:3. doi: 10.1186/s40200-016-0223-0. [ PMC Free Article] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hertz RP, Unger AN, Lustik MB. Adherence with pharmacotherapy for type 2 diabetes: a retrospective cohort study of adults with employer-sponsored health insurance. Clin Ther. 2005;27:1064–73. doi: 10.1016/j.clinthera.2005.07.009. [DOI] [PubMed] [Google Scholar]
- 38.de Oliveira SMS, Guimarães DB, Reis JS, editors Illiteracy and diabetes: educational program for people with type 2 diabetes in the public health system. Diabetol Metab Syndr. 2015;7:A177. [Google Scholar]
- 39.Souza JG, Apolinario D, Magaldi RM, Busse AL, Campora F, Jacob-Filho W. Functional health literacy and glycaemic control in older adults with type 2 diabetes: a cross-sectional study. BMJ Open. 2014;4:e004180. doi: 10.1136/bmjopen-2013-004180. [ PMC Free Article] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Garcia AA, Zuniga J, Reynolds R, Cairampoma L, Sumlin L. Evaluation of the spoken knowledge in low literacy in diabetes scale for use with Mexican Americans. J Transcult Nurs. 2015;26:279–86. doi: 10.1177/1043659614524246. [ PMC Free Article] [DOI] [PMC free article] [PubMed] [Google Scholar]


