The combination of at least three autoimmune diseases in the same patient has been defined as multiple autoimmune syndrome (MAS) type (1-3).
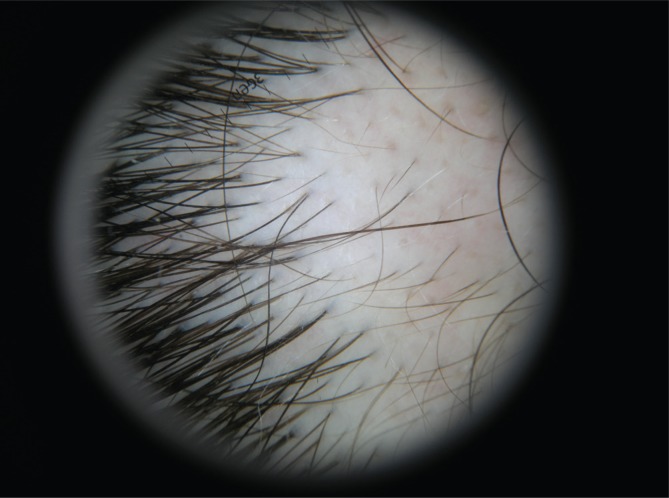
A 39 years old woman presented for white patches around the nail discovered after a manicure cosmetic procedure four months before and a localized area of hair loss observed one month before. Patient had a history of previous infectious mononucleosis in infancy and autoimmune thyroiditis for about five years without any family history of vitiligo, alopecia areata or other autoimmune disease. Clinical evaluation revealed sharp demarcated white patches around the fingernails of the hand (Fig.1a) and a sharp demarcated patch of hair loss on the scalp area (Fig.1b). Dermoscopy showed white circular sharp demarcated areas near fingernail (Fig. 2a) and “exclamation mark” hairs, atrophic hairs, yellow dots and slight pink areas between hairs on scalp (Fig. 2b). The thyroid ultrasound showed heterogeneous thyroid echotexture. Blood tests showed ATPO= 203.4UI/mL (N=0-34UI/mL), TSH=2.9 mUI/L (N=0.4-4 uUI/mL), fT4=1.43 ng/dL (N= 0.98-1.63 ng/dL). The tests for Ebstein Barr virus were VCA – IgM antibodies 2U/mL, (positive >40 U/mL), VCA – IgG antibodies positive= 35 U/mL (negative < 20 U/mL). Other laboratory findings like immunoglobulins were normal, anti-nuclear antibodies absent, circulating immune complexes 18 RU/mL(N <20 RU/mL), total complement CH 100 80 UI/mL (N= 40-200UI/mL) and C3 complement 110 mg/dL (N=90-180 d/L). The diagnostic of MAS Type III was made on the association of autoimune thyroiditis, vitiligo and alopecia areata. The differential diagnosis was made with: traction alopecia – lack of the blood drops on dermoscopy, negative anamnesis; localized cicatriceal alopecia - dermoscopy showed dots (pores, no atrophy) and “exclamation mark” hairs; Tinea capitis - there were no scales, dermoscopic “comma hairs” were absent and the direct microscopical mycological exam of the hair shaft and mycological culture were negative. The histopathological examination was not performed due the fact that the patient had dermoscopic pathognomonic features of alopecia areata. Examined first in dermatology, the patient was referred to the endocrinologist for further investigations and monitoring the values of Thyroid-Stimulating Immunoglobulin (TSI), antithyroid microsomal and thyroglobulin antibodies, thyrotropin receptor autoantibodies (TSHR). She has been treated with levothyroxine for five years, with a 25 mcg daily dose. For alopecia areata of the scalp we prescribed topical treatment with tacrolimus 0.1% ointment twice per week (weekends) in alternance with a mild potency topical steroid methylprednisolone aceponate 0.1% ointment 4 days/week. Vitiligo areas around the nails were treated only by the tacrolimus under occlusion. After two months of treatment alopecia areata improved but vitiligo areas remained unchanged. Vitiligo and alopecia areata suggest a similar pathogenesis, and may depend on any number of mechanisms due to the close proximity of melanocytes and hair follicles within the skin, including localized epitope spreading during inflammation, or the targeting of melanocytes both in the epidermis as well as the hair follicle(1)(2). The treatment options for both skin diseases were (1-3): systemic corticotherapy, very potent topical steroids, PUVA therapy, UVB narrow band therapy, Excimer laser, or novel targeted immunotherapies like oral tofacitinib, topical ruxolitinib,ustekinumab (3). We prescribed UVB narrow band therapy (ultraviolet B radiation with a wavelength of 311 nm) for 12 weeks and topical clobetasol dipropionate at 0.1% bid for 5 days then once per day for 10 days then every other day for 10 days and progressive taper for another month.
Figure 1.
a. White patches arround fingernails.
Figure 1.
b. Alopecia areata of the scalp.
Figure 2.
a. Dermoscopy - White circular areas near fingernail.
Figure 2.
b. Dermoscopy of Alopecia Areata.
Clinical and dermoscopy follow-up of the brown dots on the central vitiligo areas (islands of repigmentation) was performed every 3 months. For alopecia areata that were assessed clinically and dermoscopically peri-lesional and lesional area hairs (exclamation mark hairs and dots). The therapy response for both alopecia areata and vitiligo could be seen at six to twelve months (3).
The order of appearance of patient’s autoimmune diseases was: thyroiditis (five years previously), vitiligo and alopecia areata (four months previously). This underlines the importance of systematic screen for thyroid autoimmune disease when dermatological autoimmune diseases are diagnosed .
In conclusion, association of several autoimmune diseases can be complex, complete clinical examination and laboratory tests are important for the diagnosis of multiple autoimmune syndrome as in this rare case report of thyroiditis, vitiligo and alopecia areata.
Conflict of interest
The authors declare that they have no conflict of interest concerning this article.
References
- 1.McElwee KJ, Gilhar A, Tobin DJ, Ramot Y, Sundberg JP, Nakamura M, Bertolini M, Inui S, Tokura Y, King LE, Jr, Duque-Estrada B, Tosti A, Keren A, Itami S, Shoenfeld Y, Zlotogorski A, Paus R. What causes alopecia areata? Exp Dermatol. 2013;22:609–626. doi: 10.1111/exd.12209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Harris JE. VIEWPOINT – Vitiligo and alopecia areata: Apples and oranges? Exp Dermatol. 2013;22(12) doi: 10.1111/exd.12264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rork JF, Rashighi M, Harris JE. Autoimmunity of vitiligo and alopecia areata. Curr Opin Pediatr. 2016;28(4):463–469. doi: 10.1097/MOP.0000000000000375. [DOI] [PMC free article] [PubMed] [Google Scholar]