Abstract
Objectives:
To investigate the associations between household wealth, household consumption, and chronic disease risk behaviors among older adults in rural South Africa.
Methods:
Data were from baseline assessments of 5,059 adults aged ≥40 in the population-based “Health and Aging in Africa: A Longitudinal Study of an INDEPTH Community in South Africa” (HAALSI) in 2015. Confounder-adjusted prevalence ratios were estimated for the associations between each of household wealth and household consumption quintiles with low moderate-to-vigorous physical activity (MVPA), current smoking, frequent alcohol intake, and overweight/obese body mass index (BMI).
Results:
Low MVPA and overweight/obese BMI were common (57% and 58%, respectively), and linearly increased in prevalence across household wealth quintiles. Low MVPA decreased and overweight/obese BMI increased in prevalence across household consumption quintiles. Smoking and frequent alcohol intake were rare (9% and 6%, respectively); they decreased in prevalence across wealth quintiles but did not vary by consumption quintile.
Conclusions:
Chronic disease risk behaviors are socioeconomically graded among older, rural South African adults. The high prevalence of overweight and obesity in rural South Africa is a public health concern requiring urgent attention.
INTRODUCTION
The population of South Africa is rapidly aging. Life expectancy at birth in 2015 was 59.0 years for men and 66.0 years for women, an increase of more than 10 years for both genders since the peak of the HIV/AIDS epidemic in 2005 (World Health Organization, 2017a). Correspondingly, the burdens of aging-related chronic diseases such as Alzheimer’s disease and related dementias, cardiovascular disease, and cancers are rising dramatically (Kabudula et al. 2017; Prince et al. 215). A substantial proportion of these chronic diseases can be prevented through modifiable risk-related behaviors such as physical activity, diet, smoking, and alcohol consumption (American Cancer Society 2017; Wiseman 2008; McCullough et al. 2011). The investigation and reduction of socioeconomic gradients in these behaviors among aging populations is essential for future prevention efforts to be as equitable and effective as possible.
Although a small body of evidence from a range of countries shows socioeconomic gradients in health-related behaviors (Caldwell et al. 2008; Tehranifar et al. 2009; Akinyemiju et al. 2017; National Department of Health 2017), the socioeconomic drivers of chronic disease risk behaviors in South Africa’s older rural population are unknown. An important consideration when measuring socioeconomic status among older, low-income populations, such as in rural South Africa, is selection of the appropriate socioeconomic measures (Howe et al. 2012; Grundy and Holt 2001). Many older adults in rural South Africa do not work, and for those who do, income and employment can be sporadic, informal, and difficult to report in a simple manner (Grundy and Holt 2001; Statistics South Africa 2011). Measures of household wealth, as indexed by housing conditions and assets rather than financial wealth, as well as household consumption have therefore been advocated for in this context, rather than measures of income or occupation (Headey et al. 2008). As household consumption directly reflects daily expenditures, food production, and assistance from government support programs, it is considered to be more accurate measure of daily household welfare than income (Howe et al. 2012). The relationships between household wealth, consumption, and chronic disease risk behaviors in the older population of rural South Africa are unknown.
We therefore aimed to estimate the independent associations between each of household wealth and consumption quintiles and four chronic disease risk behaviors (moderate-to-vigorous intensity physical activity, overweight/obese body mass index, smoking, and frequent alcohol intake) in a population-based study of older adults in rural South Africa.
METHODS
Study Population
Data were from baseline assessments collected in 2015 in “Health and Aging in Africa: A Longitudinal Study of an INDEPTH Community in South Africa” (HAALSI), a population-based study of 5,059 men and women aged ≥40 years in the Agincourt Health and Socio-Demographic Surveillance System (HDSS) area covering approximately 116,000 people residing in 31 villages in Mpumalanga province, South Africa (response rate = 85.9%) (Gómez-Olivé et al. 2018). HAALSI is harmonized with the US Health and Retirement Study and other international cohort studies of aging (see: https://g2aging.org/). The demographic profile of the Agincourt region population is typical of rural South Africa (Gómez-Olivé et al. 2018). Although the social and economic situation of the region has improved since the end of Apartheid in 1994, the region has a history of systematic racism, poor infrastructure development, and low access to education, employment, and other economic opportunities (United Nations 1963; Christie and Collins 1982).
Data Collection
In-person interviews were conducted with trained, local fieldworkers in the participants’ homes in the local Shangaan language using Computer Assisted Personal Interviews (CAPI). All interview measures were translated from English and back-translated to ensure reliability. The interview covered broad topics including sociodemographic factors, health status, social networks, health risk behaviors, and living conditions (Gómez-Olivé et al. 2018).
Measures
Household wealth and consumption:
Household wealth and consumption were assessed using validated measures from the Demographic and Health Surveys (DHS) and the Longitudinal Aging Study in India (LASI) (Rutstein and Johnson 2004; Arokiasamy et al. 2012). Using the DHS methodology, we constructed a wealth index from interview data on housing, durable and non-durable assets, land ownership, and livestock (Rutstein and Johnson 2004; Arokiasamy et al. 2012). After identifying variables with variation across households, we used principal components analysis (PCA) to create the wealth index and group households into quintiles of household wealth (Riumallo-Herl et al. 2017). Household consumption was calculated by aggregating data on regular and non-regular expenditures of different food products, goods, and services as well as home-based food production. Consumption is a more appropriate measure of living standards in developing countries when compared to income, as it captures what is consumed by the household, whether it is produced or purchased (Deaton and Grosh 2000). We scaled the level of consumption according to the number of people living in the household size (Hentschel and Lanjouw 1996). For the analyses of smoking and drinking behaviors, we excluded expenditures on tobacco and alcohol from the household consumption index. As with the wealth index, households were then categorized into quintiles of household consumption.
Chronic disease risk behaviors:
Moderate-to-vigorous intensity physical activity, smoking, alcohol consumption, and body mass index were selected as the outcome variables of interest due to their strong and consistently observed associations with risks of several chronic diseases and all-cause mortality (Ford et al. 2011; Khaw et al. 2008; Kvaavik et al. 2011). All were assessed during the in-person interview. We were interested identifying the proportions of the HAALSI study population who met evidence-based public health guidelines for these behaviors and body mass index, overall and according to socioeconomic position. We therefore coded the chronic disease risk behaviors and body mass index as binary outcome variables according to evidence-based South African national public health guidelines and internationally recognized recommendations for chronic disease risk reduction (Wiseman 2008; American Cancer Society 2017; World Health Organization 2010; World Health Organization 2017b; World Health Organization 2018). The variable measurements and coding are described below:
Moderate-to-vigorous physical activity (MVPA):
Physical activity was measured using the WHO’s Global Physical Activity Questionnaire (GPAQ), which has been validated for use in low-income settings (Bull et al. 2009). Participants reported the number of hours and minutes in the average week that they spent walking or bicycling, and in moderate or vigorous intensity activity for work and for recreation (Bull et al. 2009). Minutes per week of total moderate-to-vigorous intensity physical activity (MVPA) was calculated from these responses, including walking and bicycling. The binary outcome variable indicated the harmful and protective MVPA categories, respectively: <210 vs. ≥210 minutes per week of MVPA (equivalent to 30 minutes per day), based on the South African Department of Health recommendation and the World Cancer Research Fund recommendation for cancer prevention (Wiseman 2008).
Smoking:
Participants were classified as current smokers vs. former/never smokers, based on their answer to the question “Do you currently use tobacco products?”, reflecting the harmful vs. protective categories of smoking.
Alcohol consumption:
Participants were asked about the frequency with which they consumed at least one standard serving of alcoholic beverages in the past 30 days (daily; 5–6 days per week; 1–4 days per week; 1–3 days per month; less than once; does not currently drink). While South Africa does not have uniform alcohol consumption guidelines, the American Cancer Society recommends no more than two drinks per day for men and no more than one drink per day for women, and the World Cancer Research Fund recommends drinking no alcohol or following national guidelines (American Cancer Society 2017; Wiseman 2008). Very few HAALSI participants reported drinking alcohol daily (167/5055; 3%), so the binary outcome variable was coded at the next most frequent level of ≥5 vs. <5 days per week.
Body mass index (BMI):
During the study interview, trained fieldworkers measured participants’ heights and weights using calibrated instruments. BMI was calculated as weight in kilograms divided by height in meters squared. The binary outcome variable was defined according to the World Health Organization cut-off of having a normal weight BMI (<25.0) vs. an overweight or obese BMI (≥25.0) (World Health Organization 2017b).
Covariates:
Covariates included in the analyses were age category (40–49; 50–59; 60–69; 70–79; ≥80), sex, country of birth (South Africa; Mozambique or other), highest level of educational attainment (no formal education; some primary education [1–7 years]; some secondary education [8–11 years]; secondary education or higher [12 or more years]), current employment status (not employed part- or full-time; working; homemaker), literacy (self-reported ability to read or write; yes/no), self-reported health in childhood (very bad, bad, moderate; good, very good), and father’s occupation during childhood (skilled, unskilled, other, don’t know). Age categories were used instead of continuous age to account for outliers in the oldest age group, and country of birth was included to account for any unmeasured differences between the study participants who were born in South Africa versus those who came to the Agincourt area as refugees during the 1977–1992 civil war in neighboring Mozambique (Sartorius et al. 2013). Father’s occupation during childhood was classified as skilled or unskilled according to the International Standard Classification of Occupations 2008; specific job types are detailed elsewhere (Kobayashi et al., 2017).
Statistical Analysis
The prevalence of each chronic disease risk behavior was calculated, overall and according to quintiles of household wealth and household consumption. Prevalence ratios (PRs) and associated 95% confidence intervals (CIs) for the relationships between household wealth quintile, household consumption quintile, and each chronic disease risk behavior were estimated using Poisson regression models with a robust error variance and logarithmic link function for binary outcome data (Zou 2004), adjusting for age, sex, country of birth, self-rated health in childhood, father’s occupation during childhood, education, literacy, and employment status. For both wealth and consumption, the first quintiles (i.e. the poorest and the lowest consumption) were used as the reference categories, so that the PRs demonstrated the likelihood of engaging in the harmful vs. the protective category of risk behavior associated with each increasing quintile of household wealth or consumption. Trend tests were conducted to assess the presence of linear gradients in the likelihood of engagement in each behavior across household wealth and consumption quintiles. We conducted supplementary analyses to examine the associations across all BMI categories (<18.5: underweight; 18.5–24.9: normal weight; 25.0–29.9: overweight; 30.0: obese), and separating former and never smokers into separate categories. We also conducted a supplementary analysis to compare reported expenditure on tobacco and alcohol products, according to household wealth quintile. The analyses were conducted using Stata version 15.1 (College Station, TX, USA).
Missing Data
No data were missing for household wealth or consumption, 5/5059 participants (<<1%) were missing data on physical activity, smoking, or alcohol consumption, and 370/5059 (7%) participants were missing data on BMI. Covariate data were missing for less than 1% of participants. The analytical samples for each regression model included all those with complete data on covariates and the behavior of interest.
RESULTS
Table 1 summarizes the baseline characteristics of all participants. Just over half were female, most were born in South Africa, 42% could not read or write, and 46% had no formal education. Nearly three-quarters were not working, and most reported good or very good childhood health. Overall, 57% of the sample reported engaging in <210 minutes per week of MVPA, and as such, did not meet internationally recognized physical activity recommendations (Table 1). Nine percent of the sample were current smokers, 6% reported drinking alcohol on at least five days per week in the past 30 days, and 58% had an overweight or obese BMI (Table 1).
Table 1.
Characteristics of the sample, “Health and Aging in Africa: A Longitudinal Study of an INDEPTH Community in South Africa” (HAALSI), Agincourt, South Africa, 2015
| Characteristic | N=5059 | 100% |
|---|---|---|
| Sex | ||
| Male | 2345 | 46.4% |
| Female | 2714 | 53.7% |
| Age | ||
| 40–49 | 918 | 18.2% |
| 50–59 | 1410 | 27.9% |
| 60–69 | 1304 | 25.8% |
| 70–79 | 878 | 17.4% |
| 80+ | 549 | 10.9% |
| Country of birth | ||
| South Africa | 3528 | 69.8% |
| Mozambique or other | 1526 | 30.2% |
| Literacy | ||
| Can read and/or write | 2948 | 58.3% |
| Cannot read or write | 2108 | 41.7% |
| Education level | ||
| No formal education | 2306 | 45.7% |
| Some primary (1–7 years) | 1614 | 32.0% |
| Some secondary (8–11 years) | 537 | 10.7% |
| Secondary or more (12+ years) | 585 | 11.6% |
| Employment status | ||
| Employed (part or full time) | 805 | 16.0% |
| Not working | 3719 | 73.7% |
| Homemaker | 521 | 10.3% |
| Self-rated childhood health | ||
| Moderate, bad, or very bad | 621 | 12.3% |
| Good or very good | 4434 | 87.7% |
| Father’s occupation during childhood | ||
| Skilled | 2479 | 49.1% |
| Unskilled | 1446 | 28.7% |
| Other | 575 | 11.4% |
| Don’t know | 547 | 10.8% |
| Physical activity | ||
| ≥210 minutes of MVPA | 2168 | 42.9% |
| <210 minutes of MVPA | 2886 | 57.1% |
| Smoking | ||
| Never smoker | 3977 | 78.6% |
| Former smoker | 622 | 12.3% |
| Current smoker | 460 | 9.1% |
| Alcohol consumption | ||
| <5 days per week | 4751 | 94.0% |
| ≥5 days per week | 304 | 6.0% |
| BMI | ||
| <18.5 (Underweight) | 258 | 5.5% |
| 18.5–24.9 (Normal weight) | 1719 | 36.7% |
| 25.0–29.9 (Overweight) | 1328 | 28.3% |
| ≥30.0 (Obese) | 1384 | 29.5% |
Note: The total N for each covariate may not sum to 5059 due to missing data
Note on acronyms: INDEPTH: International Network for the Demographic Evaluation of Populations and Their Health; MVPA: moderate-to-vigorous physical activity; BMI: body mass index
As household wealth quintile increased, there was a higher prevalence of low MVPA and overweight/obese BMI, and a lower prevalence of smoking and frequent alcohol intake (Table 2; Figure 1). The percentage point differences between the poorest and wealthiest quintiles were: 4 (low MVPA), 26 (overweight/obese BMI), -8 (smoking), and -9 (frequent drinking) (Table 2; Figure 1). With respect to household consumption, the only trend that mirrored the trend observed for household wealth was for overweight/obese BMI, with a 10-percentage point increase in prevalence between the lowest and highest household consumption quintile (Table 2; Figure 2). The prevalence of low MVPA decreased with increasing household consumption quintile (-6 percentage points), while smoking and frequent alcohol intake negligibly varied by household consumption quintile (Table 2; Figure 2).
Table 2.
Chronic disease risk behaviors according to household wealth and household consumption quintiles, “Health and Aging in Africa: A Longitudinal Study of an INDEPTH Community in South Africa” (HAALSI), Agincourt, South Africa, 2015
| Household wealth quintiles | Protective risk behavior | Harmful risk behavior |
|---|---|---|
| Physical activity | 210 minutes of MVPA | < 210 minutes of MVPA |
| Quintile 1 (N=1045) | 492 (47.1%) | 553 (52.9%) |
| Quintile 2 (N=1000) | 422 (42.2%) | 578 (57.8%) |
| Quintile 3 (N=990) | 430 (43.4%) | 560 (56.6%) |
| Quintile 4 (N=1006) | 390 (38.8%) | 616 (61.2%) |
| Quintile 5 (N=1013) | 434 (42.8%) | 579 (57.2%) |
| Smoking | Former/never smoker | Current smoker |
| Quintile 1 (N=1044) | 906 (86.8%) | 138 (13.2%) |
| Quintile 2 (N=1000) | 899 (89.9%) | 101 (10.1%) |
| Quintile 3 (N=989) | 899 (90.9%) | 90 (9.1%) |
| Quintile 4 (N=1007) | 926 (92.0%) | 81 (8.0%) |
| Quintile 5 (N=1014) | 964 (95.1%) | 50 (4.9%) |
| Alcohol consumption | Fewer than five days per week | Five or more days per week |
| Quintile 1 (N=1043) | 918 (88.0%) | 125 (12.0%) |
| Quintile 2 (N=1000) | 925 (92.5%) | 75 (7.5%) |
| Quintile 3 (N=991) | 945 (95.4%) | 46 (4.6%) |
| Quintile 4 (N=1007) | 978 (97.1%) | 29 (2.9%) |
| Quintile 5 (N=1014) | 985 (97.1%) | 29 (2.9%) |
| BMI | < 25.0 | ≥25.0 |
| Quintile 1 (N=960) | 520 (54.2%) | 440 (45.8%) |
| Quintile 2 (N=924) | 455 (49.2%) | 469 (50.8%) |
| Quintile 3 (N=913) | 392 (42.9%) | 521 (57.1%) |
| Quintile 4 (N=934) | 344 (36.8%) | 590 (63.2%) |
| Quintile 5 (N=958) | 266 (27.8%) | 692 (72.2%) |
| Household consumption quintiles | Protective risk behavior | Harmful risk behavior |
| Physical activity | > 210 minutes of MVPA | < 210 minutes of MVPA |
| Quintile 1 (N=1045) | 422 (40.4%) | 623 (59.6%) |
| Quintile 2 (N=1024) | 436 (41.6%) | 598 (58.4%) |
| Quintile 3 (N=1020) | 457 (44.8%) | 563 (55.2%) |
| Quintile 4 (N=974) | 406 (41.7%) | 568 (58.3%) |
| Quintile 5 (N=991) | 457 (46.1%) | 534 (53.9%) |
| Smoking | Former/never smoker | Current smoker |
| Quintile 1 (N=1045) | 947 (91.1%) | 92 (8.9%) |
| Quintile 2 (N=1023) | 943 (93.0%) | 71 (7.0%) |
| Quintile 3 (N=1020) | 923 (90.3%) | 99 (9.7%) |
| Quintile 4 (N=975) | 892 (89.7%) | 102 (10.3%) |
| Quintile 5 (N=991) | 889 (90.3%) | 96 (9.7%) |
| Alcohol consumption | Fewer than five days per week | Five or more days per week |
| Quintile 1 (N=1045) | 962 (92.6%) | 77 (7.4%) |
| Quintile 2 (N=1024) | 961 (94.8%) | 53 (5.2%) |
| Quintile 3 (N=1020) | 961 (93.9%) | 62 (6.1%) |
| Quintile 4 (N=975) | 930 (93.6%) | 64 (6.4%) |
| Quintile 5 (N=991) | 937 (95.1%) | 48 (4.9%) |
| BMI | < 25.0 | ≥25.0 |
| Quintile 1 (N=978) | 460 (47.0%) | 518 (53.0%) |
| Quintile 2 (N=952) | 427 (44.9%) | 535 (55.1%) |
| Quintile 3 (N=958) | 400 (41.8%) | 558 (58.2%) |
| Quintile 4 (N=882) | 353 (40.0%) | 529 (60.0%) |
| Quintile 5 (N=919) | 337 (36.7%) | 582 (63.3%) |
Note: Quintile 1 represents the poorest/lowest consumption quintile, and quintile 5 represents the richest/highest consumption quintile.
Note on acronyms: INDEPTH: International Network for the Demographic Evaluation of Populations and Their Health; MVPA: moderate-to-vigorous physical activity; BMI: body mass index
Fig 1.
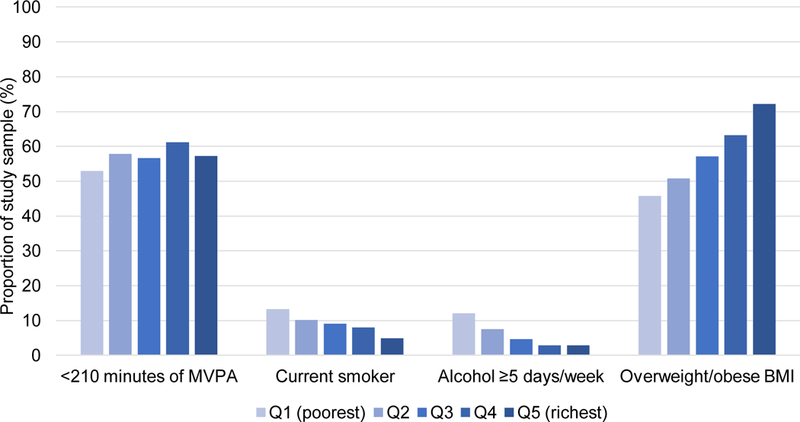
Socioeconomic gradients in chronic disease risk behaviors and body mass index, according to household wealth index quintile, “Health and Aging in Africa: A Longitudinal Study of an INDEPTH Community in South Africa” (HAALSI), Agincourt, South Africa, 2015
Fig 2.
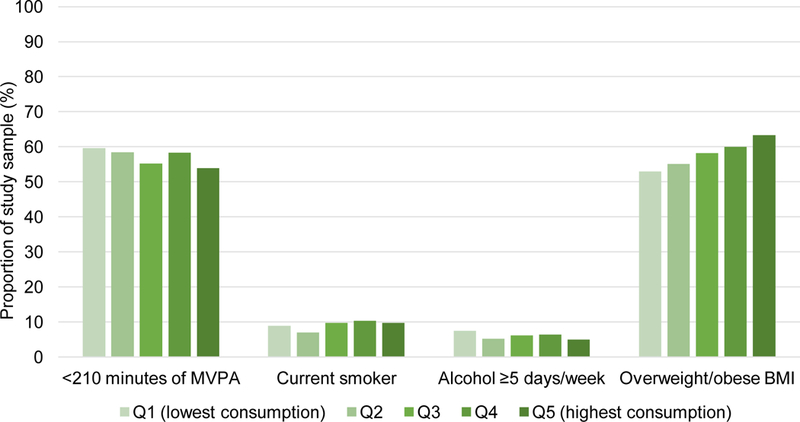
Socioeconomic gradients in chronic disease risk behaviors and body mass index, according to household consumption quintile, “Health and Aging in Africa: A Longitudinal Study of an INDEPTH Community in South Africa” (HAALSI), Agincourt, South Africa, 2015
The adjusted prevalence ratios reflected the above findings (Table 3). The likelihood of low MVPA increased with increasing household wealth quintile (p-trend<0.01; PR=1.11; 95% CI: 1.03–1.21 for the richest vs. poorest wealth quintile; Table 3). Conversely, smoking steadily decreased with increasing household wealth quintile (p-trend<0.01; PR=0.34; 95% CI: 0.25–0.47 for the richest vs. poorest wealth quintile; Table 3). Frequent alcohol consumption also decreased with increasing household wealth quintile (p-trend<0.01; PR=0.33; 95% CI: 0.22–0.50 for the richest vs. poorest wealth quintile; Table 3). The widest disparity in chronic disease risk behaviors was for BMI, where overweight or obese BMI steadily increased with increasing household wealth (p-trend<0.01) and the prevalence ratio was nearly 50% higher in the richest versus the poorest wealth quintile (PR=1.48; 95% CI: 1.36–1.60; Table 3).
Table 3.
Adjusted prevalence ratios (PRs) for the associations between household wealth and household consumption quintiles and chronic disease risk behaviors, “Health and Aging in Africa: A Longitudinal Study of an INDEPTH Community in South Africa” (HAALSI), Agincourt, South Africa, 2015
| Socioeconomic exposure variable | Chronic disease risk behavior outcome |
|||
|---|---|---|---|---|
| <210 min/week MVPA (vs. 210 min/week) PR (95% CI) | Current smoker (vs. former/never) PR (95% CI) | Alcohol 5 days/week (vs. <5 days/week) PR (95% CI) | Overweight/obese BMI (vs. normal BMI) PR (95% CI) | |
| Household wealth quintiles | ||||
| Quintile 1, poorest (N=1046) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Quintile 2 (N=1001) | 1.10 (1.01, 1.18) | 0.77 (0.62, 0.96) | 0.72 (0.55, 0.94) | 1.09 (0.99, 1.19) |
| Quintile 3 (N=991) | 1.08 (1.00, 1.17) | 0.68 (0.54, 0.86) | 0.48 (0.34, 0.67) | 1.20 (1.10, 1.31) |
| Quintile 4 (N=1007) | 1.19 (1.10, 1.28) | 0.59 (0.46, 0.76) | 0.32 (0.21, 0.47) | 1.32 (1.21, 1.43) |
| Quintile 5, richest (N=1014) | 1.11 (1.03, 1.21) | 0.34 (0.25, 0.47) | 0.33 (0.22, 0.50) | 1.48 (1.36, 1.60) |
| p-trend | <0.01 | <0.01 | <0.01 | <0.01 |
| Household consumption quintiles | ||||
| Quintile 1, lowest (N=1047) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Quintile 2 (N=1024) | 0.91 (0.84, 0.98) | 0.86 (0.66, 1.13) | 0.77 (0.55, 1.08) | 1.07 (0.99, 1.16) |
| Quintile 3 (N=1021) | 0.94 (0.88, 1.01) | 1.03 (0.81, 1.33) | 0.92 (0.67, 1.27) | 1.11 (1.03, 1.20) |
| Quintile 4 (N=975) | 0.93 (0.87, 1.00) | 1.01 (0.79, 1.29) | 0.96 (0.70, 1.32) | 1.12 (1.04, 1.21) |
| Quintile 5, highest (N=992) | 0.86 (0.79, 0.93) | 0.88 (0.67, 1.14) | 0.83 (0.58, 1.18) | 1.15 (1.06, 1.25) |
| p-trend | <0.01 | 0.70 | 0.65 | <0.01 |
Note: Quintile 1 represents the poorest/lowest consumption quintile, and quintile 5 represents the richest/highest consumption quintile.
Note: All odds ratios are adjusted for age, sex, educational attainment, employment status, country of birth, literacy, self-rated health in childhood, and father’s occupation during childhood
Note on acronyms: INDEPTH: International Network for the Demographic Evaluation of Populations and Their Health; MVPA: moderate-to-vigorous physical activity; BMI: body mass index; PR: prevalence ratio; CI: confidence interval
The consumption index was not a consistent independent predictor of differences in chronic disease risk behaviors in the regression models, although some patterns emerged (Table 3). Low MVPA was inversely associated with household consumption (p-trend<0.01; PR=0.86; 95% CI: 0.79–0.93 for the highest vs. lowest consumption quintile) and, as with household wealth, the greatest disparity was observed in overweight/obese BMI (p-trend<0.01; PR=1.15; 95% CI:1.06–1.25 for the highest vs. lowest consumption quintile; Table 3). Household consumption quintile was not a strong predictor of either smoking or alcohol consumption behaviors.
When smoking status was expanded into each of current, former, and never categories, the gradient according to household wealth quintile was stronger for current smoking than for former smoking (Supplementary Table 1). Older adults in higher household consumption quintiles appeared moderately more likely to be former smokers than those in the lowest quintile, but the effect estimates were imprecise (Supplementary Table 1). We found that the likelihood of being underweight compared to normal weight decreased with increasing household wealth quintile, although underweight was not associated with household consumption (Supplementary Table 2). The results for overweight and obesity separately were consistent with the main analysis, but the magnitudes of socioeconomic gradients were stronger for obesity than for overweight (Supplementary Table 2). We found that mean monthly reported expenditure on tobacco and alcohol products was higher in relatively wealthier households, but, that fewer households reported purchasing these products as household wealth increased (Supplementary Table 3).
DISCUSSION
In this large, population-based study of older adults in rural South Africa, we observed socioeconomic gradients in chronic disease risk behaviors according to relative measures of household wealth and consumption. Household wealth quintile was a stronger and more consistent predictor of chronic disease risk behaviors than household consumption quintile, supporting its use here as an indicator of socioeconomic disparities in chronic disease risk behaviors. Our results indicate that, in this low-income context, chronic disease risk behaviors are socioeconomically graded at later stages of life. Further, the overall prevalence of overweight and obesity according to body mass index was high, with nearly one-third being overweight and another one-third being obese. Older adults with greater levels of household wealth and consumption were disproportionately likely to be overweight or obese. This study provides some of the first evidence on socioeconomic gradients in chronic disease risk behaviors in a rural, low-income older population in South Africa. These socioeconomic gradients have been largely overlooked in rural, low-income populations of this region and require urgent public health attention.
Unlike associations observed in high-income settings, greater household wealth was not invariably associated with protective behaviors, but rather predicted a mixed combination of behaviors. For example, greater household wealth was associated with higher odds of low MVPA and with having an overweight or obese body mass index, patterns that are consistent with those observed in the general South African population (Shisana et al. 2013). Indeed, these socioeconomic gradients were consistent with well-documented trends that occur as countries increase in economic development and pass through the epidemiologic transition (Akinyemiju et al. 2017; Allen et al. 2017; Popkin et al. 2012; Katzmarzyk and Mason 2009). In this rural study context in particular, the higher prevalence of MVPA and the lower prevalence of overweight and obesity among older adults with less household wealth may be due to a greater need for physically-demanding informal and household labor and walking for transportation to resources.
In this study, 10% of older adults in the poorest household wealth quintile reported less than one hour per day of walking for transportation, compared with 17% of older adults in the richest household wealth quintile. This finding is consistent with previous research on the spatial dimension of poverty in the Agincourt sub-district, which showed that poorer households with lower rates of motor vehicle ownership and in-home running water and toilet facilities are clustered in specific villages (Sartorius et al. 2013). Only 16% of the HAALSI sample reported being employed part- or full-time and these people tended to reside in relatively wealthier households. We did not have measures of energy expenditure in informal, unpaid, or household labor to examine against household wealth or consumption measure; this should be a topic of future investigation in the aging population of rural South Africa. However, it should be noted that the wealth gradient was not steep for MVPA, with only a 4 percentage-point difference between the poorest vs. richest quintiles, while there was nearly a 30 percentage-point difference in overweight/obese BMI between the poorest vs. richest quintile.
We also found that being in a relatively wealthier household was associated with lower odds of current tobacco use. This finding is consistent with socioeconomic gradients in smoking observed in a range of country contexts, including other sub-Saharan African countries (Akinyemiju et al. 2017; Allen et al. 2017; Pampel et al. 2008; Howe et al. 2012). The evidence to date on socioeconomic gradients in the frequency of alcohol consumption in sub-Saharan African countries is relatively weak, although some studies have reported that frequent alcohol use is less common among more socioeconomically advantaged groups (Akinyemiju et al. 2017; Allen et al. 2017). Education and health knowledge, as well as the influence of local social norms may underlie socioeconomic disparities in smoking and drinking behaviors (Grundy and Sloggett 2003; Tucker 2002). However, most evidence on these relationships comes from high-income settings; further research is needed to confirm the magnitudes and directions of socioeconomic gradients in chronic disease risk behaviors of older adults in rural, low-income settings, and the underlying mechanisms for these gradients.
The value of consumption as a predictor of health behaviors in LMICs has been debated, and some have suggested that wealth and asset indices more accurately predict socioeconomic disparities in health (Howe et al. 2012). The present study suggests that household consumption is not a consistent predictor of chronic disease risk behaviors among older adults in rural South Africa. The mechanisms underlying the associations between each of wealth and consumption and chronic disease risk behaviors may vary, as consumption may not be related to the same social norm and network influences on behavior that could explain wealth-based gradients in behavior (Tucker 2002). Household consumption may influence other behaviors that are less related to lifestyle and are essential across the socioeconomic gradient, such as the utilization of healthcare services (Howe et al. 2012). Future research should examine the potential mechanisms underlying wealth- and consumption-based gradients in different aspects of the health behavior and care experience for older adults in rural South Africa.
Limitations and Strengths
Physical activity, smoking, and alcohol consumption were assessed via self-report in the study interview, and therefore recall error may bias the results of our study. If error in recall of these behaviors was randomly distributed in the study population, our estimates would be attenuated towards the null. If older adults systematically over- or under-reported behavior in a pattern that was associated with wealth or consumption, then our estimates may over- or under-report the true associations in a direction that is difficult to predict. We recognize that our dichotomization of the variables for moderate-to-vigorous physical activity, frequency of alcohol consumption, and body mass index resulted in loss of variation relative to continuous variables. However, we categorized these variables using evidence-based South African and international public health guidelines that correspond to specific cut-off points for levels of behavior where there are threshold effects for risks of chronic disease and mortality (Wiseman 2008; American Cancer Society 2017; World Health Organization 2010; World Health Organization 2017b; World Health Organization 2018).
We adjusted for a range of potential confounding variables, including measures of childhood health and socioeconomic position. However, any residual confounding by childhood circumstances not captured by these two variables could bias our results to a degree that is difficult to ascertain, although the childhood variables included in this analysis negligibly altered effect estimates. Social desirability bias may also be present in our results, which could result in the under-reporting of harmful behaviors. Our data described the frequency but not quantity of alcohol consumption, and episodic binge drinking has been associated with a variety of negative health outcomes (Roerecke and Rehm 2010; Jin et al. 2013). Future waves of data collection will assess the number of drinks consumed per drinking episode in addition to drinking frequency. The cross-sectional nature of this study means that the data do not capture changes in either the exposures or the outcomes over time. However, planned longitudinal data collection in HAALSI will allow for future assessment of these relationships.
Strengths of this study include its large, population-based sample of older men and women living in rural South Africa. This is a relatively understudied population in global health and aging and represents some of the “oldest old” adults living in South Africa. This paper presents the first study to examine socioeconomic gradients in chronic disease risk behaviors in older adults living in rural South Africa. As the burden of aging-related chronic diseases continues to rise in South Africa, this study provides useful insights as to how socioeconomic status may influence engagement in health behaviors. Further, we used a validated measure of household wealth based on housing conditions, durable and non-durable assets, land ownership, and livestock, and a validated measure of household consumption based on expenditures and food production. These measures are widely accepted as appropriate for low-income settings where the measurement of financial assets and income can be difficult and problematic.
Conclusions
This study demonstrates the presence of socioeconomic gradients in moderate-to-vigorous physical activity, smoking, alcohol intake, and overweight and obese body mass index among older adults in rural South Africa. These behaviors were more strongly graded according to household wealth than to household consumption. The directions of these gradients were consistent with other findings from LMICs and were mostly opposite to trends observed in higher-income settings. Over half of the study population was measured to have an overweight or obese body mass index, which is a cause for urgent public health concern. As South Africa’s population continues to age, equitable health polices and interventions are needed to reduce the growing burden of overweight and obesity and resulting chronic disease risk.
Supplementary Material
Acknowledgments
This work was funded by a grant from the National Institute on Aging of the National Institutes of Health (P01 AG04171). The funder had no role in the study design; in the collection, analysis, and interpretation of data; in the writing of the article; or in the decision to submit it for publication.
Footnotes
COMPLIANCE WITH ETHICAL STANDARDS
Ethical Approval
Ethical approval was granted by the University of Witwatersrand Human Research Ethics Committee (M141159), the Harvard T. H. Chan Harvard School of Public Health, Office of Human Research Administration (C13-1608-02), and the Mpumalanga Provincial Research and Ethics Committee. Informed consent was obtained from all individual participants included in the study. All procedures involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Conflict of Interest
The authors have no conflicts of interest to declare.
REFERENCES
- Akinyemiju T, Ogunsina K, Okwali M, Sakhuja S, Braithwaite D (2017) Lifecourse socioeconomic status and cancer-related risk factors: Analysis of the WHO study on global ageing and adult health (SAGE). Int J Cancer 140:777–787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen L, Williams J, Townsend N, Mikkelsen B, Roberts N, Foster C, Wickramasinghe K (2017) Socioeconomic status and non-communicable disease behavioural risk factors in low-income and lower-middle-income countries: a systematic review. Lancet Global Health 5: e277–e289. 10.1016/S2214-109X(17)30058-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arokiasamy P, Bloom D, Lee J, Feeney K, Ozolins M (2012) Longitudinal Aging Study in India: Vision, Design, Implementation, and Preliminary Findings. In: Smith JP, Majmundar M (eds) Aging in Asia: Findings From New and Emerging Data Initiatives National Academies Press, Washington, DC, pp 36–76. [PubMed] [Google Scholar]
- American Cancer Society (2017) Alcohol Use and Cancer Available from: https://www.cancer.org/cancer/cancer-causes/diet-physical-activity/alcohol-use-and-cancer.html. Accessed 24 March 2018.
- Bull FC, Maslin TS, Armstrong T (2009) Global Physical Activity Questionnaire (GPAQ): nine country reliability and validity study. J Phys Act Health 6:790–804. [DOI] [PubMed] [Google Scholar]
- Caldwell TM, Rodgers B, Clark C, Jefferis BJ, Stansfeld SA, Power C (2008) Lifecourse socioeconomic predictors of midlife drinking patterns, problems and abstention: Findings from the 1958 British Birth Cohort Study. Drug Alcohol Depend 95:269–278. [DOI] [PubMed] [Google Scholar]
- Christie P, Collins C (1982) Bantu education: Apartheid ideology or labour reproduction? Comparative Education 18:59–75. [Google Scholar]
- Deaton A, Grosh M (2000) Consumption. In: Grosh M, Glewwe P (eds) Designing Household Survey Questionnaires for Developing Countries: Lessons from 15 Years of the Living Standards Measurement Study The World Bank: Washington, DC, pp 91–134. [Google Scholar]
- Ford ES, Zhao G, Tsai J, Li C (2011) Low-risk lifestyle behaviors and all-cause mortality: findings from the National Health and Nutrition Examination Survey III Mortality Study. Am J Public Health 101:1922–1929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gómez-Olivé FX, Montana L, Wagner RG, Kabdula CW, Rohr JK, Kahn K, Barnighausen T, Canning D, Gaziano T, Salomon JA, Payne CF, Wade A, Tollman SM, Berkman L (2018) Cohort Profile: Health and Ageing in Africa: a Longitudinal Study of an INDEPTH Community in South Africa (HAALSI). Int J Epidemiol 10.1093/ije/dyx247 [DOI] [PMC free article] [PubMed]
- Grundy E, Holt G (2011) The socioeconomic status of older adults: How should we measure it in studies of health inequalities? J Epidemiol Community Health 55: 895–904. 10.1136/jech.55.12.895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grundy E, Sloggett A (2003) Health inequalities in the older population: the role of personal capital, social resources and socio-economic circumstances. Soc Sci Med 56: 935–937. 10.1016/S0277-9536(02)00093-X [DOI] [PubMed] [Google Scholar]
- Headey B (2008) Poverty is low consumption and low wealth, not just low income. Soc Indic Res 89:23–39. 10.1007/s11205-007-9231-2 [DOI] [Google Scholar]
- Hentschel J, Lanjouw P (1996) Constructing an indicator of consumption for the analysis of poverty: Principles and illustrations with reference to Ecuador World Bank, Washington, DC, LSMS Working Paper Number 124. [Google Scholar]
- Howe LD, Galobardes B, Maijasevic A, Gordon D, Johnson D, Onwujekwe O, Patel R, Webb EA, Lawlor DA, Hargreaves JR (2012) Measuring socio-economic position for epidemiological studies in low-and middle-income coutries: a methods of measurement in epidemiology paper. Int J Epidemiol 41:871–886. 10.1093/ije/dys037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jin M, Cai S, Guo J, Zhu Y, Li M, Yu Y, Zhang S, Chen K (2013) Alcohol drinking and all cancer mortality: a meta-analysis. Ann Oncol 24:807–816. 10.1093/annonc/mds508 [DOI] [PubMed] [Google Scholar]
- Kabudula CW, Houle B, Collinson MA, Kahn K, Gómez-Olivé FX, Clark SJ, Tollman S (2017) Progression of the epidemiological transition in a rural South African setting: findings from population surveillance in Agincourt, 1993–2013. BMC Public Health 17:424 10.1186/s12889-017-4312-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katzmarzyk PT, Mason CJ (2009) The physical activity transition. Phys Act Health 6:269–280. [DOI] [PubMed] [Google Scholar]
- Khaw KT, Wareham N, Bingham S, Welch A, Luben R, Day N (2008) Combined impact of health behaviours and mortality in men and women: the EPIC-Norfolk prospective population study. PLOS Med 5:e12 10.1371/journal.pmed.0050012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kobayashi LC, Glymour MM, Kahn K, Payne CF, Wagner RG, Montana L, Mateen FJ, Tollman SM, Berkman LF. Childhood deprivation and later-life cognitive function in a population-based study of older, rural South Africans. Soc Sci Med 2017;190:20–8. 10.1016/j.socscimed.2017.08.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kvaavik E, Batty D, Ursin G, Huxley R, Gale C (2011). Influence of individual and combined health behaviors on total and cause-specific mortality in men and women: The United Kingdom Health and Lifestyle Survey. Arch Intern Med 170:711–719. [DOI] [PubMed] [Google Scholar]
- McCullough ML, Patel AV, Kushi LH, Patel R, Willett WC, Doyle C, Thun MJ, Gapstur SM (2011). Following cancer prevention guidelines reduces risk of cancer, cardiovascular disease, and all-cause mortality. Cancer Epidemiol Biomarkers Prev 20:1089–1097. [DOI] [PubMed] [Google Scholar]
- National Department of Health (2017). South African Demographic and Health Survey 2016: Key Indicators Report https://www.statssa.gov.za/publications/Report%2003-00-09/Report%2003-00-092016.pdf. Accessed 5 May 2018.
- Pampel F (2008). Tobacco use in sub-Sahara Africa: Estimates from the demographic health surveys. Soc Sci Med 66, 1772–1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Popkin BM, Adair LS, Ng SW (2012) NOW AND THEN: The Global Nutrition Transition: The Pandemic of Obesity in Developing Countries. Nutr Rev 70:3–21. 10.1111/j.1753-4887.2011.00456.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prince M, Wimo A, Guerchet M, Ali G-C, Wu Y-T, Prina M, Alzheimer’s Disease International (2015) World Alzheimer Report 2015: The Global Impact of Dementia: An analysis of prevalence, incidence, cost, and trends https://www.alz.co.uk/research/WorldAlzheimerReport2015.pdf. Accessed 5 May 2018.
- Riumallo-Herl C, Canning D, Wagner R, Kabudula C, Collinson M (2017) Health gradients in South Africa: Inequalities in the measure of the beholder. PGDA Working Paper 139 https://cdn1.sph.harvard.edu/wp-content/uploads/sites/1288/2012/11/Health-Gradients-in-South-Africa-Inequalities-in-the-Measure-of-the-Beholder-May_3_2017.pdf. Accessed 5 May 2018.
- Roerecke M, Rehm J (2010) Irregular Heavy Drinking Occasions and Risk of Ischemic Heart Disease: A Systematic Review and Meta-Analysis, Am J Epidemiol 171:633–644. 10.1093/aje/kwp4515. [DOI] [PubMed] [Google Scholar]
- Rutstein SO, Johnson K (2004) DHS Comparative Reports No 6: The DHS Wealth Index https://dhsprogram.com/pubs/pdf/cr6/cr6.pdf. Accessed 7 May 2018.
- Sartorius K, Sartorius B, Tollman S, Schatz E, Kirsten J, Collinson M (2013) Rural Poverty Dynamics and Refugee Communities in South Africa: A Spatial–Temporal Model. Popul Space Place 19:103–123. 10.1002/psp.697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shisana O, et al. (2013) South African National Health and Nutrition Examination Survey (SANHANES-1). HSRC Press: Cape Town http://www.hsrc.ac.za/uploads/pageNews/72/SANHANES-launch%20edition%20(online%20version).pdf. Accessed 7 May 2018.
- Statistics South Africa (2014). Census 2011: Profile of older persons in South Africa (Report no. 03-01-60) https://www.statssa.gov.za/publications/Report-03-01-60/Report-03-01-602011.pdf. Accessed 7 May 2018.
- Tehranifar P, Liao Y, Ferris JS, Terry MB (2009) Life course socioeconomic conditions, passive tobacco exposures and cigarette smoking in a multiethnic birth cohort of U.S. women. Cancer Causes Control 20:867–876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker JS (2002) Health-related social control within older adults’ relationships. J Gerontol B Psychol Sci Soc Sci 57:3873995. [DOI] [PubMed] [Google Scholar]
- United Nations (1963) Apartheid in South Africa: Summary of the Report of the Special Committee on the Policies of Apartheid of the Government of South Africa United Nations, Geneva. [Google Scholar]
- Wiseman M (2008) The second World Cancer Research Fund/American Institute for Cancer Research expert report. Food, nutrition, physical activity, and the prevention of cancer: a global perspective. Proc Nutr Soc 67:253–256. [DOI] [PubMed] [Google Scholar]
- World Health Organization (2010) Global Recommendations on Physical Activity for Health http://www.who.int/dietphysicalactivity/global-PA-recs-2010.pdf. Accessed 7 May 2018. [PubMed]
- World Health Organization (2017a) Countries: South Africa http://www.afro.who.int/countries/south-africa Accessed 7 May 2018.
- World Health Organization (2017b) Obesity and Overweight Fact Sheet http://www.who.int/mediacentre/factsheets/fs311/en/. Accessed 7 May 2018.
- World Health Organization (2018) Tobacco Fact Sheet http://www.who.int/mediacentre/factsheets/fs339/en/. Accessed 7 May 2018.
- Zou G (2004). A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol 159:702–7066. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


