Abstract
BACKGROUND
The 2013 American College of Cardiology (ACC)/American Heart Association (AHA) cholesterol guideline recommends statin treatment based on patients’ predicted atherosclerotic cardiovascular disease (ASCVD) risk. Whether clinician-reported guideline adoption translates to implementation into practice is unknown.
OBJECTIVES
We aimed to compare clinician lipid management in hypothetical scenarios versus observed practice.
METHODS
The Patient and Provider Assessment of Lipid Management (PALM) Registry asked 774 clinicians how they would treat 4 hypothetical scenarios of primary prevention patients with: 1) diabetes; 2) high 10-year ASCVD risk (≥7.5%) with high low-density lipoprotein cholesterol (LDL-C; ≥130mg/dL); 3) low 10-year ASCVD risk (<7.5%) with high LDL-C (130–189 mg/dL); or 4) primary and secondary prevention patients with persistently elevated LDL-C (≥130mg/dL) despite high-intensity statin use. We assessed agreement between clinician survey responses and observed practice.
RESULTS
In primary prevention scenarios, 85% of clinicians reported they would prescribe a statin to a diabetic patient and 93% to a high-risk/high LDL-C patient (both indicated by guidelines), while 40% would prescribe statins to a low-risk/high LDL-C patient. In clinical practice, statin prescription rates were 68% for diabetic patients, 40% for high-risk/high LDL-C patients, and 50% for low-risk/high LDL-C patients. Agreement between hypothetical and observed practice was 64%, 39%, and 52% for patients with diabetes, high-risk/high LDL-C, and low-risk/high LDL-C, respectively. Among patients with persistently high LDL-C despite high-intensity statin treatment, 55% of providers reported they would add a non-statin lipid-lowering medication, while only 22% of patients were so treated.
CONCLUSIONS
While the majority of clinicians report adoption of the 2013 ACC/AHA guideline recommendations, observed lipid management decisions in practice are frequently discordant.
Keywords: lipids, guideline adoption, cardiovascular disease prevention
Treatment of hyperlipidemia is an important part of atherosclerotic cardiovascular disease (ASCVD) prevention and has been shown to reduce mortality and improve patient outcomes (1–6). The release of the 2013 American College of Cardiology (ACC)/American Heart Association (AHA) Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults (7) represented a shift in focus toward treating hyperlipidemia based on underlying risk factors rather than targeting a goal lipid level, as was the main objective of prior guidelines(8). Adoption of these new recommendations and inertia for treatment change in clinical practice may lag behind guideline release. Given the importance of lipid treatment in ASCVD prevention, it is essential to understand how we can expedite guideline adherence in daily clinical practice.
The Patient and Clinician Assessment of Lipid Management (PALM) registry was designed as a nation-wide cross-sectional registry aimed at evaluating the changes in lipid management after the release of the 2013 ACC/AHA guidelines(7). In this study, we examined clinician self-reported adoption of the guidelines via hypothetical scenarios and compared lipid management with observed practice for four patient types: 1) primary prevention patients with diabetes; 2) primary prevention patients with high ASCVD risk/high low-density lipoprotein cholesterol (LDL-C); 3) primary prevention patients with low ASCVD risk/high LDL-C; and 4) primary and secondary prevention patients with persistently high LDL-C despite high-intensity statin use. The first two scenarios reflect patients for whom guidelines provide Class I recommendations on primary prevention statin use; the third scenario reflects patients for whom guidelines no longer recommend routine statin use, but statins may be considered in the appropriate clinical scenario; and the fourth scenario reflects a patient population for whom guidelines provide a Class IIb recommendation for the addition of non-statin lipid-lowering treatment (7).
METHODS
STUDY POPULATION
The PALM registry consists of 7,938 patients enrolled at 140 outpatient cardiology, endocrinology, and primary care practices across the United States. The design, rationale, inclusion, and exclusion criteria for the PALM registry have been previously published (9). After each site obtained institutional review board approval for participation, all clinicians at participating sites were asked to complete a web-based provider survey. Sites were required to have completed surveys for >80% of participating clinicians prior to site activation for patient enrollment.
Patient enrollment was completed between May 27, 2015 and November 12, 2015. Each participant provided signed informed consent to participate. Patients were included in the PALM registry if they had prior ASCVD, active treatment with a statin medication, or were eligible for statin treatment based on the current lipid guidelines. For all patients, chart abstractions and core laboratory lipid panels were conducted to assess current lipid management, as per study protocol. Of the total PALM population, 6,839 had core laboratory data and were treated by a clinician who had completed a provider survey. Subjects were excluded if they were missing ASCVD information (n=4) or age (n=4). Among this study population, 2,297 fit criteria matching one of our four hypothetical patient scenarios described in the provider survey and were included in this analysis.
DATA COLLECTION AND DEFINITIONS
Provider surveys included questions regarding clinician and practice characteristics. Clinicians were asked, “Which guideline do you primarily use to guide cholesterol management in your patients?” and were, therefore, classified as adopters and non-adopters of the 2013 ACC/AHA lipid guidelines. The survey then asked clinicians to report changes in frequency of calculating ASCVD risk and treating to lipid goals in their practice over the last year (answer choices included: do more often, do less often, no change in practice, and I never do this). Next, each survey presented the clinician with four hypothetical patient scenarios (Table 1): 1) a primary prevention patient with diabetes; 2) a primary prevention patient with high ASCVD risk (≥7.5%) and high LDL-C (LDL-C ≥130 mg/dL); 3) a primary prevention patient with low ASCVD risk (<7.5%) and high LDL-C (LDL-C 130–189 mg/dL); and 4) a secondary prevention patient with reported adherence to a high-intensity statin, yet persistently elevated LDL-C (≥130 mg/dL). In the first three primary prevention scenarios, clinicians were asked the likelihood of prescribing statin therapy (answer choices included very likely, likely, neutral, unlikely, and very unlikely). For each scenario, clinicians had the option to use a provided ASCVD risk calculator to help inform their answer. For the fourth scenario, clinicians were asked about next therapeutic step, and answer choices were categorized as adding a non-statin lipid-lowering medication, change to another statin, or no change in treatment.
Table 1.
Hypothetical Scenarios Presented in Clinician Survey
| Patient Scenario | Patient Category | Patient Characteristics | Comorbidities and Symptoms | Blood Pressure | Lipid Data (mg/dL) | Lipid Treatment | 10-year ASCVD Risk |
|---|---|---|---|---|---|---|---|
| 1 | Diabetes | 45 year old African American female | Diabetes Asymptomatic | 145/70 | TC 220 LDL-C 140 HDL-C50 |
Treatment naïve | 6.1% |
| 2 | High risk High LDL-C | 54 year old white male | Active smoker Asymptomatic | 152/70 | TC 221 LDL-C 150 HDL-C 41 |
Treatment naïve | 17.3% |
| 3 | Low risk High LDL-C | 40 year old African American female | No comorbidities Asymptomatic | 130/60 | TC 220 LDL-C 165 HDL-C 30 |
Treatment naïve | 4.4% |
| 4 | High LDL-C despite adherence to male high-intensity statin | 64 year old | Prior CVA Active claudication | N/A | TC 220 LDL-C 130 HDL-C 30 |
Patient-reported adherence to atorvastatin 80 mg daily | N/A |
Scenarios 1–3: Clinicians were asked to answer their likelihood of recommending a statin; if likely or very likely to recommend, clinicians then answered their likelihood of recommending a high-intensity statin.
Scenario 4: Clinicians were asked to recommend next step in treatment: no change, change to different statin, add ezetimibe, add fibrate, add fish oil, add bile acid sequestrant, refer to lipid specialist, other.
ASCVD = atherosclerotic cardiovascular disease; CVA = cerebrovascular accident; HDL-C = high-density lipoprotein cholesterol; LDL-C = low-density lipoprotein cholesterol; TC = total cholesterol
For each enrolled patient, medical records were reviewed to collect detailed sociodemographic and medical history, as well as current and prior lipid-lowering therapy. Prior clinician-ordered lipid testing was identified with chart review, which included laboratory values for the two years prior to enrollment. If completed, the data for the highest LDL-C measurement within the last two years was collected. Each patient underwent phlebotomy on the day of enrollment. Core lab lipid panels were performed by LabCorp (Burlington, NC) and included analysis of total cholesterol, direct LDL-C, high-density lipoprotein cholesterol and triglyceride levels; results were provided to all clinicians. Enrolled patients were grouped according to the ASCVD risk category and lipid levels as described above in alignment with the four hypothetical scenarios. The highest LDL-C measurement (whether clinician ordered within the two years prior to enrollment or measured via core lab) was used to categorize patients in the first three scenarios. Core lab LDL-C levels were used for the fourth scenario.
STATISTICAL ANALYSIS
Characteristics of clinicians who reported adoption of the 2013 ACC/AHA guidelines versus preference for an alternative guideline were compared including clinician type, clinician specialty, practice type, practice location, and number of years in practice. Clinician-reported changes in management practice were grouped by reported adoption of 2013 ACC/AHA guidelines. Categorical variables were presented using frequency and continuous variables were presented using medians (25th and 75th percentiles). Mantel-Haenszel Chi-square test was used for all categorical variables and Wilcoxon test was used to compare differences in continuous variables.
Next, clinician responses to hypothetical patient clinical scenarios were evaluated based on reported adoption of the 2013 ACC/AHA guidelines. Utilizing the definitions from the hypothetical scenarios outlined above, enrolled patients were grouped according to risk category including primary prevention patients with: 1) diabetes, n=1496; 2) high risk (ASCVD risk ≥7.5%) and high LDL-C (LDL-C ≥130 mg/dL), n=457; and 3) low risk (ASCVD risk <7.5%), but high LDL-C (LDL-C 130-189 mg/dL), n=344. Patient data was then linked to survey data for their treating clinician in order to compare hypothetical scenario responses to observed management. Agreement was calculated as the proportion of patients treated the way their clinician said they would treat in the corresponding hypothetical scenario. In order to compare clinicians who answered likely/very likely to treat with clinicians who were unlikely to treat in the hypothetical scenarios, an unadjusted logistic regression model was used to generate an odds ratio (OR) with 95% confidence intervals (CIs) describing the likelihood of statin treatment in diabetes, high-risk/high LDL-C or low-risk/high LDL-C cases, or addition of non-statin lipid-lowering treatment in primary or secondary prevention patients with high LDL-C despite adherence to high-intensity statin. For the fourth scenario (high LDL-C despite adherence to high-intensity statin), we also completed a secondary analysis describing the likelihood of non-statin lipid lowering treatment for secondary prevention patients only.
A p-value of <0.05 was considered significant. All statistical analyses were performed at the Duke Clinical Research Institute using SAS version 9.4 (SAS Institute, Inc., Cary, NC).
This study was supported by Sanofi and Regeneron Pharmaceuticals. The authors are solely responsible for the design and conduct of this study, all study analyses, the drafting and editing of the paper and its final contents.
RESULTS
PROVIDER SURVEY RESULTS
The PALM Registry collected provider surveys for 774 clinicians treating patients at 51 primary care practices, 82 cardiology practices, and 8 endocrinology practices. Among surveyed clinicians, 574 (74.2%) reported that the 2013 ACC/AHA guidelines primarily guides their lipid management, 137 (17.7%) are primarily guided by the Third Report of the Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (ATPIII), 16 (2.1%) by the American Association of Clinical Endocrinologists’ (AACE) Guidelines for Management of Dyslipidemia and Prevention of Atherosclerosis, and 47 (6.2%) use other guidelines or do not apply any of guidelines in practice. Adopters of the 2013 ACC/AHA guidelines were more likely to be cardiologists and were also more likely to report that they had increased the frequency of calculating ASCVD risk and were less likely to treat patients to lipid level targets in their practice than in the last year (Table 2).
Table 2.
Clinician Characteristics by Adopter vs. Non-adopters of the 2013 ACC/AHA Guidelines
| Overall | Clinician-Reported Adoption of 2013 ACC/AHA Guidelines | ||||
|---|---|---|---|---|---|
| N=774 | Yes N=574 (74.2%) | No N=200 (25.8%) | p-value | ||
| Clinician specialty1 | Cardiologist, N (%) | 378 (57.1%) | 293 (60.2%) | 85 (48.6%) | 0.03 |
| Primary Care, N (%) | 234 (35.3%) | 161 (33.1%) | 73 (41.7%) | ||
| Endocrinology, N (%) | 24 (3.6%) | 14 (2.9%) | 10 (5.7%) | ||
| Other, N (%) | 26 (3.9%) | 19 (3.9%) | 7 (4.0%) | ||
| Clinician type | Physician, N (%) | 611 (78.9%) | 452 (78.7%) | 159 (79.5%) | 0.31 |
| Advanced Practice Provider, N (%) | 141 (18.2%) | 102 (17.8%) | 39 (19.5%) | ||
| Clinician-in-training, N (%) | 20 (2.6%) | 18 (3.1%) | 2 (1.0%) | ||
| Other, N (%) | 2 (0.3%) | 2 (0.4%) | 0 (0.0%) | ||
| Office location2 | Rural, N (%) | 83 (12.2%) | 66 (13.0%) | 17 (9.7%) | 0.87 |
| Suburban, % | 205 (30.1%) | 158 (31.2%) | 47 (26.9%) | ||
| Urban, % | 394 (57.8%) | 283 (55.8%) | 111 (63.4%) | ||
| Years in practice | Up to 5 years, % | 162 (20.9%) | 125 (21.8%) | 37 (18.5%) | 0.79 |
| 6-10 years, % | 96 (12.4%) | 71 (12.4%) | 25 (12.5%) | ||
| 10-20 years, % | 233 (30.1%) | 172 (30.0%) | 61 (30.5%) | ||
| Greater than 20 years, % | 283 (36.6%) | 206 (35.9%) | 77 (38.5%) | ||
| Calculate ASCVD risk | Do more often | 353 (45.7%) | 282 (49.2%) | 71 (35.5%) | 0.0002 |
| No change | 317 (41.0%) | 230 (40.1%) | 87 (43.5%) | ||
| Do less often | 33 (4.3%) | 22 (3.8%) | 11 (5.5%) | ||
| Never do this | 70 (9.1%) | 39 (6.8%) | 31 (15.5%) | ||
| Treat to lipid target | Do more often | 125 (16.1%) | 93 (16.2%) | 32 (16.0%) | <0.0001 |
| No change | 410 (53.0%) | 274 (47.7%) | 136 (68.0%) | ||
| Do less often | 224 (28.9%) | 197 (34.3%) | 27 (13.5%) | ||
| Never do this | 15 (1.9%) | 10 (1.7%) | 5 (2.5%) | ||
Clinician specialty for n=670 board certified physicians
Office location had 11.9% missing data but all other fields with < 1.2% missing data
ACC = American College of Cardiology; AHA = American Heart Association; All other abbreviations can be found in Table 1.
In the hypothetical primary prevention patient scenarios, 84.5% of providers reported they were likely to prescribe a statin to the diabetic patient, 92.9% to a high-risk/high LDL-C patient, and 40.2% to a low-risk/high LDL-C patient. Treatment rates were not significantly different between clinicians who reported adoption of the ACC/AHA guidelines versus not (Table 3). Approximately half of the clinicians elected to use the provided risk score calculator before answering the hypothetical scenarios (Table 4). Clinicians who reported adoption of the new guidelines were numerically more likely to employ this tool although the differences were not statistically significant. Clinicians who used the calculator were more likely to prescribe a statin to patients in the high-risk category and were less likely to prescribe a statin to the low-risk/high LDL-C patient (Table 4).
Table 3.
Proportion of Clinicians Very Likely/Likely to Prescribe Statin Therapy in the Primary Prevention Hypothetical Scenarios
| Scenario | All (N=774) | Adopted ACC/AHA Guidelines | ||
|---|---|---|---|---|
| Yes (N=574) | No (N=200) | p-value | ||
| Prescribe Statin Therapy | ||||
| Diabetes | 654 (84.5%) | 483 (84.2%) | 171 (85.5%) | 0.68 |
| High risk/high LDL-C | 719 (92.9%) | 537 (93.6%) | 182 (91.0%) | 0.23 |
| Low risk/high LDL-C | 311 (40.2%) | 234 (40.8%) | 77 (38.5%) | 0.57 |
| Add a Non-Statin Lipid Lowering Treatment | ||||
| High LDL-C despite adherence to high-intensity statin | 398 (51.4%) | 287 (50.0%) | 111 (55.5%) | 0.18 |
Table 4.
Clinician Utilization of Risk Score Calculator and Likeliness of Statin Prescription in Hypothetical Scenarios
| Percent of Clinicians Clicked to Calculate Risk Score | Percent of Clinicians Likely/Very Likely to Prescribe Statin | |||||||
|---|---|---|---|---|---|---|---|---|
| All (N=774) | Adopted New Guidelines | p-value | All (N=774) | Utilized risk score calculator | p-value | |||
| Yes (N=574) | No (N=200) | Yes | No | |||||
| Diabetes | 374 (48.3%) | 283 (49.3%) | 91 (45.5%) | 0.34 | 654 (84.5%) | 312/374 (83.4%) | 342/399 (85.7%) | 0.38 |
| High risk/high LDL-C | 411 (53.1%) | 313 (54.5%) | 98 (49.0%) | 0.18 | 719 (92.9%) | 389 /411 (94.7%) | 330 / 363 (90.9%) | 0.04 |
| Low risk/high LDL-C | 407 (52.6%) | 310 (54.0%) | 97 (48.5%) | 0.18 | 311 (40.2%) | 148 / 407 (36.4%) | 163 / 367 (44.4%) | 0.02 |
All abbreviations can be found in Table 1.
In the scenario of secondary prevention patients with persistently high LDL-C despite treatment with high-intensity statin therapy and maintaining adherence to this therapy, 26.9% of providers would change the statin, 51.4% would add a non-statin lipid-lowering agent (ezetimibe, fibrate, fish oil, or bile acid sequestrant), and 18.0% of clinicians would not change treatment. There was no difference of these medication adjustment rates for clinicians who reported adoption of the new guidelines versus those who did not (p=0.09).
OBSERVED PRACTICE
Next, we examined clinician adherence to guideline recommendations based on statin therapy use among enrolled PALM registry patients. Among enrolled patients, 1,496 patients had diabetes mellitus with no history of ASCVD. Among non-diabetic primary prevention patients, 374 patients were found to be high risk (calculated 10-year ASCVD risk ≥7.5%) and have high LDL-C (LDL-C ≥130 mg/dL). An additional 83 patients had LDL-C ≥190 mg/dL and, consequently, were also classified high risk/high LDL-C, yielding a total of 457 patients. Finally, 344 patients were found to have high LDL-C (LDL-C 130-189 mg/dL), but were low risk (calculated 10-year ASCVD risk <7.5%). Overall, diabetic patients were more likely than other groups to be treated with a statin (Figure 1); however, 475 (31.8%) of the diabetic patients and 282 (61.8%) of the high-risk/high LDL-C patients had no statin prescription at the visit. Among these, only a small number of patients had previously attempted a statin, including 61 (13.1%) of patients with diabetes and 53 (18.8%) of patients with high risk/high LDL-C. High-intensity statin therapy was infrequently prescribed in these populations.
Figure 1. Statin Prescription Patterns.
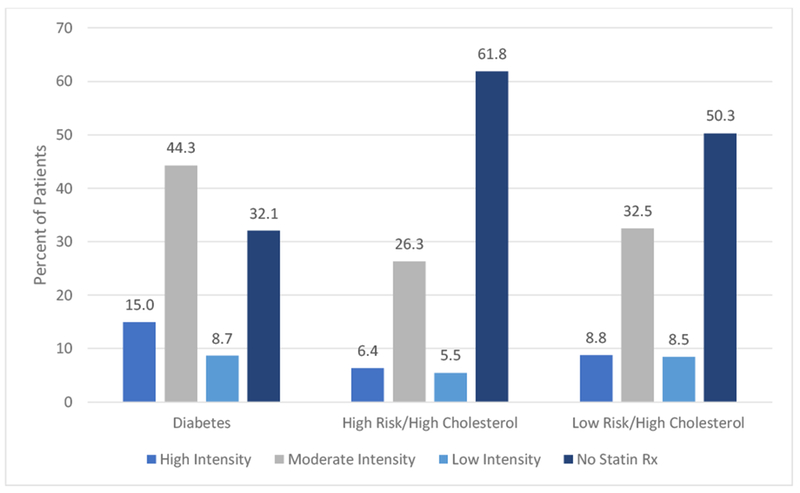
Rates of statin prescription, across statin intensities, among patients with diabetes, high risk/high cholesterol and low risk/high cholesterol.
Among the 288 primary and secondary prevention patients with LDL-C ≥130 mg/dL and already on high-intensity statin therapy, clinicians were observed to change the statin in 8 patients (2.8%), add ezetimibe in 11 patients (3.8%), and add fibrate, fish oil, or bile acid sequestrant in 57 patients (20.0%). The majority of patients (n=217, 75.4%) were managed by continuation of statin therapy without change in drug or dose, nor addition of a non-statin lipid-lowering medication. Similarly, when only secondary prevention patients were examined (n=161), 34 (21.1%) were managed with a non-statin lipid lowering medication.
COMPARING PROVIDER SURVEY RESPONSES WITH OBSERVED PRACTICE
Clinician responses to hypothetical scenarios frequently did not agree with observed statin prescription for similar clinical scenarios among enrolled patients (Table 5). Agreement was highest (63.6%) for patients with diabetes; 68.9% of these patients treated by clinicians who responded likely/very likely to use statin in the hypothetical scenario were treated with a statin at the time of their clinic visit. Among high-risk patients with high LDL-C levels, only 37.7% of patients treated by clinicians who responded likely/very likely to use statin in the hypothetical scenario were actually prescribed a statin. In patients with high LDL-C levels but low risk, 48.3% of the patients seen by clinicians who were unlikely to prescribe a statin in the hypothetical scenario were prescribed statin therapy. In patients with persistently high LDL-C despite high-intensity statin therapy, agreement was 44.1%. When only secondary prevention patients with persistently high LDL-C despite high-intensity statin therapy were evaluated, agreement between hypothetical and observed treatment was similar at 46.6%. Clinicians who would treat in the hypothetical scenario were not more likely to treat in actual practice as shown by the non-significant OR (95% CI) in Table 5.
Table 5.
Agreement between Hypothetical Treatment Responses and Observed Practice
| Hypothetical | Observed | Agreement | OR (95% CI) | |
|---|---|---|---|---|
| Statin Use Rate | ||||
| Diabetes (n=1496) | 1263 (84.4%) | 1021 (68.3%) | 63.6% | 1.20 (0.90, 1.61) |
| High risk/high LDL-C (n=457) | 432 (94.5%) | 175 (38.3%) | 38.5% | 0.65 (0.29, 1.47) |
| Low risk/high LDL-C (n=344) | 137 (39.8%) | 172 (50.0%) | 52.0% | 1.19 (0.77, 1.83) |
| Addition of Non-Statin Lipid-Lowering Treatment | ||||
| High LDL-C despite adherence to high intensity statin | 159 (55.2%) | 62 (21.5%) | 44.1% | 0.70 (0.40, 1.24) |
Non-statin lipid-lowering treatment included addition of ezetimibe in 11 patients, fibrate, fish oil or bile acid sequestrant in 57 patients
Agreement = % of patients treated the way clinician said they would treat in the corresponding hypothetical scenario.
OR = odds ratio for likelihood of treatment when comparing clinicians who reported likely vs. less likely to treat in hypothetical scenarios
CI = confidence interval; OR = odds ratio; All other abbreviations can be found in Table 1.
DISCUSSION
In this analysis of the PALM registry, we compared clinician responses to hypothetical scenarios with the observed treatment of their patients. We demonstrated that: 1) the majority of cardiologists reported adoption of the 2013 ACC/AHA guidelines and were more likely to adopt than primary care physicians or endocrinologists. 2) Clinician responses to hypothetical scenarios do not always align with observed lipid management decisions. 3) When the risk calculator was utilized, more guideline adherence was observed. 4) While clinicians are likely to prescribe statin therapy to patients with diabetes or who are at high risk of ASCVD in hypothetical scenarios, guideline-recommended statin therapy remains under-utilized in these patients in observed practice. 5) Clinicians have mixed management patterns in patients with elevated LDL-C in the absence of high ASCVD risk, as well as in patients with persistently elevated LDL-C in the presence of high-intensity statin use.
The release of the 2013 ACC/AHA lipid management guidelines resulted in a shift in management of blood lipid levels. In contrast to the Adult Treatment Panel III (ATP III) recommendations (8), which focused on achieving a target LDL-C level, the 2013 guidelines emphasize statin intensity dosing based on underlying risk (7). We observed that cardiologists were more likely to report adoption of the new guidelines when compared with primary care physicians and endocrinologists, which may be a reflection of the availability of different society guideline recommendations, including those published by the United States Preventive Services Task Force (1,10) and the American Association of Clinical Endocrinologists (11). Not surprisingly, clinicians who reported adoption of the 2013 ACC/AHA guidelines were also more likely to calculate ASCVD risk (a key component in determining the need for statin therapy in these guidelines) and were less likely to treat to an LDL-C goal.
Next, we examined whether clinician responses to hypothetical scenarios aligned with practice decisions. We specifically chose both scenarios with strong recommendations across guidelines (patients with high ASCVD risk and high cholesterol, patients with diabetes) and scenarios where guideline recommendations are ambivalent or offer less firm recommendations (low ASCVD risk and high cholesterol, persistently elevated LDL-C despite high intensity statin use). While the majority of clinicians responded to the survey questions according to guideline recommendations, this was not reflected in observed practice.
The ACC/AHA guidelines provide Class I recommendations for high-intensity statin therapy for patients with LDL-C >190 mg/dL (level of evidence B), at least moderate-intensity statin for patients with an estimated 10-year ASCVD risk ≥7.5% (level of evidence B), or those with diabetes (level of evidence A). In these scenarios, one might expect more consistent management among clinicians. Treatment rates were highest among diabetic patients, and the agreement between hypothetical and observed practice was also highest for these patients. For patients with high ASCVD risk and an LDL-C ≥130 mg/dL, the hypothetical statin treatment rate was 93%, but only 40% of these patients were observed to be on statin therapy. These results echo prior studies that showed statin underutilization and underdosing even among high-risk patients(12) (13). Little of this is explained by discontinuation of a prior statin attempt. Additionally, when statin medications were prescribed in our study, they were frequently under-dosed based on the 2013 ACC/AHA guidelines. Untreated or undertreated patients may represent missed treatment opportunities and unsuccessful previously attempted statin therapy.
In contrast, the 2013 ACC/AHA guidelines no longer recommend routine statin use for all patients with low ASCVD risk, but LDL-C levels 130–189 mg/dL; rather, these new guidelines suggest statin use based on clinical judgment and discussions with individual patients. However, the prior ATP III guidelines would support initiation of pharmacologic lipid treatment with LDL-C >160 mg/dL and the American Association of Clinical Endocrinologists guidelines currently recommend treatment for the low-risk patient to achieve an LDL-C <130 (14). In the setting of guideline change or conflicting guideline recommendations, it is not surprising to observe heterogeneity in treatment. In provider surveys, 40% of clinicians reported statin use, and half of patients in observed practice were treated with statin therapy. Similar practice inertia was seen for patients with persistently elevated LDL-C levels despite high-intensity statin use. The ACC/AHA guidelines provide a weak Class IIb recommendation to consider the addition of non-statin lipid-lowering treatment. Provider surveys and observed practices also showed mixed responses in this setting. Further data to support firmer guideline recommendations across patient risk groups and differing guideline committees may help to bridge this gap.
However, independent of the strength of guideline recommendations, this study showed a persistent disconnect between clinician self-reported treatment patterns (perceived care) and observed treatment patterns (actual care). While some of the statin underutilization observed in our study could be attributed to a delay between guideline publication and clinician uptake in practice, this does not fully explain the observed discrepancy. The discordance between hypothetical and observed treatment patterns suggests that the problem is not clinician gaps in knowledge or misinterpretation of the guideline leading to inappropriate application (18). While clinicians generally respond “correctly” to hypothetical scenarios according to guideline recommendations, this knowledge does not appear to fully translate to action. Patients may decide not to start statin therapy after having a risk discussion with their treating provider; providers may not be readily able to calculate patient risk or review blood lipid results in a busy clinical setting. While the hypothetical scenarios display all the relevant information necessary to evaluate appropriate treatment candidacy in one location, several clicks and chart searches may be required in electronic health records. In our study, clinicians who utilized the provided ASCVD risk calculator in the hypothetical settings were significantly more likely to prescribe a statin in the hypothetical high-risk/high LDL-C patient and less likely to prescribe a statin in the hypothetical low-risk/high LDL-C patient. Embedded ASCVD risk calculators are well within the capabilities of electronic health records and offer assessment of statin candidacy to busy clinicians.
CLINICAL IMPLICATIONS AND FUTURE STEPS
Translation of care from guideline recommendations to patients seen in daily practice remains a challenge. Although clinicians demonstrated good knowledge of the 2013 ACC/AHA guidelines on treatment of blood lipid levels, a disconnect persisted in the treatment of our patients. It will be important, moving forward, to utilize all tools available, including those within the electronic health record, in order to effectively change practice. A multifaceted quality improvement system, with risk stratification tools, patient education and frequent feedback to providers may help to bridge the gap between provider perception of care and known limitations in guideline recommended statin prescription. Similar coupling of risk stratification tools with interventions to remind clinicians as part of the routine clinical work flow (e.g., best practice alerts), educate patients at the point of care (e.g., shared decision-making tools), and facilitate treatment ordering (e.g., order sets) have been shown to improve guideline adherence in areas such as health screening and vaccinations, and can be easily translated to hyperlipidemia management and cardiovascular risk factor reduction (19–21).
STUDY LIMITATIONS
Our study had several limitations. First, given the observational nature of our examination, rationale for clinician management decisions at the time of the clinic appointment is not available. Second, while prior lipid testing results were abstracted via chart review, we could not assess whether these lipid levels were measured prior to or after statin initiation. Therefore, we could only examine patients with high LDL-C (with or without high ASCVD risk) and could not study patients with low LDL-C levels since we could not discern whether this was a treatment effect. Third, ASCVD risk was calculated for patients treated and not treated with statin medications. Calculating the ASCVD risk for patients on statin therapy may underestimate their risk; therefore, some patients who were high risk prior to statin treatment, but low risk with statin therapy, may have been excluded from the high-risk groups. Fourth, lower treatment rates with statins in the primary prevention setting could partially be related to patients opting not to take statin therapy after having a risk discussion with their treating provider. Finally, a minority of patient data could not be linked to their clinician; as a result, these patients were excluded from this analysis. Similarly, clinicians without linked patient data were also excluded from analyses of clinic management decisions.
CONCLUSIONS
Since the release of the 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults, there has been variable uptake in implementation of these guidelines, with cardiologists reporting the highest guideline adoption. Despite recommendations, statin therapy remains under-utilized in primary prevention patients with diabetes or with high ASCVD risk. Additional clinician treatment uncertainty remains around the management of patients with low ASCVD risk, but elevated LDL-C, as well as in patients with persistent elevation of LDL-C despite high-intensity statin use. While the majority of clinicians respond to hypothetical scenarios in accordance to guideline-directed treatment of blood lipid levels, this does not translate into their observed clinical practice. Important gaps in care persist, particularly among patients in high-risk groups where lack of treatment and under treatment remain prevalent. These results suggest gaps in implementation rather than clinician knowledge. Improved utilization of electronic health record-based tools and interventions may help improve clinician adherence to guideline recommendations.
Acknowledgements
We thank Erin Campbell, MS, for her editorial contributions to this article. Ms. Campbell did not receive compensation for her assistance, apart from her employment at the institution where this study was conducted. This study was funded by Sanofi and Regeneron Pharmaceuticals.
Sources of funding:
This study was funded by Sanofi and Regeneron Pharmaceuticals.
ABBREVIATIONS
- ACC
American College of Cardiology
- AHA
American Heart Association
- AACE
American Association of Clinical Endocrinologists
- ASCVD
atherosclerotic cardiovascular disease
- ATP III
Adult Treatment Panel III
- CI
confidence interval
- LDL-C
low-density lipoprotein cholesterol
- OR
odds ratio
- PALM
Patient and Clinician Assessment of Lipid Management
Footnotes
Dr. Lowenstern received funding through NIH T-32 training grant #5 T32 HL069749-14.
2 Ms. Li reports no relevant disclosures.
Dr. Navar reports research support from Amgen, Sanofi, and Regeneron; consulting fees from Amgen and Sanofi.
Dr. Virani reports research support from ADA/AHA/ VA; honorarium from ACC as the Associate Editor for Innovations, ACC.org.
Dr. Lee reports employment with Sanofi.
Dr. Louie reports employment with Regeneron Pharmaceuticals, Inc.; ownership interest in Regeneron Pharmaceuticals, Inc.
Dr. Peterson reports research support from Eli Lilly, Janssen, Merck, Consulting from AstraZeneca, Bayer, Boehringer Ingelheim, Genentech, Janssen, Merck, and Sanofi Aventis;
Dr. Wang reports research support from AstraZeneca, Daiichi Sankyo, Eli Lilly, Gilead, Glaxo SmithKline, Regeneron, Sanofi; consultant/advisory/education from Bristol Myers Squibb, Astra Zeneca, Eli Lilly, Premier, Inc.
REFERENCES
- 1.Chou R, Dana T, Blazina I, Daeges M, Jeanne TL. Statins for Prevention of Cardiovascular Disease in Adults: Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA 2016;316:2008–2024. [DOI] [PubMed] [Google Scholar]
- 2.Ray KK, Cannon CP, McCabe CH et al. Early and late benefits of high-dose atorvastatin in patients with acute coronary syndromes: results from the PROVE IT-TIMI 22 trial. J Am Coll Cardiol 2005;46:1405–10. [DOI] [PubMed] [Google Scholar]
- 3.Pedersen TR, Faergeman O, Kastelein JJ et al. High-dose atorvastatin vs usual-dose simvastatin for secondary prevention after myocardial infarction: the IDEAL study: a randomized controlled trial. JAMA 2005;294:2437–45. [DOI] [PubMed] [Google Scholar]
- 4.LaRosa JC, Grundy SM, Waters DD et al. Intensive lipid lowering with atorvastatin in patients with stable coronary disease. The New England journal of medicine 2005;352:1425–35. [DOI] [PubMed] [Google Scholar]
- 5.Cannon CP, Blazing MA, Giugliano RP et al. Ezetimibe Added to Statin Therapy after Acute Coronary Syndromes. The New England journal of medicine 2015;372:2387–97. [DOI] [PubMed] [Google Scholar]
- 6.Sabatine MS, Giugliano RP, Keech AC et al. Evolocumab and Clinical Outcomes in Patients with Cardiovascular Disease. The New England journal of medicine 2017;376:1713–1722. [DOI] [PubMed] [Google Scholar]
- 7.Stone NJ, Robinson JG, Lichtenstein AH et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014;129:S1–45. [DOI] [PubMed] [Google Scholar]
- 8.National Cholesterol Education Program Expert Panel on Detection E, Treatment of High Blood Cholesterol in A. Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 2002;106:3143–421. [PubMed] [Google Scholar]
- 9.Navar AM, Wang TY, Goldberg AC et al. Design and rationale for the Patient and Provider Assessment of Lipid Management (PALM) registry. American heart journal 2015;170:865–71. [DOI] [PubMed] [Google Scholar]
- 10.Force USPST. Final Recommendation Statement: Lipid Disorders in Adults (Cholesterol, Dyslipidemia): Screening., December 2014.
- 11.Jellinger PS, Smith DA, Mehta AE et al. American Association of Clinical Endocrinologists’ Guidelines for Management of Dyslipidemia and Prevention of Atherosclerosis: executive summary. Endocr Pract 2012;18:269–93. [DOI] [PubMed] [Google Scholar]
- 12.Salami JA, Warraich H, Valero-Elizondo J et al. National Trends in Statin Use and Expenditures in the US Adult Population From 2002 to 2013: Insights From the Medical Expenditure Panel Survey. JAMA Cardiol 2017;2:56–65. [DOI] [PubMed] [Google Scholar]
- 13.Gu Q, Paulose-Ram R, Burt VL, Kit BK. Prescription cholesterol-lowering medication use in adults aged 40 and over: United States, 2003-2012. NCHS Data Brief 2014:1–8. [PubMed] [Google Scholar]
- 14.Jellinger PS, Handelsman Y, Rosenblit PD et al. American Association of Clinical Endocrinologists and American College of Endocrinology Guidelines for Management of Dyslipidemia and Prevention of Atherosclerosis. Endocr Pract 2017. [DOI] [PubMed] [Google Scholar]
- 15.Newby LK, LaPointe NM, Chen AY et al. Long-term adherence to evidence-based secondary prevention therapies in coronary artery disease. Circulation 2006;113:203–12. [DOI] [PubMed] [Google Scholar]
- 16.Schoen MW, Salas J, Scherrer JF, Buckhold FR. Cholesterol treatment and changes in guidelines in an academic medical practice. Am J Med 2015;128:403–9. [DOI] [PubMed] [Google Scholar]
- 17.Pencina MJ, Navar-Boggan AM, D’Agostino RB Sr. et al. Application of new cholesterol guidelines to a population-based sample. The New England journal of medicine 2014;370:1422–31. [DOI] [PubMed] [Google Scholar]
- 18.Virani SS, Pokharel Y, Steinberg L et al. Provider understanding of the 2013 ACC/AHA cholesterol guideline. J Clin Lipidol 2016;10:497–504 e4. [DOI] [PubMed] [Google Scholar]
- 19.Grimshaw JM, Russell IT. Effect of clinical guidelines on medical practice: a systematic review of rigorous evaluations. Lancet 1993;342:1317–22. [DOI] [PubMed] [Google Scholar]
- 20.Unverzagt S, Oemler M, Braun K, Klement A. Strategies for guideline implementation in primary care focusing on patients with cardiovascular disease: a systematic review. Fam Pract 2014;31:247–66. [DOI] [PubMed] [Google Scholar]
- 21.Jeffery RA, To MJ, Hayduk-Costa G et al. Interventions to improve adherence to cardiovascular disease guidelines: a systematic review. BMC Fam Pract 2015;16:147. [DOI] [PMC free article] [PubMed] [Google Scholar]


