Abstract
In a study of 199 couples in which one person had type 1 diabetes, we examined how patient appraisal of the diabetes as shared versus individual was associated with collaborative, supportive and unsupportive behavior and whether patient shared illness appraisal was most beneficial for health when it occurred in the context of supportive behavior. We assessed illness appraisal among patients with type 1 diabetes and their partners and had patients complete relationship and health measures. Results showed partners were more likely than patients to hold shared illness appraisals. Patients’ shared appraisals were associated with more collaborative and instrumental support, more emotional support, less protective buffering, and more overprotective behavior. When patients and partners were consistent in their shared appraisals, support was highest. Regression analysis showed collaborative and instrumental support, as well as emotional support, was related to better psychological and physical health when patients held shared compared to individual illness appraisals.
Keywords: Communal coping, dyadic coping, type 1 diabetes, social support, couples
It is increasingly recognized that individuals cope with stress within a social context. Stressors not only affect the individual but also their social network, and the social network influences how the individual copes with stressors (Afifi, Hutchinson, & Krouse, 2006; Berg & Upchurch, 2007; Bodenmann, 1997; Helgeson et al., 2018; Lee & Roberts, 2018; Lyons, et al., 1998; Revenson, 1994). Communal coping is an interpersonal coping perspective that is well-suited to the situation in which a coupled individual faces a chronic illness. Illnesses such as type 1 diabetes involve daily stressors (e.g., highs and lows in blood glucose, forgetting to check blood glucose) that frequently affect not only the person with diabetes but close relationship partners (Berg et al., 2013). Communal coping is defined as one person’s perception that the illness is shared and that there is collaboration to manage the illness and its demands (Helgeson et al., 2018; Lyons et al., 1998). A shared illness appraisal is an individual’s perception that the illness is “our problem” rather than “my problem” or “your problem.” Collaboration reflects joint input, mutual effort, and a team approach to successfully manage a problem (Berg, Schindler, & Maharajh, 2008; Berg et al., 2011). For chronic illnesses like type 1 diabetes, illness management involves problems that may benefit from a shared appraisal and collaboration.
A number of theorists have focused on the collaboration component of communal coping. Collaboration is a prominent feature of Berg and Upchurch’s (2007) model of dyadic coping that occurs when the resources of both patient and partner are activated to deal with chronic illness. Positive outcomes result when dyadic coping involves support or collaboration (Berg, Wiebe et al., 2008), and negative outcomes result when dyadic coping involves control strategies such as protective buffering (Hagedoorn et al., 2000) or uninvolvement. Similarly, Bodenmann (1997) outlined a number of positive dyadic coping strategies, one of which—common dyadic coping—largely reflects collaboration (i.e., joint problem-solving, joint information-seeking), but also includes other positive ways of relating to one another (e.g., relaxing together). Patient common dyadic coping has been linked to diet and exercise adherence among persons with type 2 diabetes (Johnson et al., 2013) and to fewer depressive symptoms 5 months later among women with breast cancer (Rottman et al., 2015). The common dyadic coping scale is the subscale that shows the strongest links to good health outcomes (Falconier et al., 2015).
Much less attention has been devoted to illness appraisals, a component of communal coping that sets it apart from other interpersonal coping frameworks. The majority of research on illness appraisal has inferred an individual’s shared appraisal from linguistic markers of “we-language” that occur in the context of illness discussions. Individuals’ we-language has been linked to better relationship quality and good health (Helgeson et al., 2016; Rentscher et al., 2017). However, we-language is an indirect measure of shared illness appraisal, and does not take into consideration the context of the we-language. For instance, it does not distinguish instances in which “we-language” is tied to the illness (e.g., “We should start exercising together”) from instances in which “welanguage” is unrelated to the illness (e.g., “We dislike this discussion”). That is, the measurement of we-language—though in the context of illness-related discussions—is devoid of specific references to the illness. To address the limitations of indirect measures of illness appraisal, we use explicit measures of patient and partner illness appraisal and examine their implications for patient relationship and health outcomes.
Patient shared illness appraisal should be connected to greater supportive (both emotional and instrumental) and collaborative behaviors involving the partner. When patients perceive that the illness is shared, it may be easier for them to ask for support from partners because they recognize their partners play an active role in diabetes management (Helgeson et al., 2018). Patients may also be more receptive to support offered by partners because such support is perceived as teamwork or “working together” toward a common goal rather than assistance provided to the patient which could be perceived as threatening (Bolger & Amarel, 2007). Similarly, when partners perceive the patient’s illness as shared, it may be easier for them to provide support and collaborate with the patient in managing the illness. Partners with a shared illness appraisal expect to be involved in diabetes management, which may make them feel more comfortable providing support and not feel as if they are overstepping any bounds in doing so. When patients and partners are consistent in shared illness appraisals, they are most likely to work together to manage the illness (Helgeson et al., 2018).
Not only do we expect patient and partner shared illness appraisals to be related to greater collaboration, greater partner provision of support and to positive patient relationship and health outcomes, we also expect these collaborative and supportive behaviors to be more beneficial in the context of a patient’s shared rather than individual illness appraisals (Helgeson et al., 2018). Although there is a large literature that has linked social support to good relationship and health outcomes (see Thoits, 2011; Uchino, 2009; for reviews), there is also a substantial literature on miscarried helping that shows support efforts may fail, may not always be perceived as intended, may not be welcomed, and may undermine self-efficacy (e.g., Bolger & Amarel, 2007; McClure et al., 2014; Rafaeli & Gleason, 2009; Vangelisti, 2009). This literature has shown that it is people’s reports of received support that is most likely to be unrelated or inversely related to poor health rather than perceived availability of support. Reasons for adverse effects of support receipt include threats to self-efficacy, undermining of relationship equity, and individual differences factors that moderate perceived partner responsiveness to support (McClure et al., 2014; Rafaeli & Gleason, 2009). When the patient perceives the illness to be a joint problem and construes partner assistance as “working together,” these problems should be less likely to occur. That is, illness appraisal should moderate the relation of collaboration and received support to relationship and health outcomes.
There is some evidence to support the idea that patient illness appraisal affects the relation of collaboration and support to health. A study of couples in which one person had type 2 diabetes showed that diet-related support was related to decreases in diabetesrelated distress when illness responsibility was appraised as shared but was unrelated to diabetes-related distress when illness responsibility was not shared (Stephens et al., 2013). However, shared illness appraisals were measured by consensus between patient and partner in this study, likely inflating the extent to which patients perceived the illness to be shared. In a study of adolescents with type 1 diabetes, parent-child collaboration was related to more effective teen coping for adolescents who held a shared illness appraisal (viewed diabetes as shared between teen and parent) but less effective coping for adolescents who held an individual appraisal (viewed diabetes as belonging only to teen; Berg et al., 2009).
Given the dearth of literature on the appraisal aspect of communal coping and the potential for illness appraisal to affect how individuals perceive illness-related support, the present study undertook a more intensive examination of patient and partner shared illness appraisal in the context of couples in which one member had type 1 diabetes. Although there is a large literature on children with type 1 diabetes and adults with type 2 diabetes, literature on adults with type 1 diabetes is surprisingly sparse. We had four goals. First, we sought to describe the extent to which patients and partners reported shared illness appraisals and whether similar frequencies of shared appraisals were reported across patients and partners. Second, we aimed to examine whether patient demographic and disease background variables are linked to patient shared appraisals. Antecedent variables to shared illness appraisals have been neglected by previous research (Helgeson et al., 2018). To the extent that patient shared illness appraisals are found to have positive links to relationships and health, it is important to examine whether there are certain groups of people (i.e., those who have been married longer, those who are older) who are more likely to hold these appraisals. Third, we examined whether patient shared appraisals were linked to patient reports of collaborative, supportive, and unsupportive behaviors, hypothesizing that patient shared appraisals would be associated with patients’ reports of greater collaboration with partners, greater support received from partners, and fewer negative interactions with partners. Fourth, we examined whether consistent patient and partner shared illness appraisals were associated with even greater patient reports of collaboration and support.
Finally, we examined whether patient shared illness appraisals were linked to patient health outcomes, specifically hypothesizing that they would moderate the links of collaboration and support to health. We focus on interactions of patient appraisals with their perceptions of collaboration and support because we are focusing here on patient health outcomes. We examined a range of patient health outcomes that represented aspects of both mental health and physical health and that were general and diabetesspecific. We measured collaboration and distinguished between the receipt of emotional support (i.e., support aimed to make one feel loved and cared for) and instrumental support (i.e., support aimed to help one with tasks). The two previously described studies (Berg et al., 2009; Stephens et al., 2013) showed that illness appraisal moderated relations of instrumental support and collaboration to health outcomes, but moderation involving emotional support has not been examined. Interestingly, the literature that links support receipt to negative outcomes shows that those relations are more likely to occur in the context of emotional than instrumental support (McClure et al., 2014). Thus, shared illness appraisal might be especially helpful in the context of emotional support. We predicted that collaboration, instrumental support, and emotional support would each be more strongly linked to good patient health outcomes in the context of patient shared rather than individual appraisal.
Method
Participants
The sample included 199 couples (total of 398 individuals). The majority of the sample was married (92%) and the remainder were cohabiting, with the vast majority (97%) in heterosexual relationships with an average relationship length of 19.36 years (SD = 14.56). Patients were average age 46.81 (SD = 13.95), and partners were average age 46.40 (SD = 14.17). The majority of patients were white (90%) and non-Hispanic (94%); 52% were female. Patients had been diagnosed with type 1 diabetes for 26.97 years (SD = 13.88) and had an average HbA1c of 7.57 (SD = 1.06). Just over two-thirds (69%) used an insulin pump, and 43% used continuous glucose monitoring.
Procedure
Participants were recruited from two university-affiliated endocrinology clinics in REMOVED FOR BLINDING. Study procedures were approved by the Universities’ Institutional Review Boards. Participants were eligible to participate if they were 25 years of age or older, had a diagnosis of type 1 diabetes for at least one year, were taking insulin for type 1 diabetes within 1 year of diagnosis, spoke English as their primary language, and were married or in a cohabitating relationship for at least one year.
At the REMOVED FOR BLINDING site, patients were approached in the clinic by their diabetes care provider who obtained permission to release their name to the project director. If patients agreed, the project director called to explain the study in detail. After patients agreed to participate, partner contact information was obtained. If partners agreed to participate, couples were enrolled in the study. Of the 206 patients approached in the clinic, 4 declined to have their contact information forwarded to the project director. Of the 202 contacted by the project director, 47 were ineligible (including 2 who were found to be ineligible after they had started study procedures), 57 declined participation, and 6 could not be reached to determine eligibility. Thus, 92 couples were scheduled and included in the study.
At the REMOVED FOR BLINDING site, a trained research assistant approached the patient in the clinic and provided information about the study. If patients agreed to participate, contact information was obtained from partners, and partners were contacted by a research assistant about the study. Of the 319 patients approached and screened for eligibility, 66 were deemed ineligible and 118 declined participation. Of the remaining 135 couples, 107 were scheduled and included in the study.
Thus, the final sample included 199 couples across both sites. Participants at the first site were older (p < .01) and had diabetes for a longer period of time (p < .05) than participants at the second site, but differed on no other demographic variable. There were no site differences in illness appraisal; collaborative, supportive, or unsupportive behaviors; or any of the outcomes with the exception of self-care which was higher in the first than the second site (p < .01). More detail is provided on recruitment elsewhere (REMOVED FOR BLINDING). Informed consent was obtained from all individual participants included in the study. Once patients and partners were recruited for the study, they were emailed on-line surveys (that included consent) to complete at home prior to the in-lab visit. Couple members were asked to complete these separately. During the laboratory visit, couple members provided written consent for all study procedures and were placed in separate rooms to complete an additional online questionnaire and a brief interview. The SF-12 health survey was the only measure completed at home; all other instruments described below were completed separately in the lab. Glycemic control was obtained from patients in the lab during the study visit. Couples were compensated for study participation.
Instruments
With the exception of the illness appraisal measure, all other instruments were completed only by patients.
Illness appraisal.
Each participant was asked: “When you think about diabetes, choose one of the following phrases that best describes how you think about it.” Patients chose from the following options: “It is my issue to deal with”; “It is my issue, but I know it affects my partner”; “It is a shared issue”; or, “It is my partner’s issue to deal with.” Partners chose from the following options: “It is my partner’s issue to deal with”; “It is my partner’s issue, but I know it affects me”; “It is a shared issue”; or, “It is my issue to deal with.” No patients or partners said that it was completely the partner’s issue. This measure has been used in previous research and is linked to other measures of illness appraisal (Zajdel et al., 2016).
Collaborative, supportive, and unsupportive behaviors.
Collaborative, supportive and unsupportive behaviors relevant to diabetes were based on previous measures (Berg et al., 2011; Helgeson et al., 2016). Items were developed to reflect three positive behaviors: collaboration (i.e., couple working together on joint problem solving), patient receipt of partner emotional support (i.e., understanding, validation), patient receipt of partner instrumental support (i.e., assistance, advice); three negative behaviors: partner avoidance (i.e., avoid discussing diabetes, changing topic), partner overprotective behavior, and partner criticial behavior (i.e., criticism, argument, nagging); and two behaviors that are not clearly positive or negative: patient protective buffering (i.e., shielding partner from distress by hiding worries and acting as if nothing was the matter) and partner social control (i.e., directing patient behavior). Patients were asked to indicate how often their partner engaged in each behavior during the past month on a 5-point scale ranging from 1 (not at all) to 5 (very often).
Relationship quality.
Patients completed the 16-item version of the Couples Satisfaction Index (CSI-16; Funk & Rogge, 2007). Reliability was excellent (α = .97).
SF-12 Health Survey (SF-12).
The SF-12 is a shorter version of the SF-36 (Ware et al., 1993), which has been used to evaluate health-related quality of life in numerous healthy and chronically ill populations (Ware, Kosinski, & Keller, 1996). The Mental Health Component Score (MCS) and the Physical Health Component Score (PCS) were created. The internal consistency of the PCS-12 is reported to be between .86 and .89 and the MCS-12 between .76 and .77. Higher numbers indicate better functioning.
Depressive symptoms.
Patients completed the Center for Epidemiologic Studies Depression Scale (CES-D; Radloff, 1977), a 20-item self-report measure of depressive symptoms over the past week. Items were rated on a 0 (rarely or none of the time) to 3 (most or all of the time) scale. Reliability was good (α = .90).
Diabetes regimen distress.
Patients completed the 17-item Diabetes Distress Scale (DDS; Polonsky et al., 2005) to assess the distress individuals living with diabetes experience. We examined the subscale that was most relevant to taking care of diabetes: regimen distress (e.g., “Feeling that I am not checking my blood sugars frequently enough”; α = .85). Patients were asked to “indicate the degree to which each item may be bothering you in your life” from 1 (not a problem) to 6 (a very serious problem).
Self-care behavior.
Patients completed the revised Self Care Inventory (Lewin et al., 2009) to measure adherence. One item from the original measure (“ketone testing”) was dropped based on healthcare provider recommendations, leaving 13 items from the original scale. Patients rated how often they engaged in each recommended behavior (e.g., glucose checking, administering correct insulin dose) in the past month from 1 (did not do) to 5 (always did without fail). The scale had acceptable reliability (α = .76).
HbA1c.
Both sites used the DCA Vantage to obtain a measure of patient hemoglobin A1c (HbA1c) during the laboratory visit.
Overview of the Analysis
First, we conduct a principal components analysis of the collaborative, supportive, and unsupportive behavior items to determine if the items measure the distinct constructs outlined above. We use an oblimin rotation to allow factors to be correlated. Second, we report frequencies of patient and partner illness appraisals and examine their relation with a chi-square. Third, we examine whether demographic or disease variables are related to patient shared illness appraisal with t-tests and chi-square. To the extent demographic or disease variables are linked to patient appraisal, we statistically control for them in subsequent analyses. We use analysis of covariance to compare patients with a shared appraisal to patients with an individual appraisal on collaborative, supportive, and unsupportive behaviors. To elaborate on this issue, we examine whether consistency in patient and partner illness appraisals is related to the same collaborative, supportive, and unsupportive behaviors with analyses of covariance. We use regression analysis to examine links of patient appraisal to patient health outcomes and whether patient shared appraisals interact with supportive behaviors to predict these same health outcomes. We enter covariates and partner appraisal on the first step, patient appraisal and the relevant supportive behavior on the second step, and the interaction of patient appraisal with the supportive behaviors on the final step of the equation. When the interaction is not significant, we interpret the main effects and show the second step of the equation as the final step. As described in the factor analysis below, there were two distinct supportive behaviors, so we conducted these analyses twice—once for each of the two behaviors. In each analysis, the supportive behavior is centered before computing the interaction term.1
Results
Collaborative, Supportive, and Unsupportive Behaviors
A principal components analysis of the 28 items followed by oblimin rotation revealed 6 factors but several problematic items. The three social control items (“reminded me of the things I needed to do to manage my diabetes,” “tried to get me to improve how I take care of my diabetes,” “persuaded me to do more to manage my diabetes”) loaded on two factors—one that contained the three critical items and one that contained collaborative and instrumental support. (In hindsight, this is not surprising as social control has revealed mixed relations to outcomes; Helgeson, Novak, Lepore, & Eton, 2004; Lewis & Rook, 1999). In addition, one of the emotional support items was ambiguous (“pointed out my strengths in managing diabetes”), and loaded on both the instrumental and emotional support factors. After we removed these four items, we reran the analysis. The results of that analysis, shown in Table 1, largely corresponded to the hypothesized constructs. The first factor consisted of the three collaboration and four instrumental support items. Because these items could not be empirically distinguished, we collapsed them to form a single collaborative and instrumental support index (CIS; 7 items, alpha = .94). The other factors reflected critical behavior (3 items, alpha = .92), avoidance (4 items, alpha = .78), protective buffering (3 items, alpha = .82), overprotection (3 items, alpha = .61), and emotional support (4 items, alpha = .80).
Table 1.
Supportive and Unsupportive Behaviors - Results of Principal Components Analysis followed by Oblimin Rotation: Factor Loadings
| 1 | 2 | 3 | 4 | 5 | 6 | ||
|---|---|---|---|---|---|---|---|
| Collaboration | My partner and I discussed how to best manage diabetes. | .86 | |||||
| Collaboration | My partner and I worked together to manage diabetes. | .88 | |||||
| Collaboration | My partner and I made decisions together for diabetes management. | .94 | |||||
| Instrumental support | Helped me to figure out how to take care of diabetes. | .83 | |||||
| Instrumental support | Suggested things that might help me manage diabetes. | .68 | |||||
| Instrumental support | Helped me decide if I needed to make changes in managing diabetes. | .75 | |||||
| Instrumental support | Helped me with my diabetes care activities. | .64 | |||||
| Critical behavior | Criticized how I take care of diabetes. | .88 | |||||
| Critical behavior | Argued with me about how I take care of diabetes. | .87 | |||||
| Critical behavior | Nagged me about not taking care of diabetes. | .82 | |||||
| Avoidance | Encouraged me to stop dwelling on diabetes. | .87 | |||||
| Avoidance | Told me that I worry too much about diabetes. | .81 | |||||
| Avoidance | Changed the topic of diabetes to a happier one. | .76 | |||||
| Avoidance | Found a way to avoid discussing diabetes. | .60 | |||||
| Protective buffering | I tried to hide my worries about diabetes from my partner. | .84 | |||||
| Protective buffering | I tried to prevent my partner from worrying about diabetes. | .89 | |||||
| Protective buffering | I tried to act as if nothing was the matter when I was having problems with diabetes. | .81 | |||||
| Overprotection | Thought that I couldn’t take care of myself. | .59 | |||||
| Overprotection | Thought that he/she needed to be around for me to take proper care of diabetes. | .60 | |||||
| Overprotection | Continuously kept an eye on me. | .56 | |||||
| Emotional support | Was there for me by giving me his/her undivided attention | .76 | |||||
| Emotional support | Tried to understand my situation | .70 | |||||
| Emotional support | Listened to me talk about my feelings | .73 | |||||
| Emotional support | Tried to put him/herself in my shoes. | .64 |
Patient and Partner Appraisal Descriptives
The majority of patients appraised the illness as their own issue but affected the partner (68%). The majority of partners said the issue was shared (69%). However, patient and partner responses were related, X2(1) = 9.96, p < .005. Specifically, 8% of patients and 2% of partners said the illness was only the patient’s issue, 68% of patients and 29% of partners said the illness was the patient’s issue but affected the partner, and 24% of patients and 69% of partners said the illness was a shared issue. (Data from one partner are missing because she could not decide between two responses.) For analysis purposes, we combined “patient issue only” and “patient issue but affects the partner” into patient individual appraisal because both responses indicate that it is the individual patient’s issue to deal with and there were too few individuals who said patient issue only and used the response of “shared issue” as patient shared appraisal. We used the same procedure for partners.
The means and standard deviations as well as the inter-correlation of patient shared appraisal with the collaborative, supportive, and unsupportive behaviors and health are shown in Table 2.
Table 2.
Means and Intercorrelations Among Patient Study Variables
| mean | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. patient shared appraisal | .24 | .43 | |||||||||||||
| 2. CIS behavior | 2.82 | 1.09 | .39*** | ||||||||||||
| 3. emotional support | 3.36 | .87 | .38*** | .63*** | |||||||||||
| 4. critical | 1.80 | .97 | .11 | .36*** | −.00 | ||||||||||
| 5. avoidance | 1.49 | .70 | .10 | .20** | .05 | .32*** | |||||||||
| 6. protective buffering | 2.45 | 1.11 | −.13+ | −.02 | −.20** | .33*** | .31*** | ||||||||
| 7. overprotective behavior | 2.22 | .89 | .29*** | .53*** | .29*** | .49*** | .28*** | .18* | |||||||
| 8. relationship quality | 65.74 | 14.27 | .25*** | .40*** | .59*** | −.18* | −.13+ | −.19** | .11 | ||||||
| 9. PCS | 48.92 | 9.37 | −.19** | −.05 | .07 | −.15* | −.16* | −.15* | −.22** | .15* | |||||
| 10. MCS | 48.71 | 9.12 | .11 | −.02 | .11 | −.21** | −.15* | −.22** | −.10 | .23** | −.01 | ||||
| 11. depressive symptoms | 9.85 | 8.33 | −.06 | −.07 | −.28*** | .23** | .32*** | .35*** | .14* | −.45*** | −.24** | −.64*** | |||
| 12. regimen distress | 2.15 | .98 | −.18* | .04 | −.08 | .32*** | .08 | .35*** | .03 | −.18* | −.04 | −.38*** | .38*** | ||
| 13. self-care | 3.67 | .56 | .11 | −.00 | .13+ | −.35*** | .08 | −.11 | −.07 | .12+ | .09 | .30*** | −.28*** | −.59*** | |
| 14. HbA1c | 7.57 | 1.06 | −.02 | .06 | −.00 | .29*** | .03 | .23** | .13+ | −.07 | −.15* | −.06 | .04 | .33*** | −.32*** |
Notes: CIS behavior = collaboration and instrumental support; PCS = physical component score; MCS = mental component score; n.s. = not significant;
p < .10;
p < .05;
p < .001
Links of Demographic and Disease Variables to Patient Illness Appraisals
In terms of demographic variables, patient shared appraisal was not related to patient gender, patient race or ethnicity, income, or couple marital status. However, patient shared appraisal was related to patient age, t(197) = −2.81, p < .01, and length of marriage, t(197) = −2.32, p < .05, and marginally related to patient education, t(197) = 1.82, p = .07. Moreover, the marginal effect of education disappeared when age was statistically controlled. Patients who had a shared appraisal were older (M = 51.67, SD = 15.74) than patients who had an individual appraisal (M = 45.28, SD = 13.02). Patients who had a shared appraisal had been in a relationship with their current partner for a longer period of time (M = 23.56 years, SD = 16.57) than those with an individual appraisal (M = 18.03 years, SD = 13.65). In terms of disease variables, patient appraisal was not related to insulin delivery method, use of continuous glucose monitoring, age of diagnosis, length of disease, or overall comorbidity.
Relations of Patient Appraisal to Collaborative, Supportive, and Unsupportive Behaviors
A one-way analysis of covariance (controlling for age and relationship length) comparing patient shared and individual appraisal groups on collaborative, supportive, and unsupportive behaviors revealed group differences on most of the outcomes. As shown in the first three columns of Table 3, patient shared illness appraisals were related to more CIS behaviors, more emotional support, less protective buffering, and more overprotective behavior. There were no group differences for avoidance or critical behavior.
Table 3.
Comparison of Patient Shared and Individual Appraisal Groups on Collaborative, Supportive, and Unsupportive Behaviors
| Patient Only n = 151 |
Patient Shared n = 48 |
p | Neither Shared n = 54 |
Partner only Shared n = 94 |
Both Shared n = 42 |
p | |
|---|---|---|---|---|---|---|---|
| CIS index | 2.58 | 3.57 | *** | 2.23a | 2.76b | 3.58c | *** |
| emotional support | 3.17 | 3.94 | *** | 3.02a | 3.26a | 4.00b | *** |
| Critical | 1.74 | 1.99 | n.s. | 1.71a | 1.75a | 1.96a | n.s. |
| avoidance | 1.45 | 1.61 | n.s. | 1.44a | 1.46a | 1.62a | n.s. |
| protective buffering | 2.53 | 2.19 | * | 2.42a | 2.60a | 2.28a | n.s. |
| overprotective behavior | 2.08 | 2.68 | *** | 1.94a | 2.17a | 2.63b | *** |
Notes: CIS index = collaboration and instrumental support; n.s. = not significant,
p < .05;
p < .001;
common subscripts in columns 4–6 indicate means do not significantly differ from one another
Patient and Partner Appraisal Consistency and Collaborative, Supportive and Unsupportive Behaviors
Because partners were much more likely to view the illness as shared than patients, we examined whether there were appraisal group differences in collaborative, supportive, and unsupportive behaviors by taking into consideration both patient and partner appraisal. We compared couples in which both patient and partner appraised the issue as the patient’s problem (n = 54) to couples in which the partner appraised the issue as shared but the patient appraised the issue as his or her own problem (n = 94) to couples in which both patient and partner viewed the illness as shared (n = 42). We did not examine a group in which only the patient appraised the illness as shared because there were too few couples in this group (n = 7). We used analyses of covariance to examine group differences, followed by Tukey’s post-hoc comparison test. As shown in the last four columns of Table 3, patients reported greater CIS behaviors in the consistent shared appraisal group than the partner only shared appraisal group, which was significantly more than the neither shared appraisal group. For emotional support, the consistent shared appraisal group reported significantly greater support than either of the other two groups. Similarly, there was greater overprotective behavior in the consistent shared appraisal group compared to the other two groups.
Relations of Patient Shared Appraisal to Health Outcomes
CIS behaviors as a moderator.
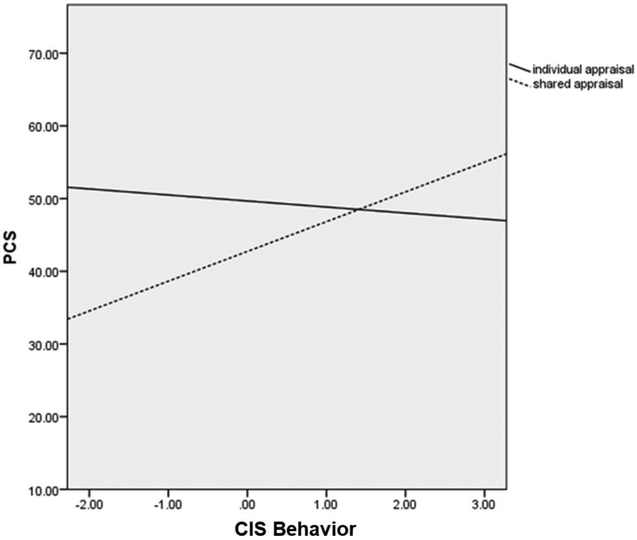
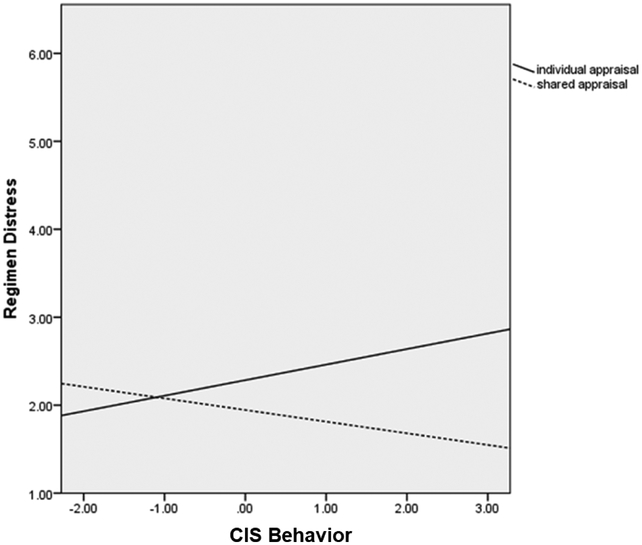
Regression results are shown in the top half of Table 4. CIS behaviors were related to higher relationship quality but did not interact with illness appraisal. There was a significant interaction of CIS behaviors with patient appraisal for physical functioning (PCS). As shown in Figure 1a, CIS behaviors were related to better physical functioning, but only among those who held a shared appraisal. There were no effects involving CIS behaviors for MCS or depressive symptoms. There was a significant CIS behaviors by illness appraisal interaction for regimen distress (see Figure 1b). CIS behaviors were related to greater regimen distress for patients with an individual appraisal but were related to less distress for those with a shared appraisal. There were no effects of illness appraisal or CIS behaviors on self-care behavior or HbA1c.
Table 4.
Multiple Regression Analyses to Predict Patient Outcomes
| Relationship Quality | PCS | MCS | CESD | Regimen Distress | Self-Care | HbA1c | |
| Age | −.30** | −.33** | −.09 | .03 | −.19 | −.06 | .13 |
| Marriage length | .20+ | .02 | .17 | −.06 | −.03 | .21+ | −.04 |
| Partner shared appraisal | .13+ | −.06 | .11 | −.11 | −.16* | .07 | −.02 |
| Patient shared appraisal | .10 | −.23** | .10 | −.01 | −.06 | .06 | −.08 |
| CIS index | .34*** | −.12 | −.08 | −.05 | .21* | −.03 | .11 |
| CIS index × patient appraisal | .30*** | −.20* | |||||
| Emotional Support | Relationship Quality | PCS | MCS | CESD | Regimen Distress | Self-Care | HbAlc |
| Age | −.21* | −.26* | −.08 | −.02 | −.23+ | .11 | .18 |
| Marriage length | .15 | −.03 | .17 | −.04 | −.02 | .18 | −.05 |
| Partner shared appraisal | .12* | −.10 | .09 | −.08 | −.12+ | .06 | −.00 |
| Patient shared appraisal | .02 | − 32*** | .05 | .09 | .01 | −.10 | .06 |
| Emotional support | .56*** | .01 | .08 | −.30*** | .03 | .07 | .11 |
| Emotional support × patient appraisal | .34*** | −.21* | .19* | −.23* |
Notes: CIS index = collaboration and instrumental support; PCS = physical component score; MCS = mental component score; patient and partner shared illness appraisal scored 1=shared, 0 = individual; n.s. = not significant;
p < .10;
p < .05;
p < .001
Figure 1a.
CIS behaviors are related to better physical functioning (PCS) for those with a shared appraisal but is unrelated to physical functioning for those with an individual appraisal.
Figure 1b.
CIS behaviors are related to more diabetes regimen distress for those with an individual appraisal but less regimen distress for those with a shared appraisal.
Emotional support as moderator.
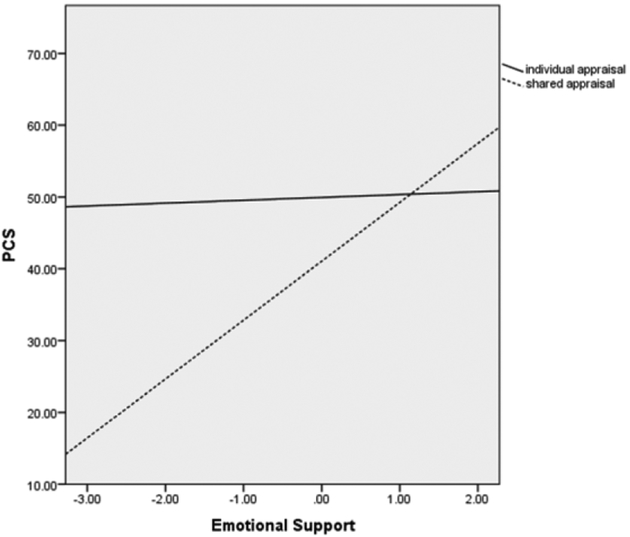
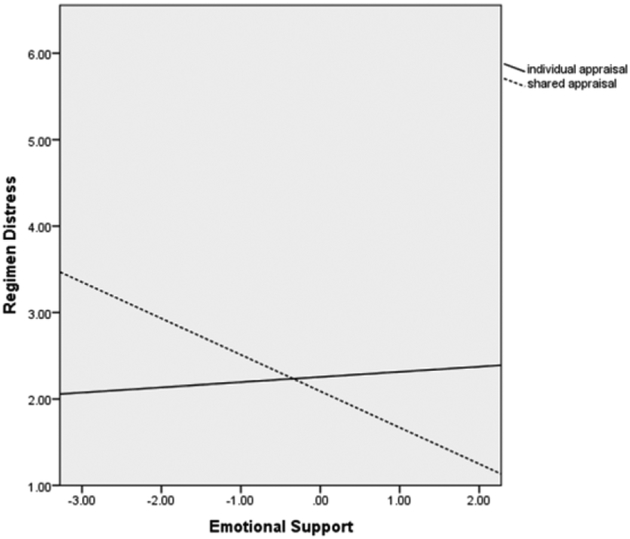
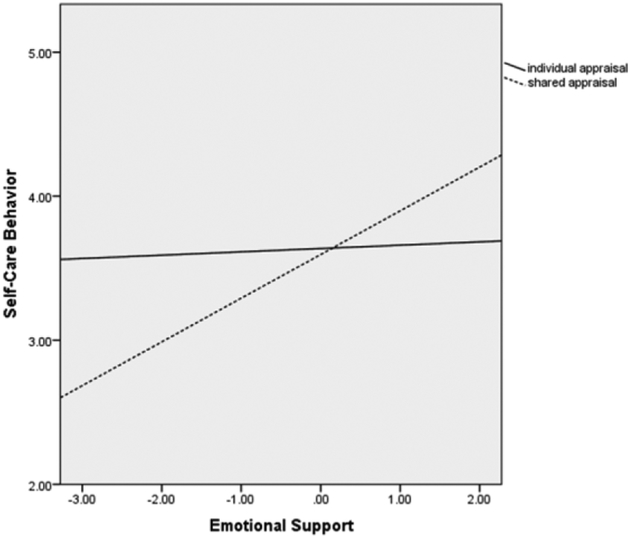
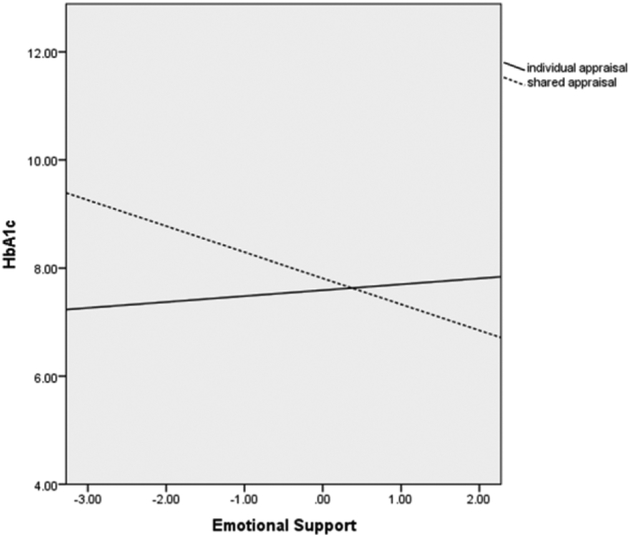
As shown in the bottom of Table 4, emotional support and partner shared appraisal were each linked to higher patient relationship quality, but there were no effects involving patient shared appraisal. For physical functioning, there was a main effect of patient shared appraisal that was qualified by an interaction with emotional support. As shown in Figure 2a, emotional support was related to better physical functioning for patients with a shared appraisal but not those with an individual appraisal. There were no effects of patient or partner appraisal for mental functioning or depressive symptoms, but emotional support was linked to fewer depressive symptoms. Emotional support interacted with shared illness appraisal to predict regimen distress (see Figure 2b). Emotional support was only related to less regimen distress when patients held shared illness appraisals. Patient appraisal interacted with emotional support to predict self-care behavior (see Figure 2c) and glycemic control (see Figure 2d). In both cases, emotional support was linked to better diabetes outcomes in the context of a shared but not an individual appraisal.
Figure 2a.
Emotional support is related to better physical functioning for those with a shared appraisal and is unrelated to physical functioning for those with an individual appraisal.
Figure 2b.
Emotional support is related to less diabetes regimen distress for those with a shared appraisal and is unrelated to regimen distress for those with an individual appraisal.
Figure 2c.
Emotional support is related to better self-care behavior for those with a shared appraisal and is unrelated to self-care behavior for those with an individual appraisal.
Figure 2d.
Emotional support is related to better glycemic control (i.e., lower HbA1c) for those with a shared appraisal and is unrelated to glycemic control for those with an individual appraisal.
Discussion
Patient and Partner Shared Illness Appraisals
Patients and partners differed in their illness appraisals, with partners viewing diabetes as more of a shared illness than patients. The majority of patients reported that diabetes was their own issue but affected the partner, whereas the majority of partners viewed the illness as shared. The greater shared illness appraisals among partners is consistent with research with couples with type 2 diabetes that assessed shared illness appraisals both explicitly as well as implicitly using “we-language” (Helgeson et al., 2016). It is not surprising that patients viewed the illness more individually than did partners, especially as the majority of patients had been diagnosed with diabetes for many years. In fact, the diagnosis preceded the initiation of the current relationship for most individuals.
Patient shared illness appraisals were associated with some demographic variables, specifically being older and being in the current relationship for a longer period of time. Greater shared illness appraisals among older adults in long-term relationships align with life-span theories regarding older adults’ optimizing existing social relationships (Carstensen, Isaacowitz, & Charles, 1999). Consistent with Helgeson et al. (2016) who found greater communal coping in couples with longer relationships, we found that patients reported more shared illness appraisals when they had been in longer relationships. With time, partners may become more involved in diabetes and patients may come to view the illness as a shared issue. Thus, intervention efforts that might aim to enhance a shared illness appraisal in patients and partners might find older couples and couples in longer relationships to be more amenable to such an intervention; however, because younger couples are likely to score lower on this dimension, they may have the most potential to benefit from such an intervention. In addition, shared illness appraisals were associated with greater marital satisfaction, consistent with a growing literature on links between positive dyadic coping and better relationship satisfaction (Falconier et al., 2015).
Shared Illness Appraisal and Collaborative and Supportive Behaviors
As predicted, shared illness appraisals were associated with greater reports of collaborative and supportive behaviors. Such a link is in line with models of dyadic (Bodenmann, 1997; Berg & Upchurch, 2007) and communal coping (Helgeson et al., in press; Lyons et al., 1998). Shared appraisals were also related to lower reports of protective buffering, a strategy of shielding one’s partner from distress that has been associated with poorer marital satisfaction among couples dealing with cancer (Hagedoorn et al., 2000). When individuals have shared illness appraisals, they may interpret their partner’s support attempts in the most positive light. In other words, shared illness appraisals may provide the lens through which patients come to view their partners’ behavior as more collaborative and supportive. In addition, engaging in collaboration and receiving support from one’s partner may lead one to develop a more shared illness appraisal. Future longitudinal research should disentangle the causal sequence between these two constructs.
Shared illness appraisals, however, were also associated with patient reports of overprotection (i.e., providing unnecessary assistance), a strategy that has been associated with poorer diabetes outcomes (Hagedoorn et al., 2006). It is important to note that overprotective behavior in this study was linked to both supportive and unsupportive behaviors, which likely reflects the idea that partner overinvolvement has both a positive and negative side to it. Consistent with this idea, a study of emerging adults with type 1 diabetes showed that partner overinvolvement revealed mixed relations to outcomes, whereas partner underinvolvement was uniformly negative (Helgeson, 2017). Thus, partners who are overprotective may collaborate and offer assistance but their assistance may cross the line and be perceived as critical and nagging. Thus, the link of partner overprotective behavior to patient and partner shared illness appraisals may reflect interdependence at a level that is excessive and could undermine patient self-efficacy.
The frequency of collaborative and supportive behaviors was highest when both patient and partner were consistent in their shared illness appraisals. Although models of communal coping and dyadic coping (Berg & Upchurch, 2007; Helgeson et al., 2018) have posited that collaborative and supportive strategies would be enhanced when couples are consistent in their illness appraisals, little research has examined whether consistency in shared illness appraisals relates to better outcomes. One study showed that inconsistency in pronoun use (e.g., more we-talk than I-talk by one person than the other person) was associated with the detrimental demand-withdraw pattern among couples dealing with health issues (Rentscher et al., 2013). It may be that when both members of the couple view diabetes as a shared illness, the daily tasks involved in diabetes management (e.g., food preparation, checking blood glucose) are performed jointly and viewed as supportive rather than controlling or critical. The finding that overprotection was reported as most frequent when both patient and partner viewed diabetes as a shared illness provides a cautionary note regarding shared illness appraisals in that they may come with assistance that is excessive at times. For couples with type 1 diabetes, enhancing collaboration and emotional support while minimizing overprotection is an important avenue for future intervention research.
It is important to note that in the present study, collaborative and instrumental supportive strategies loaded together rather than separately. The dyadic coping literature views collaboration and support as separate strategies (Berg & Upchurch, 2007; Bodenmann, 1997). It is possible that in the context of dealing with stressors surrounding type 1 diabetes that working collaboratively and receiving instrumental assistance from one’s partner are experienced similarly by those with type 1 diabetes. A contribution of the present study was in examining both instrumental and emotional support and revealed the important role that emotional support may play in understanding positive health outcomes. Frequently, the field of dyadic coping has not distinguished different forms of support (Berg & Upchurch, 2007; Bodenmann, 1997). Future work is needed to understand how persons with type 1 diabetes and their partners construe collaborative, supportive, and unsupportive behaviors.
Shared Illness Appraisals as a Moderator Variable
As predicted, supportive behaviors were most beneficial for physical health and distress outcomes when they occurred in the context of shared illness appraisals, a finding that replicates and expands on previous work (Berg et al., 2009; Stephens et al., 2013). That is, better physical health and lower regimen distress occurred when shared appraisals were matched with higher collaborative and supportive behaviors. In addition, when shared appraisals were matched with high emotional support, self-care was higher and glycemic control was better. Shared illness appraisals may be important in order for daily collaborative and supportive behaviors from one’s partner to be viewed favorably rather than as intrusive and controlling.
It is notable that neither collaborative and instrumental support nor emotional support had zero order correlations with adherence or HbA1c. Such results are in contrast to findings from a recent meta-analysis of social support that suggests support in general is beneficial for adherence but less so for those with type 1 than type 2 diabetes (Song et al., 2017). As noted in the meta-analysis, only three studies examined social support among adults with type 1 diabetes and used a range of social support measures, notably none specifically measuring support from one’s relationship partner. Clearly, further research is needed utilizing a broad array of social support measures.
The hypothesized interaction between shared appraisal and emotional support was more consistently associated with better outcomes than the hypothesized interaction between shared appraisal and collaborative and instrumental support, despite the fact that collaborative and instrumental support was highly related to emotional support (r = .63). The importance of the fit between shared appraisals and emotional support strategies may indicate that emotional support may be what is desired when patients view the illness as shared. As so much of the type 1 diabetes regimen requires actions that the individual with diabetes most likely performs independently (e.g., checking one’s blood glucose with a meter, injecting oneself with insulin), an important way in which partners may collaborate may be through the provision of emotional support. It also may be the case that the receipt of emotional support in the context of viewing the illness as an individual issue is a source of distress and a threat to self-efficacy, implying that the patient cannot handle the illness on his or her own and needs the understanding and availability of a partner.
The results should be interpreted in the context of some limitations. First, the sample was largely non-Hispanic white experiencing low levels of diabetes distress and relatively good A1c levels (though participants were above current ADA recommendations for adults to have a target HbA1c of < 7.0%; ADA, 2018). The results may not generalize to a more diverse group of couples. Some evidence suggests that social support may be more beneficial for ethnically and racially diverse individuals than for white individuals (Song et al., 2017). Second, the illness appraisal measures were based on single items, which may raise concerns about validity and reliability. Although single-item measures typically have reduced reliability compared to multiple-item measures, single-item measure have been shown to be useful under some conditions—specifically when construct measured is concrete, unambiguous, and face valid (Diamantopoulod, Sarstedt, Fuchs, Wilczynski, & Kaiser, 2012). Other research has linked this single item to other measures of shared illness appraisal (Zajdel, et al., 2016). Future research may benefit from employing multiple items and examining their stability over time. Third, with the exception of glycemic control, the variables examined in this paper were measured via self-report. Future research should consider obtaining more behavioral indicators of illness appraisal as well as self-care.
Finally, the cross-sectional nature of the study prevents strong conclusions as to whether shared illness appraisals together with receipt of partner support leads one to have better outcomes or whether better outcomes create the alignment of appraisals and support. When diabetes management outcomes are poor (e.g., low adherence, high HbA1c) partners may provide more support to get management back on track, irrespective of how patients appraise the illness. There are also potential third variables that could confound/explain these relations. Two likely candidates are length of relationship and relationship quality, as people with longer and more satisfying relationships may be more likely to appraise a stressor as shared. We statistically controlled for relationship length in all analyses. When we repeated the analyses on health outcomes with controls for relationship quality, the interactions of appraisal with emotional support and with collaboration and instrumental support remained. Future longitudinal research is needed to ascertain the causal directions of effects.
Although more work is needed in this area to establish causal links from shared appraisal to health outcomes, these results could have clinical implications. Couple-based interventions have been effective for enhancing relationship quality and regimen adherence among those facing a number of chronic illness conditions (Martire, Schulz, Helgeson, Small, & Saghafi, 2010). Such couples-based interventions frequently focus on communication (Kayser et al., 2007), support, and positive dyadic coping strategies (Bodenmann & Randall, 2012). The present results suggest that such interventions may be enhanced if there was a fit between partner illness involvement and shared illness appraisal. The benefits of pre-intervention “we-talk” in couples undergoing interventions involving smoking cessation (Rohrbaugh et al., 2012) and alcohol treatment (Rentscher et al., 2017) is evidence of this proposition. Because illnesses such as type 1 diabetes are ones that couples share throughout their life-course, there may be value in patients and partners coming to view the illness as shared and collaborating on behaviors that facilitate adherence—both of which can reduce life-long complications of the illness.
Acknowledgments
Funding: The study was funded by the National Institutes of Health DP3 DK103999.
Footnote
We repeated these analyses and controlled for relationship quality. The interactions presented in the results section remained significant.
Conflict of Interest: The authors declare that they have no conflict of interest.
Author Notes: Portions of these data were presented at the 2018 Meeting of the Society of Behavioral Medicine.
Ethical approval: “All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.”
References
- Afifi TD, Hutchinson S, & Krouse S (2006). Toward a theoretical model of communal coping in postdivorce families and other naturally occurring groups. Communication Theory, 16(3), 378–409. [Google Scholar]
- Association AD (2017). 6. Glycemic targets: Standards of medical care in diabetes 2018. Diabetes Care, 41(Supplement 1), S55–S64. [DOI] [PubMed] [Google Scholar]
- Berg CA, Butner JE, Butler JM, King PS, Hughes AE, & Wiebe DJ (2013). Parental persuasive strategies in the face of daily problems in adolescent type 1 diabetes management. Health Psychology, 32(7), 719–728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berg CA, Schindler I, & Maharajh S (2008). Adolescents’ and mothers’ perceptions of the cognitive and relational functions of collaboration and adjustment in dealing with type 1 diabetes. Journal of Family Psychology, 22(6), 865–874. [DOI] [PubMed] [Google Scholar]
- Berg CA, Schindler I, Smith TW, Skinner M, & Beveridge RM (2011). Perceptions of the cognitive compensation and interpersonal enjoyment functions of collaboration among middle-aged and older married couples. Psychology and Aging, 26(1), 167–173. [DOI] [PubMed] [Google Scholar]
- Berg CA, Skinner M, Ko K, Butler JM, Palmer DL, Butner J, & Wiebe DJ (2009). The fit between stress appraisal and dyadic coping in understanding perceived coping effectiveness for adolescents with type 1 diabetes. Journal of Family Psychology, 23(4), 521–530. [DOI] [PubMed] [Google Scholar]
- Berg CA, & Upchurch R (2007). A developmental-contextual model of couples coping with chronic illness across the adult life span. Psychological Bulletin, 133(6), 920954. [DOI] [PubMed] [Google Scholar]
- Berg CA, Wiebe DJ, Butner J, Bloor L, Bradstreet C, Upchurch R, … Patton G (2008). Collaborative coping and daily mood in couples dealing with prostate cancer. Psychology and Aging, 23(3), 505–516. [DOI] [PubMed] [Google Scholar]
- Bodenmann G (1997). Dyadic coping: A systematic-transactional view of stress and coping among couples: Theory and empirical findings. European Review of Applied Psychology, 47, 137–140. [Google Scholar]
- Bodenmann G, & Randall AK (2012). Common factors in the enhancement of dyadic coping. Behavior Therapy, 43(1), 88–98. [DOI] [PubMed] [Google Scholar]
- Bolger N, & Amarel D (2007). Effects of social support visibility on adjustment to stress: Experimental evidence. Journal of Personality and Social Psychology, 92(3), 458–475. [DOI] [PubMed] [Google Scholar]
- Carstensen LL, Isaacowitz DM, & Charles ST (1999). Taking time seriously: A theory of socioemotional selectivity. American Psychologist, 54(3), 165–181. [DOI] [PubMed] [Google Scholar]
- Diamantopoulos A, Sarstedt M, Fuchs C, Wilczynski P, & Kaiser S (2012). Guidelines for choosing between multi-item and single-item scales for construct measurement: A predictive validity perspective. Journal of the Academy of Marketing Science, 40, 434–449. [Google Scholar]
- Falconier MK, Jackson JB, Hilpert P, & Bodenmann G (2015). Dyadic coping and relationship satisfaction: A meta-analysis. Clinical Psychology Review, 42, 28–46. [DOI] [PubMed] [Google Scholar]
- Funk JL, & Rogge RD (2007). Testing the ruler with item response theory: Increasing precision of measurement for relationship satisfaction with the Couples Satisfaction Index. Journal of Family Psychology, 21(4), 572–583. [DOI] [PubMed] [Google Scholar]
- Hagedoorn M, Keers JC, Links TP, Bouma J, Ter Maaten JC, & Sanderman R (2006). Improving self-management in insulin-treated adults participating in diabetes education. The role of the overprotection by the partner. Diabetic Medicine, 23(3), 271–277. [DOI] [PubMed] [Google Scholar]
- Hagedoorn M, Kuijer RG, Buunk BP, DeJong GM, Wobbes T, & Sanderman R (2000). Marital satisfaction in patients with cancer: Does support from intimate partners benefit those who need it the most? Health Psychology, 19, 274–282. [PubMed] [Google Scholar]
- Helgeson VS, Jakubiak B, Seltman H, Hausmann LRM, & Korytkowski MT (2016). Implicit and explicit communal coping in couples with recently diagnosed type 2 diabetes. Journal of Social and Personal Relationships, 34, 1099–1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helgeson VS, Jakubiak B, Van Vleet M, & Zajdel M (2018). Communal coping and adjustment to chronic illness: Theory update and evidence. Personality and Social Psychology Review, 22, 170–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helgeson VS, Novak SA, Lepore SJ, & Eton DT (2004). Spouse social control efforts: Relations to health behavior and well-being among men with prostate cancer. Journal of Social and Personal Relationships, 21, 53–68. [Google Scholar]
- Johnson MD, Anderson JR, Walker A, Wilcox A, Lewis VL, & Robbins DC (2013). Common dyadic coping is indirectly related to dietary and exercise adherence via patient and partner diabetes efficacy. Journal of Family Psychology, 27(5), 722–730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kayser K, Watson LE, & Andrade JT (2007). Cancer as a “we-disease”: Examining the process of coping from a relational perspective. Families, Systems, & Health, 25(4), 404–418. [Google Scholar]
- Lee E, & Roberts LJ (2018). Between individual and family coping: A decade of theory and research on couples coping with health-related stress. Journal of Family Theory & Review, 10, 141–164. [Google Scholar]
- Lewin AB, LaGreca AM, Geffken GR, Williams LB, Duke DC, Storch EA, & Silverstein JH (2009). Validity and reliability of an adolescent and parent rating scale of type 1 diabetes adherence behaviors: The Self-Care Inventory (SCI). Journal of Pediatric Psychology, 34(9), 999–1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis MA, & Rook KS (1999). Social control in personal relationships: Impact on health behaviors and psychological distress. Health Psychology, 18, 63–71. [DOI] [PubMed] [Google Scholar]
- Lyons RF, Mickelson KD, Sullivan MJL, & Coyne JC (1998). Coping as a communal process. Journal of Social and Personal Relationships, 15, 579–605. [Google Scholar]
- Martire LM, Schulz R, Helgeson VS, Small BJ, & Saghafi EM (2010). Review and meta-analysis of couple-oriented interventions for chronic illness. Annals of Behavioral Medicine, 40, 325–342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClure MJ, Xu JH, Craw JP, Lane SP, Bolger N, & Shrout PE (2014). Understanding the costs of support transactions in daily life. Journal of Personality, 82(6), 563–574. [DOI] [PubMed] [Google Scholar]
- Polonsky WH, Fisher L, Earles J, Dudl RJ, Lees J, Mullan J, & Jackson RA (2005). Assessing psychosocial distress in diabetes: Development of the diabetes distress scale. Diabetes Care, 28(3), 626–631. [DOI] [PubMed] [Google Scholar]
- Radloff LS (1977). The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1, 385–401. [Google Scholar]
- Rafaeli E, & Gleason MEJ (2009). Skilled support within intimate relationships. Journal of Family Theory & Review, 1, 20–37. [Google Scholar]
- Rentscher KE, Rohrbaugh MJ, Shoham V, & Mehl MR (2013). Asymmetric partner pronoun use and demand-withdraw interaction in couples coping with health problems. Journal of Family Psychology, 27(5), 691–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rentscher KE, Soriano EC, Rohrbaugh MJ, Shoham V, & Mehl MR (2017). Partner pronoun use, communal coping, and abstinence during couple-focused intervention for problematic alcohol use. Family Process, 56(2), 348–363. [DOI] [PubMed] [Google Scholar]
- Revenson TA (1994). Social support and marital coping with chronic illness. Annals of Behavioral Medicine, 16, 122–130. [Google Scholar]
- Rohrbaugh MJ, Shoham V, Skoyen JA, Jensen M, & Mehl MR (2012). We-talk, communal coping, and cessation success in a couple-focused intervention for healthcompromised smokers. Family Process, 51(1), 107–121. [DOI] [PubMed] [Google Scholar]
- Rottman N, Hansen DG, Larsen PV, Nicolaisen A, Flyger H, Johansen C, & Hagedoorn M (2015). Dyadic coping within couples dealing with breast cancer: A longitudinal, population-based study. Health Psychology, 34(5), 486–495. [DOI] [PubMed] [Google Scholar]
- Song Y, Nam S, Park S, Shin I. s., & Ku BJ (2017). The impact of social support on selfcare of patients with diabetes: What is the effect of diabetes type? Systematic review and meta-analysis. The Diabetes Educator, 43(4), 396–412. [DOI] [PubMed] [Google Scholar]
- Stephens MAP, Franks MM, Rook KS, Iida M, Hemphill RC, & Salem JK (2013). Spouses’ attempts to regulate day-to-day dietary adherence among patients with type 2 diabetes. Health Psychology, 32(10), 1029–1037. [DOI] [PubMed] [Google Scholar]
- Thoits PA (2011). Mechanisms linking social ties and support to physical and mental health. Journal of Health and Social Behavior, 52(2), 145–161. [DOI] [PubMed] [Google Scholar]
- Uchino BN (2009). Understanding the links between social support and physical health. Perspectives on Psychological Science, 4, 236–255. [DOI] [PubMed] [Google Scholar]
- Vangelisti AL (2009). Challenges in conceptualizing social support. Journal of Social and Personal Relationships, 26(1), 39–51. [Google Scholar]
- Ware J, Kosinski M, & Keller S (1996). A 12-item short-form health survey: Construction of scales and preliminary tests of reliability and validity. Medical Care, 34(3), 220233. [DOI] [PubMed] [Google Scholar]
- Ware JE, Snow KK, Kosinski M, & Gandek B (1993). SF-36 Health Survey: Manual and interpretation guide. Boston: Nimrod. [Google Scholar]
- Zajdel M, Helgeson VS, Seltman HJ, Korytkowski MT, & Hausmann LRM (2016) Measuring communal coping in type 2 diabetes using a multi-method approach. Poster presented at the 36th Annual Meeting of the Society of Behavioral Medicine, Washington, D.C. [Google Scholar]