Abstract
Background
Results of limb lengthening in patients with achondroplasia were previously reported in many studies. However, the reports of comparison among the three long bones (femur, tibia, and humerus) are rare, especially for the results of crossed lengthening (lengthening of one femur and contralateral tibia followed by that of the opposite side) for the lower limbs. The purpose of this study was to report the surgical results of a series of limb lengthening in achondroplastic or hypochondroplasia patients at our institution.
Methods
Fifteen patients (14 with achondroplasia and 1 with hypochondroplasia) underwent lower limb lengthening of the femur (n = 32) and tibia (n = 28), and 12 of them underwent crossed lengthening. Humeral lengthening was performed in 14 patients (n = 28). The mean age at the first operation was 11.7 years, and the mean follow-up duration was 66.7 months. The healing index, consolidation period index (duration of consolidation period/gained length), and other radiographic indices were analyzed. Limb length discrepancy and hip-knee-ankle alignment in lower limbs, and the occurrence of difficulties were assessed.
Results
The average gain in length for the femur, tibia, and humerus was 8.3 cm, 8.5 cm, and 7.4 cm, respectively. The mean healing index was 29.6 days/cm for the femur, 29.0 days/cm for the tibia, and 27.2 days/cm for the humerus. The mean consolidation period index was 14.7 days/cm for the humerus, which was significantly lower than that in the lower limb (17.3 days/cm for the femur and 17.8 days/cm for the tibia). Of the 12 who underwent crossed lengthening, five showed limb length discrepancy ≥ 1.0 cm. Among their 24 lower limbs, three showed valgus alignment ≥ 5° and one showed varus alignment ≥ 5°. Thirty-two pin site infections and three fractures were conservatively managed. Three femoral fractures, eight equinus deformities, and four cases with premature consolidation of the fibula were surgically treated. Obstacle and true complication related to humeral lengthening were not observed.
Conclusions
Humeral lengthening was relatively effective and safe. Careful attention will be needed to avoid the occurrence of limb length discrepancy or malalignment in crossed lengthening.
Keywords: Achondroplasia, Distraction osteogenesis
Limb lengthening is one of the methods for improving the quality of life in achondroplastic patients.1,2) They undergo greater amount of limb lengthening, heal faster, and show fewer complications than patients with other diagnoses.3)
At our institution, achondroplatic patients undergo lower limb lengthening followed by humeral lengthening after in-depth consultation and agreement. Regarding the lower limb lengthening, we believe that patients suffer most severely from bilateral femoral lengthening due to the large volume of the thigh and external fixator in both sides. Therefore, crossed lengthening, which refers to simultaneous lengthening of one femur and contralateral tibia, has been predominantly performed at our institution. We believe that the narrower width of the lower limbs after crossed lengthening, compared to “transverse lengthening” involving bilateral femoral lengthening followed by bilateral tibial lengthening, can facilitate more comfortable care of surgical wounds and perineal area, weight bearing and other physical activities. However, owing to the asymmetry of lengthened bones in the crossed manner procedure, the occurrence of limb length discrepancy (LLD) or malalignment is concerned. To date, surgical results of crossed lengthening were very rarely reported4) compared to those of bilateral tibial lengthening followed by bilateral femoral lengthening.2,5,6) Moreover, frequencies and degrees of LLD and malalignment were reported very rarely and restrictively.4,5)
With this background, we conducted a study to report the outcomes of a series of limb lengthening in achondroplastic and hypochondroplasia patients at our institution. The aims of this study were to compare the results according to the three lengthening sites (femur, tibia, and humerus) and to describe the final length discrepancy and alignment of lower limbs after crossed lengthening.
METHODS
Selection of the Study Subjects
The protocol of this study was reviewed and approved by the Institutional Review Board of the Samsung Medical Center (IRB No. 2018-07-123). The informed consent was waived. From 2003 to 2017, 14 achondroplastic and one hypochondroplasia patients (nine males and six females) underwent limb lengthening. The mean age at the first operation was 11.7 ± 2.3 years (range, 6.8 to 15.4 years), and the mean follow-up duration was 66.7 ± 40.9 months (range, 42.0 to 209.0 months). The initial height, body weight, and body mass index were assessed according to the admission date for the first operation, which were 119.3 ± 11.6 cm (range, 90.0 to 137.0 cm), 35.9 ± 8.4 kg (range, 17 to 47 kg), and 24.9 ± 3.8 kg/m2 (range, 20.3 to 32.3 kg/m2), respectively.
Surgical Techniques
All surgical procedures were performed by the senior author (JSS). Regarding the lower limb lengthening, crossed lengthening was performed in 12 patients. The second surgery was performed on the opposite side 322.0 ± 54.8 days (range, 254 to 434 days) after the first surgery. Among the 12 patients, one patient underwent the lower limb lengthening twice for each side (i.e., four operations in total). Of the remaining three patients, one patient underwent bilateral tibial lengthening followed by bilateral femoral lengthening (308 days later) based on patient's choice; two patients visited our center after bilateral tibial lengthening at other center, so only bilateral femoral lengthening was performed at our institution.
Regarding the humeral lengthening, it was performed in 14 patients; one patient has been followed up in the out-patient clinic after the lower limb lengthening performed at our institution. Among the 14 patients, four underwent simultaneous bilateral humeral lengthening, and 10 underwent staged operation with an interval of 258.1 ± 92.7 days (range, 173 to 420 days). As a result, we operated 32 femoral, 28 tibial, and 28 humeral segments.
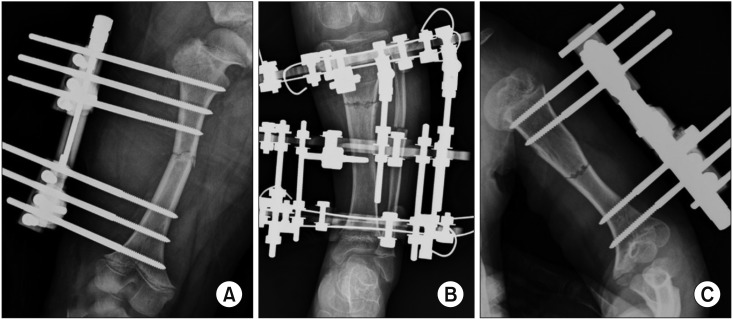
The osteotomy was outlined with a series of drill holes, and it was gently completed using an osteotome. A single diaphyseal osteotomy was performed for the femur. In 20 femoral segments, an acute correction was additionally performed to correct varus deformity of the femur. Except for two segments using an Ilizarov ring fixator, all the femoral lengthening procedures were performed using a monolateral external fixator (Fig. 1). For the tibia, a single proximal level osteotomy was performed, and an Ilizarov ring fixator was used. A fibular osteotomy was also performed (Fig. 1). In 15 tibial segments, a gradual correction to correct varus deformity of the tibia as well as lengthening was performed. A single diaphyseal osteotomy was performed, and a monolateral external fixator was used for the humerus (Fig. 1). In 11 humeral segments, an acute correction was performed to correct limited extension of the elbow joint or cubitus valgus.
Fig. 1. Simple radiographs taken after external fixator application and osteotomy in the femur (A), tibia (B), and humerus (C).
Postoperative Protocol
Distraction began approximately 7 days after the surgery at a rate of 0.25 mm every 6 hours. The rate was modified later, based on the radiographic and clinical features. Lengthening was continued considering the desired length and combined difficulties. The external fixators were removed when radiographic evidence of at least three cortices was shown. The mean duration of external fixator application was 236.9 ± 40.1 days (range, 166 to 343 days) for the femur, 242.9 ± 37.9 days (range, 196 to 343 days) for the tibia, and 194.3 ± 33.4 days (range, 152 to 278 days) for the humerus.
Radiographic Measurement
All indicators were measured using the picture archiving and communication system (PACS) system (GE Healthcare, London, UK). The gained length (cm) was defined as a difference in the length of the long bone measured at two time points, immediately before and after lengthening. The lengths of femur and tibia were measured parallel to the long axis on the anteroposterior view. The length of femur was measured from the most proximal part of the femoral head to the most distal part of the femoral condyle. The length of tibia was measured from the most proximal part of the tibial eminence to the midpoint of the tibial plafond.7) The length of humerus was measured parallel to its long axis from the most proximal part of the humeral head to the most distal part of the trochlea on the lateral view.8) Lengthening percentage (LP) was calculated by dividing the gained length by the initial length.9)
The healing index (HI) was calculated by dividing the entire duration of external fixator application by the gained length.6) The consolidation period index was calculated by dividing the duration of consolidation period (from the time of lengthening cessation to the time of external fixator removal) by the gained length. The callus shape was classified into five types: fusiform, cylindrical, concave, lateral, and central.9,10) The occurrence of subluxation or dislocation of adjacent joints was also assessed.
LLD and hip-knee-ankle (HKA) alignment in lower limbs at the last follow-up were measured using a long bone radiograph obtained in standing position. LLD was defined as difference between the vertical heights of the two lower limbs. HKA alignment was defined as alignment between the mechanical axis of the femur and that of the tibia. All indicators were measured twice (at an interval of minimum 2 weeks) by two observers, and the mean values were used for analysis. Intraclass correlation coefficients were calculated to evaluate reliabilities and all were > 0.8.
Clinical Outcomes
Limitation of range of motion (ROM) of adjacent joints was assessed. In addition, the patients were asked to rate their overall satisfaction with results as very satisfied, satisfied, fair, or dissatisfied.
Complication
Difficulties that occurred during the follow-up period were subclassified into problems, obstacles, and true complications based on a classification described by Paley.11)
Statistical Analysis
ANOVA with LSD post-hoc test and Fisher's exact test were used to compare the surgical results according the lengthening sites. Paired t-tests were performed for comparison between preoperative and postoperative values. Mann-Whitney U-tests and Fisher's exact tests were used in subgroup analysis. IBM SPSS ver. 23.0 (IBM Corp., Armonk, NY, USA) was used, and the significance level was set at p < 0.05.
RESULTS
Radiographic Measurements
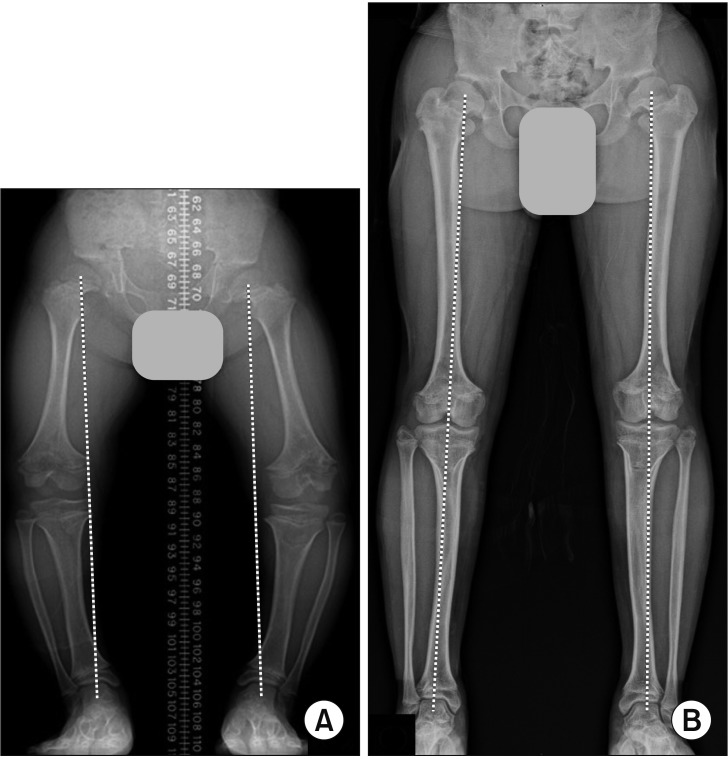
The mean gained length for the femur, tibia, and humerus was 8.3 ± 1.9 cm (32.1% ± 10.8%), 8.5 ± 1.5 cm (42.0% ± 10.3%), and 7.4 ± 1.6 cm (40.4% ± 10.4%), respectively. The LPs of tibial and humeral lengthening were greater than that of femoral lengthening (p = 0.001 and p = 0.003, respectively). The consolidation period index of humeral lengthening was lower than those of femoral and tibial lengthening (p = 0.043 and p = 0.023, respectively). Other comparisons showed no significance. Subluxation or dislocation of adjacent joints was not observed. Detailed results of radiographic indicators are shown in Table 1. The mean HKA alignment of 30 lower limbs in 15 patients was 9.7° ± 9.4° before surgery, and it significantly improved to −0.5° ± 4.9° at the last follow-up (p < 0.001). Of the 12 patients who underwent crossed lengthening, five patients showed LLD ≥ 1.0 cm. Among their 24 lower limbs, three showed valgus alignment ≥ 5° and one showed varus alignment ≥ 5°. Detailed alignment and length discrepancy of 24 lower limbs are presented in Table 2. Using the criteria of 5° and 1 cm, six showed satisfactory results in both alignment and length discrepancy at the last follow-up (Fig. 2).
Table 1. Results of Analysis of Radiographic Indicators.
| Variable | Femur (n = 32) | Tibia (n = 28) | Humerus (n = 28) |
|---|---|---|---|
| Gained length (cm) | 8.3 ± 1.9 | 8.5 ± 1.5 | 7.4 ± 1.6 |
| Lengthening (%) | 32.1 ± 10.8 | 42.0 ± 10.3* | 40.4 ± 10.4* |
| Healing index (days/cm) | 29.6 ± 6.7 | 29.0 ± 5.4 | 27.2 ± 6.3 |
| Consolidation period index (days/cm) | 17.3 ± 5.4 | 17.8 ± 4.6 | 14.7 ± 4.9* |
| Shape of the callus | |||
| Cylindrical | 23 (71.9) | 18 (64.3) | 24 (85.7) |
| Concave | 9 (28.1) | 10 (35.7) | 4 (14.3) |
Values are presented as mean ± standard deviation or number (%).
*Values with statistical significance.
Table 2. Final Alignment and Length Discrepancy of Lower Limbs in Patients Who Underwent Crossed Lengthening.
| Patient no. | Sex | Age at the first surgery (yr) | Age at the last follow-up (yr) | HKA alignment (°)* | HKA alignment (°)† | LLD (cm) |
|---|---|---|---|---|---|---|
| 1 | Male | 11.4 | 17.8 | 4.9 | −1.4 | 1.5II |
| 2 | Male | 10.3 | 14.3 | 0.2 | 1.4 | 0.4 |
| 3 | Male | 12.2 | 18.7 | 4.9 | −1.9 | 0 |
| 4 | Female | 6.8 | 20.7 | 0.3 | −2.8 | 0.2 |
| 5 | Male | 11.8 | 17.5 | −2.7 | −0.5 | 0.6 |
| 6 | Female | 10.6 | 15.3 | −3.2 | −1.9 | 1.3II |
| 7 | Female | 15.2 | 19.4 | −1.9 | −8.9II | 1.4II |
| 8 | Male | 15.3 | 19.4 | 0.2 | −1.5 | 0 |
| 9 | Male | 15.4 | 19.5 | −9.1II | −0.5 | 0.8 |
| 10 | Male | 11.5 | 15 | 7.2II | 3 | 1.3 |
| 11 | Male | 11.8 | 16.2 | 0.1 | −3 | 0.1 |
| 12 | Female | 13.3 | 16.7 | −4.5 | −6.4II | 1.0II |
HKA: hip knee ankle, LLD: limb length discrepancy.
*Side of femoral lengthening at the first surgery. †Side of tibial lengthening at the first surgery. *,†Varus alignment is presented as a positive value.
∥Alignment ≥ 5° and difference ≥ 1.0 cm.
Fig. 2. Long bone radiographs taken before the lower limb lengthening (A) and at the last follow-up (B). During the 4 years and 8 months of follow-up, the male patient (#2 in Table 2) gained 28 cm of height including physiological growth after the crossed lower limb lengthening. At the last follow-up, both alignments and length discrepancy of lower limbs were satisfactory. Dotted lines that connect the centers of the hip and ankle in each lower limb pass near the center of the knee at the last follow-up.
Clinical Outcomes
Limitation of the ROM or instability of the adjacent joints was not observed. All patients were satisfied with their surgical results: very satisfied, eight; satisfied, seven. In particular, 14 patients who underwent humeral lengthening were able to reach the perineal area and perform perineal hygiene independently.
Complications
The most common problem was the pin site infection. Three fractures after removal of the external fixators occurred but united following immobilization. Three femoral fractures, eight equinus deformities, and four cases with premature consolidation of the fibula were surgically treated. Obstacles related to humeral lengthening were not observed: the frequency (0%) was significantly lower than that for tibial lengthening (42.9%, p < 0.001). The frequency of total difficulties in humeral lengthening (42.9%) was significantly lower than that in femoral lengthening (68.8%, p = 0.039). We did not experience intraoperative injuries associated with late sequelae. Details are described in Table 3.
Table 3. Difficulties That Occurred during Limb Lengthening and Follow-up.
| Variable | Femur (n = 32) | Tibia (n = 28) | Humerus (n = 28) |
|---|---|---|---|
| Problem* | |||
| Pin site infection | 18 | 3 | 11 |
| Fracture | 1 | 1 | 1 |
| Total | 19 (59.4) | 4 (14.3) | 12 (42.9) |
| Obstacle† | |||
| Fracture | 3 | 0 | 0 |
| Premature consolidation | 0 | 4‡ | 0 |
| Equinus deformity of foot§ | NA | 8 | NA |
| Total | 3 (9.4) | 12 (42.9) | 0 |
| Total | 22 (68.8) | 16 (57.1) | 12 (42.9) |
Values are presented as number or number (%).
NA: not applicable.
*Conservatively treated. †Surgically treated. ‡Premature consolidation of fibula. §Underwent Achilles tendon lengthening.
Subgroup Analysis
To analyze the significant factors associated with complications, subgroup analyses were performed: the group with fractures after external fixator removal (n = 6) vs. the group without (n = 82); premature consolidation group (n = 4) vs. remaining tibial segments (n = 24); and equinus deformity group (n = 8) vs. remaining tibial segments (n = 20). Among the various comparisons, eight tibial segments with equinus deformity showed significantly lower LP than the other 20 tibial segments (35.2% vs. 44.7%, p = 0.043). No other comparisons showed significance.
DISCUSSION
The first main finding of the present study was that humeral lengthening was relatively effective and safe. All the humeral lengthening satisfied the patients and allowed independent perineal hygiene. Surgical results of limb lengthening in achondroplastic patients were previously reported in many studies;3) however, the studies that compared the surgical results among the three long bones were rare.12) Certainly, the relatively small number of subjects was a limitation of our study. Nevertheless, comparison of the surgical results according to the three lengthening sites based on statistical analyses was the main strength of our study.
The second main finding of the present study was the somewhat frequent occurrence of LLD (41.7%) and malalignment (16.7%) after crossed lengthening of lower limbs. Surgical results of crossed lengthening4) were very rarely reported than those of transverse lengthening.2,5,6) Different from the previous study, we tried to describe the exact frequencies and degrees of LLD and malalignment. In general, patients with LLD < 2 cm are less likely to need intervention.13,14) However, stricter criteria should be established considering the disproportionately short stature in patients with achondroplasia. In fact, one patient with LLD of 1.3 cm (#10 in Table 2) and another with LLD of 0.8 cm (#9 in Table 2) complained of subjective discomfort caused by LLD. Regarding the results of three patients who underwent transverse lengthening in our study, all showed LLD ≤ 0.5 cm.
Previous studies on limb lengthening in achondroplastic patients used mechanical axis deviation (MAD) to describe the alignment of the lower limbs in coronal plane.15) Considering the short stature and individual difference in height, we used the indicator of alignment (HKA alignment) instead of the distance indicator (MAD). As a result, four (16.7%) showed malalignment ≥ 5°. In a study by Park et al.,5) transverse lengthening on 56 lower limbs of 28 achondroplastic patients resulted in two genu valgum and three varus deformity of the femur (8.9%). Crossed lengthening has been predominantly performed at our institution because we believe that narrower width of the lower limbs can facilitate more comfortable patient self-care and activity. Despite these advantages, we recommend surgeons pay special attention to avoid the occurrence of LLD or malalignment when using the crossed manner considering the relatively high frequencies in our study.
The LP of tibial lengthening was greater than that of femoral lengthening (Table 1). This finding is consistent with results of a previous study.5) In the study, radiographic indices were more effective in tibial lengthening than in femoral lengthening.5) By contrast, the HI and consolidation period index were comparable for both procedures in our study; simultaneous removal of external fixators at the tibia and femur after crossed lengthening could have adversely affected the indices for tibial lengthening compared to the transverse manner lengthening.
Tibial segments with equinus deformity showed lower LP. It seemed that the desired length could not be achieved owing to the occurrence of equinus deformity rather than that low LP was the risk factor for equinus deformity. Lower HI, latency period less than 5 days, and shape of the callus were associated with the occurrence of postoperative fracture in humeral lengthening for achondroplasia in a previous study.16) In our study, we could not identify the significance associated with fractures. It might be due to the small number of study subjects.
There were several other limitations. First, the criteria of LLD (1 cm) and malalignment (5°) used in our study have not been validated in achondroplastic patients. Although four patients (#1, 6, 7, and 12 in Table 2) with LLD or malalignment based on the criteria did not complain of any symptom, this should be verified in future studies. Second, the heterogeneity of the cohort was one of the limitations of our study. Of the 14 patients who underwent humeral lengthening, four underwent simultaneous and 10 underwent staged lengthening based on the preferences of patients and their parents. However, this heterogeneity would not affect the main findings of our study because the difference was not found between the subgroups (simultaneous vs. staged) in additional analyses. Third, the lack of patient-reported outcome measures was also a limitation; instead, the patients were asked to rate their overall satisfaction.
Our study provides valuable data, which will be useful for consultation with achondroplastic patients. In our experience, humeral lengthening in achondroplastic patients was a relatively effective and safe method. When performing the crossed lengthening procedure, careful attention will be needed to avoid the occurrence of LLD or malalignment.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Balci HI, Kocaoglu M, Sen C, Eralp L, Batibay SG, Bilsel K. Bilateral humeral lengthening in achondroplasia with unilateral external fixators: is it safe and does it improve daily life? Bone Joint J. 2015;97(11):1577–1581. doi: 10.1302/0301-620X.97B11.36037. [DOI] [PubMed] [Google Scholar]
- 2.Kim SJ, Balce GC, Agashe MV, Song SH, Song HR. Is bilateral lower limb lengthening appropriate for achondroplasia? Midterm analysis of the complications and quality of life. Clin Orthop Relat Res. 2012;470(2):616–621. doi: 10.1007/s11999-011-1983-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim SJ, Pierce W, Sabharwal S. The etiology of short stature affects the clinical outcome of lower limb lengthening using external fixation: a systematic review of 18 trials involving 547 patients. Acta Orthop. 2014;85(2):181–186. doi: 10.3109/17453674.2014.899856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Donaldson J, Aftab S, Bradish C. Achondroplasia and limb lengthening: results in a UK cohort and review of the literature. J Orthop. 2015;12(1):31–34. doi: 10.1016/j.jor.2015.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Park KW, Garcia RA, Rejuso CA, Choi JW, Song HR. Limb lengthening in patients with achondroplasia. Yonsei Med J. 2015;56(6):1656–1662. doi: 10.3349/ymj.2015.56.6.1656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kitoh H, Mishima K, Matsushita M, Nishida Y, Ishiguro N. Early and late fracture following extensive limb lengthening in patients with achondroplasia and hypochondroplasia. Bone Joint J. 2014;96(9):1269–1273. doi: 10.1302/0301-620X.96B9.33840. [DOI] [PubMed] [Google Scholar]
- 7.Song SH, Agashe MV, Huh YJ, Hwang SY, Song HR. Physeal growth arrest after tibial lengthening in achondroplasia: 23 children followed to skeletal maturity. Acta Orthop. 2012;83(3):282–287. doi: 10.3109/17453674.2012.678802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Akman SD, Karakas P, Bozkir MG. The morphometric measurements of humerus segments. Turk J Med Sci. 2006;36(2):81–85. [Google Scholar]
- 9.Venkatesh KP, Modi HN, Devmurari K, Yoon JY, Anupama BR, Song HR. Femoral lengthening in achondroplasia: magnitude of lengthening in relation to patterns of callus, stiffness of adjacent joints and fracture. J Bone Joint Surg Br. 2009;91(12):1612–1617. doi: 10.1302/0301-620X.91B12.22418. [DOI] [PubMed] [Google Scholar]
- 10.Li R, Saleh M, Yang L, Coulton L. Radiographic classification of osteogenesis during bone distraction. J Orthop Res. 2006;24(3):339–347. doi: 10.1002/jor.20026. [DOI] [PubMed] [Google Scholar]
- 11.Paley D. Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop Relat Res. 1990;(250):81–104. [PubMed] [Google Scholar]
- 12.Chilbule SK, Dutt V, Madhuri V. Limb lengthening in achondroplasia. Indian J Orthop. 2016;50(4):397–405. doi: 10.4103/0019-5413.185604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gross RH. Leg length discrepancy: how much is too much? Orthopedics. 1978;1(4):307–310. doi: 10.3928/0147-7447-19780701-08. [DOI] [PubMed] [Google Scholar]
- 14.McCarthy JJ, MacEwen GD. Management of leg length inequality. J South Orthop Assoc. 2001;10(2):73–85. [PubMed] [Google Scholar]
- 15.Vaidya SV, Song HR, Lee SH, Suh SW, Keny SM, Telang SS. Bifocal tibial corrective osteotomy with lengthening in achondroplasia: an analysis of results and complications. J Pediatr Orthop. 2006;26(6):788–793. doi: 10.1097/01.bpo.0000242429.83866.97. [DOI] [PubMed] [Google Scholar]
- 16.Nakano-Matsuoka N, Fukiage K, Harada Y, Kashiwagi N, Futami T. The prevalence of the complications and their associated factors in humeral lengthening for achondroplasia: retrospective study of 54 cases. J Pediatr Orthop B. 2017;26(6):519–525. doi: 10.1097/BPB.0000000000000428. [DOI] [PubMed] [Google Scholar]