Abstract
Purpose: The prognostic role of programmed death-ligand 1 (PD-L1) in colorectal cancer remains unclear. We employed a meta-analysis to explore the prognostic value of PD-L1 and to ascertain the relationship between PD-L1 expression and clinicopathological characteristics in CRC patients.
Methods: We systematically searched PubMed, Embase and the Cochrane Library until October 2018. Eligible studies about colorectal cancer that pay attention to PD-L1 expression and studies reporting survival information were included. In order to evaluate the prognostic role of PD-L1 for overall survival (OS) and recurrence-free survival (RFS)/disease-free survival (DFS), Hazard ratio (HR) with 95% confidence interval (CI) was used. Odds ratio (OR) with 95% CI was selected to appraise the correlation between PD-L1 with clinicopathological characteristics of colorectal cancer patients. Begg’s funnel plot was used to assess publication bias.
Results: Twelve studies involving 4344 patients published from 2013 to 2018 were included in this meta-analysis. Pooled results revealed that PD-L1 overexpression was relevant to shorter OS (HR 1.47, 95% CI =1.01–2.15, p=0.04) and shorter RFS/DFS (HR 1.47, 95% CI =1.01–2.15, p=0.04). Moreover, Patients with high expression of PD-L1 associated with inferior tumor stage (OR=0.57, 95% CI: 0.45, 0.74, p<0.0001) and Vascular invasion-negativity (OR=0.75, 95% CI: 0.6, 0.94, p=0.01). But the expression of PD-L1 is not related to age, sex, tumor location, tumor differentiation, pT stage, pN stage, MSI/MMR status.
Conclusion: This meta-analysis revealed that PD-L1 can serve as a significant biomarker for negative prognosis and the adverse clinicopathological features of colorectal cancer and could facilitate the better management of individual patients.
Keywords: PD-L1, colorectal cancer, prognosis, meta-analysis
Introduction
Colorectal cancer (CRC) is the most commonly diagnosed cancer worldwide at present, being the third and fifth leading cause of cancer death in the United States and China, respectively.1,2 About 39% of patients were diagnosed with localized stage CRC, for which the 5-year survival rates is 90%. However, the patients diagnosed with the regional and distant-stage disease and the survival rate descend on 71% and 14%.3 New treatments for primary, regional and metastatic CRC have been developed, including laparoscopic surgery for primary; resection of the liver and lungs metastatic disease; radiotherapy for rectal cancer and some forms of metastatic disease; neoadjuvant and palliative chemotherapy; targeted therapy, immunotherapy, and vaccines.4,5 Therefore, it is critical to early detection, the effectiveness of prevention, and management to improving treatment strategies and patient outcomes.
However, some locally advanced and distant metastatic CRC patients lost the chance of surgery, so chemotherapy is basically the only option for advanced and metastatic patients; but these have only modest efficacy and are ineffective against distant metastases.6,7 Moreover, these treatments generate side effects that can limit their use. In recent years, more attention has been placed on developing immunotherapies, specially programmed death 1 (PD-1) and programmed death ligand-1 (PD-L1).PD-1/PD-L1 is one of the most important co-stimulatory signals; its-mediated immunosuppression is an important part of the dynamic balance of the immune system because it limits the immune response and prevents autoimmune diseases. The present study found that CD274 (PD-L1, B7-H1) was first cloned in 1999.8 The expression profiles of CD274 (PD-L1) in human tumors have been revealed.9,10 Hunmantumor-associated APCs include tumor microenvironment dendritic cells (DCs), tumor-draining lymph nodes DCs,11,12 macrophages,13,14 fibroblasts,15 and T cells16 were observed a high level of CD274 (PD-L1) protein expression, except tumor cell. Many studies have found that engagement of PD-L1 with its receptor PD-1 on T cells delivers a signal that inhibits T cell proliferation, resulting in tumor immune evasion.17 PD-1/PD-L1 immune checkpoint inhibitors have been used to treat melanoma, non-small cell lung cancer, renal cell carcinoma, lymphoma, and bladder cancer.18 However, the efficacy of immune checkpoint inhibitors for the treatment of CRC is limited. Different research has studied the PD-L1 expression of the prognosis role of CRC; nevertheless, the results were not consistent. Some investigations showed that overexpression of PD-L1 forecasted poor survival in CRC,19–24 but other investigations presented negative results.25,26
To tackle this problem, we employed meta-analysis to synthetic estimate the value of PD-L1 as a prognostic biomarker, and to clarify the relationship between PD-L1 expression and clinicopathological characteristic in CRC patients.
Materials and methods
This meta-analysis is based on the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) guidelines.30 Our research was based on data from previously published studies; thus ethical ratify was unnecessary.
Search strategy
The Cochrane Library, Embase and PubMed were systematically searched. The strategy used was to search for the following words in relevant literature: (“Colorectal Neoplasms” OR “Neoplasms, Colorectal” OR “Colorectal Neoplasm” OR “Neoplasm, Colorectal” OR “Colorectal Tumors” OR “Colorectal Tumor” OR “Tumor, Colorectal” OR “Tumors, Colorectal” OR“Colorectal Carcinoma” OR “Carcinoma, Colorectal” OR “Carcinomas, Colorectal” OR “Colorectal Carcinomas” OR “Colorectal Cancer” OR “Cancer, Colorectal” OR “Cancers, Colorectal” OR “Colorectal Cancers”) AND (“CD274” OR “B7-H1” OR “PD-L1” OR “PD-L1” OR “CD274 Antigens” OR “B7-H1 Immune Costimulatory Protein” OR “B7 H1 Immune Costimulatory Protein” OR “B7-H1 Antigen” OR “Antigen, B7-H1” OR “B7 H1 Antigen” OR “PD-L1 Costimulatory Protein” OR “Costimulatory Protein, PD-L1” OR “PD L1 Costimulatory Protein” OR “Programmed Cell Death 1 Ligand 1 Protein” OR “CD274 Antigen” OR “Antigen, CD274” OR “Programmed Cell Death 1 Ligand 1” OR “B7H1 Immune Costimulatory Protein”). To recognize more research, we also retrospect the reference lists of relevant articles.
Selection criteria
The eligible researches were contained in this meta-analysis based on the following criteria: (1) Patients with colorectal cancer confirmed by pathology. (2) Immunohistochemistry (IHC) was used to detect the expression of PD-L1 in colorectal cancer tissue. (3) Studies reported 5-year OS, HR with 95% confidence interval (95% CIs), or reported original survival curves. (4) Their full texts were available. This analysis exclude articles based on the following standards: (1) non-English; (2) animal experiments; (3) comment, letters, review or case reports; (4) deficiency data to report the risk ratios (RR) and 95% confidence interval (95% CI), or the Kaplan-Meier curve could not be extracted. When duplicate publications were identified, only the most complete or most recent article was included.
Data extraction
All relevant articles data were extracted by two independent reviewers (Lianzhou Yang, Rujun Xue). The information was extracted from each study included: first author, country, date of publication, number of patients, duration of follow up, age, histological type of tumor, tumor site, grade at diagnosis, number of patients with PD-L1 positive, cut-off value, antibody, survival data, Kaplan-Meier curves. ALL divergences were settled by discussion and the achievement of consensus.
Quality assessment
According to the Newcastle-Ottawa Scale (NOS), two researchers independently assessed each study for quality.(Lianzhou Yang, Rujun Xue). The NOS maximum possible score is 9 points. Each study included was judged on three perspectives: (I) the selection (representativeness, selection of the non-exposed, ascertainment of exposure and outcome of interest); (II) the comparability; and (III) the ascertainment of either the exposure or outcome of interest (assessment and follow-up). A study that received a score of 6 or higher was considered the high-quality study.
Statistical analysis
The software used in this work was Review Manager Software, Version 5.3 and Stata version12.0. The hazard ratio (HR) with 95% CI was utilized to assess the relationship between the expression of PD-L1 and OS, DFS, and RFS. The merged ORs and the 95% CIs were utilized to quantitatively determine the relationship between PD-L1 and clinicopathological feature of the patient. The heterogeneity between included studies was examined using I2 and Q text. If p<0.1 or I2>50%, which demonstrated significant heterogeneity, the fixed effect model was used for meta-analysis. If there was significant heterogeneity, the random model was used. In this analysis, p-values <0.05 were considered statistically significant.
Results
Search results
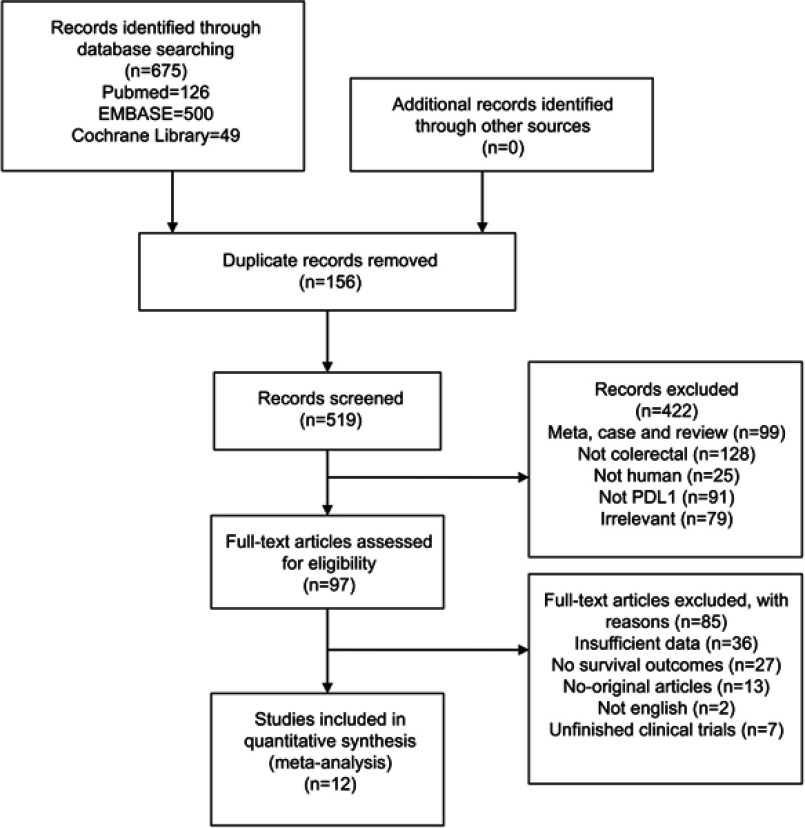
After the primary retrieval, 675 potentially relevant articles were initially identified with three databases searched. After removing 156 duplicates, still 519 studies were identified for the title/abstract; however, 422 manuscripts were excluded for the following reasons: not original papers (eg, case report, review, and meta-analysis), animal studies, not colorectal cancer-related studies, not PD-L1-related studies, irrelevant, or were not published in English. Subsequently, 95 articles remained for further full-text assessment. Thereafter, 36 articles were excluded due to insufficient data, 2 articles lack of survival outcomes, 13 were no-original articles and 7 were unfinished clinical trials. Ultimately, twelve studies19–26,31–34 published from 2013 to 2018 were included in this meta-analysis (Figure 1).
Figure 1.
Flow chart of the literature search and study selection protocols.
Characteristics of included studies
Twelve studies involving 4344 patients published from 2013 to 2018 were included in this meta-analysis. The number of patients in each study arranged from 90 to 1420. The immunochemical staining (IHC) was used to confirm PD-L1 expression oftumor tissues in all studies. Three pieces of research were performed in Western countries and nine kinds of research were implemented in Asian countries. The quality of the selected researches wasassessed by using the Newcastle-Ottawa Scale and found to range from 6 to 8, indicating that the studies were of high quality. Table 1 describes the detailed characteristics of the twelve studies.
Table 1.
Characteristics of the studies included in the meta-analysis
| Study | Year | Country | Number of patients | Age | Study period | Follow up Median(M) | Detection method | Cut-off | Antibody | PD-L1 positive/negative | Quality assessment |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Droeser et al25 | 2013 | Switzerland | 1420 | 69.9 (30–96) | 1987–1996 | - | IHC | Percentages of PD-L1 staining intensity | Clone 27A2, ab82059 | 495/913 | 8 |
| Hamada et al19 | 2017 | USA | 617 | 68.6±8.8 | 1976–2012 | Patients were observed until death or January 1, 2012 | IHC | Score32 | Anti-CD274 antibody, eBioscience | 384/233 | 8 |
| Koganemaru et al31 | 2017 | Japan | 235 | 63 (32–84) | 2009–2012 | 52.9 (4.6–78.8) | IHC | >5% | SP142 | 19/216 | 6 |
| Lee et al33 | 2016 | USA | 395 | 55±15 (18–90) | - | 55±40 (0.4–393) | IHC | >1% | Clone E1L3N | 19/375 | 6 |
| Li et al26 | 2016 | China | 276 | 57 (27–85) | 2007–2009 | 61 | IHC | Score34 | ab174838 | 138/138 | 7 |
| Liang et al20 | 2014 | China | 185 | 52 (29–72) | - | 60 | IHC | Score34 | Polyclonal antibodies, Santa Cruz Biotechnology | 102/83 | 6 |
| Saigusa et al21 | 2016 | Japan | 90 | 64 (33–80) | 2003–2014 | 46 (2–139) | IHC | Score32 | Clone 27A2 | 36 | 6 |
| Shi et al22 | 2013 | China | 143 | 59.8±12.5 | 2006–2007 | 43 (1–56) | IHC | Presence of PD-L1 staining | Abcam, ab58810 | 64 | 6 |
| Song et al23 | 2013 | China | 347 | 65 | 2000–2006 | (1–122) | IHC | Score31.49, ranged from 0 to 15.9 (median: 2.33) | Abcam | - | 8 |
| Wang et al32 | 2017 | China | 254 | 56 (28–75) | 2007–2009 | 42 (21–68) | IHC | Percentages of PD-L1 staining intensity | sp142 | 46/208 | 7 |
| Wang et al34 | 2016 | China | 262 | 56.5 (28–75) | 2007–2009 | 43.5 (21–68) | IHC | >5% | SP142 | 54/208 | 8 |
| Zhu et al24 | 2015 | China | 120 | 67 (54–80) | 2008–2013 | 39 | IHC | Score34 | Abcam | 28 | 7 |
Correlation between PD-L1 expression and survival
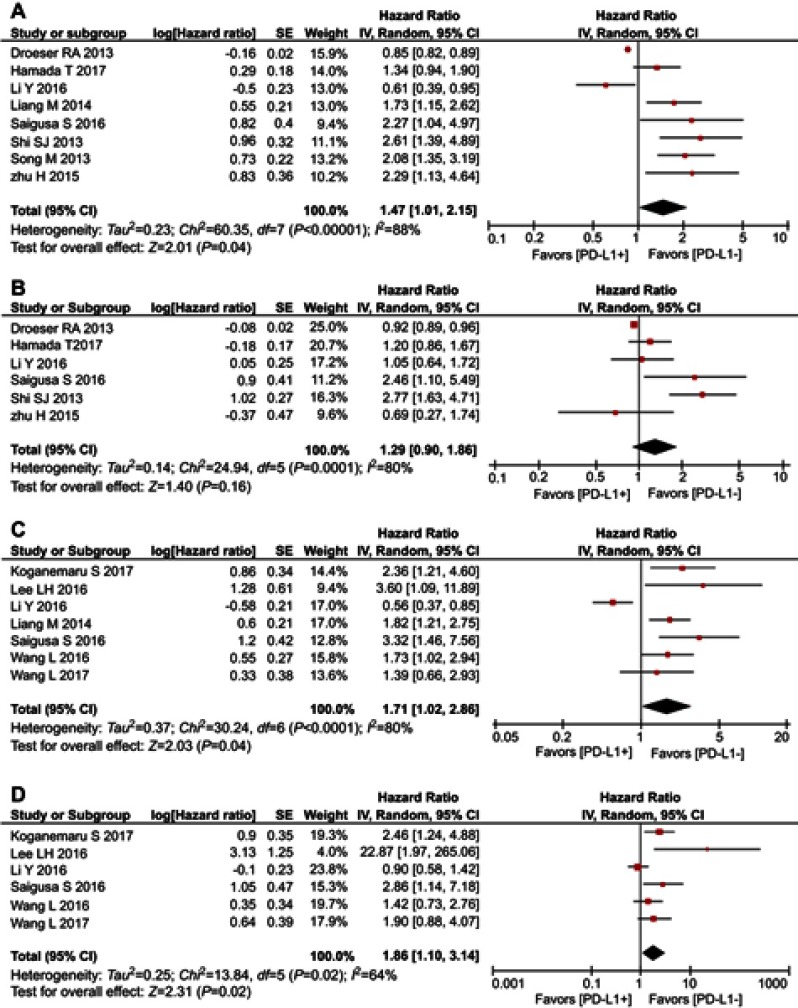
We evaluated the prognostic role of PD-L1 expression of OS, RFS, and DFS. Eight researches (n=3198) reported OS, as significant heterogeneity existed (Cochran’s Q, p<0.00001, I2=88%).Pooled result by random model revealed high expression of PD-L1 was correlated with poor OS than the absence of PD-L1 expression (HR 1.47, 95% CI =1.01–2.15, p=0.04) (Figure 2A). Because heterogeneity existed, subgroup analysis was performed. Subgroup analysis based on different analytical methods, integrated HR for OS was 1.29 (95% CI: 0.90–1.86, p=0.16) (Figure 2B). Elucidating the effect of different cut-off of PD-L1 expression of the results, we performed subgroup analysis stratified by cut-off. When score<4 or cut-off ≤5% the heterogeneity was negligible, but there was no statistical significance in all subgroup between PD-L1 expression and overall survival (Figure 3A).
Figure 2.
Forest plot describing the association between PD-L1 expression and prognosis of patients with CRC patient. (A) OS; (B) OS by multivariate analysis; (C) RFS/DFS; (D) RFS/DFS by multivariate analysis.
Figure 3.
(A) Subgroup analysis based on a different cut-off of association between PD-L1 expression and OS. (B) Subgroup analysis based on a different cut-off of association between PD-L1 expression and RFS/DFS.
Seven (n=1697) reported RFS/DFS. As significant heterogeneity existed (Cochran’s Q, p<0.0001, I2=80%).Pooled result by random model revealed PD-L1 overexpression was associated with shorter RFS/DFS than the absence of PD-L1 expression (HR 1.47, 95% CI =1.01–2.15, p=0.04) (Figure 2C). Because heterogeneity existed, subgroup analysis was performed. Subgroup analysis based on different analytical methods, integrated HR for RFS/DFS was 1.86 (95% CI: 1.10–3.14, p=0.02) (Figure 2D). Elucidating the effect of different cut-off of PD-L1 expression of the results, we performed subgroup analysis stratified by cut-off. When cut-off score <4 or ≤5% the heterogeneity was negligible. There was no statistical significance in cut-off >5% or score >4 subgroups between PD-L1 expression and RFS/DFS (Figure 3B).
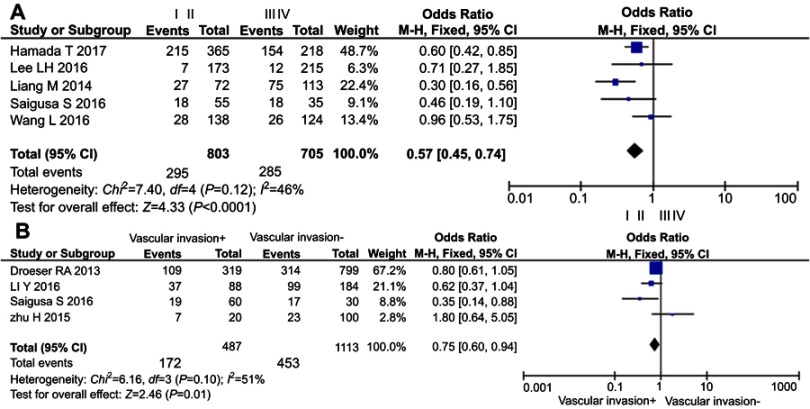
Correlation between PD-L1 expression and tumor clinicopathlogical parameters
Moreover, we investigated the relationship between PD-L1 expression and clinicopathological parameters, including sex, age, tumor location, tumor differentiation, tumor stage, pT stage, pN stage, vascular invasion, MSI/MMR status. The analysis of each parameter includes at least three studies. The merged results demonstrated that PD-L1 expression suggests in patients with poorer tumor stage (OR =0.57, 95%CI: 0.45, 0.74, p<0.0001) and Vascular invasion-negativity (OR =0.75, 95%CI: 0.6, 0.94, p=0.01) (Figure 4). However, there was no association between PD-L1 expression and age (OR =0.95, 95%CI: 0.73, 1.22, p=0.67), sex (OR =0.97, 95%CI: 0.84, 1.13, p=0.72), tumor location (OR =1.12, 95%CI: 0.87, 1.45, p=0.37), tumor differentiation (OR =1.18, 95%CI: 0.94,1.48, p=0.15), pT stage (OR =0.81, 95%CI: 0.44, 1.48, p=0.49), pN stage (OR =0.72, 95%CI: 0.44, 1.17, p=0.18), MSI/MMR status (OR =0.54, 95%CI: 0.16, 1.90, p=0.34) (Figure S1).
Figure 4.
Forest plots for the association between PD-L1 expression and clinicopathological parameters. (A) Tumor stage; (B) vascular invasion-negativity.
Sensitivity analyses
We delete any single study at a time individually, which to assess the stability of the results. The results show that there is no separate study significantly affected the total HRs, this meta-analysis of the results are credible.
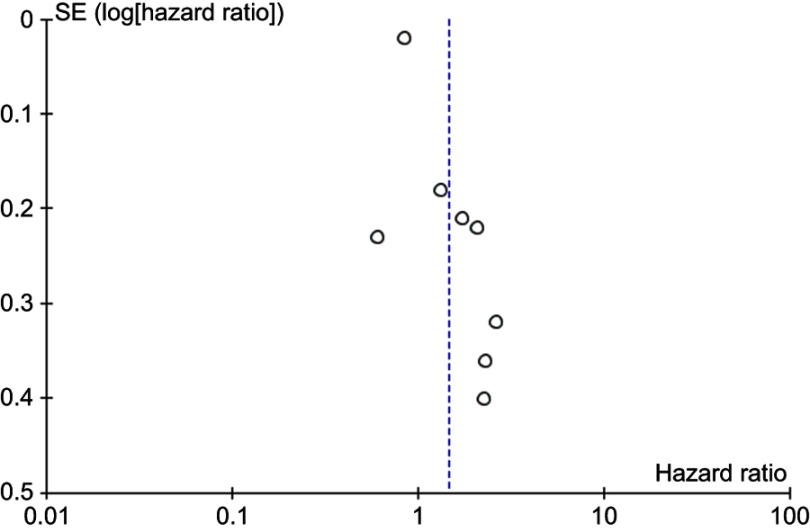
Publication bias
The funnel plot did not indicate any evidence of publication bias (Figure 5).
Figure 5.
Funnel plot of publication bias for overall survival.
Discussion
The PD-1/PD-L1 pathway has become a promising therapeutic target for various human malignancies, including melanoma, non-small-cell lung cancer, head and neck cancer, Hodgkin’s lymphoma, gastric cancer, and urothelial cancer. Some clinical trials have shown that PD-1/PD-L1 blockage could benefit prognosis.35–39 Nonetheless, there are no consistent results for the prognostic value of PD-L1 in colorectal cancer patients. Lots researches have indicated that the expression of PD-L1 is correlated with an obviously poor survival,19,10–24 while some study accounted the opposite effect.25,26 Several studies have revealed the relationship between PD-L1 and Solid Tumors.27–29 However, those studies differs from our in that their subjects include all solid tumors in which the number of colorectal cancers included too few, and our study provides an in-depth analysis between PD-L1 expression and tumor stage, vascular invasion, MSI/MMR mutation, etc. In our meta-analysis, we concentrate on the clinicopathological characteristics of patients with colorectal cancer and the prognostic validity of PD-L1 in colorectal cancer.
The interaction between PD-L1 and PD-1 can lead to exhausted phenotype and dysfunction of T-cells which protected tumor cells escape from the host immune surveillance.40 Immune-checkpoint blockades become a new way in immunotherapy for cancer and it gradually changes the standard treatment of advanced-stage cancers. According to reports, overexpression of PD-1 and PD-L1 on tumor-infiltrating lymphocytes (TIL) and tumor cells (TC) correlates with poor prognosis in several cancers.41 Such as breast cancer,42 renal cell cancer,43 lung cancer,44 glioma.45 In colorectal cancer, this is in agreement with the study by Hamada et al,19 which indicated the association of PD-L1 overexpression and poor OS in CRCs (HR 1.33, 95% CI 0.94–1.89). Additionally, Song et al,23 using tissue microarray immunohistochemistry to detect 404 CRC patient samples, univariate analysis disclosed that patients overexpression of PD-L1 had poorer overall survival (p<0.001; HR =2.07 (1.342–3.193). But, multivariate analysis did not support PD-L1 as an independent prognostic factor (p=0.548). Otherwise, some similar studies have revealed similar results. In contrast, a study of Droeser et al,25 which involved 1420 CRCs patients, found the patients with MMR-proficient with PD-L1 overexpression correlated with better OS (p=0.003; HR =0.84 (0.79–0.88); In univariate analysis, PD-L1 overexpression in MMR-proficient CRC was significantly correlated with early T stage, absence of lymph node metastases, lower tumor grade, absence of vascular invasion. Moreover, in the study by Li et al,26 this involved two cohorts; In the TCGA cohort, higher PD-L1 expressions indicated a better OS (p=0.002). In FUSCC cohort, expressions of PD-L1 on tumor cells were associated with better OS (p=0.002) and DFS (p=0.004) of CRC patients. Therefore, a meta-analysis of available data on the prognostic significance of PD-L1 will be useful and imperatively needed.
In this meta-analysis, we synthesized twelve pieces of research relevant to prognosis and clinicopathological of PD-L1 expression in colorectal cancer. As we know, this is the first meta-analysis focus on the prognosis and clinicopathological characteristics of patients with colorectal cancer. Our data indicated that PD-L1 overexpression was associated with shorter OS (HR 1.47, 95% CI =1.01–2.15, p=0.04) and shorter RFS/DFS (HR 1.47, 95% CI =1.01–2.15, p=0.04), suggesting that PD-L1 expression could serve as an important prognostic factor for colorectal cancer. Related research shows that immune evasion caused by PD-1/PD-L1 pathway may be related to poor infiltration of T cells into tumors and lack activation of cancer-specific T cells in the tumor microenvironment.46 Moreover, PD-L1 overexpression was increased in patients with inferior tumor stage (OR=0.57, 95%CI: 0.45, 0.74, p<0.0001) and Vascular invasion-negativity (OR=0.75, 95%CI: 0.6, 0.94, p=0.01). For the present study, we didn’t find relationship between PD-L1 expression and age, gender, tumor location, tumor differentiation, pT stage, pN stage, MSI/MMR status.
There were several limitations to our study. Some significant heterogeneity can be observed in our study. These heterogeneities may have different sources. Firstly, only articles published in English were included in this meta-analysis. Secondly, the sample sizes of the studies enrolled in our analysis were comparatively small. Third, PD-L1 positivity was evaluated by using different antibody and dilution which affect the sensitivity of IHC. Fourth, the cut-off value where PD-L1 expressed was varied among the studies. So, future researches should make efforts in the standardization of PDL1 expression detection. Additionally, because not all study hasa distinction about MSI/MMR status and not provide sufficient information which may bring heterogeneity to the meta-analysis. Based on our observations, we believe that the results of our meta-analysis should be noticed and should be validated by additional studies with appropriate multivariate analyses.
Our investigation exhibited that the overexpression of PD-L1 indicates a poor prognosis and clinicopathological features and that treatment with anti-PD-L1 antibodies should be attempted in patients with CRCs patient in the future.
Disclosure
The authors report no conflicts of interest in this work.
Supplementary material

References
- 1.Chen W, Zheng R, Baade PD, et al. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66(2):115–132. doi: 10.3322/caac.21338 [DOI] [PubMed] [Google Scholar]
- 2.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2017. CA Cancer J Clin. 2017;67(1):7–30. doi: 10.3322/caac.21387 [DOI] [PubMed] [Google Scholar]
- 3.Siegel RL, Miller KD, Fedewa SA, et al. Colorectal cancer statistics, 2017. CA Cancer J Clin. 2017;67(3):177–193. doi: 10.3322/caac.21395 [DOI] [PubMed] [Google Scholar]
- 4.Kuipers EJ, Grady WM, Lieberman D, et al. Colorectal cancer. Nat Rev Dis Primers. 2015;1:15065. doi: 10.1038/nrdp.2015.65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xiang B, Snook AE, Magee MS, Waldman SA. Colorectal cancer immunotherapy. Discov Med. 2013;15(84):301–308. [PMC free article] [PubMed] [Google Scholar]
- 6.Hubbard JM, Grothey A. Colorectal cancer in 2014: progress in defining first-line and maintenance therapies. Nat Rev Clin Oncol. 2015;12(2):73–74. doi: 10.1038/nrclinonc.2014.233 [DOI] [PubMed] [Google Scholar]
- 7.Fakih MG. Metastatic colorectal cancer: current state and future directions. J Clin oncol. 2015;33(16):1809–1824. doi: 10.1200/JCO.2014.59.7633 [DOI] [PubMed] [Google Scholar]
- 8.Dong H, Zhu G, Tamada K, Chen L. B7-H1, a third member of the B7 family, co-stimulates T-cell proliferation and interleukin-10 secretion. Nat Med. 1999;5(12):1365–1369. doi: 10.1038/70932 [DOI] [PubMed] [Google Scholar]
- 9.Freeman GJ, Long AJ, Iwai Y, et al. Engagement of the PD-1 immunoinhibitory receptor by a novel B7 family member leads to negative regulation of lymphocyte activation. J Exp Med. 2000;192(7):1027–1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Topalian SL, Sznol M, McDermott DF, et al. Survival, durable tumor remission, and long-term safety in patients with advanced melanoma receiving nivolumab. J Clin oncol. 2014;32(10):1020–1030. doi: 10.1200/JCO.2013.53.0105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Curiel TJ, Wei S, Dong H, et al. Blockade of B7-H1 improves myeloid dendritic cell-mediated antitumor immunity. Nat Med. 2003;9(5):562–567. doi: 10.1038/nm863 [DOI] [PubMed] [Google Scholar]
- 12.Perrot I, Blanchard D, Freymond N, et al. Dendritic cells infiltrating human non-small cell lung cancer are blocked at immature stage. J Immunol. 2007;178(5):2763–2769. [DOI] [PubMed] [Google Scholar]
- 13.Wu K, Kryczek I, Chen L, Zou W, Welling TH. Kupffer cell suppression of CD8+ T cells in human hepatocellular carcinoma is mediated by B7-H1/programmed death-1 interactions. Cancer Res. 2009;69(20):8067–8075. doi: 10.1158/0008-5472.CAN-09-0901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kuang DM, Zhao Q, Peng C, et al. Activated monocytes in peritumoral stroma of hepatocellular carcinoma foster immune privilege and disease progression through PD-L1. J Exp Med. 2009;206(6):1327–1337. doi: 10.1084/jem.20082173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nazareth MR, Broderick L, Simpson-Abelson MR, Kelleher RJ Jr., Yokota SJ, Bankert RB. Characterization of human lung tumor-associated fibroblasts and their ability to modulate the activation of tumor-associated T cells. J Immunol. 2007;178(9):5552–5562. [DOI] [PubMed] [Google Scholar]
- 16.Ghebeh H, Mohammed S, Al-Omair A, et al. The B7-H1 (PD-L1) T lymphocyte-inhibitory molecule is expressed in breast cancer patients with infiltrating ductal carcinoma: correlation with important high-risk prognostic factors. Neoplasia (New York, NY). 2006;8(3):190–198. doi: 10.1593/neo.05733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Denkert C, von Minckwitz G, Brase JC, et al. Tumor-infiltrating lymphocytes and response to neoadjuvant chemotherapy with or without carboplatin in human epidermal growth factor receptor 2-positive and triple-negative primary breast cancers. J Clin oncol. 2015;33(9):983–991. doi: 10.1200/JCO.2014.58.1967 [DOI] [PubMed] [Google Scholar]
- 18.Chen L, Han X. Anti-PD-1/PD-L1 therapy of human cancer: past, present, and future. J Clin Invest. 2015;125(9):3384–3391. doi: 10.1172/JCI80011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hamada T, Cao Y, Qian ZR, et al. Aspirin use and colorectal cancer survival according to tumor CD274 (programmed cell death 1 ligand 1) expression status. J Clin oncol. 2017;35(16):1836–1844. doi: 10.1200/JCO.2016.70.7547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liang M, Li J, Wang D, et al. T-cell infiltration and expressions of T lymphocyte co-inhibitory B7-H1 and B7-H4 molecules among colorectal cancer patients in northeast China‘s Heilongjiang province. Tumour Biol. 2014;35(1):55–60. doi: 10.1007/s13277-013-1006-6 [DOI] [PubMed] [Google Scholar]
- 21.Saigusa S, Toiyama Y, Tanaka K, et al. Implication of programmed cell death ligand 1 expression in tumor recurrence and prognosis in rectal cancer with neoadjuvant chemoradiotherapy. Int J Clin Oncol. 2016;21(5):946–952. doi: 10.1007/s10147-016-0962-4 [DOI] [PubMed] [Google Scholar]
- 22.Shi SJ, Wang LJ, Wang GD, et al. B7-H1 expression is associated with poor prognosis in colorectal carcinoma and regulates the proliferation and invasion of HCT116 colorectal cancer cells. PLoS One. 2013;8(10):e76012. doi: 10.1371/journal.pone.0076012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Song M, Chen D, Lu B, et al. PTEN loss increases PD-L1 protein expression and affects the correlation between PD-L1 expression and clinical parameters in colorectal cancer. PLoS One. 2013;8(6):e65821. doi: 10.1371/journal.pone.0065821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhu H, Qin H, Huang Z, et al. Clinical significance of programmed death ligand-1 (PD-L1) in colorectal serrated adenocarcinoma. Int J Clin Exp Pathol. 2015;8(8):9351–9359. [PMC free article] [PubMed] [Google Scholar]
- 25.Droeser RA, Hirt C, Viehl CT, et al. Clinical impact of programmed cell death ligand 1 expression in colorectal cancer. Eur J Cancer. 2013;49(9):2233–2242. doi: 10.1016/j.ejca.2013.02.015 [DOI] [PubMed] [Google Scholar]
- 26.Li Y, Liang L, Dai W, et al. Prognostic impact of programed cell death-1 (PD-1) and PD-ligand 1 (PD-L1) expression in cancer cells and tumor infiltrating lymphocytes in colorectal cancer. Mol Cancer. 2016;15(1):55. doi: 10.1186/s12943-016-0539-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wu P, Wu D, Li L, Chai Y, Huang J, Soutto M. PD-L1 and survival in solid tumors: a meta-analysis. PLoS One. 2015;10(6):e0131403. doi: 10.1371/journal.pone.0131403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pyo JS, Kang G, Kim JY. Prognostic role of PD-L1 in malignant solid tumors: a meta-analysis. Int J Biol Markers. 2017;32(1):e68–e74. doi: 10.5301/jbm.5000225 [DOI] [PubMed] [Google Scholar]
- 29.Xiang X, Yu PC, Long D, et al. Prognostic value of PD -L1 expression in patients with primary solid tumors. Oncotarget. 2018;9(4):5058–5072. doi: 10.18632/oncotarget.23580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Koganemaru S, Inoshita N, Miura Y, et al. Prognostic value of programmed death-ligand 1 expression in patients with stage III colorectal cancer. Cancer Sci. 2017;108(5):853–858. doi: 10.1111/cas.13229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wang L, Liu Z, Fisher KW, et al. Prognostic value of programmed death ligand 1, p53, and Ki-67 in patients with advanced-stage colorectal cancer. Hum Pathol. 2018;71:20–29. doi: 10.1016/j.humpath.2017.07.014 [DOI] [PubMed] [Google Scholar]
- 33.Lee LH, Cavalcanti MS, Segal NH, et al. Patterns and prognostic relevance of PD-1 and PD-L1 expression in colorectal carcinoma. Mod Pathol. 2016;29(11):1433–1442. doi: 10.1038/modpathol.2016.139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wang L, Ren F, Wang Q, et al. Significance of programmed death ligand 1 (PD-L1) immunohistochemical expression in colorectal cancer. Mol Diagn Ther. 2016;20(2):175–181. doi: 10.1007/s40291-016-0188-1 [DOI] [PubMed] [Google Scholar]
- 35.Topalian SL, Hodi FS, Brahmer JR, et al. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N Engl J Med. 2012;366(26):2443–2454. doi: 10.1056/NEJMoa1200690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rizvi NA, Mazieres J, Planchard D, et al. Activity and safety of nivolumab, an anti-PD-1 immune checkpoint inhibitor, for patients with advanced, refractory squamous non-small-cell lung cancer (CheckMate 063): a phase 2, single-arm trial. Lancet Oncol. 2015;16(3):257–265. doi: 10.1016/S1470-2045(15)70054-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ansell SM, Lesokhin AM, Borrello I, et al. PD-1 blockade with nivolumab in relapsed or refractory Hodgkin‘s lymphoma. N Engl J Med. 2015;372(4):311–319. doi: 10.1056/NEJMoa1411087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hamid O, Robert C, Daud A, et al. Safety and tumor responses with lambrolizumab (anti-PD-1) in melanoma. N Engl J Med. 2013;369(2):134–144. doi: 10.1056/NEJMoa1305133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Seiwert TY, Burtness B, Mehra R, et al. Safety and clinical activity of pembrolizumab for treatment of recurrent or metastatic squamous cell carcinoma of the head and neck (KEYNOTE-012): an open-label, multicentre, phase 1b trial. Lancet Oncol. 2016;17(7):956–965. doi: 10.1016/S1470-2045(16)30066-3 [DOI] [PubMed] [Google Scholar]
- 40.Ohaegbulam KC, Assal A, Lazar-Molnar E, Yao Y, Zang X. Human cancer immunotherapy with antibodies to the PD-1 and PD-L1 pathway. Trends Mol Med. 2015;21(1):24–33. doi: 10.1016/j.molmed.2014.10.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Meng X, Huang Z, Teng F, Xing L, Yu J. Predictive biomarkers in PD-1/PD-L1 checkpoint blockade immunotherapy. Cancer Treat Rev. 2015;41(10):868–876. doi: 10.1016/j.ctrv.2015.11.001 [DOI] [PubMed] [Google Scholar]
- 42.Guo Y, Yu P, Liu Z, et al. Prognostic and clinicopathological value of programmed death ligand-1 in breast cancer: a meta-analysis. PLoS One. 2016;11(5):e0156323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Xu F, Xu L, Wang Q, An G, Feng G, Liu F. Clinicopathological and prognostic value of programmed death ligand-1 (PD-L1) in renal cell carcinoma: a meta-analysis. Int J Clin Exp Med. 2015;8(9):14595–14603. [PMC free article] [PubMed] [Google Scholar]
- 44.Aguiar PN Jr., Santoro IL, Tadokoro H, et al. The role of PD-L1 expression as a predictive biomarker in advanced non-small-cell lung cancer: a network meta-analysis. Immunotherapy. 2016;8(4):479–488. doi: 10.2217/imt-2015-0002 [DOI] [PubMed] [Google Scholar]
- 45.Xue S, Song G, Yu J. The prognostic significance of PD-L1 expression in patients with glioma: a meta-analysis. Sci Rep. 2017;7(1):4231. doi: 10.1038/s41598-017-04023-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kim JM, Chen DS. Immune escape to PD-L1/PD-1 blockade: seven steps to success (or failure). Ann Oncol. 2016;27(8):1492–1504. doi: 10.1093/annonc/mdw217 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials