Abstract
May-Thurner syndrome most commonly involves compression of the left common iliac vein by the right common iliac artery and can result in leg pain and swelling as well as potentially precipitate deep venous thrombosis. These symptoms can be exacerbated by additional vascular abnormalities. This is a case report of a 91-year-old woman with intractable massive left lower extremity edema that interfered with walking. She was diagnosed with concurrent May-Thurner syndrome and pelvic arteriovenous fistula. Treatment with embolization of the fistula and stenting of the left common iliac vein relieved her symptoms and allowed her to walk again.
May and Thurner first characterized the anatomic variant now known as May-Thurner syndrome (MTS) wherein an overriding right common iliac artery compresses the left common iliac vein (CIV).1 This condition is also known as Cockett syndrome or simply iliac compression syndrome.2 MTS has rarely been reported with other vascular abnormalities.3, 4 We present a case of concomitant MTS and pelvic arteriovenous fistula (AVF) resulting in massive and debilitating left lower extremity edema that was successfully treated with endovascular techniques. The patient consented to publication of this case report.
Case report
A 91-year-old woman with a past medical history of hypertension, congestive heart failure, hyperlipidemia, atrial fibrillation, and hypothyroidism was referred for evaluation of severe intractable left leg swelling. She first noticed swelling 2 years before presentation after undergoing back surgery for spinal stenosis. One year before presentation, she underwent repair of a right hip fracture from a fall complicated by development of extensive left leg deep venous thrombosis (DVT) and pulmonary embolism. She underwent inferior vena cava (IVC) filter placement and was prescribed oral anticoagulation with warfarin. Since then, the left leg has become severely swollen, and she has developed superficial ulceration and serous exudate. She also complained that her toes intermittently become cyanotic and painful. She was treated with diuretics, compression therapy, and a lymphedema pump. Despite all conservative measures, her symptoms progressed, and she became wheelchair bound because of left leg heaviness and swelling. A computed tomography scan at an outside hospital showed early venous filling of the venous circulation suggestive of an AVF, and she was referred for further management. On physical examination, there was massive swelling of the left lower extremity and two areas of skin ulceration over the anterior calf (Fig 1). The swelling extended from the groin to the toes, with a measured thigh circumference of 86 cm. She had distal leg hyperemia and cyanotic toes but intact pulses. Venous duplex Doppler examination demonstrated a patent IVC with complete reversal of flow in the left common femoral vein, with a pulsatile waveform consistent with an AVF at the level of the iliac vessels (Fig 2).
Fig 1.
A, Preoperatively, the patient had severe left lower extremity edema, two areas of skin ulceration on the anterior calf, and cyanosis in the toes. B, Three months postoperatively, the patient's swelling has significantly reduced, the ulcers have healed, and the toes are no longer cyanotic.
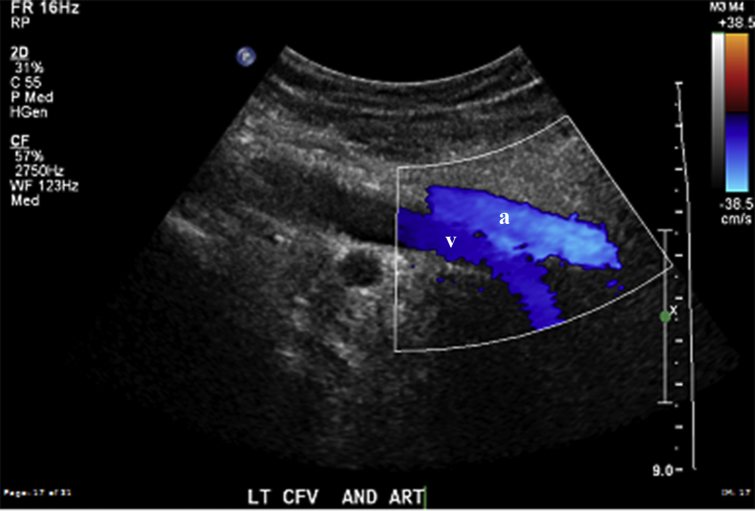
Fig 2.
Venous duplex Doppler examination. Both the left common femoral vein (v) and artery (a) exhibit the same flow direction on color Doppler examination. There is complete reversal of flow toward the lower extremity in the vein as well as pulsatile waveforms (not shown) suggestive of an arteriovenous fistula (AVF).
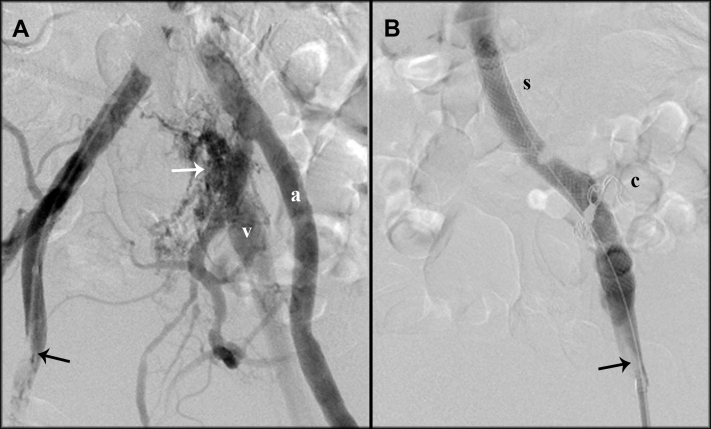
Left lower extremity arteriography was performed through a right common femoral artery puncture. The angiogram confirmed the presence of an AVF with early filling of the left common femoral vein and total reversal of flow consistent with iliac vein occlusion and MTS (Fig 3). Selective catheterization of the left internal iliac artery showed arteriovenous connections from two branches that were successfully coil embolized with 3- to 4-mm Azur coils (Terumo, Somerset, NJ). Completion angiography demonstrated complete obliteration of flow in that area. The left iliac vein demonstrated residual but minimally delayed filling that was significantly improved. A retrograde venogram obtained through left common femoral vein access showed that the proximal CIV was completely occluded. The occlusion was successfully crossed into the IVC. Intravascular ultrasound confirmed the diagnosis of MTS. Measurement of the CIV distal to the occlusion showed a diameter of 12 mm. The occlusion was balloon angioplastied and stented with two 12- × 60-mm Wallstents (Boston Scientific, Marlborough, Mass). The stents extended from the caval confluence to the most central aspect of the left external iliac vein. Completion venography showed excellent antegrade flow through the venous system into the IVC (Fig 3). The flow around the IVC filter had no evidence of obstruction or stenosis, so it was left in situ. The patient had an uneventful postoperative course. She was restarted on warfarin before discharge and given thigh-high 15 to 20 mm Hg compression stockings. After 1 month, her leg swelling decreased significantly, and she was able to walk with a walker again. The ulcers healed, and she lost 25 pounds. Follow-up ultrasound Doppler examination showed resolution of the AVF and normal venous flow in the left common femoral vein (Fig 2). The swelling continued to improve, and her thigh circumference decreased to 50 cm at 10 months (Fig 1).
Fig 3.
Angiography. A, Arteriogram obtained through right common femoral artery access (black arrow) and injection of contrast material at the aortic bifurcation. The left external iliac artery (a) and vein (v) were visualized concomitantly because of early retrograde filling of the vein from an arteriovenous fistula (AVF, white arrow) at the level of the left internal iliac artery. B, Venogram obtained through left common femoral vein access (arrow) after coil embolization of AVF (c) and stenting (s) of left common iliac vein (CIV) shows normal flow through the venous system.
Discussion
MTS most commonly affects women in their second through fourth decades of life but has been described in elderly patients as well.1 Patients with MTS typically present with leg swelling or DVT.2, 5 They account for at least 2% of patients evaluated for lower extremity venous disorders, 60% of patients with left-sided DVT, and 37% of patients with isolated left lower extremity edema.5, 6, 7 May and Thurner initially described “spurs” of the wall of the iliac vein from chronic irritation and compression by the iliac artery causing venous stenosis, which predisposes to thrombosis.1
The patient likely had some asymptomatic compression of the left iliac vein most of her life. She could have developed the iliac AVF after spine surgery because iatrogenic injuries have been recognized as a cause of AVF formation, especially after catheterization or open surgery. In a review of the literature, vascular injuries were reported to occur at a frequency of up to 5 per 10,000 lumbar disk surgeries performed through a posterior approach, with AVF accounting for 67% of such injuries.8 She did not have a DVT at that time but already noticed left leg swelling. After her hip replacement, provoked DVT and pulmonary embolism developed, and the left CIV that was providing outflow to the pelvic AVF occluded, which likely led to her symptom progression. Although she may have improved with AVF treatment alone, we believed that treating both simultaneously would give her the best symptomatic relief.
To date, only two instances similar to our case of MTS and AVF have been reported. However, we believe that we are reporting the first complete case of true MTS and AVF. Mihmanli et al9 described a case of MTS and AVF diagnosed by computed tomography, but their patient had minimal compression of the left iliac vein on our review of the imaging, and they do not discuss treatment. Link and Granchi10 treated a patient with nonhealing ulcers who reportedly had MTS and AVF. The question of true MTS vs venous occlusive disease remains, though, as none of their imaging was sufficient to confirm. They also treated only the fistula with coil embolization and Onyx (Covidien, Plymouth, Minn) liquid embolic agent, which was not sufficient for ulcer healing, thus prompting subsequent sclerotherapy. There was no consideration for recanalization of the iliac vein.
Venous stenting under intravascular ultrasound guidance has been shown to be effective for treatment of lower extremity swelling in the setting of outflow tract obstruction. At 5 years, cumulative complete relief of swelling has been reported to be 32% with 58% ulcer healing.11 Endovascular approaches have recently become more popular, and different studies have found 50% to 100% patency after 1 year.5, 12 Raju and Ward demonstrated that iliac vein stenting was safe and effective in a group of elderly patients aged 80 to 96 years.13 There was no mortality 30 days postoperatively, and the median survival after stent placement was 2 years.
Conclusions
We report the first case of concurrent MTS and pelvic AVF treated with simultaneous embolization of the AVF and recanalization and stenting of the left CIV. In a patient with such severe symptoms, clinicians should consider the presence of more than one vascular abnormality, and cross-sectional imaging is warranted. Endovascular therapy with embolization and stenting can provide substantial relief and can be safe even in patients of advanced age.
Footnotes
Author conflict of interest: none.
The editors and reviewers of this article have no relevant financial relationships to disclose per the Journal policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
References
- 1.May R., Thurner J. The cause of the predominantly sinistral occurrence of thrombosis of the pelvic veins. Angiology. 1957;8:419–427. doi: 10.1177/000331975700800505. [DOI] [PubMed] [Google Scholar]
- 2.Cockett F.B., Thomas M.L., Negus D. Iliac vein compression.—Its relation to iliofemoral thrombosis and the post-thrombotic syndrome. Br Med J. 1967;2:14–19. doi: 10.1136/bmj.2.5543.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lu T., de Grandis E., Gloviczki P., Glockner J., Shepherd R.F. May-Thurner syndrome associated with Klippel-Trenaunay syndrome. Perspect Vasc Surg Endovasc Ther. 2012;24:155–160. doi: 10.1177/1531003513482736. [DOI] [PubMed] [Google Scholar]
- 4.Cheema Z.F., Lumsden A.B., Museum of TMH Multimodality Imaging Center Congenital aplasia of the left iliac vein in a patient with concomitant Sturge-Weber syndrome and May-Thurner syndrome with congenital aberrant left femoral to right greater saphenous vein bypass. Methodist Debakey Cardiovasc J. 2012;8:49. doi: 10.14797/mdcj-8-1-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Taheri S.A., Williams J., Powell S., Cullen J., Peer R., Nowakowski P. Iliocaval compression syndrome. Am J Surg. 1987;154:169–172. doi: 10.1016/0002-9610(87)90172-3. [DOI] [PubMed] [Google Scholar]
- 6.Chung J.W., Yoon C.J., Jung S.I., Kim H.C., Lee W., Kim Y.I. Acute iliofemoral deep vein thrombosis: evaluation of underlying anatomic abnormalities by spiral CT venography. J Vasc Interv Radiol. 2004;15:249–256. doi: 10.1097/01.rvi.0000109402.52762.8d. [DOI] [PubMed] [Google Scholar]
- 7.Wolpert L.M., Rahmani O., Stein B., Gallagher J.J., Drezner A.D. Magnetic resonance venography in the diagnosis and management of May-Thurner syndrome. Vasc Endovascular Surg. 2002;36:51–57. doi: 10.1177/153857440203600109. [DOI] [PubMed] [Google Scholar]
- 8.Papadoulas S., Konstantinou D., Kourea H.P., Kritikos N., Haftouras N., Tsolakis J.A. Vascular injury complicating lumbar disc surgery. A systematic review. Eur J Vasc Endovasc Surg. 2002;24:189–195. doi: 10.1053/ejvs.2002.1682. [DOI] [PubMed] [Google Scholar]
- 9.Mihmanli I., Kantarci F., Ulus S.O., Bozlar U., Kadioglu A., Yildirim D. Lower extremity venous pathology mimicking deep vein thrombosis: 2 case reports. Ultraschall Med. 2007;28:421–425. doi: 10.1055/s-2007-963048. [DOI] [PubMed] [Google Scholar]
- 10.Link D.P., Granchi P.J. Chronic iliac vein occlusion and painful nonhealing ulcer induced by high venous pressures from an arteriovenous malformation. Case Rep Radiol. 2011;2011:514721. doi: 10.1155/2011/514721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Neglén P., Hollis K.C., Olivier J., Raju S. Stenting of the venous outflow in chronic venous disease: long-term stent-related outcome, clinical, and hemodynamic result. J Vasc Surg. 2007;46:979–990. doi: 10.1016/j.jvs.2007.06.046. [DOI] [PubMed] [Google Scholar]
- 12.Moudgill N., Hager E., Gonsalves C., Larson R., Lombardi J., DiMuzio P. May-Thurner syndrome: case report and review of the literature involving modern endovascular therapy. Vascular. 2009;17:330–335. doi: 10.2310/6670.2009.00027. [DOI] [PubMed] [Google Scholar]
- 13.Raju S., Ward M. Utility of iliac vein stenting in elderly population older than 80 years. J Vasc Surg Venous Lymphatic Disord. 2015;3:58–63. doi: 10.1016/j.jvsv.2014.08.001. [DOI] [PubMed] [Google Scholar]