Abstract
Background
The pattern of stroke in rural population differs from that in urban ones. Although there are many studies on this condition in sub-Saharan Africa, few studies about stroke pattern in a Kenyan rural area exist.. This study therefore aims at describing the characteristics of stroke in a rural Kenyan hospital.
Patients and Methods
The study was conducted on 227 consecutive patients admitted with a World Health Organization (WHO) diagnosis of stroke in Kangundo Hospital, a level IV facility in Machakos, Eastern Kenya, between April 2015 and September 2016. The sub-type and anatomical distribution of stroke as well as the age, gender of the patients were recorded prospectively. Diagnosis was made through physical neurological examination and confirmed by Computerized Tomography (CT) scan imaging. Only those with complete bio-data, past medical and social history, clinical and physical findings of the patients and imaging results were included. The data were entered into a pre-formatted questionnaire, analysed for means, standard deviations and frequencies, and are presented in tables and bar charts.
Results
Out of 3200 medical admissions, 227 (7.09%) had a confirmed diagnosis of stroke. Ischaemic stroke was more common (67.4%) than haemorrhagic stroke (32.6%). It affected mainly the anterior circulation, especially the middle cerebral artery (39%). The mean age of patients was 68.8 years, (Range 32–96). It was more common in females (62%) than in males (38%). Hypertension was the most common (74%) risk factor followed by alcohol abuse (63%), tobacco smoking (48%) and diabetes mellitus (42%).
Conclusion
Ischaemic stroke was the more common major cause of morbidity in the rural hospital studied in Kenya. It occurred most commonly among elderly females, with the most frequent comorbidities being hypertension. In addition, modifiable lifestyle factors like alcohol abuse and cigarette smoking contributed to the prevalence; hence we recommend the control of blood pressure and glucose as well as lifestyle modification to reduce the scourge in our studied population.
Keywords: Stroke, rural, types, risk factors, age
Introduction
Stroke in rural communities is a major cause of morbidity and mortality worldwide including in sub-Saharan Africa1–3. It differs from that in urban ones with regard to incidence4,5, age and gender distribution6,7, risk factor profile7,8 and mortality rate9,10. The pattern is important in informing planning and management strategies11. Data are, however, disparate and scarce from sub-Saharan Africa4,5. In Kenya, it is a substantial cause of morbidity and mortality12 but the pattern is not elucidated. The aim of this study was, therefore, to determine the pattern of stroke in a rural Kenyan hospital.
Patients and Methods
The study was done on patients admitted with a diagnosis of stroke in Kangundo Hospital during an interval of 18 months, between April 2015 and September 2016. Kangundo is a level IV rural health facility located 80 kilometres away from Nairobi City and has a bed capacity of 170. Only patients who met the World Health Organization (WHO) criteria of focal or global disturbance of cerebral function of sudden onset lasting at least 24 hours or leading to death with no apparent cause other than vascular origin were included13. This included black adults of both genders. Patients with history of head trauma or no neuro-imaging on record were excluded from study. Informed consent was obtained from all the patients and their relatives. Patients who were stable and conscious were informed about the study and its importance. For the unconscious patients, their relatives were informed about the study and permission to include these patients in the study was sought from the relatives. Those who gave consent were included in the study but only their serial numbers were used not names.
Data on age, gender and risk factors of stroke patients were obtained prospectively, directly from the patient or their next of kin. Relevant medical and social history of the patients, including history of confirmed comorbidities namely hypertension, diabetes, cardiac disorder, drug history, history of substance use (mainly alcohol abuse and cigarette smoking), history of previous stroke and HIV was also obtained. Investigations such as head Computerised Tomography (CT) scan and Brain Magnetic Resonance Imaging (MRI) were used to determine the type of stroke and assess the cerebral territory affected by ischemic stroke. Atrial fibrillation was confirmed by electrocardiography.
Data were entered into a pre-formatted questionnaire
Subjects were divided into males and females and clustered in 10 year age groups. Stroke was classified as either ischemic or haemorrhagic. Ischaemic stroke was classified according to the brain territory affected and the main arterial supply namely anterior, middle or posterior cerebral arteries. Data were entered into the computer and analysed using SPSS® (Statistical package for social science) software (Version 20.0, Chicago, Illinois) and Microsoft Office Excel, 2007 (Microsoft Corporation). Measurements were expressed in means, frequencies and standard deviations. Results were presented in tables and bar charts.
Results
Within the 18 months that this study was carried out, the Hospital recorded 3200 medical admissions of which 227 patients were admitted due to stroke. This accounted for 7.09% of all medical admissions.
1. Type and anatomical distribution of lesions
Out of the 227 patients, 153 (67.4%) had ischaemic stroke, while the remaining 74 (32.6%) had haemorrhagic stroke. Among the 153 ischaemic stroke cases, the vascular territory most commonly involved was the middle cerebral artery (77; 50.3%), followed by the anterior cerebral artery (54; 35.3%) and the posterior cerebral artery (22; 14.4%).
2. Age and gender distribution
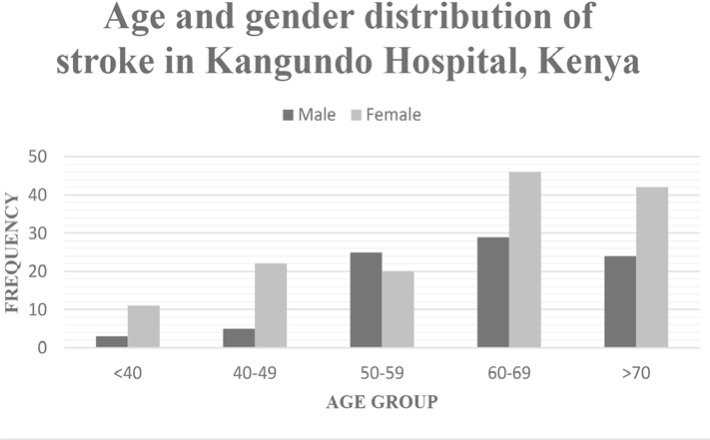
The mean age of the patients was 68.8±6.8 years (range 32–96 years). The mean age for males was 64.28±6.31 years while that for females was 69.34±7.22 years. The mode was 64 years. The incidence of stroke increased with advancing age, with majority (62%) of the patients being above 60 years. The peak was 60–69 years. Stroke was more common among female subjects (62%). Except for the 50–60 year age group, stroke was consistently higher in females. There were 86 males and 141 females, giving an overall male: female ratio of 3:5 (Figure 1).
Figure 1.
Age and gender distribution of stroke in Kangundo Hospital, Kenya
3. Risk factors
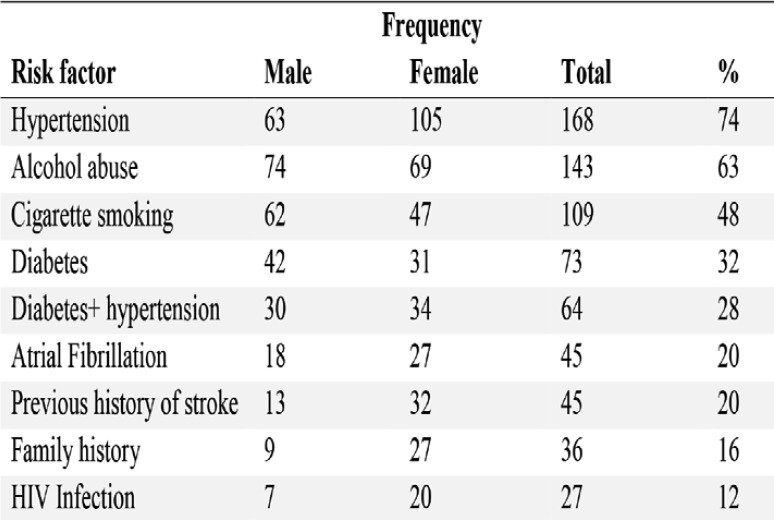
The most common risk factor of stroke was hypertension (168; 74%) followed by alcohol abuse (143; 63%), cigarette smoking (109; 48%), diabetes mellitus (73; 32%), diabetes and hypertension (64; 28%) and atrial fibrillation (45; 20%) (Table 1).
Table 1.
Risk factors for stroke in Kangundo Hospital, Kenya
Discussion
Stroke constituted over 7% of medical admissions in our studied group. This was higher than 3.04 per 1000 reported for Nairobi Hospital14 and 3.77 per 1000 reported for Kenyatta National Hospital15 both of which received predominantly urban populations. Our finding was concordant with reports that stroke was more common in rural than urban populations5. This difference has been attributed to distribution of risk factors4. In view of the poor outcome of stroke in rural Kenya16, effort should be expended in its control.
1. Type and anatomical distribution
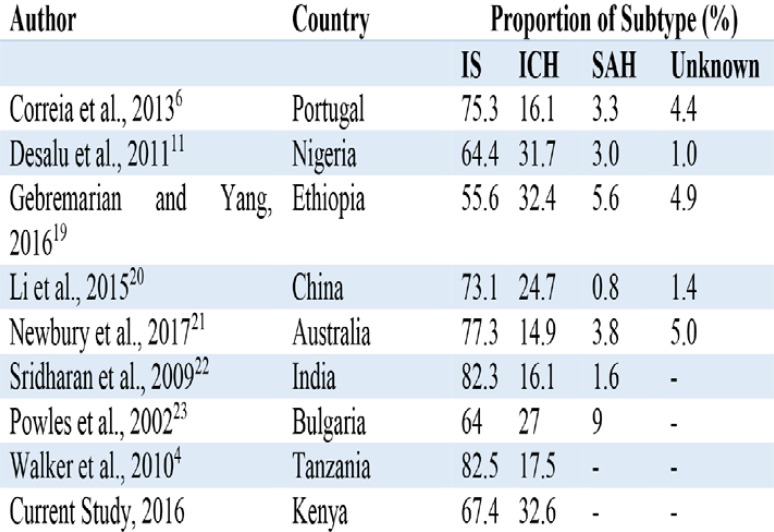
The sub-type and anatomical distribution of stroke lesions influence clinical assessment, treatment decisions, prognosis and risk of recurrence17 and are important for country — specific health care planning3. In the current study, 67.4% of the cases were ischemic stroke. This is within the range of 55–83% reported in contemporary literature from South Asian18 and other countries (Table 2).
Table 2.
Proportion of stroke subtype in rural populations of some countries
These results show wide diversity probably depending on race, genetics, gender, age, lifestyle, diet and socioeconomic status20,24,25. In the present study, the profile of risk factors and hence the mechanism may be important. Pertinent to this suggestion is the finding that hypertension which was the predominant risk factor is usually associated with haemorrhagic rather than ischaemic stroke.
The site of cerebral vessel occlusion influences the spatial pattern and temporal progression of infarction and is important in interpreting imaging findings26. In the current study, the middle cerebral artery was the most involved vessel. This is consistent with literature reports27 and is probably related to the anatomy of cerebral arterial blood supply. In this regard, recent studies reveal that the pattern of cerebral arteries in the Kenyan population resembles that of other populations28,29.
2. Age and gender distribution
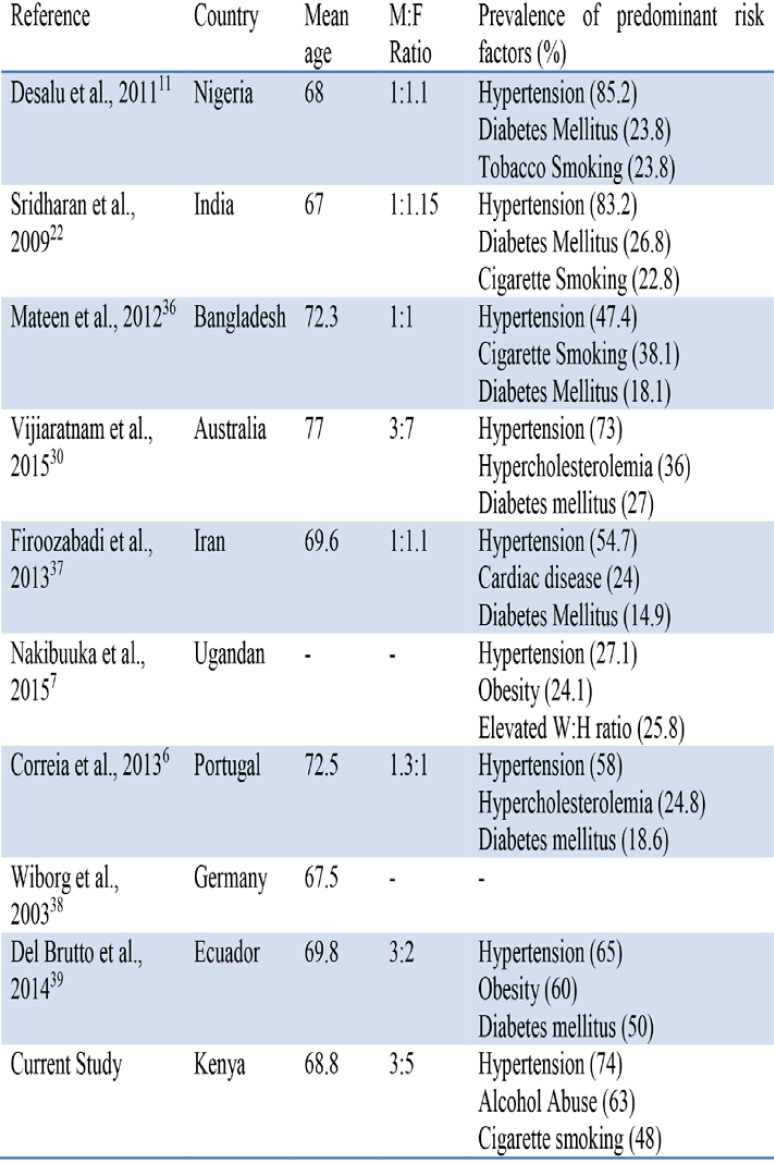
The mean age of patients was 68.8 years with a peak at 60–69 years. This mean age is higher than 54.7 and 61.5 years reported in urban Kenyan hospitals14,15. It is, nonetheless, comparable with those reported for other rural populations (Table 3). This is consistent with reports that stroke victims from rural populations are older than their urban counterparts6,7.
Table 3.
Mean age, gender distribution and risk factors for stroke in some rural communities
The male: female ratio of 3:5 is comparable with 3:7 reported for the Australian30 population. Other studies reported only marginal female predominance (Table 3). It is probably related to the loss of the protective effect of oestrogen among post-menopausal women31.
3. Risk factors
Recent studies reveal that risk factors for stroke in rural populations of sub-Saharan Africa namely hypertension, dyslipidaemia, smoking, cardiac events, diabetes and HIV infection resemble those reported for other world regions32. The distribution however varies from country to country. Whereas, in the current study, hypertension, excessive alcohol consumption, cigarette smoking and diabetes mellitus predominated, the latter four were reported to be rare in Uganda7. This implies that risk factors for stroke must be considered by country.
Hypertension
Hypertension was the predominant risk factor, similar to the urban and other rural cohorts. High blood pressure has been implicated as a major risk for stroke in many rural communities in South Africa3, Kenya33, Tanzania32 and Uganda7 (Table 3). This is consistent with the profile of cardiovascular disease risk factors reported in rural Kenyan populations34, 35. Indeed, hypertension is a highly prevalent condition in many rural parts of Kenya. This implies that control of blood pressure constitutes an important step in mitigating prevalence of stroke in these communities.
Excessive alcohol consumption
A remarkable finding of the present study is that 63% of stroke patients had a history of heavy alcohol consumption, which is an independent risk factor for ischaemic stroke40–42. It induces hypertension, promotes hypercoagulability, predisposes to atrial fibrillation, and accelerates large artery atherosclerosis, cardiac arrhythmia, cerebral arterial spasm, blood clotting disorders and, cardiogenic embolism42–44. The high prevalence of alcohol abuse in stroke patients is consistent with reports that alcohol abuse is highly prevalent in rural Kenya probably due to availability of cheap, home manufactured alcohol45. We therefore recommend campaigns and programs to educate people on the side effects of alcohol use in order to reduce the stroke burden.
Cigarette smoking
Up to 25% of all strokes are directly related to cigarette smoking which independently increases the risk of stroke up to three-fold46, 47. In the current study, 48% of the patients had a positive history of cigarette smoking. This is higher than 39% reported in Asian and other sub-Saharan African countries (Table 3). In Uganda, for example, it constituted less than 5%7. This implies that there are variations in the preponderance of the risk caused by smoking. These variations are probably related to the amount and duration of smoking46. The high prevalence in the current study is related to the prevalence of this vice in rural Kenya45,48. Cigarette smoking causes endothelial dysfunction, inflammation, insulin resistance, alteration in lipid profile, hemodynamic stress, hypercoagulable state and oxidative stress, all of which contribute to vasomotor dysfunction and atherothrombosis49,50. Health campaigns to promote smoking cessation will help reduce the risk of stroke.
Diabetes mellitus
Diabetes mellitus alone was implicated in 32% of cases. This is much higher than those reported in other studies, only lower than 50% reported in Ecuador39. This high occurrence may be related to the comparatively high prevalence of dysglycaemia reported in rural Kenyan communities34,35. Diabetics have a 2.5 greater risk of stroke than their non-diabetic counterparts51. Early diagnosis and good control of diabetes is recommended in order to reduce the risk of stroke. Having both diabetes and hypertension increases the risk of getting a stroke. In the current study, 28% of patients had both diabetes and hypertension. This compares to 28.8% by Jowi and Mativo14. Stroke prevention should therefore aim at health campaigns to increase awareness, ensure early diagnosis and achieving good control of these two non-communicable conditions.
Atrial fibrillation
Atrial fibrillation (AF) is an independent risk factor for cardio-embolic stroke52–54. Embolism of cardiac origin causes up to 25% of all ischaemic strokes55, through contractile dysfunction, structural remodelling, cardiopathy and stasis, increasing the risk of thromboembolism. Simultaneously, AF increases risk of large artery atherosclerosis, ventricular systolic dysfunction and in — situ small — vessel occlusion56,57. The prevalence of AF is generally low but increases with age58,59. In the current study, 20% of the patients had AF. This was lower than 65.9 % in an Egyptian study60. Strokes in association with AF are more often fatal, disabling and associated with greater morbidity and recurrence than other causes of stroke61. Patients with AF should therefore be monitored to forestall stroke.
Family history
A positive family history is an independent risk factor for both ischaemic and haemorrhage stroke43,62. An increase in the incidence of stroke by two-fold has been reported among first degree relatives63. It may be present in up to 37% of stroke cases64. In the current study, 16% of the patients had a positive family history of stroke. This was higher than 6.1% reported by Essa et al.60. It implied that the population may have genetic markers of stroke, and should be investigated further. There was also the need for regular screening in subjects with a positive family history.
Previous stroke
A history of previous stroke predisposes to recurrent stroke incidences60. Our study showed that 20% of the stroke patients had a positive history of stroke. This is within the range of 19–32% reported in literature65. First time stroke survivors are at a significantly increased risk for further stroke compared to the general population65. Recurrent stroke has higher mortality and poor health related quality of the life66. Accordingly, stroke victims should be closely monitored and followed up for mitigation of predisposing factors to avert recurrence.
HIV infection
HIV has recently emerged an independent risk factor for stroke including in rural populations32,67. In this study 12% of the patients had HIV infection. This is comparable with 15% reported in rural Tanzania32. HIV infection can cause stroke through accelerated atherosclerosis, hypercoagulability, inflammation of small intracranial arteries leading to a prothrombotic effect68, opportunistic infection, cardioembolism, coagulopathy, diabetes and hypertension19,21,22. In view of the high prevalence of HIV infection in Kenya, victims should be followed up and started on treatment to mitigate the risk of stroke.
Conclusion
Stroke, more commonly the ischaemic type, is a major cause of morbidity in rural hospitals in Kenya. It occurs most commonly among the elderly and more in females. The most frequent risk factors are hypertension and modifiable lifestyle factors like alcohol abuse and cigarette smoking. We recommend control of blood measure, blood sugar and lifestyle modification.
Acknowledgement
We are grateful to Antonina Odock — Opiko for typing the manuscript.
Conflict of interest
There is no conflict of interest.
References
- 1.Wasserman S, de Villiers L, Bryer A. Community — based care of stroke patients in a rural African setting. S Afr Med J. 2009;99:579–583. [PubMed] [Google Scholar]
- 2.Enwereji KO, Nwosu MC, Ogunniyi A, Nwami PO, Asomugha AL, Enwereji EE. Epidemiology of stroke in a rural community in South Eastern Nigeria. Vasc Health Risk Manag. 2014;10:375–388. doi: 10.2147/VHRM.S57623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Maredza M, Bertram MY, Tollman SM. Disease burden of stroke in rural South Africa: an estimate of incidence, mortality and disability adjusted life years. BMC Neurol. 2015;15:54. doi: 10.1186/s12883-015-0311-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Walker R, Whiting D, Unwin N, Mugusi F, Swai M, Aris E, et al. Stroke incidence in rural and urban Tanzania: a prospective community based study. Lancet Neurol. 2010;9(8):786–792. doi: 10.1016/S1474-4422(10)70144-7. [DOI] [PubMed] [Google Scholar]
- 5.Gong Y, Wei X, Liang Y, Zou G, Hu R, Deng S, et al. Urban and Rural Differences of Acute cardiovascular Disease Events: A study from the Population Based Real- Time Surveillance system in Zhejiang, China in 2012. PLOS ONE. 11(11):e0165647. doi: 10.1371/journal.pone.0165647. Https://doi.org/10.1371/Journal pone. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Correia M, Magalhaes R, Silva MR, Matos I, Silva MC. Stroke types in rural and urban Northern Portugal: Incidence and 7 — year survival in a community based study. Cardiovasc Dis Extra. 2013;3:137–149. doi: 10.1159/000354851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nakibuuka J, Sajatovic M, Nankaburwa J, Furlan AJ, Kayima J, Ddumba E, et al. Stroke risk factors differ between rural and urban communities: population survey in Central Uganda. Neuroepidemiol. 2015;44:156–165. doi: 10.1159/000381453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mi T, Sun S, Du Y, Guo S, Cong L, Cao M, et al. Differences in the distribution of risk factors for stroke among the high risk population in urban and rural areas of Eastern China. Brain Behav. 2016;6(5):e00461. doi: 10.1002/brb3.461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sergeev AV. Racial and Rural urban disparities in stroke mortality outside the stroke belt. Ethn Dis. 2011;21(3):307–313. [PubMed] [Google Scholar]
- 10.Ingram DD, Montresor-Lopez JA. Differences in stroke mortality among adults aged 45 and over: United States, 2010-2013. NCHS Data Brief. 2015 Jul;(207):1–8. [PubMed] [Google Scholar]
- 11.Desalu OO, Wahab KW, Fawole B, Olarenwaju TO, Busari OA, Adekoya AO, et al. A review of stroke admissions at a tertiary hospital in rural South Western Nigeria. Ann Afr Med. 2011;10(2):80–85. doi: 10.4103/1596-3519.82061. [DOI] [PubMed] [Google Scholar]
- 12.Etyang AO, Munge K, Bunyasi EW, Matata L, Ndila C, Kapesa S, et al. Burden of disease in adults admitted to hospital in a rural region of coastal Kenya; an analysis of data from linked clinical and demographic surveillance system. 2014 Apr 27;2(4):e216–e224. doi: 10.1016/s2214.109*(14). Published online 2014. 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thorvaldsen P, Asplund K, Kuulasmaa K, Rajakangas AM, Schroll M. Stroke incidence, case fatality and mortality in the WHO MONICA project. World Health Organization monitoring trends and determinants in cardiovascular disease. Stroke. 1995;26:361–367. doi: 10.1161/01.str.26.3.361. [DOI] [PubMed] [Google Scholar]
- 14.Jowi JO, Mativo PM. Pathological sub-types, risk factors and outcome of stroke at the Nairobi hospital, Kenya. East Afr Med J. 2008;85:572–581. doi: 10.4314/eamj.v85i12.43535. [DOI] [PubMed] [Google Scholar]
- 15.Ogeng'o JA, Gatonga P, Olabu BO. Cardiovascular causes of death in an East African country an autopsy study. Cardio J. 2011;18(1):67–72. [PubMed] [Google Scholar]
- 16.Muli G, Rhoda A. Quality of life amongst young adults with stroke living in Kenya. Afr Health Sci. 2013;13(3):632–638. doi: 10.4314/ahs.vi3.i3.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rovira A, Grive E, Rovira A, Alvarez-sabin J. Distribution territories and causative mechanisms of Ischemic stroke. Eur Radiol. 2005;15(3):416–426. doi: 10.1007/s000-004-2633-5. [DOI] [PubMed] [Google Scholar]
- 18.Wasay M, Khatri IA, Kaul S. Stroke in South Asian countries. Nat Rev Neurol. 2014;10(3):135–143. doi: 10.1038/nrneurol.2014.13. [DOI] [PubMed] [Google Scholar]
- 19.Gebremariam SA, Yang HS. Types, risk profiles and outcomes of stroke patients in a tertiary teaching hospital in Northern Ethiopia. eNeurologicalsc. 2016;3:41–47. doi: 10.1016/j.ensci.2016.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li L, Yin GS, Geraghty OC, Schulz UG, Kuker W, Mechta Z, et al. Incidence, outcome, risk factors and long term prognosis of crptogenic transient Ischaemic attack and Ischaemic stroke a population-based study. Lancet Neurol. 2015;14(9):903–913. doi: 10.10.1016/s1474-4422(15)00132-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Newbury J, Kleining T, Leyden J, Arima H, Castle S, Cranefield J, et al. Stroke epidemiology in an Australian Rural Cohort (SEARCH) Int J Stroke. 2017;12(2):161–168. doi: 10.1177/1747493016670174. [DOI] [PubMed] [Google Scholar]
- 22.Sridharan SE, Uninkrishnan JP, Sukumaran S, Sylaja PN, Nayak SD, Sarma PS, et al. Incidence, types, risk factors and outcome of stroke in a developing country. The Trivandrum Stroke Registry. Stroke. 2009;40(4):1212–1218. doi: 10.1161/STROKEAHA.108.531293. [DOI] [PubMed] [Google Scholar]
- 23.Powles J, Kirov P, Feschieva N, Stanoev M, Atanasova V. Stroke in urban and rural populations in north-east Bulgaria: incidence and case fatality findings from a ‘hot pursuit’ study. BMC Public Health. 2002;2:24. doi: 10.1186/1471-2458-2-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sacco RL, Boden-Albala B, Abel G, Lin IF, Elkund M, Hauser WA, et al. Race ethnic disparities in the impact of stroke risk factors. The Northern Manhattan stroke study. Stroke. 2001;32(8):1725–1731. doi: 10.1161/01.str.32.8.1725. [DOI] [PubMed] [Google Scholar]
- 25.Bravata DM, Wells CK, Gulanski B, Kernan WN, Brass LM, Long J, et al. racial disparities in stroke risk factors: the impact of socioeconomic status. Stroke. 2005;36(7):1507–1511. doi: 10.1161/01.STR.0000170991.63594.b6. doi: 1161/01.STR.0000170991.63594.b6. [DOI] [PubMed] [Google Scholar]
- 26.Phan TG, Donnan GA, Wright PM, Rentens DC. A digital map of middle cerebral artery infarcts associated with middle cerebral artery trunk and branch occlusion. Stroke. 2005;36(5):986–991. doi: 10.1161/01.STR.0000163087.66828.e9. [DOI] [PubMed] [Google Scholar]
- 27.Cheng B, Golaari A, Fiehler J, Rosenkranz M, Gerloff C, Thomalla G. Dynamics of regional distribution of ischemic lesions in middle cerebral artery trunk occlusion relates to collateral circulation. J Cereb Blood Flow Metab. 2011 Jan;31(1):36–40. doi: 10.1038/jcbfm.2010.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sinkeet R, Ogeng'o J, Saidi H. Topography of posterior communicating artery in a Kenyan population. Ann Afr Surg. 2010;5:37–40. [Google Scholar]
- 29.Ogeng'o J, Olabu BO, Mburu AN, Sinkect SR, Ogeng'o NM. Ischemic cortical stroke in a Kenyan Referral Hospital. J Mol Biomark Diagn. 2015;5:238. doi: 10.4172/2155-9929.1000238. [DOI] [Google Scholar]
- 30.Vijiaratnam N, Yan B, Anjara P, Kraemer T, Lau M, Knight B. Stroke care in an Australian rural private health care setting. World J Neurosci. 2015;5(1):7–12. doi: 10.4236/wjns.2015.51002. [DOI] [Google Scholar]
- 31.Lisabeth L, Bushnell C. Stroke risk in woman: the role of menopause and hormone therapy. Lancet Neurol. 2012;11(1):82–91. doi: 10.1016/s1474-4422(11)70269-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Walker RW, Jusabani A, Aris E, Gray WK, Unwin N, Swai M, et al. Stroke risk factors in an incident populations in urban and rural Tanzania: a prospective community- based, case control study. Lancet Glob Health. 2013;1(5):e282–e288. doi: 10.1016/S2214-109X(13)70068-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bloomfield GS, Nwangi A, Chege P, Simivu J, Aswa DF. Multiple cardiovascular disease risk factors in rural Kenya: evidence from a health and demographic surveillance system using the WHO STEP — wise approach to chronic disease risk factor surveillance. Heart. 2013;99(18):1323–1339. doi: 10.1136/heartjnl-2013-303913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Messer LH, Mc Fann K, Kennedy K, Hokanson JE. High prevalence of hypertension in rural and urban populations in Kenya. 138st APHA Annual Meeting and Exposition. 2010 [Google Scholar]
- 35.Pastakia SD, Karwa R, Kahn CB, Nyabundi JS. The Evolution of Diabetes care in the rural, resource constrained setting of Western Kenya. Ann Pharmacother. 2011;45(6):721–726. doi: 10.1345/aph.1P779. [DOI] [PubMed] [Google Scholar]
- 36.Mateen FJ, Carone M, Alam N, Streatfield PK, Black RE. A population — based case control study of 1250 stroke deaths in rural Bangladesh. Eur J Neurol. 2012;19(7):999–1006. doi: 10.1111/j.1468-1331.2012.03666.x. [DOI] [PubMed] [Google Scholar]
- 37.Firoozabadi MD, Kazemi T, Sharifzadeh G, Dadbeh S, Dehghan P. Stroke in Birjand, Iran: A hospital based study of acute stroke. Iran Red Cres J. 2013;15(3):264–268. doi: 10.5812/irenj.4282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wiborg A, Widder B. Telemedicine in stroke in Swabia project. Teleneurology to improve stroke care in rural areas: The Telemedicine in stroke in Swabia (TESS) project. Stroke. 2003;34(12):2951–2956. doi: 10.1161/01.STR.0000099125.30.731.97. [DOI] [PubMed] [Google Scholar]
- 39.Del Brutto OH, Santamaria M, Zambrano M, Penaherrera E, Pow-Chon-Long F, Del Brutto VJ, et al. Stroke in rural coastal Ecuador: a community — based survey. Int J Stroke. 2014;9(3):365–366. doi: 10.1111/ijs.12102. [DOI] [PubMed] [Google Scholar]
- 40.Al- Busaidi IS, Almari Y. Post stroke anxiety and depression: findings from Saudi Arabia. J Stroke cerebrovas Disease ens. 2016;25(7):1653–1654. doi: 10.1016/j.jstrokecerebrovasdis.2016.03.003. [DOI] [PubMed] [Google Scholar]
- 41.Reynolds K, Nolen JDL, Kinney G, Lewis B. Alcohol consumption and risk of stroke: A meta — analysis. JAMA. 2003;289(5):579–588. doi: 10.1001/jama.289.5.579. [DOI] [PubMed] [Google Scholar]
- 42.Sundell L, Salomaa V, Vartianen E, Poikalainen K, Laatikainen T. Increased stroke risk is related to a Binge drinking habit. Stroke. 2008;39:3179–3184. doi: 10.1161/STROKEAHA.108.520817. [DOI] [PubMed] [Google Scholar]
- 43.Smith WS, Sung G, Starkman S, Saver JL, Kidwell CS, Gobin YP, et al. Safety and efficacy of mechanical embolectomy in acute efficacy of mechanical embolectomy in acute Ischemic stroke: results of the MERCI trail. Stroke. 2005;36(7):1432–1438. doi: 10.1161/01.STR.0000171066.25248.1D. [DOI] [PubMed] [Google Scholar]
- 44.Kanyal N. The Science of Ischemic Stroke: Pathophysiology & Pharmacological Treatment. Int J Pharma Res Rev. 2015;4:65–84. [Google Scholar]
- 45.Lo TQ, Oeltmann JE, Odhiambo FO, Beynon C, Pevzner E, Cain KP, et al. Alcohol use, drunkenness and tobacco smoking in rural Western Kenya. Trop Med Int Health. 2013;18(4):506–515. doi: 10.1111/tmi.12066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hankey GJ. Smoking and Risk of Stroke. J Cardiovasc Risk. 1999;6(4):207–211. doi: 10.1177/204748739900600403. [DOI] [PubMed] [Google Scholar]
- 47.Shah SR, Cole WH. Smoking and stroke: the more you smoke the more you stroke. Expert Rev Cardiovasc Ther. 2010;8(7):917–932. doi: 10.1586/erc.10.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Poulter NR, Khaw KT, Hopwood BE, Mugambi M, Peart WS, Rose G, et al. The Kenyan Luo migration study: observations on the initiative of a rise in blood pressure. BMJ. 1990;300(6730):967–972. doi: 10.1136/bmj.300.6730.967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ambrose ZA, Barua RS. The pathophysiology of cigarette smoking and cardiovascular disease: an update. J Am Coll Cardio. 2004;43(10):1731–1737. doi: 10.1016/j.jacc.2003.12.047. http/doi:org/10.1016/jjaac2003.12.047. [DOI] [PubMed] [Google Scholar]
- 50.Salahuddin H, Hussaini S, Tietjen G. Ischemic stroke after plasma donation. Neurology. 2016;86(16 supplement)(4):365. [Google Scholar]
- 51.Danesi MA, Oyenola YA, Onitiri CA. Risk factors associated with cerebrovascular accidents in Nigerians-A case-control study. East Afr Med J. 1983;3(4):190–195. doi.org/10.1111/j.1747-4949.2008.00217.x. [PubMed] [Google Scholar]
- 52.Waldo AL, Becker RC, Tapson VF, Colgan KJ, NABOR steering committee Hospitalized patients with atrial fibrillation and a high risk of stroke not being provided with adequate anticoagulation. J Am Coll Cardiol. 2005;46(9):1729–1736. doi: 10.1016/j.jacc.2005.06.077. [DOI] [PubMed] [Google Scholar]
- 53.Legge SD, Koch G, Diomedi M, Stanzione P, Sallustio F. Stroke Prevention: Managing Modifiable Risk Factors. Stroke Research and Treatment. 2012 doi: 10.1155/2012/391538. Article ID 391538, 15 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Christeasen LM, Krieger DW, Hajberg S, Pendersen OD, Karlsen FM, Jacobsen MD, et al. Paroxysmal atrial fibrillation occurs often in cryptogenic Ischaemic stroke. Final results from the surprise study. Euro J Neurol. 2014;21(6):884–889. doi: 10.1111/ene.12400. [DOI] [PubMed] [Google Scholar]
- 55.Marini C, De Santis F, Sacco S, Russo T, Olivieri L, Totaro R, et al. Contribution of atrial fibrillation to incidence and outcome of ischemic stroke: Results from a population based study. Stroke. 2005;36(6):1115–1119. doi: 10.1161/01.STR.0000166053.83476.49. [DOI] [PubMed] [Google Scholar]
- 56.Kamel H, Okin PM, Elkind MSV, Ladecola C. Atrial Fibrillation and Mechanism of stroke. Stroke. 2016;47(3):895–900. doi: 10.1161/STROKEAHA.115.012004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kim YH, Roh SY. The mechanism of and preventive therapy for stroke in patients with atrial fibrillation. J Stroke. 2016;18(2):129–137. doi: 10.5853/jos.2016.00234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Shavadia J, Yonga G, Mwanzi S, Jinah A, Moriasi A, Otieno H. Clinical characteristics and outcomes of atrial fibrillation and flutter at the Aga Khan University Hospital, Nairobi. Cardiovasc J Afr. 2013;24(2):6–9. doi: 10.5830/CVJA-2012-064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Stambler BS, Ngunga LM. Atrial fibrillation in sub Saharan Africa: epidemiology, unmet needs and treatment options. Int J Gen Med. 2015;31(8):231–242. doi: 10.2147/IJGM.S84537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Essa AYE, Helmy TA, El Batch SAA. Study of Incidence, Risk Factors and Outcome of Acute Cerebrovascular Stroke Patients Admitted to Alexandria Main University Hospital. J Amer Sci. 2011;7(11):316–329. [Google Scholar]
- 61.Castellano JM, Chinitz J, Willner J, Fuster V. Mechanism of stroke in artrial fibrillation. Card Electrophysiol Clin. 2014;6(1):5–15. doi: 10.1016/j.ccep.2013.10.007. [DOI] [PubMed] [Google Scholar]
- 62.Kim H, Friedlander Y, Longstreth WT, Edwards KL, Schwartz SM, Siscovick DS. Family history as a risk factor for stroke in young women. Am J Prevent Med. 2004;27(5):391–396. doi: 10.1016/j.amepre.2004.08.008. [DOI] [PubMed] [Google Scholar]
- 63.Halim A, Ottman R, Logroscino G. Familial aggregation of ischemic stroke in the Northern Manhattan Stroke Study. Neurology. 1997;48:161. [Google Scholar]
- 64.Thijs V, Grittner U, Dichgans M, Enzinger C, Fazekas F, Giese A, et al. Family History in young patients with stroke. Stroke. 2015;46(7):1975–1978. doi: 10.1161/STROKEAHA.115.009341. [DOI] [PubMed] [Google Scholar]
- 65.Mohan KM, Wolfe CD, Rudd AG, Heuschmann PU, Kolominsky-Rabas PL, Grieve AP. Risk and cumulative risk of stroke reoccurrence: a systematic review and meta-analysis. Stroke. 2011;42(5):1489–1494. doi: 10.1161/SPROKEAHA.110.602615. [DOI] [PubMed] [Google Scholar]
- 66.Wang X, Donnell MJ, Chin SL, Xavier D, Liu L, Zhang H, et al. Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countires (INTERSTROKE) a case control study. The lancet. 2016;388(10046):761–775. doi: 10.1016/S0140-6736(16)30506-2. [DOI] [PubMed] [Google Scholar]
- 67.Nigo M, Walker A, Lucido D, Shah A, Skliut M, Mildvan D. Stroke in human immunodeficiency virus (HIV) infected patients; Presented as part of the International AIDS conference; July 22–27 2012; Washington DC. [Google Scholar]
- 68.Benjamin LA, Bryer A, Emsley HCA, Khoo S, Solomon T. HIV infection and stroke: current perpectives and future directions. Lancet Neurol. 2012;11(10):878–890. doi: 10.1016/S1474-4422(12)70205-3. [DOI] [PMC free article] [PubMed] [Google Scholar]