Abstract
Background:
Adversity may negatively impact young children’s sleep but receiving home-visitation services could buffer children from this potential consequence of adversity.
Objective:
This study examined whether young children’s adverse experiences increased their risk for sleep problems and if Promoting First Relationships® (PFR), a home-visitation program, reduced children’s risk for sleep problems both directly and indirectly through increased parenting sensitivity.
Participants and Setting:
Participants were 247 parents and their 10- to 24-month-old child recruited from Child Protective Services offices.
Methods:
A secondary analysis of a randomized controlled trial comparing PFR to a resource and referral control condition was conducted. Four time points of data were collected from baseline to 6 months post-intervention. Parenting sensitivity was measured at all time points using a parent-child interaction tool. Children’s adversities were measured at various time points using caregiver report tools and official state records. Children’s sleep problems were reported by parents at 6 months post-intervention.
Results:
The likelihood of having a sleep problem increased as children’s adversities increased (β = .23, SE = .08, p = .005). There was no effect (direct or indirect) of treatment assignment on children’s sleep problems (ps > .05). Post hoc analyses showed a treatment assignment by adversity interaction such that children’s odds of having a sleep problem increased as their adversities increased, but only among children in the control condition (b = −0.37, SE = 0.17, p = .030).
Conclusions:
Experiencing more adversities associated with a greater risk for sleep problems, but PFR buffered children from this risk.
Keywords: Sleep problems, young children, home visiting, child protective services, adversity, parental sensitivity
Adverse childhood experiences (ACEs), including childhood maltreatment and household dysfunction (Felitti et al., 1998), have been linked to poorer lifelong physical and mental health outcomes including increased risk for cancer (Holman et al., 2016), ischemic heart disease (Dong et al., 2004), depression (Chapman et al., 2004), hospitalization with autoimmune disease (Dube et al., 2009), behavior problems (Freeman, 2014; Jimenez, Wade, Lin, Morrow, & Reichman, 2016), and comorbidities (Anda et al., 2006). Some consequences of ACEs, such as coronary heart disease, have decades-long “incubation” periods such that symptoms do not emerge until adulthood (Moffitt & the Klaus-Grawe 2012 Think Tank, 2013, p. 1630) whereas other consequences, such as behavior problems (e.g., internalizing behavior, externalizing behavior, and/or social problems), appear early on in childhood (Freeman, 2014; Jimenez et al., 2016).
Sleep problems including difficulties settling into sleep, frequent and/or prolonged nighttime awakenings, and/or obtaining suboptimal amounts of sleep may be among the early consequences of ACEs. ACEs are highly stressful experiences that, without sensitive caregiving to help children regulate their biologic response to stress, can give rise to a “strong, frequent, and/or prolonged” stress response called toxic stress (Shonkoff, Boyce, & McEwen, 2009, p. 2256). Being in a physiologic state of arousal, or having difficulty regulating arousal, however, can negatively impact children’s sleep (Dahl, 1996). In young children, low resting respiratory sinus arrhythmia, an indicator of parasympathetic nervous system activity, is associated with poor sleep quality (Elmore-Staton, El-Sheikh, Vaughn, & Arsiwalla, 2012). Cortisol activity is also associated with sleep fragmentation (Scher, Hall, Zaidman-Zait, & Weinberg, 2010) and difficulty settling into sleep (Ward, Gay, Alkon, Anders, & Lee, 2008). ACEs may play an important role in triggering or exacerbating sleep problems early on in life. Yet historically, studies examining ACEs as risk factors for sleep problems have tended to focus on adolescents and adults (Chapman et al., 2013; Chapman et al., 2011; Koskenvuo, Hublin, Partinen, Paunio, & Koskenvuo, 2010; Wang, Raffeld, Slopen, Hale, & Dunn, 2016). Less is known about young children.
Should it be the case that experiencing adversity increases risk for early childhood sleep problems, then sensitive parenting that helps regulate young children’s response to stress could be an integral component in addressing these sleep problems. Young children develop self-regulation skills in the context of relationship with their primary caregivers (Shonkoff & Phillips, 2000), and sensitive parenting scaffolds the development of children’s stress regulation (Feldman, 2012). Sensitive caregiving also regulates young children’s sleep-wake organization (Sadeh, Tikotzky, & Scher, 2010). Young children fall and stay asleep more easily when they experience more sensitive care (Teti, Kim, Mayer, & Countermine, 2010). Programs that support young children’s primary relationships and that target parenting sensitivity may, therefore, have the capacity to prevent and/or reduce early childhood sleep problems among young children experiencing adversity.
Promoting First Relationships® (PFR) is one such program (Kelly, Sandoval, Zuckerman, & Buehlman, 2003, 2008; Kelly, Zuckerman, Sandoval, & Buehlman, 2016). PFR is a home-visiting, attachment-based intervention that supports children’s primary relationships with their caregivers (Kelly, Zuckerman, & Rosenblatt, 2008) and has demonstrated effectiveness for improving parenting sensitivity (Oxford, Spieker, Lohr, & Fleming, 2016; Spieker, Oxford, Kelly, Nelson, & Fleming, 2012). PFR has also been associated with reduced sleep problems among infants and toddlers in Child Welfare (Oxford, Fleming, Nelson, Kelly, & Spieker, 2013; Spieker et al., 2012). Just how this program may be effective at reducing sleep problems among at-risk young children, however, is not fully understood. Oxford and colleagues (2013) have shown that, in a sample of maltreated infants and toddlers recently reunified with their birth parents, a positive effect of PFR on children’s sleep problems was mediated by a decrease in children’s separation distress. Yet, if experiencing adversity plays a role in the development of young children’s sleep problems, then having a sensitive and responsive relationship with an adult, which is a powerful regulator of young children’s stress biology (Gunnar, 2006), could be another pathway by which PFR operates to reduce children’s sleep problems. PFR has shown promise for regulating children’s stress biology including normalizing children’s cortisol secretion patterns (Nelson & Spieker, 2013) and parasympathetic nervous system activity (Hastings et al., 2018). It may be that increased parenting sensitivity, as a regulator of children’s stress, is an “active ingredient” by which PFR reduces children’s sleep problems. Investigating how parenting sensitivity relates to children’s sleep problems in contexts of adversity can expand the science about how having a sensitive caregiving relationship during the early years of life is critical to development (Shonkoff & Phillips, 2000).
The Present Study
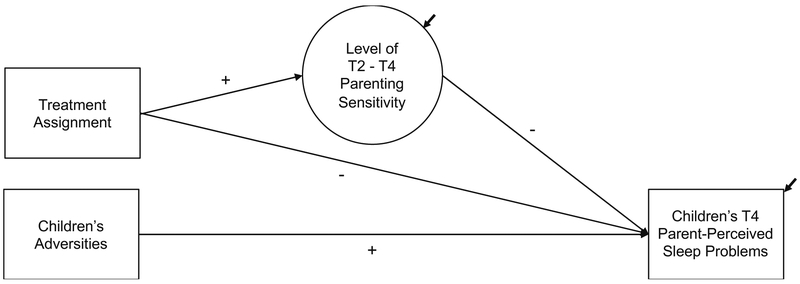
This study addresses the above gaps in knowledge by conducting a secondary analysis of data from a longitudinal, randomized controlled trial testing PFR among families with a Child Protective Services (CPS) maltreatment report. Specifically, this study tested a model (see Figure 1) in which it was hypothesized that experiencing more adversities would associate with a greater risk for having a parent-perceived sleep problem among infants and toddlers from these families. This model also hypothesized that the PFR intervention would decrease children’s risk for having a parent-perceived sleep problem and would do so, in part, by increasing parenting sensitivity.
Figure 1.
Hypothesized model. Illustrated is the hypothesized model for this secondary analysis of a longitudinal randomized controlled trial comparing the Promoting First Relationships® (PFR) intervention to a resource and referral (R&R) control condition. The + and − signs indicate directions of hypothesized relations. Children’s adversities are hypothesized to predict their odds of having a parent-perceived sleep problem at 6 months post-intervention, with more adversities predicting higher odds of having a parent-perceived sleep problem. A latent variable representing the average level of post-intervention parenting sensitivity, as aggregated across three post-intervention time points, is also hypothesized to predict children’s parent-perceived sleep problems at 6 months post-intervention, with higher parenting sensitivity predicting reduced odds of children having a parent-perceived sleep problem. Treatment assignment to the PFR condition is hypothesized to reduce children’s odds of having a parent-perceived sleep problem at 6 months post-intervention, both directly and indirectly by way of increased parenting sensitivity. Not shown for simplicity are control variables (baseline child age, baseline parenting sensitivity, time elapsed between T1 and T2) and observed T2 - T4 post-intervention parenting sensitivity measures. T1 = baseline, T2 = immediately post-intervention, T3 = 3 months post-intervention, T4 = 6 months post-intervention.
Methods
Design and Participants
This was a secondary analysis of a longitudinal, randomized controlled trial that has already shown PFR to be effective at improving parenting sensitivity (Oxford et al., 2016). Participants included 247 biological parent-child dyads (child age 10 to 24 months at baseline) from families with a recent, open case of child maltreatment reported to one of five Washington State CPS offices at least 2 weeks prior to study recruitment. Eligible parents had a 10- to 24-month-old child, spoke English, and resided in one of three Washington State counties. To be eligible for the study, children did not have to be the alleged victim of the maltreatment case. However, in a majority of dyads (87%), the child enrolled in the study was the reported victim. The remaining 13% were siblings of the reported victim.
After parents provided informed written consent and the researchers collected baseline measures, dyads were randomized to treatment condition (n = 123 resource and referral control condition, n = 124 PFR treatment condition) using a blocking method that equated groups on race and ethnicity. Table 1 gives baseline demographics by treatment assignment. Ethics approval was obtained and overseen by the Washington State Institutional Review Board.
Table 1.
Parent-Reported Baseline Demographics by Treatment Assignment
| Demographic characteristic |
Promoting First
Relationships n = 124 |
Resource & Referral n = 123 |
|---|---|---|
| M (SD) or n (%) | M (SD) or n (%) | |
| Child characteristics | ||
| Age, months | 15.98 (4.37) | 16.78 (4.55) |
| Gender, female | 62 (50) | 52 (42.3) |
| Race | ||
| American Indian or Alaska Native | 0 (0) | 2 (1.6) |
| Asian | 4 (3.2) | 0 (0) |
| Black or African American | 6 (4.8) | 5 (4.1) |
| White/Caucasian | 79 (63.7) | 69 (56.1) |
| Multiracial | 34 (27.4) | 44 (35.8) |
| Other | 1 (0.8) | 3 (2.4) |
| Parent characteristics | ||
| Age, years | 26.41 (5.19) | 27.04 (6.25) |
| Gender, female | 112 (90.3) | 112 (91.1) |
| Race | ||
| American Indian or Alaska Native | 4 (3.2) | 3 (2.4) |
| Asian | 6 (4.8) | 3 (2.4) |
| Black or African American | 6 (4.8) | 6 (4.9) |
| Native Hawaiian or other Pacific Islander | 1 (0.8) | 0 (0) |
| White/Caucasian | 95 (76.6) | 93 (75.6) |
| Multiracial | 11 (8.9) | 15 (12.2) |
| Other | 1 (0.8) | 3 (2.4) |
| Highest grade of school completed | ||
| Some or all of middle school | 7 (5.6) | 4 (3.2) |
| Some or all of high school | 73 (58.9) | 71 (57.7) |
| 1 or 2 years of college, trade, or technical school | 33 (26.6) | 40 (32.5) |
| 3 or 4 years of college | 9 (7.2) | 6 (4.9) |
| Post-college | 2 (1.6) | 2 (1.6) |
| Obtained high school diploma or GED | 94 (75.8) | 93 (75.6) |
| Marital status | ||
| Never married | 72 (58.1) | 67 (54.5) |
| Married | 26 (21.0) | 34 (27.6) |
| Divorced or separated | 26 (21.0) | 22 (17.9) |
| Employment Status | ||
| Employed full- or part-time | 41 (33.1) | 35 (28.5) |
| Unemployed/looking | 37 (29.8) | 33 (26.8) |
| Other (student, homemaker, disabled/retired) | 46 (37.1) | 55 (44.7) |
| Median | Median | |
| Past year household income, US dollars | 13792.00 | 15972.00 |
Treatment Assignment Conditions
PFR.
PFR is a manualized, relationship-based parenting intervention that seeks to promote parents’ awareness of their own and their child’s inner needs and feelings (Kelly et al., 2003, 2008; Kelly et al., 2016). PFR as used in this study is described in detail elsewhere (Oxford et al., 2016). Briefly, parents received 10 in-home visiting sessions (each approximately 1 week apart) from one of two PFR-trained and certified community-based providers. During sessions, providers used video-based feedback to guide parents in reflective observation of their child, as well as in reflection of their own and their child’s inner needs and feelings. The 8th session delivered to every dyad was videotaped and submitted to a master PFR trainer for fidelity monitoring (see Oxford and colleagues, 2018, for additional details about fidelity). Eighty-six percent of dyads received the full 10-session dose.
Resource & Referral.
A resource and referral (R&R) service was provided to participants randomized to the control condition. R&R consisted of three telephone call sessions with a social service provider who identified and provided resources for each family’s unique needs. Parents also received a mailed packet with information about local services and resources (e.g., libraries, public internet access, child care, housing, food, employment, mental health services, etc.). Eighty-nine percent of dyads received the full 3-session dose.
Data Collection Procedures
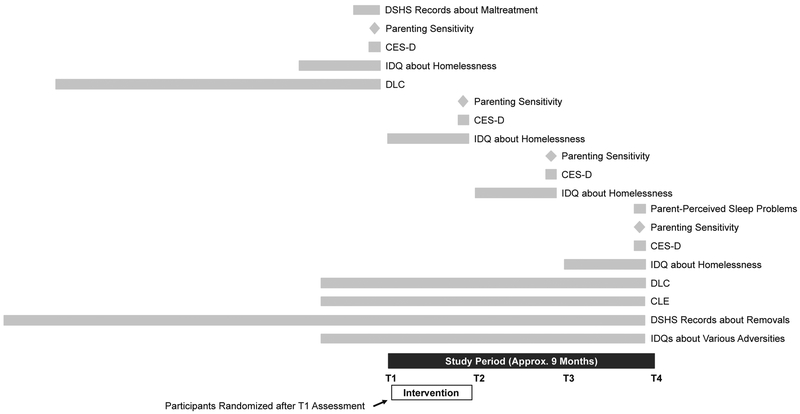
Figure 2 shows the study timeline. Trained research visitors masked to treatment assignment conducted four in-home research visits to assess dyads on the study measures at baseline (T1), immediately post-intervention (T2), 3 months post-intervention (T3), and 6 months post-intervention (T4). Visits included caregiver interviews and questionnaires, as well as observed videotaped parent-child interaction activities. Official Department of Social and Health Services (DSHS) data were also extracted prior to the close of the study to obtain children’s lifetime birth home removal histories (from birth to 6 months post-intervention). Of the 247 dyads initially enrolled in the study, 225 completed the T2 assessment (n = 116 PFR, n = 109 R&R), 215 completed the T3 assessment (n = 110 PFR, n = 105 R&R), and 211 completed the T4 assessment (n = 109 PFR, n = 102 R&R).
Figure 2.
Study timeline. Dark gray bar indicates the study period. Measures were collected at four time points (T1 = baseline, T2 = immediately post-intervention, T3 = 3 months post-intervention, T4 = 6 months post-intervention). Aligned above each time point are the measures used at that time point. Light gray bars indicate measures that covered a retrospective period, with the length of the bar roughly corresponding to the length of the retrospective period covered. Light gray diamonds indicate the measure was not retrospective but was collected at the time of the research visit. The white bar indicates the intervention period. DSHS = Department of Social and Health Services. CES-D = Center for Epidemiologic Studies Depression Scale. IDQ = investigator-developed question. DLC = Difficult Life Circumstances questionnaire. CLE = Child Life Events questionnaire.
In 14 cases, children were placed with a new non-birth parent caregiver during the study, and this new caregiver enrolled and provided data with the study child. In order to gain the most accurate count of children’s adversities based on all possible data provided by all enrolled caregivers, non-birth parent reports about children’s adversities were combined with birth parent reports. However, only data provided by birth parents were used on all remaining measures, including parenting sensitivity and children’s parent-perceived sleep problems.
Measures
Children’s adversities.
Children’s adversities were measured in a manner similar to that of the Felitti and colleagues (1998) ACEs score, which is a total count of children’s adverse event exposures. We counted nine types of adversities including potential maltreatment, removal from birth home, caregiver mental illness, caregiver incarceration, domestic violence, household substance use or abuse, caregiver divorce or separation, death of a family member or loved one, and homelessness. Because this was a secondary data analysis, and childhood adversities were not an initial focus of the study, children’s adversities were measured using several instruments. These instruments included official DSHS records, select items from the Child Life Events (CLE) questionnaire (Mongillo, Briggs-Gowan, Ford, & Carter, 2009), the Center for Epidemiologic Studies Depression Scale (CES-D) total score (Radloff, 1977), select items from the Difficult Life Circumstances (DLC) 2nd edition questionnaire (Oxford, Fleming, & Barnard, 2015), and investigator-developed questions. Table 2 describes these tools in greater detail, when they were administered, and how they were used to count children’s adversity exposures. We then summed the total number of types of adversities that children were exposed to, which yielded a total score ranging from 1 - 9 types of adversities.
Table 2.
Measurement of Children’s Adversities
| Adversity type | Assessment tool(s) | Time point |
Criteria for counting adversity exposure | |||
|---|---|---|---|---|---|---|
| T1 | T2 | T3 | T4 | |||
| Potential maltreatment | Official DSHS records | X | Exposure was counted if records indicated that a child in the family had a recent, open case of maltreatment recorded at least 2 weeks prior to recruitment (all children in this study met this criterion) | |||
| Removal from birth home | Official DSHS records | X | Exposure was counted if DSHS records indicated that the child experienced at least one birth home removal between birth and T4, or if the caregiver indicated yes on the item about foster care | |||
| One investigator-developed item asking caregivers if their child had experienced foster care within the past year (response options = yes v. no) | X | |||||
| Caregiver mental illness | The CES-D total score indicating caregivers' depressive symptoms over the past week | X | X | X | X | Exposure was counted if, at one or more time points, the caregiver scored at or above a total score cut-off of 16 points |
| Caregiver incarceration | One item from the DLC asking caregivers if they had been in prison or jail within the past year (response options = yes v. no) | X | X | Exposure was counted if the caregiver responded yes at one or both time pointsa | ||
| Domestic violence | One item from the DLC asking caregivers if they had been physically abused by their partner within the past year (response options = yes v. no) | X | X | Exposure was counted if the caregiver responded yes on one or more items at one or both time points | ||
| One item from the CLE asking caregivers if their child had witnessed someone from their family get hurt or threatened with a weapon within the past year (response options = yes v. no) | X | |||||
| One item from the CLE asking caregivers if their child had witnessed someone from their family get hit, kicked, or pushed within the past year (response options = yes v. no) | X | |||||
| Household substance use or abuse | One item from the DLC asking caregivers if they had experienced a drug or alcohol problem within the past year (response options = yes v. no) | X | X | Exposure was counted if the caregiver responded yes on one or both items at one or both time points | ||
| One item from the DLC asking caregivers if their partner had experienced a drug or alcohol problem within the past year (response options = yes v. no) | X | X | ||||
| Caregiver divorce or separation | One item from the DLC asking caregivers if they had experienced divorce or separation within the past year (response options = yes v. no) | X | X | Exposure was counted if the caregiver responded yes on one or both items at one or both time points | ||
| One investigator-developed item asking caregivers if their child had experienced parental divorce or separation within the past year (response options = yes v. no) | X | |||||
| Death of a family member or loved one | One item from the DLC asking caregivers if an immediate family member had died within the past year (response options = yes v. no) | X | X | Exposure was counted if the caregiver responded yes on one or both items at one or both time points | ||
| One investigator-developed item asking caregivers if their child had experienced the death of a loved one within the past year (response options = yes v. no) | X | |||||
| Homelessness | One investigator-developed item asking caregivers if they had received transitional housing for homelessness services within the past 3 months (response options = yes v. no) | X | X | X | X | Exposure was counted if the caregiver responded yes on one or both items at one or more time points |
| One investigator-developed item asking caregivers if their child had experienced homelessness within the past year (response options = yes v. no) | X | |||||
Note. Time point = time point at which the assessment tool was administered. T1 = baseline, T2 = immediately post-intervention, T3 = 3 months post-intervention, T4 = 6 months post-intervention. DSHS = Department of Health and Human Services. The Center for Epidemiologic Studies Depression (CES-D) scale and 16-point total score cut-off is from Radloff (1997). The Difficult Life Circumstances (DLC) questionnaire is from Oxford and colleagues (2015). The Child Life Events (CLE) questionnaire is from Mongillo and colleagues (2009). All assessment tools, except for the DSHS records, were caregiver report.
n = 47 cases had missing data about caregiver incarceration, as this item was not added to the DLC until later in this study. These cases with missing data were assumed to have no exposure to caregiver incarceration.
Parenting sensitivity.
At each time point, parent-child interactions were videotaped during a teaching activity using the Nursing Child Assessment Teaching Scale (NCATS), a 73-item observational tool that includes four parent subscales (sensitivity to child cues, response to child distress, social-emotional growth fostering, cognitive growth fostering), two child subscales (clarity of cues and responsiveness to parent) and a total score (sum of the subscale scores; Barnard, 1994; Oxford & Findlay, 2013). A total score including 56 of the original 73 items was used in this study (17 items exhibiting low variability were not scored). Higher scores (range 0 - 56) indicate more parenting sensitivity. Items were scored by a single trained observer masked to treatment assignment. The trained observed completed regular reliability checks with a master coder throughout the study. Cronbach’s alphas were α = .61 - .69. in this study.
Children’s parent-perceived sleep problems.
One item from the Sadeh (2004) Brief Infant Sleep Questionnaire (BISQ) asking parents “Do you consider your child’s sleep as a problem?” (p. e576) was used to measure parents’ perceptions about their child’s sleep problems. Parents were asked to think about the past 2 weeks when responding to this question. Response options included 0 = not a problem at all, 1 = a small problem, and 2 = a very serious problem.
Validity and reliability of the BISQ have been established (Sadeh, 2004). Prior studies have shown that this single item eliciting parents’ concerns about their child having a sleep problem is significantly associated with indicators of common infant and toddler sleep problems including frequent nighttime awakenings and prolonged sleep onset (Sadeh, 2004; Sadeh, Mindell, Luedtke, & Wiegand, 2009).
The proportion of parents in this study reporting concern for a very serious problem was small (n = 4 in the R&R group and n = 3 in the PFR group). For the purposes of this secondary analysis, therefore, we collapsed responses into two groups (0 = not a problem v. 1 = a small or very serious problem).
Covariates.
Covariates included baseline child age, baseline parenting sensitivity, and time elapsed between T1 and T2. Baseline child age was included as a covariate to adjust for developmental changes in sleep (Galland, Taylor, Elder, & Herbison, 2012; Iglowstein, Jenni, Molinari, & Largo, 2003). Baseline parenting sensitivity and time elapsed between T1 and T2 were included as covariates to adjust for differences between the treatment groups (see Oxford and colleagues, 2016, who report that parents in the PFR group scored lower on baseline parenting sensitivity and took longer to schedule their first intervention session, compared to parents in the R&R group).
Data Analytic Strategy
First, preliminary analyses including descriptives and correlations among study variables (children’s T4 parent-perceived sleep problems, T1 - T4 parenting sensitivity, children’s adversities, treatment assignment, and covariates) were examined using IBM SPSS Version 19. Next, the hypothesized path model shown in Figure 1 was tested using Mplus Version 7.31 (Muthén & Muthén, 1998-2015). To allow for inclusion of all 247 cases, including those with missing data (percentage of missing data ranged from 0 - 20.49%), we treated missing data using multiple imputation. This approach makes the assumption that data are missing at random after taking into account the variables in the imputation model (Graham, 2012). We included all study variables (children’s T4 parent-perceived sleep problems, T1 - T4 parenting sensitivity, children’s adversities, treatment assignment, and covariates) in the imputation model. All continuous variables were left in their original units, and all categorical variables were dummy coded (0 = R&R, 1 = PFR for treatment assignment; 0 = not a problem, 1 = a small or very serious problem for children’s T4 parent-perceived sleep problems). Also included were a treatment assignment by children’s adversities interaction term (forpost hoc analyses, described in greater detail below) and auxiliary demographic variables (all dichotomized). All categorical variables were specified as categorical in the imputation model. Forty data sets were imputed. These 40 data sets were then used to test the hypothesized path model given in Figure 1. The latent parenting sensitivity variable was defined using the technique described by Oxford and colleagues (2016) in which the raw T2 - T4 parenting sensitivity scores were aggregated to represent mean level of post-intervention parenting sensitivity. Covariates (baseline child age, baseline parenting sensitivity, and time between T1 and T2) were also entered into the model, to control for these factors. Maximum likelihood (ML) estimation with the logit link function was used to obtain parameter estimates, which performed linear regression on paths predicting the continuous endogenous variable (the latent parenting sensitivity variable) and logistic regression on paths predicting the categorical endogenous variable (children’s T4 parent-perceived sleep problems; Muthén & Muthén, 1998-2015b). Averaged parameter estimates and standard errors were obtained across the 40 data sets according to Rubin’s (1987) rules. For model fit statistics, we report the chi-square test statistic of the exact-fit hypothesis, the Root Mean Squared Error of Approximation (RMSEA), the Comparative Fit Index (CFI), the Tucker-Lewis Index (TLI), and the Standardized Root Mean Residual (SRMR; Kline, 2016).
Results
Descriptives and Correlations
Table 3 shows descriptives for children’s adversities by treatment assignment. Aside from potential maltreatment (which was 100% of the sample), caregiver mental illness was the most frequently reported adversity (57.3% PFR, 55.3% R&R), followed by caregiver divorce or separation (39.5% PFR, 41.5% R&R). Caregiver incarceration was the least frequently reported (8.8% PFR, 7.1% R&R). Over half of the sample reported three or more types of adversities (58.9% PFR, 60.2% R&R). There was no association between children’s adversities and treatment assignment (all ps > .05). Mean number of adversities also did not differ by treatment assignment (p > .05).
Table 3.
Descriptives for Children’s Adversities by Treatment Assignment
| Variable |
PFR n = 124 |
R&R n = 123 |
χ2(df) | P |
|---|---|---|---|---|
| n (%) | n (%) | |||
| Type of adversity | ||||
| Potential maltreatment | 124 (100.0) | 123 (100.0) | ||
| Removal from birth home | 12 (9.7) | 18 (14.6) | 1.42(1) | .23 |
| Caregiver mental illness | 71 (57.3) | 68 (55.3) | 0.10(1) | .76 |
| Caregiver incarcerationa | 9 (8.8) | 7(7.1) | 0.19(1) | .66 |
| Domestic violence | 31 (25.0) | 36 (29.3) | 0.57(1) | .45 |
| Household substance use or abuse | 21 (16.9) | 20 (16.3) | 0.02(1) | .89 |
| Caregiver divorce or separation | 49 (39.5) | 51 (41.5) | 0.10(1) | .76 |
| Death of a family member or loved one | 29 (23.4) | 29 (23.6) | 0.001(1) | .97 |
| Homelessness | 27 (21.8) | 31 (25.2) | 0.40(1) | .53 |
| Total number of adversities | ||||
| 1 | 23 (18.5) | 18 (14.6) | 0.68(1) | .41 |
| 2 | 28 (22.6) | 31 (25.2) | 0.23(1) | .63 |
| 3 | 29 (23.4) | 31 (25.2) | 0.11(1) | .74 |
| 4 | 23 (18.5) | 15 (12.2) | 1.92(1) | .17 |
| 5 | 12 (9.7) | 20 (16.3) | 2.37(1) | .12 |
| 6 or more | 9 (7.3) | 8 (6.5) | 0.06(1) | .82 |
| M (SD) | M (SD) | t(df) | ||
| Average number of adversities | 3.01 (1.51) | 3.11 (1.52) | 0.55(245) | .58 |
Note. PFR = Promoting First Relationships®, R&R = Resource and Referral.
n= 102 and n = 98 in the PFR and R&R groups, respectively, as this item was not added until later in the study. Cases with missing data on this item were assumed to have been unexposed to caregiver incarceration.
Table 4 shows descriptives by treatment assignment for T1 - T4 parenting sensitivity and children’s T4 parent-perceived sleep problems. T1 parenting sensitivity was lower in the PFR than the R&R group (t = 2.01, df= 244, p = .046; as expected based on Oxford and colleagues, 2016). The proportion of children with a T4 parent-perceived sleep problem was 20.2% in the PFR group and 26.5% in the R&R group.
Table 4.
Descriptives for Parenting Sensitivity and Children's Parent-Perceived Sleep Problems by Treatment Assignment
| T1 |
T2 |
T3 |
T4 |
|||||
|---|---|---|---|---|---|---|---|---|
| Variable |
PFR n = 124 |
R&R n = 122 |
PFR n = 114 |
R&R n = 108 |
PFR n = 109 |
R&R n = 104 |
PFR n = 109 |
R&R n = 102 |
| Parenting sensitivity, M (SD) | 35.44 (4.27) |
36.60 (4.75) |
35.65 (4.86) |
35.07 (5.03) |
36.46 (4.85) |
36.04 (4.83) |
36.90 (4.60) |
35.82 (5.46) |
| Children's parent-perceived sleep problems, n (%) | 22 (20.2) |
27 (26.5) |
||||||
Note. PFR = Promoting First Relationships®, R&R = Resource and Referral. T1 = baseline, T2 = immediately post-intervention, T3 = 3 months post-intervention, T4 = 6 months post-intervention. The T1 to T3 n's indicate cases without missing data on the parenting sensitivity variable. The T4 n's indicate cases without missing data on the parent-perceived sleep problems variable. The number of cases without missing data on the T4 parenting sensitivity variable were n = 107 PFR and n = 98 R&R. Parenting sensitivity = Nursing Child Assessment Teaching Scale raw total score, higher scores indicate more parenting sensitivity. Children's parent-perceived sleep problems indicate the proportion of parents reporting concern for a small or very serious sleep problem.
Table 5 shows correlations for children’s T4 parent-perceived sleep problems, T1 - T4 parenting sensitivity, children’s adversities, treatment assignment, and the covariates. Correlations between children’s T4 parent-perceived sleep problems and parenting sensitivity (all time points of parenting sensitivity) were negative and non-significant. The correlation between children’s T4 parent-perceived sleep problems and children’s adversities was positive and significant, indicating that having a T4 parent-perceived sleep problem became more likely as children’s adversities increased. The correlation between children’s T4 parent-perceived sleep problems and treatment assignment was negative and non-significant.
Table 5.
Zero-Order Correlations Among Study Variables
| Variable | 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. |
|---|---|---|---|---|---|---|---|---|---|
| 1. Children’s T4 parent-perceived sleep problems | -- | ||||||||
| 2. T1 parenting sensitivity | −.02 | -- | |||||||
| 3. T2 parenting sensitivity | −.02 | .23** | -- | ||||||
| 4. T3 parenting sensitivity | −.02 | .20** | .25 ** | -- | |||||
| 5. T4 parenting sensitivity | −.04 | .30** | .14 * | .25 ** | -- | ||||
| 6. Children’s adversities | .18 ** | −.05 | .06 | .06 | −.06 | -- | |||
| 7. Treatment assignment | −.07 | −.13* | .06 | .04 | .11 | −.04 | -- | ||
| 8. T1 child age | <.01 | .18** | .11 | .21 ** | .15 * | .03 | −.09 | -- | |
| 9. Time elapsed | .01 | .04 | .15 * | .05 | .03 | .11 | .17 * | .03 | -- |
Note. N= 247 at baseline. T1 = baseline, T2 = immediately post-intervention, T3 = 3 months post-intervention, T4 = 6 months post-intervention. Children’s parent-perceived sleep problems dummy coded 0 = no problem, 1 = small or very serious problem. Parenting sensitivity = Nursing Child Assessment Teaching Scale raw total score, higher scores indicate more parenting sensitivity. Children’s adversities = total count of children’s adverse event exposures, higher scores indicate more adversities. Treatment assignment dummy coded 0 = Resource & Referral, 1 = Promoting First Relationships®. Child age = months. Time elapsed = time elapsed between T1 and T2, months.
p < .05
p < .01.
Results for the Hypothesized Path Model
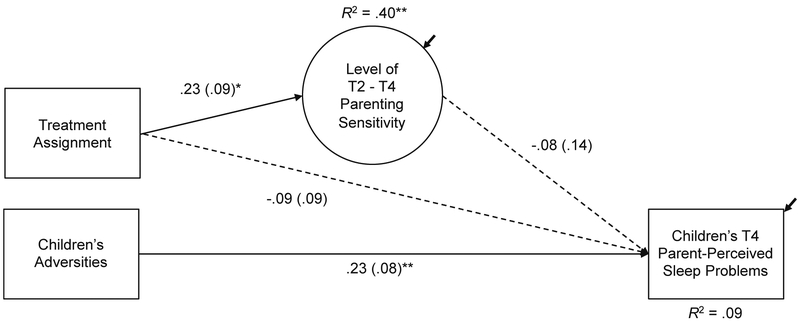
Results for the hypothesized path model are given in Figure 3. Children’s adversities positively predicted T4 parent-perceived sleep problems, indicating that, as children’s adversities increased, the odds of having a parent-perceived sleep problem at 6 months post-intervention also increased. Treatment assignment significantly predicted mean level of post-intervention parenting sensitivity, with parents in the PFR group having higher mean post-intervention parenting sensitivity scores compared to parents in the R&R group (as expected based on Oxford and colleagues, 2016). Treatment assignment failed to predict children’s T4 parent-perceived sleep problems, both directly and indirectly through post-intervention parenting sensitivity.
Figure 3.
Results for the hypothesized model. N = 247. Solid lines indicate significant paths. Dashed lines indicate non-significant paths. Reported are standardized path coefficients and, in parentheses, standard errors. Children’s adversities = total count of children’s adverse event exposures, higher scores indicate more adversities. Level of T2 - T4 parenting sensitivity is a latent variable representing the mean level of parenting sensitivity across all post-intervention time points, higher levels indicate more parenting sensitivity. Children’s parent-perceived sleep problems dummy coded 0 = no problem, 1 = small or very serious problem. Treatment assignment dummy coded 0 = Resource & Referral, 1 = Promoting First Relationships®. Not shown for simplicity are covariates (T1 child age, T1 parenting sensitivity, and time between T1 and T2) and observed T2 - T4 parenting sensitivity measures. T1 = baseline, T2 = immediately post-intervention, T3 = 3 months post-intervention, T4 = 6 months post-intervention.
* p < .05, ** p < .01.
Post Hoc Analyses
Post hoc analyses were conducted to better understand relations among PFR, children’s adversities, and children’s T4 parent-perceived sleep problems. We conducted two models in these analyses. In one model, we examined the effect of PFR alone on children’s T4 parent-perceived sleep problems. In the other model, we probed for an interaction effect between treatment assignment and children’s adversities on T4 parent-perceived sleep problems. All post hoc analyses were conducted in Mplus Version 7.31 (Muthén & Muthén, 1998-2015) using the 40 imputed data sets from the original analyses. ML estimation with the logit link function was also used in all post hoc analyses.
To examine the effect of PRF alone on children’s T4 parent-perceived sleep problems, a multiple logistic regression with standard predictor entry predicting children’s odds of having a T4 parent-perceived sleep problem was examined. We entered treatment assignment as the predictor (dummy coded 0 = R&R, 1 = PFR) and controlled for covariates (baseline child age and time between T1 and T2). Results indicated that PFR was not significantly associated with children’s T4 parent-perceived sleep problems (standardized β = −0.12, SE = 0.09, p = .188).
To probe for a potential interaction effect between treatment assignment and children’s adversities on their odds of having a T4 parent-perceived sleep problem, we conducted a multiple logistic regression with standard predictor entry, entering children’s adversities (standardized), treatment assignment (re-coded −1 = R&R, 1 = PFR), and a treatment assignment by children’s adversities interaction term as the set of predictors and controlling for covariates (baseline child age and time between T1 and T2). Results indicated the interaction was significant (raw b = −0.37, SE = 0.17, p = .030), as was the variable of children’s adversities (raw b = 0.42, SE = 0A7, p = .015), but not treatment assignment (raw b = −0.14, SE = 0.18, p = .439).
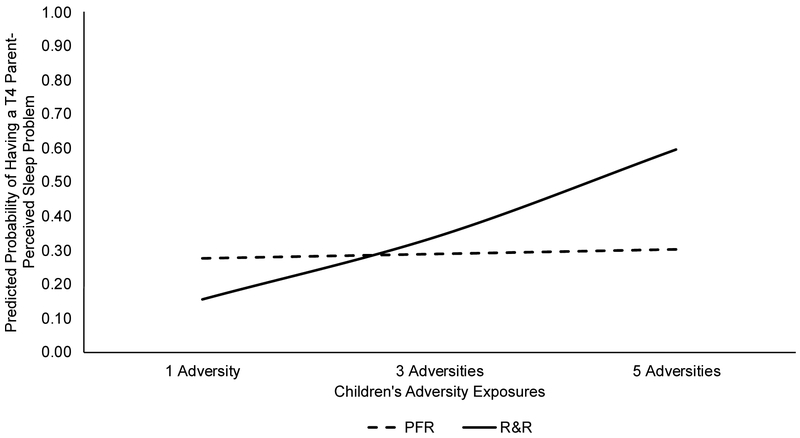
To gain a better understanding of this interaction, predicted probabilities for having a T4 parent-perceived sleep problem were calculated and graphed (see Figure 4) for children’s exposures to 1 adversity (−1.36 standard deviations away from the mean), 3 adversities (−0.04 standard deviations away from the mean), and 5 adversities (+1.29 standard deviations away from the mean) in the R&R and PFR groups, holding all else constant. As shown, the predicted probability of having a T4 parent-perceived sleep problem gradually increased as children’s adversities increased, but only for the R&R group. The predicted probability of having a T4 parent-perceived sleep problem was fairly stable as children’s adversities increased in the PFR group.
Figure 4.
Predicted probabilities of having a parent-perceived sleep problem at 6 months post-intervention for children in the R&R and PFR groups, by children's adversities. R&R = Resource and Referral, PFR = Promoting First Relationships®. T4 = 6 months post-intervention.
Discussion
Findings from this study suggest that experiencing more early life adversities confers risk for parent-perceived sleep problems among infants and toddlers from families involved with CPS for maltreatment, but this risk is mitigated when families are provided with a home-visiting, relationship-based intervention. As hypothesized, the more adverse events children experienced, the greater their risk for having a parent-perceived sleep problem. This finding is novel, as it shows that the sleep-related consequences of adversity include the earliest years of life, not just adolescence and adulthood (Chapman et al., 2013; Chapman et al., 2011; Koskenvuo et al., 2010; Wang et al., 2016). This finding also adds to the literature by showing that sleep may be among the more immediately affected domains of functioning in contexts of adversity.
Despite this risk, our findings about the interaction between treatment assignment and children’s adversities provide promising evidence to indicate that this risk can be mitigated. PFR, as a home-visiting, relationship-based intervention, appeared to buffer children in this study. Specifically, findings showed that the probability of having a parent-perceived sleep problem gradually increased as adversities increased among children in the control group, whereas the probability of having a parent-perceived sleep problem remained relatively stable among children in the PRF group. One interpretation of these findings is that children in the PFR group had fewer sleep problems as their adversities increased. PFR may have served to regulate children’s stress response systems and this, in turn, may have had the added benefit for their sleep as stress increased. This interpretation fits well with earlier findings that PFR normalizes children’s cortisol responses (Nelson & Spieker, 2013) and parasympathetic nervous system functioning (Hastings et al., 2018). Another interpretation of these findings, however, could be that parents in the PFR group became more attuned to their child’s needs and simply perceived their child’s sleep as less problematic, regardless of the number of adversities experienced. Parents in the PFR group received content about how their child’s behaviors reflected their inner social emotional needs, and this may have changed how they viewed their child’s sleep behaviors. Further research is needed to untangle these possibilities.
We failed to find evidence that PFR directly reduced children’s risk for parent-perceived sleep problems among this sample of infants and toddlers from families with a CPS maltreatment report. This finding is contrary to our hypotheses and conflicts with findings from the priormentioned study showing fewer sleep problems among infants and toddlers who received PFR (Oxford et al., 2013; Spieker et al., 2012). The population examined in this study, however, was different from the prior study, which may help to explain these discrepant findings. This study included a high-risk population of infants and toddlers (children from families with a CPS maltreatment report), but the prior study included an even higher-risk population (children with a recent caregiver change, including children recently removed from their birth home and children recently returning home to their birth parents after a foster care placement; Oxford et al., 2013; Spieker et al., 2012). It may be that PFR is effective for reducing sleep problems, but only among higher risk populations. This interpretation is supported by the buffering effect of the interaction between children’s adversities and treatment assignment, where children with most adversities evidenced the greatest benefit from PFR with regard to having a reduced risk of parent-perceived sleep problems. It is also possible that measurement differences could help explain these discrepant findings. The tool used to measure sleep problems in this study, which included one dichotomous item, was different from that used in the prior study, which included multiple items about difficulty falling asleep, difficulty staying asleep, and obtaining suboptimal amounts of sleep (Oxford et al., 2013; Spieker et al., 2012).
We also failed to find evidence that PFR indirectly reduced, by way of parenting sensitivity, children’s risk for parent-perceived sleep problems. This suggests that improved parenting sensitivity likely was not the mechanism by which PFR conferred its buffering effect. One possible explanation for these null findings is that the parenting sensitivity variable in this study, as measured by a teaching task, simply failed to capture the dimensions of the parent-child relationship most relevant to children’s sleep. It is also possible that other more potent but unaccounted-for factors were at play. In the earlier study by Oxford and colleagues (2013), for example, the effect of PFR on sleep problems among children recently reunified with their birth parents was mediated by reduced separation distress, suggesting that separation distress is potent for sleep in children experiencing changing caregivers. Further study is needed to better understand the most potent factors explaining how home-visiting, relationship-based interventions operate as a buffer for sleep behavior among infants and toddlers from families referred to CPS for maltreatment.
Strengths and Limitations
This study has some limitations. First, baseline parent-perceived sleep problems were not assessed. Although children were randomized to treatment assignment, it is not known whether the proportion of children with and without parent-perceived sleep problems was truly equal at baseline between the R&R and PFR groups. Second, all children were assigned a single, undifferentiated point for potential maltreatment. There was no variability in maltreatment type (e.g., physical neglect, physical abuse, emotional abuse). However, our results still indicate that, among this sample of children living in families with a CPS maltreatment report, each adversity, in addition to the adversity of potential maltreatment of any type, increased children’s odds of having a parent-perceived sleep problem. Third, it is possible that we underestimated the number of types of adversities that children experienced since birth. Many of our instruments did not cover children’s lifetime histories. For example, the DLC measured children’s adversities, but only over the past year. Finally, children’s sleep problems were assessed using just one general question about parents’ perceptions. We were unable to determine how parents’ views about their child’s sleep mapped on to objective measures (e.g., actigraphy). Future studies using a combination of parent-report and objective measures of children’s sleep can help address this limitation.
This study also has many strengths. First, the randomized controlled design with pre- and post-intervention measurement of parenting sensitivity added rigor to the assessment of a treatment effect on children’s parent-perceived sleep problems by way of parenting sensitivity. Second, the longitudinal nature of this study allowed for the examination of prospective relations. The longitudinal nature of this study also allowed for the measurement of children’s adversities and parenting sensitivity over time. Third, combined observational measures (parenting sensitivity), official records (DSHS reports) and parent-report tools (parent-reported adversities and sleep problems) were used, which likely minimized shared variance.
Conclusion
Findings from this study add new knowledge indicating that increasing adversity may render infants and toddlers increasingly vulnerable to sleep problems, as perceived by their parents. PFR, a home-visiting, relationship-based intervention, however, shows promise for reducing parent’s concerns about their child having a sleep problem in contexts of increasing adversity.
Acknowledgments
This work was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development of the National Institutes of Health (grant numbers R01 HD061362 and U54HD083091); the National Institutes of Health, National Institute of Nursing Research Omics and Symptom Science Training Program at the University of Washington (grant number T32NR016913); the National Institutes of Health, National Institute of Nursing Research, Center for Innovation in Sleep Self-Management (P30NR016585); and the University of Washington Warren G. Magnuson Scholarship Award. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Funders had no role in the design of this study; in the acquisition, analysis, or interpretation data; or in the preparation of this manuscript. The authors wish to thank the study participants and their families. The authors also wish to thank David Preston for providing editing assistance.
Footnotes
Declarations of interest: none.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Anda RF, Felitti VJ, Bremner JD, Walker JD, Whitfield C, Perry BD, … Giles WH (2006). The enduring effects of abuse and related adverse experiences in childhood: A convergence of evidence from neurobiology and epidemiology. European Archives of Psychiatry and Clinical Neuroscience, 256, 174–186. doi: 10.1007/s00406-005-0624-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnard KE (1994). What the Teaching Scale measures In Sumner GS & Spietz A (Eds.), NCAST: Caregiver/parent-child interaction teaching manual (pp. 98–121). Seattle, WA: NCAST, University of Washington. [Google Scholar]
- Chapman DP, Liu Y, Presley-Cantrell LR, Edwards VJ, Wheaton AG, Perry GS, & Croft JB (2013). Adverse childhood experiences and frequent insufficient sleep in 5 U.S. States, 2009: A retrospective cohort study. BMC Public Health, 13:3. doi: 10.1186/1471-2458-13-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman DP, Wheaton AG, Anda RF, Croft JB, Edwards VJ, Liu Y, … Perry GS (2011). Adverse childhood experiences and sleep disturbances in adults. Sleep Medicine, 12, 773–779. doi: 10.1016/j.sleep.2011.03.013 [DOI] [PubMed] [Google Scholar]
- Chapman DP, Whitfield CL, Felitti VJ, Dube SR, Edwards VJ, & Anda RF(2004). Adverse childhood experiences and the risk of depressive disorders in adulthood. Journal of Affective Disorders, 82, 217–225. doi: 10.1016/j.jad.2003.12.013 [DOI] [PubMed] [Google Scholar]
- Dahl RE (1996). The regulation of sleep and arousal: Development and psychopathology. Development and Psychopathology, 8, 3–27. doi: 10.1017/S0954579400006945 [DOI] [Google Scholar]
- Dong M, Giles WH, Felitti VJ, Dube SR, Williams JE, Chapman DP, & Anda RF (2004). Insights into causal pathways for ischemic heart disease: Adverse childhood experiences study. Circulation, 110, 1761–1766. doi: 10.1161/01.cir.0000143074.54995.7f [DOI] [PubMed] [Google Scholar]
- Dube SR, Fairweather D, Pearson WS, Felitti VJ, Anda RF, & Croft JB (2009). Cumulative childhood stress and autoimmune diseases in adults. Psychosomatic Medicine, 71, 243–250. doi: 10.1097/PSY.0b013e3181907888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elmore-Staton L, El-Sheikh M, Vaughn B, & Arsiwalla DD (2012). Preschoolers' daytime respiratory sinus arrhythmia and nighttime sleep. Physiology & Behavior, 107, 414–417. doi: 10.1016/j.physbeh.2012.07.005 [DOI] [PubMed] [Google Scholar]
- Feldman R (2012). Parent-infant synchrony: A biobehavioral model of mutual influences in the formation of affiliative bonds. Monographs of the Society for Research in Child Development, 77(2), 42–51. doi: 10.1111/j.1540-5834.2011.00660.x [DOI] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, …Marks JS (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) Study. American Journal of Preventative Medicine, 14, 245–258. doi: 10.1016/S0749-3797(98)00017-8 [DOI] [PubMed] [Google Scholar]
- Freeman PA (2014). Prevalence and relationship between adverse childhood experiences and child behavior among young children. Infant Mental Health Journal, 35, 544–554. doi: 10.1002/imhj.21460 [DOI] [PubMed] [Google Scholar]
- Galland BC, Taylor BJ, Elder DE, & Herbison P (2012). Normal sleep patterns in infants and children: A systematic review of observational studies. Sleep Medicine Reviews, 16, 213–222. doi: 10.1016/j.smrv.2011.06.001 [DOI] [PubMed] [Google Scholar]
- Graham J (2012). Missing data: Analysis and design. New York: Springer. [Google Scholar]
- Gunnar MR (2006). Social regulation of stress in early child development In McCartney K & Phillips DA (Eds.), Blackwell handbook of early childhood development (pp. 106–125). Malden, MA: Blackwell Publishing Ltd. [Google Scholar]
- Hastings PD, Kahle S, Fleming C, Lohr MJ, Katz LF, & Oxford ML (2018). An intervention that increases parental sensitivity in families referred to Child Protective Services also changes toddlers' parasympathetic regulation. Developmental Science, e12725. doi: 10.1111/desc.12725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holman DM, Ports KA, Buchanan ND, Hawkins NA, Merrick MT, Metzler M, & Trivers KF (2016). The association between adverse childhood experiences and risk of cancer in adulthood: A systematic review of the literature. Pediatrics, 138(Suppl 1), S81–S91. doi: 10.1542/peds.2015-4268L [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iglowstein I, Jenni OG, Molinari L, & Largo RH (2003). Sleep duration from infancy to adolescence: Reference values and generational trends. Pediatrics, 111 302–307. doi: 10.1542/peds.111.2.302 [DOI] [PubMed] [Google Scholar]
- Jimenez ME, Wade R Jr., Lin Y, Morrow LM, & Reichman NE (2016). Adverse experiences in early childhood and Kindergarten outcomes. Pediatrics, 137(2):e20151839. doi: 10.1542/peds.2015-1839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Sandoval D, Zuckerman TG, & Buehlman MA (2003). Promoting First Relationships: A program for service providers to help parents and other caregivers nurture young children's social and emotional development. Seattle, WA: NCAST Programs. [Google Scholar]
- Kelly JF, Sandoval D, Zuckerman TG, & Buehlman MA (2008). Promoting First Relationships: A program for service providers to help parents and other caregivers nurture young children's social and emotional development (2nd ed.). Seattle, WA: NCAST Programs. [Google Scholar]
- Kelly JF, Zuckerman T, & Rosenblatt S (2008). Promoting First Relationships: A relationship-focused early intervention approach. Infants & Young Children, 21, 285–295. doi: 10.1097/01.IYC.0000336541.37379.0e [DOI] [Google Scholar]
- Kelly JF, Zuckerman TG, Sandoval D, & Buehlman MA (2016). Promoting First Relationships: A program for service providers to help parents and other caregivers nurture young children's social and emotional development (3rd ed.). Seattle, WA: NCAST Programs. [Google Scholar]
- Kline RB (2016). Principles and practice of structural equation modeling (4th ed.). New York, NY: The Guilford Press. [Google Scholar]
- Koskenvuo K, Hublin C, Partinen M, Paunio T, & Koskenvuo M (2010). Childhood adversities and quality of sleep in adulthood: A population-based study of 26,000 Finns. Sleep Medicine, 11, 17–22. doi: 10.1016/j.sleep.2009.03.010 [DOI] [PubMed] [Google Scholar]
- Moffitt TE, & the Klaus-Grawe 2012 Think Tank. (2013). Childhood exposure to violence and lifelong health: Clinical intervention science and stress-biology research join forces. Development and Psychopathology, 25, 1619–1634. doi: 10.1017/s0954579413000801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mongillo EA, Briggs-Gowan M, Ford JD, & Carter AS (2009). Impact of traumatic life events in a community sample of toddlers. Journal of Abnormal Child Psychology, 37, 455–468. doi: 10.1007/s10802-008-9283-z [DOI] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (1998-2015). Mplus user's guide (7th ed.). Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Nelson EM, & Spieker SJ (2013). Intervention effects on morning and stimulated cortisol responses among toddlers in foster care. Infant Mental Health Journal, 34, 211–221. doi: 10.1002/imhj.21382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oxford M, & Findlay D (Eds.). (2013). NCAST: Caregiver/parent-child interaction teaching manual. Seattle, WA: NCAST Programs. [Google Scholar]
- Oxford M, Fleming C, & Barnard K (2015). Difficult Life Circumstances scale: A resource manual (2nd ed.). Seattle, WA: NCAST Programs. [Google Scholar]
- Oxford ML, Fleming CB, Nelson EM, Kelly JF, & Spieker SJ (2013). Randomized trial of Promoting First Relationships: Effects on maltreated toddlers' separation distress and sleep regulation after reunification. Children and Youth Services Review, 35, 1988–1992. doi: 10.1016/j.childyouth.2013.09.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oxford ML, Spieker SJ, Lohr MJ, & Fleming CB (2016). Promoting First Relationships®: Randomized trial of a 10-week home visiting program with families referred to Child Protective Services. Child Maltreatment, 21, 267–277. doi: 10.1177/1077559516668274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oxford ML, Spieker SJ, Lohr MJ, Fleming CB, Dillon C, & Rees J (2018). Ensuring implementation fidelity of a 10-week home visiting program in two randomized clinical trials. Maternal and Child Health Journal, 22, 376–383. doi: 10.1007/s10995-017-2387-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff LS (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1, 385–401. doi: 10.1177/014662167700100306 [DOI] [Google Scholar]
- Rubin DB (1987). Multiple imputation for nonresponse in surveys. New York, NY: John Wiley & Sons. [Google Scholar]
- Sadeh A (2004). A brief screening questionnaire for infant sleep problems: Validation and findings for an Internet sample. Pediatrics, 113, e570–e577. doi: 10.1542/peds.113.6.e570 [DOI] [PubMed] [Google Scholar]
- Sadeh A, Mindell JA, Luedtke K, & Wiegand B (2009). Sleep and sleep ecology in the first 3 years: A web-based study. Journal of Sleep Research, 18, 60–73. doi: 10.1111/j.1365-2869.2008.00699.x [DOI] [PubMed] [Google Scholar]
- Sadeh A, Tikotzky L, & Scher A (2010). Parenting and infant sleep. Sleep Medicine Reviews, 14, 89–96. doi: 10.1016/j.smrv.2009.05.003 [DOI] [PubMed] [Google Scholar]
- Scher A, Hall WA, Zaidman-Zait A, & Weinberg J (2010). Sleep quality, cortisol levels, and behavioral regulation in toddlers. Developmental Psychobiology, 52, 44–53. doi: 10.1002/dev.20410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shonkoff JP, Boyce WT, & McEwen BS (2009). Neuroscience, molecular biology, and the childhood roots of health disparities: Building a new framework for health promotion and disease prevention. JAMA, 301, 2252–2259. doi: 10.1001/jama.2009.754 [DOI] [PubMed] [Google Scholar]
- Shonkoff JP, & Phillips DA (Eds.). (2000). From neurons to neighborhoods: The science of early childhood development. Washington, D.C.: National Academy Press. [PubMed] [Google Scholar]
- Spieker SJ, Oxford ML, Kelly JF, Nelson EM, & Fleming CB (2012). Promoting First Relationships: Randomized trial of a relationship-based intervention for toddlers in Child Welfare. Child Maltreatment, 17, 271–286. doi: 10.1177/1077559512458176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teti DM, Kim BR, Mayer G, & Countermine M (2010). Maternal emotional availability at bedtime predicts infant sleep quality. Journal of Family Psychology, 24, 307–315. doi: 10.1037/a0019306 [DOI] [PubMed] [Google Scholar]
- Wang Y, Raffeld MR, Slopen N, Hale L, & Dunn EC (2016). Childhood adversity and insomnia in adolescence. Sleep Medicine, 21, 12–18. doi: 10.1016/j.sleep.2016.01.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward TM, Gay C, Alkon A, Anders TF, & Lee KA (2008). Nocturnal sleep and daytime nap behaviors in relation to salivary cortisol levels and temperament in preschool-age children attending child care. Biological Research for Nursing, 9, 244–253. doi: 10.1177/1099800407310158 [DOI] [PubMed] [Google Scholar]