Abstract
Evidence that anxiety disorders are associated with general medical conditions is growing. While it is known that medical and mental conditions are often comorbid, research demonstrates that there may be underlying causal mechanisms. Furthermore, comorbid anxiety and general medical conditions are associated with poorer patient outcomes than either condition alone. Comorbid general medical and mental disorders not only affect individual patient health but also strain existing medical systems. Growing health care expenditures and increasing time pressures on clinicians create a challenging environment for intensive therapy in traditional settings. Effective screening, diagnosis, and treatment of individuals with comorbid conditions require health systems that are based on interprofessional collaboration, including integrative and collaborative care services. These models encourage the provision of patient care within a network of health care professionals, working together and sharing expertise for more efficient and holistic care. Research on the design and implementation of these systems within the context of anxiety disorders and comorbid general medical conditions is in its infancy. Given the staggeringly high rates of anxiety disorders within the general population and the continued rise of many chronic medical conditions coinciding with the increasing lifespan, mental health and primary care providers should consider how they might implement integrative care methods within their own practice.
Keywords: Anxiety & anxiety disorders, Collaborative care, Integrative care, Comorbidity, Healthcare Systems, Review
Understanding mental health and how it relates to overall wellness continues to evolve. Considerable growth in research and the introduction of the biopsychosocial model in the late 1970s have changed conceptualizations of illness, indicating that disorders of the mind are intrinsically linked to diseases of the body. A significant proportion of extant literature on the topic has specifically focused on the relationships between major depressive disorders and various comorbid medical illnesses, such as cardiovascular disease, chronic obstructive pulmonary disease (COPD), and diabetes (1–3). In contrast, our understanding of how anxiety disorders relate to medical illness has notably lagged behind.
Anxiety disorders are among the most prevalent reported mental disorders. In 2014, a systematic review of anxiety epidemiology literature suggested a worldwide prevalence ranging from 3.8% to 25% (4). The wide range of estimates is likely due to a range of factors, including methodological differences in epidemiologic studies and potentially real differences between countries in the prevalence of anxiety disorders. With data from the U.S. National Comorbidity Survey, lifetime prevalence of anxiety disorders is estimated to be 16% (5).
Anxiety disorders are disproportionately prevalent among individuals with general medical conditions. For example, a 2005 U.S. population-based investigation conducted by Sareen and colleagues (6) that examined the comorbidity of anxiety disorders and general medical conditions, while controlling for common comorbid conditions such as major depression and substance use disorders, found that persons with a past-year general medical condition were nearly twice as likely to have a past-year anxiety disorder. The prevalence and degree of comorbidity of anxiety disorders vary substantially, depending on the general medical condition assessed. Data from the 2007 and 2009 Medical Expenditure Panel Survey in the United States (7) reported that, among adults (ages 22–64) with anxiety (without depression), 27.2% had comorbid arthritis. In contrast, only 2.0% of those with anxiety reported comorbid osteoporosis. Rates of comorbidity of the specified general medical conditions and anxiety (without depression) were also determined for asthma (7.2%), COPD (13.7%), diabetes (8.2%), heart disease (10.5%), and hypertension (25.5%). Although some of these differences may be attributed to the population prevalence of each condition, those with anxiety were found to have statistically higher rates of arthritis, COPD, heart disease, and hypertension than those without anxiety.
Beyond epidemiological observations, attempts to determine the causal mechanisms of how anxiety relates to general medical conditions have produced varied explanations. Most current research includes case control and longitudinal studies; however, rigorous time-series studies are lacking. In this review, we attempt to explore the current developments within this field, highlighting the progress that has been made in understanding the interplay between anxiety and general medical conditions while noting the gaps that remain in our knowledge. We examine the causal mechanisms of these complex relationships and discuss how the application of integrative and collaborative care models may be particularly relevant in our attempt to diagnose, treat, and support individuals who have comorbid conditions. Finally, we address future directions in research and treatment and identify some of the continuing challenges in modern practice.
Anxiety: Clinical Context
While the Diagnostic and Statistical Manual of Mental Disorders (5th ed.; DSM-5) organizes anxiety disorders into 12 distinct categories (including generalized and unspecified), it broadly defines anxiety disorders as “disorders that share features of excessive fear and anxiety and related behavioral disturbances” (8). It further clarifies that “fear is the emotional response to real or perceived imminent threat, whereas anxiety is anticipation of future threat.” It is important to emphasize that both fear and anxiety are not inherently pathological; indeed, both can be adaptive physiological or psychological responses (e.g., in the context of the “fight-or-flight” or acute stress response). The point at which anxiety becomes “disordered” is highly individualized and can be affected by many factors, reflecting the challenge associated with diagnosing and treating threshold cases. In a 2006 study, clinicians using common diagnostic screeners, such as the Patient Health Questionnaire (PHQ), failed to identify anxiety disorders for more than 50% of the individuals studied (9). This effect becomes more pronounced in populations with high rates of comorbid conditions, which appear to create a higher degree of false-negative results with traditional screening techniques (10). Furthermore, the recognition of anxiety disorder symptoms in a patient often does not translate into an anxiety disorder diagnosis (11). Although anxiety symptoms are often detected, there are differences in how clinically significant these symptoms are to the practitioner. Anxiety in the context of general medical conditions may further complicate diagnosis, in that health professionals may attribute anxiety symptomatology (e.g., shortness of breath) as being related to compromised health.
The particular relevance of accurately diagnosing and describing individuals with anxiety disorders and comorbid general medical conditions becomes more salient in the context of patient outcomes. Emerging literature on the topic suggests that, as one may expect, outcomes are far poorer among patients with anxiety and a comorbid general medical condition, compared with those with anxiety alone or a general medical condition alone. For example, among older individuals with common chronic conditions such as cataracts, allergies, and arthritis, those with comorbid anxiety had significantly worse self-reported mental and physical health scores (12). Another concerning comorbidity is suicide; research suggests that those with anxiety disorders and general medical conditions are more likely to experience symptoms of suicidal ideation (13). Ultimately, the combination of general medical conditions and anxiety disorders results in poorer functioning than would be seen if the general medical condition was found alone (14). The negative outcomes in the context of comorbidity are important to recognize, considering the previously described high rates of comorbid anxiety disorders in some general medical conditions.
A distinction must be drawn between anxiety disorders with comorbid general medical conditions and health anxiety or illness anxiety disorders. The classification of health anxiety or illness anxiety disorders has been modified in DSM-5, and constellations of health anxiety symptoms fall under somatic symptom disorder (SSD) and illness anxiety disorder (IAD) diagnoses (15), both of which exist in the category of somatic symptom and related disorders. This replaces the DSM-IV-TR category of somatoform disorders. These diagnoses have been separated from other anxiety disorders to emphasize the pervasive health worry associated with cognitive, behavioral, and emotional features specific to health. In particular, SSD involves the presence of excessive distress related to somatic symptoms or bodily changes that significantly affect functioning. IAD, in contrast, involves preoccupation with having or acquiring a serious illness (labeled hypochondriasis in DSM-IV-TR). What makes these diagnoses differ from that of anxiety with comorbid general medical conditions is that the fear and anxiety in SSD and IAD is specifically related to one’s health status. In SSD, a patient experiences symptomatology that may, or may not, be related to a defined medical cause. For example, chronic pain conditions often lack an active physiological trigger or exacerbation. IAD may not involve any medical condition, current or otherwise, and instead revolves around the anxiety of potentially becoming ill. As suggested by some mental health professionals, these new distinctions may reduce the stigma surrounding traditional terminology by validating the patient’s concerns and decreasing the emphasis on whether there is a medical explanation for their symptoms, all while more accurately describing the disorders themselves (16). Research on the category of SSD is in its infancy, and future research may identify a high SSD rate in the context of particular general medical conditions.
Mechanisms of Co-occurrence
Understanding the temporal relationship between anxiety and comorbid general medical conditions is important in our efforts to determine interventional, diagnostic, and treatment goals. As the body of literature on the topic expands, so does the variety of potential causal explanatory factors. We begin by exploring how those with existing anxiety disorders are at higher risk for future general medical problems. Then, we comment on research describing how medical illness increases the likelihood of future anxiety disorders and how this relationship is governed. Finally, we conclude this section with an examination of how anxiety disorders and general medical conditions mutually maintain one another, exploring possible mechanisms that govern the interplay between these conditions.
Anxiety Disorders as Precursors to General Medical Conditions
Martin is a 59-year-old male. He was diagnosed as having generalized anxiety disorder (GAD) after experiencing excessive fear and worry over a period of several months with respect to several life domains. He had trouble sleeping, difficulty concentrating, and restlessness, all of which affected his work and social activities. His psychiatrist prescribed sertraline to help manage the symptoms, which Martin has been taking for 4 years. He feels a little bit better than before but would not describe himself as “well,” because he continues to experience excessive worry. Recently, Martin has noticed that his joints are unusually sore when he gets out of bed in the morning.
As noted earlier, the lifetime prevalence of any anxiety disorder is high. Furthermore, several general medical conditions are highly prevalent, especially with the growing older adult population (17, 18). For example, it is estimated that the number of individuals in the United States with arthritis may reach 67 million by 2030 (19), a sizable portion of the population. Given these high rates, it is reasonable to question whether individuals with anxiety who later develop a general medical condition do so because of mere probability or whether a causal relationship exists. An analysis of World Mental Health surveys in 2015 (20) revealed that the presence of any major anxiety disorder increased the risk of chronic general medical conditions, including arthritis, chronic pain, heart disease, stroke, hypertension, asthma, and peptic ulcers. Longitudinal research with older adults has identified that anxiety disorders and posttraumatic stress disorder (PTSD) are predictive of incident gastrointestinal conditions (21). Similarly, Härter and colleagues (22) determined that anxiety disorders predict cardiac disorders, gastrointestinal problems, genitourinary problems, and migraines.
A recent case-control study comparing specific phobias to general medical illnesses (23) also attempted to find a temporal relationship by comparing the proportion of individuals in each disease category who showed a social phobia before receiving a medical diagnosis with the proportion who showed a social phobia after their medical diagnosis. Of the study sample, 82% of those who were diagnosed as having hypertension or gastrointestinal diseases had a comorbid social phobia before diagnosis. The conditions studied included arthritis (77.4%) and cardiac diseases (78.1%), among others. Intriguing as this is, it remains unclear whether this represents a causal relationship or simply reflects an earlier age of first presentation of social phobia, compared with these other general medical conditions.
There is also compelling literature on the significant physiological impact of stress and anxiety. In his review on neurogenic inflammation, Black (24) suggested that “repeated episodes of acute or chronic psychogenic stress may produce chronic inflammatory changes,” noting that diseases such as atherosclerosis, arthritis, and others may be created or exacerbated by psychological conditions. Inflammatory responses may also be important in coronary vascular disease, in which increased anxiety symptoms may elevate one’s risk for ischemic events (25). This may be due to the existence of specific biological mediators between stress and inflammation, including corticotropin-releasing factor. Another inflammatory marker, C-reactive protein, has been shown to be significantly higher for men with anxiety disorders than for those without, even when accounting for other disease and lifestyle factors (26). Furthermore, stress and anxiety can result in physiological changes mediated from changes to hormone levels (27). These physiological changes may be particularly robust in the case of chronic anxiety symptoms (28). Indeed, the concept of allostatic load is well recognized where prolonged stress over time can result in “wear and tear” on the body (29). Thus, the presence of anxiety, particularly over an extended period, may cause a cascade of physiological changes, putting an individual at risk of general medical conditions.
Beyond biological markers, those with anxiety disorders may exhibit a variety of maladaptive health behaviors that increase the risk of future general medical conditions. For instance, there is a known association between anxiety disorders and smoking (30), and alcohol use disorders are more prevalent among those with anxiety disorders, potentially as a consequence of self-medication (31). Anxiety disorders have also been shown to be associated with maladaptive eating and to pre-exist eating disorders such as anorexia and bulimia nervosa (32). Those with anxiety who show avoidance behaviors may be at further, compounded risk, because they are significantly less likely to access necessary care (33). It is reasonable to conclude that these resultant maladaptive behaviors may increase the risk of future general medical conditions.
As the months go by, Martin’s anxiety remains relatively unchanged. His sertraline prescription helps him remain functional, and he is able to remain productive at work. Unfortunately, his joint pain has continued to worsen, and he discusses the pain with his family physician. After examination and testing, he receives a diagnosis of osteoarthritis. Knowing that this new condition is likely going to continue worsening over time, he wonders how he will be able to manage in the future.
General Medical Conditions as Precursors to Anxiety Disorders
Henri is a 59-year-old male. He was diagnosed as having osteoarthritis after experiencing worsening knee joint pain and discomfort over a period of several months. He sometimes worries that his pain will become debilitating when he is out in public and now tends not to travel far from home or work. His physician prescribed him ibuprofen and a knee brace to help manage the symptoms. He feels a little bit better than before but would not describe himself as “well.” Yesterday at work, he felt anxious about meeting a new coworker and noticed his heart beating through his chest, a feeling that he has never had.
As an individual copes with the challenges of his or her general medical condition, it is reasonable that diminishing self-esteem and new social stressors may increase the risk of developing an anxiety disorder. For example, women diagnosed as having breast cancer are at an increased risk of mental disorders in that they tend to experience greater distress and obtrusive thoughts than average (34). Older patients, in particular, are at greater risk of pervasive health worry (35), and it is reasonable to postulate that specific health anxiety symptoms may become more generalized as a chronic medical condition progresses and functioning declines (36). Health conditions that are associated with high levels of pain and disability may put people at greater risk of future anxiety. Arthritis, for example, has been shown to result in incident GAD among older patients (21).
Although now identified as its own diagnostic category, PTSD is also important to consider in this discussion as a psychological disorder characterized by anxiety symptoms arising from the onset of a medical condition deemed as traumatic. Research on transplant patients describes a significant incidence of posttransplant/disease PTSD diagnoses, which may present years after the resolution of the medical condition (37). Illnesses that are more critical and result in more extreme stressors (e.g., pain and/or debilitation) may increase the risk of future anxiety/PTSD. This is evident by the high rates of PTSD seen among those who have been admitted to intensive care units with critical illnesses (38).
Identifying the mechanism in which general medical conditions result in anxiety disorders reveals some similarity to the reverse direction previously described. It is possible that common stress mediators may be bidirectional, causing neurochemical changes in the brain. Unique to this association is the presence of SSD as a possible mediator, given that individuals with general medical conditions may initially show significant health anxiety that becomes more generalized later through prolonged cognitive biases (e.g., misinterpretations of bodily sensations) and maladaptive behaviors (e.g., avoidance), where an individual may more appropriately meet the diagnosis for GAD, for example. Further investigation is required to elucidate the factors involved in this relationship, particularly as use of the new DSM-5 classification system expands.
Since his diagnosis of osteoarthritis, Henri has been fearful of being out on his own, in case his pain becomes unbearable and he requires assistance. As the months go by, he is able to control his fear about his pain; however, he has started to become anxious around new people at work. Even when he is alone, he finds that he is having more trouble sleeping and cannot concentrate. He discusses these feelings with his psychologist, who suggests that his symptoms are consistent with GAD. Henri wonders how he will manage to cope with his arthritis pain when he feels worried and anxious all of the time.
Mutual Maintenance of Anxiety Disorders and General Medical Conditions
Julia is a 42-year-old woman with poorly controlled type 2 diabetes that resulted in renal failure. She is currently on hemodialysis, which she completes at home. In addition, she was diagnosed as having social anxiety disorder approximately 17 years ago. Until recently, she worked as an evening custodial aide at the local elementary school. However, her recent commencement of hemodialysis therapy has made it challenging to continue working. She is struggling to manage her hemodialysis and diabetes therapies herself but is embarrassed to tell her doctor, because she has already required three more dialysis-training sessions than is typically required. This evening, she feels particularly ill and calls an ambulance to take her to the hospital.
Although there is evidence for causal mechanisms, anxiety disorders and chronic medical conditions may mutually maintain each other, hampering treatment efforts and increasing morbidity. In the case of older patients with cardiac disease who undergo cardiac surgery, those with comorbid anxiety are more likely than those without anxiety to experience major morbidity or mortality (39). Patients with coronary heart disease who also have anxiety symptoms are also more likely to suffer an adverse coronary vascular event (including stroke, nonfatal myocardial infarct, etc.) (25).
General medical conditions and poor physical-health-related quality of life are associated with persistence of particular anxiety disorders in late life (40). Furthermore, the severity and implications of anxiety symptoms may be greater in some general medical conditions than in others. A cross-sectional study (41) utilizing the Hospital Anxiety and Depression Score (HADS) found that among the conditions examined (coronary artery disease, renal transplantation, chronic hemodialysis, rheumatologic conditions, and viral hepatitis), anxiety symptoms were most severe for those with rheumatoid arthritis and viral hepatitis. The existence of tertiary comorbid conditions may further exacerbate this relationship. For example, hemodialysis patients may have increased presence of disturbed body image, which may exacerbate anxiety symptoms (42).
Various biological and neurophysiological models may help explain how anxiety disorders and general medical conditions mutually maintain one another. Anxiety is known to decrease the threshold of pain and reduce pain tolerance (43). Regions of the brain that are responsible for emotion and stress responses are commonly thought to be important, including the hypothalamus, amygdala, hippocampus, and striatal regions (44). Alterations in the behavior of these regions, including changes in neurotransmitter levels, are thought to contribute to the development and exacerbation of anxiety. The cause of these neurological changes are likely a contribution of genetic and environmental and experiential factors. Heritability of anxiety disorders ranges from 30% to 50%, and the risk of familial aggregation (family members living with someone with an anxiety disorder later exhibiting anxiety themselves) is four- to sixfold higher than baseline (45). It is plausible that the same environmental and genetic factors that increase one’s risk for anxiety also increase one’s risk for some common general medical conditions. Indeed, one recent study identified a genomewide significant locus of PTSD that has also been indicated in several autoimmune diseases—notably, rheumatoid arthritis (46). Other genetic research on PTSD sufferers has identified PTSD-risk genes that are independently associated with coronary vascular disease, giving quantifiable credence to the American Civil War term soldier’s heart. (47)
In understanding mutual maintenance, it is important to understand the impact of targeted therapies on both mental and medical health. A study (48) on the treatment of anxiety and depression with citalopram among patients with comorbid asthma found that citalopram reduced depression symptoms and improved asthma symptoms, a relationship the investigators postulated may be due to citalopram’s “increase [of] of glucocorticoid negative feedback on the hypothalamic-pituitary-adrenal axis.” Research on inflammatory bowel disease (IBD) has developed the notion of a “brain-gut pathway.” This suggests that common autonomic pathways through the brain and gut may link stress and inflammation, which may help explain the high prevalence of gastrointestinal disorders among those with anxiety (49). It is well recognized that treatments for IBD are often both pharmacological and psychological, given the high comorbidity rates (50).
Interestingly, it appears that anxiety disorders are sometimes protective in the context of general medical conditions. Specifically, a 2015 study by Ho et al. (51) discovered that among individuals with hypertension, those with comorbid anxiety achieved blood pressure control more rapidly than did those without anxiety. They theorized that, because individuals in this group were greater utilizers of health care resources, they likely received more frequent blood pressure monitoring. It has also been postulated that antidepressant medications may reduce baroreflex sensitivity, thus exerting a dual effect on symptoms of anxiety or depression and blood pressure (52). Relatedly, prazosin, a sympatholytic drug, which was originally developed for hypertension, is now regularly used to reduce the frequency and severity of PTSD-associated nightmares (53). As we learn more about the interactions between biochemical and physiological processes, it becomes evident that the combination of anxiety and general medical conditions can result in a wide range of effects. While specific directional cause-effect relationships may be present, it is apparent that the course of every individual and every disease is highly variable, depending significantly on individual, environmental, and social factors.
After arriving at the hospital, Julia is diagnosed and treated for uremia, likely due to improper use of her hemodialysis equipment. She is upset and embarrassed when the dialysis educators attempt to explain the process to her once again, and it is clear to the staff that poor dialysis is only a small piece of her current problem. The dialysis nurse suggests that Julia talk to a mental health professional about how to cope with her numerous conditions. She is reluctant to share her feelings with yet another stranger.
Recognition and Treatment Approaches
Developing an appropriate approach to patients with anxiety disorders and comorbid general medical conditions necessitates the involvement of a multidisciplinary team with emphasis on early recognition of risk factors and appropriate treatment. Personal, social, and illness-related factors can each intervene to delay or complicate treatment. Here, we describe the burden of individual conditions and complex comorbid conditions and address how integrative and collaborative care models can address these challenges. Finally, we explore alternative approaches and future challenges of implementation.
Anxiety disorders represent a significant financial burden on health care systems. Alone, anxiety disorders in the United States have indirect costs ranging from $109 million to $615 million per million inhabitants (54), and costs of chronic diseases tend to be high in most developed countries (55). Research evaluating the combined cost of anxiety and general medical conditions is more limited; however, a 2011 study (56) evaluated the costs of COPD with and without comorbid depression or anxiety, finding a significant increase in health care costs among those with comorbidity. In addition, there may be increased mental health service use among individuals with anxiety and comorbid arthritis or cardiovascular disease (57). Therefore, novel treatment approaches must be cost effective in addition to being clinically useful.
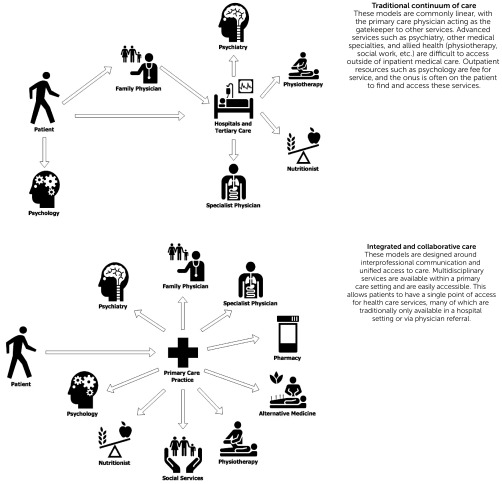
Inadequate mental health resources in the context of high demand for services presents a significant burden to health care systems. Mental health professionals are under increasing pressure to see multiple patients as rapidly as possible. Traditionally, most Western health care systems have been designed with primary care physicians as the “gatekeepers,” managing what they can on their own and referring more complicated cases to specialists (58). This is generally a unidirectional system, often causing backlogs and waitlists for specialists and increasing health care costs. Furthermore, increasing access to specialists does not necessarily improve quality of care (59). Integrative care models are designed to increase interaction among health care professionals, and evidence suggests that most primary care physicians believe that integrative care leads to better communication with mental health specialists and better treatment of anxiety (60) (Figure 1). Integrative care improves outcomes among patients with comorbid medical and mental illnesses and is more cost effective than traditional dual-system approaches (61).
FIGURE 1.
Traditional Linear Care Models and Integrative Care Networks
Multiple names exist for similar health care models that are integrative and tend to be multidisciplinary. Collaborative care emphasizes a model in which health care providers are given the means to communicate with one another effectively and work together to treat patients. Shared care is the same, focusing on a team-based approach to patient care. Integrative care often extends these models to social and cultural care and is becoming a widely used term for these types of models.
In the United States, the US Department of Health and Human Services defines integrative treatment as “any mechanism by which treatment interventions for co-occurring disorders are combined within the context of a primary treatment relationship or service setting” (62, p. 30). These models are structured as interconnected networks of health professionals and may incorporate various methods of care. Health care systems utilizing an integrative approach are often able to deliver modern medical therapies efficiently by using new technologies while also providing access to alternative medicine, complementary medicine, and other potentially useful disciplines depending on the needs of the patient (63). Integrative care has been shown to improve outcomes among individuals with anxiety disorders alone (64), depression alone (65), and among those with comorbid depression and general medical conditions (66). Accordingly, integrative care may also prove effective in managing the complex comorbid conditions found among those with anxiety and comorbid medical conditions. Literature examining the efficacy of collaborative care supports this hypothesis; however, there is evidence that the presence of certain comorbid conditions, including migraines, is associated with poorer long-term outcomes (67). Further research is required to determine effectiveness of these models in treating specific comorbid conditions.
Beyond integrative care, literature on effective treatment modalities for patients with comorbid anxiety disorders and general medical conditions is growing. In particular, there is increasing evidence that mind-body medicine techniques, such as mindfulness meditation and relaxation, may be effective. There is evidence that mind-body therapies may improve a wide array of general medical conditions, including chronic pain, coronary artery disease, headaches, and insomnia, among others (68). Among those with anxiety disorders in the United States, nearly half consider mind-body therapies “very helpful” for their condition (69). Another potentially effective treatment consideration is exercise. Research has shown that prescribed exercise may be effective in reducing anxiety symptoms and, potentially, even in the treatment of anxiety disorders (70), in addition to its well-recognized physical health benefits. Finally, evidence supports the use of psychological interventions for the treatment of comorbid anxiety and chronic pain. For example, literature suggests that the use of cognitive-behavioral therapy may improve physical capacity of those with pain-related anxiety, independent of any physical treatment modalities (71).
Despite evidence supporting many of these approaches, responses from physicians and mental health professionals are often mixed. Behavioral medicine approaches that include meditation and mind-body therapies are shown to reduce anxiety symptoms of those with other general medical conditions (72). While most physicians recognize the value of these approaches, a disproportionately low number of them are interested in receiving further biopsychosocial training to incorporate these approaches into their practices (73). As this body of research continues to evolve and these therapies are empirically validated, medical education may become more receptive of the biopsychosocial model for treatment.
Numerous novel approaches exist and continue to be developed for the treatment management of people with anxiety disorders and general medical conditions; however, each approach promotes a common theme of greater interprofessional collaboration, efficient resource utilization, and openness to approaches focused on general medical and mental wellness. These evidence-based models may be designed for incorporation into large, regional health systems or small local practices.
Conclusions and Future Directions
Methodologies for the treatment management of patients with comorbid anxiety disorders and general medical conditions are being implemented in health care systems across the globe. Although evidence promotes the efficacy of programs such as integrative care, challenges continue to exist in the development and long-term support of these systems.
Collaborative and shared-care models have been implemented and studied across North America. For example, implementation of this model reduced psychological care wait times by more than half in one primary care clinic, compared with wait times of the tertiary care setting (74). While such reductions are encouraging, detailed cost-benefit analyses of collaborative care models are necessary to evaluate feasibility of implementation. The MOSAIC study from Harvard Medical School analyzed the effectiveness of collaborative care in the inpatient setting for acute cardiac-care patients with comorbid anxiety, depression, or both (75). Compared with enhanced usual care, the collaborative care model was more expensive up front but was associated with a greater increase in quality-adjusted life years (QALY) and fewer future emergency room admissions. This model was determined to be cost effective overall, with an incremental cost-effectiveness ratio of US$3,337 per QALY, falling well below the traditional/common threshold of US$50,000/QALY.
Despite the apparent benefit of collaborative care models, the greater upfront cost makes implementation politically challenging. Cost-effectiveness research is useful in demonstrating long-term benefits; unfortunately, the significant variability in medical practice regionally and globally makes is difficult to generalize the results of such studies. IMPACT, the Integrative Medicine PrimAry Care Trial, recently developed a trial protocol attempting to explore the effects of medical systems that integrate conventional and complementary medicine within the primary care model (76). Future research utilizing this and other models will expand our understanding of collaborative and integrative care in the context treating comorbid anxiety disorders and general medical conditions.
The combination of anxiety disorders and general medical conditions creates significant challenges to accurate identification and treatment. Anxiety disorders may increase the likelihood of a variety of general medical conditions, and general medical conditions may worsen or increase the risk of anxiety. When combined with anxiety disorders, most general medical conditions incur greater morbidity and, in some cases, higher rates of mortality. As growing financial pressure on health care systems creates new challenges in providing effective care, new methods such as integrative and collaborative care models may allow health professionals to more effectively manage the treatment of patients who have complex comorbid conditions. The continued rise in prevalence in both anxiety disorders and chronic general medical conditions necessitates that we develop and encourage the use of evidence-based care models within our practices and communities.
Footnotes
Dr. Sareen reports holding stock in Johnson & Johnson and consulting for UpToDate. The other authors report no financial relationships with commercial interests.
References
- 1.Schulberg HC, McClelland M, Burns BJ: Depression and physical illness: the prevalence, causation, and diagnosis of comorbidity. Clin Psychol Rev 1987; 7:145–167 [Google Scholar]
- 2.Smyth R: Depression in physical illness. J R Coll Physicians Edinb 2009; 39:337–342 [DOI] [PubMed] [Google Scholar]
- 3.Olver JS, Hopwood MJ: Depression and physical illness. Med J Aust 2013; 199(Suppl):S9–S12 [DOI] [PubMed] [Google Scholar]
- 4.Remes O, Brayne C, van der Linde R, et al. : A systematic review of reviews on the prevalence of anxiety disorders in adult populations. Brain and Behavior 2016; 6:e00497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Somers JM, Goldner EM, Waraich P, et al. : Prevalence and incidence studies of anxiety disorders: a systematic review of the literature. Can J Psychiatry 2006; 51:100–113 [DOI] [PubMed] [Google Scholar]
- 6.Sareen J, Cox BJ, Clara I, et al. : The relationship between anxiety disorders and physical disorders in the US National Comorbidity Survey. Depress Anxiety 2005; 21:193–202 [DOI] [PubMed] [Google Scholar]
- 7.Bhattacharya R, Shen C, Sambamoorthi U: Excess risk of chronic physical conditions associated with depression and anxiety. BMC Psychiatry 2014; 14:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Anxiety disorders; in Diagnostic and Statistical Manual of Mental Disorders, 5th ed. Arlington, VA, American Psychiatric Association, 2013. doi:10.1176/appi.books.9780890425596.dsm05 [Google Scholar]
- 9.Eack SM, Greeno CG, Lee B-J: Limitations of the Patient Health Questionnaire in identifying anxiety and depression: many cases are undetected. Res Soc Work Pract 2006; 16:625–631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Leon AC, Portera L, Olfson M, et al. : Diagnostic errors of primary care screens for depression and panic disorder. Int J Psychiatry Med 1999; 29:1–11 [DOI] [PubMed] [Google Scholar]
- 11.Wilk JE, West JC, Narrow WE, et al. : Comorbidity patterns in routine psychiatric practice: is there evidence of underdetection and underdiagnosis? Compr Psychiatry 2006; 47:258–264 [DOI] [PubMed] [Google Scholar]
- 12.El-Gabalawy R, Mackenzie CS, Shooshtari S, et al. : Comorbid physical health conditions and anxiety disorders: a population-based exploration of prevalence and health outcomes among older adults. Gen Hosp Psychiatry 2011; 33:556–564 [DOI] [PubMed] [Google Scholar]
- 13.Raposo S, El-Gabalawy R, Erickson J, et al. : Associations between anxiety disorders, suicide ideation, and age in nationally representative samples of Canadian and American adults. J Anxiety Disord 2014; 28:823–829 [DOI] [PubMed] [Google Scholar]
- 14.Norman SB, Lang AJ: The functional impact of anxiety sensitivity in the chronically physically ill. Depress Anxiety 2005; 21:154–160 [DOI] [PubMed] [Google Scholar]
- 15.Somatic symptom and related disorders; in Diagnostic and Statistical Manual of Mental Disorders, 5th ed. Arlington, VA, American Psychiatric Association, 2013. doi:10.1176/appi.books.9780890425596.dsm09 [Google Scholar]
- 16.Brakoulias V: DSM-5 bids farewell to hypochondriasis and welcomes somatic symptom disorder and illness anxiety disorder. Aust N Z J Psychiatry 2014; 48:688. [DOI] [PubMed] [Google Scholar]
- 17.Dall TM, Gallo PD, Chakrabarti R, et al. : An aging population and growing disease burden will require a large and specialized health care workforce by 2025. Health Aff 2013; 32:2013–2020 [DOI] [PubMed] [Google Scholar]
- 18.Fried LP, Ferrucci L, Darer J, et al. : Untangling the concepts of disability, frailty, and comorbidity: implications for improved targeting and care. J Gerontol A Biol Sci Med Sci 2004; 59:255–263 [DOI] [PubMed] [Google Scholar]
- 19.Helmick CG, Felson DT, Lawrence RC, et al. : Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part I. Arthritis Rheum 2008; 58:15–25 [DOI] [PubMed] [Google Scholar]
- 20.Scott KM, Lim C, Al-Hamzawi A, et al. : Association of mental disorders with subsequent chronic physical conditions: World Mental Health surveys from 17 countries. JAMA Psychiatry 2016; 73:150–158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.El-Gabalawy R, Mackenzie CS, Pietrzak RH, et al. : A longitudinal examination of anxiety disorders and physical health conditions in a nationally representative sample of US older adults. Exp Gerontol 2014; 60:46–56 [DOI] [PubMed] [Google Scholar]
- 22.Härter MC, Conway KP, Merikangas KR: Associations between anxiety disorders and physical illness. Eur Arch Psychiatry Clin Neurosci 2003; 253:313–320 [DOI] [PubMed] [Google Scholar]
- 23.Witthauer C, Ajdacic-Gross V, Meyer AH, et al. : Associations of specific phobia and its subtypes with physical diseases: an adult community study. BMC Psychiatry 2016; 16:155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Black PH: Stress and the inflammatory response: a review of neurogenic inflammation. Brain Behav Immun 2002; 16:622–653 [DOI] [PubMed] [Google Scholar]
- 25.Rothenbacher D, Hahmann H, Wüsten B, et al. : Symptoms of anxiety and depression in patients with stable coronary heart disease: prognostic value and consideration of pathogenetic links. Eur J Cardiovasc Prev Rehabil 2007; 14:547–554 [DOI] [PubMed] [Google Scholar]
- 26.Vogelzangs N, Beekman ATF, de Jonge P, et al. : Anxiety disorders and inflammation in a large adult cohort. Transl Psychiatry 2013; 3:e249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lupien SJ, McEwen BS, Gunnar MR, et al. : Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nat Rev Neurosci 2009; 10:434–445 [DOI] [PubMed] [Google Scholar]
- 28.Schneiderman N, Ironson G, Siegel SD: Stress and health: psychological, behavioral, and biological determinants. Annu Rev Clin Psychol 2005; 1:607–628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McEwen BS: Protection and damage from acute and chronic stress: allostasis and allostatic overload and relevance to the pathophysiology of psychiatric disorders. Ann N Y Acad Sci 2004; 1032:1–7 [DOI] [PubMed] [Google Scholar]
- 30.Cougle JR, Zvolensky MJ, Fitch KE, et al. : The role of comorbidity in explaining the associations between anxiety disorders and smoking. Nicotine Tob Res 2010; 12:355–364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Smith JP, Randall CL: Anxiety and alcohol use disorders: comorbidity and treatment considerations. Alcohol Res 2012; 34:414–431 [PMC free article] [PubMed] [Google Scholar]
- 32.Godart NT, Perdereau F, Jeammet P, et al. : Comorbidity and time of occurrence of anxiety disorders in eating disorders [in French]. Ann Med Psychol (Paris) 2003; 161:498–503 [Google Scholar]
- 33.Chartier-Otis M, Perreault M, Bélanger C: Determinants of barriers to treatment for anxiety disorders. Psychiatr Q 2010; 81:127–138 [DOI] [PubMed] [Google Scholar]
- 34.Baum A, Posluszny DM: Health psychology: mapping biobehavioral contributions to health and illness. Annu Rev Psychol 1999; 50:137–163 [DOI] [PubMed] [Google Scholar]
- 35.El-Gabalawy R, Mackenzie CS, Thibodeau MA, et al. : Health anxiety disorders in older adults: conceptualizing complex conditions in late life. Clin Psychol Rev 2013; 33:1096–1105 [DOI] [PubMed] [Google Scholar]
- 36.Montorio I, Nuevo R, Márquez M, et al. : Characterization of worry according to severity of anxiety in elderly living in the community. Aging Ment Health 2003; 7:334–341 [DOI] [PubMed] [Google Scholar]
- 37.DiMartini A, Dew MA, Kormos R, et al. : Posttraumatic stress disorder caused by hallucinations and delusions experienced in delirium. Psychosomatics 2007; 48:436–439 [DOI] [PubMed] [Google Scholar]
- 38.Davydow DS, Gifford JM, Desai SV, et al. : Posttraumatic stress disorder in general intensive care unit survivors: a systematic review. Gen Hosp Psychiatry 2008; 30:421–434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Williams JB, Alexander KP, Morin J-F, et al. : Preoperative anxiety as a predictor of mortality and major morbidity in patients aged >70 years undergoing cardiac surgery. Am J Cardiol 2013; 111:137–142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mackenzie CS, El-Gabalawy R, Chou KL, et al. : Prevalence and predictors of persistent versus remitting mood, anxiety, and substance disorders in a national sample of older adults. Am J Geriatr Psychiatry 2014; 22:854–865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bayat N, Alishiri GH, Salimzadeh A, Izadi M, et al. : Symptoms of anxiety and depression: a comparison among patients with different chronic conditions. J Res Med Sci 2011; 16:1441–1447 [PMC free article] [PubMed] [Google Scholar]
- 42.Öyekçin DG, Gülpek D, Sahin EM, et al. : Depression, anxiety, body image, sexual functioning, and dyadic adjustment associated with dialysis type in chronic renal failure. Int J Psychiatry Med 2012; 43:227–241 [DOI] [PubMed] [Google Scholar]
- 43.Dersh J, Polatin PB, Gatchel RJ: Chronic pain and psychopathology: research findings and theoretical considerations. Psychosom Med 2002; 64:773–786 [DOI] [PubMed] [Google Scholar]
- 44.Nieto SJ, Patriquin MA, Nielsen DA, et al. : Don’t worry; be informed about the epigenetics of anxiety. Pharmacol Biochem Behav 2016; 146-147:60–72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Shimada-Sugimoto M, Otowa T, Hettema JM: Genetics of anxiety disorders: genetic epidemiological and molecular studies in humans. Psychiatry Clin Neurosci 2015; 69:388–401 [DOI] [PubMed] [Google Scholar]
- 46.Stein MB, Chen C-Y, Ursano RJ, et al. : Genome-wide association studies of posttraumatic stress disorder in 2 cohorts of US army soldiers. JAMA Psychiatry 2016; 73:695–704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Pollard HB, Shivakumar C, Starr J, et al. : “Soldier’s heart”: a genetic basis for elevated cardiovascular disease risk associated with post-traumatic stress disorder. Front Mol Neurosci 2016; 9:87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Brown ES, Vigil L, Khan DA, et al. : A randomized trial of citalopram versus placebo in outpatients with asthma and major depressive disorder: a proof of concept study. Biol Psychiatry 2005; 58:865–870 [DOI] [PubMed] [Google Scholar]
- 49.Bonaz BL, Bernstein CN: Brain-gut interactions in inflammatory bowel disease. Gastroenterology 2013; 144:36–49 [DOI] [PubMed] [Google Scholar]
- 50.Graff LA, Walker JR, Bernstein CN: Depression and anxiety in inflammatory bowel disease: a review of comorbidity and management. Inflamm Bowel Dis 2009; 15:1105–1118 [DOI] [PubMed] [Google Scholar]
- 51.Ho AK, Thorpe CT, Pandhi N, et al. : Association of anxiety and depression with hypertension control: a US multidisciplinary group practice observational study. J Hypertens 2015; 33:2215–2222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mejia-Lancheros C, Estruch R, Martínez-González MA, et al. : Blood pressure values and depression in hypertensive individuals at high cardiovascular risk. BMC Cardiovasc Disord 2014; 14:109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kung S, Espinel Z, Lapid MI: Treatment of nightmares with prazosin: a systematic review. Mayo Clin Proc 2012; 87:890–900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Konnopka A, Leichsenring F, Leibing E, et al. : Cost-of-illness studies and cost-effectiveness analyses in anxiety disorders: a systematic review. J Affect Disord 2009; 114:14–31 [DOI] [PubMed] [Google Scholar]
- 55.Zhao F-L, Xie F, Hu H, et al. : Transferability of indirect cost of chronic disease: a systematic review and meta-analysis. Pharmacoeconomics 2013; 31:501–508 [DOI] [PubMed] [Google Scholar]
- 56.Dalal AA, Shah M, Lunacsek O, et al. : Clinical and economic burden of depression/anxiety in chronic obstructive pulmonary disease patients within a managed care population. COPD 2011; 8:293–299 [DOI] [PubMed] [Google Scholar]
- 57.Karlin BE, Duffy M, Gleaves DH: Patterns and predictors of mental health service use and mental illness among older and younger adults in the United States. Psychol Serv 2008; 5:275–294 [Google Scholar]
- 58.Rosenblatt RA, Moscovice IS: The physician as gatekeeper. Determinants of physicians’ hospitalization rates. Med Care 1984; 22:150–159 [DOI] [PubMed] [Google Scholar]
- 59.Katon W, Von Korff M, Lin E, et al. : Rethinking practitioner roles in chronic illness: the specialist, primary care physician, and the practice nurse. Gen Hosp Psychiatry 2001; 23:138–144 [DOI] [PubMed] [Google Scholar]
- 60.Gallo JJ, Zubritsky C, Maxwell J, et al. : Primary care clinicians evaluate integrated and referral models of behavioral health care for older adults: results from a multisite effectiveness trial (PRISM-e). Ann Fam Med 2004; 2:305–309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ivbijaro GO, Enum Y, Khan AA, et al. : Collaborative care: models for treatment of patients with complex medical-psychiatric conditions. Curr Psychiatry Rep 2014; 16:506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Substance Abuse Treatment for Persons With Co-occurring Disorders. Treatment Improvement Protocol Series No 42. HHS Publication No (SMA) 13-3992. Rockville, MD: Substance Abuse and Mental Health Services Administration, 2005. [PubMed]
- 63.Sundberg T, Hök J, Finer D. et al. : Evidence-informed integrative care systems—the way forward. Eur J Integr Med 2014; 6:12–20 [Google Scholar]
- 64.Muntingh AD, van der Feltz-Cornelis CM, van Marwijk HW, et al. : Collaborative care for anxiety disorders in primary care: a systematic review and meta-analysis. BMC Fam Pract 2016; 17:62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Panagioti M, Bower P, Kontopantelis E, et al. : Association between chronic physical conditions and the effectiveness of collaborative care for depression: an individual participant data meta-analysis. JAMA Psychiatry 2016; 73:978–989 [DOI] [PubMed] [Google Scholar]
- 66.Katon WJ, Lin EH, Von Korff M, et al. : Collaborative care for patients with depression and chronic illnesses. N Engl J Med 2010; 363:2611–2620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Campbell-Sills L, Stein MB, Sherbourne CD, et al. : Effects of medical comorbidity on anxiety treatment outcomes in primary care. Psychosom Med 2013; 75:713–720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Astin JA, Shapiro SL, Eisenberg DM, et al. : Mind-body medicine: state of the science, implications for practice. J Am Board Fam Pract 2003; 16:131–147 [DOI] [PubMed] [Google Scholar]
- 69.Wolsko PM, Eisenberg DM, Davis RB, et al. : Use of mind-body medical therapies. J Gen Intern Med 2004; 19:43–50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Asmundson GJG, Fetzner MG, Deboer LB, et al. : Let’s get physical: a contemporary review of the anxiolytic effects of exercise for anxiety and its disorders. Depress Anxiety 2013; 30:362–373 [DOI] [PubMed] [Google Scholar]
- 71.McCracken LM, Gross RT, Eccleston C: Multimethod assessment of treatment process in chronic low back pain: comparison of reported pain-related anxiety with directly measured physical capacity. Behav Res Ther 2002; 40:585–594 [DOI] [PubMed] [Google Scholar]
- 72.Nakao M, Fricchione G, Myers P, et al. : Anxiety is a good indicator for somatic symptom reduction through behavioral medicine intervention in a mind/body medicine clinic. Psychother Psychosom 2001; 70:50–57 [DOI] [PubMed] [Google Scholar]
- 73.Astin JA, Soeken K, Sierpina VS, et al. : Barriers to the integration of psychosocial factors in medicine: results of a national survey of physicians. J Am Board Fam Med 2006; 19:557–565 [DOI] [PubMed] [Google Scholar]
- 74. Graff L a: Kaoukis G, Vincent N, Piotrowski A, Ediger J. New models of care for psychology in Canada’s health services. Can Psychol Can 2012; 53:165–177. [Google Scholar]
- 75.Celano CM, Healy B, Suarez L, et al. : Cost-effectiveness of a collaborative care depression and anxiety treatment program in patients with acute cardiac illness. Value Health 2016; 19:185–191 [DOI] [PubMed] [Google Scholar]
- 76.Herman PM, Dodds SE, Logue MD, et al. : IMPACT—Integrative Medicine PrimAry Care Trial: protocol for a comparative effectiveness study of the clinical and cost outcomes of an integrative primary care clinic model. BMC Complement Altern Med 2014; 14:132. [DOI] [PMC free article] [PubMed] [Google Scholar]