Abstract
The Affordable Care Act (ACA) provides financial incentives to prevent Substance Use Disorders (SUDs). Local health departments (LHDs) can receive funds to establish care teams that partner with primary care providers and health systems. This study estimates the potential effect of LHDs on emergency visits for SUDs, using linked data sets from the Healthcare Cost and Utilization Project (HCUP) Emergency Department Sample for the State of Maryland—2012, the National Association of County and City Health Officials Profiles Survey 2013, and Area Health Resource File 2013 to estimate potential effect of local health department’s provision of SUD preventive care and SUD-related policy implementation. LHD involvement in SUD-related policy during the past 2 years and provision of preventive care for behavioral health in the past year significantly reduced the probability of having a SUD-related ED visit by 11% and 6%, respectively, after controlling for individual characteristics (OR=0.89, p<0.001; OR=0.93, p<0.001). After adjusting for the individual and contextual factors, LHD involvement in policy was still associated with 14% reduction in SUD-related ED visits (OR=0.86, p<0.001). Results offer insight on the extent to which the LHD activities can possibly affect SUD-related ED visits and provide a foundation for work to identify effective LHD interventions.
Keywords: Local health departments, substance use disorders, population health, prevention
INTRODUCTION
Substance use disorder (SUD) refers to abuse or dependence of alcohol, tobacco, or illicit drugs.1 SUD is a major public health concern, with more than eight percent of the United States population aged 12 or older classified with some type of SUD in 2012.1 Untreated SUD is associated with high mortality rates,2 increased risks of developing major chronic diseases, and accelerated disease progression.3 Meanwhile, various subpopulations, including racial and ethnic groups4–7 and younger age groups,8–9 face increased likelihood of developing SUD. SUD can be effectively prevented10–13 and ameliorated through evidence-based public health measures, such as the provision of screening tests and treatment and education on SUD and its risk factors.14–15 Extensive evidence shows that community-based prevention programs,16–19 including parent training,20 peer-group education,21 and school-based interventions,22–23 can effectively prevent SUD, reduce violence and crime rates,24 and improve community health. Serving as the center of the community-engaged health programs and as a major source of health care for the vulnerable populations, Local Health Departments (LHDs) can play a critical role in the prevention and control of SUD.
The scientific literature makes clear that LHD activities are associated with improved self-reported health,25–26 reduced preventable deaths,27 and lower racial disparities (White vs. African American) in mortality rates.28 Additionally, research suggests that LHD involvement in mental illness preventive service provision decreases all-cause avoidable re-hospitalizations.29 The literature also provides convincing evidence that when LHDs are integrated with community partners, the incidence rates of chronic and infectious disease are reduced.30–31 The Public Health 3.0 infrastructure32 and the 21st Century Cures Act33 promote the integration of treatment for SUD to be inclusive of individual and organizational factors. LHDs can play the leadership role to establish community health teams and foster collaboration with primary care providers and health centers. Yet there remains a gap in our knowledge about how to best accomplish the integration of LHDs to improve treatment of SUDs.34
The recently released strategic plan from the National Institutes of Mental Health (2017) includes “Strengthen[ing] the Public Health Impact” to promote population behavioral health as a priority.35 The Centers for Disease Control has also outlined a process for public health systems to address SUDs in tandem with other chronic health conditions.36 Based on the literature and priorities identified by the NIMH and CDC,35–36 we expect that LHDs can make unique contributions to reduce SUDs.37–41 There are a number of roles LHDs’ can play in controlling SUDs. LHDs can impact SUDs by changing social norms around SUDs treatment,42 enforcing and implementing regulations to decrease the availability of substances (e.g., cigarette tax), identifying populations in need of referrals to appropriate treatment,15 and serving as a provider of last resort for those unable to access care through health insurance.43
To our knowledge, this is the first study to comprehensively assess the effect of LHD activities on ED use for SUDs and as such our study provides a foundation for future studies to design an integrated behavioral health care model by enlisting the active contributions of LHDs. Empirically, we test our model using hospital Emergency Department (ED) visit data from the state of Maryland. Maryland has 24 local health departments, and the communities that they serve vary widely in terms of socio-economic status, ethnic and racial characteristics of the populations served, and behavioral health disorder prevalence. We chose to measure visits to the ED because of the high cost of care delivered through the ED and the fact that EDs can serve as a key referrer to behavioral health care.43 We hypothesize that since SUDs are preventable, LHDs’ active involvement in health promotion and provision of SUD preventive care can reduce SUD-related ED visits.
METHODS
The main data set employed in our study is The National Association of County and City Health Officials (NACCHO) National Profile of Local Health Departments 2012.45 The NACCHO data provide a comprehensive description of LHD infrastructure and practice, including LHD governance, resources, and services. The response rate of NACCHO survey is 78%, and the responding agencies cover more than 90% of the US population each survey year.45 In the state of Maryland, the jurisdiction areas of LHDs are at the county level. Hence, to estimate the effect of LHDs on ED visits for SUDs, we link NACCHO data with the Healthcare Cost and Utilization Project (HCUP) State Emergency Department Database (SEDD) data from the state of Maryland for 2012, using county identifiers. The HCUP SEDD includes individuals' data on all visits to the ED that do not result in hospitalization and more than 100 clinical and non-clinical variables such as all diagnoses and procedures, demographics, expected payment source, total charges, and hospital identifiers.46 Finally, we link the data with the Area Health Resource File47 to obtain contextual factors at the county level, including demographic and health care access variables, to serve as control variables.
Outcome variable
Our outcome variable is a binary variable indicating whether a given ED visit was treatment for SUD. To be consistent with prior literature,48 we use the following ICD-9 codes for SUDs: (1) Alcohol-related disorders (ICD-9 codes: 2910–2919, 30300–30393, 30500–30503, 3575, 4255, 5353, 5710–5713, 7903); and (2) Drug abuse disorders (ICD-9 codes: 2920–2929, 30400–30493, 30520–30593).
Key independent variables
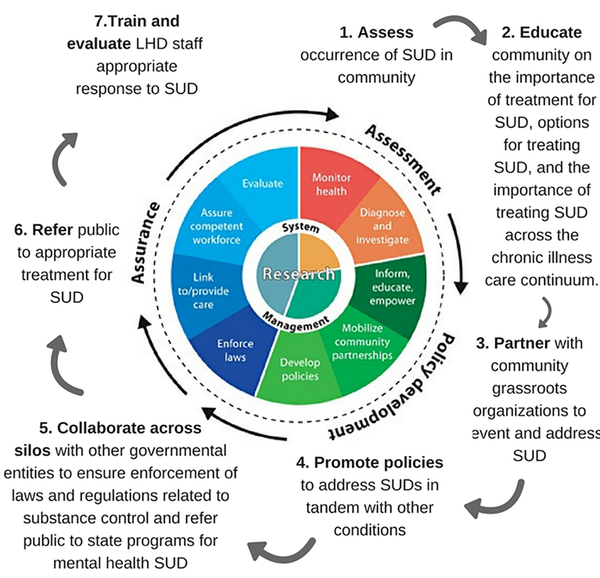
In accordance with our conceptual framework (see Figure 1), we construct two measures of LHD activities: (1) a binary variable indicating preventive services for SUDs in the past year, which equals to 1 if LHDs provide preventive services directly and 0 otherwise; and (2) a binary variable indicating whether LHD has been actively involved in policy activities focused on substance abuse issues. Policies included smoke-free indoor air (e.g., workplace, multi-unit residential), smoke-free outdoor air (e.g., parks, beaches, playgrounds, sporting events), reducing sale of tobacco to minors, raising cigarette taxes, raising alcohol taxes, diverting certain drug offenders into treatment rather than incarceration, reducing alcohol or drug impaired driving, and reducing exposure to alcohol or tobacco advertising.
Figure 1.
Public Health Model developed by the Centers for Disease Control, and available for public domain use. Public health actions related to SUD that impact ED use are conceptualized by authors around the established model.
Other covariates
Control variables include individual level characteristics (age, gender, race/ethnicity, insurance type [uninsured, Medicare, Medicaid, private, no-charge, other]), county level contextual factors (number of primary care physicians per 1,000 population, specialists per 1,000 population, number of hospitals, number of community mental health centers, and federally qualified health centers, total county population size, percent employed, percent female, percent White, percent African American, percent insured under age 65, percent with no high school education over age 25, and average median household income).
Analysis
We fit a multi-level statistical model to estimate whether LHDs’ could reduce the rates of ED utilization for SUDs.
The statistical equation:
where Y is the outcome variable of ED use for SUD treatment, X represents individual characteristics, H represents hospital characteristics, and LHD captures services provided by local health departments.
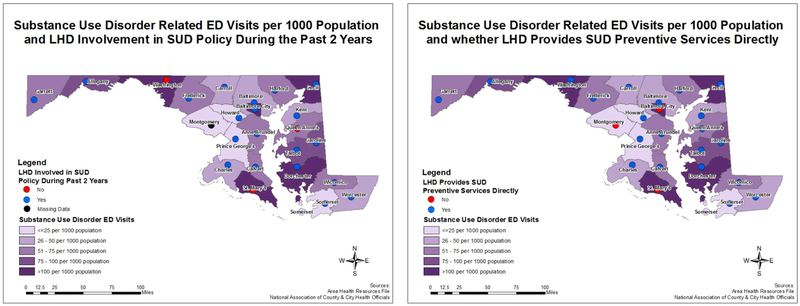
We first compare population characteristics of our sample, means of all independent, dependent and control variables for SUD-related ED visits versus non-SUD-related ED visits. T-tests and Analysis of Variance (ANOVA) tests were performed to examine significant differences between the two groups. We use Geographic Information Systems (GIS, specifically ArcMap, version 10.2) to examine our data spatially. U.S. Census Tiger/Line shapefiles were used for Maryland counties, as seen in Figure 2.49 Total SUD-related ED visits per 1,000 population were joined to the Maryland counties, which were then characterized by a graduated color scale. The addresses of each Maryland LHD, which are represented by small circles, were then geocoded and mapped on top of the Maryland counties. Our two independent LHD SUD variables of interest (policy and prevention) were then characterized by different colors indicating yes or no for each variable.
Figure 2:
LHD Policy and Prevention Activities and SUD-related ED visits in the State of Maryland
Multivariate logistic regressions were used to estimate the association between LHD policy and prevention and SUD-related ED visits, respectively. Model 1 controlled for individual characteristics, and Model 2 controlled for individual and contextual factors. In addition, fixed effects of hospital identifiers were controlled in both models. Montgomery County health department had missing data on SUD-related policy involvement. Hence, in the estimation of the LHD policy effect, data from Montgomery County were not included.
Sensitivity analyses, including step-wise regression with different covariates and fixed- versus random-effect models, were used to test the robustness of our results. Since Calvert County Health Department did not report its total expenditures, we excluded this variable from the main analyses. We ran the analyses again including the expenditures variable (and by so doing, excluding all ED visits from patients residing in Calvert County) and found similar results, which are available upon request.
The total sample consisted of 1,642,429 ED visits of adults (ages >=18) presenting to an ED in Maryland in 2012. We use Stata version 13 (StataCorp, College Station, Texas) for all analyses. Because this study involved only secondary data analysis, it was exempt from Institutional Review Board (IRB) consideration at our institution.
RESULTS
Of our total sample of 1,642,429 ED visits, 288,920 (17.59%) had an SUD-related diagnosis (Table 1). Among patients who had an SUD-related ED visit, 90% of them lived in a county where the LHD had been involved in SUD policy implementation in the past 2 years, and 73% of them lived in a county where LHD provided SUD preventive services. Among patients who did not have an SUD-related ED visit, 94% of them lived in a county where LHD had been involved in SUD policy implementation in the past 2 years, and 66% of them lived in a county where LHD provided SUD preventive services.
Table 1:
Comparisons of LHD activities, patient characteristics, and contextual factors by SUD-related and non SUD-related ED Visits in the State of Maryland in 2012
| Variable | SUD-related ED Diagnosis | ||
|---|---|---|---|
| Yes (n= 288,920) | No (n= 1,353,509) | p-value | |
| LHD Activities | |||
| LHD Involved in SUD Policy in the Past 2 Years | 0.90 | 0.94 | < 0.001 |
| LHD Provided SUD Preventive Services in the Past Year | 0.73 | 0.66 | < 0.001 |
| Individual Characteristics | |||
| Female (%) | 47.97 | 61.46 | < 0.001 |
| Age | 39.79 | 44.25 | < 0.001 |
| Race/Ethnicity | |||
| White (%) | 58.07 | 44.47 | < 0.001 |
| African American (%) | 37.53 | 47.01 | < 0.001 |
| Latino (%) | 2.47 | 4.29 | < 0.001 |
| Other Race (%) | 1.94 | 4.23 | < 0.001 |
| Insurance | |||
| Medicare (%) | 12.40 | 19.88 | < 0.001 |
| Medicaid (%) | 36.17 | 24.06 | < 0.001 |
| Private Insurance (%) | 23.85 | 36.29 | < 0.001 |
| Uninsured (%) | 24.53 | 15.70 | < 0.001 |
| No Charge (%) | 0.80 | 0.79 | < 0.001 |
| Other Payer (%) | 2.26 | 3.28 | < 0.001 |
| LHD Characteristics | |||
| Full Time Employees (count) | 461.65 | 494.14 | < 0.001 |
| County Level Contextual Factors | |||
| Total Population (1,000s) | 458.24 | 555.44 | < 0.001 |
| Percent White (%) | 60.80 | 54.41 | < 0.001 |
| Percent African American (%) | 30.86 | 35.03 | < 0.001 |
| Percent Insured <65 (%) | 75.04 | 75.12 | < 0.001 |
| Percent Urban Population (%) | 83.74 | 87.10 | < 0.001 |
| Median Household Income ( $) | 62447.92 | 65189.39 | < 0.001 |
| Percent Employed (%) | 48.16 | 48.81 | < 0.001 |
| Percent No High School >=25 (%) | 8.92 | 8.75 | < 0.001 |
| Community Mental Health Centers (count) | 0.58 | 0.68 | < 0.001 |
| Federally Qualified Health Centers (count) | 9.18 | 9.19 | 0.55 |
| PCPs per 1,000 population (count) | 0.77 | 0.85 | < 0.001 |
| Specialists per 1,000 population (count) | 1.47 | 1.63 | < 0.001 |
| Hospitals (count ) | 6.26 | 7.01 | < 0.001 |
Data source: The National Association of County and City Health Officials (NACCHO) National Profile of Local Health Departments 2012; HCUP State Emergency Department Database (SEDD) data from the state of Maryland for 2012; Area Health Resource File 2013.
Table 2 shows that LHD involvement in SUD-related policy during the past 2 years was significantly associated with a decreased probability of having an SUD-related ED visit by 11 percentage points after controlling for individual characteristics (Model 1: OR=0.89, p<0.001) and 14 percentage points after controlling for individual and contextual factors (Model 2: OR=0.86, p<0.0001). Similar results were found for LHD SUD preventive services. LHD SUD prevention efforts were significantly associated with reduced SUD-related ED visits by 7 percentage points in Model 1 (OR=0.93, p<0.001). This reduction became non-significant after controlling for contextual factors (Model 2: OR=0.94, p=0.17).
Table 2:
Multivariate Logistic Regression Results Examining the Effect of LHD Activities on Probability of Having an SUD-Related ED Visit
| Model 1 | Model 2 | |||||||
|---|---|---|---|---|---|---|---|---|
| Variable | Policy | Prevention | Policy | Prevention | ||||
| OR | p | OR | p | OR | p | OR | p | |
| LHD activities | ||||||||
| Policy | 0.89 | 0.00 | 0.86 | 0.00 | ||||
| Prevention | 0.93 | 0.00 | 0.94 | 0.17 | ||||
| Individual Characteristics | ||||||||
| Age | 0.99 | 0.00 | 0.99 | 0.00 | 0.99 | 0.00 | 0.99 | 0.00 |
| Gender | ||||||||
| Female | 0.55 | 0.00 | 0.54 | 0.00 | 0.55 | 0.00 | 0.54 | 0.00 |
| Race | ||||||||
| White | reference | reference | reference | reference | ||||
| African American | 0.62 | 0.00 | 0.62 | 0.00 | 0.62 | 0.00 | 0.63 | 0.00 |
| Latino | 0.50 | 0.00 | 0.50 | 0.00 | 0.50 | 0.00 | 0.50 | 0.00 |
| Other | 0.43 | 0.00 | 0.44 | 0.00 | 0.43 | 0.00 | 0.45 | 0.00 |
| Insurance | ||||||||
| Uninsured | reference | reference | reference | reference | ||||
| Medicare | 0.45 | 0.00 | 0.45 | 0.00 | 0.45 | 0.00 | 0.45 | 0.00 |
| Medicaid | 1.05 | 0.00 | 1.04 | 0.00 | 1.04 | 0.00 | 1.04 | 0.00 |
| Private | 0.45 | 0.00 | 0.45 | 0.00 | 0.45 | 0.00 | 0.45 | 0.00 |
| No Charge | 1.03 | 0.33 | 0.98 | 0.42 | 1.02 | 0.36 | 0.98 | 0.39 |
| Other | 0.38 | 0.00 | 0.38 | 0.00 | 0.38 | 0.00 | 0.38 | 0.00 |
| LHD FTEs | 1.00 | 0.00 | 1.00 | 0.00 | 1.00 | 0.05 | 1.00 | 0.49 |
| Contextual Factors | ||||||||
| County Total Population in 1,000s | 1.00 | 0.51 | 1.00 | 0.20 | ||||
| % White | 0.99 | 0.04 | 0.99 | 0.19 | ||||
| % African American | 0.98 | 0.00 | 0.99 | 0.01 | ||||
| % Population <65 years who were insured | 1.01 | 0.03 | 1.00 | 0.68 | ||||
| % Urban Population | 1.00 | 0.55 | 1.00 | 0.00 | ||||
| Median Household Income | 1.00 | 0.00 | 1.00 | 0.19 | ||||
| % Employed | 0.99 | 0.16 | 1.01 | 0.18 | ||||
| % Population >=25 years old had no high school degree | 0.95 | 0.00 | 1.00 | 0.91 | ||||
| Number of Community Mental Health Centers | 0.98 | 0.71 | 1.11 | 0.00 | ||||
| Number of Federally Qualified Health Centers | 1.03 | 0.00 | 1.03 | 0.00 | ||||
| Number of Primary Care Physicians Per 1,000 county population | 1.40 | 0.04 | 1.03 | 0.81 | ||||
| Number of Specialists Per 1,000 county population | 0.79 | 0.01 | 0.88 | 0.09 | ||||
| Number of Hospitals | 1.00 | 0.98 | 0.99 | 0.26 | ||||
| Hospital Fixed Effect | Controlled | Controlled | Controlled | Controlled | ||||
Notes: Individual hospital ID was controlled in all models, but results not reported.
In the estimation of the effect of LHD policy on ED visits, data of Montgomery County were not included. Montgomery County Health Department did not report this measure in 2012.
Data source: The National Association of County and City Health Officials (NACCHO) National Profile of Local Health Departments 2012; HCUP State Emergency Department Database (SEDD) data from the state of Maryland for 2012; Area Health Resource File 2013
Several covariates were significant predictors in all regression models. Racial minorities (African American, Latino, other) were less likely to have SUD-related ED visits, compared with Whites. Compared to uninsured populations, Medicaid enrollees were more likely to have SUD-related ED visits, and populations with private health insurance and Medicare were less likely to have SUD-related ED visits. An increase in number of specialists per 1,000 population was associated with a significant lower likelihood of having an SUD-related ED visit. Additionally, number of federally qualified health centers was associated with a significant increased probability of having an SUD-related ED visit.
LIMITATIONS
The study has some limitations. First, despite controlling for a wide range of individual and community characteristics, some confounding variables might be omitted due to data limitations and thus causal conclusions should be interpreted with caution.54 It is possible that LHDs in areas with fewer SUD-related issues had more resources to be involved with SUD-related policy and prevention; however, prior research has suggested a relationship between LHD interventions and community health outcomes.58, 59 Future studies on LHDs and use of EDs for SUD should also test these associations with longitudinal data sets to ensure temporal associations.
Secondly, measures of LHD activities were self-reported and measured by yes or no. Thus, we were not able to observe the level of LHD effort in each activity, which would be critical to assess in future work.
Third, our study was limited to 2012 data and the associations identified may not fully generalize to more recent years. However, this is a rich dataset and is consistent with other recent work. For example, two recently published studies examined the impact of LHD activities on preventable hospitalizations54 and avoidable readmissions55 using years HCUP data years 2012–2013. Since data from 2015/16 is now available for both substance use5–7 and HCUP data, future work should link additional years of data to examine LHD impact over time. Lastly, we limited our analysis to Maryland data; since LHD activities vary from state to state, more research is needed to understand whether local health departments across the United States are able to impact SUDs.
DISCUSSION
LHDs’ SUD activities have the potential to play an important role in addressing SUD in the community. In particular, our findings suggest that LHDs active involvement in SUD-related policy implementation can potentially reduce SUD-related ED visits by about 14 percentage points. Our findings suggest that LHDs may be optimally positioned to improve community behavioral health.
The Maryland Department of Health and Mental Hygiene has instituted a number of practices and approaches to support local health departments’ ability to improve health, including the creation of Maryland Health Enterprise Zones and the development of the Maryland State Health Improvement Process.50 Both the Health Enterprise Zones as well as the State Health Improvement Process have goals related to improving behavioral health, including comprehensive screening for depression in clinical encounters, as well as action steps to decrease alcohol related fatalities, drug-induced deaths, and Emergency Department visits for Mental Health or Addition-Related Conditions. LHDs play an active role in this model. Our findings suggest that it is critical to engage LHDs in integrated behavioral health care in Maryland and in the United States as a whole.
CONCLUSION
Our findings are also consistent with the literature on behavioral health integration model proposed by HRSA and SAMHSA51–52 and the newly released strategic objective of the National Institute of Mental Health (NIMH), to strengthen the public heath impact of NIMH’s work.32 Our findings suggest that LHDs can likely contribute to improve treatment for SUDs through policy implementation and potentially through provision of preventive care. We speculate that compared to other community interventions, programs implemented through LHDs can better reflect community health needs, be more sustainable, and are more likely to gain patient trust. In a recent conceptual framework developed by Chen and colleagues,53 LHDs are positioned to play a leadership role in a patient-centered health care system.
Our results also showed that LHDs’ provision of SUD preventive services could reduce ED visits by 7 percent after controlling for individual characteristics. The reduction decreased to 6 percent and became insignificant after controlling for individual and contextual factors. These results do not rule out the possible importance of LHD’s provision of SUD preventive services as it is seems that preventive services were implemented by LHDs in counties as a response to a high rate of SUD. Thus, it may take a number of years for these services to have a significant impact on ED visits. Longitudinal analysis over a longer period of time and more precise measures of preventive services will be needed to estimate the full impact of LHD services on ED use in the future.
IMPLICATIONS
Results of this study help us understand the extent to which LHD activities can affect SUD-related ED visits and provide a foundation for future study to identify effective LHD interventions that can promote integrated behavioral health care. Improving behavioral health prevention and treatment through integrated health care system, especially among vulnerable populations, is a major goal of the Substance Abuse and Mental Health Services Administration (SAMHSA),51 and the National Institute of Mental Health recently released Strategic Research Priorities (2017) which states the NIMH will work to “Develop innovative service delivery models to improve dramatically the outcomes of mental health services received in diverse communities and populations”.32 Our results are timely to inform the critical role of LHDs in emerging health policy initiatives under the SAMHSA-HRSA Integrated Care Model.51 Findings of this study can inform future research to further explore the complex political and financial relationships between LHDs, community health centers, state government, and other public health system components.
AUTHORS AND BIOGRAPHICAL SKETCHES
Biographical Sketch: Ms. Novak is a doctoral student at the University of Maryland at College Park. Her research focuses on using quantitative methods to analyze health disparities, expenditures, and quality of care among people living with dual diagnosis of type 2 diabetes and major depressive disorder. She holds a Master of Public Health Degree from George Mason University.
Biographical Sketch: Dr. Bloodworth is a recent graduate of the University of Maryland at College Park, where her research focused on the use of preventive services before and after the expansion of the Affordable Care Act made specific preventive services available to consumers with no out of pocket costs. She is currently employed by the Patient Centered Outcomes Research Institute where she works in the division of portfolio analysis. She holds a Doctor of Public Health (PhD) from University of Maryland and an MPH from the University of Memphis.
Biographical Sketch: Dr. Green is an associate professor in the Department of Health Services Administration at the School of Public Health, University of Maryland at College Park. Dr. Green’s work has concentrated on improving the health and well-being of disadvantaged populations. Specifically, her research has focused on identifying the causes of negative outcomes over the life course among urban African Americans. Dr. Green’s work is concentrated in two areas: (1) long-term consequences of substance use and (2) the interrelationship of substance use, violence, and mental health over the life course.
Biographical Sketch: Dr. Jie Chen is an associate professor in the Department of Health Services Administration at the School of Public Health, University of Maryland at College Park. Dr. Chen’s research fields include (1) health care disparities; (2) health care delivery system and policy; (3) behavioral health; and (4) economic evaluation. Her work uses a multidisciplinary perspective and involves collaboration with clinical leaders, community partners, and organizational decision makers.
Footnotes
CONFLICT OF INTEREST
The authors declare no conflicts of interest. Ms. N wishes to disclose that she is an employee of the Agency for Healthcare Research and Quality (AHRQ). Dr. B wishes to disclose that she is an employee of the Patient-Centered Outcomes Research Institute (PCORI). The opinions expressed in this manuscript are those of the authors and do not necessarily reflect the opinions or positions of AHRQ, PCORI, or of the US Federal government.
Contributor Information
Priscilla Novak, Department of Health Services Administration , School of Public Health, University of Maryland, College Park, MD, Also Agency for Healthcare Research and Quality (employee), pnovak1@umd.edu, Cell: (571) 201-5165.
Robin Bloodworth, Department of Health Services Administration , School of Public Health, University of Maryland College Park, MD Also Patient Centered Outcomes Research Institute (employee).
Kerry Green, Department of Behavioral and Community Health , School of Public Health, University of Maryland, College Park, MD.
Jie Chen, Department of Health Services Administration , School of Public Health, University of Maryland, College Park, MD.
References
- 1.Substance Abuse and Mental Health Services Administration. Behavioral health barometer: United States, 2013 U.S. Department of Health and Human Services. HHS Publication No. SMA-13–4796; 2013. [Google Scholar]
- 2.National Institute on Drug Abuse. Comorbidity: Addition and other mental Illness Research Report Series. 2010. Available at: http://www.drugabuse.gov/sites/default/files/rrcomorbidity.pdf. Accessed September 7, 2017. [Google Scholar]
- 3.Mancuso D, Shah M, Huber A, Felver B. The health impact of substance abuse: Accelerating disease progression and death Report to The Washington State Department of Social and Health Services, Aging and Disability Services Administration, Division of Behavioral Health and Recovery; 2011.
- 4.Wu ZH, Temple JR, Shokar NK, Nguyen-Oghalai TU, Grady JJ. Differential racial/ethnic patterns in substance use initiation among young, low-income women. Am. J. Drug Alcohol Abuse. 2010;36(2):123–9. [DOI] [PubMed] [Google Scholar]
- 5.Schmidt LA, Ye Y, Greenfield TK, Bond J. Ethnic disparities in clinical severity and services for alcohol problems: results from the National Alcohol Survey. Alcohol ClinExpRes. 2007; 31(1): 48–56. [DOI] [PubMed] [Google Scholar]
- 6.Wells K, Klap R, Kolke A, Sherbourne C. Ethnic disparities in unmet need for alcoholism, drug abuse, and mental health care. Am J Psychiatry. 2001; 158(12): 2027–32. [DOI] [PubMed] [Google Scholar]
- 7.Wallace JM Jr. The social ecology of addiction: race, risk, and resilience. Pediatrics. 1999;103:1122–7. [PubMed] [Google Scholar]
- 8.Feinberg ME, Ridenour TA, Greenberg MT. Aggregating indices of risk and protection for adolescent behavior problems: the Communities That Care Youth Survey. J Adolesc Health. 2007; 40(6):506–13. [DOI] [PubMed] [Google Scholar]
- 9.Kumpfer KL, Olds DL, Alexander JF, Zucker RA, Gary LE. Family etiology of youth problems. In: Ashery RS, Robertson EB, and Kumpfer KL, eds. Drug Abuse Prevention Through Family Interventions NIDA Research Monograph No. 177. Washington, DC: U.S. Government Printing Office; 1998: 42–77. [Google Scholar]
- 10.National Institute on Drug Abuse. Drug abuse is preventable; 2007. Available at: http://www.drugabuse.gov/publications/topics-in-brief/drug-abuse-prevention Accessed October 7, 2017.
- 11.Gerstein DR, Green LW. eds. Preventing drug abuse: What do we know? Washington, DC: National Academy Press; 1993. [PubMed] [Google Scholar]
- 12.Hansen WB, Giles SM, Fearnow-Kenney MD. Improving prevention effectiveness. Greensboro, NC: Tanglewood Research, 2000. [Google Scholar]
- 13.Wills TA, Vaccaro D, Mcnamara G, Hirky AE. Escalated substance use: a longitudinal grouping analysis from early to middle adolescence. J Abnorm Psychol. 1996;105(2):166–80. [DOI] [PubMed] [Google Scholar]
- 14.Hawkins JD, Catalano RF, Miller JY. Risk and protective factors for alcohol and other drug problems in adolescence and early adulthood: implications for substance abuse prevention. Psychol Bull. 1992;112(1):64–105. [DOI] [PubMed] [Google Scholar]
- 15.Feinstein EC, Richter L, Foster SE. Addressing the critical health problem of adolescent substance use through health care, research, and public policy. J Adolesc Health. 2012;50(5):431–6. [DOI] [PubMed] [Google Scholar]
- 16.Sturm R, Gresenz C, Sherbourne C, Minnium K, Klap R, Bhattacharya J, Farley D, Young AS, Audrey Burnam M, Wells KB. The design of healthcare for communities: A study of health care delivery for alcohol, drug abuse, and mental health conditions. Inquiry. 1999; 36(2): 221–33. [PubMed] [Google Scholar]
- 17.Chou CP, Montgomery S, Pentz MA, et al. Effects of a community-based prevention program on decreasing drug use in high-risk adolescents. Am J Public Health. 1998;88(6):944–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hawkins JD, Catalano RF, Arthur MW. Promoting science-based prevention in communities. Addict Behav. 2002;27(6):951–76. [DOI] [PubMed] [Google Scholar]
- 19.Kelly SM, O’grady KE, Schwartz RP, Peterson JA, Wilson ME, Brown BS. The relationship of social support to treatment entry and engagement: the Community Assessment Inventory. Subst Abus. 2010;31(1):43–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ashery RS, Robertson EB, Kumpfer KL, eds. Drug abuse prevention through family interventions NIDA Research Monograph No. 177. Washington, DC: U.S. Government Printing Office, 1998. [Google Scholar]
- 21.Dishion TJ, Mccord J, Poulin F. When interventions harm. Peer groups and problem behavior. Am Psychol. 1999;54(9):755–64. [DOI] [PubMed] [Google Scholar]
- 22.Dishion TJ, Kavanagh K, Schneiger A, Nelson S, Kaufman NK. Preventing early adolescent substance use: a family-centered strategy for the public middle school. Prev Sci. 2002;3(3):191–201. [DOI] [PubMed] [Google Scholar]
- 23.Spoth RL, Redmond C, Trudeau L, Shin C. Longitudinal substance initiation outcomes for a universal preventive intervention combining family and school programs. Psychol Addict Behav. 2002;16(2):129–34. [PubMed] [Google Scholar]
- 24.Aos S, Phipps P, Barnoski R, Lieb R. The comparative costs and benefits of programs to reduce crime. Volume 4 (1–05–1201). Olympia, WA: Washington State Institute for Public Policy; 2001. [Google Scholar]
- 25.Brown TT, Martinez-gutierrez MS, Navab B. The impact of changes in county public health expenditures on general health in the population. Health Econ Policy Law. 2014;9(3):251–69. [DOI] [PubMed] [Google Scholar]
- 26.Ingram RC, Scutchfield FD, Charnigo R, Riddell MC. Local public health system performance and community health outcomes. Am J Prev Med. 2012;42(3):214–20. [DOI] [PubMed] [Google Scholar]
- 27.Mays GP, Smith SA. Evidence links increases in public health spending to declines in preventable deaths. Health Aff (Millwood). 2011;30(8):1585–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Grembowski D, Bekemeier B, Conrad D, Kreuter W. Are local health department expenditures related to racial disparities in mortality?. Soc Sci Med. 2010;71(12):2057–65. [DOI] [PubMed] [Google Scholar]
- 29.Chen J, Bloodworth R, Novak P, Le Cook B, Goldman H, Rendall M, Thomas S, Reynolds CF III, Reducing Preventable Hospitalization and Disparity: Association With Local Health Department Mental Health Promotion Activities. Am J Prev Med (In Press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Erwin PC, Greene SB, Mays GP, Ricketts TC, Davis MV. The association of changes in local health department resources with changes in state-level health outcomes. Am J Public Health. 2011;101(4):609–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rodriguez HP, Chen J, Owusu-edusei K, Suh A, Bekemeier B. Local public health systems and the incidence of sexually transmitted diseases. Am J Public Health. 2012;102(9):1773–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Levi J K D Funding For Local Public Health: A Renewed Path For Critical Infrastructure. 2017; http://healthaffairs.org/blog/2017/08/22/funding-for-local-public-health-a-renewed-path-for-critical-infrastructure/. Accessed October 20, 2017.
- 33.Upton FHR 6 – 21st Century Cures Act. 2015; https://www.congress.gov/bill/114th-congress/house-bill/6 Accessed on October 20, 2017.
- 34.Lewis VA, Colla CH, Tierney K, Van citters AD, Fisher ES, Meara E. Few ACOs pursue innovative models that integrate care for mental illness and substance abuse with primary care. Health Aff (Millwood). 2014;33(10):1808–16. [DOI] [PubMed] [Google Scholar]
- 35.The National Institute of Mental Health. The National Institute of Mental Health Strategic Plan September 2017. Available at: https://www.nimh.nih.gov/about/strategic-planning-reports/strategic-research-priorities/index.shtml Accessed on October 20, 2017.
- 36.Centers for Disease Control. Public Health Action Plan to Integrate Mental Health Promotion and Mental Illness Prevention with Chronic Disease Prevention. Available at: http://www.cdc.gov/mentalhealth/docs/11_220990_Sturgis_MHMIActionPlan_FINAL-Web_tag508.pdf Accessed September 15, 2017.
- 37.Thomas SB, Fine MJ, Ibrahim SA. Health disparities: the importance of culture and health communication. Am J Public Health. 2004;94(12):2050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Derose KP, Gresenz CR, Ringel JS. Understanding disparities in health care access--and reducing them--through a focus on public health. Health Aff (Millwood). 2011;30(10):1844–51. [DOI] [PubMed] [Google Scholar]
- 39.Mays GP, Halverson PK, Baker EL, Stevens R, Vann JJ. Availability and perceived effectiveness of public health activities in the nation’s most populous communities. Am J Public Health. 2004;94(6):1019–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Luo H, Sotnikov S, Shah G. Local health department activities to ensure access to care. Am J Prev Med. 2013;45(6):720–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Scutchfield FD, Howard AF. Moving on upstream: the role of health departments in addressing socioecologic determinants of disease. Am J Prev Med. 2011;40(1 Suppl 1):S80–3. [DOI] [PubMed] [Google Scholar]
- 42.Birckmayer JD, Holder HD, Yacoubian GS, Friend KB. A general causal model to guide alcohol, tobacco, and illicit drug prevention: assessing the research evidence. J Drug Educ. 2004;34(2):121–53. [DOI] [PubMed] [Google Scholar]
- 43.Desilva M, Samele C, Saxena S, Patel V, Darzi A. Policy actions to achieve integrated community-based mental health services. Health Aff (Millwood). 2014;33(9):1595–602. [DOI] [PubMed] [Google Scholar]
- 44.Druss BG, Rosenheck RA. Patterns of health care costs associated with depression and substance abuse in a national sample. Psychiatr Serv. 1999;50(2):214–8. [DOI] [PubMed] [Google Scholar]
- 45.National Association of County and City Health Officials. Available at: http://www.naccho.org/topics/infrastructure/profile/upload/2013-National-Profile-of-Local-Health-Departments-report.pdf Accessed on January 12, 2015.
- 46.Cost Healthcare and Project Utilization (HCUP). State Emergency Department Databases. Available at: http://www.hcup-us.ahrq.gov/seddoverview.jsp.pdf Accessed on January 12, 2017.
- 47.Health Resources and Services Administration. Area Health Resources File. Available at: http://ahrf.hrsa.gov/ Accessed on April 10, 2015.
- 48.Coffey RM, Houchens R, Chu BC, Barrett M, Owens P, Stocks C, Vandivort-Warren R, Buck J, Emergency Department Use for Mental and Substance Use Disorders. Online August 23, 2010, U.S. Agency for Healthcare Research and Quality (AHRQ). Available at: http://www.hcup-us.ahrq.gov/reports.jsp Accessed on April 10, 2017.
- 49.United States Census Bureau. TIGER/Line® Shapefiles and TIGER/Line® Files. https://www.census.gov/geo/maps-data/data/tiger-line.html Accessed on April 10, 2017.
- 50.State Innovation Model. Maryland Department of Health and Mental Hygiene. Available at: http://hsia.dhmh.maryland.gov/SitePages/sim.aspx Accessed on September 7, 2017.
- 51.Substance Abuse and Mental Health Services Administration. SAMHSA Leading Change 2.0: Advancing the Behavioral Health of the Nation 2015 – 2018. U.S. Department of Health and Human Services.
- 52.The Four Quadrant Clinical Integration Model. Available at: http://www.integration.samhsa.gov/clinical-practice/four_quadrant_model.pdf Accessed on January 10, 2017.
- 53.Chen J, Mullins D, Novak P, Thomas S. Personalized Strategies to Activate and Empower Patients in Health Care and Reduce Health Disparities.Health Educ Behav. 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Chen J Bloodworth R, Novak P, Le Cook B, Goldman HH, Rendall MS… Reynolds CF 3rd (2018) Reducing Preventable Hospitalization and Disparity: Association With Local Health Department Mental Health Promotion Activities. Am J Prev Med, 54(1), 103–112. doi: 10.1016/j.amepre.2017.10.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Chen J, Novak P, Barath D, Goldman H, & Mortensen K (2018). Local Health Departments’ Promotion of Mental Health Care and Reductions in 30-Day All-Cause Readmission Rates in Maryland. Med Care, 56(2), 153–161. doi: 10.1097/MLR.0000000000000850 [DOI] [PubMed] [Google Scholar]
- 56.Hedegaard H, Warner M, Miniño AM. Drug overdose deaths in the United States, 1999–2016. NCHS Data Brief, no 294. Hyattsville, MD: National Center for Health Statistics; 2017. https://www.cdc.gov/nchs/products/databriefs/db294.htm [Google Scholar]
- 57.Weiss AJ, (IBM Watson Health), Bailey MK, (IBM Watson Health), O’Malley L, (IBM Watson Health), Barrett ML, (M.L. Barrett, Inc.), Elixhauser A, (AHRQ), Steiner CA, (Institute for Health Research, Kaiser Permanente). Patient Residence Characteristics of Opioid-Related Inpatient Stays and Emergency Department Visits Nationally and by State, 2014. HCUP Statistical Brief #226. July 2017. Agency for Healthcare Research and Quality, Rockville, MD: www.hcup-us.ahrq.gov/reports/statbriefs/sb226-Patient-Residence-Opioid-Hospital-Stays-ED-Visits-by-State.pdf. [Google Scholar]
- 58.Purtle J, Peters R, Kolker J, Klassen AC. Factors Perceived as Influencing Local Health Department Involvement in Mental Health. Am J Prev Med. 2017;52(1):64–73 Fuller RL, Atkinson G, Mccullough EC, Hughes JS. Hospital readmission rates: the impacts of age, payer, and mental health diagnoses. J Ambul Care Manage. 2013;36(2):147–55. [DOI] [PubMed] [Google Scholar]
- 59.Shah GH, Sheahan JP. Local Health Departments’ Activities to Address Health Disparities and Inequities: Are We Moving in the Right Direction?. Int J Environ Res Public Health. 2015;13(1):ijerph13010044. [DOI] [PMC free article] [PubMed] [Google Scholar]