Abstract
Purpose.
Conduct a systematic umbrella review to evaluate the relationship of physical activity (PA) with all-cause mortality, cardiovascular mortality, and incident cardiovascular disease; to evaluate the shape of the dose-response relationships; and to evaluate these relationships relative to the 2008 Physical Activity Guidelines Advisory Committee (PAGAC) Report.
Methods.
Primary search encompassing 2006 – March, 2018 for existing systematic reviews, meta-analyses, and pooled analyses reporting on these relationships. Graded the strength of evidence using a matrix developed for the PAGAC.
Results.
The association of self-reported moderate-to-vigorous physical activity (MVPA) on all-cause mortality, cardiovascular disease (CVD) mortality, and atherosclerotic cardiovascular diseases — including incident coronary heart disease, ischemic stroke and heart failure — are very similar. Increasing MVPA to Guidelines amounts in the inactive U.S. population has the potential to have an important and substantial positive impact on these outcomes in the adult population. The following points are clear: the associations of PA with beneficial health outcomes begin when adopting very modest (one-third of Guidelines) amounts; any MVPA is better than none; meeting the 2008 PA guidelines reduces mortality and CVD risk to about 75 percent of the maximal benefit obtained by physical activity alone; PA amounts beyond Guidelines recommendations amount reduces risk even more, but greater amounts of PA are required to obtain smaller health benefits; and there is no evidence of excess risk over the maximal effect observed at about three to five times the amounts associated with current guidelines. When PA is quantified in terms of energy expenditure (MET-hours per week), these relationships hold for walking, running, and biking.
Conclusions.
To avoid the risks associated with premature mortality and the development of ischemic heart disease, ischemic stroke, and all-cause heart failure, all adults should strive to reach the 2008 Physical Activity Guidelines for Americans.
Keywords: all-cause mortality, cardiovascular mortality, cardiovascular disease, heart failure, stroke
INTRODUCTION
The 2008 Physical Activity Guidelines Advisory Committee Report concluded that the amount of moderate-to-vigorous physical activity obtained per week is inversely associated with all-cause mortality, cardiovascular disease (CVD) mortality, and incident CVD (1). The 2008 Physical Activity Guidelines (PAG) for Americans recommended a target range that could be achieved by 150 to 300 minutes per week of moderate-intensity physical activity, 75 to 150 minutes of vigorous physical activity, or an equivalent volume from a combination of moderate and vigorous physical activity (2). All of the dose-response data used to develop the physical activity targets for the 2008 Physical Activity Guidelines were developed using epidemiologic data from longitudinal cohort studies—with moderate-to-vigorous aerobic physical activity as the lone physical activity exposure. Unfortunately, little literature has appeared addressing the influence of strength or resistance training on these outcomes; this continues to be a significant limitation of the field.
In 2008, the Advisory Committee relied mostly on primary literature to perform its work regarding all-cause mortality, CVD mortality, and CVD. Since then, there have continued to be published studies on the relationship of moderate-to-vigorous physical activity to these outcomes. In 2008, the assessment of CVD as an outcome was principally limited to coronary artery disease. Since then, meta-analyses have been published on additional cardiovascular outcomes, including incident cerebrovascular disease—primarily ischemic stroke—and incident heart failure. In addition, now available is a large volume of studies, reviews, pooled analyses, and meta-analyses with many component studies and large sample sizes on the relationship of moderate-to-vigorous physical activity with all-cause mortality, CVD mortality, and CVD. The abundance of meta-analyses permitted the members of the 2018 Physical Activity Guidelines Advisory Committee (Committee) to solely use meta-analyses to perform an updated review of the literature on this topic.
In 2008, the Advisory Committee began to define a dose-response relationship among moderate-to-vigorous physical activity and both all-cause and CVD mortality as a curvilinear one, with an early decrease in risk with greater amounts of moderate-to-vigorous physical activity, and with continuing benefit through obtaining greater amounts of physical activity. While undertaking the current review, the Committee believed it was important to confirm whether this relationship still holds with new data, and whether it extends to the various CVD outcomes of incident CVD, cerebrovascular disease (ischemic stroke), and incident heart failure.
For the 2018 Physical Activity Guidelines Advisory Committee Report (3), the Committee chose to address update and expand upon the 2008 Report (1): by address the relationships of physical activity and 1) all-cause mortality; 2) cardiovascular disease mortality; and 3) incident cardiovascular disease. In this new report we address stroke and heart failure for the first time. Specifically, for each of these outcomes, the Committee was interested in whether there is a dose-response relationship; what is the shape of the relationship; and does the relationship vary by age, sex, race/ethnicity, socioeconomic status, or weight status? The Committee was also interested in compiling data within this framework on whether new cardiovascular disease syndromes—for instance, heart failure and ischemic stroke—had enough new data to make statements about the relationships to physical activity. Finally, the Committee was interested in understanding whether the relationships of physical activity to disease outcomes might be modified from 2008, based upon the fact that our lives are becoming increasingly sedentary.
METHODS
The overarching methods used to conduct systematic reviews informing the 2018 Physical Activity Guidelines Advisory Committee Scientific Report have been described in detail elsewhere (3, 4). An umbrella systematic review was conducted to identify studies investigating the association between all types and intensities of physical activity and the health outcomes of interest: all-cause mortality, cardiovascular disease mortality, or cardiovascular disease incidence. Studies were restricted to those in adults and addressing mortality and disease incidence. An umbrella review is in essence a review of meta-analyses; there is no formal means yet developed to perform meta-analyses of meta-analyses. The searches for meta-analyses addressing our questions were conducted in electronic databases (PubMed®, CINAHL, and Cochrane). One search and triage process was conducted for these three outcomes. Studies were considered eligible if they were systematic reviews, meta-analyses or pooled analyses published in English from 2006 until March 2018. The titles, abstracts, and full-text articles of the identified articles were independently screened by two reviewers. Disagreement between reviewers was resolved by discussion with a third member of the Committee, when necessary. Two independent abstractors extracted relevant data from all the studies eligible at full text triage to minimize abstraction errors. Abstractors also used a tailored version of AMSTARExBP to grade the quality of the reviews and select them for analysis (5). The full search strategies and AMSTARExBP grading assessments for our three questions are available at the Physical Activity Guidelines web site: https://health.gov/paguidelines/second-edition/report/supplementary-material.aspx. The review was registered in PROSPERO #CRD42018092743.
RESULTS
Physical Activity and All-cause Mortality.
A literature tree summarizing the selection of systematic reviews, meta-analyses, and pooled analyses for this outcome is contained in Supplementary Digital Content (see Figure, SDC 1, literature search tree for all-cause mortality). The Committee determined that the initial umbrella search identified sufficient literature to answer the primary research questions. Additional searches for original research were not needed.
Articles collected from 2006 to 2017 often assessed each of the three outcomes of all-cause mortality, CVD mortality, and incident CVD. Therefore, the systematic reviews and meta-analyses contributing to the understanding of the relation of physical activity to these three outcomes had significant overlap. Similarly, many of the same studies appeared in the systematic reviews and meta-analyses identified in our searches. One additional article was identified in a supplemental search from 2017 to April 2018.
A total of 13 reviews were included in the analysis of the relation of physical activity to all-cause mortality: 2 systematic reviews (6, 7), 7 meta-analyses (8–14), and 4 pooled analyses (15–18). Follow-up for these studies ranged from 3.8 to more than 20 years, and up to 3.9 million participants in total were studied across these reviews and meta-analyses.
The two systematic reviews included a large number of contributing studies: 121 (6) and 254 (7). However, in Milton et al. (4), only seven addressed all-cause mortality, nine addressed CVD, and three addressed stroke. For Warburton (5), 70 component studies addressed all-cause mortality, 49 addressed CVD, and 25 addressed stroke. The total numbers for each outcome were not reported. The studies covered extensive timeframes: from 1990 to 2013 and from 1950 to 2008, respectively.
The meta-analyses ranged from 9 to 80 studies. Most meta-analyses covered an extensive timeframe: from inception of the database to one year before publication (8, 10, 13, 14), from 1945 to 2013 (11), and from the 1960s and 1970s to 2007 and 2006 (9, 12). Three of the pooled analyses included data from six prospective cohort studies ((15, 17) used the same six studies) and from 11 cohorts (18). The pooled analysis from the Asia Cohort Consortium (14) included nine cohort studies, with 467,729 East Asians who experienced 65,858 deaths over a mean follow-up period of 13.6 years. Incident ischemic heart disease and stroke were also assessed.
The majority of the included reviews examined self-reported leisure time moderate-to-vigorous physical activity as determined at face value in the contributing papers. Most reviews also established specific physical activity dose categories in metabolic equivalents of task (MET) for minutes or hours per week using quartiles or a variety of categories such as inactive and low, medium, and high amounts of physical activity, or high versus low amounts of physical activity.
Three reviews addressed specific types of physical activity. Kelly et al. (11) studied cycling and walking. Samitz et al. (13) studied domain-specific physical activity defined into leisure-time physical activity, activities of daily living, and occupational physical activity. Hamer and Chida (9) studied habitual walking only.
One pooled analysis (18) separately examined individuals meeting the 2008 physical activity guidelines — of 150 minutes of moderate, 75 minutes per week of vigorous or some equivalent combination — in one or two sessions in addition to the usual physical activity categories (inactive, insufficiently active, and regularly active). Merom et al. (19) examined dance versus walking.
Evidence on the Overall Relationship.
All the included reviews addressed all-cause mortality as an outcome; five of them also examined CVD mortality. All studies reported an inverse relationship between moderate-to-vigorous physical activity and all-cause mortality in a dose-response fashion as described below. There were no null studies. The pooled analysis in which individuals meeting guidelines in one or two sessions per week (so-called “weekend warrior”) and individuals meeting guidelines with three or more sessions per week were compared to an inactive group, showed no differences in the effect sizes for all-cause mortality. Compared with the inactive participants, the hazard ratio (HR) for all-cause mortality was 0.66 (95%CI, 0.62–0.72) in insufficiently active participants who reported 1 to 2 sessions per week, 0.70 (95%CI, 0.60–0.82) in weekend warrior participants, and 0.65 (95%CI, 0.58–0.73) in regularly active participants. (18).
In the analysis by Kelly et al. (11), the effect sizes for cycling and walking were similar. For exercise of 11.25 MET-hours per week (675 MET-minutes per week), the reduction in relative risk for all-cause mortality was 11 percent (95% CI: 4%−17%) for walking and 10 percent (95% CI: 6%−13%) for cycling. The shape of the dose-response relationship was modeled through meta-analysis of pooled relative risks within three exposure intervals. Consistent with other studies, the dose-response analysis showed that for walking or cycling, the greatest relative risk for all-cause mortality reduction relative to the next lower physical activity amount occurred for those with the least amounts of physical activity.
Hamer and Chida (9) studied the association of walking only with both all-cause mortality and CVD mortality. The analysis included 18 prospective studies with 459,833 total participants. The forest plots, displayed in Figure 1, show a dose-response for amount (volume of walking) and walking pace. Hamer and Chida (9) found walking pace to be a stronger independent predictor of all-cause mortality than volume when both pace and volume were in the model: 48 percent versus 26 percent risk reductions, respectively. However, the studies had considerable heterogeneity within the exposure categories. The greatest walking exposure groups averaged more than 5.2 hours per week or more than 10.7 miles per week, and the groups ranged from more than 1 hour per week to more than 2 hours per day and more than 6.0 miles per week to more than 12.4 miles per week. Walking pace was generally assessed as a “relative’’ rather than an ‘‘absolute’’ measure (relative being defined in terms such as “brisk” which may be different in absolute terms—e.g., miles per hour—for those of different ages and fitness levels), although several studies defined ‘‘brisk’’ as more than 3.0 miles per hour and ‘‘moderate’’ as 2.0 to 2.9 miles per hour. Minimal walking categories averaged approximately 3 hours per week (ranging from ~30 minutes per week to ~5 hours per week) or 6.1 miles per week (ranging from ~ 3.1 miles per week to ~9.3 miles per week), equating to a casual or moderate walking pace of approximately 2 miles per hour.
Figure 1. The Association Between Walking and All-Cause Mortality in Men and Women.
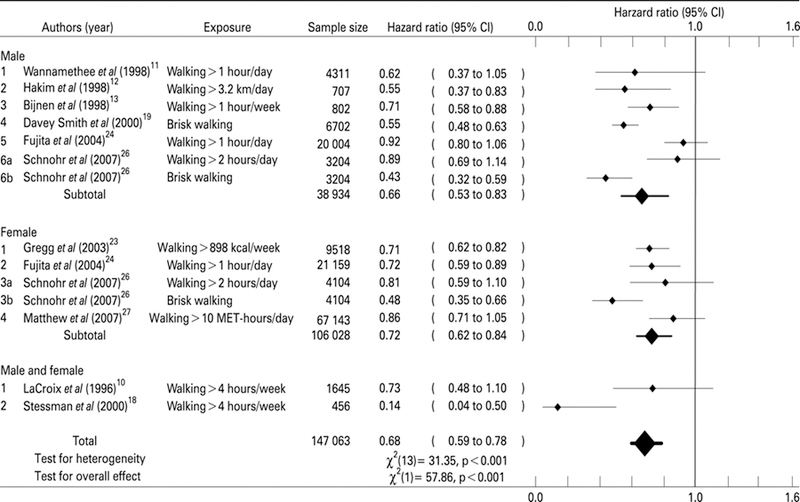
Source: M Hamer, and Y Chida, 2008 (9). Forest plot showing point and 95% confidence interval estimates of the HR for all-cause mortality associated with different amounts of PA. Relative influence on the pooled results/effect sizes are represented by varying line weights of the symbols. Walking is favored, with a shift of the estimate to the left. These estimates are similar to the associations found for CVD mortality discussed later.
Dose-response:
Every one of the 13 studies within our analysis demonstrated a significant inverse dose-response relationship with all-cause mortality across physical activity exposure groups. The uniformity and strength of these relationships led to the strength of evidence grade finding for this item. The uniformity of findings prompted us to highlight the two pooled analyses of Arem et al. (15) and Moore et al. (17). In these pooled analyses of six studies, combining data at the individual level allowed an examination of the strength of effects and confidence boundaries across large populations with great precision.
Moore et al. (17) reported a pooled analysis of the association of leisure-time physical activity with mortality during follow-up in data from six prospective cohort studies in the National Cancer Institute Cohort Consortium. The pooled cohort included 654,827 individuals, ages 21 to 90 years. Moderate-to-vigorous physical activity in MET-hours per week was used to generate adjusted survival curves (for participants ages 40 years and older), with 95% confidence intervals derived by bootstrap. The study included a median follow-up of 10 years and 82,465 deaths. Figure 2 shows the relation of leisure time physical activity and hazard ratios for mortality; it illustrates several characteristics of the relationship common among the studies reporting on dose-response on all-cause mortality. The survival curve from this analysis demonstrates several important points: (1) the beneficial effect has no lowest threshold; (2) effects are seen immediately upon moving from the least active category to the next category of moderate-to-vigorous physical activity; (3) the early part of the slope is the steepest. At least 70 percent of the population benefit on all-cause mortality is reached by achieving 8.25 MET-hours (150 minutes) per week of moderate-to-vigorous physical activity; (4) there is no obvious best amount; (5) there is no apparent upper threshold; (6); (7) activity volumes (amounts) up to four times the 2008 Guidelines (150–300 minutes moderate-intensity physical activity), show no evidence of increased mortality risk.
Figure 2. Relationships of Moderate-to-Vigorous Physical Activity to All-Cause Mortality, with Highlighted Characteristics Common to Studies of This Type.
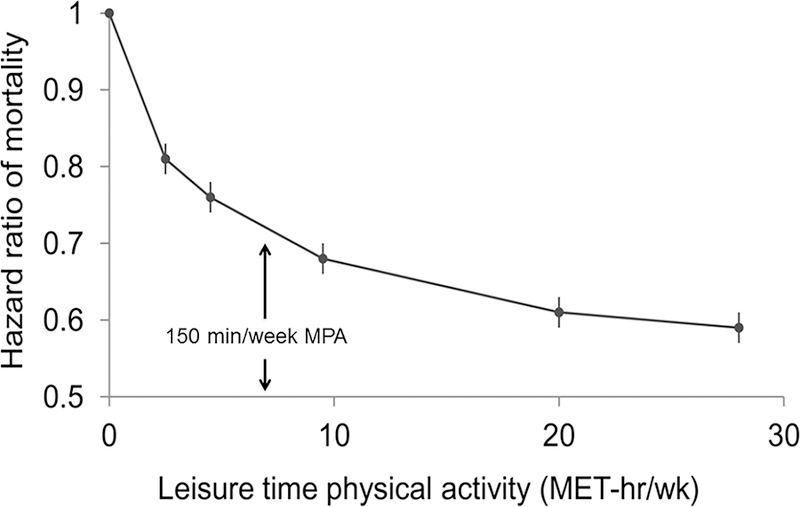
Source: adapted from Moore et al., 2012 (17). Shown is the relation of leisure time physical activity amount and hazard ratios for mortality. The points shown represent the mortality hazard ratio for each of the physical activity categories; the vertical lines represent the 95% CIs for that physical activity category. The reference category no leisure time physical activity. The lines connecting the points help to illustrate the dose–response relationship between physical activity and risk of mortality; the shape of the association shown here is similar to that obtained using spline modeling. As discussed in the text and displayed in this graphic, the characteristics of this curve seems to apply for most studies of the relationships of moderate-to-vigorous physical activity with all-cause and CVD mortality, as well as with incident coronary artery disease, ischemic stroke and all-cause heart failure: there is no lower threshold for effect; there is a steep, early slope; about 70% of the benefit obtained by physical activity alone is reached by 8.25 MET-h/w (150 minutes of “brisk walking” (3 miles per hour); there is not apparent upper threshold for effect; there is no evidence for increased risk at the greatest amounts of physical activity; and there is not obvious “best amount”.
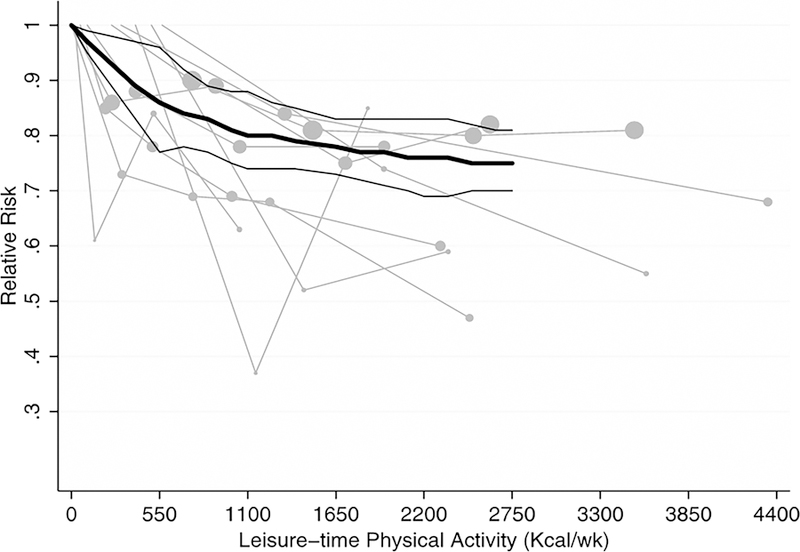
Similarly, Arem et al. (15) reported a pooled analysis of six studies in the National Cancer Institute Cohort Consortium (baseline collection in 1992–2003; the same studies reported in Moore et al. (17)). These were population-based prospective cohorts in the United States and Europe, with self-reported physical activity analyzed in 2014. A total of 661,137 men and women (median age, 62 years; range 21 to 98 years) and 116,686 deaths were included. Cox proportional hazards regression with cohort stratification was used to generate multivariable-adjusted hazard ratios and 95% CIs. Median follow-up time was 14.2 years. The dose response-relationship from this report is shown in Figure 3. Several characteristics of this dose-response relationship are reminiscent of that of Moore et al. (17) (Figure 2). However, several differences in results are described below.
Figure 3. Relationships of Moderate-to-Vigorous Physical Activity to All-Cause Mortality, with Highlighted Characteristics Common to Studies of This Type.

Source: adapted from Arem H et al., 2015 (15). The ranges of physical activity relative to 2008 US Physical Activity Guidelines for aerobic activity are shown as ranges. There is no increase in risk noted up to 10 times the current guidelines PA amounts.
Here the relationship is carried out to a category (>75 MET-hours per week) representing approximately ten times the exposure of the lower end of the 2008 Guidelines (i.e., 150 minutes per week). At the greatest exposure category, an apparent uptick in mortality risk occurs. This possible uptick is not noted in the Moore et al., 2012 study that went only to about four times the Guidelines exposure. In this pooled study of 661,137 individuals only 18,831 participants (2.8% of the total) were included in the 40 to 75 MET-hours per week category, and only 4,077 (0.62%) in the more than 75 MET-hours per week category. These accounted for only 1,390 (1.2%) and 212 (0.18%) of 116,686 deaths in the combined analysis, respectively; and the error bars are large. Figure 3 indicates that the point estimate of risk for the greatest exposure group is the same as the estimate for those meeting the 2008 Guidelines (7.5 to 15 MET-hours per week, or 150 to 300 minutes per week). This apparent uptick in risk at extreme volumes of exercise has been observed before. Paffenbarger (20, 21) reported it in the Harvard Alumni Health Study for CVD (heart attack) risk, in 1978 and 1993. However, as in these previous reports, the apparent rise in risk at very high amounts of moderate-to-vigorous physical activity did not reach the level of statistical significance (15).
In a seminal paper in 2016, Ekelund et al. (8) examined the joint associations of sedentary behaviour (sitting and television watching) and physical activity (moderate-to-vigorous physical activity) with all-cause mortality. (cf., Sedentary Behavior article in this issue.) Using 16 contributing studies, combining data across all studies to analyse the association of daily sitting time and physical activity with all-cause mortality, estimating summary hazard ratios using Cox regression, and expressing physical activity in terms of MET-hours per week of moderate-to-vigorous physical activity, Ekelund et al. found the same curvilinear relationships among physical activity and all-cause mortality as observed in Arem et al. (15) and Moore et al. for four categories of sitting time (17).
Demographic factors and weight status.
Most studies reported gross distributions of demographic factors (race, sex, weight status) across exposure groups within individual studies in their reviews and meta-analyses. Given the nature of meta-analyses—conducted at the study level versus the individual level—it is difficult to detect differential effects by demographic factors and weight status unless the specific component studies performed them within their analysis. Some studies examined subgroup effects directly in their review or meta-analysis; one focused on adults older than 60 years (10). In such studies, no subgroup effects were detected. The O’Donovan analysis of “weekend warrior” physical activity behavior on all-cause mortality, showed no differential responses by sex (18).
However, the pooled analyses (15, 17) permit a direct examination of the relative effects across demographic categories. In these studies effects were reported for strata across sex, race, and body mass index (BMI) and the aggregate event data reported according to strata. Although not directly tested in these reports, no differential effects across sex, race, or BMI strata were readily apparent. Strata for socioeconomic status and ethnicity were not reported.
Comparing 2018 Findings with the 2008 Scientific Report.
Our review of systematic reviews, meta-analyses, and pooled studies promoted the analysis of larger cohorts and provided more precision around the effect size estimates. Our review identified the same dose-effect estimates relating moderate-to-vigorous physical activity with all-cause mortality as was described in 2008. Given the large population sizes and heterogeneity studied, we have more confidence about the study effect sizes and dose response relationships (Figure 2) and their generalizability to U.S. adult men and women, and populations of all races, ages, and body sizes.
Physical Activity and Cardiovascular Disease Mortality.
A literature tree summarizing the selection of systematic reviews, meta-analyses, and pooled analyses for this outcome is contained in Supplementary Digital Content (see Figure, SDC 2, literature search tree for cardiovascular disease mortality). An initial search for systematic reviews, meta-analyses, pooled analyses, and reports identified sufficient literature to answer the research question as determined by the Committee. Additional searches for original research were not needed.
Articles collected from 2006 to 2017 typically included outcomes of all-cause mortality, CVD mortality, and incident CVD. Therefore, the systematic reviews and meta-analyses contributing to the understanding of the relation of physical activity to these three outcomes had significant overlap. Similarly, many of the same studies appeared in the systematic reviews and meta-analyses identified in our searches. In this section, we address only CVD mortality; however, the format and conclusions differ little from those made for all-cause mortality.
For this discussion, CVD mortality refers to mortality attributable to CVD in its broadest sense, referring to diseases beyond ischemic coronary artery disease, but not to include non-atheromatous or infectious valvular disease and others.
A total of six existing reviews were included: one systematic review (6), three meta-analyses (8, 9, 22), and two pooled analyses (18, 19). The reviews were published from 2008 to 2017. The systematic review (6) included 121 studies and a timeframe from 1983 to 2013. The meta-analyses included a range of 16 to 36 studies and covered an extensive timeframe: from 1970s to 2014. The pooled analyses included data from 20 cohorts, each from different population surveys (18, 19).
The majority of the included reviews examined self-reported leisure time moderate-to-vigorous physical activity. Most reviews also established specific physical activity dose categories in MET-minutes or MET-hours per week using quartiles or a variety of categories such as inactive and low, medium, and high levels of physical activity, or high versus low levels of physical activity.
One pooled analysis (18) examined a “weekend warrior” category (meeting the physical activity guidelines in one or two sessions per week) in addition to the usual physical activity categories (insufficiently active and regularly active) compared to an inactive group. Two reviews addressed specific types of physical activity: dancing (19) and habitual walking (9).
Evidence on the Overall Relationship.
All of the included reviews addressed CVD mortality and four of them also assessed all-cause mortality in addition to other outcomes. As it was for all-cause mortality, all reviews reported an inverse relationship between moderate-to-vigorous physical activity and CVD mortality in a dose-response fashion, as described below. The reviews included no null studies. The pooled analysis in which individuals meeting guidelines in one or two sessions per week and individuals meeting guidelines with three or more sessions per week were compared to an inactive group, showed no differences (overlapping hazard ratios) in the effect sizes for CVD mortality (HR 0.59 to 0.60) (16).
As noted above, Hamer and Chida (9) studied walking only on both all-cause mortality and CVD mortality. The analysis included 18 prospective studies with 459,833 total participants. The effect sizes and confidence intervals for all categories of walking pace and amount are similar to reminiscent of those determined for all-cause mortality (Figure 1). This is an example of how closely aligned the moderate-to-vigorous physical activity relationship is for both CVD mortality and all-cause mortality within and across studies.
Dose-response.
Here also, the findings for the dose-response relationships between moderate-to-vigorous physical activity and CVD mortality are basically identical to those found for the relationships between moderate-to-vigorous physical activity and all-cause mortality. Every one of the 13 studies within our analysis demonstrated a significant inverse dose-response relationship with CVD mortality across physical activity exposure groups. The uniformity and strength of these relationships led to the strength of evidence determination for this item. Wahid et al. (22) used 36 studies, 33 pertaining to CVD and 3 pertaining to type 2 diabetes mellitus to model the effects of three physical activity categories (low physical activity, 0.1–11.5 MET-hours per week; medium physical activity, 11.5–29.5 MET-hours per week; and high physical activity; ≥29.5 MET-hours per week) in a dose-response fashion on CVD incidence and mortality, coronary heart disease incidence and mortality, myocardial infarction incidence, heart failure incidence, and stroke incidence (22). For those conditions for which all three categories had entries (CVD incidence, CVD mortality, stroke incidence, and CHD incidence), all but CVD mortality demonstrated a strong curvilinear dose-response relationship across categories, as observed for all-cause mortality (Figure 2).
Demographic factors and weight status:
Similar to all-cause mortality, the studies providing the strongest evidence regarding subgroup moderation effects on CVD mortality were the pooled analyses of Merom et al. (19) and O’Donovan et al. (18). Again, as for all-cause mortality, although not directly tested in these reports, no differential effects across sex, race, or BMI strata were readily apparent. Strata for socioeconomic status and ethnicity were not reported.
Physical Activity and Incident Cardiovascular Disease.
Here cardiovascular disease refers to diseases related to ischemic vascular events, such as diseases due to coronary heart disease secondary to coronary artery disease, to cerebrovascular disease secondary to a cerebrovascular accident or stroke; or to heart failure of ischemic (coronary) or non-ischemic etiology.
A literature tree summarizing the selection of systematic reviews, meta-analyses, and pooled analyses for this outcome is contained in Supplementary Digital Content (see Figure, SDC 3, literature search tree for all-cause mortality). A total of 10 existing reviews were included: one systematic review (7) and nine meta-analyses (22–30). The reviews were published from 2008 to 2016. The systematic review (7) included 254 studies published between 1950 and 2008.
The meta-analyses included a range of 12 to 43 studies. Most meta-analyses covered an extensive timeframe: from database inception to 2013 (29), from 1954 and 1966 to 2007 (28, 30), and from the 1980s and 1990s to 2005–2016 (22–27).
The majority of included reviews examined self-reported physical activity. Different domains of physical activity were also assessed. These included total (25); occupational and leisure (24); occupational, leisure, and transport (27); and leisure physical activity only (28). Some reviews also established specific dose categories in MET-minutes or MET-hours per week (22, 25, 26, 30). Other reviews used minimal or low versus moderate or high physical activity levels as reported in individual studies (7, 23, 28). Two meta-analyses specifically examined tai chi chuan (29) and walking (30).
Included reviews addressed the incidence of CVD in a variety of ways. Several addressed incident coronary heart disease (25, 27, 28, 30), incident stroke (23, 25, 29), and incident heart failure (24, 26). Warburton et al. (7) reviewed incident stroke and coronary (ischemic) heart disease. Wahid et al. (22) used 33 studies to address CVD incidence and mortality, coronary heart disease incidence and mortality, myocardial infarction incidence, heart failure incidence, and stroke incidence. Thus, in all, six studies addressed incident coronary heart disease; five studies addressed incident stroke; and three studies addressed incident heart failure.
Evidence on the Overall Relationship.
All of the six studies addressing incident coronary heart disease, the five studies addressing incident stroke, and the three studies addressing incident heart failure demonstrated significant dose-response inverse relationships with increased amounts of physical activity. There were no null studies. The shapes of the relationships are discussed below.
Physical Activity and Coronary Heart Disease.
Sattelmair et al. (27) performed a pooled sample meta-analysis of epidemiologic studies to investigate the relationship of moderate-to-vigorous physical activity to incident coronary heart disease. Pooled dose-response estimates were derived from qualitative estimates describing low, moderate, and high amounts of physical activity. Of the 33 studies initially selected for analysis, nine permitted quantitative estimates of MET-hour per week of moderate-to-vigorous physical activity. Those participating in leisure-time physical activity at the lower limit of the 2008 Guidelines had a 14 percent reduced risk of developing coronary heart disease (RR: 0.86±0.09) compared with those reporting no leisure-time physical activity. They reported an inverse dose-response relationship similar to the curves for all-cause mortality and CVD mortality. These curves are characterized by an early decrease in risk, continued benefit with greater exposure, no lower threshold, and no upper limit (Figure 4). One MET-hour per week is approximately equal to 1.05 kcal per kilogram per week. Therefore, for a 70-kg individual, the lower boundary of the 2008 Guidelines for moderate-to-vigorous physical activity is achieved at 600 kcal per week.
Figure 4. Plot with Spline and 95% Confidence Intervals of Relative Risk of Coronary Heart Disease by Kcal Per Week of Leisure-time Physical Activity.
Source: Sattelmair et al., 2011 (27). This summary of the synthesis of nine studies displays the characteristics of this dose-response relationship with all-cause mortality as shown and discussed in Figure 2.
This analysis points to an important aspect of understanding how the interpretation of dose-response relationships may depend on the modeling parameters. When the dose-response relationships of the pooled studies are modeled using the qualitative exposures of low, moderate, and high amounts of physical activity, the dose-response relationship appears linear. When, however, the physical activity exposures are modeled according to MET-hours per week (Figure 4), the typical curvilinear relationship is unmasked.
Demographic factors and weight status:
As it was for previously studied outcomes in this article, the studies providing the strongest evidence regarding subgroup moderation effects on ischemic heart disease incidence were the pooled analyses; particularly that of Sattelmair et al. (27). Of the six studies dealing with incident CHD in our analysis, to the best of our knowledge, only Sattelmair et al. explicitly tested for disease modification by specific factors. Although no interactions were reported for effect modification by race or BMI strata, they observed a significant interaction by sex (P=0.03); the association was stronger among women than men.
Physical Activity and Stroke:
Kyu et al. (25) studied the dose-response associations of total physical activity with risk of breast cancer, colon cancer, diabetes, ischemic heart disease, and ischemic stroke events using 174 studies: 43 for ischemic heart disease, and 26 for ischemic stroke. Total physical activity—not just that within moderate-to-vigorous physical activity — in MET-minutes per week was estimated from all included studies. Continuous and categorical dose-response between physical activity and outcomes were assessed. Categorical dose-response compared insufficiently active (< 10 MET hours per week), low active (10 to 66 MET-hours) moderately active (67 to 133 MET-hours) and highly active (≥134 MET-hours). Compared with insufficiently active individuals, the relative risk reduction for those in the highly active category was 25 percent (RR=0.754; 95% CI: 0.704–0.809) for ischemic heart disease; and 26 percent (RR=0.736; 95% CI: 0.659–0.811) for ischemic stroke. Again, for ischemic stroke and ischemic heart disease (equivalent to coronary heart disease), the same typical curvilinear dose-response relationship is seen as for all-cause mortality and CVD mortality. However, the initial and maximal effect sizes are attenuated, so that achieving the lower bound of the 2008 Guidelines achieves only 36 percent reduction in initial risk for incident ischemic stroke and heart failure (Figure 5).
Figure 5. Dose-Response Relationships Between Total Physical Activity and Risk of Breast Cancer, Colon Cancer, Diabetes, Ischemic Heart Disease, and Ischemic Stroke Events Using 174 Studies (43 For Ischemic Heart Disease, and 26 For Ischemic Stroke).
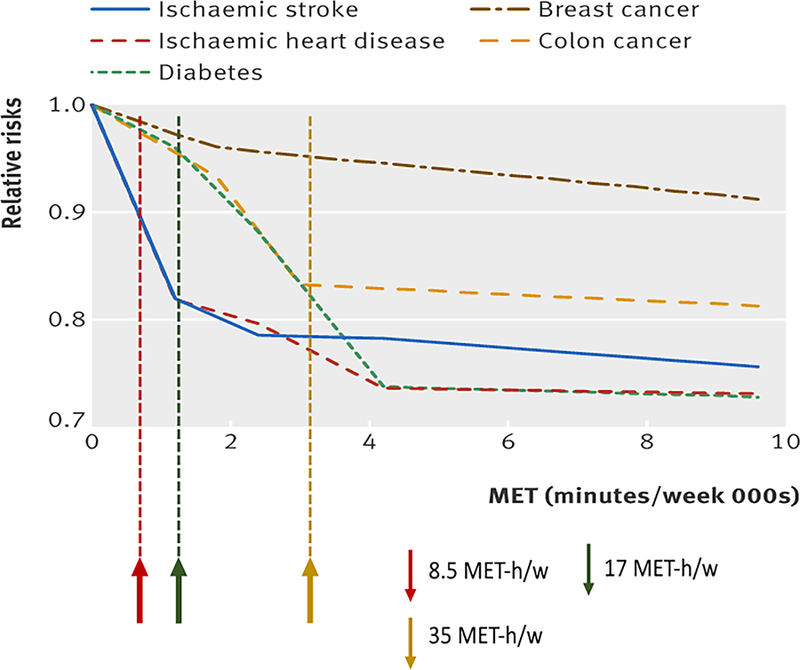
Adapted from Kyu, 2016 (25). For reference, shown are the lower end (red arrows and dotted line) and upper bounds (green arrows and dotted line) of the 2008 Guidelines for moderate-to-vigorous physical activity. Also indicated is the moderate-to-vigorous physical activity amount associated with normalization of the risk from >8h per day of sedentary activity from Ekelund, 2016 (8) (gold arrows and dotted line). The latter would represent the amount of physical activity required to compensate for an entirely sedentary lifestyle. The risk for ischemic heart disease and ischemic stroke are reminiscent of the characteristic dose-response relationships established for all-cause and cardiovascular mortality noted previously and in Figure 2. The universality of the dose-response relationships described in the caption of Figure 2 to other outcomes — such as type 2 diabetes and some cancers — are shown in this figure.
Physical Activity and Heart Failure.
Pandey et al. (26) studied the categorical dose-response relationships of physical activity to heart failure risk. As in the previously discussed analysis by Kyu et al. (25), these authors used generalized least-squares regression modeling to assess the quantitative relationship of physical activity (MET-minutes per week) to heart failure risk across studies reporting quantitative physical activity estimates. Twelve prospective cohort studies with 20,203 heart failure events among 370,460 participants (53.5% women; median follow-up, 13 years) were included. As seen in Figure 6, take from the meta-analysis of Pandy et al. (26) the greatest levels of physical activity were associated with significantly reduced risk of heart failure (pooled HR for highest versus lowest PA=0.70; 95% CI: 0.67–0.73). Compared with participants reporting no leisure-time physical activity, those who engaged in guideline-recommended minimum levels of physical activity (500 MET-minutes per week; 2008 Guidelines) had modest reductions in heart failure risk (pooled HR=0.90; 95% CI: 0.87–0.92). Only 33 percent of the maximal benefit was achieved at the 2008 Guidelines amount. Thus, for heart failure, even though the data on this are still early, by inspection it appears the dose-response relationship is more linear at lower physical activity amounts, and not the sharp, early curvilinear relationship observed for the other outcomes discussed in this chapter. Note, at this time, studies of the relationship between physical activity and heart failure incidence do not distinguish among the various types of heart failure: heart failure with preserved (HFpEF), reduced (HFrEF) heart failure, or a combination of the two. This should be a point of emphasis for future research.
Figure 6. Dose-Response Relationships Between Moderate-to-Vigorous Physical Activity and Risk of Incident Heart Failure.
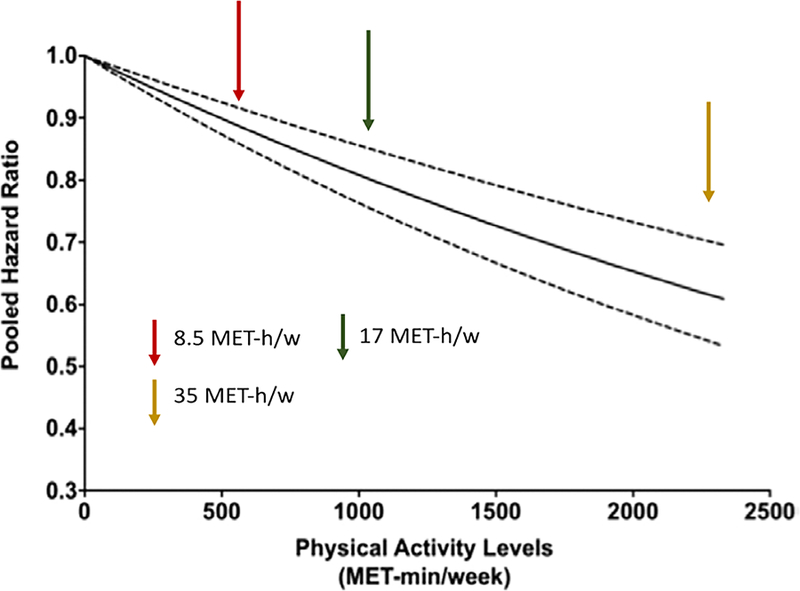
Source: Adapted from Pandey et al., 2015 (26). For reference, shown are the lower end (red arrows and dotted line) and upper bounds (green arrows and dotted line) of the 2008 Guidelines for moderate-to-vigorous physical activity. Also indicated is the moderate-to-vigorous physical activity amount associated with normalization of the risk from >8h per day of sedentary activity from Ekelund et al., 2016 (8) (gold arrows and dotted line). The latter would represent the amount of physical activity required to compensate for a highly sedentary lifestyle. Note, the colors of the arrows are important, not the direction of the arrow.
CONCLUSIONS AND PUBLIC HEALTH IMPACT
The effects of moderate-to-vigorous physical activity on ischemic cardiovascular diseases, including coronary heart disease, ischemic stroke, and heart failure are very similar to those of all-cause mortality and CVD mortality. The evidence for these conclusions was considered strong by the Committee. The grading of the accumulated evidence is available in Supplemental Digital Content (see Table, SDC 4, evidence statements for conclusions). The evidence continues to support the conclusion that increasing moderate-to-vigorous physical activity levels by modest amounts in the inactive U.S. population has the potential to have an important and substantial impact on these outcomes in the adult population. With respect to reductions in risk for these endpoints, the following points are clear: (1) the associations of physical activity with beneficial health outcomes begin when adopting very modest amounts; (2) more moderate-to-vigorous physical activity is better than none; (3) meeting the 2008 moderate-to-vigorous physical activity guidelines reduces risk of all-cause mortality to about 75 percent of the maximal benefit; (4) more physical activity reduces risk even more, but more physical activity is required to obtain less benefit; and (5) there is no evidence of excess risk over the maximal effect observed at about 3 to 5 times the moderate-to-vigorous physical activity of the current guidelines; (6) when the activity is quantified by volume in terms of energy expenditure of task (MET-hours per week), these relationships seem to hold for several modes and intensities of physical activity, including walking, running, and biking.
Needs for Future Research.
Several advances in our understanding of the relationships among physical activity and the outcomes described herein have occurred since the 2008 Report. Most of the literature upon which the 2008 conclusions were based utilized survey data and questionnaire data; physical activity exposures were assessed using self-reported estimates of time spent in aerobic continuous moderate-to-vigorous physical activity accumulated in bouts of at least ten minutes. Therefore, all other components across the physical activity spectrum – sedentary behavior, light-intensity physical activity, and any moderate to vigorous intensity physical activity in bouts less than 10 minutes – was considered “baseline” physical activity. The scientific community and public health researchers have begun to incorporate objective, device-based measures of physical activity—and sedentary behavior—into our measurement armamentarium. This has permitted assessments of the relationship of activity of less than moderate-to-vigorous intensity with health outcomes; it has permitted the assessment of the relations of episodes of moderate-to-vigorous physical activity of less than 10 minutes one health outcomes. Given this, more research is needed in these areas:
Conduct research on the role of light intensity physical activities and interaction with sedentary behavior in risk reduction for all-cause mortality, cardiovascular disease mortality, and incident cardiovascular disease (coronary heart disease, stroke and heart failure). This can most economically and efficiently be accomplished by incorporating devices (pedometers, wearables, watches) measuring physical activity into all clinical trials with all-cause mortality, cardiovascular disease mortality, or incident cardiovascular disease as outcomes.
Rationale: As reported in this chapter, the benefits of MVPA on all-cause mortality, cardiovascular disease mortality, and incident cardiovascular disease (coronary heart disease, stroke and heart failure) are well-documented and strong. However, these studies ignore the effects of physical activity that are not characterized as moderate-to-vigorous intensity (light). The development of device-based measures of physical activity (pedometers, watches, accelerometers and other wearables) provide the scientific imperative to begin to explore the relations of all intensities and amounts of physical activity—light to vigorous; small to great total amounts. These studies are beginning to appear (31–35). Unfortunately, there are not enough studies on the relation of light physical activity, total physical activity, or step counts per day to provide sufficient information for meta-analyses to be performed in these areas for the outcomes of interest here. Further, the role of sedentary behavior on disease risk is an evolving concept. The ability to quantify this objectively is now available and will allow investigators to incorporate the interaction of sedentary behavior and physical activity on disease risk—a research area that until now has been relatively ignored or not possible.
This becomes a major future research need. This goal can most economically and efficiently be accomplished by incorporating devices (pedometers, wearables, watches) measuring physical activity and sedentary behavior into all clinical trials with all-cause mortality, cardiovascular disease mortality, or incident cardiovascular disease as outcomes.
Conduct research on the possibility of increased risk associated with great amounts of physical activity.
Rationale: Whether great amounts (volumes) of aerobic physical exercise lead to increased cardiac morbidity or mortality is an important, yet open question. As discussed in this chapter, there is a hint in some studies of an increase in cardiovascular risk in high volume aerobic athletes. Recent reports document increased coronary calcium scores in masters athletes (36, 37); however, there seems to be a U-shaped relationship with life-long volume of training (36). These findings may explain the hint of an increased cardiovascular risk in long-term athletes. Clearly, this issue demands more study in athletic populations.
Conduct research on the relative importance of the various characteristics of physical activity exposure (total volume, intensity, frequency and mode) and muscular strengthening physical activity on all-cause mortality, cardiovascular disease mortality, and incident cardiovascular disease (coronary heart disease, stroke and heart failure).
Rationale: Now into our second iteration of the Physical Activity Guidelines Scientific Report, we continue to rely on studies of aerobic ambulatory moderate-to-vigorous physical activity —primarily collected via survey — to understand the relationship of physical activity to all-cause mortality, cardiovascular disease mortality, and incident cardiovascular disease. Underexplored are the importance of frequency and intensity relative to volume of aerobic exercise; the importance of muscle strengthening to these clinical outcomes; whether swimming, biking, and rowing contribute to cardiovascular health equal to that of aerobic ambulatory exercise; and what the energy expenditures and programs are for these aerobic activities for equivalent clinical outcomes. If we are going to prescribe exercise of all modalities as options for adults wanting to exercise for health, we need better understanding of the relative contributions of a general range of options.
Supplementary Material
ACKNOWLEDGEMENTS
The authors gratefully acknowledge the contributions of Anne Brown Rodgers, HHS consultant for technical writing support of the Physical Activity Guidelines Advisory Committee Report; and ICF librarians, abstractors, and additional support staff.
Role of the Funder/Sponsor
HHS staff provided general administrative support to the Committee and assured that the Committee adhered to the requirements for Federal Advisory Committees. HHS also contracted with ICF, a global consulting services company, to provide technical support for the literature searches conducted by the Committee. HHS and ICF staff collaborated with the Committee in the design and conduct of the searches by assisting with the development of the analytical frameworks, inclusion/exclusion criteria, and search terms for each primary question; using those parameters, ICF performed the literature searches.
This paper is being published as an official pronouncement of the American College of Sports Medicine. This pronouncement was reviewed for the American College of Sports Medicine by members-at-large and the Pronouncements Committee. Disclaimer: Care has been taken to confirm the accuracy of the information present and to describe generally accepted practices. However, the authors, editors, and publisher are not responsible for errors or omissions or for any consequences from application of the information in this publication and make no warranty, expressed or implied, with respect to the currency, completeness, or accuracy of the contents of the publication. Application of this information in a particular situation remains the professional responsibility of the practitioner; the clinical treatments described and recommended may not be considered absolute and universal recommendations.
Footnotes
Conflicts of Interest and Source of Funding
The results of this study are presented clearly, honestly, and without fabrication, falsification, or inappropriate manipulation. The Committee’s work was supported by the U.S. Department of Health and Human Services (HHS). Committee members were reimbursed for travel and per diem expenses for the five public meetings; Committee members volunteered their time. The authors report no other potential conflicts of interest.
REFERENCES
- 1.Physical Activity Guidelines Advisory Committee. Physical Activity Guidelines Advisory Committee Scientific Report Washington, DC: U.S. Department of Health and Human Services; 2008. [Google Scholar]
- 2.Physical Activity Guidelines for Americans In: DHHS, editor. Washington, DC: U.S. Department of Health and Human Services; 2008. [Google Scholar]
- 3.Physical Activity Guidelines Advisory Committee 2018. 2018 Physical Activity Guidelines Advisory Committee Scientific Report Washington, DC: U.S. Department of Health and Human Services; 2018. [Google Scholar]
- 4.Torres A, Tennant B, Ribeiro-Lucas I, Vaux-Bjerke A, Piercy K, Bloodgood B. Umbrella and systematic review methodology to support the 2018 Physical Activity Guidelines Advisory Committee. J Phys Act Health 2018;1–6. [DOI] [PubMed]
- 5.Johnson BT, MacDonald HV, Bruneau ML Jr., Goldsby TU, Brown JC, Huedo-Medina TB, et al. Methodological quality of meta-analyses on the blood pressure response to exercise: a review. J Hypertens 2014;32(4):706–23. Epub 2014/01/28. doi: 10.1097/hjh.0000000000000097. [DOI] [PubMed] [Google Scholar]
- 6.Milton K, Macniven R, Bauman A. Review of the epidemiological evidence for physical activity and health from low- and middle-income countries. Glob Public Health 2014;9(4):369–81. Epub 2014/04/05. doi: 10.1080/17441692.2014.894548. [DOI] [PubMed] [Google Scholar]
- 7.Warburton DE, Charlesworth S, Ivey A, Nettlefold L, Bredin SS. A systematic review of the evidence for Canada’s Physical Activity Guidelines for Adults. Int J Behav Nutr Phys Act 2010;7:39 Epub 2010/05/13. doi: 10.1186/1479-5868-7-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ekelund U, Steene-Johannessen J, Brown WJ, Fagerland MW, Owen N, Powell KE, et al. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet 2016;388(10051):1302–10. Epub 2016/08/01. doi: 10.1016/s0140-6736(16)30370-1. [DOI] [PubMed] [Google Scholar]
- 9.Hamer M, Chida Y. Walking and primary prevention: a meta-analysis of prospective cohort studies. Br J Sports Med 2008;42(4):238–43. Epub 2007/12/01. doi: 10.1136/bjsm.2007.039974. [DOI] [PubMed] [Google Scholar]
- 10.Hupin D, Roche F, Gremeaux V, Chatard JC, Oriol M, Gaspoz JM, et al. Even a low-dose of moderate-to-vigorous physical activity reduces mortality by 22% in adults aged >/=60 years: a systematic review and meta-analysis. Br J Sports Med 2015;49(19):1262–7. Epub 2015/08/05. doi: 10.1136/bjsports-2014-094306. [DOI] [PubMed] [Google Scholar]
- 11.Kelly P, Kahlmeier S, Gotschi T, Orsini N, Richards J, Roberts N, et al. Systematic review and meta-analysis of reduction in all-cause mortality from walking and cycling and shape of dose response relationship. Int J Behav Nutr Phys Act 2014;11:132 Epub 2014/10/26. doi: 10.1186/s12966-014-0132-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lollgen H, Bockenhoff A, Knapp G. Physical activity and all-cause mortality: an updated meta-analysis with different intensity categories. Int J Sports Med 2009;30(3):213–24. Epub 2009/02/10. doi: 10.1055/s-0028-1128150. [DOI] [PubMed] [Google Scholar]
- 13.Samitz G, Egger M, Zwahlen M. Domains of physical activity and all-cause mortality: systematic review and dose-response meta-analysis of cohort studies. Int J Epidemiol 2011;40(5):1382–400. Epub 2011/11/01. doi: 10.1093/ije/dyr112. [DOI] [PubMed] [Google Scholar]
- 14.Woodcock J, Franco OH, Orsini N, Roberts I. Non-vigorous physical activity and all-cause mortality: systematic review and meta-analysis of cohort studies. Int J Epidemiol 2011;40(1):121–38. Epub 2010/07/16. doi: 10.1093/ije/dyq104. [DOI] [PubMed] [Google Scholar]
- 15.Arem H, Moore SC, Patel A, Hartge P, Berrington de Gonzalez A, Visvanathan K, et al. Leisure time physical activity and mortality: a detailed pooled analysis of the dose-response relationship. JAMA Intern Med 2015;175(6):959–67. Epub 2015/04/07. doi: 10.1001/jamainternmed.2015.0533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liu Y, Shu XO, Wen W, Saito E, Rahman MS, Tsugane S, et al. Association of leisure-time physical activity with total and cause-specific mortality: a pooled analysis of nearly a half million adults in the Asia Cohort Consortium. Int J Epidemiol 2018. Epub 2018/03/01. doi: 10.1093/ije/dyy024. [DOI] [PMC free article] [PubMed]
- 17.Moore SC, Patel AV, Matthews CE, Berrington de Gonzalez A, Park Y, Katki HA, et al. Leisure time physical activity of moderate to vigorous intensity and mortality: a large pooled cohort analysis. PLoS Med 2012;9(11):e1001335 Epub 2012/11/10. doi: 10.1371/journal.pmed.1001335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.O’Donovan G, Lee IM, Hamer M, Stamatakis E. Association of “weekend warrior” and other leisure time physical activity patterns with risks for all-cause, cardiovascular disease, and cancer mortality. JAMA Intern Med 2017;177(3):335–42. Epub 2017/01/18. doi: 10.1001/jamainternmed.2016.8014. [DOI] [PubMed] [Google Scholar]
- 19.Merom D, Ding D, Stamatakis E. Dancing participation and cardiovascular disease mortality: a pooled analysis of 11 population-based british cohorts. Am J Prev Med 2016;50(6):756–60. Epub 2016/03/06. doi: 10.1016/j.amepre.2016.01.004. [DOI] [PubMed] [Google Scholar]
- 20.Paffenbarger RS Jr., Hyde RT, Wing AL, Hsieh CC. Physical activity, all-cause mortality, and longevity of college alumni. N Engl J Med 1986;314(10):605–13. Epub 1986/03/06. doi: 10.1056/nejm198603063141003. [DOI] [PubMed] [Google Scholar]
- 21.Paffenbarger RS Jr., Wing AL, Hyde RT. Physical activity as an index of heart attack risk in college alumni. Am J Epidemiol 1978;108(3):161–75. Epub 1978/09/01. [DOI] [PubMed] [Google Scholar]
- 22.Wahid A, Manek N, Nichols M, Kelly P, Foster C, Webster P, et al. Quantifying the association between physical activity and cardiovascular disease and diabetes: a systematic review and meta-analysis. J Am Heart Assoc 2016;5(9). Epub 2016/09/16. doi: 10.1161/jaha.115.002495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Diep L, Kwagyan J, Kurantsin-Mills J, Weir R, Jayam-Trouth A. Association of physical activity level and stroke outcomes in men and women: a meta-analysis. J Womens Health (Larchmt) 2010;19(10):1815–22. Epub 2010/10/12. doi: 10.1089/jwh.2009.1708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Echouffo-Tcheugui JB, Butler J, Yancy CW, Fonarow GC. Association of physical ctivity or fitness with incident heart failure: a systematic review and meta-analysis. Circ Heart Fail 2015;8(5):853–61. Epub 2015/07/16. doi: 10.1161/circheartfailure.115.002070. [DOI] [PubMed] [Google Scholar]
- 25.Kyu HH, Bachman VF, Alexander LT, Mumford JE, Afshin A, Estep K, et al. Physical activity and risk of breast cancer, colon cancer, diabetes, ischemic heart disease, and ischemic stroke events: systematic review and dose-response meta-analysis for the Global Burden of Disease Study 2013. BMJ 2016;354:i3857 Epub 2016/08/12. doi: 10.1136/bmj.i3857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pandey A, Garg S, Khunger M, Darden D, Ayers C, Kumbhani DJ, et al. Dose-response relationship between physical activity and risk of heart failure: a meta-analysis. Circulation 2015;132(19):1786–94. Epub 2015/10/07. doi: 10.1161/circulationaha.115.015853. [DOI] [PubMed] [Google Scholar]
- 27.Sattelmair J, Pertman J, Ding EL, Kohl HW 3rd, Haskell W, Lee IM. Dose response between physical activity and risk of coronary heart disease: a meta-analysis. Circulation 2011;124(7):789–95. Epub 2011/08/04. doi: 10.1161/circulationaha.110.010710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sofi F, Capalbo A, Cesari F, Abbate R, Gensini GF. Physical activity during leisure time and primary prevention of coronary heart disease: an updated meta-analysis of cohort studies. Eur J Cardiovasc Prev Rehabil 2008;15(3):247–57. Epub 2008/06/06. doi: 10.1097/HJR.0b013e3282f232ac. [DOI] [PubMed] [Google Scholar]
- 29.Zheng G, Huang M, Liu F, Li S, Tao J, Chen L. Tai chi chuan for the primary prevention of stroke in middle-aged and elderly adults: a systematic review. Evid Based Complement Alternat Med 2015;2015:742152 Epub 2015/03/19. doi: 10.1155/2015/742152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zheng H, Orsini N, Amin J, Wolk A, Nguyen VT, Ehrlich F. Quantifying the dose-response of walking in reducing coronary heart disease risk: meta-analysis. Eur J Epidemiol 2009;24(4):181–92. Epub 2009/03/24. doi: 10.1007/s10654-009-9328-9. [DOI] [PubMed] [Google Scholar]
- 31.Bennett DA, Du H, Clarke R, Guo Y, Yang L, Bian Z, et al. Association of physical activity with risk of major cardiovascular diseases in chinese men and women. JAMA Cardiol 2017;2(12):1349–58. Epub 2017/11/09. doi: 10.1001/jamacardio.2017.4069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Buchner DM, Rillamas-Sun E, Di C, LaMonte MJ, Marshall SW, Hunt J, et al. Accelerometer-measured moderate to vigorous physical activity and incidence rates of falls in older women. J Am Geriatr Soc 2017;65(11):2480–7. Epub 2017/07/30. doi: 10.1111/jgs.14960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.LaMonte MJ, Buchner DM, Rillamas-Sun E, Di C, Evenson KR, Bellettiere J, et al. Accelerometer-measured physical activity and mortality in women aged 63 to 99. J Am Geriatr Soc 2018;66(5):886–94. Epub 2017/11/17. doi: 10.1111/jgs.15201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.LaMonte MJ, Lewis CE, Buchner DM, Evenson KR, Rillamas-Sun E, Di C, et al. Both light intensity and moderate-to-vigorous physical activity measured by accelerometry are favorably associated with cardiometabolic risk factors in older women: the Objective Physical Activity and Cardiovascular Health (OPACH) Study. J Am Heart Assoc 2017;6(10). Epub 2017/10/19. doi: 10.1161/jaha.117.007064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lee IM, Shiroma EJ, Evenson KR, Kamada M, LaCroix AZ, Buring JE. Accelerometer-measured physical activity and sedentary behavior in relation to all-cause mortality: The Women’s Health Study. Circulation 2018;137(2):203–5. Epub 2017/11/08. doi: 10.1161/circulationaha.117.031300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Aengevaeren VL, Mosterd A, Braber TL, Prakken NHJ, Doevendans PA, Grobbee DE, et al. Relationship between lifelong exercise volume and coronary atherosclerosis in athletes. Circulation 2017;136(2):138–48. Epub 2017/04/30. doi: 10.1161/circulationaha.117.027834. [DOI] [PubMed] [Google Scholar]
- 37.Merghani A, Maestrini V, Rosmini S, Cox AT, Dhutia H, Bastiaenan R, et al. Prevalence of subclinical coronary artery disease in masters endurance athletes with a low atherosclerotic risk profile. Circulation 2017;136(2):126–37. Epub 2017/05/04. doi: 10.1161/circulationaha.116.026964. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


