Abstract
Purpose:
Physical activity is known to provide important health benefits in school-age youth. However, until recently few studies have examined associations between physical activity and health in young children. The purpose of this study was to conduct a systematic review of the relationship between physical activity and selected health outcomes in children under 6 years of age.
Methods:
A systematic search identified randomized controlled trials and prospective cohort studies examining the associations between physical activity and adiposity/weight status, bone health, cardiometabolic health, and cognition in children younger than 6 years of age.
Results:
27 studies met inclusion criteria and served as the basis for this systematic review. For weight status/adiposity, 12 of 15 studies found negative associations between physical activity and one or more measures of the outcome. For bone health, 10 articles based on 4 studies were identified, and 9 studies showed stronger bone in more active children. For cardiometabolic health, 3 studies were identified and findings were limited and inconsistent. For cognition, 2 systematic reviews were identified and findings were limited. For all four health outcomes, evidence of dose-response relationships and effect modification by demographic factors was very limited.
Conclusions:
There is strong evidence indicating that higher amounts of physical activity are associated with better indicators of bone health and with reduced risk for excessive increases in weight and adiposity in children 3 to 6 years of age. Evidence was too limited to support conclusions regarding the effects of physical activity on cardiometabolic health and cognition.
Keywords: Weight status, adiposity, bone health, cardiometabolic health, dose-response, effect modification
Introduction
The body of knowledge on the relationship between physical activity and health in children and youth has been growing steadily since the 1950’s, and the development of this research field has been particularly rapid over the last two decades (1). Much of the early research was focused on physical fitness and its relationship to growth and development in young persons (2). However, more recently the emphasis has shifted to the effects of physical activity on risk factors for non-communicable diseases that typically do not manifest until adulthood. These include cardiometabolic diseases such as coronary heart disease and type 2 diabetes and bone health outcomes including osteoporosis and bone fractures (3). With the marked increase in the prevalence of overweight and obesity in U.S. children, many recent studies have examined the impact of physical activity on adiposity and weight status in young persons (4).
The 2008 Physical Activity Guidelines Advisory Committee Report included an examination of the relationship between physical activity and health in children and adolescents. Key conclusions of that review were that, in school-age children and youth, higher levels of physical activity are associated with better status on indicators of cardiorespiratory and muscular fitness, body composition, cardiometabolic risk, and bone health (5). Those conclusions informed a physical activity guideline which indicated that children and adolescents should accumulate 60 minutes or more of at least moderate intensity physical activity daily and that, within that hour of activity, vigorous intensity physical activity, muscle-strengthening and bone-strengthening activities should be included at least three days per week (6). Notably, this guideline was applied only to youth in the 6 to 18 year age range. No guideline was included for children younger than age 6 years, because the body of knowledge on physical activity and health in early childhood was very limited.
During the period between 2008 and 2018 a substantial volume of research was undertaken on the relationship between physical activity and health in children of preschool age (7). Further, during that period physical activity guidelines for children under age 6 years were developed by public health agencies in some other countries, and physical activity guidelines for children attending childcare centers was released by the Institute of Medicine in the US (8). Accordingly, the Youth Subcommittee of the 2018 Physical Activity Guidelines Advisory Committee opted to consider the evidence related to relationships between physical activity and selected health outcomes in children under 6 years of age. The purpose of this article is to present the findings of a systematic review of the scientific literature addressing this issue. Specific health outcomes considered in the review were body weight and adiposity, bone health, cognition, and cardiometabolic risk factors.
Methods
The methods used to conduct systematic reviews for the 2018 Physical Activity Guidelines Advisory Committee Scientific Report have been described in detail elsewhere (9). An initial search limited to systematic reviews, meta-analyses, pooled-analyses, and high-quality reports was conducted. That search yielded too few articles, so the search was repeated to identify relevant original research articles. Accordingly, for this review, a systematic search was conducted to identify randomized controlled trials and prospective cohort studies that assessed the association between any type of physical activity and health outcomes including adiposity and weight status, bone health, and cardiometabolic health in children younger than 6 years of age. The searches were conducted in electronic databases (PubMed®, CINAHL, and Cochrane) and were supplemented by asking Subcommittee members, all experts in the area, to provide additional articles identified through their expertise/familiarity with the literature.
Articles published in English from data base inception until February 2017 were included in the Committee Report, and the search was extended to March 2018 for this manuscript. Search terms included age-appropriate physical activity, active play and sedentary behavior terms combined with outcome-specific terms. The full search strategy is available at https://health.gov/paguidelines/second-edition/report/supplementary_material/pdf/Youth_Q1_Under6_Evidence_Portfolio.pdf. The identified articles were independently screened by two reviewers. The full-text of relevant articles was reviewed to include those that met the inclusion criteria. Inclusion/exclusion criteria are presented in Supplementary Material (see Table, SDC 1, Inclusion/Exclusion Criteria). Two abstractors independently abstracted data and conducted a quality or risk of bias assessment using the USDA NEL Bias Assessment Tool (BAT) for original research (9, 10) and the AMSTAR ExBP for systematic reviews (11). Discrepancies in article selection or data abstractions were resolved by discussion or a third reviewer if needed. The protocol for this review was registered with the PROSPERO database (registration ID CRD42018092740). A summary of the bias assessment of the original research articles included in this review is available in the supplementary material [see Tables, SDC 2, Nutrition Evidence Library (NEL) Bias Assessment Tool (BAT): Original Research; and SDC 3, AMSTAR ExBP: SR/MA].
Results
Search results.
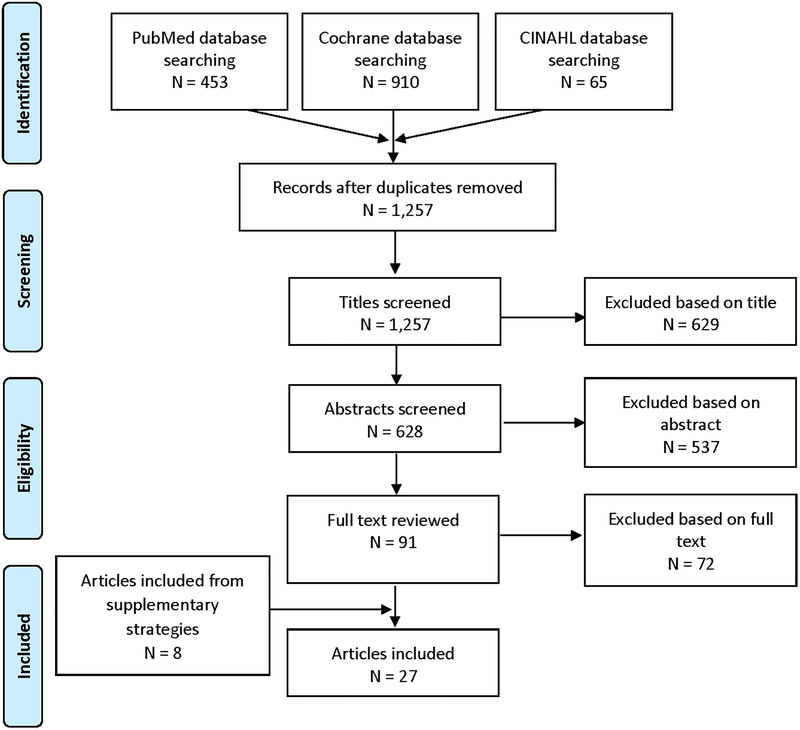
A total of 1257 studies were identified through the systematic searches (Figure 1). After screening titles and abstracts, 1166 studies were excluded and 91 reviewed in full. Of these, 19 studies met the full inclusion criteria. An additional 8 studies were identified by the authors based on their knowledge in the area. Twenty-seven studies were included in this review until the release of the 2018 Physical Activity Guidelines Advisory Committee Scientific Report. One additional original research article and three systematic reviews were found when the search was updated for the purpose of this manuscript.
Figure 1.
Summary of the Search of Primary Research on Physical Activity and Health Outcomes in Children Under 6 Years of Age
Body weight and adiposity.
In considering the evidence regarding the relationship between physical activity and body weight and/or adiposity in children under 6 years of age the Committee identified and reviewed 15 studies (12–26). The study designs, methods, and findings of these studies are summarized in Table 1. All of the studies included in this review employed prospective, longitudinal study designs. However, methods for measurement of physical activity were highly variable. Also, the studies were quite variable in terms of children’s age range, years of follow-up, measurement of weight-related outcomes, and analytic procedures. Not withstanding these differences, the studies were consistent in reporting that higher levels of physical activity were associated with lower levels of weight and/or adiposity in younger children. Twelve of the 15 studies found negative associations between physical activity and weight and/or adiposity (12–16, 18, 20–25). While these studies were consistent in observing benefit with higher amounts of physical activity, limitations in study design and variability in methodologies across the studies precluded identifying a particular dose of physical activity that was needed to provide benefits.
Table 1.
Summaries of Studies Examining Associations between Physical Activity and Weight Status on Adiposity in Children <6 Years of Age
| Study (title, citation) | Subjects | Sample Size | Study Design | Physical Activity Exposure | Adiposity Measures | Findings |
|---|---|---|---|---|---|---|
| Berkowitz RI, 1985 (12) | infants at baseline (first 3 days of life); 4–8 years old at follow up | 52 | Prospective Cohort | Neonatal physical activity measured by an electronic activity monitor inside a mattress | BMI and skinfolds | Neonatal PA was significantly correlated with measures of adiposity in childhood. |
| DuRant RH, 1993 (13) | 3–4 year olds at baseline, 4–5 years old at follow up | 123 | Prospective Cohort | Physical activity assessed by heart rate monitoring | Waist-to-hip ratio, sum of skinfolds | Mean activity level was negatively correlated with waist/hip ratio. Temporal direction of the association is unclear. |
| Jago R, 2005 (14) | 3–4 year old children at baseline; 6–7 years old at follow up | 133 | Prospective Cohort | Physical activity assessed by heart rate monitoring and direct observation of sedentary behavior and TV viewing (CARS) | BMI | PA and TV viewing were significant predictors of BMI with both PA (- associated) and TV viewing (+ associated) becoming stronger predictors as the children aged. |
| Janz KF, 2009 (15) | Ages 5, 8 and 11 years | 333 | Prospective Cohort | Moderate-to-vigorous physical activity measured by accelerometry | Body fat measured by DXA | MVPA at age 5 years was a predictor of adjusted fat mass at age 8 years and age 11 years, in both sexes. |
| Klesges RC, 1995 (16) | 4 years old at baseline | 146 | Prospective Cohort | Physical activity (Parent-reported structured, leisure, and aerobic activity) | BMI | Baseline aerobic activity predicted change in BMI over 2 years. |
| Leppanen MH, 2017 (17) | 4 years old at baseline | 138 | Prospective Cohort | Light-intensity, moderate-intensity, vigorous intensity, and moderate-to-vigorous intensity physical activity & sedentary behavior measured by accelerometry | BMI and Fat Mass Index, Fat-free Mass Index, and %FM (from air-displacement plethysmography) | Higher VPA at the age of 4.5 years was significantly associated with higher BMI and FFMI at 12-month follow-up. Higher baseline MVPA was also associated with higher FFMI at follow-up. |
| Li R, 1995 (18) | Ages 6, 9, and 12 months | 31 | Prospective Cohort | Physical activity from 6-hour direct observation (modifyied CARS) | Body fat measured by DXA | The percentage of body fat was inversely related to activity level. This association became stronger with increasing age and remained significant after adjustment for dietary energy intake. |
| Metcalf BS, 2008 (19) | 5 years old at baseline, 6–8 years old at follow up | 212 | Prospective Cohort | Physical activity measured by accelerometry | BMI, skinfolds and waist circumference | PA above the government-recommended intensity of 3 METs was associated with a progressive improvement in metabolic health but not with a change in BMI or fatness. |
| Moore LL, 2003 (20) | 4 years old at baseline (males and females) | 103 | Prospective Cohort | Physical Activity by Caltrac accelerometer | BMI, Skinfolds | Higher levels of PA during childhood may lead to less body fat by the time of early adolescence. A protective effect of activity was evident in both sexes. |
| Moore LL, 1995 (21) | 3–5 years old | 97 | Prospective Cohort | Physical activity by Caltrac acclerometer | BMI, skinfolds | There was a protective effect of PA on body fat change in both sexes. Higher levels of PA during childhood lead to less body fat by the time of early adolescence. |
| Remmers T, 2014 (22) | 4–7 years old at baseline, 6–9 years at follow-up | 470 | Prospective Cohort | Light PA, MVPA and sedentary behavior measured by accelerometry | BMI z-scores | Increments of MVPA were associated with decreases in BMI z-score in heavier children, in both sexes. |
| Roberts SB, 1988 (23) | 0–12 months old (6 infants from lean and 12 infants from overweight mothers) | 18 | Prospective Cohort | Total energy expenditure from doubly labeled water | Weight gain (1st year of life), triceps and subscapular skinfolds | Total energy expenditure at 3 months of age was 20.7% lower in infants who became overweight compared to other infants. |
| Saakslahti A, 2004 (24) | 4–7 years old at baseline | 155 | Prospective Cohort | Physical activity measured by parental report (observation diary) | BMI | In girls, low-activity playing was positively correlated with BMI at age 4–5 years and playing indoors was positively correlated with BMI at age 5–6 years. There were no significant associations in boys. |
| Sugimori H, 2004 (25) | 3 years old at baseline; 6 years old at follow up | 8170 | Prospective Cohort | Physical activity measured by questionnaire (physical exercise/playing outdoor), physical club activities, duration of TV viewing) | BMI | Physical inactivity at age 6 years was associated with temporal changes in overweight status between 3–6 years in boys. |
| Wells JCK, 1996 (26) | 12 weeks old at baseline; 2–3.5 years old at follow up | 30 | Prospective Cohort | Physical activity energy expenditure measured from total energy expenditure (doubly labeled water) and minimal metabolism (Deltatrac Metabolic monitor); mother’s diary of infant activity | Weight, BMI, skinfolds, and fat mass (from total body water) | PA energy expenditure at 12 weeks was not associated with measures of adiposity at follow-up. |
Bone health.
The literature search provided eight papers, with two additional papers added by committee members. These 10 papers represented four studies, two of which had prospective longitudinal study designs and two of which were randomized controlled trials (27–36). The study designs, methods, and findings of these studies are summarized in Table 2. Three of the four studies focused on preschool children (baseline ages 3 to 5) (27–35) and one study focused on infants (36). The dose of physical activity was defined and measured differently among the studies and included recreational gymnastics participation (months) (28–30), device-measured daily activity (min) (31–34), and bone-strengthening physical activity (sessions) (27, 35, 36). All studies used state-of-the-art imaging (dual-energy x-ray absorptiometry (DXA) and peripheral quantitative computed tomography (pQCT)) to measure bone outcomes and appropriate statistical modeling to control for growth. All studies examining children ages 3–5 years showed statistically significant stronger bone in the more active children. The benefit differences were greater than expected via measurement error and large enough (almost always >3%) to indicate meaningful biological improvements. However, similar to the evidence for body weight and adiposity, the differences in physical activity measures prevented the assignment of a specific dose of physical activity needed for bone health benefits.
Table 2.
Summary of Studies Examining the Association Between Physical Activity and Indicators of Bone Health in Children <6 Years of Age.
| Study (title, citation) | Subjects (age, sex, etc.) | Sample Size | Study Design | Physical Activity Exposure | Bone Outcomes | Findings |
|---|---|---|---|---|---|---|
| Binkley, 2004 (27) | 3–5 years old at baseline (males and females) mostly white | 161 | One year post trial follow-up | Researcher delivered Intervention gross motor vs fine motor PA (5/d week, 15–20 min/d) and calcium supplementations | pQCT, DXA measured BMC and BA leg, periosteal and endosteal circumference tibia | Children in gross motor skill group maintained greater tibial periosteal circumference difference 1-year post intervention compared to fine motor. |
| Erlandson MC, 2011 (28) | 4–6 years old at baseline (males and females) mostly white | 163 | Prospective Cohort Measured annually for 4 years | Parent report (hrs/wk) of recreational or precompetitive gymnastics | Dual-energy x-ray absorptiometry (DXA) measured total body, lumbar spine, and femoral neck bone mineral content (BMC) | Compared to non-gymnasts in other recreational sports, gymnasts had 3% more total body BMC and 7% femoral neck BMC. |
| Gruodyte-Raciene R, 2013 (29) | 4–6 years old at baseline (males and females) mostly white | 165 | Prospective Cohort Measured annually for 4 years | Parent report (hrs/wk) of recreational or precompetitive gymnastics | DXA and hip structural analysis program (HSA) estimated cross-sectional area (CSA), section modulus (Z), cortical thickness (CT) at narrow neck (NN), intertrochanter (IT), shaft (S) of hip | Compared to non-gymnasts in other recreational sports, gymnasts had 6% greater NN CSA, 7% NN Z, 5% greater IT CSA, 6% greater IT Z and 3% greater S CSA. |
| Jackowski SA, 2015 (30) | 4–6 years old at baseline (males and females) mostly white | 127 | Prospective Cohort Measured over 3 years | Parent report (hrs/wk) of recreational or precompetitive gymnastics | Peripheral quantitative computed tomography (pQCT) measured distal and shaft measures of bone structure at radius and tibia | Compared to non-gymnasts in other recreational sports, gymnasts had greater total bone area and total BMC at distal radius (8 to 21% difference). |
| Janz KF, 2006 (31) | 4 −6 years old at baseline (males and females) mostly white | 370 | Prospective Cohort with a 3 year follow-up | Device-measured MVPA 3000 ct/mn | DXA measured BMC hip, trochanter, spine, and total body | Compared to children maintaining low levels of PA, children maintaining high levels of PA throughout study accrued 14% more trochanteric BMC and 5% more total body BMC. |
| Janz K, 2007 (32) | 4–6 years old at baseline (males and females) mostly white | 468 | Prospective Cohort Measured 3 times (baseline, approximately 8 yr. and 11 yr.) | Device-measured MVPA 3000 ct/mn | DXA and HSA estimated bone structure femoral neck Z and CSA | PA positive independent predictor of Z and CSA. 40 min/d compared to 10 min/d equated to 3–5% greater CSA and Z |
| Janz KF, 2014 (33) | 4–6 years old at baseline (males and females) mostly white | 530 | Prospective Cohort Measured 6 times (baseline, approximately 8, 11, 13, 15, and 17 yr.) | Device-measured MVPA (Evenson 2296 ct/min) | pQCT, DXA and HSA estimated BMC and bone structure of hip (CSA, Z) and tibia (bone stress index, polar moment of inertia) | Greater accumulation of MVPA resulted in great bone mass and structure at age 17 years |
| Janz KF, 2010 (34) | 4–6 years old at baseline (males and females) mostly white | 333 | Prospective Cohort Measured 3 times baseline, approximately 8, and 11 yr.) | Device-measured MVPA 3000 ct/min | DXA measured BMC total body, hip, spine | Children at highest quartile of MVPA at baseline had 4–14% more BMC at age 8 and 11 years when compared to peers in lowest quartile. Results attenuate when controlled for baseline BMC but remained significant in boys. |
| Specker BL, 2003 (35) | 3–5 years old at baseline (males and females) mostly white | 239 | One year randomized control trial | Researcher delivered Intervention gross motor vs fine motor PA (5/d week, 15–20 min/d) and calcium supplementations | pQCT, DXA measured BMC total body and leg, periosteal and endosteal circumference tibia | Children in gross motor skill group have greater tibial circumferences compared to fine motor. |
| Specker BL, 1999 (36) | 6 months old at baseline (males and females) white | 72 | One year randomized control trial with outcome measures at baseline, 9, 12, 15 and 18 months. | Researcher delivered Intervention gross motor vs fine motor PA (5/d week, 15–20 min/d) and calcium supplementations | DXA measured BMC total body | No difference at follow-up between group. |
Cardiometabolic health.
Very few studies have examined the association between physical activity and indicators of cardiometabolic health in children younger than age 6 years. The literature search resulted in the identification of three prospective cohort studies that included outcomes related to serum lipid and lipoprotein levels, respiratory symptoms, and blood pressure (37–39). One study reported that physical activity appeared to have an indirect association with blood lipids and lipoproteins in 3–4 year old children, through its relationship with lower levels of body fatness and higher levels of fitness (37); while another study reported an inverse association between physical activity and diastolic blood pressure in 5–7 year-old children (39). A final study reported that physical activity at 2 years of age was not related to respiratory symptoms such as wheezing or shortness of breath at 3–4 years of age (38). On the basis of the results from these available studies, the Committee determined that there was insufficient evidence available to determine the effects of physical activity on cardiometabolic risk factors.
Cognition.
The Committee reviewed the scientific literature examining the relationship between physical activity and cognition in children under 6 years of age. This review was supported by a search of the literature that was independent of the search described above. That review process, and the Committee’s related conclusions, are described in detail in another article in this supplement (40). Two systematic reviews of the literature on physical activity and cognitive outcomes in preschool-age children met the criteria for inclusion (41, 42). One of those systematic reviews considered seven observational and experimental studies, and the authors reported that six of the seven studies found that a higher amount of physical activity was associated with a beneficial effect on at least one cognitive outcome (41). The second systematic review reported that five of six RCTs found positive effects of selected indicators of cognitive development in 4–6-year-old children (42). The existing studies and the cited systematic reviews point to possible beneficial effects of physical activity on cognitive outcomes in young children, but there is a clear need for more studies with rigorous research protocols.
Dose-response.
Few studies of physical activity and health in children younger than age 6 years have been designed in a manner that allows examination of dose-response relationships. Given the absence of this information in the extant literature, there is a clear need to design experimental trials and prospective cohort studies to answer the question of whether a dose-response relationship exists for physical activity and health during this early period of the lifespan, and if so, what is the nature of that relationship. Such information is important toward not only understanding how physical activity influences health but also toward generating knowledge and support to best provide opportunities for intervention to support public health.
Effect modification.
The studies on physical activity and health in children younger than age 6 years have rarely been designed in a manner that provided for examination of the potential modifying effects of demographic characteristics, such as sex, age, race/ethnicity, weight status, and socioeconomic status. While studies included participants across a range of demographic characteristics, studies tended to control for potential confounders (e.g., sex, body size, lifestyle) but typically did not conduct stratified analyses to examine effect modification. Given the known differences in physical activity and health outcomes by demographic characteristics in older ages, it is important to understand the extent to which the health effects of physical activity may differ across demographic subgroups across the lifespan. Such information would provide additional understanding of whether the dose of physical activity needed to produce health benefits varies across population subgroups.
Discussion
The overall conclusion of the systematic literature review presented in this article was that strong evidence demonstrates that higher amounts of physical activity are associated with more favorable indicators of bone health and with better weight status in children ages 3 to 6 years old. However, there was insufficient evidence to show a relationship between physical activity and indicators of cardiometabolic health in children under 6 years of age. Further, for all health outcomes studied in this age group, evidence was insufficient to determine dose-response relationships and to determine the whether the relationships between physical activity and health were moderated by factors such as age, sex, race/ethnicity, or socioeconomic status. Relatively few studies have addressed the impact of physical activity on health in very young children, and there are a limited number of systematic reviews of this topic. Timmons et al (7) reviewed the relevant literature for children in the 0 to 4 years age range, and studies published up to May, 2011 were included. Their conclusions were generally consistent with those of the present review. While noting widely varying qualities of evidence, they concluded that, among preschoolers, higher levels of physical activity were associated with a number of positive health outcomes including adiposity and indicators of cardiometabolic health.
More recently, systematic reviews have been undertaken to inform the development of the Canadian 24-Hour Movement Guidelines for the Early Years (43). The results of the review of the association between physical activity and health indicators indicated that intervention studies improved motor and cognitive development, and psychosocial and cardiometabolic health, while evidence from observational studies showed that physical activity was associated with favorable motor development, fitness, and bone and skeletal health (44). The Carson et al. review identified 96 studies in children 5 years of age and younger, compared to 25 studies we identified for the current review. However, we applied stricter inclusion criteria, which among other factors, excluded cross-sectional observational studies and studies which delivered parental or group-level interventions. These methodological differences may explain the somewhat different conclusions reached by the two reviews. Nonetheless, the conclusion of both reviews is that physical activity is positively associated with health indicators in pre-school age children.
Weight status/adiposity.
It is well documented that rates of overweight and obesity have increased dramatically in all segments of the U.S. population, and this includes children under 6 years of age (45). As a result of this trend, prevention of childhood obesity has become an important public health priority in the U.S. and other economically developed nations (46). In this context, the findings of the current systematic review are particularly important. It was concluded that there is strong evidence that higher amounts of physical activity are associated with better weight- and adiposity-related outcomes in 3 to 5 year old children. Several important factors were considered by the authors in arriving at that conclusion. First, rigorous standards were applied in selecting studies for inclusion in the review. Second, all studies included in this review applied prospective, observational research designs, which, in the view of the authors, is the best available method for studying the relationship between physical activity and weight/adiposity outcomes. In theory, experimental studies would be important, but there are concerns about the feasibility of treatments that would involve long term, controlled exposures to modified physical activity in children under 6 years of age. Third, most of the studies included in this review used objective, device-based measures of physical activity. Fourth, beneficial effects of higher amounts of physical activity were very consistently reported. Thirteen of the 15 studies included in this review found that more physically active children tended to gain less weight and/or fat mass than their less physically active counterparts. Other systematic reviews have drawn similar conclusions (4), although most have focused primarily on older children.
While the authors found that the available evidence supports the conclusion that physical activity provides important benefits for weight-related outcomes in preschool age children, it is acknowledged that the existing research literature on this topic has important limitations. Because the number of currently available studies is modest, more studies with device-based measures of physical activity, well validated measures of adiposity, and multi-year follow-up periods are needed. Further, future studies should carefully assess factors that might confound the relationship between physical activity and weight-related outcomes. These include diet and sleep behaviors. In addition, studies with large and diverse samples of children will be needed to determine whether or not the physical activity – weight/adiposity association is moderated by demographic factors and to describe dose-response relationships. Future studies will be needed to address these limitations. Nonetheless, it is the position of the authors that currently available evidence indicates that promotion of physical activity should be a major aim of public health efforts to prevent childhood obesity.
Bone health.
Although few studies have focused on physical activity and bone health in preschool children, the results of the existing studies indicated that young children who engaged in bone-strengthening activities or in high levels of total physical activity have stronger bones. This conclusion is supported by observational evidence that the age of independent walking in toddlers is associated with greater lower limb bone strength (47, 48) and experiments that show mechanical loads create positive adaptations in the bones of young animals (49, 50). The evidence related to relationships between physical activity and bone health in children under 6 years of age when combined with the strong evidence that impact and muscle forces due to physical activity cause positive bone adaptations in older children and adolescents (51) indicate the important role of physical activity for ensuring strong and healthy bones throughout the growing years.
Cardiometabolic health.
There is a paucity of information on the relationship between physical activity and cardiometabolic risk factors in children younger than 6 years of age. In general, most pre-school age children have a healthy cardiometabolic profile. Although the primordial prevention of cardiovascular disease is a life-long endeavor, children do not typically begin to develop adverse cardiometabolic health outcomes until after being exposed to poor lifestyle behaviors for several years. With the exception of overweight and obesity, most available studies did not recruit children with elevated cardiometabolic risk factors. Therefore, there is a pressing need for studies among children with elevated levels of risk factors, in addition to the identification of novel cardiometabolic health markers that are sensitive to lifestyle changes such as increased physical activity.
Cognition.
The study of cognition sits within the broader field of brain health, which is a broad term conceptualized as the optimal or maximal functioning of behavioral and biological measures of the brain including subjective experiences that arise from brain function (e.g., attention, mood). Brain health can be measured using biological markers of the brain (e.g., structural brain morphology) or via subjective manifestations of brain function, including mood and anxiety, perceptions of quality of life, cognitive function (e.g., attention and memory), and sleep. Relative to children under the age of 6 years, little is known regarding the relationship of physical activity to cognition and brain health. The available, preliminary evidence points to a beneficial association of physical activity to cognitive and academic outcomes, which should not be surprising given that findings in studies of older children and adults populations is much further along, and has evidenced benefits to brain structure and function, and a variety of cognitive outcomes. Regardless, further research is necessary to extend these effects to children under 6 years of age, and to understand the nature of physical activity effects on cognition in this age group.
Children and youth – 6 to 17 years of age.
The systematic review described above was focused on children under 6 years of age. Though not described in detail in this article, the Committee also reviewed systematic reviews and meta-analyses addressing the relationships between physical activity, sedentary behavior, and health outcomes in school-aged children and youth (ages 6 to 17 years; see detailed search description in the Committee’s report (51)). The findings for 6- to 17-year-olds are consistent with, but go beyond, the findings for preschool-age children (3 to 6 years of age). Similar to 3- to 6-year-olds, higher amounts of physical activity were found to be associated with better indicators of bone health and with reduced risk for excessive increases in weight and adiposity among older children (51). Accordingly, for those two important health outcomes, the Committee concluded that physical activity provides important benefits for young persons across the entire 3 to 17 years age range. However, for several other health outcomes, beneficial effects of physical activity were found for older children but not documentable for children under 6 years of age. These included indicators of cardiometabolic health, cardiorespiratory fitness, muscular fitness, cognition and risk of depression (40, 51). The body of knowledge on physical activity and health is much more robust for school-aged children than for children under 6. Therefore, additional research will be needed to determine whether or not all the benefits of physical activity that have been documented for older children also accrue to those under age 6 years.
Strengths, limitations and delimitations.
The strengths of the review include a well-designed and transparent search and review process. In addition, most of the studies of adiposity or weight status used device-measured physical activity. All the studies of bone health used state-of-the-art bone imaging procedures. The primary limitation is that relatively little research has been conducted on the relationship between physical activity and health in children under age 6 years. The existing volume and quality of research is sufficient to conclude that a beneficial relationship exists for bone health and weight status, but provides insufficient information about dose-response or any potential effect modification by age, sex, or race/ethnicity.
In the context of developing physical activity guidelines for dissemination to the public and professional groups, it is highly desirable to identify a specific amount of physical activity, or range of amounts of activity, that is known to be associated with important health outcomes. Hence the authors’ finding that the existing research is not sufficient to inform conclusions about dose-response relationships is particularly limiting. It was concluded that higher amounts of physical activity are associated with better outcomes for weight/adiposity and bone health than lower amounts of activity. But the available research did not point to a specific dose of activity that was needed to produce these benefits. It is recognized that some authoritative groups have provided public health guidelines on physical activity for children under age 6 years (52–54). These guidelines have recommended that young children engage in three or more hours of total physical activity (light, moderate and vigorous intensity), a level that corresponds approximately to the median for device-based measurement of physical activity in 3 to 5 year old children (8).
Further, it is important to acknowledge that the authors conducted this systematic review within certain delimitations. The charge to the 2018 Physical Activity Guidelines Advisory Committee was to consider new evidence that might inform revision of the 2008 Physical Activity Guidelines for Americans. Children under age 6 years were not included in the 2008 Guidelines because, at that time, very limited research had been conducted on the health effects of physical activity in that age group. Accordingly, an important goal of the 2018 Committee was to determine whether or not the available scientific evidence supported a conclusion that physical activity is related to important health outcomes in children under 6. Hence the focus of the review was on studies in which amount of physical activity, of various types, was examined in relationship to one or more physiologic risk factors for development of non-communicable diseases such as cardiovascular disease, type 2 diabetes and osteoporosis. The Committee did not consider exposures such as the behavioral quality of the physical activity exposure (e.g., enjoyment) or outcomes such as fundamental motor skills. Nonetheless, it is noted that these are important constructs and are worthy of consideration in future comprehensive reviews of physical activity and health in young children.
Recommendations for future research.
In reviewing the research evidence on the relationships between physical activity and health outcomes in children under 6 years of age the committee found many areas in which existing evidence is limited and new studies are needed. Table 3 lists seven research recommendations that, if addressed in future investigations, would address current limitations and markedly expand the body of knowledge on physical activity and health in young people. The rationale for each of these recommendations is provided in the full 2018 Physical Activity Guidelines Advisory Committee Scientific Report (51). In particular there is a need for studies in large samples using rigorous designs and methodologies. Since the Committee’s charge was to address questions and draw conclusions that inform public health guidelines on physical activity, the research recommendations identified by the Committee were selected on the basis of their relevance to the guidelines development process. It is acknowledged that much remains to be learned about the effects of physical activity on health-related factors in children and youth in many areas that are not directly relevant to public health guidance.
Table 3.
Recommendations for further research on physical activity and health in children and youth under 6 years of age
| Conduct randomized controlled trials and prospective observational studies to elucidate the dose-response relationships for physical activity and health outcomes, including adiposity, cardiometabolic health, and bone health. |
| Undertake randomized controlled trials and prospective observational studies to determine whether the health effects of physical activity during early childhood differ across groups based on sex, age, maturational status, race/ethnicity, and socioeconomic status. |
| Conduct randomized controlled and prospective observational studies to examine the health effects of physical activity in young children with elevated risk status based on adiposity, cardiometabolic health, and bone health. |
| Develop valid methods for measuring physical activity and examine the health effects of physical activity in very young children between birth and 2 years. |
| Examine the interactive effects of sedentary behavior and physical activity on health outcomes in young children. |
| Undertake prospective observational studies to examine the effects of physical activity during early childhood on health outcomes later in life. |
| Determine in young children the impact of genetic profiles on behavioral and physiological responses to physical activity and on the health effects of physical activity. |
For children under age 6 years the evidence linking physical activity to health was rated as strong only for two outcomes, weight/adiposity and bone health. Accordingly, there is a great need for research that will bolster our knowledge of other health outcomes, particularly including indicators of cardiometabolic health and cognition. Further, existing research is not adequate to identify clear dose-response relationships or to determine whether or not the health effects of physical activity are influenced by demographic factors such as sex, age, maturational status, race/ethnicity or socioeconomic status. In addition, the research evidence on physical activity and health is very limited in children younger than age 3 years, and for this age group methodological studies are needed to identify appropriate measures of physical activity for use in future investigations.
Summary and conclusions.
The 2018 Physical Activity Guidelines Advisory Committee reviewed the primary research literature addressing the relationship between physical activity and health outcomes in children under 6 years of age. It was concluded that there is strong evidence indicating that higher amounts of physical activity are associated with better bone health and with better weight status/reduced risk for increases in weight and adiposity in children 3 to 6 years of age. The evidence was too limited to support conclusions regarding the effects of physical activity on cardiometabolic health and cognition, to delineate dose-response relationships, or to determine the influence of demographic effect modifiers. The evidence is particularly limited for children under 3 years of age.
The Committee also considered the relationships between physical activity and multiple health outcomes in children and youth across developmental stages from birth to adolescence. Most of the available evidence addressed these relationships in school-aged youth (ages 6–17 years). The conclusions for the older age group were consistent with the findings for children under age 6 in that higher amounts of physical activity were found to be associated with beneficial effects on adiposity and bone health.
Supplementary Material
SDC 1: Table A-Inclusion/Exclusion Criteria
SDC 2: Table B-Nutrition Evidence Library (NEL) Bias Assessment Tool (BAT): Original Research
SDC 3: Table 3-AMSTAR ExBP: SR/MA
Acknowledgments –
The authors thank Janna Borden and Gaye Groover Christmus, MPH of the University of South Carolina and Deborah Galuska, PhD of the Centers for Disease Control and Prevention for their contributions to the development of the manuscript. The authors do not have any conflicts of interest.
This paper is being published as an official pronouncement of the American College of Sports Medicine. This pronouncement was reviewed for the American College of Sports Medicine by members-at-large and the Pronouncements Committee.
Footnotes
Publisher's Disclaimer: Disclaimer: Care has been taken to confirm the accuracy of the information present and to describe generally accepted practices. However, the authors, editors, and publisher are not responsible for errors or omissions or for any consequences from application of the information in this publication and make no warranty, expressed or implied, with respect to the currency, completeness, or accuracy of the contents of the publication. Application of this information in a particular situation remains the professional responsibility of the practitioner; the clinical treatments described and recommended may not be considered absolute and universal recommendations.
The authors do not have any conflicts of interest.
References
- 1.Shephard RJ. Physical Activity and Growth. Chicago: Year Book Medical Publishers; 1982. [Google Scholar]
- 2.Malina RM, Bouchard C, Bar-Or O. Growth, Maturation, and Physical Activity. Champaign, IL: Human Kinetics; 2004. [Google Scholar]
- 3.Poitras VJ, Gray CE, Borghese MM, Carson V, Chaput JP, Janssen I, et al. Systematic review of the relationships between objectively measured physical activity and health indicators in school-aged children and youth. Appl Physiol Nutr Metab. 2016;41(6 Suppl 3):S197–239. doi: 10.1139/apnm-2015-0663. [DOI] [PubMed] [Google Scholar]
- 4.Pate RR, O’Neill JR, Liese AD, Janz KF, Granberg EM, Colabianchi N, et al. Factors associated with development of excessive fatness in children and adolescents: A review of prospective studies. Obes Rev. 2013;14(8):645–58. doi: 10.1111/obr.12035 [doi]. [DOI] [PubMed] [Google Scholar]
- 5.U.S. Department of Health and Human Services. Physical Activity Guidelines Advisory Committee Report. Washington, DC: USDHHS; 2008. [Google Scholar]
- 6.U.S. Department of Health and Human Services. 2008 Physical Activity Guidelines for Americans. 2008.
- 7.Timmons BW, LeBlanc AG, Carson V, Connor GS, Dillman C, Janssen I, et al. Systematic review of physical activity and health in the early years (aged 0–4 years). Appl Physiol Nutr Metab. 2012;37(4):773–92. doi: 10.1139/h2012-070 [doi]. [DOI] [PubMed] [Google Scholar]
- 8.Institute of Medicine. Early Childhood Obesity Prevention Policies. Washington, DC: The National Academies Press; 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Torres A, Tennant BL, Ribeiro-Lucas I, Vaux-Bjerke A, Piercy K, Bloodgood B. Umbrella and systematic review methodology to suppor the 2018 Physical Activity Guidelines Advisory Committee. J Phys Act Health. 2018; 15(11):805–10. [DOI] [PubMed] [Google Scholar]
- 10.Dietary Guidelines Advisory Committee. 2015 Dietary Guidelines Advisory Committee (DGAC) Nutrition Evidence Library Methodology. Washington, DC: USDA, 2017. 01/16/2018. Report No. [Google Scholar]
- 11.Johnson BT, MacDonald HV, Bruneau ML Jr., Goldsby TU, Brown JC, Huedo-Medina TB, et al. Methodological quality of meta-analyses on the blood pressure response to exercise: a review. J Hypertens. 2014;32(4):706–23. doi: 10.1097/HJH.0000000000000097. [DOI] [PubMed] [Google Scholar]
- 12.Berkowitz RI, Agras WS, Korner AF, Kraemer HC, Zeanah CH. Physical activity and adiposity: a longitudinal study from birth to childhood. J Pediatr. 1985;106(5):734–8. [DOI] [PubMed] [Google Scholar]
- 13.Durant RH, Baranowski T, Rhodes T, Gutin B, Thompson WO, Carroll R, et al. Association among Serum-Lipid and Lipoprotein Concentrations and Physical-Activity, Physical-Fitness, and Body-Composition in Young-Children. J Pediatr-Us. 1993;123(2):185–92. doi: Doi 10.1016/S0022-3476(05)81687-7. [DOI] [PubMed] [Google Scholar]
- 14.Jago, Baranowski, Baranowski. BMI from 3–6 y of age is predicted by TV viewing and physical activity, not diet. Int J Obes (Lond). 2005. 29(6):557–64;. [DOI] [PubMed] [Google Scholar]
- 15.Janz KF, Kwon S, Letuchy EM, Eichenberger Gilmore JM, Burns TL, Torner JC, et al. Sustained effect of early physical activity on body fat mass in older children. Am J Prev Med. 2009;37(1):35–40. doi: 10.1016/j.amepre.2009.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Klesges RC, Klesges LM, Eck LH, Shelton ML. A longitudinal analysis of accelerated weight gain in preschool children. Pediatrics. 1995;95(1):126–30. [PubMed] [Google Scholar]
- 17.Leppanen MH, Henriksson P, Delisle Nystrom C, Henriksson H, Ortega FB, Pomeroy J, et al. Longitudinal Physical Activity, Body Composition, and Physical Fitness in Preschoolers. Med Sci Sports Exerc. 2017;49(10):2078–85. doi: 10.1249/MSS.0000000000001313. [DOI] [PubMed] [Google Scholar]
- 18.Li R, O’Connor L, Buckley D, Specker B. Relation of activity levels to body fat in infants 6 to 12 months of age. J Pediatr. 1995;126(3):353–7. [DOI] [PubMed] [Google Scholar]
- 19.Metcalf BS, Voss LD, Hosking J, Jeffery AN, Wilkin TJ. Physical activity at the government-recommended level and obesity-related health outcomes: a longitudinal study (early bird 37). Archives of Disease in Childhood. 2008;93(9):772–7. doi: 10.1136/adc.2007.135012. [DOI] [PubMed] [Google Scholar]
- 20.Moore LL, Gao D, Bradlee ML, Cupples LA, Sundarajan-Ramamurti A, Proctor MH, et al. Does early physical activity predict body fat change throughout childhood? Preventive Medicine. 2003;37(1):10–7. doi: 10.1016/S0091-7435(03)00048-3. [DOI] [PubMed] [Google Scholar]
- 21.Moore LL, Nguyen US, Rothman KJ, Cupples LA, Ellison RC. Preschool physical activity level and change in body fatness in young children. The Framingham Children’s Study. Am J Epidemiol. 1995; 142(9):982–8. [DOI] [PubMed] [Google Scholar]
- 22.Remmers T, Sleddens EFC, Gubbels JS, De Vries SI, Mommers M, Penders J, et al. Relationship between Physical Activity and the Development of Body Mass Index in Children. Med Sci Sport Exer. 2014;46(1):177–84. doi: 10.1249/MSS.0b013e3182a36709. [DOI] [PubMed] [Google Scholar]
- 23.Roberts SB, Savage J, Coward WA, Chew B, Lucas A. Energy expenditure and intake in infants born to lean and overweight mothers. N Engl J Med. 1988;318(8):461–6. doi: 10.1056/NEJM198802253180801. [DOI] [PubMed] [Google Scholar]
- 24.Saakslahti A, Numminen P, Varstala V, Helenius H, Tammi A, Viikari J, et al. Physical activity as a preventive measure for coronary heart disease risk factors in early childhood. Scand J Med Sci Spor. 2004;14(3):143–9. doi: 10.1046/j.1600-0838.2003.00347.x. [DOI] [PubMed] [Google Scholar]
- 25.Sugimori H, Yoshida K, Izuno T, Miyakawa M, Suka M, Sekine M, et al. Analysis of factors that influence body mass index from ages 3 to 6 years: A study based on the Toyama cohort study. Pediatrics International. 2004;46(3):302–10. doi: DOI 10.1111/j.1442-200x.2004.01895.x. [DOI] [PubMed] [Google Scholar]
- 26.Wells JCK, Stanley M, Laidlaw AS, Day JME, Davies PSW. The relationship between components of infant energy expenditure and childhood body fatness. Int J Obesity. 1996;20(9):848–53. [PubMed] [Google Scholar]
- 27.Binkley T, Specker B. Increased periosteal circumference remains present 12 months after an exercise intervention in preschool children. Bone. 2004;35(6):1383–8. doi: 10.1016/j.bone.2004.08.012. [DOI] [PubMed] [Google Scholar]
- 28.Erlandson MC, Kontulainen SA, Chilibeck PD, Arnold CM, Baxter-Jones AD. Bone mineral accrual in 4- to 10-year-old precompetitive, recreational gymnasts: a 4-year longitudinal study. J Bone Miner Res. 2011;26(6):1313–20. doi: 10.1002/jbmr.338. [DOI] [PubMed] [Google Scholar]
- 29.Gruodyte-Raciene R, Erlandson MC, Jackowski SA, Baxter-Jones ADG. Structural Strength Development at the Proximal Femur in 4-to 10-Year-Old Precompetitive Gymnasts: A 4-Year Longitudinal Hip Structural Analysis Study. Journal of Bone and Mineral Research. 2013;28(12):2592–600. doi: 10.1002/jbmr.1986. [DOI] [PubMed] [Google Scholar]
- 30.Jackowski SA, Baxter-Jones ADG, Gruodyte-Raciene R, Kontulainen SA, Erlandson MC. A longitudinal study of bone area, content, density, and strength development at the radius and tibia in children 4–12 years of age exposed to recreational gymnastics. Osteoporosis Int. 2015;26(6):1677–90. doi: 10.1007/s00198-015-3041-1. [DOI] [PubMed] [Google Scholar]
- 31.Janz KF, Gilmore JM, Burns TL, Levy SM, Torner JC, Willing MC, et al. Physical activity augments bone mineral accrual in young children: The Iowa Bone Development study. J Pediatr. 2006;148(6):793–9. doi: 10.1016/j.jpeds.2006.01.045. [DOI] [PubMed] [Google Scholar]
- 32.Janz KF, Gilmore JM, Levy SM, Letuchy EM, Burns TL, Beck TJ. Physical activity and femoral neck bone strength during childhood: the Iowa Bone Development Study. Bone. 2007;41(2):216–22. doi: 10.1016/j.bone.2007.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Janz KF, Letuchy EM, Burns TL, Eichenberger Gilmore JM, Torner JC, Levy SM. Objectively measured physical activity trajectories predict adolescent bone strength: Iowa Bone Development Study. Br J Sports Med. 2014;48(13):1032–6. doi: 10.1136/bjsports-2014-093574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Janz KF, Letuchy EM, Eichenberger Gilmore JM, Burns TL, Torner JC, Willing MC, et al. Early physical activity provides sustained bone health benefits later in childhood. Med Sci Sports Exerc. 2010;42(6):1072–8. doi: 10.1249/MSS.0b013e3181c619b2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Specker B, Binkley T. Randomized trial of physical activity and calcium supplementation on bone mineral content in 3- to 5-year-old children. J Bone Miner Res. 2003;18(5):885–92. doi: 10.1359/jbmr.2003.18.5.885. [DOI] [PubMed] [Google Scholar]
- 36.Specker BL, Mulligan L, Ho M. Longitudinal study of calcium intake, physical activity, and bone mineral content in infants 6–18 months of age. J Bone Miner Res. 1999;14(4):569–76. doi: 10.1359/jbmr.1999.14.4.569. [DOI] [PubMed] [Google Scholar]
- 37.DuRant RH, Baranowski T, Rhodes T, Gutin B, Thompson WO, Carroll R, et al. Association among serum lipid and lipoprotein concentrations and physical activity, physical fitness, and body composition in young children. J Pediatr. 1993;123(2):185–92. [DOI] [PubMed] [Google Scholar]
- 38.Driessen LM, Kiefte-de Jong JC, Jaddoe VW, Hofman A, Raat H, de Jongste JC, et al. Physical activity and respiratory symptoms in children: the Generation R Study. Pediatr Pulmonol. 2014;49(1):36–42. doi: 10.1002/ppul.22839. [DOI] [PubMed] [Google Scholar]
- 39.Knowles G, Pallan M, Thomas GN, Ekelund U, Cheng KK, Barrett T, et al. Physical activity and blood pressure in primary school children: a longitudinal study. Hypertension. 2013;61(1):70–5. doi: 10.1161/HYPERTENSIONAHA.112.201277. [DOI] [PubMed] [Google Scholar]
- 40.Erickson KI, Hillman C, Stillman CM, Ballard RM, Bloodgood B, Conroy DE, et al. Physical activity and cognition: An umbrella review and summary of the Scientific Report for the 2018 Physical Activity Guidelines for Americans Advisory Committee. Med Sci Sports Exerc. 2018;in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Carson V, Hunter S, Kuzik N, Wiebe SA, Spence JC, Friedman A, et al. Systematic review of physical activity and cognitive development in early childhood. J Sci Med Sport. 2016;19(7):573–8. doi: 10.1016/j.jsams.2015.07.011. [DOI] [PubMed] [Google Scholar]
- 42.Zeng N, Ayyub M, Sun H, Wen X, Xiang P, Gao Z. Effects of Physical Activity on Motor Skills and Cognitive Development in Early Childhood: A Systematic Review. Biomed Res Int. 2017;2017:2760716. doi: 10.1155/2017/2760716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tremblay MS, Chaput JP, Adamo KB, Aubert S, Barnes JD, Choquette L, et al. Canadian 24-Hour Movement Guidelines for the Early Years (0–4 years): An Integration of Physical Activity, Sedentary Behaviour, and Sleep. BMC Public Health. 2017;17(Suppl 5):874. doi: 10.1186/s12889-017-4859-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Carson V, Lee EY, Hewitt L, Jennings C, Hunter S, Kuzik N, et al. Systematic review of the relationships between physical activity and health indicators in the early years (0–4 years). BMC Public Health. 2017;17(Suppl 5):854. doi: 10.1186/s12889-017-4860-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Skinner AC, Ravanbakht SN, Skelton JA, Perrin EM, Armstrong SC. Prevalence of Obesity and Severe Obesity in US Children, 1999–2016. Pediatrics. 2018. doi: 10.1542/peds.2017-3459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Institute of Medicine. Preventing Childhood Obesity: Health in the Balance. Washington, D.C.: The National Academies Press; 2005. 2005. [PubMed] [Google Scholar]
- 47.Ireland A, Rittweger J, Schonau E, Lamberg-Allardt C, Viljakainen H. Time since onset of walking predicts tibial bone strength in early childhood. Bone. 2014;68:76–84. doi: 10.1016/j.bone.2014.08.003. [DOI] [PubMed] [Google Scholar]
- 48.Ireland A, Sayers A, Deere KC, Emond A, Tobias JH. Motor Competence in Early Childhood Is Positively Associated With Bone Strength in Late Adolescence. J Bone Miner Res. 2016;31(5):1089–98. doi: 10.1002/jbmr.2775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Warden SJ, Fuchs RK, Castillo AB, Nelson IR, Turner CH. Exercise when young provides lifelong benefits to bone structure and strength. J Bone Miner Res. 2007;22(2):251–9. doi: 10.1359/jbmr.061107. [DOI] [PubMed] [Google Scholar]
- 50.Warden SJ, Galley MR, Hurd AL, Wallace JM, Gallant MA, Richard JS, et al. Elevated mechanical loading when young provides lifelong benefits to cortical bone properties in female rats independent of a surgically induced menopause. Endocrinology. 2013;154(9):3178–87. doi: 10.1210/en.2013-1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Physical Activity Guidelines Advisory Committee. 2018 Physical Activity Guidelines Advisory Committee Scientific Report. Washington, DC: US DHHS, 2018. [Google Scholar]
- 52.Okely AD, Ghersi D, Hesketh KD, Santos R, Loughran SP, Cliff DP, et al. A collaborative approach to adopting/adapting guidelines - The Australian 24-Hour Movement Guidelines for the early years (Birth to 5 years): an integration of physical activity, sedentary behavior, and sleep. BMC Public Health. 2017;17(Suppl 5):869. doi: 10.1186/s12889-017-4867-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Chief Medical Officers of England Scotland Wales and Northern Ireland. Start Active, Stay Active: A Report on Physical Activity for Health from the Four Home Countries Chief Medical Officers. London: Department of Health, Physical Activity, Health Improvement and Protection; 2011. [Google Scholar]
- 54.Tremblay MS, Leblanc AG, Carson V, Choquette L, Connor Gorber S, Dillman C, et al. Canadian Physical Activity Guidelines for the Early Years (aged 0–4 years). Appl Physiol Nutr Metab. 2012;37(2):345–69. doi: 10.1139/h2012-018. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
SDC 1: Table A-Inclusion/Exclusion Criteria
SDC 2: Table B-Nutrition Evidence Library (NEL) Bias Assessment Tool (BAT): Original Research
SDC 3: Table 3-AMSTAR ExBP: SR/MA