Abstract
Purpose:
To provide an overview of relationships between sedentary behavior and mortality as well as incidence of several non-communicable diseases and weight status reported in the 2018 Physical Activity Guidelines Advisory Committee Scientific Report (2018 PAGAC Scientific Report), and to update the evidence from recent studies.
Methods:
Evidence related to sedentary behavior in the 2018 PAGAC Scientific Report was summarized and a systematic review was undertaken to identify original studies published between January 2017 and February 2018.
Results:
The 2018 PAGAC Scientific Report concluded there was strong evidence that high amounts of sedentary behavior increase the risk for all-cause and cardiovascular disease (CVD) mortality and incident CVD and type 2 diabetes. Moderate evidence indicated sedentary behavior is associated with incident endometrial, colon and lung cancer. Limited evidence suggested sedentary behavior is associated with cancer mortality and weight status. There was strong evidence that the hazardous effects of sedentary behavior are more pronounced in physically inactive people. Evidence was insufficient to determine if bout length or breaks in sedentary behavior are associated with health outcomes. The new literature search yielded seven new studies for all-cause mortality, two for CVD mortality, two for cancer mortality, four for type 2 diabetes, one for weight status, and four for cancer; no new studies were identified for CVD incidence. Results of the new studies supported the conclusions in the 2018 PAGAC Scientific Report.
Conclusions:
The results of the updated search add further evidence on the association between sedentary behavior and health. Further research is required on how sex, age, race/ethnicity, socioeconomic status, and weight status may modify associations between sedentary behavior and health outcomes.
Keywords: sitting, mortality, cohort, chronic disease
Introduction
Sedentary behavior is defined as any waking behavior characterized by the expenditure of 1.5 metabolic equivalents of task (MET)s or less of energy while in a sitting, reclining or lying posture (1). On an absolute scale of intensity, sedentary behaviors are at the low end of the physical activity continuum; however, the postural component of the definition suggests that sedentary pursuits may represent distinct behaviors (2). In most research studies, sedentary behavior has been operationalized as daily sitting time, television (TV) viewing, or low counts on an activity monitor such as an accelerometer. Representative data collected by accelerometry in the U.S. National Health and Nutrition Examination Survey (NHANES) indicate that children and adults spend approximately 55% of their awake time (7.7 hours per day) being sedentary (3).
Given that much of the evidence on the negative health effects associated with sedentary behavior has been published in the last decade, the 2008 Physical Activity Guidelines for Americans (4) did not specifically address this (5). However, given the emerging evidence on the negative health effects and the potential public health burden associated with high levels of sedentary behavior in the population, the 2018 Physical Activity Guidelines Advisory Committee decided to review this evidence. In this regard, the interplay between sedentary behavior and physical activity on health were of particular interest.
The purpose of this article is to summarize the evidence on the associations between sedentary behavior and health reviewed by the 2018 Physical Activity Guidelines Advisory Committee and to perform a systematic review of prospective observational studies published subsequently. In addition to updating the systematic review, we identified articles from the searches to provide evidence on the relationship between changes in sedentary behavior and risk of mortality.
2018 Physical Activity Guidelines Advisory Committee Scientific Report
The 2018 Physical Activity Guidelines Advisory Committee (Committee) recently conducted a systematic review of the associations between sedentary behavior and several health outcomes (6). The Committee reviewed the scientific evidence on the associations between sedentary behavior and all-cause mortality, cardiovascular disease mortality, cancer mortality, type 2 diabetes, weight status, cardiovascular disease and cancer published through early 2017. Table 1 provides the specific questions addressed by the Committee in its report.
Table 1.
Questions Related to Sedentary Behavior and Health Outcomes in Adults Addressed by the 2018 Physical Activity Guidelines Advisory Committee
| Major Questions |
|---|
| 1. What is the relationship between sedentary behavior and all-cause mortality? |
| 2. What is the relationship between sedentary behavior and cardiovascular disease mortality? |
| 3. What is the relationship between sedentary behavior and cancer mortality? |
| 4. What is the relationship between sedentary behavior and (1) type 2 diabetes, (2) weight status, (3) cardiovascular disease, and (4) cancer? |
| 5. Does the effect of moderate-to-vigorous physical activity on all-cause mortality vary by amount of sedentary behavior? |
| Subquestions1 |
| a) Is there a dose-response relationship? If yes, what is the shape of the relationship? |
| b) Does the relationship vary by age, sex, race/ethnicity, socioeconomic status, or weight status? |
| c) Is the relationship independent of amounts of light, moderate, or vigorous physical activity? |
| d) Is there any evidence that bouts or breaks in sedentary behavior are important factors? |
The subquestions apply to questions 1 through 4 only.
A single literature search was conducted to answer questions 1, 2, and 3. Subsets of the resulting body of evidence were used to answer each question and relevant subquestions. The search strategy included 1) a search for systematic reviews and meta-analyses, 2) reviewing the original research articles contained in the systematic reviews and meta-analyses, and 3) a search for more recent original research studies published after the systematic reviews and meta-analyses. The systematic literature search to address question 4 included 1) a search for systematic reviews and meta-analyses, and 2) a search of more recent original research studies published after the systematic reviews and meta-analyses. The evidence used to address question 5 was obtained from the articles retrieved for question 1.
Evidence to inform each question was graded as strong, moderate, limited, or not assignable based on several grading criteria, including applicability, generalizability, risk of bias/study limitations, quantity and consistency of results across studies, and magnitude and precision of effect (See Supplementary Table 1; SDC 1, 2018 Physical Activity Guidelines Advisory Committee Grading Criteria)(6). Table 2 provides a summary of the relationships and level of evidence for each health outcome. Overall, there was strong evidence for a direct association between greater amounts of sedentary behavior and higher risk of mortality from all-causes and cardiovascular disease, and for higher risk of incident type 2 diabetes and cardiovascular disease. There was moderate evidence for an association between sedentary behavior and incident cancer (especially colon, endometrial and lung cancer), and limited evidence for associations between sedentary behavior and cancer mortality and weight status. For a detailed summary of the meta-analyses, systematic reviews and original research studies that contributed evidence to these conclusions, please see the PAGAC Scientific Report (Part F, Chapter 2) (6). Specific details on each study can be found in the online supplementary tables (https://health.gov/paguidelines/second-edition/report/supplementary-material.aspx).
Table 2.
Summary of Relationships between Sedentary Behavior and Health Outcomes in the 2018 Physical Activity Guidelines Advisory Committee Scientific Report
| Health Outcome | Level of Evidence for Association | Level of Evidence for Dose-response | Level of Evidence for Variation in Association by Physical Activity | Level of Evidence for Variation in Association by Age, Sex, Race/Ethnicity, Socioeconomic Status or Weight Status? | Level of Evidence for Bouts or Breaks as Important Factors |
|---|---|---|---|---|---|
| All-Cause Mortality | Strong | Strong | Strong | Limited for no interaction by age, sex, race/ethnicity and weight status; Not Assignable for socioeconomic status | Not Assignable |
| Cardiovascular Disease Mortality | Strong | Strong | Moderate | Limited for no interaction by age, sex, race/ethnicity and weight status; Not Assignable for socioeconomic status | Not Assignable |
| Cancer Mortality | Limited | Limited | Not Assignable | Not Assignable | Not Assignable |
| Incident Type 2 Diabetes | Strong | Limited | Not Assignable | Not Assignable | Not Assignable |
| Weight Status | Limited | Limited | Not Assignable | Not Assignable | Not Assignable |
| Incident Cardiovascular Disease | Strong | Strong | Not Assignable | Not Assignable | Not Assignable |
| Incident Cancer | Moderate | Limited | Not Assignable | Not Assignable | Not Assignable |
There was strong evidence for the existence of dose-response associations between sedentary behavior and all-cause mortality, cardiovascular disease mortality, and incident cardiovascular disease, while there was limited evidence for cancer mortality, incident type 2 diabetes, weight status, and incident cancer. Two meta-analyses were identified that reported significant dose-response relationships between daily sitting (7), TV viewing (8), and all-cause mortality. Further, 24 of the 29 original studies that tested for the existence of a dose-response relationship with all-cause mortality reported statistical significance (6). Two meta-analyses tested for dose-response associations between sedentary behavior and incident cardiovascular disease (9, 10). Grontved and Hu (9) reported a significant linear dose-response association between TV viewing and incident fatal and nonfatal cardiovascular disease, while Pandey et al. (10) reported a significant, curvilinear dose-response association with increasing slope of risk for cardiovascular disease at increasingly higher levels of sedentary time.
An important subquestion addressed by the Committee was the degree to which the observed relationships vary by age, sex, race/ethnicity, socioeconomic status, or weight status. For all outcomes, there was insufficient evidence to inform the degree to which socioeconomic status was an effect modifier in the associations with sedentary behavior. For both all-cause and cardiovascular disease mortality, studies generally reported no significant effect modification by age, sex, race/ethnicity, or weight status. Further age-, sex-, race/ethnicity-, and weight status-stratified analyses were generally significant in all strata examined. Evidence was insufficient for other outcomes to determine whether the relationships varied by these factors.
A bout of sedentary behavior can be operationalized as a period of uninterrupted sedentary time, whereas a break in sedentary behavior can be operationalized as a non-sedentary bout in between two sedentary bouts (1). The degree to which bouts and breaks in sedentary behavior are related to health outcomes is of interest. Unfortunately, there was insufficient evidence to inform the degree to which bouts and breaks in sedentary behavior are important factors in the major questions addressed by the Committee. At the time of the review, only one study was identified that included bouts of sedentary time as a variable in a latent class analysis prediction of all-cause mortality (11); no studies could be identified for the other health outcomes. This resulted in a grade of “not assignable” for this subquestion.
The degree to which sedentary behavior and physical activity interact in their associations with health outcomes was of particular interest to the Committee. There was evidence that the associations between sedentary behavior and all-cause mortality (strong) and cardiovascular disease mortality (moderate) vary by level of moderate-to-vigorous physical activity. The effect of sedentary behavior on all-cause and cardiovascular disease mortality is stronger among people who have low amounts of moderate-to-vigorous physical activity. In the meta-analysis of Biswas et al. (12), the summary hazard ratio (HR) for all-cause mortality associated with sedentary time was 1.16 (95% Confidence Interval (CI): 0.84–1.56) among those with high physical activity and 1.46 (95% CI: 1.22–1.75) among those with low physical activity. Further, Ekelund et al. (13) conducted a harmonized meta-analysis using individual-level data from more than 1 million adults and reported that increasingly higher amounts of moderate-to-vigorous physical activity attenuated the relationships between sedentary behavior and all-cause and cardiovascular disease mortality. At the highest amounts of moderate-to-vigorous physical activity, the HRs for all-cause mortality associated with the four levels of sedentary behavior appear to converge at about 1 (reference value). The number of minutes per day needed to achieve this estimated volume of moderate-to-vigorous physical activity (35.5 MET-hours per week) varies inversely with the MET value of the activity, ranging from approximately 40 minutes per day at 8 METs to 50 minutes per day at 6 METs to 100 minutes per day at 3 METs. According to data from the 2015 National Health Interview Survey, the prevalence of people participating in more than 300 minutes per week (~ 43 minutes per day) of moderate-to-vigorous physical activity is approximately 33%, whereas the prevalence of people participating in more than 700 minutes per week (~ 100 minutes per day) is approximately 11% (2018 PAGAC Scientific Report, Figure D1 (6, 14)).
Evidence to inform question 5 was largely derived from the meta-analysis of Ekelund et al. (13). The overall shape of the dose-response relationships between moderate-to-vigorous physical activity and all-cause mortality are generally similar when stratified by level of sitting or TV viewing. However, the relative risks are consistently higher in the high sitting and high TV viewing groups. The reduction in risk of all-cause mortality associated with moderate-to-vigorous physical activity is relatively greater for those who are the most sedentary. This is especially apparent at the lower amounts of moderate-to-vigorous physical activity.
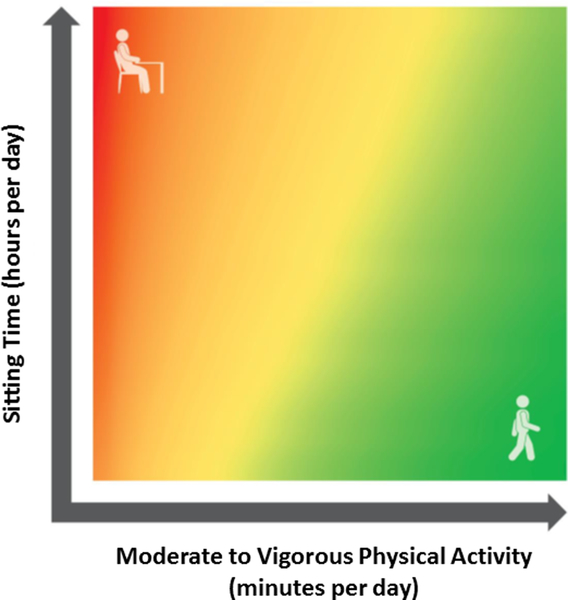
In order to visually describe the joint associations among sedentary behavior, moderate-to-vigorous physical activity and all-cause mortality, the Committee developed a heat map figure which depicts the risk of all-cause mortality associated with various combinations of sitting time and moderate-to-vigorous physical activity (Figure 1). Linear and non-linear regression techniques were used to interpolate the hazard ratios between four levels of sitting time and four levels of moderate-to-vigorous physical activity reported in Ekelund et al. (13). In the heat map, red represents higher risk of all-cause mortality, and green represents lower risk. The greatest risk of mortality is borne by those who sit the most and who do the least moderate-to-vigorous physical activity, while the lowest risk of mortality is achieved by individuals who sit the least and do the most moderate-to-vigorous physical activity.
Figure 1.
Joint associations of sitting time and moderate-to-vigorous physical activity with risk of all-cause mortality. From the 2018 Physical Activity Guidelines Advisory Committee Scientific Report (6), and based on data presented by Ekelund et al. (13).
Methods for Updated Literature Search
This systematic review is reported according to the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines (15). The systematic review followed an established protocol, and was registered prospectively at PROSPERO (#CRD42018092817). Our aim was to update the systematic review conducted by the 2018 Physical Activity Guidelines Advisory Committee and to additionally examine the association between changes in sedentary behavior and risk of all-cause mortality.
Literature Search Strategy
We searched the PubMed, Cochrane, and CINAHL bibliographic databases for studies published in English between January 1, 2017 and February 28, 2018. Two separate searches were conducted for 1) all-cause, cardiovascular disease and cancer mortality, and 2) type 2 diabetes, weight status, cardiovascular disease and cancer. Our search strategy was similar to that employed by the 2018 Physical Activity Guidelines Advisory Committee, and included a comprehensive list of search terms including several combinations of sedentary, sitting, screen time, television, TV, inactivity, physically inactive, sedentarism, etc., along with relevant terms to identify the mortality and disease outcomes of interest (see 2018 Physical Activity Guidelines Advisory Committee Scientific Report (6) for a full list of specific search terms).
Study Selection Criteria
The inclusion criteria were pre-defined, and studies were considered potentially eligible if they were original prospective observational studies, only involved adults aged 18 years and older, were published in English, and investigated the association between sedentary behavior and one of the health outcomes of interest. Studies of non-ambulatory adults, hospitalized patients, or samples with pre-existing health conditions were excluded. A sample size of at least 1000 people was required for the mortality outcomes. Two authors independently reviewed the titles, abstracts and full-text articles, and disagreements about eligibility were resolved through consensus. Although intervention studies that examine changes in chronic disease risk factors in response to alterations in sedentary behavior provide valuable information about potential mechanisms, this type of evidence was beyond the scope of this review which focused on mortality and non-communicable disease outcomes.
The systematic search for the mortality outcomes (all-cause, cardiovascular disease, cancer) identified 780 unique records after duplicates were removed. Of these, 770 were excluded after a review of the titles and abstracts. Based on full-text reviews, four were excluded for all-cause mortality, nine were excluded for cardiovascular disease mortality, and nine were excluded for cancer mortality. One additional study that was relevant for cardiovascular disease and cancer mortality was identified in the search for disease outcomes, and was added at this stage. Thus, the final number of eligible studies was seven for all-cause mortality, two for cardiovascular disease mortality, and two for cancer mortality (See Supplementary Figure 1, SDC 2, article selection process for mortality studies). The systematic search for disease outcomes identified 922 unique records after duplicates were removed. Of these, 910 were excluded after a review of the titles and abstracts. Based on full-text reviews, an additional five studies were excluded, leaving a total of two studies of type 2 diabetes, one study for weight status, and four studies for incident cancer; no studies were identified for incident cardiovascular disease (See Supplementary Figure 2, SDC 3, article selection process for incident condition studies).
Data Extraction and Quality Assessment
The following information was extracted from each eligible article: name of the first author, year of publication, study sample, sample size, age (range or mean), definition of sedentary behavior, dates and length of follow-up, risk estimates with corresponding 95% confidence interval (CI)s comparing levels of sedentary behavior, and whether the study tested and reported a dose-response association. If a study provided several risk estimates, we used the fully adjusted estimate. Extraction of data was performed by one author, and the resulting table was checked by another author.
Quality assessment and risk of bias in the eligible studies was done using the USDA Nutrition Evidence Library (NEL) Bias Assessment Tool (BAT)(16). The NEL BAT uses a domain-based evaluation to help determine whether any systematic error exists that could either over- or underestimate the study results. Selection, performance, detection, and attrition bias are addressed in the NEL BAT. The results of studies’ risk of bias assessments were used to develop a risk of bias summary chart (see Supplementary Table 2, SDC 4, original research bias assessment chart). The NEL BAT assessment was performed by one author, and the resulting table was checked by another author.
Results
Study Characteristics
The main characteristics of the eligible studies identified in the updated search are presented in Table 3 for all-cause, cardiovascular disease and cancer mortality, and in Table 4 for incident type 2 diabetes, weight status, incident cardiovascular disease and incident cancer. All studies used prospective cohort designs, with follow-up periods ranging from 2.3 to 19.4 years. The sedentary exposures varied across studies: five studies used self-reported sitting time (17–21), seven studies used self-reported TV viewing time (17, 18, 22–26), and five studies used accelerometer-derived estimates of sedentary time (27–31). All studies included an estimate of duration of sedentary behavior (sedentary time) as an exposure, while three studies also included a marker of bouts or breaks in sedentary time as an exposure (27–29).
Table 3.
Summary of Original Research Studies on Sedentary Behavior and All-cause, Cardiovascular Disease and Cancer Mortality Published between January 1, 2017 and February 28, 2018.
| Reference | Year of Publication | Population | Sample Size | Age | Definition of Sedentary Behavior | Mortality Follow-up Period | Main Results | Dose-Response |
|---|---|---|---|---|---|---|---|---|
| All-Cause Mortality | ||||||||
| Diaz et al.(27) | 2017 | U.S. Adults; Reasons for Geographic and Racial Differences in Stroke (REGARDS) | 7985 | ≥45 y | Actical waist accelerometry Total sedentary time: <50 counts/min Sedentary bout: consecutive minutes <50 counts/min |
2009–13 to 2015 Median of 4.0 y |
HR (95% CI) across quartiles of total sedentary time in fully adjusted model: Q1 1.00 (reference) Q2: 1.22 (0.74–2.02) Q3: 1.61 (0.99–2.63) Q4: 2.63 (1.60–4.30) P for trend < 0.001 HR (95% CI) across quartiles of total sedentary bout duration in fully adjusted model: Q1 1.00 (reference) Q2: 1.03 (0.67–1.60) Q3: 1.22 (0.80–1.85) Q4: 1.96 (1.31–2.93) P for trend < 0.001 Participants classified as high for both high sedentary time [≥12.5 h/d] and high bout duration [≥10 min/bout]) had the greatest risk for death. Associations of sedentary time and bout duration did not vary by age, sex, race, BMI or moderate-to-vigorous physical activity (p>0.10). |
Yes |
| Hamer et al.(23) | 2017 | U.K. Adults: The English Longitudinal Study of Ageing (ELSA) | 8451 | Mean of 64.8 y | Self-reported TV viewing | 2008–09 to 2012 Mean of 4 y |
HR (95% CI) across levels of TV viewing time in fully adjusted model: <2 h/d: 1.00 (reference) 2–<4 h/d: 1.63 (1.02–2.61) 4-<6 h/d: 1.49 (0.92–2.39) ≥6 h/d: 1.98 (1.25–3.15) Per SD increase: 1.17 (1.06–1.28) |
Yes |
| Rillamas-Sun et al.(21) | 2017 | U.S. Women: Women’s Health Initiative Observational Study | 29,090 | 62–81 y | Self-reported daily sitting time | 1993–98 to 2015 Mean of 13.7 y |
OR (95% CI) of dying before age 85 y across daily sitting categories in fully adjusted model: ≤ 5h/day: 1.00 (reference) 6–9 h/day: 1.02 (0.94–1.11) ≥10 h/day: 1.16 (1.04–1.29) P for trend ≤ 0.05 No interaction by race/ethnicity. |
Yes |
| Theou et al.(31) | 2017 | U.S. Adults; 2003–04 & 2005–06 U.S. National Health and Nutrition Examination Survey (NHANES) |
3141 | ≥50 y | ActiGraph waist accelerometry (≤100 counts/min) | 2003–2006 to 2011 Mean of 6.5 y |
HR (95% CI) per hour of sedentary time in fully adjusted model: 1.15 (1.11–1.20) HR (95% CI) per hour of sedentary time in fully adjusted models, stratified by physical activity level: Physically Inactive 1.20 (1.12–1.29) Physically Active 0.98 (0.78–1.24) HR (95% CI) per hour of sedentary time in fully adjusted models including physical activity, stratified by level of frailty: Frailty Index Score ≤0.1 0.90 (0.70–1.15) Frailty Index Score 0.1 to ≤ 0.2 1.13 (1.00–1.28) Frailty Index Score 0.2 to ≤0.3 1.27 (1.11–1.46) Frailty Index Score >0.3 1.36 (1.22–1.52) |
Yes |
| Imran et al.(24) | 2018 | U.S. African American Adults: Jackson Heart Study (JHS) | 5289 | Mean of 55 y | Self-reported TV viewing | Baseline in 2000–04 Median of 9.9 y |
HR (95% CI) across levels of TV viewing time in fully adjusted model: <2 h/d: 1.00 (reference) 2–<4 h/d: 1.08 (0.86–1.37) ≥4 h/d: 1.48 (1.19–1.83) P for trend = 0.002 The results were similar in models which excluded those who died in the first two years of follow-up, those with low or high BMI, those with low leisure physical activity, those with low eGFR, and those without a high school diploma. |
Yes |
| Jefferis et al.(29) | 2018 | U.K. Older Men: British Regional Heart Study | 1181 | 71–92 y | ActiGraph waist accelerometry Total sedentary time: <100 counts/min Sedentary breaks: interruption of a sedentary bout lasting >1 min |
2010–11 to 2016 Median of 5.0 y |
HR (95% CI) across quartiles of total sedentary time in fully adjusted model: Q1 1.00 (reference) Q2: 1.14 (0.69–1.91) Q3: 1.55 (0.91–2.64) Q4: 2.73 (1.50–4.95) HR per 30 min per day: 1.15 (1.06–1.26) HR (95% CI) across quartiles of sedentary breaks per hour in fully adjusted model: Q1 1.00 (reference) Q2: 1.22 (0.81–1.82) Q3: 0.95 (0.56–1.61) Q4: 1.01 (0.50–2.02) The numbers of minutes spent in sedentary bouts lasting 1–15 min, 16–30, 31–60 and >61 min were all similarly associated with mortality. |
Yes |
| Lee et al.(30) | 2018 | U.S. Women; Women’s Health Study | 16,741 | Mean of 72 y | ActiGraph waist accelerometry Total sedentary time: <200 counts/min |
2011–15 to 2015 Mean of 2.3 y |
HR (95% CI) across quartiles of total sedentary time in fully adjusted model: Q1 1.00 (reference) Q2: 0.97 (0.62–1.50) Q3: 1.18 (0.77–1.82) Q4: 0.92 (0.56–1.50) P for trend = 0.99 |
No |
| Cardiovascular Disease Mortality | ||||||||
| Grace et al.(22) | 2017 | Australian Adults: Australian Diabetes, Obesity and Lifestyle Study (AusDiab) | 8907 | ≥25 y | Self-reported TV viewing | 1999–2000 to 2013 Median of 13.6 y |
HR (95% CI) across levels of TV viewing time in fully adjusted model: Non-Smokers <2 h/d: 1.00 (reference) 2–<4 h/d: 0.93 (0.69–1.26) ≥4 h/d: 1.04(0.69–1.57) P for Trend = 0.99 Current Smokers <2 h/d: 1.00 (reference) 2–<4 h/d: 1.11 (0.46–2.63) ≥4 h/d: 2.02 (0.80–5.12) P for Trend = 0.16 |
No |
| Hamer et al.(23) | 2017 | U.K. Adults: The English Longitudinal Study of Ageing (ELSA) | 8451 | Mean of 64.8 y | Self-reported TV viewing | 2008–09 to 2012 Mean of 4 y |
HR per SD increase in daily TV viewing: 1.22 (1.00–1.49). | Yes |
| Cancer Mortality | ||||||||
| Grace et al.(22) | 2016 | Australian Adults: Australian Diabetes, Obesity and Lifestyle Study (AusDiab) | 8907 | ≥25 y | Self-reported TV viewing | 1999/2000 to 2013 Median of 13.6 y |
HR (95% CI) across levels of TV viewing time in fully adjusted model: Non-Smokers <2 h/d: 1.00 (reference) 2–<4 h/d: 0.92 (0.72–1.19) ≥4 h/d: 0.91(0.61–1.34) P for Trend = 0.52 Current Smokers <2 h/d: 1.00 (reference) 2–<4 h/d: 1.44 (0.77–2.69) ≥4 h/d: 2.27 (1.11–4.67) P for Trend = 0.02 |
Yes: in current smokers only |
| Hamer et al.(23) | 2017 | U.K. Adults: The English Longitudinal Study of Ageing (ELSA) | 8451 | Mean of 64.8 y | Self-reported TV viewing | 2008–09 to 2012 Mean of 4 y |
HR per SD increase in daily TV viewing: 1.16 (0.96–1.39). | No |
BMI, body mass index; eGFR: estimated glomerular filtration rate; CI, confidence interval; HR, hazard ratio; OR, odds ratio; SD: standard deviation; TV, television.
Table 4.
Summary of Original Studies on Sedentary Behavior and Type 2 Diabetes, Weight Status, and Cancer Published Between January 1, 2017 and February 28, 2018.*
| Reference | Year of Publication | Population | Sample Size | Age | Definition of Sedentary Behavior | Follow-up Period | Main Results | Dose-Response |
|---|---|---|---|---|---|---|---|---|
| Type 2 Diabetes | ||||||||
| Joseph et al.(25) | 2017 | U.S. African American Adults; Jackson Heart Study (JHS) | 3252 | 21–94 y | Self-reported TV viewing | 2000–04 to 2005–12 Median of 7.5 y |
IRR (95% CI) across levels of daily TV viewing time in fully adjusted models: ≥4 h/d: 1.00 (reference) 1–3.9 h/d: 0.99 (0.82–1.18) <1 h/d: 0.95 (0.72–1.25) Continuous IRR = 0.98 (0.86–1.11) |
No |
| Stamatakis et al.(17) | 2017 | U.K. Adults: Whitehall II Study | 4811 | Mean of 44 y | Self-reported work-related sitting time, TV viewing time, non-TV leisure time sitting, total leisure sitting time, total sitting time, non-TV total sitting time | 1997–99 to 2011 Mean of 13.0 y |
HR (95% CI) across levels of sedentary behavior in fully adjusted models: Work Sitting <15 h/wk: 1.00 (reference) 15-<35 h/wk: 1.14 (0.87–1.51) ≥35 h/wk: 1.17 (0.89–1.53) P for trend = 0.48 TV Sitting <11 h/wk: 1.00 (reference) 11-<16 h/wk: 1.33 (1.00–1.77) ≥16 h/wk: 1.39 (1.03–1.88) P for trend = 0.05 Non-TV Leisure Sitting at Home <8 h/wk: 1.00 (reference) 8-<16 h/wk: 0.78 (0.57–1.05) ≥16 h/wk: 0.98 (0.70–1.36) P for trend = 0.15 Leisure Sitting at Home <15 h/wk: 1.00 (reference) 15-<25 h/wk: 1.26 (0.97–1.64) ≥25 h/wk: 1.27 (0.98–1.66) P for trend = 0.15 Total Sitting <15 h/wk: 1.00 (reference) 15-<25 h/wk: 0.87 (0.67–1.13) ≥25 h/wk: 1.26 (1.00–1.62) P for trend = 0.01 Total Sitting Excluding TV <15 h/wk: 1.00 (reference) 15-<25 h/wk: 0.93 (0.68–1.27) ≥25 h/wk: 1.23 (0.91–1.66) P for trend = 0.15 After additional adjustment for BMI the results were attenuated and no longer significant for TV sitting and total sitting. |
Yes – for TV sitting and total sitting before adjustment for BMI No – after adjustment for BMI |
| Weight Status | ||||||||
| Barone Gibbs et al.(28) | 2017 | U.S. Adults; Coronary Artery and Risk Development in Young Adults (CARDIA) |
1826 | 38–50 y | ActiGraph waist accelerometry (<100 counts/min) Total sedentary time and bouts of ≥10 min |
2005–06 to 2010–11 ~ 5 y |
Higher total sedentary time at baseline was not associated with 5-year changes in BMI and waist circumference. Each hour of sedentary time at baseline accumulated in bouts of ≥10 min was associated with 0.077 kg/m2 higher gain in BMI (p=0.033) and 0.198 cm higher gain in waist circumference (p=0.028). |
Yes |
| Cancer | ||||||||
| Eaglehouse et al.(18) | 2017 | Chinese Adults Living in Singapore: Singapore Chinese Health Study | 61,321 | 45–74 y | Self-reported TV viewing and “other” sitting activities | 1993–1998 to 2014 Mean of 16.8 y |
HR (95% CI) for incident colorectal cancer across levels of TV viewing in fully adjusted model: <2 h/d: 1.00 (reference) ≥3 h/d: 1.04 (0.95–1.14) HR (95% CI) for incident colorectal cancer across levels of “other” sitting activities in fully adjusted model: None: 1.00 (reference) <1 h/d:: 0.99 (0.87–1.13) 1–2 h/d: 1.00 (0.87–1.15) ≥ 3 h/d 0.99 (0.84–1.17) P for trend = 0.99 |
No |
| Gorczca et al.(19) | 2017 | U.S. Women: Women’s Health Initiative Observational Study | 74,870 | 50–79 y | Self-reported daily sitting time | Median of 13.4 y | HR (95% CI) for incident colorectal cancer across levels of daily sitting time in fully adjusted model: ≤5 h/d: 1.00 (reference) 5.1–9.9 h/d: 1.10 (0.95–1.26) ≥10 h/d: 1.12 (0.92–1.35) P for trend = 0.29 HR (95% CI) for incident rectal cancer across levels of daily sitting time in fully adjusted model: ≤5 h/d: 1.00 (reference) 5.1–9.9 h/d: 1.08 (0.78–1.51) ≥10 h/d: 0.94 (0.59–1.48) P for trend = 0.74 HR (95% CI) for incident colon cancer across levels of daily sitting time in fully adjusted model: ≤5 h/d: 1.00 (reference) 5.1–9.9 h/d: 1.10 (0.95–1.28) ≥10 h/d: 1.14 (0.92–1.40) P for trend = 0.25 No interaction between sitting time and physical activity (p=0.62), age group (p=0.97), BMI (p=0.66) or employment status (p=0.99). |
No |
| Nomura et al.(20) | 2017 | U.S. Women; Women’s Health Initiative Observational Study | 70,233 | 50–79 y | Self-reported daily sitting time and total sedentary time | 1994–98 to 2015 | HR (95% CI) for incident postmenopausal breast cancer across levels of daily sitting time in fully adjusted model: ≤5 h/d: 1.00 (reference) 6–9 h/d: 1.03 (0.96–1.11) ≥10 h/d: 1.00 (0.92–1.09) P for trend = 0.88 Continuous HR (h/d) = 1.00 (0.98–1.02) No interactions between sitting and race/ethnicity, hormone receptor status, BMI, weight gain since age 18, waist circumference, or wait-to-hip ratio. |
No |
| Ukawa et al.(26) | 2018 | Japanese Women; Japan Collaborative Cohort Study for Evaluation of Cancer Risk (JACC Study) | 34,758 | 40–79 y | Self-reported TV viewing | 1988–90 to 2009 Median of 19.4 y |
HR (95% CI) for incident ovarian cancer across levels of TV viewing time in fully adjusted model: <2 h/d: 1.00 (reference) 2–2.9 h/d: 1.03 (0.70–1.50) 3–3.9 h/d: 1.18 (0.82–1.70) 4–4.9 h/d: 0.81 (0.54–1.21) ≥5 h/d: 2.15 (1.54–2.99) |
Not tested |
BMI, body mass index; CI, confidence interval; HR, hazard ratio; IRR, incident rate ratio; OR, odds ratio; RR, relative risk; TV, television.
no studies were identified for incident cardiovascular disease.
Mortality Outcomes
Seven studies reported on the association between sedentary behavior and all-cause mortality (Table 3) (21, 23, 24, 27, 29–31). Six of the studies reported a statistically significant association (21, 23, 24, 27, 29, 31). For example, an analysis from the Women’s Health Initiative reported a significant (p<0.05) association between self-reported daily sitting time and all-cause mortality (odds ratio for dying before age 85 for ≥10 h/day versus < 5 h/day = 1.16 (95% CI: 1.04–1.29)) over 13.7 years of follow-up (21). Two additional studies, one from the United Kingdom and one among African Americans, demonstrated significant associations between daily TV viewing and all-cause mortality (23, 24). Hamer et al. reported a HR for all-cause mortality of 1.98 (95% CI: 1.25–3.15) comparing ≥6 h/d versus <2 h/d of TV viewing (23), while Imran et al. reported a HR for all-cause mortality of 1.48 (95% CI: 1.19–1.83) comparing ≥4 h/d < 2 h/d of TV viewing (24). Three studies that used accelerometer-derived estimates of sedentary time as the exposure reported a significant association with all-cause mortality (27, 29, 31), while one did not (30). The three positive studies were in samples of US and UK adults and had follow-up period ranging from 4.0 to 6.5 years, whereas the negative study was conducted among older US women (mean age = 72 y), with a mean follow-up time of 2.3 y (Table 3). Among the three positive studies, Diaz et al. (27) and Jefferis et al.(29) reported HRs of 2.63 (95% CI: 1.60–4.30) and 2.73 (95% CI: 1.50–4.95), respectively, for the upper versus lowest quartiles of sedentary time, while Theou et al.(31) reported a HR of 1.15 (95% CI: 1.11–1.20) per each additional hour of sedentary time.
In addition to total duration of sedentary behavior, two studies examined the effects of bouts or breaks in sedentary behavior in relation to all-cause mortality (27, 29). Diaz and colleagues reported a significant association (p for trend <0.001) between bout duration and all-cause mortality in US adults, and participants classified as both highly sedentary (≥12 h/d) and with high bout duration (≥10 min/bout) had the highest risk of death (27). On the other hand, Jefferis and colleagues reported that neither breaks in sedentary behavior nor sedentary bout duration were related to all-cause mortality in a sample of older men (ages 71–92 y) from the UK (29).
Two studies reported on the association between sedentary behavior and cardiovascular disease mortality (22, 23). Grace and colleagues reported a significant association between TV viewing and cardiovascular disease mortality among smokers (but not non-smokers) after adjustment for age and sex in the Australian Diabetes, Obesity and Lifestyle Study (AusDiab) (22). However, this association was no longer significant after the inclusion of additional covariates in the model. On the other hand, Hamer and colleagues reported a multivariable-adjusted HR of 1.22 (95% CI: 1.00–1.49) per standard deviation of daily TV viewing for cardiovascular disease mortality in the English Longitudinal Study of Ageing (23).
Two studies reported on the association between sedentary behavior and cancer mortality (22, 23). Hamer and colleagues reported a non-significant HR of 1.16 (95% CI: 0.96–1.39) per standard deviation of daily TV viewing for cancer mortality in the English Longitudinal Study of Ageing (15). Results from the AusDiab study indicated a significant association between TV viewing and cancer mortality among smokers (p for trend = 0.02) but not among non-smokers (p for trend = 0.52) (22).
A total of six of seven studies reported a dose-response association between sedentary behavior and all-cause mortality (Table 3). Only one of two studies of cardiovascular disease mortality and one of two studies of cancer mortality reported dose-response associations. Few studies formally tested for interactions between sedentary behavior and demographic characteristics on mortality outcomes; however, Rillamas-Sun et al. reported no interaction by race/ethnicity on all-cause mortality in the Women’s Health Initiative (21). Diaz and colleagues reported that the positive associations of sedentary time and bout duration with all-cause mortality did not vary by age, sex, race, BMI or moderate-to-vigorous physical activity (27). Further, Imran et al. reported that in African Americans the results were similar when they excluded those with high and low BMI, those with low leisure physical activity, and those without a high school diploma (24). Theou and colleagues reported a significant association between accelerometer-derived sedentary time and all-cause mortality in NHANES; the association was statistically significant in physically inactive adults but not in physically active adults (31).
Diseases and Conditions
Two studies were identified that examined the association between sedentary behavior and incident type 2 diabetes (17, 25). Stamatakis and colleagues reported a significant association of TV sitting and total sitting with incident diabetes in UK adults enrolled in the Whitehall II study in models adjusting for several covariates, but the results were attenuated and were no longer significant after adjustment for BMI (17). Joseph and colleagues reported no associations between self-reported TV viewing and incident diabetes in African American adults in the Jackson Heart Study, both before and after including BMI as a covariate (25).
A single study was identified that examined the association between sedentary behavior and weight status (28). Among adults in the CARDIA Study, there was no association between total duration of sedentary behavior and 5-year changes in BMI or waist circumference. However, each additional hour of sedentary time accumulated in bouts of greater than or equal to 10 min was associated with greater gain in BMI (p = 0.033) and waist circumference (p = 0.028) (Table 4).
Four studies were identified that addressed the association between sedentary behavior and incident cancer: two studied colorectal cancer (18, 19), one studied breast cancer (20), and one studied ovarian cancer (26). Neither of the two studies of colorectal cancer reported a significant effect of sedentary behavior (TV viewing or sitting time) on cancer incidence (Table 4). Nomura and colleagues reported no significant association between sedentary behavior and incident breast cancer in post-menopausal US women in the Women’s Health Initiative Observational Study (20). On the other hand, Ukawa and colleagues reported that Japanese women who watched TV for greater than or equal to 5 h/day were more likely to develop ovarian cancer than those who watched TV for less than 2 h/day (HR 2.15; 1.54–2.99). Two studies tested for interactions, and reported no interactions between sedentary behavior and race/ethnicity, age, hormone receptor status, BMI, weight gain since age 18, waist circumference, waist-to-hip ratio, employment status or physical activity (19, 20).
A total of six of the seven studies of sedentary behavior, disease incidence or weight status tested for dose-response associations (17–20, 25, 28). Only Barone-Gibbs and colleagues reported significant dose-response associations - between sedentary time and weight status (BMI and waist circumference) (28).
Changes in Sedentary Behavior and Risk of Mortality
We identified several papers from the original systematic review search (32–35) and the updated search (36) that addressed changes in sedentary behavior over time and risk of mortality (n = 4 for all-cause mortality, n = 1 for cardiovascular disease mortality) (Table 5). In each of the studies, mortality rates were compared across categories of changes in sitting time (consistently sedentary, increased or decreased sedentary time, or consistently non-sedentary). Changes in sedentary time were evaluated over approximately 2 to 11 years, and the mean or median follow-up time for mortality surveillance ranged from approximately 5 to 9 years following the second assessment of sedentary behavior. In all studies, the risk of mortality was significantly lower in those who were consistently non-sedentary over time, compared to those who were consistently sedentary. In general, those who decreased sedentary behavior over time had an intermediate risk of mortality, compared to those who were consistently sedentary or non-sedentary. Three studies reported lower risk of mortality associated with increased sedentary behavior over time, compared to those who were consistently sedentary (32, 33, 36); while two studies reported an increased risk of mortality among those who increased sedentary behavior over time, compared to those who were consistently sedentary (34, 35). It is plausible that using two measurements of sedentary behavior over a period of time may be a better marker of long-term levels of sedentary behavior rather than a measure of precise changes over time given the self-reported nature of the data. Two concordant responses may classify participants more accurately than two discordant responses over time, making the later more susceptible misclassification and inconsistent findings.
Table 5.
Summary of Original Studies on Changes in Sedentary Behavior and Mortality.
| Authors | Year of Publication | Population | Sample Size | Age (y) | Definition of Sedentary Behavior | Mortality Follow-up Period | Main Results |
|---|---|---|---|---|---|---|---|
| Leon-Munoz et al.(32) | 2013 | Spanish Adults | 2635 | ≥60 y | Changes in daily sitting time between 2001–2003 | 2003 to 2011 | HR (95% CI) for all-cause mortality across categories of sitting time in fully adjusted model: Consistently Sedentary: 1.00 (reference) Newly Sedentary: 0.91 (0.76–1.10) Formerly Sedentary: 0.86 (0.70–1.05) Consistently Non-sedentary: 0.75 (0.62–0.90) |
| Lee et al.(33) | 2015 | U.S. Women; Women’s Health Initiative (WHI) |
77,801 | 50–79 y | Changes in daily sitting time from baseline and year 6 | 1998 to 2008 Mean of 5.1 y |
HR (95% CI) for all-cause mortality across categories of sitting time in fully adjusted model: Consistently High Sitting: 1.00 (reference) Increased Sitting: 0.79 (0.58–1.07) Decreased Sitting: 0.71 (0.54–0.95) Consistently Low Sitting: 0.49 (0.39–0.63) |
| Keadle et al.(34) | 2015 | U.S. Adults; NIH-AARP Diet and Health Study |
165,087 | 50–71 y | Changes in TV viewing time between 1994–96 and 2004–06 | 2004–2006 to 2011 Mean of 6.6 y |
HR (95% CI) for all-cause mortality across categories of TV viewing in fully adjusted model: Consistent 5+ h/day: 1.28 (1.21–1.34) Decreased from 5+ to 3–4 h/day: 0.85 (0.80–0.91) Decreased from 5+ to <3 h/day: 0.88 (0.79–0.97) Increased from <3 to 3.4 h/day: 1.17 (1.10–1.24) Increased from <3 to 5+ h/day: 1.45 (1.32–1.58) Consistent <3 h/day: 1.0 (reference) |
| Grunseit et al.(35) | 2017 | Norwegian Adults; Nord-Trondelag Health Study (HUNT) |
25,651 | ≥20 y | Changes in daily sitting time between 1995–97 and 2006–08 | 2006–2008 to 2013 Mean of 6.2 y |
HR (95% CI) for all-cause mortality across categories of sitting time in fully adjusted model: Consistently High Sitting: 1.26 (1.06–1.51) Increased Sitting: 1.51 (1.28–2.78) Decreased Sitting: 1.03 (0.88–1.20) Consistently Low Sitting: 1.00 (reference) |
| Cabanas-Sanchez et al.(36) | 2017 | Spanish Adults | 2657 | ≥60 y | Changes in daily sitting time between 2001 and 2003 | 2003 to 2014 Mean of 9.2 y |
HR (95% CI) of cardiovascular disease mortality across categories of sitting time in fully adjusted model: Consistently Sedentary: 1.00 (reference) Newly Sedentary: 1.18 (0.87–1.59) Formerly Sedentary: 0.77 (0.56–1.07) Consistently Non-sedentary: 0.67 (0.46–0.96) |
CI, confidence interval; HR, hazard ratio.
Discussion
The results from the updated search provide further evidence of an association between sedentary behavior and all-cause mortality. Further, the new results from studies of changes in sedentary behavior and mortality suggest that individuals who maintain sedentary behavior over time have the highest risk of mortality, those with sustained low levels of sedentary behavior have lowest risk, and those who report changes in sedentary behavior have an intermediate mortality risk. The updated results obtained for cardiovascular disease mortality (22, 23) do not alter the strength of evidence for the strong association with sedentary behavior. Although Grace and colleagues did not find a significant multivariable-adjusted association between TV viewing and cardiovascular disease mortality when the AusDiab sample was stratified by smoking status (22), these results are in contrast with an earlier report from that cohort that reported a HR of 1.80 (1.00–3.25) between high amounts of TV viewing (≥4 h/d versus <2 h/d) and cardiovascular disease mortality in the full sample (8). The smaller sample size and small number of events in the sub-group analyses likely contributed to the non-significant results. The two new studies identified for cancer mortality (22, 23) do not alter the conclusion of the Committee that the evidence for an association between sedentary behavior and cancer mortality is limited. Associations between sedentary behavior and cancer mortality are affected by cancer screening and treatment availability and efficacy. A limitation of most studies is a failure to take these factors into account.
Similar to the results of previous studies on the association between sedentary behavior and type 2 diabetes, the observed associations in the updated review are not statistically significant in fully-adjusted models where BMI is included as a covariate (17, 25). The effects of sedentary behavior on risk of type 2 diabetes may be operating, in part, through its association with BMI; however, whether or not BMI is in the causal pathway between sedentary behavior and type 2 diabetes is not known. The extent to which sedentary behavior and BMI represent independent risk factors will require further research to disentangle the effects of BMI and sedentary behavior on risk of incident disease, especially type 2 diabetes.
Strong evidence demonstrates that the association between sedentary behavior and all-cause mortality is more pronounced among physically inactive people. In addition, individuals who are highly sedentary appear to require higher amounts of physical activity to achieve the same level of absolute mortality risk as those who are less sedentary (37). Therefore, moderate-to-vigorous physical activity should be part of every adult’s lifestyle, especially for those who are sedentary for large portions of the day. These results also illustrate the need to individualize and tailor lifestyle recommendations for maximum benefit to the individual, which will in turn will have a greater impact on population health. Further, the finding that the association between physical activity and health varies by level of sedentary behavior also highlights the importance of integrating sedentary behavior and physical activity guidelines
U.S. adults spend a large portion of each day engaging in sedentary behavior (3). Therefore, limiting excessive time spent sitting would reduce the population health impact associated with premature mortality and several major chronic diseases such as type 2 diabetes, cardiovascular disease, and several cancers. For physically inactive adults, replacing sedentary behavior with light intensity physical activities is likely to produce some health benefits; however, among all adults, replacing sedentary behavior with higher intensity physical activities may produce even greater benefits (38–41). The updated systematic review identified several new papers addressing the relationship between sedentary behavior and health outcomes. However, the new studies did not provide results that would change the levels of evidence that addressed the Committee’s questions.
Several research recommendations were generated by this work. As described in the introduction, the current consensus definition of sedentary behavior has both an energy expenditure component (≤ 1.5 METS) and a postural component (sitting, reclining or lying) (1). There is a pressing need to develop objective field methods to simultaneously assess these two components of the definition that can be applied in both surveillance and research settings in order to properly quantify time spent in sedentary behavior. Analysis strategies to identify different bout lengths as well as breaks in sedentary behavior vary among studies and is also an important area for future research. Further, research using prospective cohorts is required 1) on the interactive effects of physical activity (especially light intensity activity) and sedentary behavior on mortality and incident CVD, 2) on the role of bouts and breaks in sedentary behavior in relation to mortality and other health outcomes, and 3) on disentangling the independent effects of sedentary behavior and adiposity on risk of type 2 diabetes, and the degree to which adiposity may be in the causal pathway in this association. Further research is also required to determine how sex, age, race/ethnicity, socioeconomic status, and weight status relate to the association between sedentary behavior and cardiovascular disease incidence and mortality. Finally, randomized controlled trials are required to test the health effects of interventions to replace time spent in sedentary behaviors with standing and light, moderate, and vigorous intensity activity.
Supplementary Material
Acknowledgements
The authors gratefully acknowledge the contributions of Emily Bhutiani, MS (National Cancer Institute, National Institutes of Health through June 2017) and Kyle Sprow, MPH (National Cancer Institute, National Institutes of Health) for management support; Anne Brown Rodgers, HHS consultant for technical writing support; and ICF librarians, abstractors, and additional support staff.
Source of Funding
The results of this study do not constitute endorsement by ACSM, and are presented clearly, honestly, and without fabrication, falsification, or inappropriate manipulation. The Committee's work was supported by the U.S. Department of Health and Human Services (HHS). Committee members were reimbursed for travel and per diem expenses for the five public meetings; Committee members volunteered their time. Dr. Jakicic received an honorarium for serving on the Scientific Advisory Board for Weight Watchers International and was a co-investigator on a grant awarded to the University of Pittsburgh by Weight Watchers International.
Role of the Funder/Sponsor
HHS staff provided general administrative support to the Committee and assured that the Committee adhered to the requirements for Federal Advisory Committees. HHS also contracted with ICF, a global consulting services company, to provide technical support for the literature searches conducted by the Committee. HHS and ICF staff collaborated with the Committee in the design and conduct of the searches by assisting with the development of the analytical frameworks, inclusion/exclusion criteria, and search terms for each primary question; using those parameters, ICF performed the literature searches.
Footnotes
Conflicts of Interest
The authors report no other potential conflicts of interest.
Publisher's Disclaimer: This paper is being published as an official pronouncement of the American College of Sports Medicine. This pronouncement was reviewed for the American College of Sports Medicine by members-at-large and the Pronouncements Committee. Disclaimer: Care has been taken to confirm the accuracy of the information present and to describe generally accepted practices. However, the authors, editors, and publisher are not responsible for errors or omissions or for any consequences from application of the information in this publication and make no warranty, expressed or implied, with respect to the currency, completeness, or accuracy of the contents of the publication. Application of this information in a particular situation remains the professional responsibility of the practitioner; the clinical treatments described and recommended may not be considered absolute and universal recommendations.
References
- 1.Tremblay MS, Aubert S, Barnes JD, Saunders TJ, Carson V, Latimer-Cheung AE, et al. Sedentary Behavior Research Network (SBRN) - Terminology consensus project process and outcome. Int J Behav Nutr Phys Act 2017;14(1):75. doi: 10.1186/s12966-017-0525-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barone Gibbs B, Hergenroeder AL, Katzmarzyk PT, Lee IM, Jakicic JM. Definition, measurement, and health risks associated with sedentary behavior. Med Sci Sports Exerc 2015;47(6):1295–300. doi: 10.1249/MSS.0000000000000517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Matthews CE, Chen KY, Freedson PS, Buchowski MS, Beech BM, Pate RR, et al. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am J Epidemiol 2008;167:875–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.U.S. Department of Health and Human Services. 2008 Physical Activity Guidelines for Americans Washington, DC: US Government Printing Office; 2008. 62 p. [Google Scholar]
- 5.US Department of Health and Human Services. 2008 Physical Activity Guidelines for Americans: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2008. 61 p. [Google Scholar]
- 6.2018 Physical Activity Guidelines Advisory Committee. Physical Activity Guidelines Advisory Committee Scientific Report Washington, D.C.: U.S. Department of Health and Human Services; 2018. 779 p. [Google Scholar]
- 7.Chau JY, Grunseit AC, Chey T, Stamatakis E, Brown WJ, Matthews CE, et al. Daily sitting time and all-cause mortality: a meta-analysis. PloS One 2013;8(11):e80000. doi: 10.1371/journal.pone.0080000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sun JW, Zhao LG, Yang Y, Ma X, Wang YY, Xiang YB. Association between television viewing time and all-cause mortality: A meta-analysis of cohort studies. Am J Epidemiol 2015;182(11):908–16. doi: 10.1093/aje/kwv164. [DOI] [PubMed] [Google Scholar]
- 9.Grontved A, Hu FB. Television viewing and risk of type 2 diabetes, cardiovascular disease, and all-cause mortality: a meta-analysis. JAMA 2011;305(23):2448–55. doi: 305/23/2448 [pii] 10.1001/jama.2011.812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pandey A, Salahuddin U, Garg S, Ayers C, Kulinski J, Anand V, et al. Continuous dose-response association between sedentary time and risk for cardiovascular disease: A meta-analysis. JAMA Cardiol 2016;1(5):575–83. doi: 10.1001/jamacardio.2016.1567. [DOI] [PubMed] [Google Scholar]
- 11.Evenson KR, Herring AH, Wen F. Accelerometry-assessed latent class patterns of physical activity and sedentary behavior with mortality. Am J Prev Med 2017;52(2):135–43. Epub 2017/01/23. doi: 10.1016/j.amepre.2016.10.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Biswas A, Oh PI, Faulkner GE, Bajaj RR, Silver MA, Mitchell MS, et al. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: A systematic review and meta-analysis. Ann Intern Med 2015;162(2):123–32. doi: 10.7326/M14-1651. [DOI] [PubMed] [Google Scholar]
- 13.Ekelund U, Steene-Johannessen J, Brown WJ, Fagerland MW, Owen N, Powell KE, et al. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet 2016;388:1302–10. doi: 10.1016/S0140-6736(16)30370-1. [DOI] [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention NCfHS. National Health Interview Survey (NHIS), 1997–2015: 2015 data release https://www.cdc.gov/nchs/nhis/nhis_2015_data_release.htm. Updated November 3, 2017. Accessed January 11, 2018 2018.
- 15.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 2009;62(10):1006–12. doi: 10.1016/j.jclinepi.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 16.2015 Dietary Guidelines Advisory Committee. Scientific Report of the 2015 Dietary Guidelines Advisory Committee Washington, D.C.: U.S Department of Health and Human Services and U.S. Department of Agriculture; 2015. [Google Scholar]
- 17.Stamatakis E, Pulsford RM, Brunner EJ, Britton AR, Bauman AE, Biddle SJ, et al. Sitting behaviour is not associated with incident diabetes over 13 years: the Whitehall II cohort study. Br J Sports Med 2017;51(10):818–23. doi: 10.1136/bjsports-2016-096723. [DOI] [PubMed] [Google Scholar]
- 18.Eaglehouse YL, Koh WP, Wang R, Aizhen J, Yuan JM, Butler LM. Physical activity, sedentary time, and risk of colorectal cancer: the Singapore Chinese Health Study. Eur J Cancer Prev 2017;26(6):469–75. doi: 10.1097/CEJ.0000000000000369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gorczyca AM, Eaton CB, LaMonte MJ, Garcia DO, Johnston JD, He K, et al. Association of physical activity and sitting time with incident colorectal cancer in postmenopausal women. Eur J Cancer Prev 2017;epub ahead of print. doi: 10.1097/CEJ.0000000000000351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nomura SJO, Dash C, Sheppard VB, Bowen D, Allison M, Barrington W, et al. Sedentary time and postmenopausal breast cancer incidence. Cancer Causes Control 2017;28(12):1405–16. doi: 10.1007/s10552-017-0968-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rillamas-Sun E, LaMonte MJ, Evenson KR, Thomson CA, Beresford SA, Coday MC, et al. The influence of physical activity and sedentary behavior on living to age 85 years without disease and disability in older women. The journals of gerontology 2017. doi: 10.1093/gerona/glx222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Grace MS, Lynch BM, Dillon F, Barr EL, Owen N, Dunstan DW. Joint associations of smoking and television viewing time on cancer and cardiovascular disease mortality. Int J Cancer 2017;140:1538–44. doi: 10.1002/ijc.30580. [DOI] [PubMed] [Google Scholar]
- 23.Hamer M, Yates T, Demakakos P. Television viewing and risk of mortality: Exploring the biological plausibility. Atherosclerosis 2017;263:151–5. doi: 10.1016/j.atherosclerosis.2017.06.024. [DOI] [PubMed] [Google Scholar]
- 24.Imran TF, Ommerborn M, Clark C, Correa A, Dubbert P, Gaziano JM, et al. Television viewing time, physical activity, and mortality among African Americans. Prev Chronic Dis 2018;15:E10. doi: 10.5888/pcd15.170247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Joseph JJ, Echouffo-Tcheugui JB, Talegawkar SA, Effoe VS, Okhomina V, Carnethon MR, et al. Modifiable lifestyle risk factors and incident diabetes in African Americans. Am J Prev Med 2017;53(5):e165–e74. doi: 10.1016/j.amepre.2017.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ukawa S, Tamakoshi A, Mori M, Ikehara S, Shirakawa T, Yatsuya H, et al. Association between average daily television viewing time and the incidence of ovarian cancer: findings from the Japan Collaborative Cohort Study. Cancer Causes Control 2018;29(2):213–9. doi: 10.1007/s10552-018-1001-8. [DOI] [PubMed] [Google Scholar]
- 27.Diaz KM, Howard VJ, Hutto B, Colabianchi N, Vena JE, Safford MM, et al. Patterns of sedentary behavior and mortality in U.S. middle-aged and older adults: A national cohort study. Ann Intern Med 2017;167:465–75. doi: 10.7326/M17-0212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Barone Gibbs B, Pettee Gabriel K, Carnethon MR, Gary-Webb T, Jakicic JM, Rana JS, et al. Sedentary time, physical activity, and adiposity: Cross-sectional and longitudinal associations in CARDIA. Am J Prev Med 2017;53(6):764–71. doi: 10.1016/j.amepre.2017.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jefferis BJ, Parsons TJ, Sartini C, Ash S, Lennon LT, Papacosta O, et al. Objectively measured physical activity, sedentary behaviour and all-cause mortality in older men: does volume of activity matter more than pattern of accumulation? Br J Sports Med 2018. doi: 10.1136/bjsports-2017-098733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lee IM, Shiroma EJ, Evenson KR, Kamada M, LaCroix AZ, Buring JE. Accelerometer-measured physical activity and sedentary behavior in relation to all-cause mortality: The Women’s Health Study. Circulation 2018;137(2):203–5. doi: 10.1161/CIRCULATIONAHA.117.031300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Theou O, Blodgett JM, Godin J, Rockwood K. Association between sedentary time and mortality across levels of frailty. CMAJ 2017;189(33):E1056–E64. doi: 10.1503/cmaj.161034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Leon-Munoz LM, Martinez-Gomez D, Balboa-Castillo T, Lopez-Garcia E, Guallar-Castillon P, Rodriguez-Artalejo F. Continued sedentariness, change in sitting time, and mortality in older adults. Med Sci Sports Exerc 2013;45:1501–7. doi: 10.1249/MSS.0b013e3182897e87. [DOI] [PubMed] [Google Scholar]
- 33.Lee J, Kuk JL, Ardern CI. The relationship between changes in sitting time and mortality in post-menopausal US women. J Public Health 2016;38(2):270–8. doi: 10.1093/pubmed/fdv055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Keadle SK, Arem H, Moore SC, Sampson JN, Matthews CE. Impact of changes in television viewing time and physical activity on longevity: a prospective cohort study. Int J Behav Nutr Phys Act 2015;12:156. doi: 10.1186/s12966-015-0315-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Grunseit AC, Chau JY, Rangul V, Holmen TL, Bauman A. Patterns of sitting and mortality in the Nord-Trondelag health study (HUNT). Int J Behav Nutr Phys Act 2017;14(1):8. doi: 10.1186/s12966-016-0457-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cabanas-Sanchez V, Guallar-Castillon P, Higueras-Fresnillo S, Rodriguez-Artalejo F, Martinez-Gomez D. Changes in sitting time and cardiovascular mortality in older adults. Am J Prev Med 2018;54(3):419–22. doi: 10.1016/j.amepre.2017.10.010. [DOI] [PubMed] [Google Scholar]
- 37.Katzmarzyk PT, Pate RR. Physical activity and mortality: The potential impact of sitting. Trans J ACSM 2017;2:32–3. [Google Scholar]
- 38.Fishman EI, Steeves JA, Zipunnikov V, Koster A, Berrigan D, Harris TA, et al. Association between objectively measured physical activity and mortality in NHANES. Med Sci Sports Exerc 2016;48(7):1303–11. Epub 2016/02/06. doi: 10.1249/MSS.0000000000000885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Matthews CE, Keadle SK, Troiano RP, Kahle L, Koster A, Brychta R, et al. Accelerometer-measured dose-response for physical activity, sedentary time, and mortality in US adults. Am J Clin Nutr 2016;104(5):1424–32. Epub 2016/11/03. doi: 10.3945/ajcn.116.135129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Matthews CE, Moore SC, Sampson J, Blair A, Xiao Q, Keadle SK, et al. Mortality benefits for replacing sitting time with different physical activities. Med Sci Sports Exerc 2015;47(9):1833–40. Epub 2015/01/30. doi: 10.1249/MSS.0000000000000621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Schmid D, Ricci C, Baumeister SE, Leitzmann MF. Replacing sedentary time with physical activity in relation to mortality. Med Sci Sports Exerc 2016;48(7):1312–9. Epub 2016/02/27. doi: 10.1249/MSS.0000000000000913. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.