Abstract
Interventions are needed to increase physical activity throughout the day in adults with chronic stroke, but mechanisms of action for doing so have not been identified. In this descriptive, exploratory study of 36 ambulatory, community-dwelling adults with chronic stroke, participants completed questionnaires investigating self-efficacy, self-regulation, social support, and outcomes expectations for daily physical activity. In the absence of any intervention, participants consistently reported high self-efficacy and outcomes expectations but low use of self-regulation and social support strategies. Discussion of how these results can inform the development of interventions to facilitate daily physical activity in adults with chronic stroke is provided.
Keywords: outcomes expectations, physical activity, self efficacy, self-regulation, social support, stroke
An estimated 7.2 million U.S. adults report that they have had a stroke (Benjamin et al., 2018), and history of stroke is a non-modifiable risk factor for diabetes, recurrent stroke, and cardiovascular mortality. For this reason, it is essential for individuals with stroke to address modifiable risk factors for these conditions, including hypertension, high cholesterol, and obesity (Benjamin et al., 2018). Physical activity is a particularly important health behavior because it favorably modifies these risk factors and is associated with improved post-stroke quality of life (Billinger et al., 2014; Rand, Eng, Tang, Hung, & Jeng, 2010).
Unfortunately, physical inactivity (i.e. <150 minutes of weekly moderate-to-vigorous physical activity) and sedentary behavior (i.e. low energy expenditure while sitting or lying down) are high in people with stroke (Billinger et al., 2014). For many, stroke-related motor impairment makes it difficult to meet exercise recommendations and likely contributes to high amounts of physical inactivity and sedentary behavior observed in people with stroke. Fortunately, experimental and epidemiologic studies have demonstrated that reducing sitting time and increasing physical activity, regardless of type or intensity, decreases cardiovascular and metabolic risk (Dunstan et al., 2012; Healy, Winkler, Owen, Anuradha, & Dunstan, 2015). For this reason, a whole-of-day approach for participating in daily physical activity (e.g. activities of daily living [ADLs], instrumental ADLs, leisure, occupation, sports, exercise) has been encouraged (Manns, Dunstan, Owen, & Healy, 2012).
It is important to understand what psychosocial characteristics influence daily physical activity before implementing any clinical or public health intervention because such characteristics may be important mechanisms of action for health behavior change. Social Cognitive Theory (SCT; Bandura, 2004), which is conceptually similar to the Person-Environment-Occupation Model of occupational performance (Law et al., 1996), theorizes that person, environment, and behavioral factors interact to influence behavior. More specifically, SCT theorizes that individuals are agents-of-change, capable of influencing their own actions and external events, and that individuals are influenced by external factors (e.g. environment, social support) (Bandura, 1991). SCT psychosocial constructs include self-efficacy (i.e. one’s confidence in one’s ability to perform a specific task), self-regulation (e.g. self-monitoring, self-appraisal, self-reaction), social support (i.e. modeling, support, and feedback from family and friends), and outcomes expectations (i.e. expected positive and negative consequences) (Bandura, 1991; Bandura, 2004). These mutually influential internal and external factors influence the selection and performance of many health behaviors, including physical activity (Young, Plotnikoff, Collins, Callister, & Morgan, 2014).
Figure 1 illustrates several SCT constructs common to both SCT and the Occupational Therapy Practice Framework: Domain & Process 3rd Edition (American Occupational Therapy Association, 2014) that are potential mechanisms of action by which daily physical activity could be modified. Numerous studies have demonstrated that self-efficacy, self-regulation, social support, and outcomes expectations are established mechanisms of action for physical activity in non-stroke populations (Bauman, Sallis, Dzewaltowski, & Owen, 2002; Young, Plotnikoff, Collins, Callister, & Morgan, 2014). Furthermore, while the relationship between these mechanisms of action and exercise-based physical activity in people with stroke has been established (Damush, Plue, Bakas, Schmid, & Williams, 2007; Shaughnessy, Resnick, & Macko, 2006), no study to date has explored these mechanisms as they relate to daily physical activity in adults with chronic stroke.
Figure 1.

Potential mechanisms of action for daily physical activity. Asterisk (*) indicates mechanisms of action investigated in this study.
Therefore, the purpose of this descriptive, exploratory study was to examine self-efficacy, self-regulation, social support, and outcomes expectations for daily physical activity in a sample of community-dwelling adults with chronic stroke. Identifying potential mechanisms of action for daily physical activity in adults with stroke is necessary for informing clinical decision-making and developing clinical and public health interventions that enhance health and decrease risk for cardiovascular and metabolic conditions.
Methods
Participants
Thirty-six adults with chronic stroke were recruited between February 2016 and April 2018 from community-based stroke support groups and stroke research registries maintained by Emory University in Atlanta, GA, and Washington University School of Medicine in St. Louis, MO. All participants provided written, informed consent for participation in this study, which was approved by the Institutional Review Board of both research institutions.
People with stroke were eligible to participate if they were at least 6 months post-stroke (ischemic or hemorrhagic), aged 30–80, living at home, able to ambulate at least 50 feet unsupervised with or without an assistive device, and had sufficient cognitive ability to provide informed consent. Participants were excluded if they had any other neurological diagnosis, were pregnant, or had an expected mortality within the next 12 months.
Procedure
Participants completed a 45 minute, face-to-face interview where information on demographics, health characteristics, and stroke-specific factors were collected. Descriptive information included Body Mass Index (BMI, kg/m2), time since stroke, number of strokes, and functional disability in activities of daily living measured using the Barthel Index (Wade & Collin, 1988). Participants then completed several self-report questionnaires to investigate potential mechanisms of action for daily physical activity.
Outcome Measures
Potential mechanisms of action underling daily physical activity included self-efficacy, self-regulation, social support, and outcomes expectations. Standardized questionnaires have not yet been developed to measure these potential mechanisms for daily physical activity, much less for their specific use in people with stroke. Therefore, wording of exercise-based questionnaires was modified, replacing the word “exercise” with “physical activity.” Examples of daily physical activity (e.g. ADLs, instrumental ADLs, leisure, occupation, sports, exercise) were provided to participants. Questionnaire responses were categorized into High, Moderate, and Low response categories to facilitate interpretation of participants’ agreement with each questionnaire item.
Self-Efficacy.
Self-Efficacy for daily physical activity was investigated using the 10-item Spinal Cord Injury Exercise Self-Efficacy Scale (Kroll, Kehn, Ho, & Groah, 2007). Although originally validated for use in people with spinal cord injury, the questionnaire has previously been used in stroke (Jones, Dear, Hush, Titov, & Dean, 2016). Participants were asked to indicate their confidence for being physically active across a variety of circumstances using a 10-point scale (1=low confidence, 10=high confidence). Questions asked about confidence in overcoming barriers and challenges; accomplishing goals; and being physically active in the absence of support from family, friends, therapists, and trainers, or when feeling tired or depressed. All questions were modified to reflect daily physical activity. Item scores were categorized into Low (score: 1–3), Moderate (score: 4–6), and High (score: 7–10) categories reflecting low, moderate, and high self-efficacy for daily physical activity.
Self-Regulation.
Self-regulation for daily physical activity was investigated using 11 questions from two different questionnaires. Six questions from Petosa’s (1993) 10-item Reinforcement Strategy scale were used, which was originally validated in a sample of middle-aged adults. Five questions from Rovniak, Anderson, Winett, & Stephens’s (2002) 10-item Exercise Planning and Scheduling Scale were also used, which has been validated in inactive (Monroe, Bassett, Fitzhugh, Raynor, & Thompson, 2016) and older adults (Park, Elavsky, & Koo, 2014). Specific items from the original questionnaires were selected based on their face validity for daily physical activity (e.g., “I engaged in physical activity with someone else”) while items that had less relevance (e.g., “On trips away from home, I purposely stay at places that have access to exercise facilities”) were omitted. Participants indicated how often during the previous month they used different self-regulatory strategies for engaging in daily physical activity using a 5-point scale (1=never, 5=often). Questions asked about frequency of self-reward, environmental cues, establishing routines, planning, self-monitoring, and self-praise. All questions were modified to reflect daily physical activity. Item scores were categorized into Low (score: 1–2), Moderate (score: 3) and High (score: 4–5) categories, reflecting low, moderate, and high use of self-regulation strategies for daily physical activity.
Social Support.
Social support for daily physical activity was investigated using the 12-item Family Participation and Involvement Scale (Sallis, Grossman, Pinski, Patterson, & Nader, 1987). The original scale was validated in middle-aged adults, but has also been validated in sedentary adults (Monroe et al., 2016), older women (Walker, Pullen, Hertzog, Boeckner, & Hageman, 2006) and individuals with spinal cord injury (Keegan, Chan, Ditchman, & Chiu, 2012). Participants indicated how often during the previous month different types of social support were available using a 5-point scale (1=never, 5=often). Questions asked about frequency of a family member or friend offering to be physically active with the participant, making positive comments, providing reminders or rewards, and discussing or planning physical activity with the participant. All questions were modified to reflect daily physical activity. Item scores were categorized into Low (score: 1–2), Moderate (score: 3) and High (score: 4–5) categories, reflecting low, moderate, and high availability of social support for daily physical activity.
Outcomes Expectations.
Positive and negative outcomes expectations for daily physical activity were measured using the 16-item Positive and Negative Orientations Toward Exercise Scale (Marcus, Rakowski, & Rossi, 1992). Originally validated in middle-aged adults, the scale has also been validated in older adults (Wilcox, Bopp, Oberrecht, Kammermann, & McElmurray, 2003) and people with diabetes (Vickers, Nies, Patten, Dierkhising, & Smith, 2006). Participants indicated how strongly they agreed with 10 positive and 6 negative outcomes expectations using a 5-point scale (1=strong disagreement, 5=strong agreement). Positive outcomes expectations questions asked participants if they would feel less tension, sleep better, and feel more confident by being physically active routinely. Negative outcomes expectations questions asked whether routine physical activity would take too much time, lead to exhaustion, and disrupt one’s daily routine. All questions were modified to reflect daily physical activity. Item scores were categorized into Low (score: 1–2), Moderate (score: 3) and High (score: 4–5) categories. Negative outcomes expectations items were reverse scored. Thus, categories reflected low, moderate, and high agreement with positive outcomes expectations; and low, moderate, and high disagreement with negative outcomes expectations.
Data Analysis
Because this was a descriptive, exploratory study, no sample size calculations or analytic statistics were performed; instead, only descriptive statistics are presented to characterize the results. Medians, interquartile ranges (IQR, i.e. 25th-75th percentile), and percentages were computed for participant characteristics because data were not normally distributed. For each questionnaire, the percentage of Low, Moderate, and High responses was calculated across participants (i.e. for the group as a whole).
Results
Thirty-six, community-dwelling, ambulatory adults participated in this study. Participants were relatively equally distributed for African-American and Caucasian race (African-American, n=16; Caucasian, n=19; Asian, n=1) and sex (male, n=18; female, n=18). Median age was 61 (IQR: 16) years; median BMI was 29 (IQR: 6) kg/m2, indicating overweight; and median number of strokes was 1 (IQR: 0), with 50% of strokes having occurred within 1–5 years for 50% of participants. Additionally, the majority of participants reported only mild functional disability as indicated by a median Barthel Index score of 100 (IQR: 0).
Percentages of Low, Moderate, and High category responses across participants are displayed in Figure 2. Overall, High responses consistently exceeded Low responses for self-efficacy, positive outcomes expectations, and negative outcomes expectations, indicating that participants reported high self-efficacy for daily physical activity, agreement with positive outcomes expectations for daily physical activity, and disagreement with negative outcomes expectations for daily physical activity. In contrast, responses for self-regulation and social support were much more variable with Low category responses exceeding High category responses, indicating that participants reported low use of self-regulation strategies and low availability of social support for daily physical activity.
Figure 2.
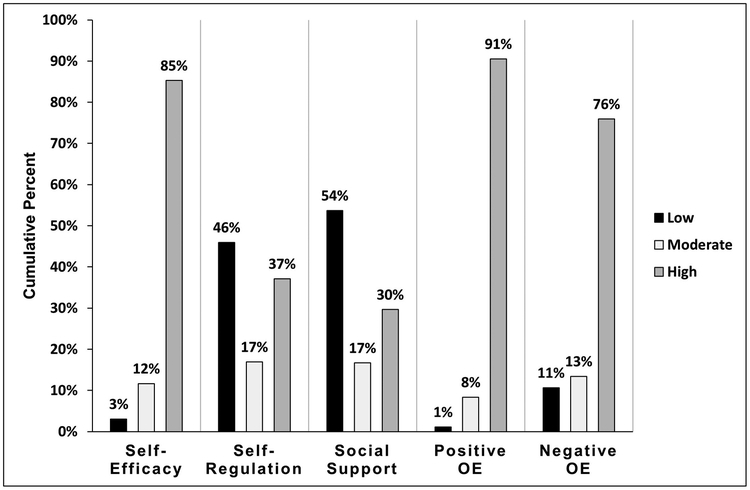
Percent of questionnaire responses by category (Low, Moderate, High) for each questionnaire. Questionnaire responses were converted into categorical responses reflecting degree of agreement with questionnaire items. For self-efficacy (10-point scale), original responses of 1–3 = Low, 4–6 = Moderate, and 7–10 = High. For the remaining questionnaires (5-point scales), original responses of 1–2 = Low, 3 = Moderate, 4–5 = High. High responses consistently exceeded Low responses for self-efficacy, positive outcomes expectations, and negative outcomes expectations, whereas responses were much more variable for self-regulation and social support. Abbreviation: OE, outcomes expectations.
Discussion
Social Cognitive Theory is an evidence-based framework that can be used for investigating mechanisms of action for physical activity behavior (Young et al., 2014). Potential mechanisms of action for daily physical activity have not been previously examined in people with stroke, but understanding these mechanisms is important for increasing daily physical activity in this at-risk population. Therefore, we investigated SCT constructs as potential mechanisms of action in a community-dwelling sample of adults with stroke. Although the generalizability of this study’s findings is limited by the heterogeneous sample and lack of validated questionnaires, this exploratory study provides valuable insight into potential mechanisms by which daily post-stroke physical activity might be enhanced, which can be used to guide future research investigations and inform clinical decision-making.
In this study, participants reported high self-efficacy, agreement with positive outcome expectations, and disagreement with negative expectations for daily physical activity, in the absence of any intervention. Although we did not collect information on participation in rehabilitation during participant interviews, some participants mentioned that they received rehabilitation services following their stroke. A possible explanation for the observed results may be that participants that received rehabilitation services developed self-efficacy for daily physical activity and obtained knowledge about the importance of daily physical activity during inpatient and outpatient rehabilitation because occupational and physical therapy services directly address daily physical activity (e.g. ambulation, ADLs, stroke self-management education) (Lang et al., 2009). An alternative or additional explanation could be that public health messaging about the importance of health-enhancing physical activity influenced participants’ reports of self-efficacy and outcomes expectations for daily physical activity because physical activity mass media campaigns have demonstrated efficacy for improving physical activity-related knowledge and attitudes (Cavill & Bauman, 2004). As it pertains to future research and clinical judgment, these findings may indicate that for ambulatory, community-dwelling, chronic stroke survivors, self-efficacy and outcomes expectations for daily physical activity are relatively robust such that additional intervention for enhancing these mechanisms of action may not be needed; instead, intervention could address less robust mechanisms for increasing daily physical activity.
In contrast, participants reported infrequent use (i.e. Low category responses) of self-regulation and social support strategies. Perhaps these findings should not be surprising given that community-dwelling adults in other studies have also reported low baseline use of self-regulation strategies (Nothwehr & Yang, 2007) and low baseline availability of social support for physical activity (Eyler et al., 1999). Two recent studies, however, have made use of self-regulation and social support strategies to decrease sedentary behavior and increase daily physical activity among people with stroke. In one study, motivational interviewing was used to help participants implement self-regulation strategies (i.e. action plans, goals, problem-solving), which led to decreased time spent sitting and increased time spent standing and stepping (English et al., 2016). In another study, a mobile phone application utilizing goal setting, planning, self-monitoring, feedback, and social support led to an increase in time spent walking (Paul et al., 2016). Both studies used self-regulation and social support strategies to increase daily physical activity, which suggests that self-regulation and social support may be mechanisms of action for daily physical activity. Neither study measured the dose nor the frequency of strategy usage, however; thus, the relationship between use of self-regulation and social support strategies and daily physical activity cannot be determined. Taken together, these two studies and the current study’s findings may suggest that baseline use of self-regulation and social support strategies among ambulatory, community-dwelling, chronic stroke survivors is variable, and that future clinical interventions and public health programs should investigate self-regulation and social support as potential mechanisms of action for increasing daily physical activity.
Directions for Future Research
Although only preliminary, the results of this study suggest that SCT constructs may be potential mechanisms of action for daily physical activity; thus, these constructs warrant further investigation. There are several directions for future research that could enhance this area of study for informing clinical practice and intervention development. First, additional information is needed about factors that might influence baseline levels of self-efficacy and outcomes expectations. As mentioned previously, some participants indicated that they received rehabilitation services, which may have enhanced self-efficacy and outcomes expectations for daily physical activity. Indeed, among individuals with impaired mobility, self-efficacy for mobility can increase as a result of receiving rehabilitation services (Sanford et al., 2006), which may be true of daily physical activity as well. Second, type and quality of social support should be examined because both quantity and quality of social support independently influence health (House, Umberson, & Landis, 1988). Third, inclusion of qualitative data through in-depth interviews could facilitate a better understanding of how the investigated mechanisms of action function in an individual’s daily life, which would be particularly helpful for informing clinical practice and developing interventions to enhance daily physical activity.
Lastly, SCT constructs should be investigated from an occupational performance perspective. Within the Occupational Therapy Practice Framework: Domain & Process 3rd Edition, the SCT constructs self-efficacy and outcomes expectations are client factors, self-regulation is a performance skill, and social support is an environment factor. These factors, in turn, interact with one’s daily activities and occupations to influence occupational performance for daily physical activity (American Occupational Therapy Association, 2014). Viewed in this way, SCT and the Occupational Therapy Practice Framework are complementary frameworks that can be used jointly in the development and testing of interventions to promote daily physical activity in adults with chronic stroke, and should be explored.
Limitations
As has been previously acknowledged, study results were obtained from a relatively small sample of adults with chronic stroke who were ambulatory, living in the community, and who reported minimal functional disability. Thus, findings likely do not generalize to individuals with greater functional impairment. Despite the heterogeneity of study participants, this study provides baseline values for several theory-based mechanisms of action known to influence different types of physical activity and can be used to inform the development of future physical activity interventions and influence clinical decision-making. Another limitation is the use of modified questionnaires that have not yet been validated. Because only one word was changed (i.e. “physical activity” was substituted for “exercise”), however, face validity is assumed. Face validity is further assumed because modified SCT-informed questionnaires were used. Future studies should examine the validity of the modified questionnaires for predicting objectively-measured daily physical activity (e.g. accelerometry, pedometer) to establish validity of the modified questionnaires and to investigate the underlying mechanisms of action for daily physical activity. Additionally, qualitative investigation should be used in conjunction with objective, quantitative exploration (e.g. mixed-methods) to strengthen the design of future studies.
Conclusion
Physical activity, regardless of type or intensity, confers protective effects against cardiovascular and metabolic conditions experienced by individuals with stroke. Understanding mechanisms of action for increasing daily physical activity is important for designing acceptable and effective interventions for stroke survivors. In this descriptive, exploratory study of ambulatory, community-dwelling adults with chronic stroke, participants provided ratings of several mechanisms of action that have the potential to directly influence daily physical activity. Self-efficacy and outcomes expectations were consistently rated high while use of self-regulation and social support strategy ratings were much less consistent. Although these results are not definitive, they do suggest that future interventions should examine the role of self-regulation and social support as potential mechanisms of action for increasing daily physical activity in adults with chronic stroke.
Acknowledgments
Declaration of Interest
The author reports no conflicts of interest. This work was supported by the National Institutes of Health under Grant 5T32HL130357–02.
References
- American Occupational Therapy Association. (2014). Occupational Therapy Practice Framework: Domain and Process (3rd Edition). American Journal of Occupational Therapy, 68(Supplement_1), S1–S48. doi: 10.5014/ajot.2014.682006 [DOI] [Google Scholar]
- Bandura A (1991). Social cognitive theory of self-regulation. Organizational Behavior and Human Decision Processes, 50(2), 248–287. doi: 10.1016/0749-5978(91)90022-L [DOI] [Google Scholar]
- Bandura A (2004). Health promotion by social cognitive means. Health Education & Behavior, 31(2), 143–164. doi: 10.1177/1090198104263660 [DOI] [PubMed] [Google Scholar]
- Bauman AE, Sallis JF, Dzewaltowski DA, & Owen N (2002). Toward a better understanding of the influences on physical activity. American Journal of Preventive Medicine, 23(2), 5–14. doi: 10.1016/S0749-3797(02)00469-5 [DOI] [PubMed] [Google Scholar]
- Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, . . . Muntner P (2018). Heart Disease and Stroke Statistics—2018 Update: A Report From the American Heart Association. Circulation, 137(12), e67–e492. doi: 10.1161/cir.0000000000000558 [DOI] [PubMed] [Google Scholar]
- Billinger SA, Arena R, Bernhardt J, Eng JJ, Franklin BA, Johnson CM, . . . Tang A (2014). Physical Activity and Exercise Recommendations for Stroke Survivors: A Statement for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. doi: 10.1161/str.0000000000000022 [DOI] [PubMed] [Google Scholar]
- Cavill N, & Bauman A (2004). Changing the way people think about health-enhancing physical activity: do mass media campaigns have a role? Journal of Sports Sciences, 22(8), 771–790. doi: 10.1080/02640410410001712467 [DOI] [PubMed] [Google Scholar]
- Damush TM, Plue L, Bakas T, Schmid A, & Williams LS (2007). Barriers and facilitators to exercise among stroke survivors. Rehabilitation Nursing, 32(6), 253–260, 262. [DOI] [PubMed] [Google Scholar]
- Dunstan DW, Kingwell BA, Larsen R, Healy GN, Cerin E, Hamilton MT, . . . Owen N (2012). Breaking up prolonged sitting reduces postprandial glucose and insulin responses. Diabetes Care, 35(5), 976–983. doi: 10.2337/dc11-1931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- English C, Healy GN, Olds T, Parfitt G, Borkoles E, Coates A, . . . Bernhardt J (2016). Reducing Sitting Time After Stroke: A Phase II Safety and Feasibility Randomized Controlled Trial. Archives of Physical Medicing and Rehabilitation, 97(2), 273–280. doi: 10.1016/j.apmr.2015.10.094 [DOI] [PubMed] [Google Scholar]
- Eyler AA, Brownson RC, Donatelle RJ, King AC, Brown D, & Sallis JF (1999). Physical activity social support and middle- and older-aged minority women: results from a US survey. Social Science & Medicine, 49(6), 781–789. doi: 10.1016/S0277-9536(99)00137-9 [DOI] [PubMed] [Google Scholar]
- Healy GN, Winkler EA, Owen N, Anuradha S, & Dunstan DW (2015). Replacing sitting time with standing or stepping: associations with cardio-metabolic risk biomarkers. European Heart Journal, 36(39), 2643–2649. doi: 10.1093/eurheartj/ehv308 [DOI] [PubMed] [Google Scholar]
- House JS, Umberson D, & Landis KR (1988). Structures and processes of social support. Annual Review of Sociology, 14(1), 293–318. [Google Scholar]
- Jones TM, Dear BF, Hush JM, Titov N, & Dean CM (2016). myMoves Program: Feasibility and Acceptability Study of a Remotely Delivered Self-Management Program for Increasing Physical Activity Among Adults With Acquired Brain Injury Living in the Community. Physical Therapy, 96(12), 1982–1993. doi: 10.2522/ptj.20160028 [DOI] [PubMed] [Google Scholar]
- Keegan JP, Chan F, Ditchman N, & Chiu CY (2012). Predictive Ability of Pender’s Health Promotion Model for Physical Activity and Exercise in People With Spinal Cord Injuries: A Hierarchical Regression Analysis. Rehabilitation Counseling Bulletin, 56(1), 34–47. doi: 10.1177/0034355212440732 [DOI] [Google Scholar]
- Kroll T, Kehn M, Ho PS, & Groah S (2007). The SCI Exercise Self-Efficacy Scale (ESES): development and psychometric properties. International Journal of Behavioral Nutrition and Physical Activity, 4(34). doi:1479–5868-4–34 [pii] 10.1186/1479-5868-4-34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lang CE, MacDonald JR, Reisman DS, Boyd L, Jacobson Kimberley T, Schindler-Ivens SM, . . . Scheets PL (2009). Observation of Amounts of Movement Practice Provided During Stroke Rehabilitation. Archives of Physical Medicine and Rehabilitation, 90(10), 1692–1698. doi: 10.1016/j.apmr.2009.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Law M, Cooper B, Strong S, Stewart D, Rigby P, & Letts L (1996). The Person-Environment-Occupation Model: A Transactive Approach to Occupational Performance. Canadian Journal of Occupational Therapy, 63(1), 9–23. doi: 10.1177/000841749606300103 [DOI] [PubMed] [Google Scholar]
- Manns PJ, Dunstan DW, Owen N, & Healy GN (2012). Addressing the nonexercise part of the activity continuum: a more realistic and achievable approach to activity programming for adults with mobility disability? Physical Therapy, 92(4), 614–625. doi: 10.2522/ptj.20110284 [DOI] [PubMed] [Google Scholar]
- Marcus BH, Rakowski W, & Rossi JS (1992). Assessing motivational readiness and decision making for exercise. Health Psychology, 11(4), 257–261. [DOI] [PubMed] [Google Scholar]
- Monroe CM, Bassett DR Jr., Fitzhugh EC, Raynor HA, & Thompson DL (2017). Effect of Adding Online Social Support Tools to an Adult Walking Program: A Pilot Randomized Controlled Trial. Health Promotion Practice, 18(1), 84–92. doi: 10.1177/1524839915626674 [DOI] [PubMed] [Google Scholar]
- Nothwehr F, & Yang J (2007). Goal setting frequency and the use of behavioral strategies related to diet and physical activity. Health Education Research, 22(4), 532–538. doi: 10.1093/her/cyl117 [DOI] [PubMed] [Google Scholar]
- Park CH, Elavsky S, & Koo KM (2014). Factors influencing physical activity in older adults. Journal of Exercise Rehabilitatoin, 10(1), 45–52. doi: 10.12965/jer.140089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paul L, Wyke S, Brewster S, Sattar N, Gill JM, Alexander G, . . . Dybus A (2016). Increasing physical activity in stroke survivors using STARFISH, an interactive mobile phone application: a pilot study. Topics in Stroke Rehabilitation, 23(3), 170–177. doi: 10.1080/10749357.2015.1122266 [DOI] [PubMed] [Google Scholar]
- Petosa PS (1993). Use of Social Cognitive Theory to Explain Exercise Behavior Among AdultsI (Doctoral dissertation). The Ohio State University, Columbus, OH: Retrieved from http://rave.ohiolink.edu/etdc/view?acc_num=osu1219340693 [Google Scholar]
- Rand D, Eng JJ, Tang PF, Hung C, & Jeng JS (2010). Daily physical activity and its contribution to the health-related quality of life of ambulatory individuals with chronic stroke. Health and Quality of Life Outcomes, 8, 80. doi: 10.1186/1477-7525-8-80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rovniak LS, Anderson ES, Winett RA, & Stephens RS (2002). Social cognitive determinants of physical activity in young adults: a prospective structural equation analysis. Annals of Behavioral Medicine, 24(2), 149–156. [DOI] [PubMed] [Google Scholar]
- Sallis JF, Grossman RM, Pinski RB, Patterson TL, & Nader PR (1987). The development of scales to measure social support for diet and exercise behaviors. Preventive Medicine, 16(6), 825–836. [DOI] [PubMed] [Google Scholar]
- Sanford JA, Griffiths PC, Richardson P, Hargraves K, Butterfield T, & Hoenig H (2006). The effects of in-home rehabilitation on rask self-efficacy in mobility-impaired adults: A randomized clinical trial. Journal of the American Geriatrics Society, 54(11), 1641–1648. doi:doi: 10.1111/j.1532-5415.2006.00913.x [DOI] [PubMed] [Google Scholar]
- Shaughnessy M, Resnick BM, & Macko RF (2006). Testing a model of post-stroke exercise behavior. Rehabilitation Nursing, 31(1), 15–21. [DOI] [PubMed] [Google Scholar]
- Vickers KS, Nies MA, Patten CA, Dierkhising R, & Smith SA (2006). Patients with diabetes and depression may need additional support for exercise. American Journal of Health Behavior, 30(4), 353–362. doi: 10.5555/ajhb.2006.30.4.353 [DOI] [PubMed] [Google Scholar]
- Wade DT, & Collin C (1988). The Barthel ADL Index: a standard measure of physical disability? International Disability Studies, 10(2), 64–67. [DOI] [PubMed] [Google Scholar]
- Walker SN, Pullen CH, Hertzog M, Boeckner L, & Hageman PA (2006). Determinants of older rural women’s activity and eating. Western Journal of Nursing Research, 28(4), 449–468. doi: 10.1177/0193945906286613 [DOI] [PubMed] [Google Scholar]
- Wilcox S, Bopp M, Oberrecht L, Kammermann SK, & McElmurray CT (2003). Psychosocial and perceived environmental correlates of physical activity in rural and older african american and white women. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 58(6), 329–337. [DOI] [PubMed] [Google Scholar]
- Young MD, Plotnikoff RC, Collins CE, Callister R, & Morgan PJ (2014). Social cognitive theory and physical activity: a systematic review and meta-analysis. Obesity Reviews, 15(12), 983–995. doi: 10.1111/obr.12225 [DOI] [PubMed] [Google Scholar]


