Abstract
Introduction
U.S. hospital discharges for opioid overdose increased substantially during the past two decades. This brief report describes 90-day readmissions among patients discharged from inpatient stays for opioid overdose.
Methods
In 2018, survey-weighted analysis of hospital stays in the 2016 Healthcare Cost and Utilization Project National Readmissions Database yielded the national estimated proportion of patients with opioid overdose stays that had all-cause readmissions within ≤90 days. A multivariable logistic regression model assessed index stay factors associated with readmission by type (opioid overdose or not). Number of readmissions per patient was assessed.
Results
More than 24% (n=14,351/58,850) of patients with non-fatal index stays for opioid overdose had at least one all-cause readmission ≤90 days of index stay discharge and 3% (n=1,658/ 58,850) of patients had at least one opioid overdose readmission. Less than 0.2% (n=104/58,850) of patients had more than one readmission for opioid overdose. Patient demographic characteristics (e.g., male, older age), comorbidities diagnosed during the index stay (e.g., drug use disorder, chronic pulmonary disease, psychoses), and other index stay factors (Medicare or Medicaid primary payer, discharge against medical advice) were significantly associated with both opioid overdose and non-opioid overdose readmissions. Nearly 30% of index stays for opioid overdose included heroin, which was significantly associated with opioid overdose readmissions.
Conclusions
A quarter of opioid overdose patients have ≤90 days all-cause readmissions, although opioid overdose readmission is uncommon. Effective strategies to reduce readmissions will address substance use disorder as well as comorbid physical and mental health conditions.
INTRODUCTION
Hospital discharges in the U.S. for opioid overdose increased substantially during the past two decades.1–4 Substance use disorder (SUD) is a risk factor for hospital readmission5–11 but readmissions after opioid overdose have not been described using national data. The readmission rate following opioid overdose and risk factors for readmission constitute meaningful information for clinical and public health decision making on “tertiary prevention” in the context of the opioid overdose epidemic; that is, efforts that increase access to effective addiction treatment when SUD is diagnosed.12 Intervention following overdose is critical; substance use–associated diseases are the most common cause of death among adults with Medicaid aged less than 65 years in the year following non-fatal opioid overdose.13 This brief report describes 90-day readmissions among patients discharged from opioid overdose inpatient stays.
METHODS
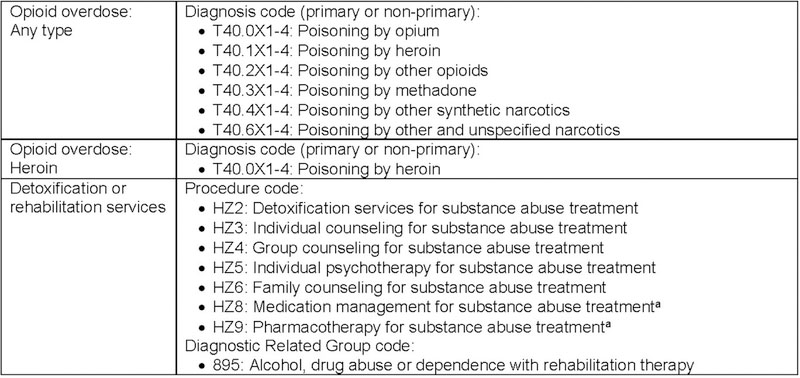
In 2018, authors analyzed the 2016 Healthcare Cost and Utilization Project National Readmissions Database (HCUP-NRD), which can be used for survey-weighted national estimates of same-year, same-state readmissions to community hospitals.14 Opioid overdose stays were classified by ICD-10-CM and other administrative codes (Figure 1), including whether patients received inpatient drug detoxification or rehabilitation services (e.g., counseling or pharmacotherapy).3,15,16 Comorbidities were classified by Elixhauser Comorbidity Software for ICD-10-CM.17 Patient age, sex, primary payer, and discharge status were reported in the data source.
Figure 1.
Administrative codes used to classify opioid overdose index stays.
Source: www.icd10data.com. Accessed November 28, 2018.
aNicotine, antabuse, and bupropion not included.
Index stays were patients’ first admission with opioid (illicit or prescribed) overdose during January–September. Readmission was any inpatient stay during January–December ≤90 days of index stay discharge. Multivariable logistic regression models assessed whether index stay factors were associated with readmissions by type (opioid overdose and non-opioid overdose). The number of readmissions per patient by type was assessed. Authors used SAS, version 9.4. All results reflect index stay survey weighting.
RESULTS
During January–September 2016, an estimated 61,170 patients had index stays for opioid overdose (Table 1). Mean patient age was 47 years and 50% of patients were female. Patients had a high prevalence of diagnosed drug use disorder (45%) and other comorbidities (e.g., fluid and electrolyte disorders, hypertension, depression, chronic pulmonary disease); just 4% of patients had no comorbidities (Table 1). Nearly 28% of patients had heroin overdose and just 3% had documented inpatient substance detoxification or rehabilitation services. More than 63% of patients were routinely discharged, 16% were transferred, 9% were discharged to home health care, 8% were discharged against medical advice, 4% died in hospital, and <1% were discharged to an unknown destination. Medicare (34%) and Medicaid (30%) were the primary payer for a majority of index stays.
Table 1.
Opioid Overdose Index Stay Factors Associated With Readmissions, Healthcare Cost and Utilization Project National Readmissions Database, 2016
| Readmissions ≤90 days among patients with non-fatal index staysa January-December 2016 (N=58,850) |
||||||
|---|---|---|---|---|---|---|
| Opioid overdose |
Other (non-opioid overdose) |
|||||
| Index stay measure | Patients with index stay discharged January–September 2016, n (%) | All-cause, n (%)b | n (%)b | AOR (95% CI) | n (%)b | AOR (95% CI) |
| Sample size | 61,170 (100.0) | 14,351 (24.4) | 1,658 (2.8) | NA | 13,311 (22.6) | NA |
| Age, years | 46.8 (0.19)c | 51.7 (0.24)c | 48.5 (0.66)c | 1.01 (1.00,1.01) | 52.1 (0.25)c | 1.01 (1.00, 1.01) |
| Female | 30,630 (50.1) | 7,528 (25.4) | 723 (2.4) | 0.79 (0.69, 0.92) | 7,088 (23.9) | 0.98 (0.92,1.05) |
| Comorbiditiesd | ||||||
| Drug abuse | 27,771 (45.4) | 6,525 (24.5) | 946 (3.5) | 1.47 (1.22,1.77) | 5,926(22.2) | 1.15 (1.08,1.24) |
| Fluid and electrolyte disorders | 27,558 (45.1) | 6,695 (25.9) | 794 (3.1) | 1.11 (0.93, 1.33) | 6,183 (24.0) | 0.94 (0.88, 1.00) |
| Hypertension | 25,205 (41.2) | 7,488 (30.7) | 697 (2.9) | 0.90 (0.74,1.09) | 7,093 (29.0) | 1.21 (1.11,1.32) |
| Depression | 19,371 (31.7) | 4,542 (23.9) | 531 (2.8) | 1.12 (0.94, 1.35) | 4,205 (22.1) | 0.94 (0.88, 1.02) |
| Chronic pulmonary disease | 15,812 (25.8) | 4,949 (32.2) | 540 (3.5) | 1.32 (1.09,1.59) | 4,659 (30.3) | 1.30 (1.21,1.39) |
| Other neurologic disorders | 12,838 (21.0) | 3,439 (27.8) | 381 (3.1) | 1.13 (0.93, 1.38) | 3,216 (26.0) | 1.09 (1.01, 1.18) |
| Alcohol abuse | 9,997 (16.3) | 2,387 (24.7) | 296 (3.1) | 1.03 (0.83, 1.28) | 2,199 (22.8) | 1.08 (0.99,1.18) |
| Deficiency anemias | 9,323 (15.2) | 2,934 (32.8) | 286 (3.2) | 1.10 (0.89, 1.36) | 2,776 (31.0) | 1.31 (1.20,1.44) |
| Psychoses | 7,960 (13.0) | 2,159 (27.9) | 260 (3.4) | 1.25 (1.01,1.53) | 2,018 (26.0) | 1.22 (1.11,1.34) |
| Obesity | 7,750 (12.7) | 2,073 (27.7) | 161 (2.2) | 0.74 (0.57, 0.94) | 1,999 (26.7) | 0.97 (0.89, 1.07) |
| Other comorbidities | 27,766 (45.4) | 8,582 (32.2) | 855 (3.2) | 1.27 (1.06,1.54) | 8,109 (30.5) | 1.61 (1.50,1.73) |
| None | 2,690 (4.4) | 293 (11.1) | 45 (1.7) | 1.07 (0.63, 1.82) | 254 (9.7) | 0.77 (0.62, 0.95) |
| Heroin overdose | 17,110 (28.0) | 3,160 (19.8) | 617 (3.9) | 1.67 (1.37, 2.04) | 2,731 (17.1) | 0.88 (0.81, 0.96) |
| Detoxification or rehabilitation services | 1,812 (3.0) | 448 (24.8) | 51 (2.8) | 0.89 (0.59, 1.35) | 425 (23.5) | 1.26 (1.04, 1.52) |
| Discharge status | ||||||
| Routine | 38,807 (63.4) | 8,512 (21.9) | 1,084 (2.8) | ref | 7,804 (20.1) | ref |
| Transfers | 10,014 (16.4) | 2,718 (27.1) | 222 (2.2) | 0.74 (0.59, 0.93) | 2,604 (26.0) | 1.12 (1.03,1.22) |
| Home health care | 5,182 (8.5) | 1,899 (36.6) | 156 (3.0) | 0.95 (0.71,1.27) | 1,811 (35.0) | 1.38 (1.25, 1.52) |
| Against medical advice | 4,771 (7.8) | 1,206 (25.3) | 190 (4.0) | 1.29 (1.02,1.64) | 1,080 (22.6) | 1.30 (1.14,1.48) |
| Died in hospital | 2,320 (3.8) | NA | NA | NA | NA | NA |
| Discharged alive, destination unknown | 76 (0.1) | NR | NR | 2.60 (0.93, 7.32) | NR | 0.74 (0.35, 1.55) |
| Primary payer | ||||||
| Medicare | 20,902 (34.2) | 6,546 (32.3) | 670 (3.3) | 1.77 (1.34, 2.35) | 6,169 (30.4) | 1.53 (1.37,1.71) |
| Medicaid | 18,521 (30.3) | 4,345 (24.6) | 575 (3.3) | 1.54 (1.21,1.96) | 3,995 (22.6) | 1.54 (1.40, 1.70) |
| Private | 12,572 (20.6) | 1,996 (16.4) | 216 (1.8) | ref | 1,834 (15.1) | ref |
| Self-pay | 6,470 (10.6) | 947 (15.4) | 145 (2.4) | 1.10 (0.76, 1.59) | 827 (13.4) | 1.01 (0.87, 1.16) |
| Othere | 1,907 (3.1) | 365 (20.0) | NR | 0.57 (0.32, 1.03) | 355 (19.4) | 1.19 (0.99,1.42) |
| No charge | 683 (1.1) | 131 (19.7) | 29 (4.3) | 1.91 (1.05, 3.50) | 114 (17.1) | 1.30 (0.92, 1.83) |
| Unknown | 115 (0.2) | NR | NR | 0.71 (0.11, 4.54) | NR | 1.03 (0.54, 1.96) |
Note: 2016 Healthcare Cost and Utilization Project National Readmissions Database. All data reflect Index stay survey weights. Logistic regression model Included all factors reported In the table. Boldface Indicates statistical significance (p<0.05).
Survey-weighted estimates of the number of patients readmitted ≤90 days (i.e., either a patient was readmitted during that period or not). Each patient is counted only once in each readmission category: Any, opioid overdose, non-opioid overdose. Analysis details: Index stays defined using HCUP-NRD variable DQTR=1–3 for stays with qualifying opioid overdose diagnosis codes (Figure 1). Readmissions per patient (NRD_VisitLInk) defined as all NRD_DaysToEvent ≤90 of the value of NRD_DaysToEvent plus length of stay (LOS) for the index stay.
Data are % of patients with non-fatal index stay discharges (n=58,850; excluding patients that died during the index stay [n=2,320, reported in the table]) by measure (or, table row) that had readmissions ≤90 days.
Data are mean (SE).
Comorbidities affecting ≥10% of index stay patients reported.
Includes Worker’s Compensation, CHAMPUS, CHAMPVA, Title V, and other government programs.
NA, not applicable; NR, not reported (when relative SE was >30% or the SE=0 the survey-weighted estimate was considered unreliable).
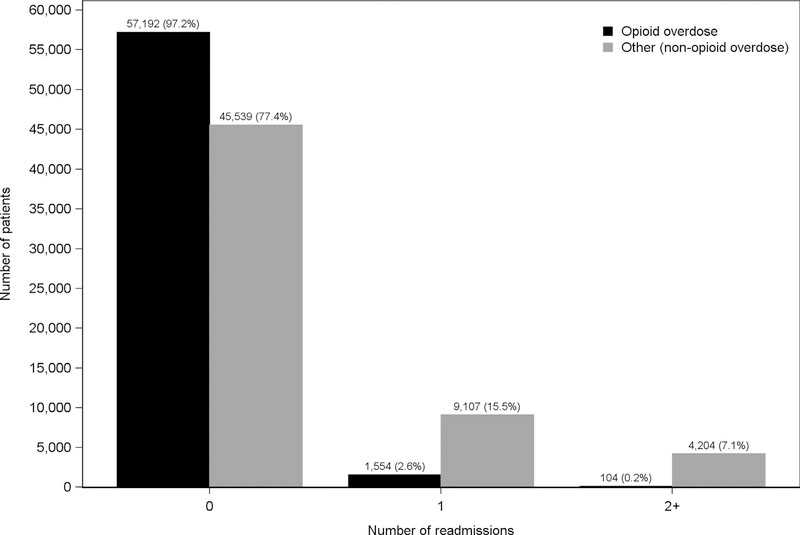
Twenty-four percent (n=14,351/58,850) of patients with non-fatal index stays (excludes n=2,320 fatalities) had at least one all-cause readmission ≤90 days (Table 1). Just 3% (n=1,658/58,850) of patients were readmitted for opioid overdose, whereas 23% (n=13,311/58,850) had non-opioid overdose readmissions (a patient could be in both categories). Three percent (n=1,554/58,850) of patients had one readmission for opioid overdose <90 days of index stay discharge and 0.2% (n=104/58,850) had two or more such readmissions (Figure 2). More than 15% (n=9,107/58,850) of patients had one readmission for non-opioid overdose conditions and 7% (n=4,204/58,850) had two or more such readmissions.
Figure 2.
Readmissions ≤90 days following discharge from non-fatal opioid overdose index stays (N=58,850 patients).
Note: “0” refers to the number of patients with non-fatal index stays for opioid overdose who had zero readmissions ≤90 days of index stay discharge. Admissions by type – opioid overdose and other (non-opioid overdose) – each sum to 100% of analyzed patients.
Females (compared with males) and obese patients (compared with non-obese patients) were significantly less likely to have an opioid overdose readmission, whereas older patient age was associated with both opioid and non-opioid overdose readmissions (Table 1). Patients with diagnosed drug use disorder, chronic pulmonary disease, psychoses, and other comorbidities (i.e., observed among <10% of patients) were more likely to have both opioid and non-opioid overdose readmissions. Patients with hypertension, other neurologic disorders, and deficiency anemias were more likely and patients with fluid and electrolyte disorders or no diagnosed comorbidities were less likely to have non-opioid overdose readmissions.
Patients treated for heroin overdose (compared with other opioids) were more likely to have opioid overdose readmissions but less likely to have non-opioid overdose readmissions, whereas patients with inpatient substance detoxification or rehabilitation services were more likely to have only non-opioid overdose readmissions. Patients discharged against medical advice (compared with routine discharge) and those with Medicare or Medicaid as primary payer for the index stay (compared with private payer) were more likely to have both readmission types. Patients not charged for index stays were more likely to be readmitted for opioid overdose and patients discharged to home health care were more likely to have non-opioid overdose readmissions. Patients transferred after the index stay were less likely to have opioid overdose readmission but more likely to have non-opioid overdose readmission.
DISCUSSION
Twenty-four percent of patients discharged after 2016 hospital admissions for opioid overdose had 90 or less days all-cause readmissions, but just 3% were readmitted for another opioid overdose. A 90-day follow-up period aimed to provide a longer-term perspective than common readmissions assessment periods of 7 or 30 days. For some context, nationally 14% of inpatient stays have 30 or less days all-cause readmissions and the index stay principal diagnosis with the highest 30-day readmissions rate is schizophrenia and other psychotic disorders (23 readmissions per 100 index stays).18
Consistent with previous research demonstrating differences between heroin and non-heroin overdose inpatients,1 heroin overdose patients were more likely to be readmitted for opioid overdose; however, just 3.9% of heroin overdose patients had such readmissions (Table 1). This study supports previous research indicating that opioid use disorder is a risk factor for readmissions7,11 and that many patients admitted for drug and alcohol overdose have serious comorbid health conditions.19–21 High prevalence of comorbidities among opioid overdose inpatients highlights the need for a coordinated, careful, “warm handoff” transfer of patients to outpatient SUD treatment services, including effective communication between inpatient and outpatient clinicians.
Medication-assisted treatment (MAT) and residential treatment within 14 days of discharge for SUD inpatients are associated with reduced risk of behavioral health readmissions.22 Inpatient addiction consultation is associated with reduced alcohol and drug addiction severity and increased number of abstinence days immediately following discharge.23 Ongoing outreach—including phone calls and counseling—has helped some SUD inpatients initiate treatment following discharge.24,25 Previous research suggests inpatient-initiated MAT can help some opioid use disorder inpatients initiate treatment programs following discharge.26 MAT integration in primary care settings aims to treat SUD before overdose.27
Despite urgent need, many opioid overdose inpatients do not receive timely follow-up treatment services and many continue to misuse opioids.22,28–30 Current regulations provide strict oversight regarding use of buprenorphine and methadone for opioid MAT.31 In addition to regulatory considerations, workforce capacity (e.g., limited waivered clinicians), geographic disparities, reimbursement (payer) policy, and stigma toward addiction inhibit MAT.32–34
Limitations
This study did not address overdoses in non-inpatient settings (e.g., emergency departments), length of index stay, non-opioid overdoses, potential drug misclassification on the discharge record, non-hospital mortality, nor related outpatient services. Index stays were patients’ first 2016 opioid overdose admission, but not necessarily first ever such admission. This analysis did not control for patient race/ethnicity (not reported in HCUP-NRD). Readmissions in other U.S. states and calendar years are not observable through HCUP-NRD; however, these circumstances likely have a modest impact on readmission rates.14 This study period comprises hospitals’ first full year of ICD-10-CM diagnosis coding, which may be more sensitive to identify opioid-related hospital stays.15
CONCLUSIONS
A quarter of opioid overdose patients have 90 or less days all-cause readmissions, although opioid overdose readmission is uncommon. Effective strategies to reduce readmissions following opioid overdose likely require greater coordination of general medical, substance use, and mental health care.27
ACKNOWLEDGMENTS
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Author responsibilities were as follows: led the study design and interpretation of results (CP), assisted with the study design and interpretation of results (YL, LX, NN, KZ, CAM), conducted data analysis (YL, LX), drafted the manuscript (CP), edited the manuscript (CP, YL, LX, NN, KZ, CAM), and approved the final manuscript as submitted (CP, YL, LX, NN, KZ, CAM).
REFERENCES
- 1.Hsu DJ, McCarthy EP, Stevens JP, Mukamal KJ. Hospitalizations, costs and outcomes associated with heroin and prescription opioid overdoses in the United States 2001–12. Addiction. 2017;112(9):1558–1564. 10.1111/add.13795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stevens JP, Wall MJ, Novack L, Marshall J, Hsu DJ, Howell MD. The critical care crisis of opioid overdoses in the United States. Ann Am Thorac Soc. 2017;14(12):1803–1809. 10.1513/Annal-sATS.201701-022OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tedesco D, Asch SM, Curtin C, et al. Opioid abuse and poisoning: trends in inpatient and emergency department discharges. Health Aff (Millwood). 2017;36(10):1748–1753. 10.1377/hlthaif.2017.0260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Weiss AJ, Elixhauser A, Barrett ML, Steiner CA, Bailey MK, O’Malley L. Opioid-related inpatient stays and emergency department visits by state, 2009–2014: Statistical Brief #219 In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville, MD: Agency for Healthcare Research and Quality; 2016. [Google Scholar]
- 5.Mark TL, Tomic KS, Kowlessar N, Chu BC, Vandivort-Warren R, Smith S. Hospital readmission among Medicaid patients with an index hospitalization for mental and/or substance use disorder. J Behav Health Serv Res. 2013;40(2):207–221. 10.1007/s11414-013-9323-5. [DOI] [PubMed] [Google Scholar]
- 6.Walley AY, Paasche-Orlow M, Lee EC, et al. Acute care hospital utilization among medical inpatients discharged with a substance use disorder diagnosis. J Addict Med. 2012;6(1):50–56. 10.1097/ADM.0b013e318231de51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gupta A, Nizamuddin J, Elmofty D, et al. Opioid abuse or dependence increases 30-day readmission rates after major operating room procedures: a national readmissions database study. Anesthesiology. 2018;128 (5):880–890. 10.1097/ALN.0000000000002136. [DOI] [PubMed] [Google Scholar]
- 8.Mosher HJ, Jiang L, Vaughan Sarrazin MS, Cram P, Kaboli PJ, Vander Weg MW. Prevalence and characteristics of hospitalized adults on chronic opioid therapy. J Hosp Med. 2014;9(2):82–87. 10.1002/jhm.2113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Micic D, Gaetano JN, Rubin JN, et al. Factors associated with readmission to the hospital within 30 days in patients with inflammatory bowel disease. PLoS One. 2017;12(8):e0182900 10.1371/journal.pone.0182900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Morizio KM, Baum RA, Dugan A, Martin JE, Bailey AM. Characterization and management of patients with heroin versus nonheroin opioid overdoses: experience at an academic medical center. Pharmacotherapy. 2017;37(7):781–790. 10.1002/phar.1902. [DOI] [PubMed] [Google Scholar]
- 11.Gulur P, Williams L, Chaudhary S, Koury K, Jaff M. Opioid tolerance — a predictor of increased length of stay and higher readmission rates. Pain Physician. 2014;17(4):E503–E507. [PubMed] [Google Scholar]
- 12.Kolodny A, Courtwright DT, Hwang CS, et al. The prescription opioid and heroin crisis: a public health approach to an epidemic of addiction. Annu Rev Public Health. 2015;36:559–574. 10.1146/annurev-publhealth-031914-122957. [DOI] [PubMed] [Google Scholar]
- 13.Olfson M, Crystal S, Wall M, Wang S, Liu SM, Blanco C. Causes of death after nonfatal opioid overdose. JAMA Psychiatry. 2018;75 (8):820–827. 10.1001/jamapsychiatry.2018.1471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cost Healthcare and Project Utilization. Introduction to the HCUP Nationwide Readmissions Database (NRD). www.hcup-us.ahrq.gov/db/nation/nrd/Introduction_NRD_2010-2015.pdf. Published 2017. Accessed July 18, 2018.
- 15.Heslin KC, Owens PL, Karaca Z, Barrett ML, Moore BJ, Elixhauser A Trends in opioid-related inpatient stays shifted after the U.S. transitioned to ICD-10-CM diagnosis coding in 2015. Med Care. 2017;55 (11):918–923. 10.1097/MLR.0000000000000805. [DOI] [PubMed] [Google Scholar]
- 16.Peterson C, Xu L, Mikosz CA, Florence C, Mack KA. U.S. hospital discharges documenting patient opioid use disorder without opioid overdose or treatment services, 2011—2015. J Subst Abuse Treat. 2018;92:35–39. 10.1016/j.jsat.2018.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cost Healthcare and Project Utilization. Beta Elixhauser Comorbidity Software for ICD-10-CM. www.hcup-us.ahrq.gov/toolssoftware/comor-bidityicd10/comorbidity_icd10.jsp. Published March 23, 2018. Accessed September 10, 2018.
- 18.Fingar KR, Barrett ML, Jiang HJ. A comparison of all-cause 7-day and 30-day readmissions, 2014: Statistical Brief #230. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville, MD: Agency for Healthcare Research and Quality; 2006. [PubMed] [Google Scholar]
- 19.Kingston REF, Marel C, Mills KL. A systematic review of the prevalence of comorbid mental health disorders in people presenting for substance use treatment in Australia. Drug Alcohol Rev. 2017;36 (4):527–539. 10.1111/dar.12448. [DOI] [PubMed] [Google Scholar]
- 20.Mitchell AJ, Malone D, Doebbeling CC. Quality of medical care for people with and without comorbid mental illness and substance misuse: systematic review of comparative studies. Br J Psychiatry. 2009;194(6):491–499. 10.1192/bjp.bp.107.045732. [DOI] [PubMed] [Google Scholar]
- 21.Raven MC, Carrier ER, Lee J, Billings JC, Marr M, Gourevitch MN. Substance use treatment barriers for patients with frequent hospital admissions. J Subst Abuse Treat. 2010;38(1):22–30. 10.1016/j.jsat.2009.05.009. [DOI] [PubMed] [Google Scholar]
- 22.Reif S, Acevedo A, Garnick DW, Fullerton CA. Reducing behavioral health inpatient readmissions for people with substance use disorders: do follow-up services matter? Psychiatr Serv. 2017;68(8):810–818. 10.1176/appi.ps.201600339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wakeman SE, Metlay JP, Chang Y, Herman GE, Rigotti NA. Inpatient addiction consultation for hospitalized patients increases post-discharge abstinence and reduces addiction severity. J Gen Intern Med. 2017;32(8):909–916. 10.1007/s11606-017-4077-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McKay JR. Continuing care research: what we have learned and where we are going. J Subst Abuse Treat. 2009;36(2):131–145. 10.1016/j.jsat.2008.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McKay JR, Gustafson DH, Ivey M, et al. Effects of automated smartphone mobile recovery support and telephone continuing care in the treatment of alcohol use disorder: study protocol for a randomized controlled trial. Trials. 2018;19(1):82 10.1186/s13063-018-2466-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Suzuki J, DeVido J, Kalra I, et al. Initiating buprenorphine treatment for hospitalized patients with opioid dependence: a case series. Am J Addict. 2015;24(1):10–14. 10.1111/ajad.12161. [DOI] [PubMed] [Google Scholar]
- 27.Korthuis PT, McCarty D, Weimer M, et al. Primary care-based models for the treatment of opioid use disorder: a scoping review. Ann Intern Med. 2017;166(4):268–278. 10.7326/M16-2149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Larochelle MR, Liebschutz JM, Zhang F, Ross-Degnan D, Wharam JF. Opioid prescribing after nonfatal overdose and association with repeated overdose: a cohort study. Ann Intern Med. 2016;164(1):1–9. 10.7326/M15-0038. [DOI] [PubMed] [Google Scholar]
- 29.Bailey GL, Herman DS, Stein MD. Perceived relapse risk and desire for medication assisted treatment among persons seeking inpatient opiate detoxification. J Subst Abuse Treat. 2013;45(3):302–305. 10.1016/j.jsat.2013.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Naeger S, Mutter R, Ali MM, Mark T, Hughey L. Post-discharge treatment engagement among patients with an opioid-use disorder. J Subst Abuse Treat. 2016;69:64–71. https://doi.org/10.1016Zj.jsat.2016.07.004. [DOI] [PubMed] [Google Scholar]
- 31.Substance Abuse and Mental Health Services Administration. Medication and counseling treatment. www.samhsa.gov/medication-assisted-treatment/treatment. Published September 28, 2015. Accessed November 26, 2018.
- 32.Sharma A, Kelly SM, Mitchell SG, Gryczynski J, O’Grady KE, Schwartz RP. Update on barriers to pharmacotherapy for opioid use disorders. Curr Psychiatry Rep. 2017;19(6):35 10.1007/s11920-017-0783-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dick AW, Pacula RL, Gordon AJ, et al. Growth in buprenorphine waivers for physicians increased potential access to opioid agonist treatment, 2002–11. Health Aff (Millwood). 2015;34(6):1028–1034. 10.1377/hlthaff.2014.1205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rosenblatt RA, Andrilla CH, Catlin M, Larson EH. Geographic and specialty distribution of U.S. physicians trained to treat opioid use disorder. Ann Fam Med. 2015;13(1):23–26. 10.1370/afm.1735. [DOI] [PMC free article] [PubMed] [Google Scholar]