Abstract
Introduction:
This study determines the incidence of opioid use before shoulder arthroplasty and analyzes its influence on postoperative use.
Methods:
A retrospective analysis of patients undergoing shoulder arthroplasty with at least 2-year follow-up was performed. Then, at pre- and postoperative appointments, the patients were asked “Do you take narcotic pain medication (codeine or stronger)?”
Results:
Among 490 patients included in the study, 35.5% reported preoperative opioid use. These patients had higher incidence of opioid use at 1-year follow-up (29.1% versus 4.9%; odds ratio, 8.320; P < 0.001) and at final follow-up (35.1% versus 7.3%; odds ratio, 6.877; P < 0.001). Opioid usage did not change markedly from 1 year follow-up to final follow-up (P > 0.18).
Discussion:
Approximately one-third of patients used opioids preoperatively and were seven times more likely to continue opioid use postoperatively. Opioid usage did not change from 1 year follow-up to final follow-up, suggesting that patients still using opioids at their 1-year appointment were likely to continue opioid use.
Level of Evidence:
Level III
Nationally, the current opioid epidemic has become an important topic because of the adverse consequences of these medications and the notable morbidity associated with its overuse. Opioid use accounts for nearly 40% of poisoning deaths in the United States1 and causes more deaths than suicide or motor vehicle collisions.2 More than half of opioid-associated deaths occur despite patients being prescribed opioids in accordance with guidelines from medical boards.2 The number of opioid medications being prescribed per quarter in the United States has increased from 47 million in 2006 to 62 million in 2012.3 In 2008, a report showed that United States is responsible for approximately 80% of the world’s opioid consumption despite only representing 4.6% of the world’s population.4 Understanding the effect of opioid abuse is especially important in orthopaedic practice, because orthopaedic surgeons are the third largest provider of opioid prescriptions among physicians.5 The cause of a largely disproportionate consumption of opioids in the United States is likely multifactorial and can be attributed to the belief that pain is under- treated,2 patient expectations of being relatively pain free after surgery, and surgeons striving to maximize patient satisfaction through pain control.
Patients suffering from degenerative conditions of the glenohumeral joint are frequently offered shoulder arthroplasty as a means to decrease shoulder pain and to improve shoulder function. A notable number of these patients are likely consuming opioids preoperatively for pain control. Preoperative opioid use in patients undergoing shoulder arthroplasty has been linked to an increased risk of falls,6 worse overall postoperative motion, and lower patient-reported outcomes.7,8 Additionally, preoperative opioid use has been associated with patients reporting higher postoperative pain and increased use of opioids during hospitalization.9 However, no study to date has analyzed the effect of preoperative opioid use on continued postoperative opioid use at 1- and 2-year follow-up after shoulder arthroplasty. This study determines the incidence of preoperative opioid use in patients undergoing shoulder arthroplasty, analyzes the influence of preoperative opioid use on prolonged postoperative use, and determines whether the incidence of opioid use markedly changes after the first postoperative year. We hypothesize that patients who were using opioids preoperatively will have a higher incidence of postoperative use compared with patients who were not taking opioids preoperatively. Furthermore, we suspect that the incidence of opioid use will not markedly change after the first postoperative year.
Methods
A retrospective query of a Western Institutional Review Board (WIRB)-approved Levy Shoulder and Elbow Surgical Repository (WIRB Study #1138999, WIRB Protocol #: 20130731) was performed from November 2006 to May 2015. An Institutional Review Board exemption determination (Protocol #: 2017–017-EX) was obtained before initiation of this study. As part of the standard registry protocol, using the American Shoulder and Elbow Surgeons Assessment Form, at preoperative and all subsequent postoperative appointments, the patients are asked “Do you take narcotic pain medication (codeine or stronger)?” All patients undergoing hemiarthroplasty, anatomic total shoulder arthroplasty (TSA), or reverse TSA, which provided answers to the above-mentioned question at pre- and postoperative appointments were included. Patients who did not complete this portion of the questionnaire at the preoperative visit were excluded. The percentage of patients using opioids at 1-year follow-up and at most recent follow-up appointments were compared based on preoperative narcotic pain medication usage.
All surgeries were performed by a single, high-volume, fellowship-trained shoulder surgeon. No patient was prescribed opioids by the operating surgeon before surgery. All shoulder arthroplasties were performed in a beach chair position under general anesthesia with a preoperative, singleshot, interscalene block. Postoperative narcotic prescriptions were routinely given to patients after surgery and refilled as necessary for up to 3 months after surgery. Opioid medication used by patients outside this window was obtained elsewhere.
Statistical comparison was performed by way of odds ratios and chi squares. Odds ratios (ORs) are presented with their respective 95% confidence intervals (95% CIs). An alpha value of less than 0.05 was deemed as significant. The analysis was conducted on SPSS Version 19 (IBM).
Results
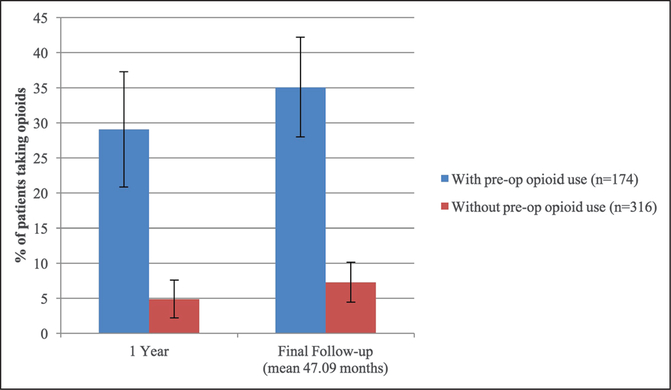
After exclusion of 28% of patients who did not answer the question related to narcotic usage at the pre-operative visit, the retrospective query identified 490 patients having at least 2-year follow-up (mean age, 71 years; range, 30 to 90 years). Preoperative opioid use was reported by 35.5% of patients (n = 174) and 17.1% (n = 84) reported opioid use at final follow-up (mean, 47 months; range, 24 to 124 months). Patients reporting preoperative narcotic use had a markedly higher incidence of opioid use at 1-year follow-up (29.1% versus 4.9%; OR, 8.320; 95% CI, 4.509 to 15.355; P < 0.001) and at final follow-up (35.1% versus 7.3%; OR, 6.877; 95% CI, 4.062 to 11.641; P < 0.001) compared with patients without preoperative use (Figure 1). Opioid usage did not change markedly between 1-year follow-up and final follow-up visits for patients with preoperative opioid use (29.1% versus 35.1%; OR, 0.768; 95% CI, 0.489 to 1.206; P = 0.251) or for patients without preoperative opioid use (4.9% versus 7.3%; OR, 0.635; 95% CI, 0.325 to 1.241; P = 0.181) (Table 1). At most recent follow-up, 31 of the 84 patients taking narcotic pain medication reported experiencing shoulder pain. Opioid usage based on indications is highlighted in Table 2.
Figure 1.
Opioid use after shoulder arthroplasty for patients with at least 2-year follow-up (n = 490).
Table 1.
Patients With At Least 2-Year Follow-up Reporting Opioid Use at Postoperative Intervals
| With Preoperative Opioid Use | Without Preoperative Opioid Use | P Value | |
|---|---|---|---|
| Minimum 2-year follow-up (n = 490) | 174 (35.5%) | 316 (64.5%) | |
| 1 year postoperatively | 34a (29.1%) | 12b (4.9%) | <0.001 |
| Final follow-up (mean, 47 mo) | 61 (35.1%) | 23 (7.3%) | <0.001 |
| P value | 0.251 | 0.181 |
Of 117 patient responses.
Of 246 patient responses.
Table 2.
Report of Opioid Use Based on Indication
| Indicationa | Number | Average Age (yr) | % Female Patients | % Opioid Use Preoperatively | % Opioid Use at 3 mo | % Opioid Use at 6 mo | % Opioid Use at 12 mo | % Opioid Use at 24 mo |
|---|---|---|---|---|---|---|---|---|
| OA without RCT | 261 | 71 | 50 | 27 | 13 | 10 | 10 | 10 |
| OA with RCT | 146 | 74 | 60 | 38 | 25 | 18 | 12 | 12 |
| Fracture sequelae | 27 | 75 | 67 | 50 | 35 | 16 | 13 | 12 |
| Avascular necrosis | 15 | 59 | 47 | 55 | 33 | 36 | 23 | 21 |
| Failed arthroplasty | 26 | 68 | 54 | 56 | 44 | 42 | 30 | 26 |
| Locked dislocation | 12 | 72 | 83 | 57 | 50 | 10 | 10 | 10 |
| Inflammatory arthritis | 25 | 72 | 72 | 35 | 32 | 20 | 16 | 8 |
OA = osteoarthritis, RCT = rotator cuff tear
Some patients have more than one listed surgical indication and are thus included in multiple categories.
Discussion
The opioid epidemic is one of the largest medical issues facing the United States and is particularly concerning in the field of orthopaedic surgery. As one of the top prescribers of opioid medications,5 it is imperative that orthopaedic surgeons understand what factors may predict prolonged opioid usage. The current study demonstrates that among all patients undergoing shoulder arthroplasty, more than one-third were taking opioids at their preoperative appointment. Patients taking opioids before surgery had five times higher incidence of opioid usage and were nearly seven times (OR, 6.877; P < 0.001) more likely to be using narcotics at an average of 4 years after surgery, thus confirming our original hypothesis. Furthermore, the percentage of patients taking opioids did not change markedly from 1 year postoperatively to final follow-up.
The high percentage of patients using opioid medications before shoulder arthroplasty surgery is alarming, especially in light of the numerous negative effects of preoperative opioid use demonstrated in the literature. Morris and colleagues7,8 concluded that opioid use before shoulder arthroplasty resulted in worse motion after TSA and worse patient-reported outcomes for pain and function after both TSA and reverse shoulder arthroplasty. A recent study by Cheah et al9 demonstrated that patients using opioids preoperatively had worse postoperative visual analog scale pain scores and required greater amounts of morphine equivalents during their postoperative hospitalization. The prevalence of opioid dependence and abuse among orthopaedic patients has grown by 152% from 2002 to 2011, and these patients have an increased risk of postoperative morbidity and mortality.10 Therefore, it should be a priority for orthopaedic surgeons to identify patients using narcotics in the preoperative period and council these patients on the potentially negative effects of opioid use before undergoing shoulder arthroplasty. The American Academy of Orthopaedic Surgeons has issued a statement in support of a comprehensive opioid program for more effective control of opioid use in orthopaedic patients. Recommendations in this statement include the restriction of preoperative opioid use in patients with degenerative, nonacute disease, as well as limitations on postoperative opioid prescriptions.11 Many orthopaedic patients are not prescribed opioid medications by the surgeon, so it is necessary for orthopaedic surgeons to collaborate and communicate with primary care physicians and pain management specialists in an effort to wean patients off opioid medications before elective orthopaedic surgery whenever possible.
In the current study, patients using opioids before shoulder arthroplasty were far more likely to continue prolonged opioid use in the postoperative period. This is in agreement with the study by Bedard et al which used the Humana database to analyze opioid use in patients undergoing total knee arthroplasty. In concordance with the current study, approximately one-third of patients undergoing total knee arthroplasty were taking opioids preoperatively. Preoperative opioid use was found to be the strongest predictor of postoperative use.12
The current study showed no notable difference in the percentage of patients using postoperative opioids from 1-year follow-up to final follow-up, suggesting that patients taking opioids at 1 year postoperatively are likely to continue use. This further highlights the importance of preoperative screening for opioid use in patients undergoing elective orthopaedic procedures in an effort to curtail prolonged postoperative use.
Providing patients with sufficient preoperative counseling regarding the nature of the procedure along with education on multimodal pain management efforts may help calm fears of postoperative pain and establish appropriate patient expectations for the anticipated surgery. Multimodal pain management protocols have been shown to reduce the need for opioid use after shoulder arthroplasty.13 Furthermore, clearly defined preoperative education on postoperative opioid consumption has been shown to limit postoperative opioid use.14 With a renewed focus of surgeons on preoperative patient education for pain management after shoulder arthroplasty, we should see a decrease in postoperative opioid use in the near future.
Among the strengths of the current study is the large number of patients included, because 490 patients had at least 2-year follow-up, decreasing the fragility of the observational data reported. Furthermore, all patients were treated with the same pain management protocols throughout the perioperative period.
This study has several limitations. First, opioid use was patient reported and thus relied on the honesty of the patient. Second, opioid use was measured qualitatively rather than quantitatively. We therefore could not determine whether correlations existed between the quantity of opioids ingested preoperatively (measured in morphine equivalents) and postoperative use. Patient characteristics such as the presence of chronic pain, illicit drug use, psychological disorders, or other comorbidities were not accounted for and certainly may have influenced opioid use in certain patients. These limitations do not, however, detract from the significance of our conclusion which clearly demonstrated that high rates of preoperative opioid use predict high rates of postoperative use. Finally, although a single-surgeon, single-center study provides the advantage of a standardized surgical protocol, it is limited to a single geographic region that may not be representative of the entire United States where narcotic use may vary by geographic location.
Conclusions
More than one-third of the patients included in this study were taking opioids before shoulder arthroplasty. The cohort of patients taking preoperative opioids had five times greater incidence of opioid use postoperatively and was nearly seven times more likely to be using opioids at an average of 4 years later. Furthermore, narcotic usage did not markedly change from 1-year follow-up to final follow-up. This suggests that patients who remain on opioid medications at their 1-year postoperative appointment will likely continue to use opioids.
Contributor Information
Dr. Derek D. Berglund, Holy Cross Orthopedic Institute, Oakland Park, FL.
Dr. Samuel Rosas, Holy Cross Orthopedic Institute, Oakland Park, FL; Wake Forest School of Medicine, Winston-Salem, NC.
Dr. Jennifer Kurowicki, Holy Cross Orthopedic Institute, Oakland Park, FL; Seton Hall University School of Health and Medical Sciences, South Orange, NJ.
Dr. Brandon Horn, Witham Orthopaedic Associates, Lebanon, IN.
Dr. Dragomir Mijic, Holy Cross Orthopedic Institute, Oakland Park, FL.
Dr. Jonathan C. Levy, Holy Cross Orthopedic Institute, Oakland Park, FL.
References
- 1.Warner M, Chen LH, Makuc DM: Increase in fatal poisonings involving opioid analgesics in the United States, 1999–2006. NCHS Data Brief 2009:1–8. [PubMed] [Google Scholar]
- 2.Manchikanti L, Helm S II, Fellows B, et al. : Opioid epidemic in the United States. Pain Physician 2012;15:ES9–38. [PubMed] [Google Scholar]
- 3.Dart RC, Surratt HL, Cicero TJ, et al. : Trends in opioid analgesic abuse and mortality in the United States. N Engl J Med 2015;372:241–248. [DOI] [PubMed] [Google Scholar]
- 4.Manchikanti L, Singh A: Therapeutic opioids: A ten-year perspective on the complexities and complications of the escalating use, abuse, and nonmedical use of opioids. Pain Physician 2008;11:S63–S88. [PubMed] [Google Scholar]
- 5.Volkow ND, McLellan TA, Cotto JH, Karithanom M, Weiss SR: Characteristics of opioid prescriptions in 2009. JAMA 2011;305:1299–1301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Menendez ME, Ring D, Jawa A: Inpatient falls after shoulder arthroplasty. J Shoulder Elbow Surg 2017;26:14–19. [DOI] [PubMed] [Google Scholar]
- 7.Morris BJ, Sciascia AD, Jacobs CA, Edwards TB: Preoperative opioid use associated with worse outcomes after anatomic shoulder arthroplasty. J Shoulder Elbow Surg 2016; 25:619–623. [DOI] [PubMed] [Google Scholar]
- 8.Morris BJ, Laughlin MS, Elkousy HA, Gartsman GM, Edwards TB: Preoperative opioid use and outcomes after reverse shoulder arthroplasty. J Shoulder Elbow Surg 2015;24:11–16. [DOI] [PubMed] [Google Scholar]
- 9.Cheah JW, Sing DC, McLaughlin D, Feeley BT, Ma CB, Zhang AL: The perioperative effects of chronic preoperative opioid use on shoulder arthroplasty outcomes. J Shoulder Elbow Surg 2017;26:1908–1914. [DOI] [PubMed] [Google Scholar]
- 10.Menendez ME, Ring D, Bateman BT: Preoperative opioid misuse is associated with increased morbidity and mortality after elective orthopaedic surgery. Clin Orthop Relat Res 2015;473: 2402–2412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Opioid Use, Misuse, and Abuse in Orthopaedic Practice. Chicago, IL, American Academy of Orthopaedic Surgeons, 2015, Information Statement 1045. [Google Scholar]
- 12.Bedard NA, Pugely AJ, Westermann RW, Duchman KR, Glass NA, Callaghan JJ: Opioid use after total knee arthroplasty: Trends and risk factors for prolonged use. J Arthroplasty 2017;32:2390–2394. [DOI] [PubMed] [Google Scholar]
- 13.Routman HD, Israel LR, Moor MA, Boltuch AD: Local injection of liposomal bupivacaine combined with intravenous dexamethasone reduces postoperative pain and hospital stay after shoulder arthroplasty. J Shoulder Elbow Surg 2017;26:641–647. [DOI] [PubMed] [Google Scholar]
- 14.Tjoumakaris FP, Syed UAM, Aleem AW, et al. : Does patient education prior to arthroscopic rotator cuff repair decrease narcotic consumption? A randomized prospective study. Orthopaedic J Sports Med 2017;5:2325967117S00280. [Google Scholar]