Abstract
Background
In rural areas of Bangladesh, the majority of patients with ST segment elevation myocardial infarction (STEMI) have little access to reperfusion therapy. Even though thrombolysis can be an affordable life-saving treatment in a low income setting, there are few publications in regards to the clinical and socioeconomic features of STEMI with thrombolytic therapy in rural Bangladesh.
Method
The information of the patients who were admitted for STEMI between 2010 and 2016 from one rural hospital were collected and reviewed. This audit evaluated clinical outcomes and socioeconomic characteristics of the patients.
Result
164 patients with STEMI were identified in the period and 136 patients (82.93%) underwent thrombolysis. The mean pain-to-door time was 472 min (7.87 h ± 12.40). Only 5.49% of the patients traveled to hospital by ambulances. Overall in-hospital mortality rate and major adverse cardiovascular event (MACE) after STEMI were 19.51% (32/164), 23.17% (38/164), respectively. The need of inotropics (Odds ratio [OR] 16.43, 95% confidence interval [CI] 1.99–135.75, P < 0.01), the use of defibrillation due to ventricular arrhythmias (OR 33.58, 95% CI 2.96–380.49, P < 0.01) were independent predictors of increased in-hospital mortality.
Conclusion
In a rural hospital of Bangladesh, in-hospital mortality rate after STEMI is high in spite of thrombolysis and adherence to published guidelines. The prolonged pain-to-door time and the poor coverage of ambulance services in our study highlight the need of community awareness of acute coronary syndrome and comprehensive emergency medical services in rural Bangladesh.
Keywords: STEMI, Thrombolysis, Low income setting, Bangladesh
1. Introduction
Cardiovascular disease takes the lives of 17.7 million people each year, and estimated 31% of all deaths worldwide with over 75% of cardiovascular deaths occurring in low-income and middle-income countries (LMIC) [1,2]. During recent decades, Bangladesh has experienced a rapid epidemiological transition from communicable to non-communicable diseases [3]. Of these, being the fourth leading cause of death in Bangladesh, ischemic heart disease claimed 50,700 deaths in 2012 [4]. ST elevation myocardial infarct (STEMI) is a life-threatening heart disease, particularly with high early mortality rate if not treated properly. Despite global agreement on most issues related to the management of STEMI, clinical practice and outcome after STEMI varies with a great deal between countries and regions [2,5]. Moreover, in rural areas of Bangladesh, most patients with STEMI have little access to thrombolysis or primary coronary intervention, because very few rural hospitals are ready to treat STEMI patients. Bangladesh is one of the LMICs with an estimated population of approximately 161.9 million, and with 71.6% living in rural settings. [6] Nevertheless, there are few publications in regards to the clinical management and socioeconomic evaluations of STEMIs for populations that reside in low income rural Bangladesh. The aim of this study therefore is to decrease the gap of knowledge regarding the care for these patients by evaluating the in-hospital clinical outcome of patients with STEMI who were treated in a rural hospital in a low-income setting of Bangladesh.
2. Materials and methods
2.1. Data collection
The authors conducted a retrospective chart review of clinical data from January 2010 to December 2016 of patients diagnosed with STEMI at a primary care hospital in rural Bangladesh. This study was reviewed and approved by LAMB hospital ethics committee (#1/REC/19, January 20, 2019). Patients were identified with assistance from the hospital's medical information system by searching the records for charts containing the ICD-9 code for STEMI. The patient clinical data including ECG results, medical management in regards to adherence to hospital STEMI guidelines, thrombolytic or defibrillator use, transthoracic echocardiogram results, patient co-morbidities, risk factors, and in-hospital mortality, major adverse cardiovascular event (MACE) were reviewed. MACE was defined as composite mortality, re-infarction, stroke, and target vessel revascularization (TVR). Failed thrombolysis could not be defined well in our study because coronary angiography was rarely done among our patients. To assess the adherence to 2013 ACCF/AHA guideline for the management of patients with STEMI, the utilization of dual antiplatelet therapy (DAPT), angiotensin converting enzyme inhibitor (ACEI), beta-blocker and statin was counted [7]. In addition, socioeconomic data including patient use of financial subsidy, demographic data including location, financial income, and means of transportation to hospital were also recorded. Patients' address information was matched on Google map to determine latitude and longitude for geographic analysis.
2.2. Hospital care setting
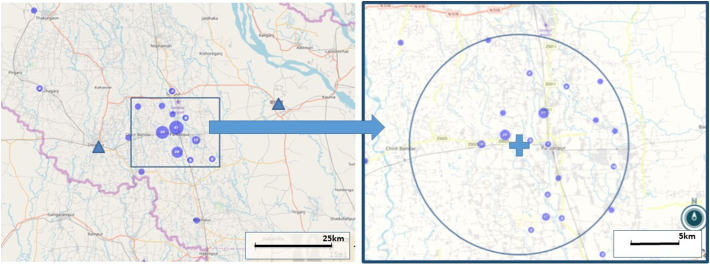
LAMB hospital is a 150-bed capacity hospital in a rural area of Dinajpur district, Bangladesh. The population of the district is approximately 3 million with three hospitals (including LAMB hospital) which can offer thrombolysis for STEMI patients in this region (Fig. 1). In our limited resource, 12 leads-ECG machines, cardiac monitors, defibrillators, oxygen supply and transthoracic echocardiography were utilized, but a percutaneous coronary intervention (PCI) facility was not available. The nearest PCI centers are located at 1.5 hour-distance by car.
Fig. 1.
The case distribution around LAMB hospital.
Triangles: other thrombolytic centers, Cross: LAMB hospital, Dots: cases in the region. Circle: radius 10 km. A magnified map (right) shows the patients distribution in Parbatipur around LAMB hospital. 86.6% (142/164) of STEMI patients traveled <10 km.
The published guidelines for STEMI management were implemented for patient care [7]. Streptokinase was the only available thrombolytic agent in our institute. Junior doctors, hospital paramedics and nurses were trained with a summary of the guidelines. At least one senior physician was available for the management of STEMI 24 h per day.
2.3. Socioeconomic assessment and support
Social workers evaluated patients' income and asset comprehensively after admission. The patients' socioeconomic status was divided into 6 groups according to the composite income on the evaluation. Patients who could not pay the bill for treatment received a subsidy in accordance with financial ability from a charity fund which was named as ‘poor fund’.
2.4. Statistical analysis
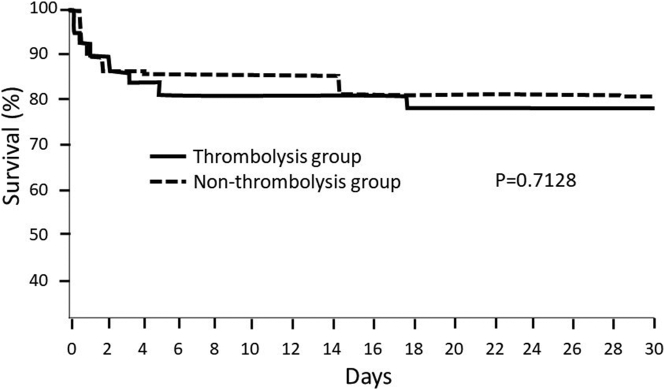
The socioeconomic, demographic data, along with risk factors, therapeutics used, diagnostic tests ordered, left ventricular ejection fractions (LVEF), defibrillator use and outcome, infarct territory, mortality outcomes were presented as standard descriptive statistics. The clinical data was compared between Thrombolysis group and Non-thrombolysis group as well as between the mortality group and the survival group. Data was shown in numbers, means ±standard deviation (SD), percentages and frequencies. Nominal variables were compared using Χ2 test. Continuous variables were analyzed with Student's t-test or Mann-Whitney test for intergroup comparisons. Kaplan-Meier survival curve was drawn to compare the survival rates of the thrombolysis group and the non-thrombolysis group up to 30 days after STEMI. Binary logistic regression was performed to evaluate the independent predictors for in-hospital mortality and the risk of not being thrombolysed after STEMI. A P-value <0.05 was accepted statistically significant. All statistical analysis was done with Epi-Info 7.2.2.2. software (the Centers for Disease Control and Prevention, USA).
3. Results
3.1. Patient demographics and risk factors
During the study period of 7 years from February 2010 to December 2016, 12,513 patients (1787.6 patients per year in average) were admitted to the internal medicine department. Of these patients, 164 patients (1.31% of the total admitted patients) had been recorded to have the diagnosis of STEMI (Table 1). On the review of ECG findings, all of 164 patients met the clinical and ECG diagnostic criteria of STEMI as described by 2013 ACCF/AHA guidelines [7]. 28 patients (17.1%) were not eligible for thrombolysis mainly because of delayed arrival to hospital. The average age of STEMI patient was 57.07(±12.40) and of these women represented 25% (41/164) of study participants. Smoking appeared to be the most common risk factor (83/164, 50.61%). Non-thrombolysis group has significantly more female patients, compared to Thrombolysis group (Table 1).
Table 1.
Demographics and risk factors.
| Study subjects (n = 164) | Non-thrombolysis (n = 28) | Thrombolysis (n = 136) | P-value | |
|---|---|---|---|---|
| Age | 57.07 (±12.40) | 53.5(±13.51) | 57.75(±12.57) | 0.11 |
| Female sex | 41 (25.00) | 12 (42.86) | 29 (21.32) | 0.03* |
| Hypertension | 70 (42.68) | 12 (42.86) | 58 (42.65) | 0.98 |
| Diabetes mellitus | 36 (23.78) | 6 (21.43) | 30 (22.06) | 0.94 |
| Smoking | 83 (50.61) | 12 (42.86) | 71 (52.21) | 0.49 |
| Systolic blood pressure | 122.7 (±36.70) | 122 (±36.94) | 126.31 (±35.92) | 0.57 |
| Diastolic blood pressure | 78.86 (±22.36) | 78.49 (±22.45) | 80.77 (±22.26) | 0.62 |
| Body mass index | 22.72 (±3.45) | 22.89 (±3.29) | 22.10 (±4.04) | 0.27 |
| Transport | 0.51 | |||
| Man-powered vehicle | 86 (52.44) | 12 (42.86) | 74 (54.41) | |
| Motor vehicle | 51 (31.10) | 12 (42.86) | 39 (28.68) | |
| Ambulance | 9 (5.49) | 1 (3.57) | 8 (5.88) | |
| Not reported | 18 (10.98) | 3 (10.71) | 15 (11.03) | |
| Residence area | 0.16 | |||
| Parbatipur residents | 138 (84.15) | 21 (75.00) | 117 (86.03) | |
| Non-Parbatipur residents | 26 (15.85) | 7 (25.00) | 19 (13.97) | |
| Family income per month | 0.23 | |||
| Less than 35 USD | 3 (1.83) | 0 (0.00) | 3 (2.21) | |
| 35–69.9 USD | 58 (35.37) | 12 (42.86) | 46 (33.82) | |
| 70–106.9 USD | 30 (18.29) | 2 (7.14) | 28 (20.59) | |
| 107–176.9 USD | 34 (20.73) | 7 (25.00) | 27 (19.85) | |
| 177–354.9 USD | 15 (9.15) | 1 (3.57) | 14 (10.29) | |
| More than 355 USD | 4 (2.44) | 0 (0.00) | 4 (2.94) | |
| Missing assessment | 20 (12.20) | 6 (21.43) | 14 (10.29) |
Continuous variables are expressed as means with standard deviation in brackets; all others represent numbers of patients with values in brackets representing percentages.
P < 0.05.
3.2. Geographic distribution and mode of transport
84.15% (138/164) of STEMI patients resided in Parbatipur upazila (subdistrict), where our institute is located, specifically 75.00% (21/28) of Non-thrombolysis group and 86.03% (117/136) of Thrombolysis group (Table 1). 86.59% (142/164) of the patients traveled <10 km (Fig. 1). 52.44% (86/164) of the patients traveled by man-powered vehicles (rickshaw or vangari) and there was no significant difference between Thrombolysis group and Non-thrombolysis group in terms of the mode of transport (Table 1). Only 5.49% (9/164) of STEMI patients were transported by ambulance. None of the local ambulances offered emergency medical services by trained paramedics.
3.3. Socioeconomic status
The monthly income <9000 taka (106 US dollar) was considered as the poverty threshold in our hospital. 55.49% (91/164) of patients were below the poverty threshold (Table 1). 12.20% (20/164) of patients eluded financial assessment by social workers.
3.4. Management and outcomes
Non-thrombolysis group has significantly prolonged pain-to-door time (25.83 ± 29.20 h) when compared to Thrombolytic group (4.17 ± 3.86 h) (Table 2). The average door-to-needle time was 38.28 min, and 62.50% (85/136) of thrombolysed patients received streptokinase <30 min after arrival to hospital. 98.17% (161/164) of study subjects had dual anti-platelet therapy (DAPT). The overall utilization rate of beta blocker, ACEI, and statin was 64.02%, 84.15%, and 93.90%, respectively. The prescription rate of 3 drugs (DAPT plus ACEI), 4 drugs (3 drugs plus beta blocker), and 5 drugs (4 drugs plus statin) at the time of discharge was 83.54%, 59.76%, and 57.93%, respectively. 18 patients (18/164, 10.98%) received defibrillation due to ventricular fibrillation or sustained ventricular tachycardia (Table 2). 9 of them (9/18, 50.00%) died after defibrillation.
Table 2.
Clinical management and outcomes.
| Study subjects (n = 164) | Non-thrombolysis (n = 28) | Thrombolysis (n = 136) | P-value | |
|---|---|---|---|---|
| PTD (h) | 7.87 (±12.40) | 25.83 (±29.20) | 4.17 (±3.86) | <0.0001⁎ |
| DTN (min) | 38.28 (±41.19) | |||
| DTN < 30 min | 85(62.50) | |||
| PTN (h) | 4.86 (±4.16) | |||
| Aspirin | 163 (99.39) | 27 (96.43) | 136 (100) | 0.38 |
| Clopidogrel | 161 (98.17) | 26 (92.86) | 135 (99.26) | 0.13 |
| Beta blocker | 105 (64.02) | 16 (57.14) | 89 (65.44) | 0.54 |
| ACEI | 138 (84.15) | 21 (75.0) | 117 (86.03) | 0.16 |
| Atorvastatin < 40 mg | 154 (93.90) | 25 (89.29) | 129 (94.85) | 0.49 |
| Atorvastatin ≧ 40 mg | 65 (39.63) | 13(46.43) | 52 (38.24) | 0.55 |
| DAPT | 161 (98.17) | 26 (92.86) | 135 (99.26) | 0.13 |
| 3 Drug (DAPT + ACEI) | 137 (83.54) | 20 (71.43) | 117 (86.03) | 0.11 |
| 4 Drug (3 drug + β blocker) | 98 (59.76) | 14 (50.00) | 84 (61.76) | 0.35 |
| 5 Drug (4 drug + statin) | 95 (57.93) | 14 (50.00) | 81 (59.56) | 0.47 |
| Heparin | 147 (89.63) | 22 (78.57) | 125 (91.91) | 0.08 |
| LMWH | 91 (55.49) | 15 (53.57) | 76 (55.88) | 0.99 |
| Shock at presentation | 43 (26.22) | 6 (21.43) | 37 (27.21) | 0.69 |
| Inotropics | 51 (31.10) | 8 (28.57) | 43 (31.62) | 0.93 |
| Defibrillation d/t VF/VT | 18 (10.98) | 1 (3.57) | 17 (12.50) | 0.30 |
| Mortality | 32 (19.51) | 5 (17.86) | 27 (19.85) | 0.98 |
| Bleeding required transfusion | 2 (1.22) | 0 (0.00) | 2 (1.47) | 0.69 |
| Stroke | 3 (1.83) | 0 (0.00) | 3 (2.21) | 0.57 |
| Referred for PCI | 3 (1.83) | 1 (3.57) | 2 (1.47) | 0.43 |
| CABG | 1 (0.61) | 0 (0.00) | 1 (0.74) | 0.83 |
| TVR | 4 (2.44) | 1 (3.57) | 3 (2.21) | 0.53 |
| MACE at 30 days | 38 (23.17) | 6 (21.43) | 32 (23.53) | 0.51 |
| LVEF (%) | 45.37 (±16.84) | 40.20 (±13.33) | 47.14 (±17.39) | 0.09 |
| LVEDD (mm) | 48.91 (±8.29) | 46.73 (±5.83) | 49.43 (±8.72) | 0.15 |
| LVESD (mm) | 38.05(±8.54) | 37.68(±6.53) | 38.14 (±8.98) | 0.81 |
| Treatment cost (US dollars) | 178.4 ± 74.3 | 135.6 ± 42.1 | 186.0 ± 76.7 | <0.01⁎ |
| Financial support | 74.6 ± 53.1 | 42.5 ± 47.3 | 80.4 ± 70.8 | 0.04⁎ |
| Patient's payment | 100.8 ± 68.6 | 91.4 ± 38.2 | 101.2 ± 55.7 | 0.44 |
Continuous variables are expressed as means with standard deviation in brackets; all others represent numbers of patients with values in brackets representing percentages.
PTD: pain-to-door time; DTN: door-to-needle time; PTN: pain-to-needle time; ACEI: angiotensin converting enzyme inhibitor; DAPT: dual antiplatelet therapy; PCI: percutaneous coronary intervention; TVR: target vessel revascularization; CABG: coronary artery bypass graft; MACE: major adverse cardiovascular event; LVEF: left ventricle ejection fraction; LVEDD: left ventricle end-diastolic dimension; LVESD: left ventricle end-systolic dimension; LMWH: low molecular weight heparin; VF/VF: ventricular fibrillation/ventricular tachycardia.
P < 0.05.
The overall in-hospital mortality rate, MACE at 30 days after STEMI patients was 19.51% (32/164), 23.17% (38/164), respectively. Cardiogenic shock (18/32, 56.25%) was the most common cause of death, followed by ventricular arrhythmia (12/32, 37.5%) and intractable heart failure (2/32, 6.25%). No death was reported to be related with bleeding or anaphylaxis after thrombolytic therapy. There was no significant difference in terms of in-hospital mortality (17.86% vs 19.85%, P = 0.98) and MACE at 30 days (21.43% vs. 23.53%, P = 0.51) between Non-thrombolysis group and Thrombolysis group (Table 2). Bleeding complications requiring transfusion occurred in two cases (1.47%, 2/136) in Thrombolysis group. Stroke was noted in three cases (1.83%, 3/164). Of these, one patient experienced major stroke with poor neurologic outcome after thrombolysis and intracranial hemorrhage was clinically suspected. Only three patients (1.83%, 3/164) were referred to PCI capable centers. One patient received coronary artery bypass graft (CABG) after thrombolysis (Table 2). Thus, only four patients (2.44%, 4/164) had TVR after STEMI.
The average echocardiographic ejection fraction (EF) of STEMI patients was 45.37%. There was no significant difference in terms of EF, left ventricle end diastolic dimension (LVEDD) and left ventricle end systolic dimension (LVESD) between Non-thrombolysis group and Thrombolysis group (Table 2).
The comparison between the mortality group and the survival group showed no significant differences of age, sex, hypertension, diabetes, pain-do-door time, thrombolytic treatment, and diastolic pressure between the two groups (Table 3). Initial presentation as shock, the need of inotropics, and defibrillation were more common in the mortality group in the chi square test (Table 3). Nevertheless, the binary logistic regression analysis showed that only the use of inotropics (Odds ratio [OR] 16.43, 95% confidence interval [CI] 1.99–135.75, P < 0.01) and the requirement of defibrillation (OR 33.58, 95% CI 2.96–380.49, P < 0.01) were the independent predictors of increased in-hospital mortality, but shock on arrival wasn't (Table 4).
Table 3.
Mortality vs survival associations.
| Mortality group (n = 32) | Survival group (n = 132) | P-value | |
|---|---|---|---|
| Age | 59.26 ± 10.53 | 56.57 ± 12.77 | 0.28 |
| Female sex | 9/32 (28.13%) | 32/132 (24.24%) | 0.65 |
| Hypertension | 11/32 (34.38%) | 59/132 (44.70%) | 0.32 |
| Diabetes | 11/32 (34.38%) | 25/132 (18.94%) | 0.09 |
| Smoking | 11/32 (34.38%) | 72/132 (54.55%) | 0.049⁎ |
| Thrombolysis | 21/32 (84.38%) | 109/132 (82.58%) | 0.52 |
| Shock | 20/32 (62.50%) | 23/132 (17.42%) | <0.0001⁎ |
| Inotropics | 26/32 (81.25%) | 25/132 (18.94%) | <0.0001⁎ |
| Defibrillation | 9/32 (28.13%) | 9/132 (6.82%) | 0.0019⁎ |
| SBP | 108.46 ± 47.95 | 125.72 ± 32.29 | 0.02⁎ |
| DBP | 71.46 ± 28.53 | 80.4242 ± 20.61 | 0.05 |
| PTD (h) | 9.12 ± 16.92 | 7.57 ± 14.57 | 0.60 |
SBP: systolic blood pressure; DBP: diastolic blood pressure; PTD: pain-to-door time.
P < 0.05.
Table 4.
Binary logistic regression in regard to in-hospital mortality.
| Independent variables | In-hospital mortality |
||
|---|---|---|---|
| OR | 95% CI | P-value | |
| Aspirin | 0.00 | 0.00–1012 | 0.98 |
| Clopidogrel | 0.92 | 0.00–243.03 | 0.98 |
| ACE inhibitor | 0.04 | 0.01–0.27 | <0.001⁎ |
| Beta blocker | 0.19 | 0.03–1.01 | 0.05 |
| High dose statin | 0.37 | 0.06–2.37 | 0.29 |
| Heparin | 5.01 | 0.38–65.77 | 0.22 |
| LMWH | 1.76 | 0.24–12.90 | 0.58 |
| Furosemide | 2.83 | 0.37–21.96 | 0.32 |
| Spironolactone | 11.42 | 0.69–187.85 | 0.09 |
| Oral nitroglycerin | 0.60 | 0.07–4.96 | 0.64 |
| Inotropics | 16.43 | 1.99–135.75 | <0.01⁎ |
| Thrombolysis | 0.89 | 0.13–6.22 | 0.91 |
| Defibrillation | 33.58 | 2.96–380.49 | <0.01⁎ |
| Old age (>60 year) | 0.68 | 0.15–3.06 | 0.62 |
| Diabetes | 2.35 | 0.47–11.59 | 0.30 |
| Hypertension | 3.86 | 0.56–26.49 | 0.17 |
| Smoking | 0.21 | 0.04–1.11 | 0.07 |
| Low LVEF (<40%) | 0.16 | 0.03–1.02 | 0.05 |
| Female sex | 0.18 | 0.02–1.81 | 0.15 |
| Shock on arrival | 0.75 | 0.09–6.04 | 0.79 |
| Lower income (<107 USD/month) | 0.39 | 0.07–2.10 | 0.27 |
| Parbatipur residents | 0.21 | 0.02–2.46 | 0.22 |
ACE: angiotensin converting enzyme; LMWH: low molecular weight heparin; LVEF: left ventricle ejection fraction.
P < 0.05.
The use of ACEI (OR 0.04, 95% CI 0.01–0.27, P < 0.001) was an independent predictor of reduced in-hospital mortality (Table 4). None of other medications such as aspirin, clopidogrel, beta blockers, and statin independently predicted lower in-hospital mortality. Even though smoking was more commonly found in the survival group, smoking was not an independent predictor of increased in-hospital mortality after adjustment by binary logistic regression (Tables 3, 4). Family income <9000 taka per month, female sex were not independently associated with increased in-hospital mortality or the risk of not being thrombolysed (Tables 4, 5). Delayed arrival was the only independent predictor of not being thrombolysed.
Table 5.
Logistic regression analysis on the independent variables for the risk of not being thrombolysed.
| Independent variables | Risk of not being thrombolysed |
||
|---|---|---|---|
| OR | 95% CI | P-value | |
| Delayed arrival (>12 h) | 13.82 | 4.81–39.67 | <0.0001⁎ |
| Diabetes | 0.98 | 0.30-3.22 | 0.98 |
| Hypertension | 0.69 | 0.25–1.94 | 0.48 |
| Female sex | 2.85 | 0.97–8.39 | 0.06 |
| Old age (>60 yr) | 0.40 | 0.12–1.29 | 0.12 |
| Smoking | 1.42 | 0.49–4.13 | 0.52 |
| Lower income (<9000 taka/month) | 0.66 | 0.25–1.74 | 0.40 |
| Shock | 0.51 | 0.15–1.79 | 0.30 |
P < 0.05.
The log rank test showed no significant difference between Thrombolysis group and Non-thrombolysis group in regard to 30-days survival after STEMI (Fig. 2). Thrombolysis group had significantly higher cost than Non-thrombolysis group, requiring more financial support (Table 2). The cost of streptokinase was approximately 5000 Bangladesh taka (62.5 USD).
Fig. 2.
Comparison of early mortality after STEMI between Thrombolysis group and Non-thrombolysis group.
4. Discussion
Our study is a hospital-based audit in a low income setting in rural Bangladesh. Even though the mortality rate of STEMI is decreasing in developed countries in last decade, this study shows that the patients after STEMI have increased in-hospital mortality in a rural area of Bangladesh in spite of evidence-based management.
4.1. High mortality despite thrombolysis and evidence based therapeutics
The average door-to-needle time was 38 min in our study. 62.5% (85/136) of thrombolysis group had DNT <30 min (Table 2). Comparably, a study in Sri Lanka showed 42.3% of STEMI patients had DNT <30 min [8].
17.07% of STEMI patients were not thrombolysed in our study. Delayed arrival appeared to be the independent predictor of not being thrombolysed in our study (Table 5). DAPT, statin were applied >90%. The usage of beta-blocker at the time of discharge was quite low as 64.02%, compared to the other therapeutics. Since shock at the time of presentation was as high as 26.22% in our study, clinicians might have been reluctant to use beta-blocker in the fear of worsening shock or heart failure. 3 drugs (DAPT + ACEI) were applied for 83.54% of patients (Table 2). The use of ACEI was the only independent predictor of reduced in-hospital mortality (Table 3). Other medications which were known to have survival benefit for STEMI patients failed to predict reduced in-hospital mortality in our study, most likely due to small sample size.
The binary logistic regression analysis showed that inotropics use, defibrillation were the independent predictors of increased in-hospital mortality, though shock at the presentation was not. We would explain this with several ways. First, the initial presentation of shock did not always require inotropics and significant number of patients had good clinical outcome in spite of shock at arrival. For example, of 43 patients who presented as shock initially, 26 patients (26/43, 60.47%) had inferior wall MI with/without RV infarct. 11.54% (3/26) of the patients with inferior wall/RV infarct and shock did not require inotropics and had good clinical course. Those who needed inotropics may have represented patients with more severe cardiogenic shock in our study than those who did not need inotropics. Second, small patients number may weaken the statistical power in our study.
Despite the use of thrombolysis and evidence based therapeutics, our study demonstrated a high mortality rate (19.51%, 32/164) when compared to a multi-center study conducted in Sri Lanka [8] where the mortality rate of STEMI patients was as low as 3.95%. There was no significant difference of in-hospital mortality rate between Thrombolysis group and Non-thrombolysis group. One small study on STEMI in a tertiary hospital of Dhaka in Bangladesh showed that mortality rate as high as 12% among the 50 STEMI patients with age >40 years [9]. We could not find any other information regarding the mortality rate after STEMI in rural Bangladesh in the literatures.
There are several factors which could explain the high in-hospital mortality rate. First, pain-to-door time was prolonged in our study. In the Sri Lanka study [8] the average time from symptoms onset to arrival was 190 min for the patients with acute coronary syndrome. In our study, the average pain-to-door time of all STEMI patients was 472 min. The average pain-to-door time of Thrombolysis group was 250 min, which might have diminished the benefit of thrombolysis on early mortality after STEMI. Second, our population had very poor coverage of emergency medical services (EMS). Even with 86.6% of STEMI patients coming from the area within 10 km of the hospital, <6% of patients had ambulance transport services, which may have caused delayed arrival to hospital. Previous studies demonstrated that the use of EMS significantly shortened pain-to-door time and door-to-thrombolysis time [[10], [11], [12]]. One study showed that the paramedic-referred PCI benefited the STEMI patients with lower in-hospital mortality rate by means of rapid and effective reperfusion [10]. A well-trained and equipped EMS can provide early diagnosis, proper referral to proper cardiac centers and aspirin on spot, which is shown to reduce mortality rate of STEMI patients who are going through thrombolysis [13]. Community awareness to shorten pain-to-door time, more efficient EMS and equipping rural hospital for STEMI management would be a cornerstone to reduce early mortality rate after STEMI in rural Bangladesh.
Third, thrombolysis was the only mean of reperfusion in our study in a very low income setting. In a previous study in Denmark, PCI appeared to be superior to thrombolysis in terms of reducing mortality rate at 30 days after STEMI, when the patients were referred to PCI capable hospital within 2 h by means of reducing reperfusion failure [14]. The study in Sri Lanka showed that only 3.8% (23/604) of patients had PCI for reperfusion after STEMI [8]. In our study, none of the STEMI patients received primary PCI for reperfusion. Only 1.83% (3/164) of patients were referred for PCI in our study.
4.2. Economic issues
One study reported that the lack of medical insurance was independently associated with increased in-hospital mortality after STEMI [15]. The patients' income lower than national median was associated with higher in-hospital mortality in the study. Not to mention medical insurance in rural Bangladesh, 54.9% (90/164) of our study patients earn <9000 taka ($106 US dollars) per month. There was no significant association with lower income and in-hospital management or mortality in our study, possibly due to the institutional financial support for lower income family (Tables 3, 5). Thrombolysis group costed 186 US dollars per patient and required the greater amount of financial subsidy (Table 2). There was no previously published data elucidating appropriate and cost-effective practice for STEMI patients who are living with very low income in Bangladesh. More comprehensive data should be collected to know how to improve the clinical outcomes in a very low resource setting by means of clinical and community level interventions.
4.3. Gender issues
Though female sex was significantly more common in Non-thrombolysis group, binary regression showed that female sex was not an independent predictor of not being thrombolysed after STEMI in our study (Tables 1, 5). A larger study may show the real association between female sex and the risk of not being thrombolysed in rural Bangladesh. It is known that women are more prone to presenting with atypical symptoms (fatigue, dyspnea, nausea, and abdominal complaints) during STEMI and more likely to have the delay in seeking medical care. Moreover, several studies showed that there were differences in terms of clinical presentation, applying evidence-based therapies and clinical outcomes according to gender [[16], [17], [18]]. Understanding social barriers for female patients to seek emergent medical treatment after STEMI in a low income setting would be crucial in regard to improving clinical outcomes of female patients. Sex was not independently associated with increased in-hospital mortality in our study (Table 3), presumably due to small sample size and other confounding variables, while one study showed that the mortality rate of female patients after STEMI was two times higher than male counterparts [18]. More clinical and socioeconomic differences in female patients with STEMI should be scrutinized particularly in a low income setting in Bangladesh.
4.4. Limitations of study
First, this was a retrospective observation study in a rural hospital. Because of the small sample size, this study only partly depicts the real picture of STEMI treatment outcome in a rural community. Second, there may be other variables regarding pre-hospital conditions that were not measured specifically regarding decision-making process and reasons for the delayed arrival to the hospital. More community level information should be collected to understand the reasons of delay after STEMI. Finally, a long-term outcome could not be assessed in this hospital-based study.
5. Conclusions
This study in a rural hospital in Bangladesh showed that in-hospital mortality of STEMI patients remained high (19.51%) in spite of good adherence to therapeutic management guidelines. The need of inotropics and the use of defibrillation were independently associated with higher mortality rate. The use of ACEI was independently associated with lower in-hospital mortality. Prolonged pain-to-door time, lack of EMS may have contributed to the high prevalence of cardiogenic shock (26.22%) and increased mortality in our study. The effort to shorten pain-to-door time through community awareness and EMS on top of evidence-based management may reduce further early death after STEMI in a low income setting in Bangladesh.
Declaration of Competing Interest
The authors have no external grant for this work. We have no potential conflict of interest to declare.
Acknowledgement
Authors give thanks to Dr. Alfred Prince Singh for his valuable contribution to establish the initial database of this study.
References
- 1.World Health Organization Cardiovascular Diseases. 2017. http://www.who.int/news-room/fact-sheets/detail/cardiovascular-disease-(cvd) available at. (accessed October 2018); World Health Organization. Cardiovascular Diseases: available at www.who.int/news-room/fact-sheets/detail/cardiovascular-disease-(cvd) 2017 (accessed October 2018)
- 2.Chan MY, Du X, Eccleston D et al. Acute coronary syndrome in the Asia-Pacific region. Int. J. Cardiol. 202;861–869, (201). [DOI] [PubMed]
- 3.Chowdhury R., Alam D.S. Fakir, et al. The Bangladesh Risk of Acute Vascular Events (BRAVE) study: objectives and design. Eur. J. Epidemiol. 2015;30(7):577–587. doi: 10.1007/s10654-015-0037-2. [DOI] [PMC free article] [PubMed] [Google Scholar]; Chowdhury R, Alam DS, Fakir, et al. The Bangladesh Risk of Acute Vascular Events (BRAVE) Study: Objectives and Design. European J Epidemiology, 2015 30 (7): 577–587. [DOI] [PMC free article] [PubMed]
- 4.World Health Organization. Bangladesh; WHO statistical profile: available at www.who.int/gho/countries/bgd.pdf 2015 (accessed October 2018).
- 5.Guha S., Sethi R., Ray S. Cardiological Society of India: position statement for the management of ST elevation myocardial infarction in India. Indian Heart J. 2017;69(23):63–97. doi: 10.1016/j.ihj.2017.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]; Guha S, Sethi R, Ray S et al. Cardiological Society of India: Position Statement for the Management of ST Elevation Myocardial Infarction in India. Indian Heart Journal, 2017; 69 (23): 63–97. [DOI] [PMC free article] [PubMed]
- 6.World Health Organization Bangladesh- Noncommunicable Diseases (NCD) Country Profiles. 2014. http://www.who.int/nmh/countries/bgd_en.pdf?ua=1; World Health Organization. Bangladesh- Noncommunicable Diseases (NCD) Country Profiles, 2014, available at www.who.int/nmh/countries/bgd_en.pdf?ua=1
- 7.O'Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of patients with ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;127:e362-e425. [DOI] [PubMed]
- 8.Galappatthy P, Bataduwaarachchi VR, Ranasinghe et al. Management, characteristics and outcomes of patients with acute coronary syndrome in Sri Lanka. Heart 2018 (0):1–8. [DOI] [PubMed]
- 9.Karim M.A., Majumder A.A.S., Islam K.Q. Risk factors and in-hospital outcome of acute ST segment elevation myocardial infarction in young Bangladeshi adults. BMC Cardiovasc. Disord. 2015;15:73. doi: 10.1186/s12872-015-0069-2. [DOI] [PMC free article] [PubMed] [Google Scholar]; Karim MA, Majumder AAS,Islam KQ et al. Risk factors and in-hospital outcome of acute ST segment elevation myocardial infarction in young Bangladeshi adults. BMC Cardiovasc Disorders. 2015;15:73 [DOI] [PMC free article] [PubMed]
- 10.Le May M.R., Davies R.F., Dionne R. Comparison of early mortality of paramedic-diagnosed ST-segment elevation myocardial infarction with immediate transport to a designated primary percutaneous coronary intervention center to that of similar patients transported to the nearest hospital. Am. J. Cardiol. 2006;98:1329–1333. doi: 10.1016/j.amjcard.2006.06.019. [DOI] [PubMed] [Google Scholar]; Le May MR, Davies RF, Dionne R et al. Comparison of Early Mortality of Paramedic-Diagnosed ST-Segment Elevation Myocardial Infarction With Immediate Transport to a Designated Primary Percutaneous Coronary Intervention Center to That of Similar Patients Transported to the Nearest Hospital. Am J Cardiol 2006;98:1329-1333. [DOI] [PubMed]
- 11.Barbash I., Freimark D., Gottlieb S. Israeli Working Group on Intensive Cardiac Care, Israel Heart Society. Outcome of myocardial infarction in patients treated with aspirin is enhanced by pre-hospital administration. Cardiology. 2002;98(3):141–147. doi: 10.1159/000066324. [DOI] [PubMed] [Google Scholar]; Barbash I, Freimark D, Gottlieb S et al; Israeli working group on intensive cardiac care, Israel heart society. Outcome of myocardial infarction in patients treated with aspirin is enhanced by pre-hospital administration. Cardiology 2002;98(3) 141-7. [DOI] [PubMed]
- 12.Canto J.G., Zalenski R.J., Ornato J.P. Use of emergency medical services in acute myocardial infarction and subsequent quality of care: observations from the National Registry of Myocardial Infarction 2. Circulation. 2002;106:3018–3023. doi: 10.1161/01.cir.0000041246.20352.03. [DOI] [PubMed] [Google Scholar]; Canto JG, Zalenski RJ, Ornato JP et al. Use of emergency medical services in acute myocardial infarction and subsequent quality of care: observations from the National Registry of Myocardial Infarction 2. Circulation. 2002;106:3018-3023. [DOI] [PubMed]
- 13.D1 Freimark, Matetzky S., Leor J. Timing of aspirin administration as a determinant of survival of patients with acute myocardial infarction treated with thrombolysis. Am. J. Cardiol. 2002;89(4):381–385. doi: 10.1016/s0002-9149(01)02256-1. 15. [DOI] [PubMed] [Google Scholar]; Freimark D1, Matetzky S, Leor J et al. Timing of aspirin administration as a determinant of survival of patients with acute myocardial infarction treated with thrombolysis. Am J Cardiol 2002;15:89(4); 381-385. [DOI] [PubMed]
- 14.Andersen H.R., Nielsen T.T., Rasmussen K. A comparison of coronary angioplasty with fibrinolytic therapy in acute myocardial infarction. NEJM. 2003;349:733–742. doi: 10.1056/NEJMoa025142. [DOI] [PubMed] [Google Scholar]; Andersen HR, Nielsen TT, Rasmussen K et al. A Comparison of Coronary Angioplasty with fibrinolytic therapy in acute myocardial infarction. NEJM 2003;349;733-742. [DOI] [PubMed]
- 15.Pancholy S., Patel G., Pancholy M. Association between health insurance status and in-hospital outcomes after ST-segment elevation myocardial infarction. Am. J. Cardiol. 2017;120:1049–1054. doi: 10.1016/j.amjcard.2017.06.041. [DOI] [PubMed] [Google Scholar]; Pancholy S, Patel G, Pancholy M et al. Association Between Health Insurance Status and In-Hospital Outcomes After ST-Segment Elevation Myocardial Infarction. Am J Cardiol 2017;120:1049-1054. [DOI] [PubMed]
- 16.Bangalore S., Fonarow G.C., Peterson E. Age and gender differences in quality of care and outcomes for patients with ST-segment elevation myocardial infarction. Am. J. Med. 2012;125:1000–1009. doi: 10.1016/j.amjmed.2011.11.016. [DOI] [PubMed] [Google Scholar]; Bangalore S, Fonarow GC, Peterson E et al. Age and gender differences in quality of care and outcomes for patients with ST-segment elevation myocardial infarction. Am J Med. 2012;125:1000-1009 [DOI] [PubMed]
- 17.Hochman J.S., Tamis J.E., Tompson T.D. Sex, clinical presentation, and outcome in patients with acute coronary syndromes. Global use of strategies to open occluded coronary arteries in acute coronary syndromes iib investigators. N. Engl. J. Med. 1999;341:226–232. doi: 10.1056/NEJM199907223410402. [DOI] [PubMed] [Google Scholar]; Hochman JS, Tamis JE, Tompson TD, et al. Sex, clinical presentation, and outcome in patients with acute coronary syndromes. Global use of strategies to open occluded coronary arteries in acute coronary syndromes iib investigators. N Engl J Med. 1999;341:226-232 [DOI] [PubMed]
- 18.Juhan N., Zubairi Y.Z., Zuhdi A.S. Gender differences in mortality among ST elevation myocardial infarction patients in Malaysia from 2006 to 2013. Ann. Saudi Med. 2018;38:1–7. doi: 10.5144/0256-4947.2018.1. [DOI] [PMC free article] [PubMed] [Google Scholar]; Juhan N, Zubairi YZ, Zuhdi AS, et al. Gender differences in mortality among ST elevation myocardial infarction patients in Malaysia from 2006 to 2013. Ann Saudi Med 2018;38:1-7 [DOI] [PMC free article] [PubMed]