Abstract
An abundance of evidence suggests that the size and quality of our social relationships improves humans' physical and mental health while increasing lifespan. However most of this evidence comes from observational rather than experimental (randomised trial) evidence, leaving open the possibility that the connection between social relationships and health could be associational rather than causal. However there are examples, including the link between smoking and lung cancer, where a cause was established without experimental evidence. This was sometimes achieved by looking at the totality of evidence, using the ‘Bradford Hill Guidelines’, which considers factors including the strength of association, reversibility, and evidence of a plausible mechanism. In this paper we apply the Bradford Hill Guidelines to the link between social relationships and health. We conclude that having strong and supportive social relationships causes better health and longer life. Beyond establishing that social relationships are a causal factor for health, the method we used here can be applied to other areas where randomised trials are unethical or not feasible.
Keywords: Social relationships, Social networks, Health, Bradford Hill, Causation, Experiment, Evidence-based medicine, Randomised trial, Urban planning
Highlights
-
•
Systematic reviews of observational studies suggest that strong social relationships improve health and extend life.
-
•
Randomised trials are not feasible in this context; it is unethical to randomise people to be divorced, for example.
-
•
The lack of randomised trials leads to skepticism about whether strong social relationships cause better health.
-
•
Appealing to Bradford Hill’s Guidelines, we found that strong social relationships cause better health and longer life.
-
•
The method we used here can be applied to other areas where randomised trials are unethical or not feasible.
1. Introduction
1.1. Changing demographics and increasing loneliness
-
1.
The nature of our social relationships has recently changed. In recent years, most developed societies have experienced reduced intergenerational living, greater social mobility, delayed marriage, increased single-residence households, and increased age-related disabilities. Urbanisation has also increased: in 2009 the number of people in the world living in cities exceeded those living in rural areas for the first time in human history (United Nations, 2009), and the proportion of urban dwellers has been increasing ever since. Cities bring people in closer physical contact, which, according to Aristotle, should make people more connected (Aristotle & Jowett, 1977). Paradoxically, however, it seems that as people move from rural to urban areas they seem to become more isolated (Savikko, Routasalo, Tilvis, Strandberg, & Pitkala, 2005). Income inequality has also increased, which could present a barrier to establishing certain social relationships (Pickett & Wilkinson, 2015). The changes in social relationships seem to be associated with worse health outcomes. Urban dwellers appear to suffer from more stress and other ailments (Abbott, 2012; Pinker, 2014; Srivastava, 2009), and over the last 20 years, the number of Americans and British who report being lonely has increased dramatically (Sherwood, Kneale, & Bloomfield, 2014).
-
3.
Given these trends affecting the nature of social relationships, understanding the nature and extent of the association between social relationships and health is timely and relevant. A problem with the evidence connecting social relationships and health is that (in humans) it comes mostly from observational rather than experimental (randomised trial) evidence. This opens it up to the objection that the link is associational but not causal (Jeremy Howick, 2011b). In this paper we address this gap by analysing the link between social relationships and health using the Bradford Hill guidelines for causation. To anticipate, we conclude that strong social relationships (defined below) do in fact cause better health and longer life. Our method can be applied to other areas where randomised trial evidence is unfeasible or unethical.
1.2. A brief history of the observational evidence linking social relationships and longer life
The French sociologist Emile Durkheim made the earliest empirical mention of the link between social relationships and health that we are aware of when he observed the protective effects of social solidarity against suicide in 1897 (Durkheim, 1897). Brown, Cobb, and others took this idea up in the 1970s (G. W. Brown et al., 1975; Cobb, 1976), finding that social support was associated with better mental health. In the 1980s House et al. presented a range of prospective cohort and experimental evidence (in animals) suggesting that belonging to social groups improves health and extends life (House, Landis, & Umberson, 1988). At the same time, Berkman and Syme conducted a large cohort study showing an association between community ties and mortality (Berkman & Syme, 1979). Since then numerous studies have shown a link between social relationships and health (Alter et al., 2006; C. S.; Brown, Lloyd, & Murray, 2006; Cheng, Leung, & Chan, 2014; Cohen & Wills, 1985; Decety & Fotopoulou, 2014; Marquez et al., 2014; Martire & Franks, 2014; Martire et al., 2013; Ozbay et al., 2007; Sorkin et al., 2014), and a bestselling book has been written about it (Pinker, 2014).
In addition to prolonging life, having strong social relationships is associated with the prevention and even cure of diseases ranging from the common cold (Cohen et al., 1998) and diabetes (Sorkin et al., 2014), to some cancers (Alter et al., 2006). It also appears to improve pulmonary function (Cheng et al., 2014), osteoarthritis (Martire & Franks, 2014), hypertension (Sneed & Cohen, 2014), and a variety of physical health symptoms and conditions (Bookwala, Marshall, & Manning, 2014), while promoting positive health-related lifestyle behaviours (Marquez et al., 2014). A conceptual model for the underlying mechanisms linking social relationships and health has also been proposed (Berkman, Glass, Brissette, & Seeman, 2000). The model includes ‘upstream factors’ (such as culture), and ‘downstream factors’ (including physiological pathways) which seem to explain the connection between social relationships and health. In 2010, Holt-Lunstad et al. synthesized much of this evidence in a systematic review and meta-analysis of 148 prospective cohort studies involving 308,849 participants. They found that strong social relationships were associated with increased likelihood of survival by 50% during the average 7.5 years of follow up, even after adjusting for initial health status (Holt-Lunstad, Smith, & Layton, 2010). They concluded that “the influence of social relationships on mortality are comparable with … risk factors for mortality such as smoking and alcohol consumption and exceed the influence of other risk factors such as physical inactivity and obesity” (Holt-Lunstad et al., 2010). This strong conclusion has been supported by other researchers (Jetten, Haslam, & Haslam, 2012), and was mirrored in a more recent systematic review conducted by Shor et al., in 2013, who investigated the impact on perceived social support (but not the degree of integration in social networks or the number of social interactions intended to be supportive). Compared with the subgroup analysis within the Holt-Lunstad review investigating perceived social support, Shor et al. found a similar effect size (Shor, Roelfs, & Yogev, 2013). A more recent systematic review (70 studies, 3,407,134 participants) showed that the opposite of social support, namely social isolation, had a similar sized negative impact on health and mortality as obesity (Holt-Lunstad, Smith, Baker, Harris, & Stephenson, 2015).
1.3. The observational problem with the evidence linking social relationships and health
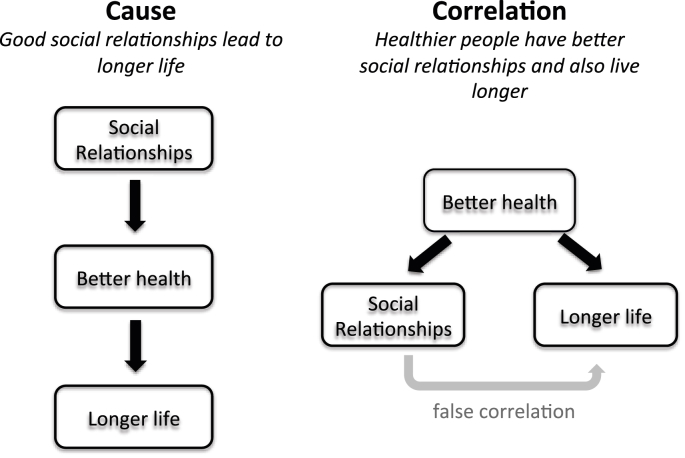
The quantity of evidence supporting the hypothesis that strong social relationships cause better health is undeniable. However most of the evidence in humans is observational and thus is prone to bias. In the absence of trials, sceptics will doubt whether strong social relationships cause longer life, or whether healthier people are likely to have strong social relationships and also live longer (see Fig. 1) (J. Howick, Glasziou, & Aronson, 2009). Sick people, may after all, have less energy and time to develop and maintain strong social relationships, while healthy energetic people may be more “attractive” as friends and social companions (Jones et al., 2001). Alternatively, the relationship may be bi-directional with health and social relationships interacting to influence each other, in virtuous circles or spirals of despair.
Fig. 1.
Causation versus correlation. On the left the cause of longer life is social relationships (via better health). On the right side the cause of longer life is better health (which also makes better social relationships possible). (Note: more complicated models where social relationships and health interact to influence each other are plausible and perhaps even likely, but are not shown in this simplified example.)
Aware of this potential problem, many of the studies within the Holt-Lunstad systematic review controlled for baseline health status, which reduces the risk of spurious correlations (2010). For example one of the studies included in their review measured and controlled for 96 initial health conditions ranging from different forms of heart disease, various respiratory conditions, electrolyte abnormalities, coeliac disease, and mental health conditions such as dementia and depression (Alter et al., 2006). When baseline health status was controlled for, the effect size seemed to become smaller in both the Holt-Lunstad et al. and Shor et al. reviews (Holt-Lunstad et al., 2010; Shor et al., 2013).
Yet controlling for initial health status does not suffice to rule out the possibility of a spurious correlation, because less conspicuous indicators of poor health may have gone undetected. For example, initial health status may not include more subtle indicators of poor health including unexplained medical symptoms, chronic pain or fatigue (Hatcher & Arroll, 2008). These symptoms might go unnoticed in a test for ‘baseline health status’ yet represent a real condition that limits people from developing and maintaining social relationships. Hence these less conspicuous initial health markers could have confounded the studies. These challenges to the evidence linking social relationships and health could explain why calls to address social relationships into health policy (Morgan, 2010; Putnam, 2000; Umberson & Montez, 2010), have rarely been implemented. Recent calls to tackle the ‘epidemic of loneliness’ are also likely to be questioned in the absence of stronger evidence for causation (Stokes-Lampard, 2018).
A randomised trial could, at least in principle, establish causation more definitively. Problems with randomised trials notwithstanding (Deaton & Cartwright, 2018), if we randomised one group of people to have strong social relationships, and they lived longer than those randomised to be lonely, we would be more certain that the social relationships were the cause of, and not merely correlated with, better health outcomes. However just as we cannot randomise people to be long-term smokers, it is nether feasible or ethical to randomise people to be married, divorced, or to (not) have friends. Moreover, such a trial faces the pragmatic challenge that social relationships are complex and dynamic. Their constituent members may interact with each other in highly unpredictable ways over short and long time frames (Kriznik, Kinmonth, Ling, & Kelly, 2018). This makes them much more difficult to create, manipulate and test than, for example, pills to reduce pain or speed bumps to reduce car accidents.
The challenge of detecting causes in the absence of randomised trials is a persistent problem for policy and decision makers and healthcare practitioners in many fields. This problem has been tackled by examining the problems with randomised trials (Deaton & Cartwright, 2018), and proposing ways to enhance observational studies such that they do a better job of ruling out confounders (Cartwright & Hardie, 2012). In this paper, we build on those challenges by appealing to the Bradford Hill ‘guidelines for causation’. The guidelines have been used to investigate whether relationships are causal or associational, especially in cases where randomised trials are unfeasible (J. Howick et al., 2009).
1.4. Bradford Hill's solution to the problem of the lack of experimental evidence
Bradford Hill was aware that we needed more than observational data when assessing the epidemiological association between smoking and lung cancer. To address this, he developed a system to help us make judgments about whether an association is causal in the absence of experimental (randomised trial) evidence (Glasziou, Chalmers, Rawlins, & McCulloch, 2007; A. B. Hill, 1965; Jeremy Howick, 2011b). In this paper we will explore whether applying the Bradford Hill Guidelines to the association between social relationships and health justifies asserting that the relationship is causal. More specifically, we propose to answer the following two questions:
-
1.
Do social relationships influence health outcomes such as disease or premature death?
-
2.
Can we be sure, of a large enough effect, to make policy and health care decisions based on the available evidence?
Before we proceed, however, we will say a few words about causality and social relationships.
1.5. Clarifying concepts: causality and the ‘strength’ of social relationships
We acknowledge the lively and interesting debate about whether establishing causation is possible at all, in philosophy starting with Hume (Hume, 2004), and in public health most notably by Glass et al. (Glass, Goodman, Hernan, & Samet, 2013). While establishing that one factor (strong social relationships) causes another (longer life) with absolute certainty may be an elusive goal, in many cases it is the wrong goal. It is driven by the dominance of individually based risk factor epidemiology (McMichael, 1999), and the general reductionist approach to policy in public health (Kriznik et al., 2018). But this approach is really a non-problem if the dynamic approach to complexities, which we advocate, is taken (Kelly, Kelly, & Russo, 2014). We suggest that if it is possible to predict whether one factor is very likely to produce an effect (Spirtes, Glymour, & Scheines, 2000), then it is acceptable (even if philosophically unsatisfactory) for present purposes, to use the term ‘cause’ to describe the phenomena. Since establishing causality beyond any doubt is elusive, the approach we suggest may the only approach as far as practical policymaking in a complex world is concerned. With that in mind, if the Bradford Hill Guidelines provide us with a reasonable basis for asserting that strong social relationships are likely to cause better health, then it is also reasonable for policymakers to research and implement the best ways to do this.
The other concept that requires clarification is that of social relationships. Studies in the Holt-Lunstad et al. review were heterogeneous in the way they defined social relationships. Yet with few exceptions, the definitions included the following components:
-
1.
the degree of integration in social networks (i.e. number of close friends, family members, and degree of participation in social groups);
-
2.
the social interactions that are intended to be supportive (i.e. the number of interactions with these groups); and
-
3.
the beliefs and perceptions of support availability held by the individual being supported (i.e., perceived social support).
The first of these represents the structural aspects of social relationships while the latter two represent the functional aspects. They are all important, and the third component shows that it is not merely the size and degree of integration within social networks, but also the more subjective feelings a person has about the support they have from the relationships they do have. Studies suggest that the three features are largely independent (Reinhardt, Boerner, & Horowitz, 2006). More importantly for present purposes, the effect of social relationships on health appears to be present independent of the definition, with the studies within the Holt-Lunstad meta-analysis showing remarkable consistency of effect direction.
Following Holt-Lunstad et al. (2010) we take social relationships to include at least one of these three factors. The way these factors were operationalised within the studies differed. For example one of the larger studies within the review measured the potential influence of structural aspects of social relationships on health (Kawachi et al., 1996) using the ‘Social Networks Index’, which measures four types of connection: marital status; sociability; church group membership; and membership in other community organisations. Responses to the index variables are then categorised into four levels of social connection ranging from low to high. Studies that measured potential influences of perceived social support on health (Brummett et al., 2005) used measures such as the Interpersonal Support Evaluation List (ISEL) (Cohen & Hoberman, 1983). The ISEL consists of 40 statements that participants are asked to reflect on, mostly relating to how they feel supported by their friends and family. Studies measuring the potential combined influence of structural and perceived support often used the Lubben Social Network Scale (Rutledge, Matthews, Lui, Stone, & Cauley, 2003), which asks study participants to rate the number of social contacts, whether the contacts are supportive, and how supported they feel by the people they contact (Lubben & Gironda, 2003). Again higher numbers characterise higher quantity and quality of social relationships. Following Holt-Lunstad et al. we will say that people have ‘strong social relationships’ when they score highly according to these individually validated scales. We discuss the potential problem with heterogeneity of these measures under ‘Limitations’, below.
2. Applying Bradford Hill Guidelines to the association between social relationships and health
The term ‘guidelines’ to describe Bradford Hill's approach is more suitable than the more commonly used ‘criteria’ (Holt & Peveler, 2009; Ioannidis, 2016; Phillips & Goodman, 2004; Staudenmayer, Binkley, Leznoff, & Phillips, 2003). This is because apart from temporality (causes must precede their effects), Bradford Hill did not regard any of the guidelines as necessary (A. B. S. Hill & Hill, 1991). Equally important, satisfying any single guideline does not suffice to establish causation; rather satisfying all or most of them can suggest that social relationships are likely to be causal rather than merely associational. Therefore rather than ‘criteria’, they are best viewed as factors to be considered when assessing whether there is evidence for causation, or ‘guidelines’ for short. With some exceptions (Ioannidis, 2016), the Guidelines are accepted as useful for establishing whether relationships between interventions and outcomes are causal. Indeed Glass et al. recommended their use for investigating causal inferences in public health (Glass et al., 2013). Bradford Hill's Guidelines have recently been updated and separated into three categories: direct (whether the effect size is large enough to rule out plausible confounders; mechanistic (whether there is an established and plausible mechanism of action); and parallel (whether the results have been replicated in similar studies) (see Table 1) (J. Howick et al., 2009). These guidelines have been elucidated in detail elsewhere (A. B. Hill, 1965), so the following is a brief description together with an analysis of whether there is evidence that the relationship between social relationships and health satisfies the guideline.
Table 1.
Evidence for whether the relationship between social relationships and health satisfies the Bradford Hill Guidelines (original and revised).
| Guidelines (revised) | Guideline (original) | Evidence (yes/no) | Evidence that the guideline has been satisfied for social relationships and health |
|---|---|---|---|
| Experiment | Yes (but in animals) | Animal experiments demonstrate a link between mother's care and mortality; one randomised trial in humans indicates reduced depression resulting from improved perception of social support. | |
| Direct – effect size greater than combined effect of confounders | Strength | Yes | The effect size is very strong – odds ratio of 1.5 |
| Direct – Appropriate temporal/special proximity | Temporality | Yes | The effect comes after the cause and occurs in as little as 1.5 years. |
| Direct – dose responsiveness and reversibility | Biological gradient | Yes | Animal experiments where subjects were deprived of contact led to increased mortality |
| Mechanistic – plausible mechanism of action | Biological plausibility | Yes | Stress buffering, main effect models are plausible explanations |
| Mechanistic – coherence | Coherence | Yes | Coheres with animal experiments and studies of foster children who were deprived of mother contact. |
| Parallel – replicability | Replicability | Yes | There were 148 studies included in Holt-Lunstad review. |
| Parallel – Similarity | Similarity | Yes | Similar studies show consistent results. |
2.1. Experiment
‘Experiment’ is one of the original guidelines that refers to whether an experimental trial such as a randomised trial was conducted. As noted in section 1.3, experimental evidence in the form of high quality randomised trials, could overcome the objection that the relationship between social relationships and health could be associational but not causal. We are aware of one randomised trial in humans suggesting a causal relationship between social support and improved health. In 2003, Berkman et al. (2003) randomised patients recovering from myocardial infarction to either receive cognitive behavioural therapy to improve perception of social support, or usual care. The group receiving therapy had better mental health outcomes, but not increased survival compared with the usual care group. The trial, however, did not randomise participants to having or not having actual social relationships; doing so may have increased the effect size but, as noted above, would have been unethical. There have also been numerous experimental (non-randomised) trials that support a causal link between social relationships and health. In the 1940s some foster children were removed from sterile environments and given temporary mother carers. As a result, their IQs rose (Spitz, 1945). Other similar studies followed (Casler, 1961; Karen, 1994), and eventually the World Health Organisation published a report that emphasised the importance of human contact and warmth for both the mental and physical health of those in foster care (J. Bowlby, 1951). Decades of research linking early strong maternal attachment and subsequent good health provides additional supportive evidence (John Bowlby, 1982).
More dramatic experiments have shown that social contacts improve health in monkeys. In the 1960s, scientists took baby monkeys from their mothers and kept them separated for periods of several weeks (Harlow, Gluck, & Suomi, 1972; Kaufman & Rosenblum, 1967, 1969; Suomi, 1997). The baby monkeys screamed, scratched, and sucked on the wires of their cages, and eventually curled up into little balls and stopped moving. Many became ill and at least one died. In some of the experiments, the baby monkeys were reunited with their mothers and became apparently happy again.
Some relevant natural experiments have been reported. In one of these, Hikichi et al. evaluated a community intervention programme introduced by the Japanese government to promote social interactions among older people (Hikichi et al., 2015). Conducting surveys before and after the introduction of the programme, researchers found that participants in the programme had 6.3% less physical or cognitive disability (identified from insurance databases). Hikichi et al. also found that greater levels of social participation protected against cognitive disability in the aftermath of the 2011 earthquake and Tsunami in Japan (Hikichi et al., 2018). While not randomised or blinded, the experimental evidence we are aware of supports the hypothesis that stronger social relationships cause better health, and vice versa.
2.2. Direct evidence
‘Direct evidence’ is evidence of a probabilistic relationship (associational or causal) between exposure and outcome. It is often in the form of observational studies, but can also come in the form of experimental studies such as randomised trials (see above). Three factors related to direct evidence must be considered when investigating whether a relationship is causal. First, the size of effect should not be attributable to plausible confounding. A confounding factor is something that might explain the difference in outcomes between two study groups but that is not the factor under test. For example initial health status is a plausible confounder in the epidemiological studies investigating the relationship between social relationships and health. Importantly: we do not need to rule out all plausible confounders. If the effect size outweighs the combined effect of plausible confounders, this provides good evidence that the relationship is causal (Jeremy Howick, 2011b). Examining the evidence linking social relationships and health, there is good direct evidence linking social relationships and health outcomes. Specifically, the size of the effect in the Holt-Lunstad studies of social relationships was large: a 50% reduction in mortality. Even if confounders influenced the result, they would have to have large effects to outweigh this. Also, known confounding factors such as measures of initial health were controlled and there was still a large effect.
Second, appropriate temporal and/or spatial proximity can strengthen the case for causality. Relationships involving factors that are temporally and spatially proximal are more easily identifiable as causal. For example, the Heimlich manoeuvre results in an immediate expulsion of an item lodged in someone's throat, so we can observe the causal action directly. This also applies to the context of this paper. If a friend dissuades someone moments before attempting suicide, we can confidently say that the friend's intervention was likely to have prevented the suicide. We find that this aspect of the guideline is satisfied, as studies within the Holt-Lunstad meta-analysis with the observed difference in mortality was observed over an average of 7.5 years, with effects often showing up in as few as 1.5 years. While the cause and effect are not always directly observable, the cause and effect are more temporally proximal than many other environmental factors.
Third, dose-responsiveness and reversibility makes it more likely that the relationship is causal. The link between social relationships and health appears to be dose-responsive and reversible. Studies within the Holt-Lunstad meta-analysis that took multiple measures of social integration (a surrogate for ‘higher dose’) had a larger effect than those measuring fewer indices of social integration. Reversibility is a form of dose-responsiveness, and the phenomena also appear to be reversible. The more recent Holt-Lunstad et al. systematic review showed that the opposite of social support, namely social isolation, had a similar sized negative impact on health and mortality as obesity (Holt-Lunstad et al., 2015). Another aspect not covered in the systematic reviews is that the wrong social relationships can shorten life (Berkman et al., 2000). To take a rather dramatic example of this, if one chooses gang members as friends, they are more likely to die (Coid et al., 2013). Homophily, meaning that less healthy people interact with each other to the exclusion of healthier individuals, is relevant here (Centola, 2011). Social groups composed of less healthy people might encourage unhealthy behaviours even if its members benefit from social contact.
2.3. Mechanistic evidence
‘Mechanistic evidence’ refers to evidence of the underlying mechanisms connecting the putative cause with the putative effect. The number of definitions of ‘mechanism’ and ‘mechanistic’ evidence exceeds the number of philosophers who are interested in the topic (Gillies, 2019), and a full review of all the similarities and differences is beyond the scope of this paper. However all of the definitions all share the view that a mechanism includes interacting parts that link an exposure with an outcome (Cartwright, 1989; Clarke, Gillies, Illari, Russo, & Williamson, 2014; Glennan, 2017; Jeremy; Howick, 2011a; Illari & Williamson, 2012; Russo & Williamson, 2007). Whereas epidemiological studies and randomised trials (often) leave what happens between the exposure and the outcome as a ‘black box’, the mechanism includes what happens between the exposure and the outcome by looking at the often complex causal relationships ‘inside the black box’. Mechanistic evidence, then, is evidence that the relationships inside the black box are actually there. There are two factors to be considered when seeking to determine whether a relationship is supported by mechanistic evidence: evidence supporting a mechanism, and not contradicting other known mechanisms of action.
Berkman et al. reviewed potential mechanisms in detail (Berkman et al., 2000), and the following two have strong evidence to support them: stress buffering and ‘main effects’. The stress-buffering hypothesis is that social relationships can reduce stress and anxiety, which results in all the benefits of stress reduction (Cohen & Wills, 1985). The biochemical pathways through which this occurs include: hindering immune system function, detrimental volume reductions in prefrontal cortices, and increased inflammation (McEwen, 2017). Additional evidence for this mechanism comes from a study of 700 Swedish men experiencing stressful life events; those with emotional support from friends were less likely to die of cardiovascular disease than those without such support (Rosengren, Orth-Gomer, Wedel, & Wilhelmsen, 1993).
The main effects model notes that friends, family, and social groups can offer actual support which could be emotional, instrumental, informational, co-participation in health enhancing behaviours, modeling of these behaviours, or some combination of these. For example, someone might drive their ill friend to a medical appointment (instrumental), inform them about new treatments (informational), or offer informal counselling (emotional support) (Cohen & Wills, 1985). Peers can also facilitate encourage healthy behaviours such as encouraging them to exercise (Laird, Fawkner, Kelly, McNamee, & Niven, 2016), or discouraging smoking (Cohen, 2004).
Other mechanisms including social capital, group efficacy, resilience, and others—see Berkman et al. (2000) - may also be operative, but they are not currently supported by very strong evidence. For example, moderation through influence on other health behaviours is plausible. Strong social relationships could promote better sleep from reduced stress, or reduced risk-taking (e.g. drink driving) due to the presence of positive social pressure or provision of alternate travel options. There are also various physiological mechanisms through which social relationships can influence health. Uchino (2006) reviewed these and found that cardiovascular, neuroendocrine, and immune function identified are likely to be the main biological systems thought to influence disease risk. He recognised that these mechanisms could be mediated through behavioural and psychological processes.
The evidence-based mechanisms explaining how strong social relationships improve health also do not contradict other known mechanisms. They cohere, for example, with what we know from animal studies and other human studies about how increasing care support for children and neonates improves their health (J. Bowlby, 1951; Lewis, Gluck, Petitto, Hensley, & Ozer, 2000; Plaut, Thal, Haynes, & Wagner, 1974; Shaw, Levitt, Wong, Kaczorowski, & McMaster University Postpartum Research, 2006).
2.4. Parallel evidence
‘Parallel evidence’ refers to related evidence, such as evidence from different yet similar populations, settings, or outcomes. There are two factors to consider when investigating whether parallel evidence supports a causal hypothesis. First, the evidence has to be replicable. Systematic reviews themselves provide evidence of replication because the reviews contain replicated studies by design. Both the Holt-Lunstad et al. (2010) and Shor et al. (2013) reviews included numerous replicated studies that pointed in the same direction. None of the 148 studies within the 2010 Holt-Lunstad review revealed a statistically significant effect in the negative direction. Three studies (2% of the total number) showed a (non-statistically significant) negative effect. This is fewer than we would expect due to chance, based on a 5% significance level. However some studies may have gone unpublished, and both the Holt-Lunstad et al. (2010) and Shor et al. (2013) reviews conducted statistical tests to investigate the possibility of publication bias. They found little evidence that it was likely to affect the results (Shor et al., 2013). Also, while there was some overlap between the Holt-Lunstad et al. (2010) and Shor et al. (2013) reviews, the latter meta-analysis can also be viewed as evidence of replication of the former.
Second, if similar evidence (in terms of populations, interventions, and outcomes) all yield similar results, the causal relationship is taken to be more robust. The studies within the 2010 Holt-Lunstad meta-analysis conducted in a range of ages (ranging from 30 to 85), and outcome measures. They also came from 16 different countries (Australia, Canada, China, Denmark, Finland, France, Israel, Italy, Japan, the Netherlands, Norway, Spain, Sweden, Taiwan, the United Kingdom, and the United States). Holt-Lunstad et al. did numerous subgroup analyses and found that the benefits of social relationships were maintained whether the study measured structural or functional aspects of social relationships. Saliently, the Shor et al. review found no statistically significant difference between geographical regions (Shor et al., 2013). The fact that strong social relationships seem to produce improved health across a range of contexts strengthens the causal hypothesis.
2.5. Summary
Bradford Hill states that if these Guidelines are all satisfied, then we have good reason to assert that a relationship is causal and not spurious. We have discussed evidence that all the Bradford Hill Guidelines are satisfied in the case of the link between social relationships and health.
3. Limitations
Our analysis has some limitations. For one, the term ‘social relationship’ is a synthesized construct that will be relative to specific contexts that change over time. When implementing this evidence, it is likely to be important to take the different contexts into account. For example, Protestant fishermen from a village in Northern Finland could have different views about what counts as strong social relationships compared with Hindu religious leaders living in a bustling Indian city. Hence to operationalise the evidence and put it into practice would require additional cross-cultural research and investigations.
In addition, as noted above, the studies linking social relationships and health are heterogeneous in numerous ways, ranging from the way social relationships are measured to the outcomes reported. This heterogeneity is an important limitation when it comes to implementing the research (where it will be necessary to specify all relevant variables carefully). At the same time, we do not believe it detracts from our conclusion that social relationships cause better health. On the contrary, the positive direction of the results in spite of the heterogeneity is evidence of a robust phenomena (see section 2.4).
Next, we have taken the Bradford Hill Guidelines as given without critically appraising them, and some have criticized the guidelines for being difficult to interpret and apply (Ioannidis, 2016). While critically appraising the Bradford Hill Guidelines is valuable, it is beyond the scope of this paper to do so. And in defence of their use, the Guidelines are widely recognised as being both useful and influential (Chalmers, 2003; Doll, 1992; Hardy & Magnello, 2002; Horton, 2000; Phillips & Goodman, 2004; Wilkinson, 1997) and seen to reflect pragmatic or ‘common sense’ philosophical principles (Worrall, 2011).
Another potential problem is that the Bradford Hill Guidelines were designed for clinical settings. Whereas medical interventions such as pills (or giving up smoking) have relatively simple (constrained, in vivo, biological) mechanisms, the pathway linking social relationships to health is one that is more heavily mediated, confounded, iterative and full of feedback loops (Berkman et al., 2000). Social relationships are by definition, relational phenomena, and need to be conceptualised dynamically. This potential objection points to the need to describe social relationships adequately and in a way they can be operationalised, and to avoid the mistake of trying to reduce them entirely to facts about individuals. It also demands that social relationships be adequately conceptualised by policymakers who wish to implement our findings (see below). However we do not see why the complexity of the association between social relationships should preclude them from being analysed using the Bradford Hill Guidelines. In fact, we believe that, on the contrary, Bradford Hill was aware of complexity, and they are perhaps better than simpler tools (such as randomised trial) for investigating causality in more complex domains. In fact, Bradford Hill himself considered many complex problems such as infant mortality, and life expectancy that are far from simple, and was well aware of complexities involving human health. His solution was not to give up hunting for causes, but to investigate the determinant causal factors (A. B. S. Hill & Hill, 1991).
4. Implications for policy and research
We believe we have established, with as much certainty as is possible with these kinds of data, that strong social relationships extend life and improve health. Indeed, even if one didn't agree that we have established a causal link between social relationships and health with philosophical certainty, the relevant question for policymakers is whether our evidence for, and assertion of, causation is sufficiently strong to act. This includes considering whether we have enough evidence to suggest that not acting would be pernicious for population health. And the evidence linking social isolation with poor health outcomes suggests that it is harmful to not act. At a policy level, therefore, well-designed interventions (with prospective evaluation) to promote social relationships are now warranted.
For example, within the context of growing urban environments there is emerging consensus that the health of a city can be promoted by: easily accessible public spaces—preferably green spaces so people can congregate (Toppi et al., 2016); affordable transport so people can access the social groups that can benefit their health; pedestrian and cycle friendly cities seem especially beneficial because they involve more contact with others (Marmot, 2010; Montgomery, 2013; World Health Organization, 2007); sufficient proximity to work (to avoid long commutes which detracts from important family/social time); and access to a wide variety of experiences and resources that provide a variety of opportunities for contact, interaction, and communication (World Health Organization, 2017). Close proximity to transport and opportunities for social integration is especially important in the context of an ageing population who walk more slowly and are generally less mobile (Recalcati, 2015). The link between increased social media use and mental health outcomes provides another reason to promote strong social relationships (Hussain & Griffiths, 2018).
At the same time, open questions remain about how to optimise interventions designed to strengthen social relationships and therefore health. More research is required in order to act in an evidence-based way. The following are a list of desiderata that should be considered for future research and policy implementation.
-
1.
Interventions attempting to improve social relationships should be monitored carefully to ensure the health benefits are achieved. The monitoring should also include careful analysis of mediators and moderators to understand mechanisms and further optimise interventions.
-
2.
Policy recommendations should include input from relevant experts (such as urban planners). Box 1, Box 2 contain case studies of how social relationships can impact on the health of individuals and groups that can be used as paradigmatic for policy makers wishing to intervene to encourage strong social relationships.
-
3.
Research and policies need to consider the complexity of social relationships and the structures upon which many of them are based. This challenge reflects the very nature of social life itself, which only appears overly complex if we naively try to apply the methods of randomised trials to things that should not be reduced to simple linear interactions between variables. A protection against an oversimplified approach is participatory governance of urban areas that includes input from many citizens (World Health Organization, 2007). Another aspect of this complexity concerns homophily—the similarity of social contacts.
-
4.
Solutions focused on individuals (whether behavioural or pharmacological) in the name of experimental purity, must be avoided. Social relationships are complex and may resist analyses that focus on simplistic relationships between an independent and a dependent variable. As social creatures, human conduct involves relations with other humans (even if those humans are not present and exist only in the imagination or some virtual reality). Humans do things in co-operative relationships with one another, including providing warm and supportive contact and acting in aggressive and hostile ways to other people. We have to conceptualise social support and its opposite, in terms of interactions between both individual acting and thinking humans and the communities in which they are embedded (Whitehead et al., 2016).
Box 1. Case study: Case study – how social relationships influences health of individuals.
Mr and Mrs Smith live on the same street as Mr and Mrs Jones. Mr and Mrs Smith have a strong social network, but Mr and Mrs Jones do not. They are similar in many of the other demographic ways that traditionally influence health.
When Mrs Smith lost her job, a close friend was able to provide emotional support and counselling that reduced stress and impact on sleep. Mrs Jones did not have this support when she lost her job.
When Mr Smith was unwell, wider family members were able to provide practical support by driving him to health care appointments on the edge of town. This increased access to healthcare services and reduced the financial and time burden of travelling by bus that Mr Jones experienced when he became unwell.
The Smiths and the Jones work for the same company. Mr and Mrs Smith share child care responsibilities with their neighbours including travel to and from school. This means they can both work part time. Mr and Mrs Jones must choose between paying for childcare or one of them taking a career break. The financial implications are clear.
When Mr and Mrs Smith wanted to quit smoking/go on a diet/exercise more they had access to friends who were willing to help. When they discovered asbestos in their garage, a friend recommended a builder who could remove this at a discount. When friends at the local social club discovered their own parents had high blood pressure Mr and Mrs Smith were motivated to speak to their GP and are now on a medication for this. They do not often suffer from feelings of loneliness or isolation.
As isolated events, these incidents may not have manifested as detectable long-term health outcomes. But cumulatively they build very different environments in which to exist. The health and life expectancy of the Smiths and Jones are likely to be different.
For the Jones' to reap the social network benefits of the Smiths, they could (re)connect with family and friends on a regular basis, and join a group that they attend regularly. At least one randomised trial (Berkman et al., 2003) and a systematic review provided evidence that the Smith and Jones case can be generalised (Strom & Egede, 2012).
Alt-text: Box 1
Box 2. Case study – how social and economic policies which break social relationships are bad for health.
Many social bonds were broken when mass privatisation was introduced in most post-communist European countries. A longitudinal study investigated factors associated with mortality in working-age men (15–59 years) in post-communist countries of Europe and the former Soviet Union between 1989 and 2002 during mass privatisation (Stuckler, King, & McKee, 2009). They controlled for price and trade liberalisation, income change, initial country conditions, structural predispositions to higher mortality, and other potential confounders. They found that short-term adult male mortality rates rose 12.8% (95% CI 7.9–17.7; p < 0.0001). They also found that each 1% increase in the percentage of population who were members of at least one social organisation decreased the association of privatisation with mortality by 0.27%; when more than 45% of a population was a member of at least one social organisation, privatisation was no longer significantly associated with increased mortality rates (3.4% [95% CI -5.4 to 12.3]; p = 0.44). This suggests that policies that are disruptive to social networks, should not be introduced without compensating for them.
Alt-text: Box 2
Finally, we believe that our analysis has implications for future investigations of potential causal relationships that resist analysis from randomised trials. The abovementioned critique of simple linear and reductionist methods to human life has been around a long time (Blumer, 1972; Lazarsfeld, 1966). But that makes it no less pertinent. Here we have argued that it is not the method of trials or experimentation that is wrong, but that using the Bradford Hill guidelines can be helpful for establishing causation in the absence of randomised trials to cases that resist, for pragmatic, ethical, or other reasons, from being analysed using randomised trials.
5. Conclusions
Applying the Bradford Hill Guidelines suggests that strong social relationships cause better health and longer life. Individuals, communities, and urban planners should work together to find measurable ways for improving social relationships and evaluate these carefully. Moreover, the methods we have used in this paper might also be applied to other areas where there is a wealth of strong non-experimental evidence yet where randomised trials cannot be conducted.
Ethics statement
This paper did not involve research with human or animal subjects so ethical approval was required.
Acknowledgement
MK was supported by a grant from the Arts and Humanities Research Council (Grant number AH/M005917/1) (‘Evaluating Evidence in Medicine’). None of the other authors have any financial or personal relationships that could have biased this work.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2019.100402.
Contributor Information
Jeremy Howick, Email: jeremy.howick@phc.ox.ac.uk.
Paul Kelly, Email: p.kelly@ed.ac.uk.
Mike Kelly, Email: mk744@medschl.cam.ac.uk.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Abbott A. Stress and the city: Urban decay. Nature. 2012;490:162–164. doi: 10.1038/490162a. [DOI] [PubMed] [Google Scholar]
- Alter D.A., Chong A., Austin P.C., Mustard C., Iron K., Williams J.I. Socioeconomic status and mortality after acute myocardial infarction. Annals of Internal Medicine. 2006;144:82–93. doi: 10.7326/0003-4819-144-2-200601170-00005. [DOI] [PubMed] [Google Scholar]
- Aristotle, Jowett B. Franklin Library; Pa: 1977. Politics. Franklin center. [Google Scholar]
- Berkman L.F., Blumenthal J., Burg M., Carney R.M., Catellier D., Cowan M.J. Effects of treating depression and low perceived social support on clinical events after myocardial infarction: The enhancing recovery in coronary heart disease patients (ENRICHED) randomized trial. Journal of the American Medical Association. 2003;289:3106–3116. doi: 10.1001/jama.289.23.3106. [DOI] [PubMed] [Google Scholar]
- Berkman L.F., Glass T., Brissette I., Seeman T.E. From social integration to health: Durkheim in the new millennium. Social Science & Medicine. 2000;51:843–857. doi: 10.1016/s0277-9536(00)00065-4. [DOI] [PubMed] [Google Scholar]
- Berkman L.F., Syme S.L. Social networks, host resistance, and mortality: A nine-year follow-up study of Alameda county residents. American Journal of Epidemiology. 1979;109:186–204. doi: 10.1093/oxfordjournals.aje.a112674. [DOI] [PubMed] [Google Scholar]
- Blumer H. Sociological analysis and the variable. In: Lazarsfeld P.F., Pasanella A.K., Rosenberg M., editors. Continuities in the language of social research. The Free P; New York: 1972. [Google Scholar]
- Bookwala J., Marshall K.I., Manning S.W. Who needs a friend? Marital status transitions and physical health outcomes in later life. Health Psychology. 2014;33:505–515. doi: 10.1037/hea0000049. [DOI] [PubMed] [Google Scholar]
- Bowlby J. Maternal care and mental health. Bulletin of the World Health Organization. 1951;3 355–533. [PMC free article] [PubMed] [Google Scholar]
- Bowlby J. Hogarth; London: 1982. Attachment and loss. [Google Scholar]
- Brown C.S., Lloyd S., Murray S.A. Using consecutive Rapid Participatory Appraisal studies to assess, facilitate and evaluate health and social change in community settings. BMC Public Health. 2006;6:68. doi: 10.1186/1471-2458-6-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown G.W., Ni Bhrolchain M., Harris T. Social-class and psychiatric disturbance among women in an urban population. Sociology-the Journal of the British Sociological Association. 1975;9:225–254. [Google Scholar]
- Brummett B.H., Mark D.B., Siegler I.C., Williams R.B., Babyak M.A., Clapp-Channing N.E. Perceived social support as a predictor of mortality in coronary patients: Effects of smoking, sedentary behavior, and depressive symptoms. Psychosomatic Medicine. 2005;67:40–45. doi: 10.1097/01.psy.0000149257.74854.b7. [DOI] [PubMed] [Google Scholar]
- Cartwright N. Clarendon; Oxford: 1989. Nature's capacities and their measurement. [Google Scholar]
- Cartwright N., Hardie J. Oxford University Press; New York: 2012. Evidence-based policy: A practical guide to doing it better. Oxford. [Google Scholar]
- Casler L. Maternal deprivation: A critical review of the literature. Monographs of the Society for Research in Child Development. 1961;26(2):1–64. [PubMed] [Google Scholar]
- Centola D. An experimental study of homophily in the adoption of health behavior. Science. 2011;334:1269–1272. doi: 10.1126/science.1207055. [DOI] [PubMed] [Google Scholar]
- Chalmers I. Fisher and Bradford Hill: Theory and pragmatism? International Journal of Epidemiology. 2003;32:922–924. doi: 10.1093/ije/dyg295. discussion 945–928. [DOI] [PubMed] [Google Scholar]
- Cheng S.T., Leung E.M., Chan T.W. Physical and social activities mediate the associations between social network types and ventilatory function in Chinese older adults. Health Psychology. 2014;33:524–534. doi: 10.1037/hea0000026. [DOI] [PubMed] [Google Scholar]
- Clarke B., Gillies D., Illari P., Russo F., Williamson J. Mechanisms and the evidence hierarchy. Topoi. 2014;33:339–360. [Google Scholar]
- Cobb S. Social support as a moderator of life stress. Psychosomatic Medicine. 1976;38:300–314. doi: 10.1097/00006842-197609000-00003. [DOI] [PubMed] [Google Scholar]
- Cohen S. Social relationships and health. American Psychologist. 2004;59:676–684. doi: 10.1037/0003-066X.59.8.676. [DOI] [PubMed] [Google Scholar]
- Cohen S., Frank E., Doyle W.J., Skoner D.P., Rabin B.S., Gwaltney J.M., Jr. Types of stressors that increase susceptibility to the common cold in healthy adults. Health Psychology. 1998;17:214–223. doi: 10.1037//0278-6133.17.3.214. [DOI] [PubMed] [Google Scholar]
- Cohen S., Hoberman H.M. Positive events and social supports as buffers of life change stress. Journal of Applied Social Psychology. 1983;13:99–125. [Google Scholar]
- Cohen S., Wills T.A. Stress, social support, and the buffering hypothesis. Psychological Bulletin. 1985;98:310–357. [PubMed] [Google Scholar]
- Coid J.W., Ullrich S., Keers R., Bebbington P., Destavola B.L., Kallis C. Gang membership, violence, and psychiatric morbidity. American Journal of Psychiatry. 2013;170:985–993. doi: 10.1176/appi.ajp.2013.12091188. [DOI] [PubMed] [Google Scholar]
- Deaton A., Cartwright N. Understanding and misunderstanding randomized controlled trials. Social Science & Medicine. 2018;210:2–21. doi: 10.1016/j.socscimed.2017.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Decety J., Fotopoulou A. Why empathy has a beneficial impact on others in medicine: Unifying theories. Frontiers in Behavioral Neuroscience. 2014;8:457. doi: 10.3389/fnbeh.2014.00457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doll R. Sir Austin Bradford Hill and the progress of medical science. BMJ. 1992;305:1521–1526. doi: 10.1136/bmj.305.6868.1521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durkheim E.m. 1897. Le Suicide. E\0301tude de sociologie. Paris. [Google Scholar]
- Gillies D.a. Routledge; London: 2019. Causality, probability, and medicine. [Google Scholar]
- Glass T.A., Goodman S.N., Hernan M.A., Samet J.M. Causal inference in public health. Annual Review of Public Health. 2013;34:61–75. doi: 10.1146/annurev-publhealth-031811-124606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasziou P., Chalmers I., Rawlins M., McCulloch P. When are randomised trials unnecessary? Picking signal from noise. BMJ. 2007;334:349–351. doi: 10.1136/bmj.39070.527986.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glennan S. Oxford University Press; Oxford: 2017. The new mechanical philosophy. [Google Scholar]
- Hardy A., Magnello M.E. Statistical methods in epidemiology: Karl Pearson, ronald ross, major greenwood and Austin Bradford Hill, 1900-1945. Sozial- und Präventivmedizin. 2002;47:80–89. doi: 10.1007/BF01318387. [DOI] [PubMed] [Google Scholar]
- Harlow H.F., Gluck J.P., Suomi S.J. Generalization of behavioral data between nonhuman and human animals. American Psychologist. 1972;27:709–716. [Google Scholar]
- Hatcher S., Arroll B. Assessment and management of medically unexplained symptoms. BMJ. 2008;336:1124–1128. doi: 10.1136/bmj.39554.592014.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hikichi H., Aida J., Matsuyama Y., Tsuboya T., Kondo K., Kawachi I. Community-level social capital and cognitive decline after a natural disaster: A natural experiment from the 2011 great East Japan earthquake and Tsunami. Social Science & Medicine. 2018 Sep 28 doi: 10.1016/j.socscimed.2018.09.057. pii: S0277-9536(18)30553-7. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- Hikichi H., Kondo N., Kondo K., Aida J., Takeda T., Kawachi I. Effect of a community intervention programme promoting social interactions on functional disability prevention for older adults: Propensity score matching and instrumental variable analyses, JAGES Taketoyo study. Journal of Epidemiology & Community Health. 2015;69:905–910. doi: 10.1136/jech-2014-205345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill A.B. The environment and disease: Association or causation? Proceedings of the Royal Society of Medicine. 1965;58:295–300. [PMC free article] [PubMed] [Google Scholar]
- Hill A.B.S., Hill I.D. Edward Arnold; 1991. Bradford Hill's principles of medical statistics. [Google Scholar]
- Holt-Lunstad J., Smith T.B., Baker M., Harris T., Stephenson D. Loneliness and social isolation as risk factors for mortality: A meta-analytic review. Perspectives on Psychological Science. 2015;10:227–237. doi: 10.1177/1745691614568352. [DOI] [PubMed] [Google Scholar]
- Holt-Lunstad J., Smith T.B., Layton J.B. Social relationships and mortality risk: A meta-analytic review. PLoS Medicine. 2010;7:e1000316. doi: 10.1371/journal.pmed.1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt R.I., Peveler R.C. Antipsychotic drugs and diabetes-an application of the Austin Bradford Hill criteria. Diabetologia. 2009 Jul;11(7):665–679. doi: 10.1007/s00125-006-0279-3. Epub 2009 May 19. [DOI] [PubMed] [Google Scholar]
- Horton R. Common sense and figures: The rhetoric of validity in medicine (Bradford Hill memorial lecture 1999) Statistics in Medicine. 2000;19:3149–3164. doi: 10.1002/1097-0258(20001215)19:23<3149::aid-sim617>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- House J.S., Landis K.R., Umberson D. Social relationships and health. Science. 1988;241:540–545. doi: 10.1126/science.3399889. [DOI] [PubMed] [Google Scholar]
- Howick J. Exposing the vanities – and a qualified defence – of mechanistic evidence in clinical decision-making. Phillosophy of Science. 2011;78:926–940. [Google Scholar]
- Howick J. Wiley-Blackwell; Oxford: 2011. The philosophy of evidence-based medicine. [Google Scholar]
- Howick J., Glasziou P., Aronson J.K. The evolution of evidence hierarchies: What can Bradford hill's 'guidelines for causation' contribute? Journal of the Royal Society of Medicine. 2009;102:186–194. doi: 10.1258/jrsm.2009.090020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hume D. Dover Publications; Mineola, N.Y.: 2004. An enquiry concerning human understanding. Newton Abbot: David & Charles. [Google Scholar]
- Hussain Z., Griffiths M.D. Problematic social networking site use and comorbid psychiatric disorders: A systematic review of recent large-scale studies. Frontiers in Psychiatry. 2018;9:686. doi: 10.3389/fpsyt.2018.00686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Illari P.M., Williamson J. What is a mechanism? Thinking about mechanisms across the sciences. European Journal for Philosophy of Science. 2012;2:119–135. [Google Scholar]
- Ioannidis J.P. Exposure-wide epidemiology: Revisiting Bradford Hill. Statistics in Medicine. 20 May 2016;35(11):1749–1762. doi: 10.1002/sim.6825. [DOI] [PubMed] [Google Scholar]
- Jetten J., Haslam C., Haslam S.A. Psychology Press; Hove: 2012. The social cure : Identity, health and well-being. [Google Scholar]
- Jones B.C., Little A.C., Penton-Voak I.S., Tiddeman B.P., Burt D.M., Perrett D.I. Facial symmetry and judgements of apparent health: Support for a “good genes” explanation of the attractiveness–symmetry relationship. Evolution and Human Behavior. 2001;22:417–429. [Google Scholar]
- Karen R. Warner; New York: 1994. Becoming attached : Unfolding the mystery of the infant-mother bond and its impact on later life. [Google Scholar]
- Kaufman I.C., Rosenblum L.A. The reaction to separation in infant monkeys: Anaclitic depression and conservation-withdrawal. Psychosomatic Medicine. 1967;29:648–675. doi: 10.1097/00006842-196711000-00010. [DOI] [PubMed] [Google Scholar]
- Kaufman I.C., Rosenblum L.A. Effects of separation from mother on the emotional behavior of infant monkeys. Annals of the New York Academy of Sciences. 1969;159:681–695. doi: 10.1111/j.1749-6632.1969.tb12971.x. [DOI] [PubMed] [Google Scholar]
- Kawachi I., Colditz G.A., Ascherio A., Rimm E.B., Giovannucci E., Stampfer M.J. A prospective study of social networks in relation to total mortality and cardiovascular disease in men in the USA. Journal of Epidemiology & Community Health. 1996;50:245–251. doi: 10.1136/jech.50.3.245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly M.P., Kelly R., Russo F. The integration of social, behavioural and biological mechanisms in models of pathogenesis. Perspectives in Biology and Medicine. 2014;57:308–328. doi: 10.1353/pbm.2014.0026. [DOI] [PubMed] [Google Scholar]
- Kriznik N.M., Kinmonth A.L., Ling T., Kelly M.P. Moving beyond individual choice in policies to reduce health inequalities: The integration of dynamic with individual explanations. Journal of Public Health Dentistry. 2018;40:764–775. doi: 10.1093/pubmed/fdy045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laird Y., Fawkner S., Kelly P., McNamee L., Niven A. The role of social support on physical activity behaviour in adolescent girls: A systematic review and meta-analysis. International Journal of Behavioral Nutrition and Physical Activity. 2016;13:79. doi: 10.1186/s12966-016-0405-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarsfeld P.F. Concept formation and measurement in the behavioural sciences: Some historical observations. In: Renzo D., editor. Concepts, theory, and explanation in the behavioral sciences : Symposium : Papers. Random House; New York: 1966. [Google Scholar]
- Lewis M.H., Gluck J.P., Petitto J.M., Hensley L.L., Ozer H. Early social deprivation in nonhuman primates: Long-term effects on survival and cell-mediated immunity. Biological Psychiatry. 2000;47:119–126. doi: 10.1016/s0006-3223(99)00238-3. [DOI] [PubMed] [Google Scholar]
- Lubben J., Gironda M. Centrality of social ties to the health and well-being of older adults. In: Harootyan B.B.L., editor. Social work and health care in an aging society. Springer Publishing Company; New York: 2003. [Google Scholar]
- Marmot M. 2010. Fair society, healthy lives: The Marmot review. [London]: Marmot Review. [Google Scholar]
- Marquez B., Elder J.P., Arredondo E.M., Madanat H., Ji M., Ayala G.X. Social network characteristics associated with health promoting behaviors among Latinos. Health Psychology. 2014;33:544–553. doi: 10.1037/hea0000092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martire L.M., Franks M.M. The role of social networks in adult health: Introduction to the special issue. Health Psychology. 2014;33:501–504. doi: 10.1037/hea0000103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martire L.M., Stephens M.A., Mogle J., Schulz R., Brach J., Keefe F.J. Daily spousal influence on physical activity in knee osteoarthritis. Annals of Behavioral Medicine. 2013;45:213–223. doi: 10.1007/s12160-012-9442-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEwen B.S. 2017. Neurobiological and systemic effects of chronic stress. Chronic stress. (Thousand Oaks), 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMichael A.J. Prisoners of the proximate: Loosening the constraints on epidemiology in an age of change. American Journal of Epidemiology. 1999;149:887–897. doi: 10.1093/oxfordjournals.aje.a009732. [DOI] [PubMed] [Google Scholar]
- Montgomery C.a. Random House; London: 2013. Happy city: Transforming our lives through urban design. [Google Scholar]
- Morgan A. Social capital as a health asset for young people's health and wellbeing. Journal of child and adolescent psychology. Supplément, Le. 2010;2:19–42. [Google Scholar]
- Ozbay F., Johnson D.C., Dimoulas E., Morgan C.A., Charney D., Southwick S. Social support and resilience to stress: From neurobiology to clinical practice. Psychiatry (Edgmont) 2007;4:35–40. [PMC free article] [PubMed] [Google Scholar]
- Phillips C.V., Goodman K.J. The missed lessons of sir Austin Bradford Hill. Epidemiologic Perspectives & Innovations. 2004;1:3. doi: 10.1186/1742-5573-1-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pickett K.E., Wilkinson R.G. Income inequality and health: A causal review. Social Science & Medicine. 2015;128:316–326. doi: 10.1016/j.socscimed.2014.12.031. [DOI] [PubMed] [Google Scholar]
- Pinker S. Random House; Toronto: 2014. The village effect: Why face-to-face contact matters. [Google Scholar]
- Plaut S.M., Thal A., Haynes E.E., Wagner J.E. Maternal deprivation in the rat: Prevention of mortality by nonlactating adults. Psychosomatic Medicine. 1974;36:311–320. doi: 10.1097/00006842-197407000-00005. [DOI] [PubMed] [Google Scholar]
- Putnam R.D. Simon & Schuster; New York ; London: 2000. Bowling alone : The collapse and revival of American community. [Google Scholar]
- Recalcati S. Arup. 2015. Shaping ageing cities: 10 European case studies. [Google Scholar]
- Reinhardt J., Boerner K., Horowitz A. Good to have but not to use: Differential impact of perceived and received support on well-being. Journal of Social and Personal Relationships. 2006;23:117–129. [Google Scholar]
- Rosengren A., Orth-Gomer K., Wedel H., Wilhelmsen L. Stressful life events, social support, and mortality in men born in 1933. BMJ. 1993;307:1102–1105. doi: 10.1136/bmj.307.6912.1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russo F., Williamson J. Interpreting causality in the health sciences. International Studies in the Philosophy of Science. 2007;21:1157–1170. [Google Scholar]
- Rutledge T., Matthews K., Lui L.Y., Stone K.L., Cauley J.A. Social networks and marital status predict mortality in older women: Prospective evidence from the study of osteoporotic fractures (SOF) Psychosomatic Medicine. 2003;65:688–694. doi: 10.1097/01.psy.0000041470.25130.6c. [DOI] [PubMed] [Google Scholar]
- Savikko N., Routasalo P., Tilvis R.S., Strandberg T.E., Pitkala K.H. Predictors and subjective causes of loneliness in an aged population. Archives of Gerontology and Geriatrics. 2005;41:223–233. doi: 10.1016/j.archger.2005.03.002. [DOI] [PubMed] [Google Scholar]
- Shaw E., Levitt C., Wong S., Kaczorowski J., McMaster University Postpartum Research G. Systematic review of the literature on postpartum care: Effectiveness of postpartum support to improve maternal parenting, mental health, quality of life, and physical health. Birth. 2006;33:210–220. doi: 10.1111/j.1523-536X.2006.00106.x. [DOI] [PubMed] [Google Scholar]
- Sherwood C., Kneale D., Bloomfield B. 2014. The way we are now. (Edinburgh) [Google Scholar]
- Shor E., Roelfs D.J., Yogev T. The strength of family ties: A meta-analysis and meta-regression of self-reported social support and mortality. Social Networks. 2013;35:626–638. [Google Scholar]
- Sneed R.S., Cohen S. Negative social interactions and incident hypertension among older adults. Health Psychology. 2014;33:554–565. doi: 10.1037/hea0000057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorkin D.H., Mavandadi S., Rook K.S., Biegler K.A., Kilgore D., Dow E. Dyadic collaboration in shared health behavior change: The effects of a randomized trial to test a lifestyle intervention for high-risk latinas. Health Psychology. 2014;33:566–575. doi: 10.1037/hea0000063. [DOI] [PubMed] [Google Scholar]
- Spirtes P., Glymour C.N., Scheines R. MIT Press; Cambridge, MA: 2000. Causation, prediction, and search. [Google Scholar]
- Spitz R.A. Hospitalism; an inquiry into the genesis of psychiatric conditions in early childhood. Psychoanalytic Study of the Child. 1945;1:53–74. [PubMed] [Google Scholar]
- Srivastava K. Urbanization and mental health. Industrial Psychiatry Journal. 2009;18:75–76. doi: 10.4103/0972-6748.64028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Staudenmayer H., Binkley K.E., Leznoff A., Phillips S. Idiopathic environmental intolerance: Part 1: A causation analysis applying Bradford hill's criteria to the toxicogenic theory. Toxicological Reviews. 2003;22:235–246. doi: 10.2165/00139709-200322040-00005. [DOI] [PubMed] [Google Scholar]
- Stokes-Lampard H. 2018. National campaign needed to tackle loneliness 'epidemic', says RCGP London: Royal College of General Practitioners. [Google Scholar]
- Strom J.L., Egede L.E. The impact of social support on outcomes in adult patients with type 2 diabetes: A systematic review. Current Diabetes Reports. 2012;12:769–781. doi: 10.1007/s11892-012-0317-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stuckler D., King L., McKee M. Mass privatisation and the post-communist mortality crisis: A cross-national analysis. Lancet. 2009;373:399–407. doi: 10.1016/S0140-6736(09)60005-2. [DOI] [PubMed] [Google Scholar]
- Suomi S.J. Early determinants of behaviour: Evidence from primate studies. British Medical Bulletin. 1997;53:170–184. doi: 10.1093/oxfordjournals.bmb.a011598. [DOI] [PubMed] [Google Scholar]
- Toppi J., Borghini G., Petti M., He E.J., De Giusti V., He B. Investigating cooperative behavior in ecological settings: An EEG hyperscanning study. PLoS One. 2016;11 doi: 10.1371/journal.pone.0154236. e0154236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uchino B.N. Social support and health: A review of physiological processes potentially underlying links to disease outcomes. Journal of Behavioral Medicine. 2006;29:377–387. doi: 10.1007/s10865-006-9056-5. [DOI] [PubMed] [Google Scholar]
- Umberson D., Montez J.K. Social relationships and health: A flashpoint for health policy. Journal of Health and Social Behavior. 2010;(51 Suppl):S54–S66. doi: 10.1177/0022146510383501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations . In: Urban and rural areas 2009. Affairs D.o.E.a.S., editor. 2009. http://www.unpopulation.org United Nations. [Google Scholar]
- Whitehead M., Pennington A., Orton L., Nayak S., Petticrew M., Sowden A. How could differences in 'control over destiny' lead to socio-economic inequalities in health? A synthesis of theories and pathways in the living environment. Health & Place. 2016;39:51–61. doi: 10.1016/j.healthplace.2016.02.002. [DOI] [PubMed] [Google Scholar]
- Wilkinson L. Sir Austin Bradford Hill: Medical statistics and the quantitative approach to prevention of disease. Addiction. 1997;92:657–666. [PubMed] [Google Scholar]
- World Health Organization . 2007. Global age-friendly cities: A guide. [Google Scholar]
- World Health Organization . 2017. Healthy city checklist. [Google Scholar]
- Worrall J. Causality in medicine: Getting back to the Hill top. Preventive Medicine. 2011;53:235–238. doi: 10.1016/j.ypmed.2011.08.009. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.