Abstract
Purpose
The Lanxi Cohort was established to systematically investigate the aetiology and interplay of body fat distribution and multiple factors with obesity and obesity-related non-communicable diseases in China.
Participants
The baseline investigation of the Lanxi Cohort study took place between June 2015 and August 2017 in Lanxi, Zhejiang Province, China. Permanent residents from one urban community and four rural villages were involved in this study. The baseline investigation included questionnaire survey, physical examination, dual-energy X-ray absorptiometry (DXA) scan, blood samples collection and traditional Chinese medicine (TCM) inquiry.
Findings to data
A total of 5132 participants, aged 18 to 80 years, were recruited at baseline; among them, 38.7% were men and 64.8% were from the urban area. The mean age was 53.04±12.77 years. The completion rates of physical examination, DXA scan, blood collection and TCM inquiry were 99.9%, 98.5%, 99.9% and 96.5%, respectively. The mean body mass index (BMI) was 23.42±3.20 kg/m2 with 8.1% of the study population being obese (BMI ≥28 kg/m2). The crude prevalence of hypertension, diabetes and metabolic syndrome were 34.9%, 10.0% and 30.4%, respectively.
Future plans
All participants will be monitored annually for cause-specific mortality and morbidity and hospital admission and will be followed up by in-person survey every 4 years. The baseline population is considered to expand in the future depending on the availability of funding support.
Ethics approval
This study was approved by the Ethical Committee of the School of Public Health, Zhejiang University.
Keywords: epidemiology, public health, obesity, cohort study, non-communicable disease, body composition
Strengths and limitations of this study.
The Lanxi Cohort was a comprehensive cohort study that recruited both urban and rural participants and collected extensive data at baseline.
Over 5000 participants underwent whole-body dual-energy X-ray absorptiometry scans, which was a large database of body composition in China.
The blood sample and body constitution in the traditional Chinese medicine were included in this study.
The Lanxi Cohort study has established good linkages to various health records for annual monitoring, which increased the success in cohort maintenance and long-term follow-up.
The proportion of male or young participants at baseline was lower than the national census.
Introduction
The obese population in China has been rapidly increasing. According to the WHO criteria, obesity is defined as a body mass index (BMI) of ≥30 kg/m2, and the numbers of obese men and women were 43.2 and 46.4 million in 2014, both ranked first worldwide compared with their ranks as 13th and 10th, respectively, 40 years ago.1 Using the definition of obesity specific to Chinese population as BMI of ≥28 kg/m2 proposed by Working Group on Obesity in China, the prevalence of obesity among Chinese adults was 12.0% in 2010.2 The prevalence of obesity is likely to increase along with the development of socioeconomics in China.
Obesity is a well-established risk factor for multiple non-communicable diseases (NCDs), including cardiovascular disease (CVD), diabetes, hypertension, pulmonary disease and cancer.3 4 The morbidity and mortality rates of obesity-related NCDs have placed a high burden on China. In 2012, CVD accounted for 45% of total deaths in China compared with the 31% reported in the USA.5 The prevalence of hypertension and diabetes in Chinese adults were reported to be 23.2% and 10.9%, respectively.6 7 Both of them were close to those in the developed countries.8 9 In 2010, overweight and obesity were estimated to account for 4.5% of the national health expenditure, or 90.8 billion ¥ (amounting to 13.4 billion US$) in China.10
Obesity is a multi-factorial condition, and various factors are involved in the development of obesity and obesity-related diseases.11 Since rapid economic growth and urbanisation have led to great changes in all aspects of the society in both urban and rural areas in China,12 13 the interplays between heredity, lifestyle, environment, mentality, obesity and obesity-related NCDs are complicated. Therefore, the severe epidemic of obesity and obesity-related NCDs in China has not been well addressed. Our previous studies showed that Chinese adults have higher body and central fat accumulation than white people for a given BMI, and body fat distribution rather than body fat percentage accounts for higher metabolic risk when an ethnic comparison was made between Chinese and white people.14 15 To our knowledge, the large-scaled population study focused on body fat distribution and obesity-related NCDs was inadequate in China.
Cohort study is considered a solid method to study association between disease and exposure, as it is essential for the unbiased assessment of the relevance of both heredity and environmental factors, and their interactions.16Thus, the demand for the comprehensive cohort study including both rural and urban areas focusing on body fat distribution, obesity and related risk factors in China is emerging in order to solve the predicament of obesity and obesity-related NCDs.
Therefore, the Lanxi Cohort study was designed as a community-based prospective cohort study, enrolling participants from both the urban and rural areas in China. This study aimed to investigate the aetiology and interplay of body fat mass (FM), body fat distribution, heredity, behaviours and socioeconomical and environmental changes with obesity and obesity-related NCDs. With these findings, this cohort will help to develop practical strategies (eg, lifestyle guidance, environment building, criteria making, screening method) to prevent obesity and obesity-related NCDs and promote health for larger population.
Cohort description
Selection of study site and pre-work
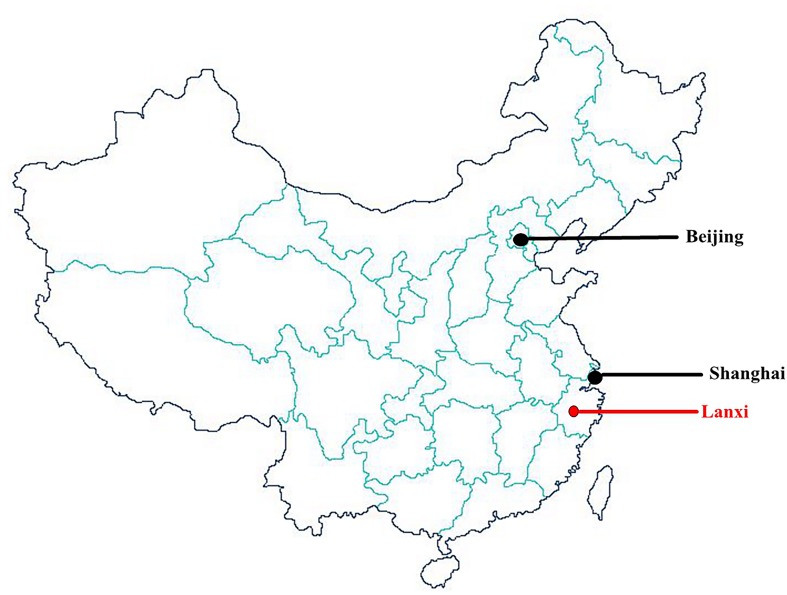
This study was conducted in Lanjiang Subdistrict, which was under the jurisdiction of Lanxi. Lanxi was a county with a population of 0.67 million located in the centre of Zhejiang Province, China, which is a transitional zone from the eastern coast to the inland mountains (figure 1). In 2016, the per capita gross domestic product of Lanxi was 8101 US$ and the urbanisation rate was 50.1%,17 both of which were close to the national average.18
Figure 1.
Location of Lanxi in China.
Calculation of sample size
The following formula was used to determine the sample size: n=P×Q/(D/T)2. P was the incidence rate of obesity. According to the Working Group on Obesity in China, the prevalence of obesity among Chinese adults was 12.0%.2 Q was calculated as 1 minus P value. D was the tolerance, which was normally 10% of P value. T was the statistic for the significance test, which was 1.96 in this formula. The original sample size was 2817. Considering the imbalance among different regions nationwide and cluster sampling methodology, the original sample size was multiplied by 1.5. There was also a possibility that 20% of the baseline participant drop off in the following up, the sample size was multiplied by 1.2. Therefore, the final sample size was estimated to be 5071 participants.
Participant eligibility and recruitment
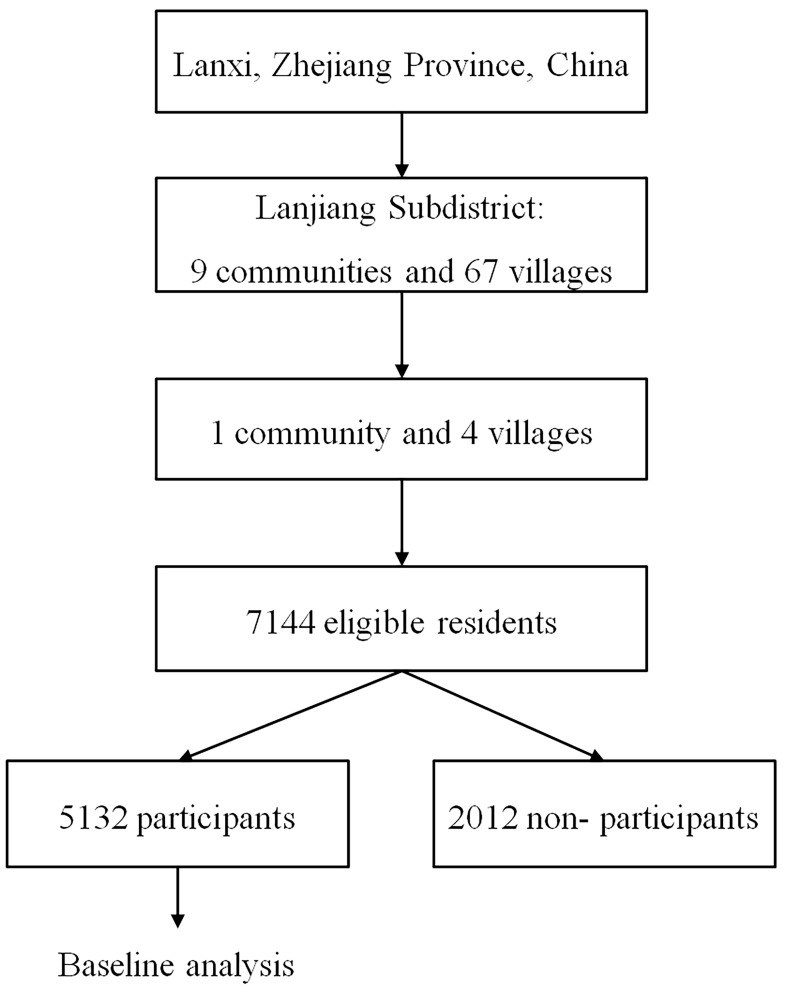
Participants’ inclusion criteria were as follows: (1) local permanent resident aged 18 to 80 years at baseline, (2) being physically and mentally capable of completing the questionnaire interviews and physical examination and (3) women who are not pregnant or breastfeeding. Permanent resident was defined as living in this district for at least 6 months per year and would stay for the next more than 5 years. Unique identification was created for each participant using their national identification cards. In the Lanjiang Subdistrict, there are nine communities and 67 villages in total. Cluster sampling was employed to recruit participants in Lanjiang Subdistrict. Binjiang community was selected as the representative cluster of the urban area, and four villages (Shuidong, Waidong, Yingjia and Hongshi) were selected for rural areas. These selected clusters had a low portion of floating population (people who did not permanently reside) and a similar demographical profile to the Lanxi average.17 Meanwhile, they were close to the Lanxi Red Cross Hospital in space. Extensive publicity campaigns were launched including disseminating banners, posters, advertisements and radio programmes. Invitation letters were delivered door-to-door, volunteers, community social workers and health workers to the 7144 eligible residents of the selected clusters (figure 2).
Figure 2.
Flowchart of participant recruitment.
The baseline study was conducted from June 2015 to August 2017 in the Lanxi Red Cross Hospital. Written informed consent forms were obtained from all participants when they enroled in the study. All the participants joined this study voluntarily and signed the consent forms.
Questionnaire
A validated electronic questionnaire was conducted face-to-face by the trained interviewers from the School of Public Health, Zhejiang University and local health nursing college. The questionnaire included general demographical information, socioeconomical status, lifestyle habits, menstrual cycle, menopause and pregnancy history (for female participants only), mental status, family history, individual medical history, sickness or injury within the last 2 weeks, hospitalisation in the last 12 months and quality of life.
Physical examination
All participants underwent an extensive physical examination, including anthropometrical, internal and surgical examinations, electrocardiography, ultrasonography, spirometry and measurements of flexibility and handgrip strength.
Anthropometrical measurements were conducted by well-trained staff, and all participants were wearing light clothing without shoes. Weight, standing height and sitting height were measured to the nearest 0.01 kg (SECA 704, Germany), 0.1 cm and 0.1 cm, respectively. Waist (WC), hip, neck, upper-arm and thigh circumferences were measured using plastic flexible tape to the nearest 0.1 cm (SECA 201, Germany). BMI and waist-to-hip ratio (WHR) were calculated. Skinfold thickness was measured at the upper arm and subscapular angle (Harpenden M402762, UK). All protocols of the anthropometrical measurements were in accordance with the State Standard of the People’s Republic of China (Standard NO.: GB/T 5703–2010).
Palpation and auscultation were conducted by registered physicians from the Lanxi Red Cross Hospital. The palpation covered the head, neck, thyroid, lymph, liver, spine, joints and movements, and auscultation covered heart and lung. Blood pressure was measured at least twice by well-trained staff using an auscultation mercury sphygmomanometer after a 10 min sitting rest. The average value of two consecutive recorded measurements with a difference of <5 mm Hg was used.
Electrocardiography was performed (Edan SE-300B, China), and the physician reviewed each cardiogram. Abdominal ultrasound test (Medison SA6000CMT, Korea) was conducted for all participants after a ≥12 hour overnight fast. Ultrasonographical evaluation of the liver and gall bladder was performed by ultrasound technicians.
Forced vital capacity was measured using a spirometer (Jianmin GMCS-II, China). Flexibility was determined by sit-and-reach. Handgrip strength was measured for the dominant hand with a hand dynamometer (Jianmin GM-II, China). Forced vital capacity, flexibility and handgrip strength were all measured twice for each participant, and the higher value was recorded.
All values and diagnoses during the physical examination were directly entered into an electronic physical examination system, which was technically built by an information technology company and managed by the research team.
Dual-energy X-ray absorptiometry
A whole-body dual-energy X-ray absorptiometry (DXA) (GE-lunar Prodigy, USA) scan was performed to measure the total and regional body FM, lean mass and bone mineral densitometry. Regions with FM and lean mass are the head, trunk, arms, legs, android and gynoid areas. The lower boundary of the android region is at the pelvis cut, and the upper boundary is 20% above the pelvis cut based on the distance between the pelvis and femoral neck cuts.19 20 Gynoid region is defined as an the upper boundary below the pelvis cut line by 1.5 times the height of the android region, and the height is equal to two times the height of the android region.19 20 The per cent of body FM (%BF) and body lean mass were calculated as body FM and body lean mass divided by total body weight. The per cent of trunk FM, android FM (%AF) and gynoid FM were calculated as trunk FM, android FM and gynoid FM divided by the total body FM, respectively. Android-to-gynoid FM ratio (AOI) was calculated as android FM divided by gynoid FM. The device was operated by well-trained staff following the standard protocol provided by the manufacturer.
Blood sample collection, processing and storage
The day before the blood sample collection, the participants were required to have a 12 hours overnight fast. A 15 mL blood sample was collected from each participant. The whole blood and serum were used to test physiological and biochemical indicators (eg, fasting blood-glucose, haemoglobin A1c (HbA1c), insulin, lipid profile), and additional biomarkers (eg, C-reactive protein). The remaining whole blood samples were processed into whole blood, plasma, white and red cells, and the remaining serum was saved 0.2 mL each tube. All samples were temporarily stored at −80°C freezer (Haier DW-86L386, China) in the Lanxi Red Cross Hospital and later transferred to Zhejiang University Zijingang Campus for long-term storage and further analysis.
Tradition Chinese Medicine
Tradition Chinese medicine (TCM) was an institutional part of Chinese healthcare system, and one of the most important and frequently used types of complementary medicine in the world.21 22 Most of the principles of TCM were derived from the traditional Chinese philosophical basis (eg, Taoism and Confucianism), and Yin and Yang were the fundamental conception of TCM.21 For TCM, the systematic body constitutional theory was recently proposed.23 A number of previous studies demonstrated that body constitution was associated with obesity, diabetes and a cluster of metabolic indicators.22–24 This might indicate that TCM is a promising tool for obesity prevention and health maintenance. In this study, each participant had a clinical diagnosis of body constitution by a registered TCM practitioner, and the diagnosis was directly entered into the electronic physical examination system. The procedures and criteria of clinical diagnosis on body constitution were in accordance with the Classification and Criterion of TCM Body Constitution proposed by China Association of Chinese Medicine in 2009.
Annual monitoring and long-term follow-up
The main outcomes during the follow-up were the incidences of death and obesity-related NCDs. Considering the practicality and efficiency, the Lanxi Cohort has two ways to follow-up the participants: annual monitoring and long-term follow-up. The information on disease occurrence and hospital admission will be collected annually through the record linked by the Lanxi Municipal Bureau of Health, and the health insurance database by the Labour and Social Security Bureau of Lanxi. The current coverage rate of health insurance in Lanxi has been >98% of the population in Lanxi,17 which provides the opportunity to follow-up disease incidences and hospital admissions efficiently as possible. The mortality information will be reported annually using the registration system in the Lanxi Red Cross Hospital, which covers the whole Lanjiang Subdistrict. Annual monitoring for both rural and urban participants will start in late 2018.
A long-term follow-up will be conducted every 4 years. Each participant will be visited for an in-person survey, which is the same as in the baseline, including questionnaire, physical examination, DXA, blood sample collection and TCM.
Statistical analysis
The baseline characteristics of the urban and rural participants were compared by Student’s t-test for continuous variables and by X2 test for categorical variables. The baseline prevalence of obesity and selected diseases were standardised for age and sex by the sixth national census in 2010. All analyses were performed using STATA V.13.0 (Stata Corporation, College Station, Texas, USA). Statistical significance was set at p<0.05 (two-tailed).
Patient and public involvement
Patients were not involved in the design or conduct of this study. The results of all the examinations and tests were integrated into a brief health report to each participant. The health report would point out abnormal result and advise the participant for the further examination.
Findings
A total of 5132 participants (71.8% of eligible residents) were enroled at baseline (figure 2), which met the requirement of the sample size. Two thousand twelve eligible residents did not join this study, and the most common reasons for non-participation were: (1) not interested in this study and (2) no time to take the examinations.
The completion rate of each component at baseline is presented in table 1. Among the 5132 participants, 98.0% (n=5027) completed the questionnaire surveys, 99.9% (n=5127) took physical examinations, 98.5% (n=5055) had whole-body DXA scans, 99.9% (n=5128) provided blood samples and 96.5% (n=4951) had TCM body constitution diagnoses.
Table 1.
Completion rate of each component at baseline in the Lanxi cohort study
| Components | Overall (n=5132) | Urban (n=3327) | Rural (n=1805) | |||
| N | % | N | % | N | % | |
| Questionnaire survey | 5027 | 98.0 | 3260 | 98.0 | 1767 | 97.90 |
| Physical examination | 5127 | 99.9 | 3320 | 99.8 | 1805 | 100.0 |
| Dual-energy X-ray absorptiometry | 5055 | 98.5 | 3263 | 98.1 | 1792 | 99.3 |
| Blood sample collection | 5128 | 99.9 | 3327 | 100.0 | 1801 | 99.8 |
| Traditional Chinese medicine | 4951 | 96.5 | 3202 | 96.2 | 1749 | 96.9 |
The baseline characteristics of participants are presented in table 2. Among the 5132 participants, 64.8% were from the urban area, 38.7% were men, 97.7% were Han and the mean age was 53.04±12.77 years. About 59.2% of the participants had attended at least middle school. The rate of married participants was 89.1%. The prevalence of current smoking and regular drinker were 15.7% and 23.5% in total participants, respectively. There were significant differences between urban and rural areas in age, education, marital status and drinking.
Table 2.
The basic characteristics of the participants at baseline in the Lanxi cohort study
| Characteristic | Overall (n=5132) | Urban (n=3327) | Rural (n=1805) | P value* | |||
| Mean or N | SD or % | Mean or N | SD or % | Mean or N | SD or % | ||
| Sex | |||||||
| Male | 1988 | 38.7 | 1260 | 37.87 | 728 | 40.3 | 0.084 |
| Female | 3144 | 61.3 | 2067 | 62.13 | 1077 | 59.7 | |
| Age (yrs) | |||||||
| 18–29 | 222 | 4.33 | 176 | 5.29 | 46 | 2.55 | <0.001 |
| 30–39 | 581 | 11.32 | 392 | 11.78 | 189 | 10.47 | |
| 40–49 | 1112 | 21.67 | 749 | 22.51 | 363 | 20.11 | |
| 50–59 | 1472 | 28.68 | 932 | 28.01 | 540 | 29.92 | |
| 60–69 | 1257 | 24.49 | 760 | 22.84 | 497 | 27.53 | |
| 70–80 | 488 | 9.51 | 318 | 9.56 | 170 | 9.42 | |
| Mean age (yrs) | 53.04 | 12.77 | 52.42 | 13.15 | 54.17 | 11.94 | <0.001 |
| Ethnics | |||||||
| Han | 5013 | 97.7 | 3250 | 97.7 | 1763 | 97.7 | 0.749 |
| Minority | 10 | 0.2 | 6 | 0.2 | 4 | 0.2 | |
| Unknown | 109 | 2.1 | 71 | 2.1 | 38 | 2.1 | |
| Education | |||||||
| Illiteracy | 922 | 17.8 | 478 | 14.4 | 444 | 24.6 | <0.001 |
| Primary school | 1061 | 20.7 | 510 | 15.3 | 551 | 30.5 | |
| Middle/high school | 2488 | 48.5 | 1783 | 53.6 | 705 | 39.1 | |
| College or above | 549 | 10.7 | 485 | 14.6 | 64 | 3.6 | |
| Unknown | 112 | 2.2 | 71 | 2.1 | 41 | 2.3 | |
| Marital status | |||||||
| Unmarried | 177 | 3.5 | 130 | 3.9 | 47 | 2.6 | <0.001 |
| Married | 4570 | 89.1 | 2913 | 87.6 | 1657 | 91.8 | |
| Ex-married | 276 | 5.4 | 216 | 6.5 | 60 | 3.3 | |
| Unknown | 109 | 2.1 | 68 | 2.0 | 41 | 2.3 | |
| Smoking | |||||||
| Never smoker | 3942 | 76.8 | 2551 | 76.7 | 1391 | 77.1 | 0.206 |
| Current smoker | 808 | 15.7 | 519 | 15.6 | 289 | 16.0 | |
| Former smoker | 269 | 5.2 | 188 | 5.7 | 81 | 4.5 | |
| Unknown | 113 | 2.2 | 69 | 2.1 | 44 | 2.4 | |
| Drinking | |||||||
| Never | 2723 | 53.1 | 1775 | 53.4 | 948 | 52.5 | <0.001 |
| <12/year | 973 | 19.0 | 581 | 17.5 | 392 | 21.7 | |
| ≥12/year | 1204 | 23.5 | 832 | 25.0 | 372 | 20.6 | |
| Former drinker | 117 | 2.3 | 68 | 2.0 | 49 | 2.7 | |
| Unknown | 115 | 2.2 | 71 | 2.1 | 44 | 2.4 | |
*Comparison between the urban and rural participants, Student’s t-test for continuous variables and χ2 test for categorical variables. yrs, years.
Table 3 shows the baseline characteristics of anthropometry and body fat distribution of the participants. In men, the mean BMI, WC, WHR and %BF were 23.76±3.15 kg/m2, 85.82±9.25 cm, 0.93±0.07 and 22.67%±6.61%, respectively. In women, the mean BMI, WC, WHR and %BF were 23.21±3.21 kg/m2, 80.80±9.30 cm, 0.89±0.07 and 32.68%±5.72%, respectively. The urban men had higher %BF and lower %AF and AOI than the rural men. It was consistent in the female participants.
Table 3.
The baseline characteristics of anthropometry and body composition in the Lanxi cohort study
| Variables* | Overall | Urban | Rural | P value† | |||
| Mean | SD | Mean | SD | Mean | SD | ||
| Male participants | |||||||
| Weight (kg) | 66.32 | 9.95 | 66.60 | 9.76 | 65.86 | 10.24 | 0.113 |
| Standing height (cm) | 166.98 | 5.71 | 167.51 | 5.58 | 166.07 | 5.82 | <0.001 |
| Sitting height (cm) | 90.16 | 3.83 | 90.87 | 3.81 | 88.96 | 3.55 | <0.001 |
| Body mass index (kg/m2) | 23.76 | 3.15 | 23.71 | 3.11 | 23.84 | 3.23 | 0.392 |
| Waist circumference (cm) | 85.82 | 9.25 | 85.99 | 9.11 | 85.52 | 9.49 | 0.277 |
| Hip circumference (cm) | 91.81 | 5.64 | 92.20 | 5.56 | 91.13 | 5.73 | <0.001 |
| Waist-to-hip ratio | 0.93 | 0.07 | 0.93 | 0.06 | 0.94 | 0.07 | 0.071 |
| Body fat mass percent (%) | 22.67 | 6.61 | 23.59 | 6.30 | 21.10 | 6.82 | <0.001 |
| Body lean mass percent (%) | 73.08 | 6.50 | 72.34 | 6.24 | 74.34 | 6.75 | <0.001 |
| Trunk fat mass percent (%) | 61.79 | 5.12 | 61.81 | 4.93 | 61.76 | 5.42 | 0.833 |
| Android fat mass percent (%) | 11.77 | 1.34 | 11.69 | 1.29 | 11.91 | 1.42 | <0.001 |
| Gynoid fat mass percent (%) | 15.82 | 2.85 | 15.84 | 2.85 | 15.79 | 2.85 | 0.706 |
| Android-to-gynoid fat mass ratio | 0.78 | 0.19 | 0.77 | 0.19 | 0.79 | 0.20 | 0.034 |
| Female participants | |||||||
| Weight (kg) | 56.43 | 8.62 | 56.50 | 8.61 | 56.29 | 8.64 | 0.523 |
| Standing height (cm) | 155.86 | 5.45 | 156.29 | 5.30 | 155.06 | 5.63 | <0.001 |
| Sitting height (cm) | 84.71 | 3.71 | 85.27 | 3.67 | 83.63 | 3.55 | <0.001 |
| Body mass index (kg/m2) | 23.21 | 3.21 | 23.11 | 3.23 | 23.39 | 3.18 | 0.024 |
| Waist circumference (cm) | 80.80 | 9.30 | 80.39 | 9.31 | 81.59 | 9.24 | 0.001 |
| Hip circumference (cm) | 91.16 | 6.02 | 91.17 | 5.82 | 91.14 | 6.39 | 0.925 |
| Waist-to-hip ratio | 0.89 | 0.07 | 0.88 | 0.07 | 0.89 | 0.06 | <0.001 |
| Body fat mass percent (%) | 32.68 | 5.72 | 33.18 | 5.62 | 31.75 | 5.79 | <0.001 |
| Body lean mass percent (%) | 62.99 | 5.70 | 62.54 | 5.65 | 63.84 | 5.68 | <0.001 |
| Trunk fat mass percent (%) | 56.48 | 4.98 | 56.27 | 4.85 | 56.88 | 5.19 | 0.001 |
| Android fat mass percent (%) | 10.19 | 1.41 | 10.10 | 1.40 | 10.35 | 1.42 | <0.001 |
| Gynoid fat mass percent (%) | 17.42 | 2.98 | 17.50 | 2.95 | 17.25 | 3.03 | 0.027 |
| Android-to-gynoid fat mass ratio | 0.61 | 0.17 | 0.60 | 0.17 | 0.63 | 0.18 | <0.001 |
*The variable sample size varied due to that participants did not complete the physical examination or dual-energy X-ray absorptiometry scans.
†Comparison between the urban and rural male/female participants, Student’s t-test for continuous variables and X2 test for categorical variables.
The metabolic characteristics of participants at baseline are presented in table 4. Significant differences were observed between urban and rural areas in almost all selected metabolic indicators except for fasting blood glucose and triglyceride. The urban participants had significant higher HbA1c, lipid indicators, blood uric acid and C-reactive protein, while the rural participants had significant higher blood pressure and insulin. The baseline prevalence of selected metabolic disease is presented in table 5. Obesity was defined as BMI ≥28 kg/m2, and central obesity was defined as WC ≥90 cm for men and WC ≥80 cm for women.2 Hypertension was defined as systolic blood pressure ≥140 mm Hg and/or diastolic blood pressure ≥90 mm Hg and/or self-reported history of hypertension.6 Diabetes was defined as fasting glucose ≥7.0 mmol/L and/or HbA1c ≥6.5% and/or self-reported history of diabetes.7 Metabolic syndrome (MS) was defined as the presence of any three of five risk factors: (1) waist circumference ≥90 cm for men and waist circumference ≥80 cm for women, (2) triglycerides ≥1.7 mmol/L or self-reported history of elevated triglycerides, (3) high-density lipoprotein <1.0 mmol/L for men and high-density lipoprotein <1.3 mmol/L for women or self-reported history of reduced high-density lipoprotein, (4) systolic blood pressure ≥130 mm Hg and/or diastolic blood pressure ≥85 mm Hg or self-reported history of hypertension and (5) fasting glucose ≥5.6 mmol/L or self-reported history of elevated glucose.25 Fatty liver and gallstone was diagnosed by ultrasonography, and coronary heart disease (CHD) was recorded by face-to-face questionnaire survey. After standardising for age and sex, the prevalence of obesity, central obesity, hypertension, diabetes, MS, fatty liver, gallstone and CHD were 9.0%, 35.8%, 25.0%, 6.8%, 23.6%, 30.9%, 8.5% and 1.2%, respectively. Compared with the rural participants, the urban participants had higher prevalences of diabetes, fatty liver, gallstone and CHD.
Table 4.
The metabolic characteristics at baseline in the Lanxi cohort study
| Variables* | Overall | Urban | Rural | P value† | |||
| Mean | SD | Mean | SD | Mean | SD | ||
| Systolic blood pressure (mm Hg) | 124.61 | 19.07 | 122.76 | 19.32 | 128.01 | 18.12 | <0.001 |
| Diastolic blood pressure (mm Hg) | 78.74 | 10.72 | 78.21 | 11.15 | 79.71 | 9.81 | <0.001 |
| Fasting blood glucose (mmol/L) | 5.24 | 1.28 | 5.23 | 1.28 | 5.26 | 1.28 | 0.423 |
| HbA1c (%) | 5.61 | 0.90 | 5.67 | 0.92 | 5.52 | 0.84 | <0.001 |
| Insulin (μU/mL) | 6.90 | 6.42 | 6.74 | 6.94 | 7.19 | 5.32 | 0.016 |
| Triglyceride (mmol/L) | 1.76 | 1.51 | 1.78 | 1.50 | 1.72 | 1.52 | 0.183 |
| Cholesterol (mmol/L) | 4.69 | 0.95 | 4.80 | 0.98 | 4.49 | 0.86 | <0.001 |
| High-density lipoprotein (mmol/L) | 1.40 | 0.35 | 1.44 | 0.34 | 1.33 | 0.36 | <0.001 |
| Low-density lipoprotein (mmol/L) | 2.52 | 0.75 | 2.57 | 0.76 | 2.41 | 0.72 | <0.001 |
| Blood uric acid (μmol/L) | 307.57 | 84.66 | 311.71 | 85.13 | 299.99 | 83.27 | <0.001 |
| C-reactive protein (mg/L) | 1.50 | 3.46 | 1.59 | 3.60 | 1.35 | 3.17 | 0.021 |
*The variable sample size varied due to those participants did not donate blood samples.
†Comparison between the urban and rural participants, Student’s t-test for continuous variables and χ2 test for categorical variables. HbA1c, haemoglobin A1c.
Table 5.
The prevalence of selected metabolic disease at baseline in the Lanxi cohort study
| Variables* | Overall | Urban | Rural | P value† | |||
| N | %‡ | N | %‡ | N | %‡ | ||
| Obese§ | 409 | 8.1/9.0 | 255 | 7.8/8.7 | 154 | 8.6/9.7 | 0.34 |
| Central obese¶ | 2265 | 44.6/35.8 | 1423 | 43.3/34.7 | 842 | 46.9/39.1 | 0.015 |
| Hypertension** | 1744 | 34.9/25.0 | 1064 | 32.9/24.1 | 680 | 38.6/26.7 | <0.001 |
| Diabetes†† | 499 | 10.0/6.8 | 357 | 11.0/7.5 | 142 | 8.1/5.4 | 0.001 |
| Metabolic syndrome‡‡ | 1502 | 30.4/23.6 | 930 | 29.2/22.8 | 572 | 32.7/25.1 | 0.009 |
| Fatty liver§§ | 1678 | 33.1/30.9 | 1204 | 36.8/34.5 | 474 | 26.4/23.2 | <0.001 |
| Gallstone§§ | 670 | 13.2/8.5 | 489 | 14.9/9.8 | 181 | 10.1/6.1 | <0.001 |
| Coronary heart disease¶¶ | 110 | 2.2/1.2 | 88 | 2.7/1.5 | 22 | 1.3/0.6 | 0.001 |
*The variable sample size varied due to that participants did not complete physical examination or questionnaire, or did not donate blood samples.
†Comparison between the urban and rural participants, Student’s t-test for continuous variables and X2 test for categorical variables.
‡Crude/adjusted for age and gender using national census data in 2010.
§Body mass index ≥28 kg/m2.
¶Waist circumference ≥90 cm for men and waist circumference ≥80 cm for women.
**Systolic blood pressure ≥140 mm Hg and/or diastolic blood pressure ≥90 mm Hg and/or self-reported history of hypertension.
††Fasting glucose ≥7.0 mmol/L and/or HbA1c ≥6.5% and/or self-reported history of diabetes.
‡‡Presence of any three of five risk factors: (1) waist circumference ≥90 cm for men and waist circumference ≥80 cm for women, (2) triglycerides ≥1.7 mmol/L or self-reported history of elevated triglycerides, (3) high-density lipoprotein <1.0 mmol/L for men and high-density lipoprotein <1.3 mmol/L for women or self-reported history of reduced high-density lipoprotein, (4) systolic blood pressure ≥130 mm Hg and/or diastolic blood pressure ≥85 mm Hg or self-reported history of hypertension and (5) fasting glucose ≥5.6 mmol/L or self-reported history of elevated glucose.
§§According to diagnosis by ultrasonography.
¶¶According to the self-reported medical history by face-to-face interview.
HbA1c, haemoglobin A1c.
Strengths and limitations
The Lanxi Cohort is a community-based prospective study, focusing on obesity and obesity-related NCDs. At baseline, a total of 5132 participants were enroled with high completion rate of each component, and an extensive range of data was collected. After standardising for age and sex using the 2010 national census data, the baseline characteristics of the participants showed lower prevalence of obesity (9.0% vs 12.0%), central obesity (35.8% vs 40.7%) and diabetes (6.8% vs 10.9%) compared with the national statistics in last decade.2 7 In addition, the prevalence of hypertension, MS and CHD were higher than those in the national level (25.0% vs 23.0% for hypertension, 23.6% vs 21.3% for MS and 1.2% vs 0.8% for CHD).6 25 Regarding fatty liver and gallstone, the data on national average was limited. However, compared with the previous studies, the prevalence of fatty liver was higher (30.9% vs 17.0%), and the prevalence of gallstone was lower (8.5% vs 11.6%).26 27The different prevalence of obesity-related NCDs between Lanxi and the national average might be attributed to the regional lifestyle and environment, which is one of our research interests in the future.
The urban-rural dual structure used in this study is one of the major strengths of the Lanxi Cohort. The increasing trend of obesity-related NCDs in the rural areas of China is pronounced.2 However, the comprehensive comparison and investigation of body fat distribution, obesity and obesity-related NCDs between urban and rural areas in China is limited. At baseline of the Lanxi Cohort study, 35.2% of the participants were from the rural areas. The presented results demonstrated significant differences in body fat distribution and metabolism based on urbanity. For example, rural participants had higher central fat accumulation (%AF and AOI) than the urban participants. It is consistent in both male and female participants. Meanwhile, there were also significant differences between urban and rural areas in socioeconomical factors (eg, education and marital status). The extensive data collected from both urban and rural areas provided the opportunity to investigate these urbanity differences and explore the underlying mechanisms.
Body fat distribution and body composition are one of the research foci of the Lanxi Cohort. Over 5000 participants underwent the whole-body DXA scan and thorough anthropometrical measurements at baseline. Thus, the Lanxi Cohort study obtained a large database of FM, lean mass, bone mineral densitometry and their distribution in China, even in Asia. Moreover, the images of the whole-body DXA scans could be used for further analysis of regional fat distribution. Additional software for DXA device was under consideration to estimate more detailed fat depot (eg, visceral fat).28 All of these collected data and planned investigation will provide insights to a better understanding of body fat distribution and body composition in Chinese population. This will also contribute to the development of Chinese-specific diagnostic criteria, screening method and prevention strategy against obesity-related NCDs.
Moreover, the Lanxi Cohort is a blood-based prospective study. The whole blood and blood components were collected at baseline and during the follow-up, which will allow us to assess the nutritional and metabolic states of the participants and provide the possibility for the future analyses of genetical and other blood-related factors.
For TCM, the body constitution refers to an individual character compatible with nature and the social environment and might indicate the susceptibility to diseases, metabolism and response to stimuli.23 Several cross-sectional studies have revealed that body constitution is associated with certain NCDs, such as obesity and diabetes.22–24 To our knowledge, however, only few longitudinal population studies were available to explore the association between body constitution and obesity-related NCDs. Integrating TCM body constitution in the Lanxi Cohort study will provide the possibility to investigate the interplays of body constitution with obesity-related NCDs and multiple modifiable factors, and also help us have a new perspective on TCM’s potential in disease prevention and health maintenance.
One limitation of this study was a low proportion of male or young participants at baseline. However, the compliance and stability are the primary considerations of a cohort study. As the Lanxi Cohort study aimed to explore the aetiology other than the epidemic of obesity and obesity-related NCDs, the representativeness was not the primary concern of participant recruitment. Meanwhile, the low mobility and good compliance of elderly population will greatly contribute to the cohort maintenance and long-term follow-up.29 Another limitation of this study was that the non-participants among the target population did not provide their socioeconomical information. Thus, there might be a possibility of selection bias at baseline. In the future plans, the number of the baseline population would be considered to expand in the future and the non-participants among the target population would be invited again which depends on the availability of funding support. The age and sex balance would be also considered in the potential baseline expansion in the future. The single racial composition of the participants might be the third limitation. Considering that 97.7% of the total participants were Han (East Asians), it should be cautious when the results were applied to other races.
In conclusion, this study has successfully established a baseline of 5132 participants and good linkages with various health record systems for annual monitoring and long-term follow-up. The extensive data collected, especially the blood sample, DXA scan and TCM body constitution at baseline and in each follow-up will be a powerful tool and unique resource in investigating the aetiology and interplay of body fat distribution, obesity and obesity-related NCDs not only in China but also in other developing or developed countries.
Acknowledgments
We acknowledge the Lanxi Red Cross Hospital and the Lanxi Municipal Bureau of Health for their full support. We express our great gratitude to all the participants in this study. We are also grateful to all the volunteers, social workers and health workers for inviting eligible participants.
Footnotes
Contributors: SZ conceived and designed the study. CW and DG analysed the data. CW and SZ drafted the manuscript. SZ, CW, SY, YR, DG, WZ, CH, LC, PG, JL, MY, FY and XZ provided comments and revised the manuscript. All authors read and approved the final manuscript.
Funding: This study was supported by the grant from the Cyrus Tang Foundation (419600-11102), with additional grants from the China Medical Board (CMB) Collaborating Program (15-216 and 12-108).
Disclaimer: The depiction of boundaries on the map(s) in this article do not imply the expression of any opinion whatsoever on the part of BMJ (or any member of its group) concerning the legal status of any country, territory, jurisdiction or area or of its authorities. The map(s) are provided without any warranty of any kind, either express or implied.
Competing interests: None declared.
Ethics approval: The ethics approval (NO: ZGL2012-12) was provided by the Ethics Committee of School of Public Health Zhejiang University.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: The data are not freely available, but we welcome any potential collaboration with other researchers. For further information, please email Shankuan Zhu at zsk@zju.edu.cn.
Collaborators: The study data are currently not freely available; however, the research team welcomes all potential collaborations with other researchers. For further information, please email the corresponding author at zsk@zju.edu.cn.
Patient consent for publication: Obtained.
References
- 1. NCD Risk Factor Collaboration (NCD-RisC). Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19·2 million participants. Lancet 2016;387:1377–96. 10.1016/S0140-6736(16)30054-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Weiwei C, Runlin G, Lisheng L, et al. Outline of the report on cardiovascular diseases in China, 2014. Eur Heart J Suppl 2016;18:F2–F11. 10.1093/eurheartj/suw030 [DOI] [PubMed] [Google Scholar]
- 3. Pi-Sunyer X. The Medical Risks of Obesity. Postgrad Med 2009;121:21–33. 10.3810/pgm.2009.11.2074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Organization WH. Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser 2000;894:1–253. [PubMed] [Google Scholar]
- 5. Organization WH. Noncommunicable diseases country profiles 2014, 2014. [Google Scholar]
- 6. Wang Z, Chen Z, Zhang L, et al. Status of hypertension in china: Results from the china hypertension survey, 2012-2015. Circulation 2018;137:2344–56. 10.1161/CIRCULATIONAHA.117.032380 [DOI] [PubMed] [Google Scholar]
- 7. Ma RCW, Rcw M. Epidemiology of diabetes and diabetic complications in China. Diabetologia 2018;61:1249–60. 10.1007/s00125-018-4557-7 [DOI] [PubMed] [Google Scholar]
- 8. NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet 2016;387:1513–30. 10.1016/S0140-6736(16)00618-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Mills KT, Bundy JD, Kelly TN, et al. Global disparities of hypertension prevalence and control: A systematic analysis of population-based studies from 90 countries. Circulation 2016;134:441–50. 10.1161/CIRCULATIONAHA.115.018912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Zhang J, Shi XM, Liang XF. [Economic costs of both overweight and obesity among Chinese urban and rural residents, in 2010]. Zhonghua Liu Xing Bing Xue Za Zhi 2013;34:598. [PubMed] [Google Scholar]
- 11. de Mutsert R, den Heijer M, Rabelink TJ, et al. The Netherlands Epidemiology of Obesity (NEO) study: study design and data collection. Eur J Epidemiol 2013;28:513–23. 10.1007/s10654-013-9801-3 [DOI] [PubMed] [Google Scholar]
- 12. Gong P, Liang S, Carlton EJ, et al. Urbanisation and health in China. Lancet 2012;379:843–52. 10.1016/S0140-6736(11)61878-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ebenstein A. The consequences of industrialization: Evidence from water pollution and digestive cancers in China. Rev Econ Stat 2012;94:186–201. 10.1162/REST_a_00150 [DOI] [Google Scholar]
- 14. He W, Zhang S, Song A, et al. Greater abdominal fat accumulation is associated with higher metabolic risk in Chinese than in white people: an ethnicity study. PLoS One 2013;8:e58688 10.1371/journal.pone.0058688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. He W, Li Q, Yang M, et al. Lower BMI cutoffs to define overweight and obesity in China. Obesity 2015;23:684–91. 10.1002/oby.20995 [DOI] [PubMed] [Google Scholar]
- 16. Chen Z, Chen J, Collins R, et al. China Kadoorie Biobank of 0.5 million people: survey methods, baseline characteristics and long-term follow-up. Int J Epidemiol 2011;40:1652–66. 10.1093/ije/dyr120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lanxi Government Network. The profile on Lanxi [Web page]. http://www.lanxi.gov.cn/ (Accessed 29 Jun 2018).
- 18. National Bureau of Statistics of the People’s Republic of China Tabulation on the 2010 population census of the People’s Republic of China [Web page]. http://www.stats.gov.cn/tjsj/pcsj/rkpc/6rp/indexch.htm (Accessed 29 Jun 2018).
- 19. Fu X, Ma X, Lu H, et al. Associations of fat mass and fat distribution with bone mineral density in pre- and postmenopausal Chinese women. Osteoporos Int 2011;22:113–9. 10.1007/s00198-010-1210-9 [DOI] [PubMed] [Google Scholar]
- 20. Samsell L, Regier M, Walton C, et al. Importance of android/gynoid fat ratio in predicting metabolic and cardiovascular disease risk in normal weight as well as overweight and obese children. J Obes 2014;2014:1–7. 10.1155/2014/846578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Tang JL, Liu BY, Ma KW, Kw M. Traditional Chinese medicine. Lancet 2008;372:1938–40. 10.1016/S0140-6736(08)61354-9 [DOI] [PubMed] [Google Scholar]
- 22. Lee CH, Li TC, Tsai CI, et al. Yang deficiency body constitution acts as a predictor of diabetic retinopathy in patients with type 2 diabetes: Taichung diabetic body constitution study. Evid Based Complement Alternat Med 2015;2015:1–8. 10.1155/2015/940898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Li M, Mo S, Lv Y, et al. A study of traditional chinese medicine body constitution associated with overweight, obesity, and underweight. Evid Based Complement Alternat Med 2017;2017:1–8. 10.1155/2017/7361896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Lee CH, Li TC, Tsai CI, et al. Association between albuminuria and different body constitution in type 2 diabetes patients: Taichung diabetic body constitution study. Evid Based Complement Alternat Med 2015;2015:1–8. 10.1155/2015/603048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Xi B, He D, Hu Y, Yh H, et al. Prevalence of metabolic syndrome and its influencing factors among the Chinese adults: the China Health and Nutrition Survey in 2009. Prev Med 2013;57:867–71. 10.1016/j.ypmed.2013.09.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Fan J-G. Epidemiology of alcoholic and nonalcoholic fatty liver disease in China. J Gastroenterol Hepatol 2013;28:11–17. 10.1111/jgh.12036 [DOI] [PubMed] [Google Scholar]
- 27. Zhu L, Aili A, Zhang C, et al. Prevalence of and risk factors for gallstones in Uighur and Han Chinese. World J Gastroenterol 2014;20:14942–9. 10.3748/wjg.v20.i40.14942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Micklesfield LK, Goedecke JH, Punyanitya M, et al. Dual-energy X-ray performs as well as clinical computed tomography for the measurement of visceral fat. Obesity 2012;20:1109–14. 10.1038/oby.2011.367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Wong MC, Jiang JY, Griffiths SM. Factors associated with antihypertensive drug compliance in 83,884 Chinese patients: a cohort study. J Epidemiol Community Health 2010;64:895–901. 10.1136/jech.2009.091603 [DOI] [PubMed] [Google Scholar]