Abstract
Congenital long QT syndrome (LQTS) has been the most investigated cardiac ion channelopathy. Although congenital LQTS remains the domain of cardiologists, cardiac electrophysiologists and specialised centres, the much more frequently acquired LQTS is the domain of physicians and other members of healthcare teams required to make therapeutic decisions. This paper reviews the electrophysiological mechanisms of acquired LQTS, its ECG characteristics, clinical presentation, and management. The paper concludes with a comprehensive review of the electrophysiological mechanisms of torsade de pointes.
Keywords: Long QT syndrome, torsade de pointes, electrophysiology
Since its initial description by Jervell and Lange-Nielsen in 1957,[1] congenital long QT syndrome (LQTS) has been the most investigated cardiac ion channelopathy. A prolonged QT interval on the surface ECG is a surrogate measure of prolonged ventricular action potential duration (APD).
Congenital as well as acquired alterations in certain cardiac ion channels can affect their currents in such a way as to increase the APD and hence the QT interval. The inhomogeneous lengthening of the APD across the ventricular wall results in dispersion of APD, i.e. dispersion of repolarisation (DR). This, together with the tendency of prolonged APD to be associated with oscillations at the plateau level, termed early afterdepolarisations (EADs), provides the substrate of ventricular tachyarrhythmia (VT) associated with LQTS, usually referred to as torsade de pointes (TdP) VT.[2]
Acquired LQTS is by far, more prevalent than congenital LQTS. The vast majority of acquired LQTS is the result of the adverse effect of drugs[3] and/or electrolyte abnormalities,[4] which, in the majority of cases, interact with the human ether-à-go-go-related gene (hERG) encoding the pore-forming subunits (Kv11.1) of the rapidly activating delayed rectifier current, IKr. However, recent reports suggest that some drugs can also increase the late sodium current, which may contribute to their proarrhythmic effect.[5]
Acquired Long QT Syndrome
ECG Characteristics of Torsade de Pointes
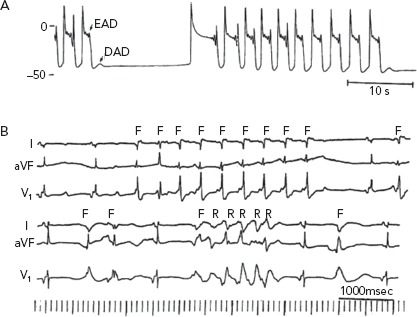
In an analysis of 150 different episodes of sustained VT obtained from 62 patients with acquired LQTS, the arrhythmia ranged in length from 3 beats (the definition of non-sustained VT) up to 117 beats (Figure 1A), with an average length of 16 ± 8 beats.[2] The cycle length (CL) of these episodes ranged from 193 to 364 ms, with an average of 279 ± 47 ms. The VT was frequently preceded by a variable period of bigeminal rhythm due to one or two premature ventricular beats coupled to the prolonged QT segment of the preceding basic beat (Figure 1A and C). This ‘short-long cardiac sequence’ is seen in both acquired and congenital LQTS, and the arrhythmogenic mechanism may be related to increased dispersion of repolarisation (DR).[6]
Figure 1: Electrocardiographic Examples of Acquired Long QT Syndrome (LQTS) and Torsade de Pointes (TdP).
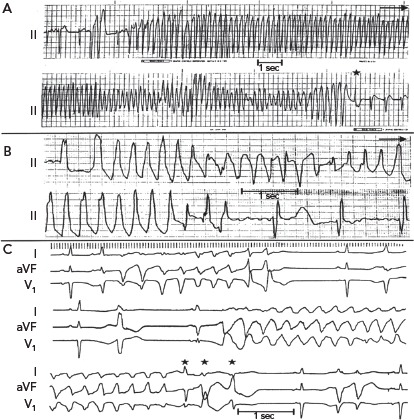
A: 23-year-old woman, human immunodeficiency virus (HIV)-positive, receiving pentamidine. The patient was admitted with severe diarrhoea and hypokalaemia. B: 62-year-old man with hypertension and chronic atrial fibrillation, receiving digoxin and hydrochlorothiazide, with a potassium level of 3.2 mEq/L. TdP tachycardia developed 12 hours after the patient received a total of four tablets of quinidine gluconate in an attempt to restore normal sinus rhythm. C: 64-year-old man receiving procainamide for suppression of very frequent ventricular premature complexes. NB: Pentamidine, quinidine and procainamide are considered drugs with high risk of drug-induced acquired QT syndrome. Their use is currently curtailed. Source: El-Sherif N, et al. 1999.2 Reproduced with permission from © Wiley Periodicals, Inc.
Following termination of an episode of fast VT, it is not uncommon to see one or more ectopic beats of variable configuration occurring at much longer CL compared to that of the VT (see beats marked by arrowheads in Figure 2). The change in QRS configuration during VT can take several forms. During a very fast VT, periodic decrease in the amplitude of the entire QRS-T complex is seen with less distinct shifts in QRS axis (Figure 1A). In VTs with slower rates, the classic twisting of the QRS axis from a predominantly positive to a predominantly negative configuration with a variable number of transitional complexes and vice versa is commonly seen as originally described by Dessertenne (Figure 1B).[7] Sometimes, a polymorphic QRS configuration is seen without any of the two previously characteristic patterns (as verified in multiple simultaneous leads, Figure 2C, middle recording). Different patterns can be seen in different VT episodes from the same patient (Figure 1C).
Figure 2: Twelve-lead ECG from a Patient with Hypokalaemia and Hypomagnesaemia.
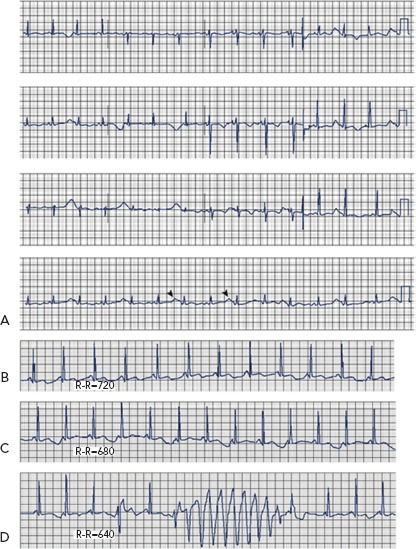
A: Marked QTU prolongation and QTU alternans (arrowheads). B–D: Representative rhythm strips from the same patient showing tachycardia-dependent QTU alternans and torsade de pointes. Source: El-Sherif N, et al. 2011.4 Reproduced with permission from © Via Medica.
QT/T Wave Alternans and Torsade de Pointes
It has long been known that tachycardia-dependent T wave alternans (TWA) occurs in patients with the congenital or acquired form of LQTS and may presage the onset of TdP (Figure 2).[2,8]
In an analysis of 1,103 LQTS patients with QTc interval >0.44 seconds from the International LQTS Registry, TWA was recorded in 30 patients.[8] The frequency of occurrence of TWA was directly proportional to the length of the QTc interval on the enrolment ECG. TWA occurred in one or more occasions during an average 4-year follow up in 21% of patients with QTc >0.60 seconds, but in <0.2% of patients with QTc <0.50 seconds. Patients with advanced forms of TWA (those with bidirectional beat-to beat changes in T wave polarity; n=21) were younger, had longer QTc values, had a higher incidence of complex VT, and were more likely to experience a cardiac event (syncope or cardiac arrest) than those with less advanced forms of TWA (those without bidirectional beat-to-beat changes in T wave polarity; n=9).
In contrast to TWA in congenital LQTS, the incidence of TWA in acquired LQTS is unknown. It has been reported in acquired LQTS due to hypokalaemia and hypomagnesemia (Figure 3)[4] as well as in association with medications that prolong the QT interval (Figure 3).[9] Patients with acquired LQTS and TWA are likely to develop TdP (Figures 2 and 3).
Figure 3: Efavirenz-associated QT Prolongation and Torsade de Pointes Arrhythmia.
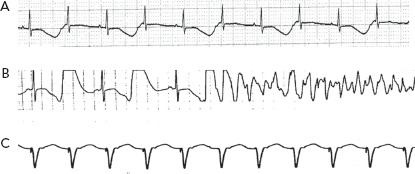
Representative ECG recordings from a 63-year old woman with HIV who developed efavirenz-related QT prolongation and torsade de pointes arrhythmia. A: Sinus rhythm at 95 bpm and QT alternans. B: Sinus bradycardia, marked QT interval prolongation and onset of a TdP arrhythmia that required cardioversion for termination. C: The arrhythmia could be suppressed by overdrive ventricular pacing at a rate of 100 bpm. QT prolongation and non-sustained TdP episodes developed when the pacing rate was lowered to <100 bpm. QT returned to normal several days after discontinuation of the long-acting efavirenz. Source: Castillo R, et al. 2002.9 Reproduced with permission from © SAGE Publications.
Although overt TWA in the ECG is not common, in recent years, digital signal processing techniques have made it possible to detect subtle degrees of TWA.[10] This suggests that the phenomenon may be more prevalent than previously recognised and may represent an important marker of vulnerability to VT. A recent report confirms this view, showing that microvolt TWA is far more prevalent in LQTS patients than previously reported and is strongly associated with TdP history.[11] Interest in TWA is attributed to the hypothesis that it reflects a greater degree of underlying DR.[12]
Aetiology of Acquired Long QT Syndrome
The vast majority of acquired LQTS is the result of adverse effects of drugs that interact with the hERG gene, and the IKr. However, although most drugs that cause TdP do so via hERG channel blockade, TdP is not necessarily a potential consequence of all drugs blocking the hERG pathway. Milberg et al.[13] compared the TdP induction ability of two hERG-blocking drugs, DL-sotalol and amiodarone. While both drugs can increase the QT interval, the former causes transmural DR and triangulation of the action potential by prolonging phase 3, and triggers both EADs and TdP. However, amiodarone does not usually cause DR, EADs, or TdP, and prolonging phase 2 results in a squared-shaped action potential. While squared-shaped action potentials are considered antiarrhythmic, triangulated action potentials are considered proarrhythmic.[14] Several authors have suggested that DR, attributed to preferential prolongation of the APD of M cells, is a preclinical marker of drug-induced proarrhythmia.[15] However, the existence, location, and clinical contribution of M cells has been a matter of debate.[16]
Recent studies have shown that some drugs designated as arrhythmogenic IKr blocker can generate arrhythmias by augmenting INa-L through the PI3K pathway.[5] For example, while acute exposure of flecainide to adult mouse cardiomyocyte that lack IKr produced no change in ion currents and action potential duration, extended exposure up to 48 hours of the drug generated up to a 15-fold increase in INa-L and resulted in arrythmogenic EADs. However, not all IKr blockers modulate INa-L, and this diversity of effects, in return, may contribute to the apparent difference in TdP frequency across culprit drugs.[5] A major implication of this data has to be that relying on an assay to assesses acute block of IKr may not provide a comprehensive assessment of a candidate drug arrhythmogenic potential.
Antidepressant and antipsychotic drugs modulate the cardiac APD by blocking a variety of cardiac ion channels.[17] Some antidepressant and antipsychotic drugs increase the risk of VT and SCD by prolonging the QT interval and inducing TdP arrhythmia. Other antidepressant and antipsychotic drugs increase arrhythmic risk by inducing a Brugada syndrome phenotype. Antipsychotic drugs generally have a higher torsadogenic potential than antidepressants. Based on recent literature, the risk of QT/QTc prolongation with newer non-SSRI antidepressants at therapeutic doses is low.[18]
Other causes of acquired LQTS include electrolyte abnormalities (hypokalaemia, hypomagnesaemia, and hypocalcaemia [Figure 3]), hypothyroidism, hypothermia, and marked bradycardia, (sinus bradycardia as in Figure 4, or atrioventricular block).[19] Any of these factors can cause acquired LQTS or contribute to the risk of drug-induced LQTS. In addition, there is recent evidence of the high prevalence of QTc interval prolongation in patients with anti-SSA/Ro antibodies, as well as autoimmune and inflammatory diseases.[20–22]
Figure 4: Correlation Between Specific Molecular Changes of Na Channel in Canine Surrogate Model of Long QT Syndrome Type 3, Electrophysiological Consequence, and Final Phenotype Presentation of Long QT Syndrome and Torsade de Pointes.
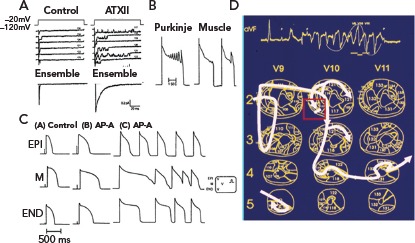
A: Cell-attached patch clamp recordings of the Na channel during control and following superfusion with sea anemone toxin ATXII. This neurotoxin faithfully reproduces the molecular changes associated with the clinical mutations of the Na channel in patients with LQT3. Sequential recordings of single Na channel current responses during depolarising steps from -120 to -20 mV from rabbit cardiomyocytes. Left panel shows control recordings and right panel shows recordings from a patch exposed to 100 nM of ATXII that resulted in long-lasting bursts consisting of repetitive long opening interrupted by brief closures. Ensemble current from this patch shows markedly slowed relaxation. B: Action potential recordings from a Purkinje fibre (PF) and a mid-myocardial (M) cell, both isolated from a 10-week-old puppy and placed in the same chamber perfused with 50 mg/l anthopleurin-A (AP-A) and stimulated at 3000 ms. The PF shows a series of early afterdepolarisations (EADs) that increased gradually in amplitude before final repolarisation. C: Simultaneous recordings from a subepicardial cell (EPI), M cell and a subendocardial cell (END) from a transmural strip isolated from the left ventricle of a 12-week-old puppy and transfused with 50 mg/l AP-A and stimulated at 4000 ms. Because of the different ionic characteristics of different myocardial fibres, AP-A resulted in marked differential prolongation of the action potential of the M cell resulting in asynchronous activation in the preparation, which is a substrate of reentrant excitation. D: Tridimensional activation maps of a 12-beat run of TdP from the in vivo canine surrogate AP-A model of LQT3 helps summarise the final electrophysiological mechanism of TdP in the LQTS. The first beat of a TdP is due to an EAD-triggered beat from the subendocardial Purkinje network that acts on the transmural dispersion of myocardial repolarisation to induce reentrant excitation in the form of circulating tridimensional wave fronts (the thick continuous line that traces the activation wave front from one beat to the next).14 The twisting QRS pattern of the classic TdP is attributed in this example to transient bifurcation of a predominantly single rotating wavefront into two separate simultaneous wave fronts rotating around the left and right ventricular cavities.15 Source: Sherif N, et al., 2015.67 Reproduced with permission from © 2015 Published by Elsevier Inc.
Several recent reports from this laboratory have provided strong evidence for a pathogenic role of autoimmune and inflammatory conditions in the development of QTc prolongation. Anti-Ro antibodies from patients with autoimmune disease were shown to inhibit IKr by directly cross-reacting with the hERG channel, likely at the pore region where homology between 52Ro antigen and hERG channel was demonstrated.[23] In addition, an animal model of autoimmune-associated QTc prolongation was established, for the first time, whereby induction of anti-SSA/Ro antibodies by immunisation resulted in QTc prolongation on the surface ECG.[23]
Conversely, inflammatory channelopathies are related to systemically or locally released inflammatory cytokines (mainly TNF-a, interleukin-1, and interleukin-6) able to directly affect the expression and/or function of several cardiac ion channels, resulting in a decrease of K+ currents (IKr, Ito, or the slow activating components of the delayed K+ current [IKs]) and/or an increase of ICaL.[24,25]
In another report,[26] we tested the hypothesis that IL-6 may cause QT prolongation by suppressing IKr. Electrophysiological and biochemical assays were used to assess the impact of IL-6 on the functional expression of IKr in HEK293 cells and adult guinea-pig ventricular myocytes. In HEK293 cells, IL-6 alone or in combination with the soluble IL-6 receptor (IL-6R), produced a significant depression of IKr peak and tail current densities. Block of IL-6R or Janus kinase (JAK) reversed the inhibitory effects of IL-6 on IKr. In adult guinea-pig ventricular myocytes, IL-6 prolonged APD, which was further prolonged in the presence of IL-6R. Similar to heterologous cells, IL-6 reduced endogenous guinea-pig ERG channel mRNA and protein expression. The data are first to demonstrate that IL-6 inhibition of IKr and the resulting prolongation of APD is mediated via IL-6R and JAK pathway activation and forms the basis for the observed clinical QT interval prolongation. In summary, cardiac or systemic inflammation promotes QTc-interval prolongation via cytokine-mediated effects and this may increase SCD risk.
The ‘Multihit Theory’
A single channelopathy per se is not able in most cases to induce symptoms, and rarely even the related clinical phenotype.[25] This is well demonstrated for inherited forms, including LQTS, Brugada syndrome, and catecholamine polymorphic VT, where provocative tests can unmask latent genetic defects. Consistent data are also available for drug-induced, autoimmune and inflammatory/fever-induced channelopathies. Indeed, only a small proportion of the large number of exposed subjects develops drug-induced LQTS-related arrhythmias, despite the resulting channel dysfunction. Similarly, cytokines, and anti-ion channel autoimmune antibodies induce cardiac channelopathy and QTc prolongation. However, inflammatory, and autoimmune-induced phenotypes and arrhythmias occur only in a fraction of the subjects at risk. Such evidence strongly suggests that multiple, often-redundant ion channel mechanisms are implicated in preserving normal AP genesis, thus rendering the clinical phenotype unapparent, despite subtle channel dysfunction. Therefore, more than one single component needs to be impaired for ECG/clinical symptoms to emerge, and the number of required hits will depend on the functional impact of each single offending factor. In a single patient, multiple QT-prolonging factors are concomitantly required to significantly disrupt repolarisation. Accordingly, patients developing marked QTc prolongation and TdP concomitantly present multiple risk factors. In a recent analysis, 18 of 40 consecutive unselected patients with TdP, an average of more than four factors per subject were detectable (electrolyte imbalances, cardiac and extracardiac diseases, drugs, anti-Ro/SSA antibodies, and inflammation), with a high prevalence of acquired channelopathies.[24,25]
Pharmacogenetics of Acquired Long QT Sydrome
The susceptibility to acquired QT interval prolongation can be influenced by genetic variations.[27] This is supported by the fact that the heritability of QT interval duration in the general population (excluding congenital LQTS patients) is estimated to be around 35%.[28,29] Further, first-degree relatives of patients with congenital LQTS have a higher risk of drug-induced QT prolongation than non-related individuals.[30] In genome-wide association studies (GWAS), a large number of genes associated with QT interval duration has been identified.[31] The gene with the strongest signal related to QT interval duration is the nitric oxide synthase 1 adaptor protein gene (NOS1AP), located on chromosome 1 (1q23.3),[31,32] which inhibits L-type calcium channel and influences impulse propagation.[33] Other findings from GWAS included polymorphisms within genes known to be mutated in congenital LQTS, genes associated with intracellular calcium handling, as well as genes previously not known to influence cardiac repolarisation.[34] A recent study that compared 188 patients with drug-induced LQTS and more than 1000 patients with congenital LQTS found disease-causing mutations in 28% of patients with drug-induced LQTS.[35] Of interest, under basal conditions, the QTc of drug-induced LQTS patients (453 ± 39 ms) was significantly longer than that of control subjects (406 ± 26 ms).[35]
It is important to consider pharmacogenetics of drug-induced LQTS as related to both pharmacokinetic and pharmacodynamic properties.[27,34] Pharmacokinetics constitute the effect of the body on the drug, which is usually categorised into effect on absorption, distribution, metabolism, and elimination of the drug. Pharmacokinetic genetic susceptibility is mainly characterised by variation in genes encoding drug-metabolising cytochrome P450 or drug transporter like the P-glycoprotein. However, the pharmacodynamics component of genetic susceptibility is mainly characterised by genes known to be associated with QT prolongation in the general population and genes in which the causal mutations of congenital LQTS are located.[35]
Incidence of Drug-induced Long QT Syndrome
The overall incidence of drug-induced LQTS in a given population is difficult to estimate. One study estimated that between 5% and 7% of reports of VT, VF, or SCD were in fact drug-induced LQTS and TdP.[36] European pharmacovigilance centres in Sweden, Germany and Italy have found an annual reporting rate of drug-induced LQTS or TdP of approximately 0.8 to 1.2 per million person-years[36] An epidemiological study of drug-induced LQTS in Germany found the reporting rate for symptomatic acquired LQTS to be 2.5% per million person-years for men and 4.0% per million person-years for women, with 60% attributed to drugs.[37]
QT prolongation is one of the most common reasons for drug withdrawal from the market, despite the fact that these drugs may be beneficial for certain patients and not harmful in every patient.[34] Since 1989, 14 clinically important drugs have been removed from the market due to TdP,[38] and development of an unknown number has been stopped, due to concerns that these might pose a risk of causing QT prolongation and TdP.[38] In the 1990s, the US Food and Drug Administration (FDA) and the European Medicine Agency (EMA) began requiring routine preclinical and clinical testing to determine whether drugs have the potential to cause QT prolongation.[39] Today, according to the CredibleMeds website, which has become the standard reference for drug-induced TdP, 38 marketed drugs are recognised for their potential to cause TdP and another 72 to cause QT prolongation.[40]
In the past decade, hERG channel-mediated cardiac toxicity, manifested as QT interval prolongation, has become a major safety issue in drug development, superseding liver injury as the main cause of drug withdrawals. In vitro electrophysiological testing of the drug's effects on the function of the hERG channel may be cheaper, faster, and potentially more sensitive than other current surrogates for TdP risk, such as in vivo QT prolongation and action potential prolongation in cardiomyocytes.[41]
Ethnicity and Gender Differences in Drug-induced Long QT Syndrome
As ethnic differences ultimately reflect genetic variation, it is useful to study ethnicity with regard to susceptibility to drug-induced QT interval prolongation and TdP. However, the role of ethnic differences has not been well established in published studies on drug-induced QT interval prolongation. In 20 QT/QTc studies, only 10% of the total study population was African-American and only 7% was Asian.[42] Nevertheless, the frequency of polymorphisms in genes known from congenital LQTS showed varying distribution among ethnic groups.[43] African-Americans had the highest risk of prolonged QT interval after acute overdose of QT-prolonging drugs, while Hispanics had the lowest risk compared to all other ethnic groups.[44]
Females with inherited LQTS demonstrate pronounced gender difference in cardiac repolarisation and arrhythmic risk. Adult women with LQT1 and LQT2 have longer QT intervals, a more pronounced transmural QT dispersion, and a higher risk of TdP and SCD than men.[45,46] Interestingly, in female patients with LQT2, the arrhythmogenic risk remains elevated after menopause, suggesting that other gender-related factors besides sex hormones may contribute to gender difference in arrhythmogenesis.[47]
Gender is a risk factor for adverse drug reactions.[48,49] The concept of reduced repolarisation reserve in females compared to males has been used to explain sex differences in arrhythmia risk in acquired LQTS.[50] The reduced repolarisation reserve of the female heart is attributed to lower repolarising K+ currents. This difference was thought to be primarily due to testosterone-mediated increase in IKr and IK1 resulting in shorter APD and QTc interval in male hearts. However, in a recent review, the effects of sex hormones go well beyond their modulation of K+ currents.[51] The underlying mechanisms can be summarised as follows:[52] an estradiol-induced decrease in Ikr as well as increase of ICaL, NCX expression and activity, RyR2 leakiness, Ca2+ transient amplitude, and a1- and b2-adrenoreceptor responsiveness; a testosterone-induced increase in Ikr, Iks, and Ik1, increased SERCA activity, and shortened Ca2+ transient; and a progesterone-induced increase in Iks, increased CERCA expression and activity, and increased ICA-L current sensitivities with reduced Ca2+ oscillations upon sympathetic stimulation. In a recent study, we have shown that modulation of voltage-Ca2+ uncoupling[53] may provide one more attractive electrophysiological mechanism for the increased vulnerability of female to drug-induced LQTS.
Acute and Long-term Management of Acquired Long QT Syndrome
The American College of Cardiology (ACC), American Heart Association (AHA), and European Society of Cardiology (ESC) published guidelines for management of ventricular arrhythmias, including drug-induced TdP,[54] in 2006 and the key recommendations have been endorsed in a more recent ACC/AHA statement.[55]
When monitoring for drug-induced prolonged QT interval, a baseline QTc should be obtained. If any one of the following conditions are observed during QT interval monitoring the patient should be admitted to the hospital for telemetry: QTc >500 ms; QTc increase >60 ms above baseline; QT prolongation accompanied by syncope; any evidence of ECG instability, specially TWA, AV block, QRS widening, or ventricular ectopy. The offending drug should be discontinued, electrolyte abnormalities corrected, and a defibrillator placed at bedside.[55]
Non self-terminating TdP with hemodynamic collapse should obviously be cardioverted with adequate post-cardioversion management. More typical TdP occurs as recurrent self-terminating episodes. In these cases, the first line of management is intravenous administration of magnesium sulphate as a single 2 g (8 mmol) dose over 1–2 minutes followed by a second dose if necessary. Magnesium sulphate is effective in suppressing TdP without reducing the QT interval.[56] The mechanism of action may be related to suppression of late calcium influx via L-type calcium current and reduction in the amplitude of EADs.[57] If magnesium sulphate fails to suppress TdP, the next step is to increase the heart rate, typically by transvenous pacing. In the interim if necessary, isoproterenol administration could promptly increase the heart rate while waiting for insertion of pacing electrode. Increasing the heart rate is associated with shortening of the QT interval and suppression of TdP. At the same time, the culprit drug should be discontinued and acid-base and electrolytes should be corrected as necessary.
There are novel experimental drugs that can enhance the delayed rectifier conductance[52] or activate the cardiac ATP-sensitive potassium channel,[58] which may have future value for the treatment of acquired LQTS.
Long-term management of acquired LQTS is important. All patients with previous drug-induced prolongation of the QT interval should be instructed about the importance of subsequent avoidance of QT-prolonging drugs and should have a list of QT-prolonging medications provided by their physicians. In patients with acquired LQTS, the risk of further episodes of TdP is reduced once the culprit drug is removed and other aggravating situations as electrolyte abnormalities or marked bradycardia are corrected. This should result in normalisation of the QTc interval. If it does not, the patient and symptomatic first-degree family members should be considered for genetic testing for the presence of LQTS-associated mutations.[55,59] This is especially important for relatives of patients with drug-induced case fatality.
Comprehensive Electrophysiological Mechanisms of Torsade de Pointes
Experimental Models of Long QT Syndrome
Both drug-induced and genetically modified animal models of various species have been generated and utilised to investigate the electrophysiological mechanisms of arrhythmogenesis in LQTS and potential pro- and antiarrhythmic agents. However, due to species differences in features of cardiac electrical function, particularly in repolarisation currents, these models do not completely recapitulate all aspects of the electrophysiology of the human disease. Genetically modified animal models, such as mice and rabbit are commonly used to investigate the arrhythmogenicity of LQTS. Current transgenic LQTS rabbit models have already been instrumental to increasing our understanding of the role of spatial and temporal dispersion of repolarisation to provide an arrhythmogenic substrate, genotype differences in the mechanisms for EAD formation and arrhythmia maintenance, and mechanisms of hormonal modification of arrhythmogenesis.[60]
In contrast, two dog model of LQTS and TdP have been extensively investigated. One model is the dog with induced complete atrioventricular conduction block (AVB). Complete AVB results within few weeks in hypertrophy and remodelling of the left ventricle associated with prolongation of the QT interval, APD, as well as spatial DR.[61] When the animal is challenged with a drug that blocks the IKr, like dofetilide, it results in further prolongation of the QT interval and creation of a drug-induced model of acquired LQTS and TdP.[62]
The other dog model of LQTS and TdP is the Anthopleurin-A (AP-A) canine surrogate model of LQT3 that was developed in this laboratory.[63] The model is created by the neurotoxin anthopleurin-A or ATX2.[64] that faithfully reproduces the molecular changes associated with clinical mutations of the Na channel in patients with LQT3.[65] Of interest, the experimental surrogate model of LQT3 anticipated the first description of the clinical LQT37 by 7 years.[66] Figure 4 is a representative composite of the salient experimental techniques that were utilised to investigate the model and illustrate the correlation between the modulation of a cardiac ion current, its electrophysiological consequence and the final phenotype presentation as LQTS and TdP.
Electrophysiological Mechanisms of the Trigger of Torsade de Pointes in the Long QT Syndrome
There is an almost complete agreement that the initiating one or two beats of TdP are due to EAD-triggered focal activity from the subendocardial Purkinje network.[60,66–70] A study by Caref et al. has confirmed beyond reasonable doubt the subendocardial origin of the trigger of TdP.71[71] In this study the canine surrogate model of LQT3 was placed on cardiopulmonary bypass and chemical ablation of the endocardial Purkinje network was obtained using Lugol's iodine following which spontaneous TdP were no longer observed. However, a properly timed premature stimulus-induced reentrant Veterans Administration (VA) based on the underlying marked DR. However, the perpetuation of TdP remains controversial and could be attributed to focal activity, reentrant excitation, or a combination of both mechanisms.
The ionic mechanism(s) that underlie the generation of EADs have been widely investigated. The central hypothesis on the generation of EADs suggests that a spontaneous release of calcium from the sarcoplasmic reticulum would temporarily increase cytosolic calcium concentration with a subsequent sudden activation of the sodium-calcium exchanger inward current. This inward current could ‘re-depolarise’ the sarcolemmal membrane to a potential from which sodium or calcium currents become reactivated, triggering an afterdepolarisation.[72] Although this model has been primarily discussed to explain delayed afterdepolarisations, there is also evidence that this mechanism may be the trigger for EADs.[73] This hypothesis is also supported by studies that showed that inhibition of the sodium-calcium exchanger suppresses TdP in the intact heart model of LQTS2 and LQTS3.[74]
Electrophysiological Mechanisms of Perpetuation of Torsade de Pointes
Contrary to the established mechanism of the trigger of TdP, the perpetuation of TdP remains controversial and could be attributed to focal activity, reentrant excitation, or a combination of both mechanisms.[75,76] Both reentrant and focal activity are assumed to be non-stationary. For reentrant excitation this could be due to a heterogeneity-induced drift of a reentrant circuit,[77] or a meandering reentrant spiral wave[78] (Figure 1D). Alternatively, ectopic beats originating from different locations may explain the perpetuation of TdP. The original description of TdP by Dessertenne attributed the pattern to two variable opposing foci (deux foyers)[7]. In computational modelling as well as experimental observation of the canine chronic AVB model, both multiple competing foci and reentrant excitation could develop depending on heterogeneity of repolarisation in comparison to the surrounding tissue.[75] Large heterogeneities can produce ectopic TdP, while smaller heterogeneities will produce reentrant type TdP. The authors of an experimental study in the same model reported that short-lasting episode of TdP had a focal mechanism while long-lasting episodes were maintained by reentrant excitation.[76] However, the results were criticised because of the controversial definition of focal versus reentrant excitation.[79]
It remains an open question as to why and how ectopic beats emerge and compete, and what their relationship is to observe EAD activity. EADs arising from subendocardial Purkinje network conducted to overlying myocardium through Purkinje-muscle junctions (PMJ). Electrotonic interactions across PMJs can modulate APD locally. A recent study has proposed that, dependent on resistive properties across PMJs, large spatial gradient of APD can develop at the endocardium and the transmural plane.[80] This may provide a better explanation compared to the concept of mid-myocardial (M) cells with different ionic characteristics.[81]
One of the problems of sustained fast EAD-induced focal activity is that the short cycle length will be associated with short APD that would suppress further EADs generation unless there is some form of protected islands of prolonged APD with EADs capable of conduction across PMJs to activate the ventricular myocardium. A study that combined computational simulation and experimental observations in isolated myocytes showed that in electrically homogeneous tissue models, chaotic EADs synchronise globally when the tissue is smaller than a critical size. However, when the tissue exceeds the critical size, electronic coupling can no longer globally synchronise EAD, resulting in regions of partial synchronisation that shift in time and space. These regional partially synchronised EADs then form premature ventricular complexes that propagate into recovered tissue without EADs, thus creating ‘shifting’ foci that resemble polymorphic VT.[82]
Delayed After Depolarisation-triggered Activity Contributes to VA in the Long QT Syndrome
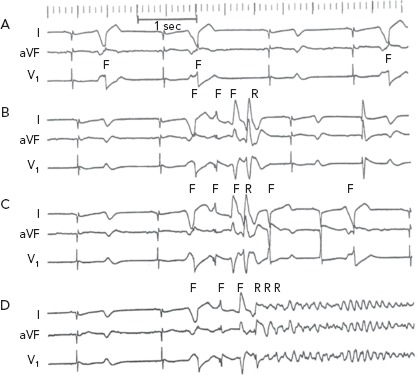
The electrophysiological mechanism of VT in LQTS is somewhat more complex than that described earlier. Figure 5A was obtained from one of the classic reviews of cellular mechanisms of cardiac arrhythmias by Hoffman and Rosen.[83] It shows transmembrane AP recording from a canine Purkinje-fiber-superfused with 20-mM caesium chloride (a surrogate experimental model for LQT2). The recording illustrates the classic bradycardia-dependent prolongation of AP duration associated with membrane oscillation on late phase 2/early phase 3 of the repolarisation phase characteristic of EADs. But it also shows that complete repolarisation of the AP is followed by a sub threshold delayed afterdepolarisation (DAD). The latter is simply explained on the basis of increased intracellular Ca2+ associated with the prolonged AP duration triggering a transient inward current. This, almost forgotten, observation strongly suggests that some VT and ectopic beats in LQTS could be secondary to DADs.
Figure 5: Early and delayed afterdepolarizations in Long QT Syndrome.
A: Transmembrane action potential recording from a Purkinje fiber-superfused with 20 mM caesium chloride showing both early and delayed afterdepolarisations. B: ECG recording from an in vivo canine anthopleurin-A surrogate model of LQT3. F = focal discharge; R = reentrant excitation. Source: El-Sherif, 2001.84 Reproduced with permission from © Futura Publishing Company, Inc. 2001.
Figure 5B shows a corroboration of this observation from the canine surrogate model of LQT3.[84] The top ECG tracing was obtained 10 minutes after infusion of AP-A and shows moderate prolongation of the QT interval and a run of non-sustained monomorphic VT at a rate of 150 bpm. The VT starts with a late coupled beat that is well beyond the end of the QT interval of the preceding sinus beat. Tridimensional mapping of activation showed that the VT arose as a focal discharge (F) from the same subendocardial site. For all practical purposes, the focal discharge could be attributed to DAD-triggered activity.
The bottom ECG tracing was obtained from the same experiment 10 minutes later and shows further prolongation of the QT interval. The ectopic beats labeled F now seem to be coupled to the end of the prolonged QT interval of the preceding sinus beats. The middle of the tracing illustrates a six-beat run of polymorphic VT. Tridimensional mapping shows that the first beat arose from a subendocardial focal site and could be safely attributed to EAD-triggered activity, whereas subsequent beats were due to reentrant excitation in the form of continuously varying scroll waves.
Electrophysiological Mechanisms of Self-terminating versus Non-self-terminating Torsade de Pointes Ventricular Tachyarrhythmia
The majority of TdP episodes terminate spontaneously (self-terminating [ST]), (Figure 1). However, a minority can degenerate in VF (non-self-terminating [NST]). The electrophysiological mechanisms of the NST episodes of TdP have never been elucidated. Obviously this is a more important issue than the ‘twisting and turning’ to see if perpetuation of TdP VT is due to focal or reentrant activation.[79] Figures 6 and 7 obtained from the canine surrogate model of LQT3 provides one possible electrophysiological mechanism.[84] The lesson gained from this example is that subtle changes in underlying spatial DR and conduction characteristics can result in fractionation of activation wavefronts and VF. It also demonstrates clearly the difficulty in predicting which TdP episodes will be ST of NST.
Figure 6: ECG Recordings from an In Vivo Canine Anthopleurin-A Surrogate Model of Long QT Syndrome Type 3.
The recordings are arranged chronologically, a few minutes apart. A: Stable bigeminal and trigeminal rhythm due to subendocardial discharge attributed to EAD-triggered activity from the same focus. This was followed several minutes later by runs of four- or five-beat polymorphic VT with remarkable repetition of the same QRS morphology (panels B and C). The first beat of each run arose from the same site of the bigeminal/ trigeminal beats in panel A. The second and third beats of each run arose from two different subendocardial focal sites; the fourth beat was reentrant in origin. The fifth beat in a five-beat run again was focal in origin and arose well after the end of the reentrant excitation and could be attributed to DAD-triggered activity. After approximately 10 minutes of repetitive non-sustained VT, the same three initial focal beats were followed by reentrant excitation that degenerated into ventricular fibrillation (VF) (panel D). F = focal discharge; R = reentrant excitation. Source: El-Sherif, 2001.84 Reproduced with permission from © Futura Publishing Company, Inc. 2001.
Figure 7: Isochronal Maps of Nonsustained and Sustained Ventricular Tachyarrhythmia Shown in Figure 6.

(A) Selected electrograms of the five-beat nonsustained ventricular tachyarrhythmia shown in Figure 6C (V1–V5) and the first five beats of the ventricular tachyarrhythmia that degenerated into ventricular fibrillation shown in Figure 6D (V1–V5). A limited activation map of both V3 beats is shown. The electrophysiological mechanism of the different consequences of the same V3 ectopic beat in the two episodes is shown. The inter-ectopic intervals V l–V2 and V2–V3 increased by approximately 30–40 ms in the second episode compared with the first episode (the equivalent of a slight slowing of the discharge of the focal activity). This resulted in lengthening of local repolarisation following the V2 beat by 30–40 ms. However, the degree of lengthening of repolarisation was disparate at contiguous sites, resulting in functional conduction block and the initiation of a more complex reentrant wavefront. One such site where new conduction block developed during the NST TdP is shown in the electrograms between sites D and E, as well as in the isochronal maps on the right side of the figure (lower panel B). The numbers without brackets represent cycle lengths in milliseconds, and the numbers in brackets represent activation-recovery intervals. Source: El-Sherif, 2001.84 Reproduced with permission from © Futura Publishing Company, Inc. 2001.
Future Directions
Although congenital LQTS remains the domain of cardiologists, cardiac electrophysiologists and specialised centres, the far more frequently acquired drug-induced LQTS is the domain of all physicians and other members of healthcare teams who are required to make therapeutic decisions. To support better prescribing of medicines, clinical decision support systems to date have issued alerts that warn of potential harm from a prescribing decision.[85] However, the impact of these systems has been limited. Moving away from the use of alerts to signal prescribing errors, the concept of ‘medical autopilots’ has been suggested as a preferred approach.[86] These programs will monitor the electronic medical record and send signals to guide prescribers toward decisions that result in maximum benefit and minimal risk of TdP.
Acknowledgments
Supported in part by Cardiovascular Research Program, the Narrows Institute for Biomedical Research and Education, and a MERIT Award Number I01 BX002137 from the Biomedical Laboratory Research & Development Service of the Veterans Affairs Office of Research and Development.
References
- 1.Jervell A, Lange-Nielsen F. Congenital deaf-mutism, functional heart disease with prolongation of the Q-T interval and sudden death. Am Heart J. 1957;54:59–68. doi: 10.1016/0002-8703(57)90079-0. [DOI] [PubMed] [Google Scholar]
- 2.El-Sherif N, Turitto G. The long QT syndrome and torsade de pointes. PACE. 1999;22:91–110. doi: 10.1111/j.1540-8159.1999.tb00305.x. [DOI] [PubMed] [Google Scholar]
- 3.Kannankeril P, Roden DM, Darbar D. Drug-induced long QT syndrome. Pharmacol Rev. 2010;62:760–81. doi: 10.1124/pr.110.003723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.El-Sherif N, Turitto G. Electrolyte disorders and arrhythmogenesis. Cardiology J. 2011;18:1–13. [PubMed] [Google Scholar]
- 5.Yang T, Chun YW, Stroud DM et al. Screening for acute IKr block is insufficient to detect torsade de pointes liability: role of late sodium current. Circulation. 2014;130:224–34. doi: 10.1161/CIRCULATIONAHA.113.007765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.El-Sherif N, Caref EB, Chinushi M, Restivo M. Mechanism of arrhythmogenicity of the short-long cardiac sequence that precedes ventricular tachyarrhythmias in the long QT syndrome. J Am Coll Cardiol. 1999;33:1415–23. doi: 10.1016/s0735-1097(98)00700-1. [DOI] [PubMed] [Google Scholar]
- 7.Dessertenne F. Ventricular tachycardia with two variable opposing foci. Arch Mal Coeur Vaiss. 1966;59:263–72. [In French] [PubMed] [Google Scholar]
- 8.Moss AJ. Long QT syndrome. In: Podrid PJ, Kowey PR (eds) Cardiac Arrhythmias. Mechanisms, Diagnosis, and Management. 1995. pp. 1110–20. Baltimore: MD, Williams & Wilkins.
- 9.Castillo R, Pedalino R, El-Sherif N, Turitto G. Efavirenz-associated QT prolongation and torsade de pointes arrhythmia. Ann Pharmacother. 2002;36:1006–8. doi: 10.1345/aph.1A454. [DOI] [PubMed] [Google Scholar]
- 10.Verrier RL, Klingenheben T, Malik M et al. Microvolt T-wave alternans: physiological basis, methods of assessment, and clinical utility consensus guideline by International Society of Holter and Noninvasive Electrocardiology. J Am Coll Cardiol. 2011;58:1309–24. doi: 10.1016/j.jacc.2011.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Takasugi N, Goto H, Takasugi M et al. Prevalence of microvolt T-wave alternans in patients with long QT syndrome and its association with torsade de pointes. Circ Arrhythm Electrophysiol. 2016;9:e003206. doi: 10.1161/CIRCEP.115.003206. [DOI] [PubMed] [Google Scholar]
- 12.Chinushi M, Restivo M, Caref EB, El-Sherif N. Electrophysiological basis of the arrhythmogenicity of QT/T alternans in the long QT syndrome: Tridimensional analysis of the kinetics of cardiac repolarization. Circ Res. 1998;83:614–28. doi: 10.1161/01.res.83.6.614. [DOI] [PubMed] [Google Scholar]
- 13.Milberg P, Ramtin S, Monnig G et al. Comparison of the in vitro electrophysiologic and proarrhythmic effects of amiodarone and sotalol in a rabbit model of acute atrioventricular block. J Cardiovasc Pharmacol. 2004;44:278–86. doi: 10.1097/01.fjc.0000129581.81508.78. [DOI] [PubMed] [Google Scholar]
- 14.Hondenghem LM, Carlsson L, Duker G. Instability and triangulation of the action potential predict serious proarrhythmia, but action potential duration prolongation is antiarrhythmic. Circulation. 2001;103:2004–13. doi: 10.1161/01.CIR.103.15.2004. [DOI] [PubMed] [Google Scholar]
- 15.Said TH, Lance DW, Jeyaraj D et al. Transmural dispersion of repolarization as a preclinical marker of drug-induced proarrhythmia. J Cardiovasc Pharmacol. 2012;60:165–171. doi: 10.1097/FJC.0b013e3182597f67. [DOI] [PubMed] [Google Scholar]
- 16.Nattel S, Antzelevich C, Noble D. Resolving the M-cell debate: why and how. Heart Rhythm. 2011;8:1293–5. doi: 10.1016/j.hrthm.2011.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sicouri S, Antzelevitch C. Mechanisms underlying the actions of antidepressant and antipsychotic drugs that cause sudden cardiac arrest. Arrhythm Electrophysiol Rev. 2018;7:199–209. doi: 10.15420/aer.2018.29.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jasiak NM, Bostwick JR. Risk of QT/QTc prolongatiom among newer non-SSRI antidepressants. Ann Pharmacother. 2014;48:1620–8. doi: 10.1177/1060028014550645. [DOI] [PubMed] [Google Scholar]
- 19.Cho MS, Nam GB, Kim YG et al. Electrocardiographic predictors of bradycardia-induced torsades de pointes in patients with acquired atrioventricular block. Heart Rhythm. 2015;12:498–505. doi: 10.1016/j.hrthm.2014.11.018. [DOI] [PubMed] [Google Scholar]
- 20.Lazzerini PE, Capecchi PL, Laghi-Pasini F. Long QT syndrome: an emerging role for inflammation and immunity. Front Cardiovasc Med. 2015;2:1–17. doi: 10.3389/fcvm.2015.00026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Boutjdir M, Lazzerini PE, Capecchi PL et al. Potassium channel block and novel autoimmune-associated long QT syndrome. Card Electrophysiol Clin. 2016;8:373–84. doi: 10.1016/j.ccep.2016.02.002. [DOI] [PubMed] [Google Scholar]
- 22.Lazzerini PE, Yue Y, Srivastava U et al. Arrythmogenicity of anti Ro/SSA antibodies in patients with torsade de pointes. Circ Arrhythm Electrophysiol. 2016; 9:e003419. doi: 10.1161/CIRCEP.115.003419. [DOI] [PubMed] [Google Scholar]
- 23.Yue Y, Castrichini M, Srivastava U et al. Pathogenesis of the novel autoimmune-associated long-QT syndrome. Circulation. 2015;132:230–40. doi: 10.1161/CIRCULATIONAHA.115.009800. [DOI] [PubMed] [Google Scholar]
- 24.Lazzerini PE, Laghi-Pasini F, Bertolizi I et al. Systemic inflammation as a novel QT-prolonging risk factors in patients with torsade de pointes. Heart. 2017;103:1821–9. doi: 10.1136/heartjnl-2016-311079. [DOI] [PubMed] [Google Scholar]
- 25.Lazzarini PE, Capecci PL, El-Sherif M et al. Emerging arrhythmic risk of autoimmune and inflammatory cardiac channelopathies. J Am Heart Assoc. 2018;7:e010595. doi: 10.1161/JAHA.118.010595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Aromolaran AS, Srivastava U, Ali A et al. Onterleukin-6 inhibition of hERG underlies risk of acquired long QT in cardiac and systemic inflammation. PloS One. 2018;13:1–17. doi: 10.1371/journal.pone.0208321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mahida S, Hogarth AJ, Cowan C et al. Genetics of congenital and drug-induced long QT syndromes: current evidence and future research perspectives. J Interv Card Electrophysiol. 2013;37:9–19. doi: 10.1007/s10840-013-9779-5. [DOI] [PubMed] [Google Scholar]
- 28.Hong Y, Rautaharju PM, Hopkins PN et al. Familial aggregation of QT-interval variability in a general population: results from the NHLBI Family Heart Study. Clin Genet. 2001;59:171–7. doi: 10.1034/j.1399-0004.2001.590305.x. [DOI] [PubMed] [Google Scholar]
- 29.Newton-Cheh C, Larson MG, Corey DC et al. QT interval is a heritable quantitative trait with evidence of linkage to chromosome 3 in a genome-wide linkage analysis: The Framingham Heart Study. Heart Rhythm. 2005;2:277–84. doi: 10.1016/j.hrthm.2004.11.009. [DOI] [PubMed] [Google Scholar]
- 30.Kannankeril PJ, Roden DM, Norris KJ et al. Genetic susceptibility to acquired long QT syndrome: pharmacologic challenge in first-degree relatives. Heart Rhythm. 2005;2:134–40. doi: 10.1016/j.hrthm.2004.10.039. [DOI] [PubMed] [Google Scholar]
- 31.Pfeufer A, Sanna S, Arking DE et al. Common variants at ten loci modulate the QT interval duration in the QTSCD Study. Nat Genet. 2009;41:407–14. doi: 10.1038/ng.362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jamshidi Y, Nolte IM, Dalageorgou C et al. Common variation in the NOS1AP gene is associated with drug-induced QT prolongation and ventricular arrhythmia. J Am Coll Cardiol. 2012;60:841–50. doi: 10.1016/j.jacc.2012.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kapoor A, Sekar RB, Hansen NF et al. An enhancer polymorphism at the cardiomyocyte intercalated disc protein NOS1AP locus is a major regulator of the QT interval. Am J Human Genet. 2014;94:854–69. doi: 10.1016/j.ajhg.2014.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Niemeijer MN, van den Berg ME, Eijgelsheim M. Pharmacogenetics of drug-induced QT interval prolongation: An update. Drug Saf. 2015;38:855–67. doi: 10.1007/s40264-015-0316-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ito H, Crotti L, Aiba T et al. The genetics underlying acquired long QT syndrome: Impact for genetic screening. Eur Heart J. 2016;37:1456–64. doi: 10.1093/eurheartj/ehv695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Molokhia M, Pathak A, Lapeyre-Mestre M et al. Case ascertainment and estimated incidence of drug-induced long-QT syndrome: Study in Southwest France. Brit J Clin Pharmacol. 2008;66:386–95. doi: 10.1111/j.1365-2125.2008.03229.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sarganas G, Garbe E, Klimple A et al. Epidemiology of symptomatic drug-induced long QT syndrome and torsade de pointes in Germany. Europace. 2014;16:101–8. doi: 10.1093/europace/eut214. [DOI] [PubMed] [Google Scholar]
- 38.Ninan B, Wertheimer A. Withdrawing drugs in the US versus other countries. Innov Pharm. 2012;3:1–12. [Google Scholar]
- 39.Shah RR. Drugs, QTc interval prolongation and final ICH E14 guideline: An important milestone with challenges ahead. Drug Saf. 2005;28:1009–28. doi: 10.2165/00002018-200528110-00003. [DOI] [PubMed] [Google Scholar]
- 40.Woosley RL, Romero K. Assessing cardiovascular drug safety for clinical decision-making. Nat Rev Cardiol. 2013;13:330–37. doi: 10.1038/nrcardio.2013.57. [DOI] [PubMed] [Google Scholar]
- 41.Barra S, Agarwal S, Begley D et al. Post-acute management of the acquired long QT syndrome. Postgrad Med J. 2014;90:348–58. doi: 10.1136/postgradmedj-2013-132398. [DOI] [PubMed] [Google Scholar]
- 42.Florian JA, Tornoe CW, Brundage R et al. Population pharmacokinetics and concentration - QTc models for moxifloxacin: pooled analysis of 20 thorough QT studies. J Clin Pharmacol. 2011;51:1152–62. doi: 10.1177/0091270010381498. [DOI] [PubMed] [Google Scholar]
- 43.Ackerman MJ, Splawski I, Makielski JC et al. Spectrum and prevalence of cardiac sodium channel variants among Black, White, Asian, and Hispanic individuals: implications for arrhythmogenic susceptibility and Brugada/long QT syndrome genetic testing. Heart Rhythm. 2004;1:600–7. doi: 10.1016/j.hrthm.2004.07.013. [DOI] [PubMed] [Google Scholar]
- 44.Manini AF, Stimmel B, Vlahov D. Racial susceptibility for QT prolongation in acute drug overdoses. J Electrocardiol. 2014;47:244–50. doi: 10.1016/j.jelectrocard.2013.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sauer AJ, Moss AJ, McNitt S et al. Long QT syndrome in adults. J Am Coll Cardiol. 2007;49:329–37. doi: 10.1016/j.jacc.2006.08.057. [DOI] [PubMed] [Google Scholar]
- 46.Conrath CE, Wilde AA, Jongbloed RJ et al. Gender difference in the long QT syndrome: effects of beta-adrenoreceptor blockade. Cardiovasc Res. 2002;53:770–6. doi: 10.1016/s0008-6363(01)00477-1. [DOI] [PubMed] [Google Scholar]
- 47.Buber J, Mathew J, Moss AJ et al. Risk of recurrent cardiac events after onset of menopause in women with congenital Long QT syndrome type 1 and 2. Circulation. 2011;123:2784–91. doi: 10.1161/CIRCULATIONAHA.110.000620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Drici MD, Clement N. Is gender a risk factor for adverse drug reactions? The example of drug induced long QT syndrome. Drug Saf. 2001;24:575–85. doi: 10.2165/00002018-200124080-00002. [DOI] [PubMed] [Google Scholar]
- 49.Coker SJ. Drugs for men and women-how important is gender as risk factor for TdP? Pharmacol Ther. 2009;119:186–94. doi: 10.1016/j.pharmthera.2008.03.005. [DOI] [PubMed] [Google Scholar]
- 50.Roden DM. Drug-induced prolongation of the QT interval. N Engl J Med. 2004;350:1013–22. doi: 10.1056/NEJMra032426. [DOI] [PubMed] [Google Scholar]
- 51.Salama G, Bett GCL. Sex differences in the mechanism underlying long QT syndrome. Am J Physiol Heart Circ Physiol. 2014;307:H640–8. doi: 10.1152/ajpheart.00864.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Odening KE, Koren G. How do sex hormones modify arrhythmogenesis in long QT syndrome? Sex hormones effects on arrhythmogenic substrate and trigger activity. Heart Rhythm. 2014;11:2107–15. doi: 10.1016/j.hrthm.2014.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.El-Sherif N, Himel HG, Yue Y Electrophysiological substrates for gender difference in the incidence of Torsade de Pointes Arrhythmias. In: Shenasa M, Hindricks G, Borggrefe M, Breithardt G (eds) Cardiac Mapping. 5th ed Elsevier, 2018, In press.
- 54.Zipes DP, Camm AJ, Borggrefe M et al. ACC/AHA/ESC Guidelines for Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death: a report of the American College of Cardiology/American Heart Association Task Force and the European Society of Cardiology Committee for Practice Guidelines (writing committee to develop Guidelines for Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death) developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. Circulation. 2006;114:e385–484. doi: 10.1161/CIRCULATIONAHA.106.178233. [DOI] [PubMed] [Google Scholar]
- 55.Drew BJ, Ackerman MJ, Funk M et al. Prevention of torsade de pointes in hospital setting: a scientific statement from the American Heart Association and the American College of Cardiology Foundation. Circulation. 2010;121:1047–60. doi: 10.1161/CIRCULATIONAHA.109.192704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kaye P, O'Sullivan I. Role of magnesium in the emergency department. Emerg Med J. 2002;19:288–91. doi: 10.1136/emj.19.4.288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Diness T, Yeh YH, Qi XY et al. Antiarrhythmic properties of rapid delayed-rectifier current activator in rabbit models of acquired long QT syndrome. Cardiovasc Res. 2008;79:61–9. doi: 10.1093/cvr/cvn075. [DOI] [PubMed] [Google Scholar]
- 58.Testai L, Cecchetti V, Sabatini S et al. Effects of K openers on the QT prolongation induced by HERG-blocking drugs in Guinea-pigs. J Pharmacol. 2010;62:924–30. doi: 10.1211/jpp.62.06.0014. [DOI] [PubMed] [Google Scholar]
- 59.Priori SG, Wilde AA, Horie M et al. Executive summary: HRS/EHRA/APHRS expert consensus statement on the diagnosis and management of patients with inherited primary arrhythmia syndromes. Europace. 2013;15:1389–1406. doi: 10.1093/europace/eut272. [DOI] [PubMed] [Google Scholar]
- 60.Lang CN, Koren G, Odening KE. Transgenic rabbit models to investigate the cardiac ion channel disease long QT syndrome. Progress Biophys Mol Biol. 201(21):142–56. doi: 10.1016/j.pbiomolbio.2016.05.004. [DOI] [PubMed] [Google Scholar]
- 61.Vos MA, de Groot SH, Verduyn SC et al. Enhanced susceptibility for acquired torsade de pointes arrhythmias in the dog with chronic complete AV block is related to cardiac hypertrophy and electrical remodeling. Circulation. 1998;98:1125–35. doi: 10.1161/01.cir.98.11.1125. [DOI] [PubMed] [Google Scholar]
- 62.Kozhevnikov DO, Yamamoto K, Robotis D et al. Electrophysiological mechanisms of enhanced susceptibility of hypertrophied heart to acquired torsade de pointes arrhythmias: tridimensional mapping of activation and recovery. Circulation. 2002;105:1128–34. doi: 10.1161/hc0902.104711. [DOI] [PubMed] [Google Scholar]
- 63.El-Sherif N, Zeiler RH, Craelius W et al. QTc prolongation and polymorphic ventricular tachyarrhythmias due to bradycardia-dependent early after depolarizations. Circ Res. 1988;63:286–305. doi: 10.1161/01.res.63.2.286. [DOI] [PubMed] [Google Scholar]
- 64.El-Sherif N, Fozzard HA, Hanck DA. Dose-dependent modulation of the cardiac sodium channel by the sea anemone toxin ATXII. Circulation Res. 1992;70:285–301. doi: 10.1161/01.res.70.2.285. [DOI] [PubMed] [Google Scholar]
- 65.Bennett PB, Yazawa K, Makita N, George AL Jr. Molecular mechanism for an inherited cardiac arrhythmia. Nature. 1995;37:683–5. doi: 10.1038/376683a0. [DOI] [PubMed] [Google Scholar]
- 66.Wang O, Shen J, Splawski I et al. SCN5A mutations associated with an inherited cardiac arrhythmia, long QT syndrome. Cell. 1995;80:805–11. doi: 10.1016/0092-8674(95)90359-3. [DOI] [PubMed] [Google Scholar]
- 67.El-Sherif N, Boutjdir M. Role of pharmacotherapy in cardiac ion channelopathies. Pharmacol Ther. 2015;155:132–42. doi: 10.1016/j.pharmthera.2015.09.002. [DOI] [PubMed] [Google Scholar]
- 68.El-Sherif N, Caref EB, Yin H, Restivo M. The electrophysiological mechanism of ventricular tachyarrhythmias in the long QT syndrome. Tridimensional mapping of activation and recovery patterns. Circ Res. 1996;79:474–92. doi: 10.1161/01.res.79.3.474. [DOI] [PubMed] [Google Scholar]
- 69.El-Sherif N, Chinushi M, Caref EB, Restivo M. Electrophysiological mechanism of the characteristic electrocardiographic morphology of torsade de pointes tachyarrhythmias in the long-QT syndrome. Detailed analysis of ventricular tridimensional activation patterns. Circulation. 1997;96:4392–9. doi: 10.1161/01.cir.96.12.4392. [DOI] [PubMed] [Google Scholar]
- 70.Schreiner KD, Voss F, Senges JC, Becker R et al. Tridimensional activation patterns of acquired torsde de pointes tachycardiaon dogs with chronic AV block. Basic Res Cardiol. 2004;99:288–98. doi: 10.1007/s00395-004-0469-4. [DOI] [PubMed] [Google Scholar]
- 71.Caref EB, Boutjdir M, Himel HD, El-Sherif N. Role of subendocardial Purkinje network in triggering torsade de pointes arrhythmias in experimental long QT syndrome. Europace. 2008;10:1218–23. doi: 10.1093/europace/eun248. [DOI] [PubMed] [Google Scholar]
- 72.Spido KR, Varro A, Eisner D. Sodium calcium exchange as a target for antiarrhythmic therapy. Handb Exp Pharmacol. 2006;171:159–99. doi: 10.1007/3-540-29715-4_6. [DOI] [PubMed] [Google Scholar]
- 73.Pogwizd SM, Bers DM. Cellular basis of triggered arrhythmias in heart failure. Trends Cardiovasc Med. 2004;14:61–6. doi: 10.1016/j.tcm.2003.12.002. [DOI] [PubMed] [Google Scholar]
- 74.Milberg P, Pott C, Fink M et al. Inhibition of the Na+/Ca2+ exchanger suppresses torsade de pointes in an intact heart model of long QT syndrome-2 and long QT syndrome-3. Heart Rhythm. 2008;5:1444–52. doi: 10.1016/j.hrthm.2008.06.017. [DOI] [PubMed] [Google Scholar]
- 75.Vandersickel N, de Boer TP, Vos MA, Panfilov AV. Perpetuation of torsade de pointes in heterogeneous hearts: competing foci or re-entry. J Physiol. 2016;594:6865–78. doi: 10.1113/JP271728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Vandersickel N, Bossu A, De Neve J et al. Short-lasting episodes of torsade de pointes in the chronic atrioventricular block dog model have focal mechanism, while longer-lasting episodes are maintained by re-entry. J Am Coll Cardiol. 2017;3:1565–76. doi: 10.1016/j.jacep.2017.06.016. epub ahead of press. [DOI] [PubMed] [Google Scholar]
- 77.Gray RA, Jalife J, Panfilov A. Non stationary vortexlike reentrant activity as a mechanism of polymorphic ventricular tachycardia in the isolated rabbit heart. Circulation. 1995;91:2454–69. doi: 10.1161/01.cir.91.9.2454. [DOI] [PubMed] [Google Scholar]
- 78.Winfree AT. Mechanism of cardiac fibrillation. Reply. Science. 1995;270:1222–5. [PubMed] [Google Scholar]
- 79.Nayyar S, Porta-Sanchez A, Nanthakumar K. Twisting and turning to find an explanation for torsade de pointes. JACC Electrophysiol. 2017;3:1577–9. doi: 10.1016/j.jacep.2017.09.174. [DOI] [PubMed] [Google Scholar]
- 80.Walton RD, Martinez ME, Bishop MJ et al. Influence of the Purkinje-muscle junction on transmural repolarization heterogeneity. Cardiovasc Res. 2014;103:629–40. doi: 10.1093/cvr/cvu165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Sicouri S, Antzelevitch C. Electrophysiologic characteristics of M cells in the canine left ventricular free wall. J Cardiovasc Electrophysiol. 1995;6:591–603. doi: 10.1111/j.1540-8167.1995.tb00435.x. [DOI] [PubMed] [Google Scholar]
- 82.Sato D, Xie L-H, Sovari AA et al. Synchronization of chaotic early afterdepolarizations in the genesis of cardiac arrhythmias. Proc Natl Acad Sci. 2009;106:2983–8. doi: 10.1073/pnas.0809148106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Hoffman BF, Rosen MR. Cellular mechanisms for cardiac arrhythmias. Circ Res. 1981;49:1–15. doi: 10.1161/01.res.49.1.1. [DOI] [PubMed] [Google Scholar]
- 84.El-Sherif N. Mechanism of ventricular arrhythmias in the long QT syndrome: on hermeneutics. J Cardiovasc Electrophysiol. 2001;12:973–6. doi: 10.1046/j.1540-8167.2001.00973.x. [DOI] [PubMed] [Google Scholar]
- 85.Payne TH, Hines LE, Chan RC et al. Recommendations to improve the usability of drug-drug interaction clinical decision support alerts. J Am Med Inform Assoc. 2015;22:1243–50. doi: 10.1093/jamia/ocv011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Woosley RL, Whyte J, Mohamadi A, Romero K. Medical decision support systems and therapeutics: the role of autopilots. Clin Pharmacol Ther. 2016;99:161–4. doi: 10.1002/cpt.259. [DOI] [PubMed] [Google Scholar]


