Abstract
Aims
To investigate the association of estimated total daily sleep duration and daytime nap duration with deaths and major cardiovascular events.
Methods and results
We estimated the durations of total daily sleep and daytime naps based on the amount of time in bed and self-reported napping time and examined the associations between them and the composite outcome of deaths and major cardiovascular events in 116 632 participants from seven regions. After a median follow-up of 7.8 years, we recorded 4381 deaths and 4365 major cardiovascular events. It showed both shorter (≤6 h/day) and longer (>8 h/day) estimated total sleep durations were associated with an increased risk of the composite outcome when adjusted for age and sex. After adjustment for demographic characteristics, lifestyle behaviours and health status, a J-shaped association was observed. Compared with sleeping 6–8 h/day, those who slept ≤6 h/day had a non-significant trend for increased risk of the composite outcome [hazard ratio (HR), 1.09; 95% confidence interval, 0.99–1.20]. As estimated sleep duration increased, we also noticed a significant trend for a greater risk of the composite outcome [HR of 1.05 (0.99–1.12), 1.17 (1.09–1.25), and 1.41 (1.30–1.53) for 8–9 h/day, 9–10 h/day, and >10 h/day, Ptrend < 0.0001, respectively]. The results were similar for each of all-cause mortality and major cardiovascular events. Daytime nap duration was associated with an increased risk of the composite events in those with over 6 h of nocturnal sleep duration, but not in shorter nocturnal sleepers (≤6 h).
Conclusion
Estimated total sleep duration of 6–8 h per day is associated with the lowest risk of deaths and major cardiovascular events. Daytime napping is associated with increased risks of major cardiovascular events and deaths in those with >6 h of nighttime sleep but not in those sleeping ≤6 h/night.
Keywords: Sleep duration, Naps, Cardiovascular diseases, Mortality
See page 1630 for the editorial comment on this article (doi: 10.1093/eurheartj/ehy772)
Introduction
Sleep is essential to human health, and people spend about a third of their hours sleeping. It is increasingly regarded as an important lifestyle behaviour that can affect cardiovascular disease (CVD) and death.1 Sleep deprivation could increase the risk of cardiovascular outcomes by reduced energy expenditure, up-regulation of appetite, and altered glucose metabolism.2 Some studies also found that people with excessive sleep are at greater risk of CVDs or death.3–5 However, other studies reported contradictory results.6–8 Although several meta-analyses9–11 were conducted, the results were less compelling due to different study types (cross-sectional or prospective study), diverse target populations, variations in reference groups (like 6–8 h, 7–8 h, or 7–9 h), and definitions of sleep durations that were too broad (nocturnal or 24 h). Moreover, most studies were from North America, Europe, Japan, and China. A recent consensus recommendation12 developed by the American Academy of Sleep Medicine (AASM) and the Sleep Research Society (SRS) recommends that the optimal duration of sleep for adults is 7 or more hours per night. It is not clear whether longer (>8 h) sleep duration is associated with lower or increased risk of death and CVD.
Daytime napping is more common in South America, Middle East, some European countries like Greece, and China,13–16 and is considered to be a healthy habit. Most studies on the association between daytime naps and death or CVD have been conducted in select countries,17–21 and little information is available from other parts of the world. Furthermore, the inconsistency of those results makes its influence unclear.
By analysing the data in regions with different sleep patterns (more likely to take naps or not), it is possible to explore whether the effects of total daily sleep duration are similar in regions where daytime naps are common or not. However, actual sleep time is usually difficult to measure precisely in large epidemiological studies due to the lack of feasibility of using objective measurements like polysomnography. In this large-scale, international prospective cohort study where sleep duration was estimated based on the amount of time in bed, we investigated the associations of estimated total daily sleep duration (primary exposure) with all-cause mortality and major cardiovascular events among individuals aged 35–70 years, and whether the associations are consistent in different regions of world. We also examined the effects of different sleep patterns (nocturnal sleep of different durations with or without daytime naps). Moreover, we assessed the effects of daytime napping on deaths and CVD.
Methods
Study design and participants
The Prospective Urban Rural Epidemiology (PURE) study included participants aged 35–70 years from 21 countries with different income levels in seven geographic regions (North America and Europe, South America, the Middle East, South Asia, Southeast Asia, China, and Africa). These countries were classified based on gross national income per capita from the World Bank classification at the beginning of the study. There were four high-income countries (Canada, Sweden, Saudi Arabia, and United Arab Emirates), 12 middle-income countries (Argentina, Brazil, Chile, China, Colombia, Iran, Malaysia, Palestine, Philippines, Poland, South Africa, and Turkey), and five low-income countries (Bangladesh, India, Pakistan, Tanzania, and Zimbabwe). The detailed description of study design, participant selection, and methods has been published previously.22 The study was initiated and co-ordinated by the Population Health Research Institute (PHRI; Hamilton, Ontario, Canada) and was approved by institutional research ethics boards at all sites.
Standardized questionnaires (same questions using local languages in different countries) were used to obtain information about demographic factors, socioeconomic status, lifestyle behaviours (sleep duration, smoking, alcohol consumption, physical activity, and diet), disease history, family history of diseases, and medication use at baseline. As it is not feasible to accurately measure the actual sleep time using objective methods like polysomnography in large studies, sleep duration was recorded by asking the following questions: (i) during your longest or nocturnal sleep period, what time do you normally go to bed and wake up (time was recorded in 24 h format); (ii) do you usually take naps/siestas and if yes, how long (min) the nap duration is. The estimated nocturnal sleep duration was defined as the time space between bedtime and waking up time and napping duration was estimated by self-reported daytime sleep time. Estimated total daily sleep duration was the sum of the two parameters. In general, actual sleep time is about 85% of the time in bed23 and such information is more appropriate to make public health recommendations. Physical activity was assessed with the International Physical Activity Questionnaire24 and grouped based on the metabolic equivalent of task (MET) into low (<600 MET × minutes per week), moderate (600–3000 MET × minutes per week), and high (>3000 MET × minutes per week) activity. Diet pattern was recorded using country- or region-specific validated food frequency questionnaires.25,26 Weight, height, waist and hip circumferences, and blood pressure were measured by using a standardized protocol. The follow-up of each participant occurred at least every 3 years after baseline recruitment either by telephone or by a face-to-face interview with the local research team. Standardized case-report forms were used to collect data on deaths, cardiovascular events, and other health outcomes. Medical records, death certificates, and verbal autopsies were used to ensure the accuracy of data. All deaths and major cardiovascular events were adjudicated centrally within each country by trained physicians utilizing common definitions (Supplementary material online, Appendix).
In the present analyses, we include all outcome events known until September 2017. A total of 161 241 participants have at least one follow-up, of which 21 566 people from India were recruited in the initial pilot study prior to the decision to include questions on sleep. Among the remaining individuals, 137 337 (98.3%) provided sleep information at baseline and 129 939 (93.0%) participants had estimated sleep durations [between 4–12 h per night and 0–3 h of naps per day, which were considered to be plausible; 7180 (5.1%) slept <4 or >12 h/night and 199 (0.1%) napped >3 h/day] and complete data on age and gender. We also excluded 1326 participants (0.9%) with unavailable last follow-up date and 11 981 participants (8.6%) with pre-existing CVDs, cancers, human immunodeficiency virus infection, or acquired immune deficiency syndrome (HIV/AIDS) to minimize reverse causality from the potential effects of illnesses on sleep. A total of 116 632 individuals were included in the primary analysis (Supplementary material online, Appendix Figure S1).
Outcomes
The primary outcome was time to all-cause mortality plus major cardiovascular events (defined as fatal cardiovascular events and non-fatal myocardial infarction, stroke, and heart failure). All-cause mortality and major cardiovascular events were also examined separately.
Statistical analysis
Baseline characteristics of participants were summarized by categories of estimated total daily sleep duration. The event rates (per 1000 person-years) and the corresponding 95% confidence intervals (CIs) were computed for different sleep duration groups. Restricted cubic splines were used to explore the shape of the association between estimated total daily sleep duration and the outcomes (created by SAS LGTPHCURV9 Macro). On the basis of the splines and previous studies,9,10 we categorized the estimated total daily sleep duration into five groups (≤6 h, 6–8 h which was used as the reference, 8–9 h, 9–10 h, and >10 h). To quantify the associations between estimated total daily sleep duration and time to the occurrence of the composite outcome and all-cause mortality, Cox frailty models with random intercepts for centre were applied to calculate the adjusted hazard ratios (HRs) and to account for clustering within centres (Supplementary material online, Appendix for more details).27 As for major CVDs, we did the competing risk analyses using cause-specific hazard models28,29 given that non-cardiovascular deaths occurring in the absence of major cardiovascular events are the competing risks. The Fine–Gray model was further adopted for analysing competing risks as sensitivity analysis (Supplementary material online, Appendix Table S1). In the minimally adjusted models, we adjusted only for age and sex. Further, the fully adjusted models included age, sex, educational attainment, smoking status (current/former vs. never smoker), drinking status (drinker vs. non-drinker), urban or rural residency, family history of CVDs (coronary heart disease and stroke), history of diabetes (defined as self-reported diabetes or taking medications for diabetes), hypertension (defined as systolic blood pressure >140 mmHg, diastolic blood pressure >90 mmHg, self-reported hypertension or taking medications for hypertension), chronic obstructive pulmonary disease, and depression. Additionally, we investigated the effects of different sleep patterns (≤6 h, 6–8 h, or >8 h of estimated nocturnal sleep, and taking daytime naps or not) on these outcomes. For the effects of daytime nap duration, an interaction test between estimated nocturnal sleep duration and daytime napping was performed and it showed a significant interaction for all three outcomes. Stratified models by estimated nocturnal sleep duration (≤6 h/night or >6 h/night) were utilized to examine the associations between daytime napping and events.
Given that taking daytime naps are more common in some countries, we assessed the consistency of associations between estimated total sleep duration and events separately in those regions where naps were more or less common. In our study, regular naps were more common in the Middle East, China, Southeast Asia, and South America (percentage of taking nap: 60.5%, 48.0%, 35.5%, and 34.4%, respectively compared with an average of 25.9% in other countries; Supplementary material online, Appendix Table S2). Furthermore, considering that the need for sleep might increase with increased age, we examined whether the effects of estimated total sleep duration on events were consistent in different age groups by using the median age as the cut-off (<50 years old vs. ≥50 years old). Stratified analysis by employment status (working vs. unemployed) was also performed.
In addition, to address concerns related to potential reverse causality, we re-examined the effects of estimated total daily sleep duration after excluding less healthy individuals (i.e. those with known disability, symptoms, or those with history of prior non-cardiovascular and non-cancer diseases). Further, we performed sensitivity analysis by excluding those who had events (n = 1368) in the first 2 years of follow-up. Given that obesity [defined as body mass index (BMI) ≥30 kg/m2], particularly for severe obesity (≥40 kg/m2), has been shown strongly associated with sleep apnea,30,31 sensitivity analysis by additional adjustment for BMI of ≥30 as surrogate for sleep apnoea to correct for its effects was done. Moreover, to rule out the effects of sleep disorders like insomnia, we performed sensitivity analyses by exclusion of those who were of high suspicion of sleep disorders (taking sleep pills, BMI ≥40 kg/m2 or feeling depressed for ≥2 weeks in a row in the past 1 year). We also removed potential shift workers (n = 6403, those who woke up before 4:00 AM or in the afternoon, or went to bed before 6:00 PM or after 4:00 AM) to rule out the effects of night shifts. The fully adjusted models were not adjusted for BMI because it might be part of the causal pathway2,32 and is associated with diabetes, CVDs, and deaths. We conducted sensitivity analysis by also adjusting for BMI, physical activity, and diet. Additionally, to examine the specificity of the associations between estimated daily sleep duration and total mortality or major cardiovascular events, we assessed the association of estimated daily sleep duration with injuries, which might be related to tiredness from sleep deprivation. All statistical analyses were done with SAS version 9.4 (Cary, NC, USA) and STATA 15.1.
Results
During a median follow-up of 7.8 years [interquartile range (IQR) 5.1–9.2], a total of 7342 individuals died or had a major cardiovascular event (4381 participants died and 4365 had a major cardiovascular event). Compared with those who had an estimated sleep duration of 6–8 h per day, individuals who slept more than 9 h per day were more often ≥50 years old, females, smokers, and hypertensives, were less educated, and were more likely to live in rural areas (Table 1). People with an estimated sleep duration of ≤6 h per day had higher BMI and waist-to-hip ratio, less likely to consume alcohol, and more likely to have diabetes. There were more participants with shorter- or longer-estimated sleep duration reporting symptoms of depression and having at least one prior health condition (disability, symptom or history non-cardiovascular, and non-cancer disease). The proportion of population taking sleep medications was 1.6% in the overall population, but this was much higher (6.3%) in high-income countries. The median estimated total sleep duration in the population was 8.0 h (IQR 7.0–9.0) per day.
Table 1.
Baseline characteristics of participants by estimated total sleep duration per day
| ≤6 h (n = 11 108) | 6–8 h (n = 50 041) (Reference group) | 8–9 h (n = 31 003) | 9–10 h (n = 16 316) | >10 h (n = 8164) | |
|---|---|---|---|---|---|
| Age (years), mean (SD) | 50.2 (9.5) | 50.0 (9.5) | 50.6 (9.9) | 51.1 (10.2) | 51.6 (10.5) |
| ≥50 years (%) | 5579 (50.2) | 25 040 (50.0) | 16 372 (52.8) | 8853 (54.3) | 4521 (55.4) |
| Male (%) | 5051 (45.5) | 21 743 (43.5) | 12 412 (40.0) | 6329 (38.8) | 3238 (39.7) |
| Urban resident (%) | 6977 (62.8) | 29 848 (59.7) | 16 017 (51.7) | 7351 (45.1) | 3516 (43.1) |
| Body mass index (kg/m2), mean (SD) | 27.2 (5.5) | 26.3 (5.0) | 25.7 (4.9) | 25.7 (5.0) | 25.9 (5.6) |
| Waist to hip ratio, mean (SD) | 0.885 (0.086) | 0.877 (0.084) | 0.870 (0.080) | 0.869 (0.079) | 0.873 (0.084) |
| Education (Trade, college, or university, %) | 2325 (21.0) | 12 314 (24.6) | 5935 (19.2) | 2242 (13.8) | 858 (10.5) |
| Physical activity, MET × min/week | |||||
| Low (<600) | 2562/10 379 (24.7) | 8328/47 645 (17.5) | 4429/29 540 (15.0) | 2464/15 317 (16.1) | 1499/7299 (20.5) |
| Moderate (600–3000) | 3548/10 379 (34.2) | 17 276/47 645 (36.3) | 11 573/29 540 (39.2) | 6133/15 317 (40.0) | 2864/7299 (39.2) |
| High (>3000) | 4269/10 379 (41.1) | 22 041/47 645 (46.3) | 13 538/29 540 (45.8) | 6720/15 317 (43.9) | 2936/7299 (40.2) |
| AHEI score, mean (SD) | 34.8 (8.5) | 34.7 (8.4) | 35.2 (8.3) | 35.1 (8.3) | 34.7 (8.4) |
| Smoker (current and former, %) | 3441 (31.1) | 16 178 (32.5) | 9730 (31.6) | 5273 (32.6) | 2902 (35.8) |
| Drinker (current and former, %) | 2215 (20.3) | 16 379 (33.2) | 10 041 (32.7) | 5152 (31.9) | 2952 (36.6) |
| Hypertension (%) | 4272 (38.5) | 19 100 (38.2) | 12 411 (40.1) | 6756 (41.4) | 3581 (43.9) |
| Diabetes (%) | 1188 (10.7) | 3316 (6.6) | 1739 (5.6) | 984 (6.0) | 568 (7.0) |
| Depression (%) | 1056 (9.5) | 3741 (7.5) | 1975 (6.4) | 1259 (7.8) | 917 (11.3) |
| Chronic obstructive pulmonary disease (%) | 81 (0.7) | 318 (0.6) | 188 (0.6) | 121 (0.7) | 77 (0.9) |
| Health conditiona (%) | 8196 (73.8) | 35 739 (71.4) | 21 688 (70.0) | 11 860 (72.7) | 6441 (78.9) |
| No. of participants taking nap (%) | 2279 (20.5) | 13 723 (27.4) | 13 647 (44.0) | 9790 (60.0) | 5842 (71.6) |
| Duration of daytime naps (min), median (q1–q3) | 30 (30–60) | 45 (30–60) | 60 (30–60) | 60 (40–90) | 60 (60–120) |
| Total estimated sleep duration (h), median (q1–q3) | 5.5 (5.0–6.0) | 7.5 (7.0–8.0) | 9.0 (8.5–9.0) | 9.5 (9.5–10.0) | 11.0 (10.5–11.5) |
AHEI, alternate healthy eating index; SD, standard deviation.
aHealth condition is defined as having any disabilities, symptoms, or history diseases.
Disabilities: having trouble grasping/handling with fingers, walking about (or require a walking stick cane/walker), bending down and picking up objects, reading, seeing the individual grains of rice/corn on the plate or a person from across the room (with glass worn), speaking, or hearing in a normal conversation. Symptoms: having experienced any of the following in the last 6 months: chest pain or breathlessness with usual activity, cough (≥2 weeks), sputum while coughing, blood in sputum, wheezing or whistling in the chest, early morning cough with chest tightness, diarrhoea (≥3 days), vomiting, loss of appetite, painful or bleeding teeth/gums, jaundice, burning while passing urine, swelling of feet or face, blood in urine, involuntary weight loss of >3 kg. History diseases: having been diagnosed with diabetes, hypertension (or high blood pressure), hepatitis (or jaundice), chronic obstructive pulmonary disease, asthma, tuberculosis, malaria, or Chagas.
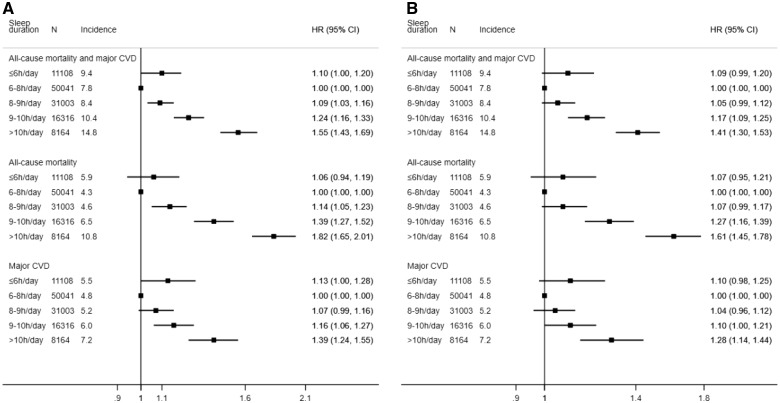
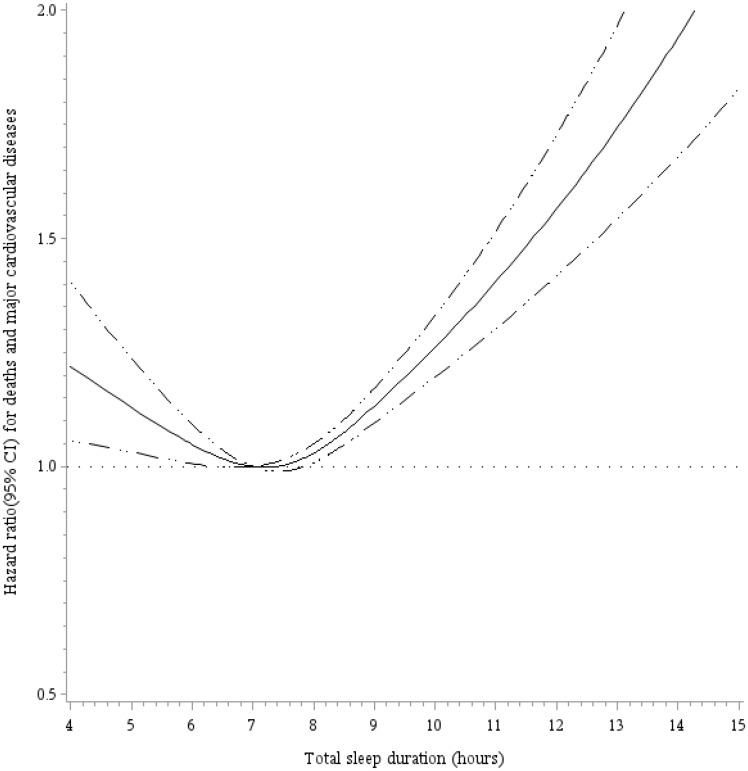
The associations of estimated total daily sleep duration with all-cause mortality and major cardiovascular events are illustrated in Figure 1. Participants with an estimated sleep duration of 6–8 h per day had the lowest incidences of all outcomes. After adjustment for age, sex, and centre (as random effect), both shorter (≤6 h/day) and longer (>8 h/day) estimated daily sleep durations were associated with higher risks of major cardiovascular events, and the combination of all-cause mortality and major cardiovascular events. Risk of mortality was significantly higher in those with longer sleep durations, and high (but not statistically significant) in those with shorter sleep durations. In the fully adjusted models, the associations were moderately attenuated but still indicated a J-shaped relationship between estimated total sleep duration and each of the three outcomes. Restricted cubic splines for estimated total sleep duration and events are shown in Figure 2 and Supplementary material online, Appendix Figure S2, and illustrate these observations.
Figure 1.
Associations of estimated total sleep duration per day with all-cause mortality and major cardiovascular events. (A) Adjusted for age, sex, and centre as random effect. (B) Adjusted for age, sex, education attainment, smoking status, drinking status, urban or rural residency, family history of cardiovascular diseases (coronary heart disease and stroke), the history of diabetes, hypertension and chronic obstructive pulmonary disease, depression, and centre as random effect. CI, confidence interval; CVD, cardiovascular disease; HR, hazard ratio. Incidence: per 1000 person-years.
Figure 2.
Restricted spline curve for association between estimated total daily sleep duration and the composite of total deaths and major cardiovascular diseases. Adjusted for age, sex, education attainment, smoking status, drinking status, urban or rural residency, geographic regions, family history of cardiovascular diseases (coronary heart disease and stroke), the history of diabetes, hypertension and chronic obstructive pulmonary disease, and depression.
The results were consistent when examined by region, employment status, and in those <50 years old and ≥50 years old (Table 2; Supplementary material online, Appendix Table S3). The J-shaped association of estimated total sleep duration with events was consistently observed both in regions where daytime napping is common and where it is less common. The association of longer sleep durations per day with composite outcome was more pronounced in those ≥50 years of age. Sensitivity analysis by excluding those with disabilities, symptoms or prevalent diseases did not alter our results. Additional sensitivity analysis by excluding events observed in the first 2 years indicated consistent results in the association of sleep with events recorded in the subsequent years. The results did not change by additional adjustment for those with high likelihood of sleep apnoea (obesity), or by exclusion of those who were highly suspected of sleep disorders (e.g. those taking sleeping tablets), or by exclusion of potential shift workers. The association for longer estimated sleep duration was slightly attenuated but did not alter when further adjusted for BMI, physical activity, and diet (Supplementary material online, Appendix Table S4). In addition, to address the specificity of the association, we examined the association of total daily sleep duration with injuries and found only shorter (but not longer) estimated sleep duration was associated with increased risk of injuries (Supplementary material online, Appendix Table S5).
Table 2.
Association of estimated total sleep duration per day with the composite of deaths and cardiovascular diseases by region and by age
| Hazard ratioa (95% CI) |
P for interaction | |||||
|---|---|---|---|---|---|---|
| ≤6 h | 6–8 h | 8–9 h | 9–10 h | >10 h | ||
| Overall (n = 116 632) | ||||||
| Incidence (per 1000 person-years, 95% CI) | 9.4 (8.7–10.2) | 7.8 (7.5–8.1) | 8.4 (8.0–8.7) | 10.4 (9.8–11.0) | 14.8 (13.8–15.8) | NA |
| Fully adjusted model | 1.09 (0.99–1.20) | 1.00 (Ref) | 1.05 (0.99–1.12) | 1.17 (1.09–1.25) | 1.41 (1.30–1.53) | |
| Regions | ||||||
| Regions where naps are common (Middle East, China, Southeast Asia, and South America, n=83 322) | 0.42 | |||||
| Incidence (per 1000 person-years, 95% CI) | 9.1 (8.3–10.0) | 7.5 (7.2–7.9) | 7.8 (7.4–8.3) | 9.7 (9.0–10.3) | 12.5 (11.5–13.7) | |
| Fully adjusted model | 1.10 (0.98–1.23) | 1.00 (Ref) | 1.02 (0.94–1.09) | 1.13 (1.04–1.24) | 1.33 (1.20–1.47) | |
| Other regions where naps are uncommon (North America and Europe, South Asia, and Africa, n = 33 310) | ||||||
| Incidence (per 1000 person-years, 95% CI) | 10.3 (8.9–12.0) | 8.2 (7.7–8.7) | 9.9 (9.1–10.8) | 12.9 (11.6–14.3) | 19.9 (17.9–22.1) | |
| Fully adjusted model | 1.08 (0.91–1.27) | 1.00 (Ref) | 1.14 (1.03–1.27) | 1.24 (1.09–1.41) | 1.57 (1.36–1.81) | |
| Age (years) | ||||||
| <50 years old (n = 56 267) | 0.76 | |||||
| Incidence (per 1000 person-years, 95% CI) | 4.4 (3.7–5.2) | 3.8 (3.5–4.1) | 4.0 (3.7–4.4) | 4.7 (4.2–5.3) | 7.2 (6.2–8.3) | |
| Fully adjusted model | 1.14 (0.94–1.38) | 1.00 (Ref) | 1.04 (0.92–1.18) | 1.12 (0.96–1.30) | 1.40 (1.17–1.67) | |
| ≥50 years old (n = 60 365) | ||||||
| Incidence (per 1000 person-years, 95% CI) | 14.3 (13.1–15.7) | 11.7 (11.2–12.2) | 12.3 (11.7–12.9) | 15.2 (14.3–16.2) | 20.9 (19.4–22.6) | |
| Fully adjusted model | 1.06 (0.96–1.19) | 1.00 (Ref) | 1.08 (1.00–1.15) | 1.26 (1.16–1.37) | 1.54 (1.41–1.70) | |
CI, confidence interval; NA, not applicable.
When stratified by region, we adjusted for age, sex, education attainment, smoking status, drinking status, urban or rural residency, family history of cardiovascular diseases (coronary heart disease and stroke), the history of diabetes, hypertension and chronic obstructive pulmonary disease, depression, and centre as random effect. Age was removed from the model when stratified by age.
As for the sleep patterns, compared with those who slept 6–8 h at night and did not take naps during the day, individuals with same estimated duration of nocturnal sleep plus daytime naps (mean 8.4 h/day), shorter nocturnal sleepers without daytime naps (mean 5.4 h/day), and longer nocturnal sleepers (>8 h per night with or without daytime napping, mean 9.6 h/day) were associated with increased risk of death and major CVDs. Those who slept ≤6 h at night but took daytime naps (total mean 6.4 h/day) had a non-significantly increased risk compared to those who slept for 6–8 h only at night (Supplementary material online, Appendix Figure S3).
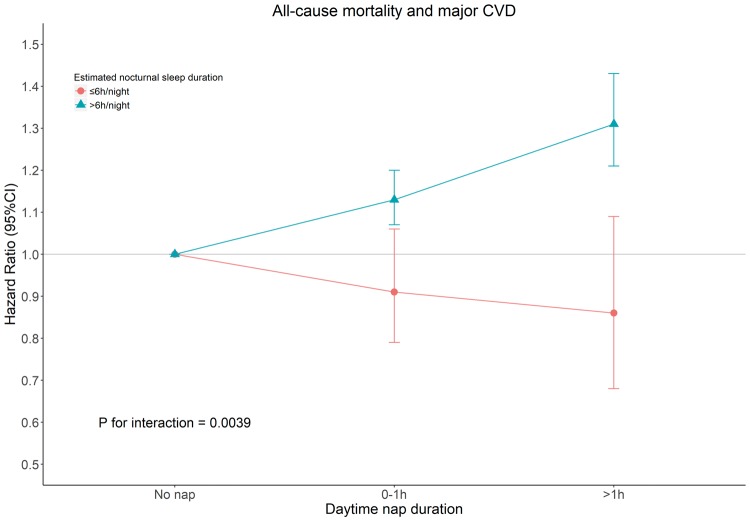
When analysing the impact of daytime naps, those who napped had a graded increase in risk of composite outcome regardless of employment status, and separate outcomes (Supplementary material online, Appendix Tables S6 and S7). However, there was a significant interaction between nap duration and estimated nocturnal sleep duration for all outcomes. After stratification by estimated nocturnal sleep duration (≤6 h/night or >6 h/night), the association between naps and greater risk of outcomes was only observed in those who slept at least 6 h at night but not in those with shorter duration of nocturnal sleep (Figure 3).
Figure 3.
The effects of nap duration on the risk of the composite of deaths and major cardiovascular events in those with different estimated durations of nocturnal sleep. Adjusted for age, sex, education attainment, smoking status, drinking status, urban or rural residency, family history of cardiovascular diseases (coronary heart disease and stroke), the history of diabetes, hypertension and chronic obstructive pulmonary disease, depression, and centre as random effect. CI, confidence interval; CVD, cardiovascular disease.
Discussion
In this global prospective cohort study, we observed a J-shaped association between estimated total daily sleep duration and mortality and major cardiovascular events. An estimated sleep duration of 6–8 h per day was associated with the lowest risk of deaths and major cardiovascular events. Longer sleep durations were associated with elevated risk of the composite outcome and shorter durations showed a non-significant trend for increased risk of the composite outcome. Daytime napping was associated with higher risks of all outcomes in those with sufficient or longer sleep at night (i.e. over 6 h of estimated nocturnal sleep) but not in those with shorter estimation of nocturnal sleep (i.e. under 6 h per night). Individuals with short sleep at night appeared to mitigate their risks if they napped during the day.
Insufficient sleep is of importance in today’s ‘24 h/7 days’ modern society, where long hours at work, or for social and leisure activities inevitably limit sleep time.1 The recommended minimum duration of sleep is 7 h/day for cardiovascular health,12 but there is no recommendation for what an upper limit of sleep duration is for optimal health.
The association of short estimated sleep duration was relatively weaker in our analysis than some previous findings. Those discrepancies could be possible in light of the various definitions of short sleep. The association seems stronger in studies4,33 with a short sleep of ≤5 h per day. A recent meta-analysis reported no association between short duration of sleep and total CVD10 and another showed weaker association for the reduction of sleep duration than increment of sleep time.34 The Shanghai Women’s and Men’s Health Studies35 (n = 113 138) separately evaluated the associations of sleep duration per day with CVD (4–5 h vs. 7 h: HR 1.05, 95% CI 0.87–1.26; 6 h vs. 7 h: HR 1.10, 95% CI 0.94–1.29) and all-cause mortality (6 h vs. 7 h: HR 1.06, 95% CI 0.97–1.16) and showed modest but similarly non-significant increases in events with short duration of sleep, comparable to the magnitude of excess risk that we observed. Consistent with previous studies,9,10,34,36 we observed that longer estimated sleep duration had a stronger and graded association with mortality and CVD. It is possible that those who sleep longer may have underlying conditions (which may not yet be clinically apparent) that in themselves increase the risk of CVD and mortality, indicating that prolonged sleep could be a marker of illness. We reanalysed the data among those who did not have disabilities at baseline, prevalent diseases, or symptoms. Such analyses resulted in similar findings. Furthermore, excluding those who had events within the first 2 years also did not alter the results. This suggests that sleep duration per se may be associated with increased risks but causality cannot be definitively proven from this or other observational studies (and randomized studies of different sleep durations may be difficult to conduct). In addition, we found that the associations were consistent in populations from different regions, which was similar with the results of a meta-analysis.10
We found that daytime nap duration was associated with a graded increase in risk of all outcomes in those who slept over 6 h per night. The association between daytime naps and an elevated risk of mortality was also reported in previous longitudinal studies21,37 and meta-analysis.38 Compared with sleep duration per night or per day, fewer studies have assessed the associations between naps and mortality or cardiovascular events, and no recommendation with respect to daytime nap exists. Individuals nap in the daytime for several reasons. Naps may compensate for sleep loss during the night among those who stay up late for work or leisure, or naps may be related to cultural factors. It could also be a countermeasure for daytime sleepiness or fatigue which might be the early clinical manifestations of underlying diseases.39–41 Irrespective of the duration, daytime napping elevated the risk of deaths or major CVDs if individuals got adequate or long nocturnal sleep; but it might be beneficial if individuals slept less at night (≤6 h/night) and compensated for lack of nocturnal sleep. Our findings of the possible protective effects of daytime naps among those with short estimated night time sleep is in keeping with results from a prior study.42
Some mechanisms have been proposed to explain the increased risk of CVDs among those with shorter sleep durations. Evidence has shown that sleep debt regulates the metabolic and endocrine hormones, like insulin and leptin, leading to alterations of appetite and glucose metabolism that may accelerate the development of obesity and diabetes.2,43,44 Alternatively, excessive sleep duration may be a subclinical marker of those with undiagnosed diseases.45
Increased total sleep time or taking daytime naps among those with adequate duration of nocturnal sleep might be early indicators of poorer health and help identify those at higher risk of CVD and mortality. Therefore, including questions about sleep patterns (duration and status of daytime naps) in the clinical history may be of value in identifying higher risk individuals.
Our study has several limitations. First, we estimated the nocturnal sleep duration based on the time space between going to bed and waking up. The potential misclassifications might occur by using time in bed as substitute for actual sleep duration. However, the use of objective methods (like polysomnography) to accurately measure the sleep time is usually not feasible in large studies of general populations which is a common limitation of sleep-related epidemiological studies. Inaccuracies in estimating the duration of sleep would tend to dilute the associations between sleep duration and events and so the true effects of sleep duration may be more marked than what we have observed in our study. Previous studies46,47 have shown subjective estimates of sleep duration and more precise measurements like sleep diaries, actigraphy, and polysomnography are highly correlated. Additionally, a large study23 (n = 2162) using polysomnography has shown high averaged sleep efficiency (actual sleep time divided by time in bed) in general population, which indicates the high correlation between sleep duration and time in bed. Second, we assumed that durations of night time and daytime naps did not change during the follow-up period. If such changes occurred, they would have weakened the contrast between groups and the observed associations would have been underestimated. Third, we did not collect sleep disorders (like apnoea and insomnia) which can impact on sleep and might also affect health outcomes.48,49 We attempted to correct for sleep disorders by using a BMI of ≥30 kg/m2 as surrogate for sleep apnoea and exclusion of those who were highly suspected of sleep disorders and those were less healthy. Our results were unchanged. Last, as with other observational studies, we cannot completely rule out the possible confounding from unmeasured factors despite the fact that we had adjusted extensively for participant characteristics. Ideally large randomized trials of different sleep durations would be desirable from a methodologic perspective but how they could be designed to be feasible is not presently clear. We hope our paper will stimulate others to consider the designs of future studies on this question.
Our study shows a J-shaped association between estimated total daily sleep duration and all-cause mortality and cardiovascular events. An estimated total sleep duration of 6–8 h per day is associated with the lowest risk. Daytime naps are associated with excessive risks of major cardiovascular events and deaths except in those with less nocturnal sleep suggesting that this may be a compensatory mechanism when nocturnal sleep is short.
Funding
S.Y. is supported by M.W.B. endowed chair of the Heart and Stroke Foundation of Ontario. The PURE Study is an investigator-initiated study that is funded by the Population Health Research Institute, the Canadian Institutes of Health Research (CIHR), Heart and Stroke Foundation of Ontario, Support from CIHR’s Strategy for Patient Oriented Research (SPOR), through the Ontario SPOR Support Unit, as well as the Ontario Ministry of Health and Long-Term Care and through unrestricted grants from several pharmaceutical companies [with major contributions from AstraZeneca (Canada), Sanofi-Aventis (France and Canada), Boehringer Ingelheim (Germany and Canada), Servier, and GlaxoSmithKline], and additional contributions from Novartis and King Pharma and from various national or local organizations in participating countries; these include: Argentina: Fundacion ECLA (Estudios Clínicos Latino America); Bangladesh: Independent University, Bangladesh and Mitra and Associates; Brazil: Unilever Health Institute, Brazil; Canada: Public Health Agency of Canada and Champlain Cardiovascular Disease Prevention Network; Chile: Universidad de la Frontera; China: National Center for Cardiovascular Diseases; Colombia: Colciencias [grant number: 6566-04-18062]; India: Indian Council of Medical Research; Malaysia: Ministry of Science, Technology and Innovation of Malaysia [grant numbers: 100-IRDC/BIOTEK 16/6/21 (13/2007), 07-05-IFN-BPH 010], Ministry of Higher Education of Malaysia [grant number: 600—RMI/LRGS/5/3 (2/2011)], Universiti Teknologi MARA, Universiti Kebangsaan Malaysia (UKM-Hejim-Komuniti-15-2010); occupied Palestinian territory: the United Nations Relief and Works Agency for Palestine Refugees in the Near East (UNRWA), occupied Palestinian territory; International Development Research Centre (IDRC), Canada; Philippines: Philippine Council for Health Research & Development (PCHRD); Poland: Polish Ministry of Science and Higher Education [grant number 290/W-PURE/2008/0], Wroclaw Medical University; Saudi Arabia: Saudi Heart Association, The Deanship of Scientific Research at King Saud University, Riyadh, Saudi Arabia (Research group number: RG-1436-013); South Africa: The North-West University, SANPAD (SA and Netherlands Programme for Alternative Development), National Research Foundation, Medical Research Council of SA, The SA Sugar Association (SASA), Faculty of Community and Health Sciences (UWC); Sweden: Grants from the Swedish state under the Agreement concerning research and education of doctors; the Swedish Heart and Lung Foundation; the Swedish Research Council; the Swedish Council for Health, Working Life and Welfare, King Gustaf V’s and Queen Victoria Freemasons Foundation, AFA Insurance; Turkey: Metabolic Syndrome Society, AstraZeneca, Turkey, Sanofi Aventis, Turkey; United Arab Emirates: Sheikh Hamdan Bin Rashid Al Maktoum Award For Medical Sciences and Dubai Health Authority, Dubai UAE. The work of C.W. at McMaster University is supported by China Scholarship Council (CSC). G.H. from Medical College of Georgia, Augusta University gave helpful comments on the paper.
Conflict of interest: none declared.
Supplementary Material
References
- 1. St-Onge MP, Grandner MA, Brown D, Conroy MB, Jean-Louis G, Coons M, Bhatt DL.. Sleep duration and quality: impact on lifestyle behaviors and cardiometabolic health: a scientific statement from the American Heart Association. Circulation 2016;134:e367–e386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Knutson KL, Van Cauter E.. Associations between sleep loss and increased risk of obesity and diabetes. Ann N Y Acad Sci 2008;1129:287–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Qureshi AI, Giles WH, Croft JB, Bliwise DL.. Habitual sleep patterns and risk for stroke and coronary heart disease: a 10-year follow-up from NHANES I. Neurology 1997;48:904–911. [DOI] [PubMed] [Google Scholar]
- 4. Ikehara S, Iso H, Date C, Kikuchi S, Watanabe Y, Wada Y, Inaba Y, Tamakoshi A.. Association of sleep duration with mortality from cardiovascular disease and other causes for Japanese men and women: the JACC study. Sleep 2009;32:295–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kim Y, Wilkens LR, Schembre SM, Henderson BE, Kolonel LN, Goodman MT.. Insufficient and excessive amounts of sleep increase the risk of premature death from cardiovascular and other diseases: the Multiethnic Cohort Study. Prev Med 2013;57:377–385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Stone KL, Ewing SK, Ancoli-Israel S, Ensrud KE, Redline S, Bauer DC, Cauley JA, Hillier TA, Cummings SR.. Self-reported sleep and nap habits and risk of mortality in a large cohort of older women. J Am Geriatr Soc 2009;57:604–611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hall MH, Smagula SF, Boudreau RM, Ayonayon HN, Goldman SE, Harris TB, Naydeck BL, Rubin SM, Samuelsson L, Satterfield S, Stone KL, Visser M, Newman AB.. Association between sleep duration and mortality is mediated by markers of inflammation and health in older adults: the health, aging and body composition study. Sleep 2015;38:189–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Jung K-I, Song C-H, Ancoli-Israel S, Barrett-Connor E.. Gender differences in nighttime sleep and daytime napping as predictors of mortality in older adults: the Rancho Bernardo study. Sleep Med 2013;14:12–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Cappuccio FP, D'Elia L, Strazzullo P, Miller MA.. Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep 2010;33:585–592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Cappuccio FP, Cooper D, D'Elia L, Strazzullo P, Miller MA.. Sleep duration predicts cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. Eur Heart J 2011;32:1484–1492. [DOI] [PubMed] [Google Scholar]
- 11. Krittanawong C, Tunhasiriwet A, Wang Z, Zhang H, Farrell AM, Chirapongsathorn S, Sun T, Kitai T, Argulian E.. Association between short and long sleep durations and cardiovascular outcomes: a systematic review and meta-analysis. Eur Heart J Acute Cardiovasc Care 2017; doi: 10.1177/2048872617741733. [DOI] [PubMed] [Google Scholar]
- 12. Watson NF, Badr MS, Belenky G, Bliwise DL, Buxton OM, Buysse D, Dinges DF, Gangwisch J, Grandner MA, Kushida C, Malhotra RK, Martin JL, Patel SR, Quan SF, Tasali E, Twery M, Croft JB, Maher E, Barrett JA, Thomas SM, Heald JL.. Joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society on the recommended amount of sleep for a healthy adult: methodology and discussion. Sleep 2015;38:1161–1183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Burazeri G, Gofin J, Kark JD.. Siesta and mortality in a Mediterranean population: a community study in Jerusalem. Sleep 2003;26:578–584. [DOI] [PubMed] [Google Scholar]
- 14. Bouscoulet LT, Vázquez-García JC, Muiño A, Márquez M, López MV, de Oca MM, Talamo C, Valdivia G, Pertuze J, Menezes AMB, Pérez-Padilla R.. Prevalence of sleep related symptoms in four Latin American cities. J Clin Sleep Med 2008;4:579–585. [PMC free article] [PubMed] [Google Scholar]
- 15. Fang W, Li Z, Wu L, Cao Z, Liang Y, Yang H, Wang Y, Wu T.. Longer habitual afternoon napping is associated with a higher risk for impaired fasting plasma glucose and diabetes mellitus in older adults: results from the Dongfeng-Tongji cohort of retired workers. Sleep Med 2013;14:950–954. [DOI] [PubMed] [Google Scholar]
- 16. Naska A, Oikonomou E, Trichopoulou A, Psaltopoulou T, Trichopoulos D.. Siesta in healthy adults and coronary mortality in the general population. Arch Intern Med 2007;167:296–301. [DOI] [PubMed] [Google Scholar]
- 17. Bursztyn M, Stessman J.. The siesta and mortality: twelve years of prospective observations in 70-year-olds. Sleep 2005;28:345–347. [PubMed] [Google Scholar]
- 18. Tanabe N, Iso H, Seki N, Suzuki H, Yatsuya H, Toyoshima H, Tamakoshi A.. Daytime napping and mortality, with a special reference to cardiovascular disease: the JACC study. Int J Epidemiol 2010;39:233–243. [DOI] [PubMed] [Google Scholar]
- 19. Lan TY, Lan TH, Wen CP, Lin YH, Chuang YL.. Nighttime sleep, Chinese afternoon nap, and mortality in the elderly. Sleep 2007;30:1105–1110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Wang C, Hao G, Bo J, Li W.. Correlations between sleep patterns and cardiovascular diseases in a Chinese middle-aged population. Chronobiol Int 2017;34:601–608. [DOI] [PubMed] [Google Scholar]
- 21. Leng Y, Wainwright NW, Cappuccio FP, Surtees PG, Hayat S, Luben R, Brayne C, Khaw KT.. Daytime napping and the risk of all-cause and cause-specific mortality: a 13-year follow-up of a British population. Am J Epidemiol 2014;179:1115–1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Teo K, Chow CK, Vaz M, Rangarajan S, Yusuf S.. The Prospective Urban Rural Epidemiology (PURE) study: examining the impact of societal influences on chronic noncommunicable diseases in low-, middle-, and high-income countries. Am Heart J 2009;158:1–7.e1. [DOI] [PubMed] [Google Scholar]
- 23. Haba-Rubio J, Marques-Vidal P, Andries D, Tobback N, Preisig M, Vollenweider P, Waeber G, Luca G, Tafti M, Heinzer R.. Objective sleep structure and cardiovascular risk factors in the general population: the HypnoLaus Study. Sleep 2015;38:391–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Craig C, Marshall A, Sjöström M, Bauman A, Booth M, Ainsworth B, Pratt M, Ekelund U, Yngve A, Sallis J, Oja P.. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 2003;35:1381–1395. [DOI] [PubMed] [Google Scholar]
- 25. Dehghan M, Mente A, Zhang X, Swaminathan S, Li W, Mohan V, Iqbal R, Kumar R, Wentzel-Viljoen E, Rosengren A, Amma LI, Avezum A, Chifamba J, Diaz R, Khatib R, Lear S, Lopez-Jaramillo P, Liu X, Gupta R, Mohammadifard N, Gao N, Oguz A, Ramli AS, Seron P, Sun Y, Szuba A, Tsolekile L, Wielgosz A, Yusuf R, Hussein Yusufali A, Teo KK, Rangarajan S, Dagenais G, Bangdiwala SI, Islam S, Anand SS, Yusuf S.. Associations of fats and carbohydrate intake with cardiovascular disease and mortality in 18 countries from five continents (PURE): a prospective cohort study. Lancet 2017;390:2050–2062. [DOI] [PubMed] [Google Scholar]
- 26. Miller V, Mente A, Dehghan M, Rangarajan S, Zhang X, Swaminathan S, Dagenais G, Gupta R, Mohan V, Lear S, Bangdiwala SI, Schutte AE, Wentzel-Viljoen E, Avezum A, Altuntas Y, Yusoff K, Ismail N, Peer N, Chifamba J, Diaz R, Rahman O, Mohammadifard N, Lana F, Zatonska K, Wielgosz A, Yusufali A, Iqbal R, Lopez-Jaramillo P, Khatib R, Rosengren A, Kutty VR, Li W, Liu J, Liu X, Yin L, Teo K, Anand S, Yusuf S.. Fruit, vegetable, and legume intake, and cardiovascular disease and deaths in 18 countries (PURE): a prospective cohort study. Lancet 2017;390:2037–2049. [DOI] [PubMed] [Google Scholar]
- 27. Collett D. Modelling Survival Data in Medical Research, 3rd ed Boca Raton: Chapman and Hall/CRC; 2015. [Google Scholar]
- 28. Wolbers M, Koller MT, Stel VS, Schaer B, Jager KJ, Leffondre K, Heinze G.. Competing risks analyses: objectives and approaches. Eur Heart J 2014;35:2936–2941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Austin PC, Lee DS, Fine JP.. Introduction to the analysis of survival data in the presence of competing risks. Circulation 2016;133:601–609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Schwartz AR, Patil SP, Laffan AM, Polotsky V, Schneider H, Smith PL.. Obesity and obstructive sleep apnea: pathogenic mechanisms and therapeutic approaches. Proc Am Thorac Soc 2008;5:185–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Romero-Corral A, Caples SM, Lopez-Jimenez F, Somers VK.. Interactions between obesity and obstructive sleep apnea: implications for treatment. Chest 2010;137:711–719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ford ES, Wheaton AG, Chapman DP, Li C, Perry GS, Croft JB.. Associations between self-reported sleep duration and sleeping disorder with concentrations of fasting and 2-h glucose, insulin, and glycosylated hemoglobin among adults without diagnosed diabetes. J Diabetes 2014;6:338–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Gangwisch JE, Heymsfield SB, Boden-Albala B, Buijs RM, Kreier F, Opler MG, Pickering TG, Rundle AG, Zammit GK, Malaspina D.. Sleep duration associated with mortality in elderly, but not middle-aged, adults in a large US sample. Sleep 2008;31:1087–1096. [PMC free article] [PubMed] [Google Scholar]
- 34. Yin J, Jin X, Shan Z, Li S, Huang H, Li P, Peng X, Peng Z, Yu K, Bao W, Yang W, Chen X, Liu L.. Relationship of sleep duration with all-cause mortality and cardiovascular events: a systematic review and dose-response meta-analysis of prospective cohort studies. J Am Heart Assoc 2017;6:e005947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Cai H, Shu XO, Xiang YB, Yang G, Li H, Ji BT, Gao J, Gao YT, Zheng W.. Sleep duration and mortality: a prospective study of 113 138 middle-aged and elderly Chinese men and women. Sleep 2015;38:529–536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Jike M, Itani O, Watanabe N, Buysse DJ, Kaneita Y.. Long sleep duration and health outcomes: a systematic review, meta-analysis and meta-regression. Sleep Med Rev 2018;39:25–36. [DOI] [PubMed] [Google Scholar]
- 37. Bursztyn M, Ginsberg G, Stessman J.. The siesta and mortality in the elderly: effect of rest without sleep and daytime sleep duration. Sleep 2002;25:187–191. [DOI] [PubMed] [Google Scholar]
- 38. Zhong G, Wang Y, Tao T, Ying J, Zhao Y.. Daytime napping and mortality from all causes, cardiovascular disease, and cancer: a meta-analysis of prospective cohort studies. Sleep Med 2015;16:811–819. [DOI] [PubMed] [Google Scholar]
- 39. Newman AB, Spiekerman CF, Enright P, Lefkowitz D, Manolio T, Reynolds CF, Robbins J.. Daytime sleepiness predicts mortality and cardiovascular disease in older adults. The Cardiovascular Health Study Research Group. J Am Geriatr Soc 2000;48:115–123. [DOI] [PubMed] [Google Scholar]
- 40. Hossain JL, Ahmad P, Reinish LW, Kayumov L, Hossain NK, Shapiro CM.. Subjective fatigue and subjective sleepiness: two independent consequences of sleep disorders? J Sleep Res 2005;14:245–253. [DOI] [PubMed] [Google Scholar]
- 41. Slater G, Steier J.. Excessive daytime sleepiness in sleep disorders. J Thorac Dis 2012;4:608–616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Cohen-Mansfield J, Perach R.. Sleep duration, nap habits, and mortality in older persons. Sleep 2012;35:1003–1009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Spiegel K, Leproult R, Van Cauter E.. Impact of sleep debt on metabolic and endocrine function. Lancet 1999;354:1435–1439. [DOI] [PubMed] [Google Scholar]
- 44. Spiegel K, Tasali E, Penev P, Van Cauter E.. Brief communication: sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann Intern Med 2004;141:846–850. [DOI] [PubMed] [Google Scholar]
- 45. Hossin MZ. From habitual sleep hours to morbidity and mortality: existing evidence, potential mechanisms, and future agenda. Sleep Health 2016;2:146–153. [DOI] [PubMed] [Google Scholar]
- 46. Patel SR, Ayas NT, Malhotra MR, White DP, Schernhammer ES, Speizer FE, Stampfer MJ, Hu FB.. A prospective study of sleep duration and mortality risk in women. Sleep 2004;27:440–444. [DOI] [PubMed] [Google Scholar]
- 47. Signal TL, Gale J, Gander PH.. Sleep measurement in flight crew: comparing actigraphic and subjective estimates to polysomnography. Aviat Space Environ Med 2005;76:1058–1063. [PubMed] [Google Scholar]
- 48. Sofi F, Cesari F, Casini A, Macchi C, Abbate R, Gensini GF.. Insomnia and risk of cardiovascular disease: a meta-analysis. Eur J Prev Cardiol 2014;21:57–64. [DOI] [PubMed] [Google Scholar]
- 49. Gottlieb DJ, Yenokyan G, Newman AB, O'Connor GT, Punjabi NM, Quan SF, Redline S, Resnick HE, Tong EK, Diener-West M, Shahar E.. Prospective study of obstructive sleep apnea and incident coronary heart disease and heart failure: the sleep heart health study. Circulation 2010;122:352–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.