Abstract
Research on home-based long-term care has centered almost solely on the costs; there has been very little, if any, attention paid to the relative benefits. This study exploits the randomization built into the Cash and Counseling Demonstration and Evaluation program that directly impacted the likelihood of having family involved in home care delivery. Randomization in the trial is used as an instrumental variable for family involvement in care, resulting in a causal estimate of the effect of changing the combination of home health care providers on health care utilization and health outcomes of the beneficiary. We find that some family involvement in home-based care significantly decreases health care utilization: lower likelihood of ER use, Medicaid-financed inpatient days, any Medicaid hospital expenditures and fewer months with Medicaid-paid inpatient use. We find that individuals who have some family involved in home-based care are less likely to have several adverse health outcomes within the first 9 months of the trial, including lower prevalence of infections, bedsores, or shortness of breath, suggesting that the lower utilization may be due to better health outcomes.
Keywords: Informal Care, Instrumental Variables, Medicaid, Cash and Counseling
Introduction
Well-known demographic trends point to an increasing need for health care services in coming decades, especially among individuals with long-term care (LTC) needs (CDC 2003).1 How best to meet this need should depend on an assessment of the costs and benefits of each potential source and type of care, but the current evidence base is sparse.
The costs of home-based LTC are substantial. Genworth (2016) reports that median annual costs range from $17,680 for adult day care to $46,333 for a full-time (40 hour/week) home health aide. From a narrow perspective of public payment, informal care is a vastly cheaper alternative, since it is provided “for free” by family and friends. However, researchers have pointed out that from a societal perspective, unpaid care incurs substantial costs, once one includes the labor market and health effects on the care providers themselves (recent examples include Van Houtven, Coe, and Skira 2013; Skira 2015; Ciccarelli and Soest 2018; Coe, Skira, and Larson 2018). Indeed, Skira (2015) and Coe, Skira, and Larson (2018) estimate the welfare costs of informal care to be roughly equivalent to the cost of a nursing home.
In contrast to costs, we know little about the relative benefit of home care based on the type of home-based care provider. The benefits of each type of care are largely inferred indirectly from studies of cost offsets between unpaid care and paid formal care. Many studies have shown that unpaid family care is a net substitute for paid home care (for example, Hanaoka and Norton 2008; Van Houtven and Norton 2004; Greene 1983; Bonsang 2009; Bolin, Lindgren, and Lundborg 2008).2 One exception is recent work by Barnay and Juin (2016), who find that informal care and formal care are complements in France, where each type of care impacts mental health differentially.
Theoretically, the marginal benefit of family care on the care recipient’s outcomes and costs is ambiguous. Formal home care is provided by trained staff, while family and friends are largely untrained, so it is possible that the care recipient experiences worse outcomes with family care. On the other hand, family and friends likely have a stronger personal connection to the care recipient and may provide more diligent, reliable care, with less loss of information across care episodes than formal home care. David and Kim (2018) find that handoffs between formal home care workers increase hospital readmissions. Family may also be less able to be objective about care needs and may disagree with formal caregivers, which could lead to friction and either underuse or overuse of inpatient care when both types of care are used together. Ultimately, the net marginal benefit of family care remains an empirical question.
One empirical problem that researchers face when assessing the relative benefits of family care is that the care provision is not random, and is likely correlated with unobserved or ill-measured factors, such as the health of the care recipient. In order to surmount the endogeneity problem, we use a unique setting that randomized Medicaid LTC recipients to one of two arms of care as part of the Cash and Counseling Demonstration and Evaluation program (CCDE). The control group had access to the default Medicaid home care: receiving care from a Medicaid-certified agency (hereafter called agency care), and unpaid family care. The treatment group received an allowance that could be used to pay for agency care and/or pay for care from family and friends (paid family care). The CCDE provides a vehicle for pseudo-randomization of the combination of care providers among beneficiaries eligible for Medicaid home care services because being randomized into the treatment group encouraged family to be involved in care. This randomization has previously been shown to strongly predict subsequent use of home-based care (Guo, Konetzka, and Manning 2015; Leibner and Lockwood 2013; Lieber and Lockwood 2018). No one has yet used this randomized trial to examine outcomes based on who provides the home-based care.
Another empirical issue with assessing the relative benefits of home-based care by type of care provider is identifying the proper outcome measures. While nursing homes and home care agencies are mandated to report uniform clinical data in order to assess patient outcomes, these measures are not required and generally unavailable for those receiving family care. There is largely no regulation, no assessment of family caregiver skill, no certification, and yet there is very likely heterogeneity in the skill required and the skill provided. Historically, the only measure of the benefit of unpaid care was adequacy, i.e. whether or not the care needs are routinely satisfied (Morrow-Howell, Proctor, and Rosario 2001; Morrow-Howell, Proctor, and Dore 1998; Skinner et al. 1999). While this measure can identify unmet needs in the community, it is quite limited in terms of assessing benefits. Data about the health care utilization and cost are difficult to interpret without additional information about underlying health. For example, a decrease in utilization could be due to improved health or to substandard home care delaying necessary hospital treatments. We use a combination of claims-based utilization data and six self-reported health indicators to measure the relative benefits of family involvement in home care and to help put any measured effect on utilization into context.
We contribute to the broader literature on LTC financing and outcomes by providing the first rigorous causal estimates of the benefits of changing the combination of care providers involved in home care. Overall, we assess the marginal impact of having some family involvement in home health care on patient health care utilization, the relative financial impact on the Medicaid program, and patient health outcomes. Section 1 details Medicaid LTC coverage and the CCDE program. Section 2 describes our data and our sample while Section 3 details our methodology. Section 4 provides the results while section 5 discusses the generalizability of our findings. Section 6 concludes that payment-induced family care leads to substantial decreases in hospital utilization and better patient self-assessed health within 9 months after randomization.
1. Long-Term Care in the US and the CCDE program
Medicare, the health insurance program for the elderly (65+), explicitly does not cover LTC, only acute and post-acute care. Instead, the US relies heavily on Medicaid, the health insurance program for the poor, for LTC. Medicaid finances half of all LTC in the U.S. (Reaves and Musumeci 2015), and is relatively generous – it covers institutional and home-based care, which can include both home health (care delivered by aides or therapists) and personal care. However, Medicaid coverage is limited to low-resource populations. In 2013, almost 3 million beneficiaries received home health, personal care, or home and community-based waiver services, with expenditures totaling $56.5 billion or just about $18,870 per beneficiary (Ng et al. 2016). Since Medicaid covers both LTC and acute care, it can internalize cost-offsets between the two insured risks.
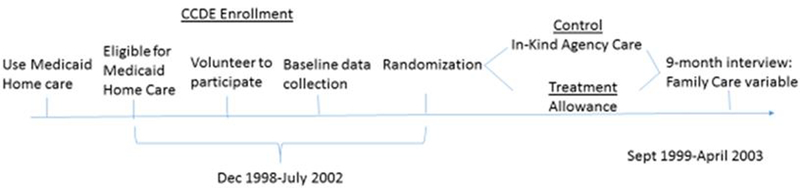
The CCDE was designed to assess how a more flexible consumer-directed manner of receiving Medicaid home care services affected Medicaid service use and cost (Dale and Brown 2007). The three-state (Arkansas, New Jersey, Florida) demonstration enrolled Medicaid beneficiaries already assessed for or receiving home care who volunteered for the CCDE program and consented to randomization (Doty, Mahoney, and Simon-Rusinowitz 2007). Enrollment occurred from December 1998 through July 2002. While the overall CCDE evaluation included 24 months of follow-up, we use only the 9-month follow-up data because it includes the family care variable in relation to outcomes of interest.3
The CCDE used a randomized experimental design to assess the effects of Cash and Counseling on the well-being of consumers and on their caregivers. After completing a baseline interview, half of the CCDE enrollees were assigned to the control group, where they received the standard Medicaid home care services secured through the traditional agency-based model. These services could be provided by Medicaid-contracted state-licensed home health care agencies, who agree to additional levels of regulation in order to serve the Medicaid community. The other half were randomized into the treatment group, where, instead of in-kind benefits, they received a monthly allowance equal to the amount Medicaid would have paid for their home care under the traditional model.4 Recipients could use this allowance in the way they deemed best to meet their care needs: hiring agency care; hiring non-agency workers (including family members) directly; and purchasing selected care-related goods and services. Individuals randomly assigned to the treatment group were more likely to use family care after randomization than those in the control group, who could use Medicaid money only to pay for agency care (See Table 2). In addition, the treatment group was eligible for counseling services which was designed to provide oversight to the program to make sure that every purchase with the Medicaid allowance was for home-care-related qualified goods and services. The original evaluation found the counseling to be very successful, with little to no fraud or abuse of funds found (Schore, Foster, and Phillips 2007).
Table 2:
Descriptive Statistics: After Randomization
| Control (N=2468) |
Treatment (N=2420) |
|||
|---|---|---|---|---|
| Dependent Variables | ||||
| Utilization and Spending | ||||
| Any ER Visit | 0.22 | (0.42) | 0.20 | (0.40) |
| Any Inpatient Spending | 0.28 | (0.46) | 0.29 | (0.45) |
| Medicaid Inpatient Days | 4.77 | (13.17) | 4.22 | (11.72) |
| Months with Inpatient Spending | 0.46 | (0.94) | 0.43 | (0.90) |
| Medicaid Inpatient Spending | 903.76 | (5010.24) | 821.15 | (4067.86) |
| Health Outcomes | ||||
| Current Health is Poor Relative to Peers | 0.41 | (0.49) | 0.39 | (0.49) |
| Had a Urinary Tract Infection | 0.18 | (0.38) | 0.16 | (0.36) |
| Had a Respiratory Infection | 0.25 | (0.44) | 0.24 | (0.42) |
| Bedsores Developed or Worsened | 0.08 | (0.27) | 0.06 | (0.24) |
| Contractures Developed or Worsened | 0.21 | (0.41) | 0.18 | (0.38) |
| Shortness of Breath Developed or Worsened | 0.32 | (0.47) | 0.27 | (0.45) |
| Key Independent Variable | ||||
| Family involvement in care | 89.5% | (30.7) | 94.3% | (23.2) |
This paper is not evaluating the CCDE itself, which has been widely studied. Instead, we are taking advantage of the rare opportunity of the CCDE’s randomized controlled study design to answer a different question which has not yet been addressed. The CCDE randomized assignment caused individuals to use a different combination of care providers to meet their home health care needs, for reasons that are orthogonal to their baseline health and other characteristics. The randomization thus addresses the endogeneity of the choice of LTC providers and allows us to estimate the benefits of family involvement in care when formal home health is being provided.
2. Data and Measurement
2.1. Data.
The primary data sources for this project include 1998–2003 Medicaid claims data for adult enrollees of the CCDE program, the baseline CCDE survey, and a 9-month follow-up CCDE survey.
2.2. Sample.
The original randomization included 5,555 participants; 2774 randomized to the treatment and 2781 randomized to the control group. 90 percent of each group remained covered by Medicaid during the 12-month follow-up period; 6 percent died and 4 percent lost Medicaid eligibility. We limit the study to those continuously enrolled in Medicaid so we have a consistent time period in which to measure the outcomes. We also limit the sample to the individuals who answered the 9-month follow-up survey, and answered the specific questions allowing us to assess whether the home health care team included family members, cutting 90 people from the dataset.5 Finally, we eliminate 30 people who did not receive any formal home care during this time period, to make sure we are not comparing receiving home care versus no care. Our final sample is 4,888 individuals.
2.3. Outcome Measures.
The dependent variables of interest are hospital utilization and nominal costs covered by Medicaid, derived from the Medicaid claims data at 9-months post-randomization, and self-reported health outcomes from the 9-month follow-up survey. The hospital utilization measures we examine include: any emergency room use; any hospital inpatient days; the number of inpatient hospital days. These outcomes are of particular interest because inpatient care is expensive, and there is growing attention to inpatient admissions, readmissions, and emergency room admissions in the US and all OECD countries (Berchet 2015). While utilization measures are not payer-specific and therefore should capture all utilization, in terms of our cost-related outcomes, we adopt the perspective of the Medicaid program and examine Medicaid reimbursed costs. Besides being dictated by data availability (as we have no data on Medicare or private spending), focusing on Medicaid spending is critical because Medicaid is a major player in the home care market, especially to address chronic LTC needs. We use “costs” to refer to costs to (or spending by) the Medicaid program. The costs measures include any Medicaid inpatient spending, the number of months with Medicaid inpatient spending, and the total Medicaid inpatient expenditure. As an additional robustness check on our main outcomes, we examine risk of hospitalization over 9 months and 24 months, to provide context to any findings that hospital costs or utilization are different by whether family is involved.
There are 6 binary health outcomes measures in the 9-month survey. First, care recipients can indicate if their current health is poor relative to their peers. Second, we know if two types of infections have occurred since the baseline interview: urinary tract infections and respiratory infections, the two most common infections among the disabled elderly (Rowe and Juthani-Mehta 2013). Finally, we have three indicators of the presence or worsening of three conditions: bedsores, muscle contractures, and shortness of breath.
2.4. Explanatory Variables.
The key explanatory variable is an indicator for family involvement in home care provision.. We focus on the extensive margin and define an indicator variable for family involvement in home care as having either unpaid care or indicating that any of the Medicaid payments went to related individuals.6 The receipt of unpaid care in the baseline period is consistent between the treatment and control groups; 88 percent of the control group and 87 percent of the treatment group received unpaid care. After randomization, the treatment group was allowed to use Medicaid dollars to pay family members, and 45 percent of the treatment group did so. This treatment increased family involvement in care from 87 to 94.3 percent in the treatment group while it was relatively stable at 89.5 percent in the control group.
While claims data typically have limited demographic information, we are able to use the baseline survey data, measured before randomization, as additional controls. These measures include demographics, baseline health and health spending, and baseline unpaid care received.
3. Analytic approach
We estimate two models based on the care recipient outcome of interest: probits for binary outcomes; two-part models for expenditures.
3.1. Utilization and Expenditure Models.
This study uses a two-part model (2PM) to estimate the impact of having family involvement in care on inpatient care use and spending, given the size of the zero-mass and skewed distribution of the outcome variables.7 The first part of the 2PM estimates the risk of any inpatient care use, or the probability of positive Medicaid inpatient care expenditures using a logit model, while the second part estimates the inpatient care days or the amount of Medicaid costs conditional on having any. Both parts are conditional on observed characteristics.
Specifically, we estimate the first part of the two-part model as:
| (1) |
where Y is the outcome of interest – emergency room days, inpatient length of stay, or inpatient spending. In the first part of the model we are estimating the probability of Y>0, conditional on the controls, under the assumption of a standard logistic distribution of the error term. The independent variables include FCi,t+9 as an indicator of whether family was involved in care received by patient i, as measured at (t+9), month 9 after randomization. Xi,t is a vector of individual demographic and socioeconomic variables, including gender, race (black or other race; white is reference), ethnicity (not Hispanic is reference), age measured in ranges (18–64 and age 80 and above, 65–79 is reference), marital status at baseline, two types of unpaid care received at baseline (transportation, house or community activities), and a set of pre-randomization health status variables, all measured at baseline. σi is a state fixed effect.
The second part of the model estimates the expenditure and utilization among individuals with any utilization of that type:
| (2) |
where Y is the continuous outcome variable of interest – inpatient length of stay, months with inpatient spending, or total inpatient spending, and the controls are as stated above. The expenditures and utilization among those with any inpatient care were right-skewed. To take this issue into account in the second part and avoid the potential bias problems in retransformation, generalized linear models (GLM) (McCullagh and Nelder 1989) are used and specified with log link and Gamma family based on a series of model specification tests.
3.2. Emergency Room Use and Patient Outcome Models.
All six measures of patient health are binary outcomes. Additionally, we have an indicator for the use of an emergency room. For these outcomes we estimate a probit of the following form:
| (3) |
where Yi is the binary outcome of interest – one of the six health outcome of individual i measured 9 months after randomization or the use of the emergency room. All controls are as defined above.
3.4. Endogeneity and instrumental variable(IV) approach.
As noted earlier, there are several major sources of potential endogeneity that need to be considered when estimating the causal effect of using family care on acute care use, costs, and health outcomes. To obtain consistent estimates, we use an IV approach. Random assignment into the treatment group serves as our instrument for having family involved in the home care received. Thus, conditional on assumptions of the IV model, we identify the causal effects of interest among individuals who were induced to use some family care as a result of being in the treatment group of the CCDE. We use a two-stage residual inclusion (2SRI) technique, the preferred approach when using nonlinear models (Terza, Basu, and Rathouz 2008). The first-stage residual based on all analysis observations is calculated from a probit regression of having family involvement in home care on CCDE treatment status:
| (4) |
where FC, M, X, and σ are as defined above. Treatment is an indicator for being randomly assigned to the treatment group as part of the CCDE project. For binary outcomes, the second stage model augments equation (3) with the predicted residual from the first stage (equation 4). For the utilization and expenditure models, the predicted residual is included in both parts of the 2PM. Marginal effects are calculated as the derivative of the response with respect to the variable of interest average across the sample, or the average marginal effect (AME). The 95% confidence intervals of the marginal effects from recombined models are obtained via 1,000 nonparametric bootstrap replicates on the whole analysis sample using the percentile method (Efron 1979). In addition, we adjust the significance for multiple hypothesis testing using Benjamini and Hochberg (1995) adjusted q-values (Anderson 2008).
IV estimates should be interpreted as local average treatment effects. That is, the estimate is derived from observations in which the instrument causes exogenous changes in behavior (“compliers”) and may not be applicable to all observations. In our case, the IV estimate is derived from observations where family care was used because the individual was in the treatment arm of the CCDE experiment and thus was allowed to pay family members, but would not have been used had the individual been assigned to the control group. This might be the case, for example, if the payment allowed a family caregiver to allocate time to caregiving that would not have been possible in the absence of payment, perhaps due to competing work demands (He and McHenry 2016).
4. Results
4.1. Descriptive Results.
Table 1 presents the prevalence of individual characteristics measured at baseline. Column 1 is for the full sample; columns 2 and 3 present the descriptive statistics for individuals receiving family care and those not receiving any family care, with column 4 presenting the Pearson tests of the differences between these two groups. Columns 5 and 6 present the descriptive statistics based on the randomized treatment; the CCDE control group and treatment group respectively. The seventh and final column presents the significance of the Pearson test of the differences in the mean between the treatment and control groups.
Table 1:
Descriptive statistics at Baseline
| Baseline Status (%) | Total Sample |
Receiving Family Care |
Receiving No Family Care |
Pearson Test |
Control | Treatment | Pearson Test |
|---|---|---|---|---|---|---|---|
| N | 4888 | 4268 | 397 | 2468 | 2420 | ||
| Gender | |||||||
| Female | 70.6 | 70.6 | 70.3 | 70.3 | 71.0 | ||
| Age | |||||||
| Age 18–64 | 43.8 | 44.0 | 41.3 | 44.0 | 43.6 | ||
| Age 65–79 | 30.9 | 30.1 | 40.1 | *** | 29.8 | 32.0 | |
| Age 80+ | 25.3 | 25.9 | 18.6 | *** | 26.3 | 24.4 | |
| State | |||||||
| Arkansas | 34.0 | 34.6 | 27.7 | *** | 34.2 | 33.8 | |
| Florida | 33.6 | 33.3 | 26.2 | *** | 33.4 | 33.9 | |
| New Jersey | 32.4 | 31.2 | 46.1 | *** | 32.4 | 32.4 | |
| Race & Ethnicity | |||||||
| Black | 29.2 | 29.3 | 28.2 | 29.3 | 29.1 | ||
| Hispanic | 21.4 | 21.4 | 21.5 | 21.8 | 21.80 | ||
| Potential Informal Care Resources | |||||||
| Married | 15.0 | 15.3 | 11.4 | ** | 14.5 | 15.5 | |
| Unpaid help: transportation | 60.6 | 62.9 | 34.9 | *** | 60.9 | 60.3 | |
| Unpaid help: house/community activities | 82.6 | 85.6 | 49.4 | *** | 83.3 | 82.0 | |
| Health Status & Disease History | |||||||
| Skeletal | 16.2 | 15.9 | 19.4 | * | 17.0 | 15.4 | |
| Skin high cost | 7.7 | 7.6 | 8.6 | 7.6 | 7.8 | ||
| Cancer | 10.1 | 9.8 | 13.6 | ** | 10.0 | 10.2 | |
| Cardiovascular | 27.1 | 26.8 | 30.2 | 26.2 | 27.9 | ||
| Gastrointestinal | 6.8 | 6.7 | 7.6 | 6.5 | 7.1 | ||
| Hematological | 6.4 | 6.1 | 10.1 | *** | 6.1 | 6.8 | |
| Psychiatric | 3.3 | 3.0 | 6.8 | *** | 3.4 | 3.2 | |
| Pulmonary | 9.7 | 9.7 | 10.1 | 8.7 | 10.7 | ** | |
Note: The significance levels of 1%, 5%, and 10% are denoted by ***, **, and * respectively.
The baseline characteristics are as expected, given the eligibility criteria for the CCDE. Almost 71 percent of the population is female and over half of the population is over the age of 65. Eighty-five percent are unmarried. Approximately one-third of the population is from each of the three states participating in the CCDE. 29 percent of the population is African-American; 21 percent is Hispanic. The majority are already receiving some sort of unpaid help at baseline, ranging from 61 percent getting help with transportation needs to 83 percent receiving assistance with household or community activities.
Since individuals had to be eligible to receive Medicaid home care already to qualify for the program, the health care needs are relatively high. Cardiovascular problems are prevalent, reported by over one-quarter of the population. Almost one in six reports a musculoskeletal issue.
There are considerable differences between the population receiving family care and those who are not at baseline, consistent with endogeneity concerns. Those receiving family care are older, more likely to be married, and more likely to be receiving unpaid help. There are also differences in the disease composition of the groups, with those receiving family care being less likely to have skeletal problems, cancer, hematological issues, and psychiatric problems.
Importantly, illustrating that the original random assignment was successful, columns 5 and 6 highlight the improved balance in the potential confounders using the randomized treatment status. We include all of these baseline measures in the models as controls.
Table 2 presents the averages of the outcome variables measured 9 months after randomization, by treatment status. The control group has slightly higher utilization for four out of the five utilization outcome measures, although none is statistically different. The control group reports worse health outcomes across the board, and significant differences are found in four out of the six outcomes: urinary tract infections, bedsores, contractures, and shortness of breath.
4.2. Instrument validity.
In order to be a valid instrument, randomization into the treatment group must be correlated with the receipt of family care. Table 2 shows that it is true in the unadjusted means; the treatment group is more likely to have family involved in home care (94.3 percent) than the control group (89.5 percent). In the regression analysis, individuals in the treatment group were estimated to be 5.2 percentage points (p<0.01) more likely to have family involved in home care than those in the control group. The Chi-squared statistic is 47.48 and significant at the < 0.01 level, comfortably passing the standard thresholds of 10 (Staiger and Stock 1997) and 16 (Stock and Yogo 2005).
Another condition, albeit untestable, for our instrument to be valid is that it cannot be correlated with the error term in the cost, utilization, or health outcome equations. The main concern in this case is that we know among those treated in the CCDE program, there was lower prevalence of unmet needs, higher spending on counseling, higher quality of life of caregivers, and higher Medicaid personal care costs and utilization, with no adverse health outcomes (Brown et al. 2007; Carlson et al. 2007). The pathways through which these effects were attained in the CCDE study are unclear – for example, these effects could be due to increased family involvement, the mechanism we study here, or due to increased agency and independence.
To consider mechanisms, it is useful to examine how CCDE consumers spent their allowances. While the treatment group could spend their Medicaid allowances in a variety of ways, the vast majority (80–90 percent) hired workers (Brown et al. 2007); few modified homes (2–10 percent) and even fewer modified cars (1 percent) (Carlson et al. 2007). While the treatment group received more paid personal assistance, unpaid care hours were lower, and thus the treatment and control groups received roughly the same total hours of care (Brown et al. 2007). Together, these factors suggest that a primary mechanism of the intervention was changing who provided care and whether that care was paid or unpaid.
The CCDE required that the treatment group create a care plan and allowance spending plan as part of their counseling services and to use fiscal agency services to make sure that their expenditures qualified for Medicaid coverage. Less than half of the consumers took advantage of other types of counseling services, such as advice about recruiting workers (Brown et al. 2007), suggesting that the bulk of the counseling money was spent teaching consumers about the program itself. These facts, and subsequent validity checks in Section 5.1, help alleviate concerns that there are other mechanisms through with the CCDE acts.
4.3. Main results.
In models that do not control for selection (naïve models), we find that there is a modest negative effect of having family involved in care on all utilization and spending measures. These results suggest that having family involved in care is associated with a 4 and 8 percentage point lower likelihood of using the ER and hospital, respectively, 2 fewer days in the hospital over 9 months, and $296 less in Medicaid spending over 9 months (p<0.10) (Panel A, Table 3). They are also healthier on four out of six health measures. This is consistent with individuals who have family involved in care being healthier than those who do not have family involvement.
Table 3:
Marginal effects of receiving family care on acute care utilization and spending
| Panel A: Naïve | Panel B: Reduced Form | Panel C: IV Model | ||||
|---|---|---|---|---|---|---|
| Family Involvement | Marginal Effect |
95% CI | Marginal Effect |
95% CI | Marginal Effect |
95% CI |
| First Stage | 0.0519*** | [−0.574,0.00631] | ||||
| Utilization | ||||||
| Any ER Use | −0.0412* | [−0.0807,−0.00158] | −0.0260** | [−0.0476,−0.00436] | −0.284* | [−0.574,0.00631] |
| Inpatient Days | ||||||
| Any Inpatient Days | −0.0769*** | [−0.121,−0.0324] | −0.0202 | [−0.0443,0.00388] | −0.324* | [−0.658,0.0112] |
| Number of Inpatient Days | −2.221*** | [−3.285,−1.158] | −0.759** | [−1.369,−0.148] | −10.14* | [−17.91,−2.358] |
| Medicaid Inpatient Spending | ||||||
| Any Medicaid Inpatient Spending | −0.0685*** | [−0.112,−0.0252] | −0.0223* | [−0.0459,0.00128] | −0.371* | [−0.697,−0.0455] |
| # Months with Inpatient $ | −0.165*** | [−0.248,−0.0830] | −0.0460* | −0.0939,0.00183] | −0.735* | [−1.373,−0.0974] |
| Medicaid Inpatient $ | −296.2* | [−616.2,23.81] | −188.7* | [−363.2,−14.12] | −1603.8 | [−3801.6,594.1] |
| Health Outcomes | ||||||
| Health Poor | −0.00466 | [−0.0556,0.0462] | −0.0228 | [−0.0509,0.00530] | −0.0634 | [−0.462,0.335] |
| Urinary Tract Infection | −0.0408** | [−0.0806,−0.00100 | −0.0266** | [−0.0488,−0.00435] | −0.305* | [−0.615,0.00451] |
| Respiratory Infection | −0.0417* | [−0.0866,0.00321] | −0.0200 | [−0.0453,0.00529] | −0.416* | [−0.767,−0.0651] |
| Bedsores | −0.0414*** | [−0.0665,−0.0162] | −0.0211** | [−0.0363,−0.00593] | −0.160 | [−0.365,0.0465] |
| Contractures | 0.0138 | [−0.0300,0.0576] | −0.0354** | [−0.0591,−0.0117] | −0.183 | [−0.517,0.150] |
| Shortness of Breath | −0.0509* | [−0.0975,−0.00432] | −0.0547*** | [−0.0807,−0.0287] | −0.499* | [−0.859,−0.139] |
Note: The significance levels of 1%, 5%, and 10% are denoted by ***, **, and *, respectively. 95% confidence intervals in brackets. All regressions include the following controls: gender, race (black or other race; white is reference), ethnicity (not Hispanic is reference), age measured in ranges (18–64 and age 80 and above, 65–79 is reference), marital status at baseline, two types of unpaid care received at baseline (transportation, house or community activities), and a set of pre-randomization health status variables and state fixed effects.
The second set of columns (Panel B, Table 3) presents the reduced form results, essentially replicating the CCDE evaluation on our sample. Here we find that the CCDE intervention is correlated with lower utilization and better health, and the effect sizes are roughly half of that in the naïve model.
In the IV model, we find that family involvement in care decreases utilization, and increases health, with substantial effect sizes. Emergency room visits decrease by 28 percentage points, the likelihood of having an inpatient hospital stay decreases by 32 percentage points and decreases the likelihood of Medicaid spending on inpatient care by 37 percentage points. Overall, these utilization changes sum to $1604 saved in the Medicaid program over 9 months, although the spending amount is not statistically significant. As is typical in IV models, we lose precision, and thus may not be able to detect small effects.
The estimates also show that family care plays an important causal role in preserving health. Individuals who use family care as a result of being randomized to the treatment group are significantly less likely to have infections, bedsores, or shortness of breath 9 months after randomization.
5. Robustness and Generalizability
5.1. Checks of Instrument Validity.
The validity of our approach requires that the randomization to treatment only influence the outcomes through the induced family involvement in care. We conduct two tests for instrument validity.
We expect, based on the original CCDE evaluations, some differences between the treatment and control groups post-randomization (Carlson et al. 2007; Anderson et al. 2012; Foster, Dale, and Brown 2007). Table 4 shows the means outcomes that might be of concern, by treatment status. As anticipated, the treatment group spends significantly more Medicaid dollars on counseling than the control group. While the total number of home care hours is similar between the treatment and control arms in our sample (Brown et al. 2007), the treatment group receives more paid care and fewer unpaid hours of care than the control group, consistent with the intervention where individuals can pay family members. There are also some differences in spending on home health and skilled nursing facilities in the subsequent 9 months after randomization. Excluding these variables, as we have done so far, could introduce an omitted variable bias. Including them, as we do in this robustness check, runs the risk of introducing endogeneity bias. Our main results are stable to the inclusion of additional controls (Medicaid dollars spent on counseling, hospice care, home health, and skilled nursing facilities; total hours of care and percent of care hours that were paid8) (Table 5).
Table 4:
Descriptive Statistics: CCDE-related outcomes
| Control (N=2468) |
Treatment (N=2420) |
t-test | |||
|---|---|---|---|---|---|
| Counseling Spending | $82 | (257) | $1736 | (3158) | *** |
| Hospice Spending | $14 | (510) | $39 | (1060) | |
| Total home care hours | 155 | (120) | 152 | (113) | |
| Paid hours/total home care hours | 27.7% | (30.5) | 32.5% | (28.1) | *** |
| Home Care Spending | $6967 | (8225) | $8679 | (10405) | *** |
| SNF Spending | $428 | (3060) | $149 | (1420) | *** |
| Key Independent Variable | |||||
| Family involvement in care | 89.5% | (30.7) | 94.3% | (23.2) | *** |
Table 5:
Marginal effects of receiving family care on acute care utilization and spending; adding additional CCDE Controls
| Panel A: Naïve | Panel B: Reduced Form | Panel C: IV Model | ||||
|---|---|---|---|---|---|---|
| Family Involvement | Marginal Effect | 95% CI | Marginal Effect |
95% CI | Marginal Effect |
95% CI |
| First Stage | 0.0391*** | [−0.146,0.0294] | ||||
| Utilization | ||||||
| Any ER Use | −0.0571** | [−0.103,−0.0113] | −0.0199* | [−0.0434,0.00366] | −0.0584 | [−0.146,0.0294] |
| Inpatient Days | ||||||
| Any Inpatient Days | −0.0960*** | [−0.148,−0.0436] | −0.00868 | [−0.0347,0.0173] | −0.0923* | [−0.191,0.00662] |
| Number of Inpatient Days | −2.567*** | [−3.696,−1.438] | −0.405 | [−1.056,0.246] | −0.948 | [−3.158,1.261] |
| Medicaid Inpatient Spending | ||||||
| Any Medicaid Inpatient Spending | −0.0815*** | [−0.132,−0.0306] | −0.0111 | [−0.0366,0.0144] | −0.0995** | [−0.195,−0.00374 |
| # Months with Inpatient $ | −0.208*** | [−0.302,−0.113] | −0.0245 | [−0.0757,0.0267] | −0.177* | [−0.361,0.00695] |
| Medicaid Inpatient $ | −369.2** | [−683.2,−55.27] | −148.9* | [−325.0,27.17] | −92.39 | [−737.7,553.0] |
| Health Outcomes | ||||||
| Health Poor | −0.0221 | [−0.0794,0.0351] | −0.0257* | [−0.0563,0.00484] | −0.0875 | [−0.204,0.0293] |
| Urinary Tract Infection | −0.0308 | [−0.0766,0.0149] | −0.0301** | [−0.0544,−0.00585] | −0.0158 | [−0.110,0.0781] |
| Respiratory Infection | −0.0499* | [−0.101,0.00125] | −0.0268* | [−0.0543,0.000767] | −0.110** | [−0.213,−0.00703] |
| Bedsores | −0.0466*** | [−0.0764,−0.0168] | −0.0181** | [−0.0346,−0.00154] | −0.0863*** | [−0.146,−0.0270] |
| Contractures | 0.0137 | [−0.0356,0.0630] | −0.0367*** | [−0.0625,−0.0109] | 0.0505 | [−0.0508,0.152] |
| Shortness of Breath | −0.0177 | [−0.0698,0.0344] | −0.0568*** | [−0.0850,−0.0286] | −0.0494 | [−0.158,0.0593] |
Note: The significance levels of 1%, 5%, and 10% are denoted by ***, **, and *, respectively. 95% confidence intervals in brackets. All regressions include all controls included in table 3, plus CCDE-related controls, including the amount spent on counseling, hospice, skilled nursing facilities, and home health, total home care hours, and the ratio of paid care to total home care hours.
Second, since counseling is part of the treatment, we use the sub-sample without any family involvement in care to examine the impact of counseling on outcomes (Table 6). While this is not a random sub-sample, and the treatment was not randomized within this subsample, it allows us to shed light on the relationship between counseling and out outcomes of interest. In Panel A, we estimate the correlation between amount spent on counseling and outcomes. Other than a marginal (and positive) correlation with ER use, we find no relationship. Panel B presents the reduced form results for the subsample. We find no impact of the CCDE on this subsample, which suggests that more counseling alone is not conducive to better health. Finally, in Panel C, while being randomized into treatment is significantly associated with spending on counseling, that spending has no causal relationship on the outcomes of interest if the assumption of treatment being random is met within this subsample. These results support the validity of the instrument in identifying the effects of family care.
Table 6:
Marginal effects of Counseling on acute care utilization and spending among those without family care
| Panel A: Naïve | Panel B: Reduced Form | Panel C: IV Model | ||||
|---|---|---|---|---|---|---|
| $ spent on Counseling (in $1,000s) |
Marginal Effect |
95% CI | Marginal Effect |
95% CI | Marginal Effect |
95% CI |
| First Stage | 0.558*** | [0.4000,0.717] | ||||
| Utilization | ||||||
| Any ER Use | 0.0286* | [0.00781,0.0495] | 0.00165 | [−0.0869,0.0902] | −0.00213 | [−0.059,0.0552] |
| Inpatient Days | ||||||
| Any Inpatient Days | 0.0206 | [−0.00414,0.0453] | −0.000237 | [−0.0989,0.0984] | −0.000870 | [−0.064,0.0627] |
| Number of Inpatient Days | −0.117 | [−0.839,0.605] | −2.552 | [−6.515,1.410] | −1.66 | [−4.239,0.923] |
| Medicaid Inpatient Spending | ||||||
| Any Medicaid Inpatient Spending | 0.0112 | [−0.0123,0.0347] | −0.0182 | [−0.115,0.0783] | −0.0123 | [−0.0745,0.05] |
| # Months with Inpatient $ | −0.0162 | [−0.0621,0.0298] | −0.197 | [−0.410,0.0170] | −0.126 | [−0.265,0.0125] |
| Medicaid Inpatient $ | 166.6 | [−65.62,398.9] | −46.56 | [−780.3,687.1] | −74.36 | [−524.4,375.7] |
| Health Outcomes | ||||||
| Health Poor | 0.00549 | [−0.0214,0.0324] | 0.00865 | [−0.0929,0.110] | 0.00540 | [−0.060,0.0709] |
| Urinary Tract Infection | −0.00910 | [−0.0349,0.0167] | −0.00390 | [−0.0913,0.0835] | −0.00345 | [−0.0599,0.053] |
| Respiratory Infection | −0.00216 | [−0.0292,0.0249] | −0.0205 | [−0.117,0.0756] | −0.0132 | [−0.075,0.0487] |
| Bedsores | 0.00358 | [−0.0124,0.0195] | −0.00722 | [−0.0714,0.0570] | −0.00458 | [−0.0457,0.037] |
| Contractures | 0.0103 | [−0.0112,0.0317] | −0.0116 | [−0.101,0.0776] | −0.00941 | [−0.067,0.0485] |
| Shortness of Breath | 0.00417 | [−0.0225,0.0308] | −0.00219 | [−0.102,0.0979] | −0.00168 | [−0.066,0.0629] |
Note: The significance levels of 1%, 5%, and 10% are denoted by ***, **, and *, respectively. 95% confidence intervals in brackets. All regressions include the same controls as Table 3. The sample is limited to the 397 beneficiaries that do not have family involved in their home care.
5.2. Robustness Check using Hazard Model.
Having family involved in care might impact not only the amount of care received, but also the timing of such care. We estimate the impact of family care on the chance of being admitted to the hospital using a Cox proportional hazard model. This hazard analysis treats death, leaving the Medicaid program (after a year), and the end of CCDE program as random right-censoring events. We estimate this for the first 9 months after randomization, to be consistent with the rest of our outcomes, and 24 months after randomization, to see if the effect persists.
The hazard ratios indicate that having family involved in care lowers the likelihood of a hospital admission at both 9 and 24 months after randomization, complementing the main results. Table 7 indicates that for those with treatment-induced family involvement in care, the risk of hospitalization was one-fifth (one-third) of those in the control group over 9 months (24 months).
Table 7:
Cox proportional hazard model: hospitalization
| Panel A: Naïve | Panel B: Reduced Form | Panel C: IV Model | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Family Involvement | Hazard Ratio |
95% CI | Hazard Ratio |
95% CI | Hazard Ratio |
95% CI | |||
| Utilization in 9 months after randomization | |||||||||
| Hospitalization risk | 0.747 | *** | [0.620, 0.90] | 0.907 | * | [0.815, 1.009] | 0.218 | ** | [0.054, 0.886] |
| Utilization in first 24 months after randomization | |||||||||
| Hospitalization Risk | 0.866 | * | [0.740,1.013] | 0.934 | [0.86, 1.014] | 0.363 | * | [0.1212,1.09] | |
Note: The significance levels of 1%, 5%, and 10% are denoted by ***, **, and *, respectively. 95% confidence intervals in brackets. All regressions include the same controls in Table 3.
5.3. Generalizability.
While the CCDE program provides the randomization necessary to achieve causal estimates, the potential tradeoff is loss in generalizability. The three-state sample might not represent the national Medicaid population well, or the participating population may not represent Medicaid home care users generally, because only a modest proportion (6% to 10%) of eligible adults voluntarily enrolled in the demonstration. In order to assess external validity of this study sample, we compare the CCDE analysis sample with the national Medicaid population of home and community-based service users in 2005 on several selected characteristics, as reported by Konetzka et al. (2012).
Table 8 presents this comparison on two samples, those age 65 and older (column 1) and the total population (column 2). One known non-comparability between the CCDE and the Medicaid HCBS total population is that the latter includes a small proportion of children with LTC needs, while the CCDE population only contains adults. In general, the mean years of age and the percentage of dually eligible are very similar between the two samples. However, the CCDE sample includes more women. There are also some discrepancies in racial characteristics, but it is unclear if these differences appear due to differences in categorization or reporting, since the CCDE sample has fewer people in the “other” or “missing” race categories. Overall, most characteristics of CCDE participants are similar to a broader population of Medicaid home care users.
Table 8:
Selected characteristics of Cash & Counseling Demonstration enrollees
| Selected characteristics | Total* | |
|---|---|---|
| 2005 HCBS | CCDE | |
| Dual eligible (Medicaid and Medicare) | 66.18% | 67.26% |
| Age | 55.57 | 61.38 |
| Female | 61.43% | 70.60% |
| Race | ||
| White | 56.08% | 59.51% |
| Black** | 29.43% | 29.02% |
| Other race | 6.32% | 6.06% |
| Race unknown | 8.17% | 5.26% |
Note: the total 2005 HCBS population includes children, while the analysis sample of CCDE population does not.
The 2005 HCBS data consider Hispanic as a race, while the CCDE data use US Census definition and see Hispanic as ethnicity. Because there is no ethnicity definition and Black and Hispanic are mutually exclusive in 2005 HCBS data , we combined the Black and Hispanic as one race category in HCBS data, and use Black only in CCDE to compare race groups and make all the categories within the same population adding to 100%.
6. Discussion
We find that using payment-induced family care decreases inpatient utilization and the likelihood of Medicaid spending on inpatient care. That is, on average, family involvement in home care is a substitute to hospital care. In addition, given that total hours of care received remained largely unchanged, this work suggests that substituting family care for some formal care could be beneficial. This is consistent with findings of Bonsang (2009), who finds that informal care is a complement to skilled home health care. In our study’s context, it could be that the combination of informal and formal home care creates synergies between providers that lead to the net substitution for inpatient care.
To assess whether the overall marginal benefit of family care is positive, we also estimated the health impacts of family care to frame the benefits against the cost savings found in the inpatient setting. There are many ways in which hospital care decreases but health outcomes of participants are worse. For example, family care could be lower quality, could result in neglect or delay in meeting the care recipient’s needs (either due to a desire to maximize their payments or reluctance to admit that they need further assistance in providing care). In those cases, the welfare effects of decreased expenditures would be ambiguous, because lower spending could be offset by worse outcomes. On the other hand, it may also be that the presence of family caregivers in the hospital leads to the ability to discharge earlier from the hospital, but without any change in patient outcomes, which would make the use of family caregivers potentially welfare-enhancing for the participants. Our analysis of six measures of health taken 9 months after randomization indicate that payment-induced family care leads to sizable decreases in infection rates and development of bedsores and shortness of breath. We hypothesize that increased attention from family, which might also include more visits at “off-hours” or more frequent but shorter visits, could lead to the decrease in infections and bedsores. Shortness of breath is associated with many chronic conditions such as heart and lung diseases, and family attention may help with adherence to medication regimens that prevent exacerbations of such conditions. Together, these findings provide suggestive evidence that family involvement in care could both increase health of the patient while decreasing utilization and costs. Further exploration of the health benefits on more recent data with more health outcomes that are sensitive to home care is needed, as well as examination of the care recipients’ experience of care with and without family involved in care, an important patient-centered health outcome (Bergeson 2006; Epstein 2011).
Limitations of this study include its potential inability to generalize beyond the Medicaid population. However, as Medicare does not provide LTC and only 15 percent of the elderly hold private insurance, Medicaid is and likely will continue to be the primary payer of formal LTC in the US. While Medicaid pays for approximately one-half of LTC expenditures in the US, the findings from this population may not be generalizable to the home care population as a whole, especially affluent and private-pay home care markets. Further, the data from the CCDE are relatively old and have limitations. For example, measurement of effects is limited to the 9-month window after randomization, and available measures preclude examining the intensive margin of family care. Finally, our estimates are of the local average treatment effect and thus are applicable for households who have family that will provide care when paid to do so. This is a very policy-relevant parameter of interest as countries debate how to best meet their looming LTC demand at the lowest cost and as more proposals are introduced to financially support caregivers, but may not be informative about the quality of care provided by family when there is little ability to pay caregivers. For example, compliers may be more financially constrained than families who can provide care without financial incentives, or are simply more motivated by the payment. While we feel the strong identification stemming from re-use of the randomization to identify the causal relationship outweighs these drawbacks and our robustness checks reduce concern about several of these issues.
Given current interest in shifting resources away from institutional care and into the home in the US and many OECD countries, our findings have important implications for policy. By summer 2019 the US must have a national caregiver strategy, according to the Recognize, Assist, Include, Support and Engage (RAISE) Family Caregivers Act, signed into law in January 2018, and based on the recommendation of the 2016 report from the National Academy of Sciences, Families Caring for an Aging America (National Academies of Sciences 2016; Wolff, Feder, and Schulz 2016; Jefferson 2018). The Our results indicate that, depending on the cost of the policies associated with the national caregiver strategy and any benefits to caregivers, policies to support family caregivers may hold promise in improving care recipient outcomes while holding down costs. It is also important to note that any policy that encourages home and community-based health care inevitably relies more on family caregivers (Konetzka 2014). Thus, more careful consideration of the marginal benefits of family care will help properly frame the optimal investment decisions between expanding formal care versus expanding informal care supports. Further work to discern the mechanisms through which family care leads to these effects would be helpful to guide policy development to improve home care.
Figure1:
CCDE and data timeline
Acknowledgements:
We would like to acknowledge two anonymous reviewers, Barbara Schone, John Bowblis, Peter Groenfeld, participants in the PHEnOM seminar at the University of Washington, Health Services seminar at the University of Pennsylvania, American Economic Association annual meetings, American Society of Health Economists meeting, and the International Conference on Evidence-based Policy in Long-Term Care for their helpful comments on previous versions of this paper. Research reported in this publication was supported by The National Institute on Aging of the National Institutes of Health under award number R01AG057501 (PI: Coe). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Any errors are our own.
Footnotes
Conflict of Interest: Dr. Coe reports grants from National Institutes of Health during the conduct of the study. Dr. Konetzka reports grants from National Institutes of Health and the Agency for Healthcare Research and Quality during the conduct of the study. Dr. Van Houtven reports grants from National Institutes of Health and Veterans Health Administration, during the conduct of the study. She also is an evaluator and advisory board member for Elizabeth Dole Foundation’s Campaign for Inclusive Care. Guo has no disclosures.
Long-term care is generally defined as the need for ongoing assistance due to functional or cognitive impairment, the risks of which increase with age.
For example, (Hanaoka and Norton 2008; Van Houtven and Norton 2004; Greene 1983; Bonsang 2009; Bolin, Lindgren, and Lundborg 2008).
See Figure 1 for a timeline of the CCDE experiment and data used in this study.
The CCDE program was authorized through a section 1115 waiver, and thus was subject to the Center for Medicaid and Medicare Services (CMS)’s budget-neutrality condition on Home and Community Based Services (HCBS). Therefore, the allowance received by individuals in the treatment group was set so that the expected cost per recipient was the same as if they were in the control group.
Tests on baseline variables comparing the treatment arms suggest that the additional sample inclusion criteria do not introduce statistically significant selection bias at a 10 percent significant level based on observed variables. 94% of pre-randomization attributes were not significantly different across the treatment and control groups, after final inclusion restrictions, at a 5 percent significant level.
Although we have data on the total hours of home care, total hours paid and total hours unpaid care, we do not have total hours separated by family vs agency care which would allow us to model the intensity of family care.
We conducted a series of goodness of fit tests, and the two-part models do not appear to have significant specification errors (Hosmer 1989; Pregibon 1980).
The 9-month survey asked about the total hours of care provided in the previous two weeks for up to three visiting paid caregivers, three visiting unpaid caregivers, two live-in paid caregivers, and two live-in unpaid caregivers. We sum over all types and include the total paid hours, and the percent of hours of care received that were paid.
References
- Anderson Michael. 2008. ‘Multiple Inference and Gender Differences in the Effects of Early Intervention: A Reevaluation of the Abecedarian, Perry Preschool, and Early Training Projects’, Journal of the American Statistical Association, 103: 1481–95. [Google Scholar]
- Anderson RA, Corazzini K, Porter K, Daily K, McDaniel RR Jr., and Colon-Emeric C. 2012. ‘CONNECT for quality: protocol of a cluster randomized controlled trial to improve fall prevention in nursing homes’, Implement Sci, 7: 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnay Thomas, and Juin Sandrine. 2016. ‘Does home care for dependent elderly people improve their mental health?’, Journal of Health Economics, 45: 149–60. [DOI] [PubMed] [Google Scholar]
- Benjamini Y, and Hochberg Y. 1995. ‘The Control of the False Discovery Rate in Multiple Testing Under Dependency’, The Annals of Statistics, 29: 1165–88. [Google Scholar]
- Berchet C 2015. “Emergency Care Services : Trends, Drivers and Interventions to Manage the Demand.” In, edited by OECD Health Working Papers. [Google Scholar]
- Bergeson Steven C., Dean John D.. 2006. ‘A Systems Approach to Patient-Centered Care’, The Journal of the American Medical Association, 296: 2848–951. [DOI] [PubMed] [Google Scholar]
- Bolin K, Lindgren B, and Lundborg P. 2008. ‘Informal and formal care among single-living elderly in Europe’, Health Econ, 17: 393–409. [DOI] [PubMed] [Google Scholar]
- Bonsang E 2009. ‘Does informal care from children to their elderly parents substitute for formal care in Europe?’, J Health Econ, 28: 143–54. [DOI] [PubMed] [Google Scholar]
- Brown RS, Dale SB, Randall S Brown, and Dale Stacy B. 2007. ‘The research design and methodological issues for the Cash and Counseling Evaluation’, Health Services Research, 42: 414–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlson BL, Foster L, Dale SB, and Brown R. 2007. ‘Effects of Cash and Counseling on personal care and well-being’, Health Serv Res, 42: 467–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC. 2003. ‘Public health and aging: trends in aging--United States and worldwide’. http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5206a2.htm.
- Ciccarelli Nicoal, and Van Soest Arthur. 2018. ‘Informal Caregiving, Employment Status and Work Hours of the 50+ Population in Europe’, De Economist, 166: 363–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coe, Norma B, Meghan Skira, and Eric Larson. 2018. ‘A More Comprehensive Measure of the Costs of Caring for a Parent: Differences by Functional Status’, Journal of the American Geriatrics Society, 66: 2003–08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dale SB, and Brown RS. 2007. ‘How does Cash and Counseling affect costs?’, Health Serv Res, 42: 488–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- David Guy, and Kunhee Lucy Kim. 2018. ‘The effect of workforce assignment on performance: Evidence from home health care’, Journal of Health Economics, 59: 25–45. [DOI] [PubMed] [Google Scholar]
- Doty P, Mahoney KJ, and Simon-Rusinowitz L. 2007. ‘Designing the Cash and Counseling Demonstration and Evaluation’, Health Serv Res, 42: 378–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Efron B 1979. ‘Bootstrap Methods: Another Look at the Jackknife’, The Annals of Statistics, 7: 1–26. [Google Scholar]
- Epstein, Ronald M, Street Richard L. 2011. ‘The Values and Value of Patient-Centered Care’, The Annals of Family Medicine, 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foster L, Dale SB, and Brown R. 2007. ‘How caregivers and workers fared in Cash and Counseling’, Health Serv Res, 42: 510–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greene VL. 1983. ‘Substitution between formally and informally provided care for the impaired elderly in the community’, Medical Care, 21: 609–19. [DOI] [PubMed] [Google Scholar]
- Guo Jing, Konetzka RT, and Manning W. 2015. ‘The causal effects of home care use on institutional long-term care utilization and expenditures’, Health Economics, 24: 4–17. [DOI] [PubMed] [Google Scholar]
- Hanaoka C, and Norton EC. 2008. ‘Informal and formal care for elderly persons: how adult children’s characteristics affect the use of formal care in Japan’, Soc Sci Med, 67: 1002–8. [DOI] [PubMed] [Google Scholar]
- He Deifang, and Peter McHenry. 2016. ‘Doe Formal Imployment Reduce Informal Caregiving?’, Health Economics, 25: 829–43. [DOI] [PubMed] [Google Scholar]
- Hosmer DW and Lemeshow S. 1989. Applied Logistic Regression (Wiley: New York: ). [Google Scholar]
- Jefferson RS 2018. “Congress Passes, Trump Signs RAISE Family Caregivers Act ‘Elevating Caregiving To A Priority’.” In Forbes. [Google Scholar]
- Konetzka RT 2014. ‘The hidden costs of rebalancing long-term care’, Health Serv Res, 49: 771–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konetzka RT, Karon SL, and Potter DE. 2012. ‘Users of medicaid home and community-based services are especially vulnerable to costly avoidable hospital admissions’, Health Aff (Millwood), 31: 1167–75. [DOI] [PubMed] [Google Scholar]
- Leibner Ethan MJ , and Lockwood Lee M.. 2013. ‘Costs and Benefits of In-Kind Transfers: The Case of Medicaid Home Care Benefits’, University of Michigan Retirement Research Center Working Paper, 2013–294. [Google Scholar]
- Lieber, Ethan MJ, and Lee M Lockwood. 2018. “Targeting with In-kind Transfers: Evidence from Medicaid Home Care.” In, edited by NBER Working Paper. [PubMed] [Google Scholar]
- McCullagh P, and Nelder JP. 1989. Generalized Linear Models (Chapman and Hall: UK: ). [Google Scholar]
- Morrow-Howell N, Proctor E, and Dore P. 1998. ‘Adequacy of care: The concept and its measurement.’, Research on Social Work Practice, 8: 86–102. [Google Scholar]
- Morrow-Howell N, Proctor E, and Rosario P. 2001. ‘How much is enough? Perspectives of care recipients and professionals on the sufficiency of in-home care’, Gerontologist, 41: 723–32. [DOI] [PubMed] [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine. 2016. “Families caring for an aging America.” In. Washington DC: The National Academies Press. [PubMed] [Google Scholar]
- Ng Terrence, Harrington Charlene, Meumeci MaryBeth, and Ubri Petry. 2016. ‘Medicaid Home and Community-Based Service Programs: 2013 Data Update’, Kaiser Family Foundation. [Google Scholar]
- Pregibon D 1980. ‘Goodness of Link Tests for Generalized Linear Models’, Journal of the Royal Statistical Society Series B (Applied Statistics), 29: 15–23. [Google Scholar]
- Rapp Thomas , Chauvin Pauline, and Sirven Nicolas. 2015. ‘Are public subsidies effective to reduce emergency care use? Evidence from the PLASA study ‘, Social Science & Medicine, 138: 31–37. [DOI] [PubMed] [Google Scholar]
- Reaves, Erica L, and Musumeci MaryBeth. 2015. “Medicaid and Long-Term Services and Supports: A Primer.” In The Kaiser Commission on Medicaid and the Uninsured. [Google Scholar]
- Rowe TA, and Juthani-Mehta M 2013. ‘Urinary tract infection in older adults’, Aging Health, 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schore Jennifer, Foster Lesie, and Phillips Barbara. 2007. ‘Consumer Enrollment and Experiences in the Cash and Counseling Program’, Health Serv Res, 42: 446–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skinner E, D Steinwach K Handley, Lehman A, Fahey M, and Lyles C. 1999. ‘Met and unmet needs for assistance and quality of life for people with severe and persistent mental disorders.’, Mental Health Services Research, 1: 109–18. [Google Scholar]
- Skira Meghan M. 2015. ‘Dynamic wage and employment effects of elder parent care’, International Economic Review, 56: 63–93. [Google Scholar]
- Staiger D, and Stock JH. 1997. ‘Instrumental variables regression with weak instruments’, Econometrica, 65: 557–86. [Google Scholar]
- Stock, James H, and Yogo Motohiro. 2005. ‘Testing for Wealk Instruments in IV Regressions’ in Donald WK Andrews and Stock James H.(eds.), Indentification and Inference for Econometric Models: A Festschrift in Honor of Thomas Rothenberg (Cambridge University Press: UK: ). [Google Scholar]
- Terza JV, Basu A, and Rathouz PJ. 2008. ‘Two-stage residual inclusion estimation: addressing endogeneity in health econometric modeling’, J Health Econ, 27: 531–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Houtven CH, Coe NB, and Skira MM. 2013. ‘The effect of informal care on work and wages’, J Health Econ, 32: 240–52. [DOI] [PubMed] [Google Scholar]
- Van Houtven CH, and Norton Edward. 2008. ‘Informal care and Medicare expenditures: Testing for heterogeneous treatment effects’, Journal of Health Economics, 28: 134–56. [DOI] [PubMed] [Google Scholar]
- Van Houtven CH, and Norton EC. 2004. ‘Informal Care and Elderly Health Care Use’, Journal of Health Economics, 23: 1159–80. [DOI] [PubMed] [Google Scholar]
- Weaver France, Sterns Sally C., Norton Edward C., and Spector William. 2009. ‘Proximity to death and participation in the long‐term care market’, Health economics, 19: 867–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolff JL, Feder J, and Schulz R. 2016. ‘Supporting Family Caregivers of Older Americans’, New England Journal of Medicine, 375: 2513–15. [DOI] [PubMed] [Google Scholar]


