Abstract
Background
Elevated resting heart rate (HR) is a risk factor and therapeutic target in patients with heart failure (HF) and reduced ejection fraction (HFrEF). Previous studies indicate a genetic contribution to HR in population samples but there is little data in patients with HFrEF.
Methods
Patients who met Framingham criteria for HF and had an ejection fraction < 50% were prospectively enrolled in a genetic HF registry (2007–2015, n = 1060). All participants donated blood for DNA and underwent genome-wide genotyping with additional variants called via imputation. We performed testing of previously identified variant “hits” (43 loci) as well as a genome-wide association (GWAS) of HR, adjusted for race, using Efficient Mixed-Model Association Expedited (EMMAX).
Results
The cohort was 35% female, 51% African American, and averaged 68 years of age. There was a 2 beats per minute (bpm) difference in HR by race, AA being slightly higher. Among 43 candidate variants, 4 single nucleotide polymorphisms (SNPs) in one gene (GJA1) were significantly associated with HR. In genome-wide testing, one statistically significant association peak was identified on chromosome 22q13, with strongest SNP rs535263906 (p = 3.3 × 10−8). The peak is located within the gene Cadherin EGF LAG Seven-Pass G-Type Receptor 1 (CELSR1), encoding a cadherin super-family cell surface protein identified in GWAS of other phenotypes (e.g., stroke). The highest associated SNP was specific to the African American population.
Conclusions
These data confirm GJA1 association with HR in the setting of HFrEF and identify novel candidate genes for HR in HFrEF patients, particularly CELSR1. These associations should be tested in additional cohorts.
Electronic supplementary material
The online version of this article (10.1186/s40246-019-0206-6) contains supplementary material, which is available to authorized users.
Keywords: Genetics, Heart rate, African Americans, Single nucleotide polymorphisms
Introduction
Heart failure (HF) remains a considerable public health problem, with an estimated 5.7 million people living with HF in the USA, resulting in > 1 million HF hospitalizations and > $30 billion in health care costs annually [1]. Chronic HF is associated with repeated hospitalizations, substantially reduced quality of life, and a yearly mortality rate in the USA of 7.5% [2]. Observational and interventional studies in adults demonstrate that elevated heart rate (HR) is a modifiable risk factor in patients with HF [3–6]. Beta-blockers represent one of the most important therapeutic options for reducing morbidity and mortality in HF, which may partly be contributed to by their capacity to reduce HR. More recently, the Systolic Heart treatment with the If inhibitor ivabradine Trial (SHIFT) demonstrated that specifically targeting HR reduction in HF patients with reduced ejection fraction (HFrEF) lowers the risk of hospitalization for worsening HF, establishing HR as not only a marker of risk but a treatment target [6]. Therefore, understanding the genetic and biologic drivers of HR particularly in the setting of HFrEF may aid in understanding HF pathophysiology, improve prognostication, or inform treatment decision-making.
Previous studies have examined genetic factors influencing HR in various settings. It has recently become clear that HR is a heritable trait [7, 8], suggesting important genetic influences. In the context of beta-blocker (BB) therapy, GRK5 was suspected of influencing this but in one study showed no association of GRK5 genotype with heart rate [9]. Several GWAS of HR in non-HF populations have been performed [10–14], which have reported a number of significant variants; however, the impact of these loci in HF patients remains uncharacterized; and to our knowledge, the genetic contribution to HR in patients with established HFrEF has not been previously investigated. The overall goal of this study was to test the validity of previous candidate gene associations and to identify novel genetic determinants of HR in a diverse cohort of HFrEF patients via GWAS.
Methods
Study population
The study population (n = 1060) was from a genetic registry of HF patients collected at the Henry Ford Health System (September 13, 2007 to April 1, 2015). Entry criteria included patients ≥ 18 years of age meeting the Framingham criteria for HF, with a previously measured left ventricular ejection fraction (LVEF) < 50%, who were enrolled in our covered entity (Health Alliance Plan) for at least 1 year prior to the date of registry enrollment. Left ventricular EF < 50% was used as eligibility criteria because at the time of registry initiation, this was considered standard for systolic HF. Since EF cutoffs for HFrEF have subsequently changed and ivabradine is indicated in EF < 35%, we include additional restricted analyses in this group. The study was approved by local ethics committees and participants provided written informed consent.
Genotyping and imputation
We performed genotyping on all registry participants using the Axiom Biobank array (Affymetrix®). This array contains 600K single nucleotide polymorphisms (SNPs) including: (1) 300K GWAS markers with minor allele frequencies of > 1%, (2) > 250K markers low frequency (< 1%) coding variants from the exome sequencing project, and (3) an additional 50K variants to improve African ancestry coverage (YRI Booster). This array provides excellent coverage of genomic variation, capturing 90% in European ancestry and ~ 80% in African ancestry patients. It also allows for ancestral quantification and admixture mapping. The genotyping and standard quality checks were carried out in a standard accepted fashion. In brief, SNPs with a minor allele frequency less than 0.01 or not in Hardy–Weinberg equilibrium (HWE, P < 1 × 10−7) in each major ethnicity group were removed. Multi-allelic sites and ambiguous SNPs were also deleted. Additionally, study participant samples with questioned validity due to either sex inconsistency (between reported and genetically inferred) or duplicate genotyping were removed.
The imputation was conducted on the Michigan Imputation Server. The computation engine is Minimac3 (https://genome.sph.umich.edu/wiki/Minimac3), and the reference panel used was 1000 Genome Phase 3 v5 [15]. Following imputation, we assessed accuracy at each SNP as the squared Pearson correlation (R2) between the masked genotypes and the imputed allele dosages (also known as posterior mean genotypes). We retained variants passing commonly used imputation quality thresholds (R2 > 0.3, MAF > 0.01, HWE P value > 1 × 10−7) for use in the subsequent analyses.
Clinical data
Patient characteristics including demographic, medical, and lifestyle data were collected at registry enrollment via a standardized questionnaire and physical exam and supplemented by using administrative data maintained by the system. Primary data collection via the questionnaire and study staff assessment included age, sex, HR, blood pressure, New York Heart Association class, self-identified race, and co-morbidities. We utilized electronic administrative databases maintained by HFHS (including data from Health Alliance Plan our covered entity), such as patient encounters, medical claims, laboratory data, and pharmacy claims membership files to supplement primary data collection from the patient. This included medical diagnoses established via ICD-9 diagnosis related groupings (DRG). ICD-9 classification does not contain discriminators for permanent vs. paroxysmal atrial arrhythmias. In patients with a history of atrial fibrillation diagnostic/billing codes, diagnosis additional data was collected and reviewed (clinical ECG’s), and additional sensitivity analyses were performed as described below. HR was a single measurement obtained as a resting pulse rate measured by hand or with an automatic blood pressure cuff by a qualified study personnel during physical exam at registry enrollment.
The assessment of possible non-sinus rhythm (see adjusted analyses below) was done by querying all available ECG data in the system for patients with previous diagnoses of atrial arrhythmia, reviewing ECG tracings temporally closest to, and surrounding enrollment date (i.e., both before and after the enrollment date). We classified patients as likely or unlikely to be in non-sinus rhythm, and this was used as an excluding factor in a secondary analysis. To quantify beta-blocker exposure for adjusted analyses, we chose to use the average beta-blocker exposure over 6 months prior to enrollment. This was accomplished using pharmacy claims data to generate a beta-blocker exposure metric as previously described [16]. This metric summarizes exposure (both dose and adherence) of all BB medications as a proportion of target exposure for HFrEF (per consensus guidelines). Regarding individual agent use, among patients on BB carvedilol (39%) and metoprolol succinate (38%) were most frequently used, but there were smaller groups of patients using metoprolol tartrate (18%) or another beta-blocker (4%).
Statistical analysis
We first sought to assess previously published genetic loci for HR found by other GWAS studies (in non-heart failure patients) and test for significance in our HFrEF cohort. We reviewed literature for GWAS studies published that identified significant loci for HR. We found five publications [10–14] that identified a total of 43 loci (listed in Additional file 1: Table S1). We tested the association of these genotypes using linear regression adjusted for self-identified race and kinship. For this analysis, we used the Bonferroni correction for 43 multiple comparisons, which yields a critical P value threshold of 1.16 × 10−3.
The primary objective of our study was to identify individual SNPs and genes associated with resting HR, adjusted for race (since this was associated with HR). We used Efficient Mixed-Model Association eXpedited (EMMAX) analyses for genome-wide association analysis [17]. This approach uses a kinship matrix to take into account population structure and relatedness. Associations with P < 5 × 10−8 were considered genome-wide significant [18]. We performed several adjusted and sensitivity analyses to mitigate the contribution of potential confounders and assess the robustness of our findings. First, we repeated our primary analysis excluding patients that may have had non-sinus rhythm (e.g., atrial fibrillation or flutter) upon enrollment. Next, we performed similar analyses adjusted for beta-blocker exposure (quantified as described above).
We secondarily also took a gene-based analytic approach, combining the data from all SNPs within each gene region using the SNP-set kernel-machine association test (SKAT) [19]. This method uses a logistic kernel-machine model, aggregating individual score test statistics of SNPs, and provides a global P value for the set of variants tested that takes into account the joint effect of the SNPs in a given SNP set. Gene regions were defined based upon the GENCODE annotation [20]. Multiple comparisons were accounted for using the false discovery rate method of Benjamini-Hochberg [21].
Results
The study cohort baseline characteristics are shown in Table 1. Overall, the cohort was 35% female and 51% AA and had an average age of 68 years. We tested HR differences by race which revealed a clinically small but statistically significant difference in HR by race, with African Americans having on average around 2 bpm higher rates (70 ± 13 vs. 72 ± 13 bpm; P = 0.0021). As expected, several characteristics varied across the two racial groups, including HF etiology, co-morbidities, and demographics.
Table 1.
Baseline characteristics of the study cohort
| Characteristic | Overall (N = 1060) |
African American (N = 543) |
White (N = 517) |
P |
|---|---|---|---|---|
| Female | 374 (35%) | 220 (41%) | 154 (30%) | 0.001 |
| Age | 68 (± 12) | 65 (± 12) | 71 (± 11) | 0.001 |
| Ejection fraction (%) | 34.9 (± 11) | 33.6 (± 11.4) | 36.2 (± 10.4) | 0.001 |
| Ischemic etiology | 608 (57%) | 267 (49%) | 341 (66%) | 0.001 |
| Hx COPD | 234 (22%) | 114 (21%) | 120 (23%) | 0.375 |
| Hx CKD | 239 (± 23%) | 149 (± 27.4) | 90 (± 17.4) | 0.001 |
| Hx A-Fib | 295 (28%) | 104 (19%) | 191 (37%) | 0.001 |
| Hx stroke/TIA | 129 (12%) | 69 (12.7%) | 60 (11.6%) | 0.375 |
| Hx diabetes | 441 (42%) | 250 (46%) | 191 (37%) | 0.003 |
| Sys BP (mmHg) | 129 ± 23 | 131 ± 24 | 126 ± 22 | 0.002 |
| HR (beats per min.) | 71.1 ± 13 | 72.2 ± 13 | 69.9 ± 13 | 0.007 |
| NTproBNP (ng/L) | 348 (± 374) | 336 (± 386) | 362 (± 360) | 0.001 |
| Creatinine (mg/dL) | 1.29 | 1.36 (± 1.08) | 1.17 (± 0.57) | 0.003 |
| BB exposurea | 0.26 (± 0.29) | 0.26 (± 0.3) | 0.26 (± 0.29) | 0.832 |
aThis is the proportion of target BB exposure over 6 months in patients taking BB
Identified from previous reports of GWAS of HR, we tested 43 previously implicated loci in our cohort of HFrEF patients. In total, the association with HR for four of these SNPs were replicated in our study, with P values ranging from 2.55 × 10−4 to 7.75 × 10−5 (Bonferroni corrected critical P value threshold 1.16 × 10−3). All four of these SNPS were within a single region of chromosome 6, within the gene GJA1 which encodes connexin 43. The SNP ID, P value, and original publication citation for these significant loci are listed in Table 2.
Table 2.
Replication of other GWAS studies in HFrEF patients
Genome-wide analyses of genotype influence on heart rate
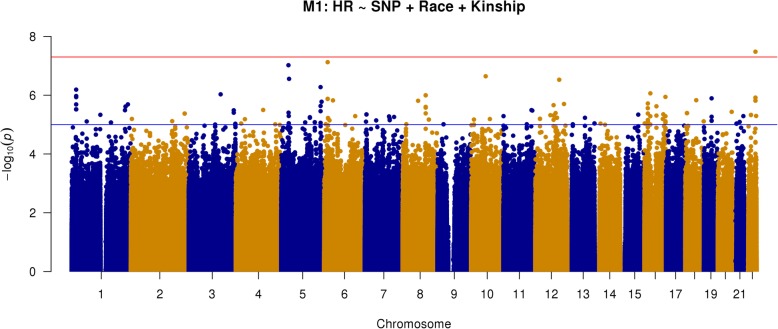
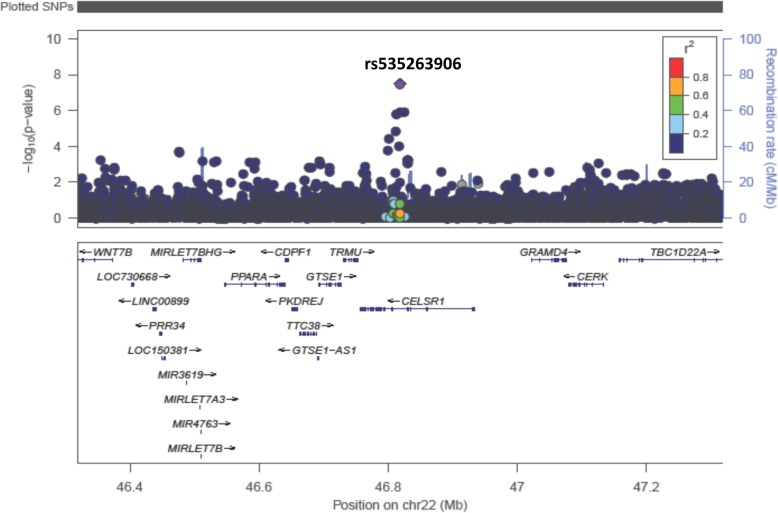
The analysis was adjusted for self-identified race (African American or white) and the analytic method accounted for population stratification and relatedness of individuals (i.e., kinship). These primary results (model 1) are depicted in the Manhattan plot in Fig. 1 (Q-Q plot depicted in Fig. 2). The top 20 SNPs associated with heart rate are listed in Table 3, showing the allele frequencies and effect sizes, and whether the SNP was present in only one racial group or not. One locus, rs535263906 on chromosome 22q13, met the genome-wide statistical significance (p = 3.3 × 10−8). A zoomed in view (1 Mb) of this association peak is shown in Fig. 3. This association peak lies within the gene Cadherin EGF LAG Seven-Pass G-Type Receptor 1 (CELSR1), though there are a number of other genes nearby.
Fig. 1.
Manhattan plot of GWAS results from model 1: SNP + race + kinship (n = 1043; AA = 520, white = 523). Blue reference line: 1 × 10−5; red reference line: 5 × 10−8
Fig. 2.
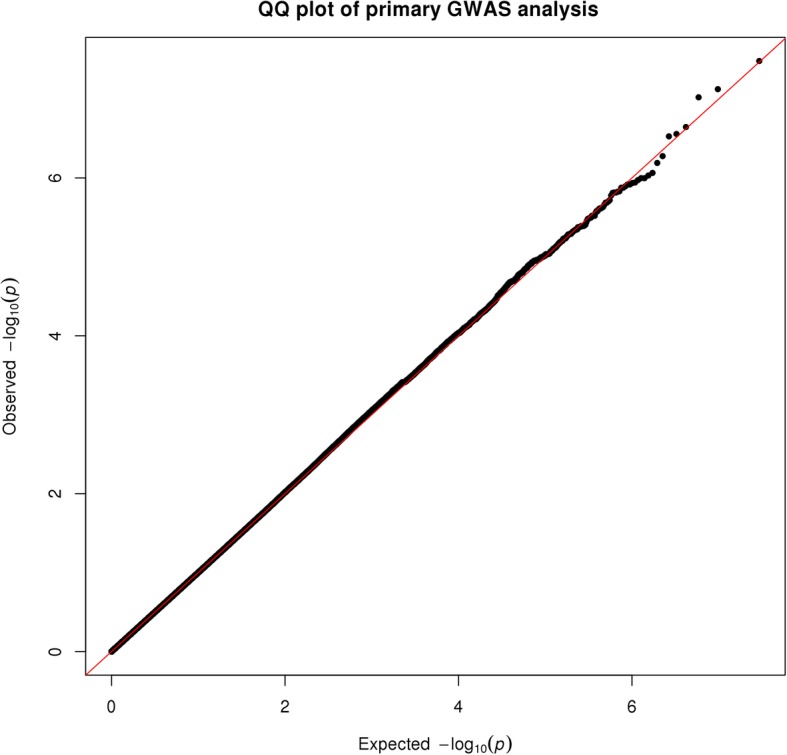
Q-Q plot of primary GWAS analysis
Table 3.
Top 20 GWAS results from model 1: SNP + race + kinship (n = 1043; AA = 520, white = 523)
| SNP | A1 | A2 | MAF_AA | MAF_W | MAF_All | Coef | P value | Group |
|---|---|---|---|---|---|---|---|---|
| rs535263906 | A | G | 0.02381 | NA | 0.02381 | 14.768 | 3.30E−08 | AA only |
| rs149447933 | G | C | 0.01524 | NA | NA | 17.793 | 7.51E−08 | AA only |
| rs541284506 | A | G | 0.01714 | NA | NA | 17.652 | 9.52E−08 | AA only |
| rs11006544 | C | T | 0.01714 | NA | NA | 16.175 | 2.27E−07 | AA only |
| rs112434206 | G | A | 0.02286 | NA | NA | 14.598 | 2.77E−07 | AA only |
| rs11110004 | C | T | 0.01143 | NA | NA | 19.543 | 2.97E−07 | AA only |
| rs114821210 | A | C | 0.01714 | NA | NA | 15.695 | 5.30E−07 | AA only |
| rs74056623 | A | G | 0.05238 | NA | NA | 9.270 | 6.46E−07 | AA only |
| rs148133894 | C | T | 0.00952 | NA | NA | 20.479 | 8.64E−07 | AA only |
| rs189919070 | T | C | 0.00762 | NA | NA | 22.822 | 9.33E−07 | AA only |
| rs74864598 | A | C | 0.09524 | 0.01912 | 0.05725 | 5.793 | 1.01E−06 | Complete |
| rs16917667 | A | G | 0.09524 | 0.01912 | 0.05725 | 5.793 | 1.01E−06 | Complete |
| rs74056624 | A | G | 0.04952 | NA | NA | 9.318 | 1.06E−06 | AA only |
| rs149322277 | T | C | 0.02286 | NA | NA | 13.281 | 1.14E−06 | AA only |
| rs188344082 | A | G | 0.04952 | NA | NA | 9.287 | 1.16E−06 | AA only |
| rs150381023 | C | T | 0.02 | NA | NA | 14.152 | 1.21E−06 | AA only |
| rs150109621 | T | C | 0.02 | NA | NA | 14.152 | 1.21E−06 | AA only |
| rs8105292 | C | T | 0.3371 | 0.1128 | 0.2252 | 3.433 | 1.28E−06 | Complete |
| rs139130723 | G | A | 0.01714 | NA | NA | 15.126 | 1.33E−06 | AA only |
| rs142803096 | C | G | 0.01714 | NA | 0.01714 | 15.126 | 1.33E−06 | AA only |
Fig. 3.
1 MB view of statistically significant peak on chromosome 22 with gene tracks overlaid
There were two additional association peaks that were close to statistical significance in the primary analysis. One was on chromosome 5 centered on rs541284506 (P = 9.5 × 10−8), and another was on chromosome 6 with the strongest SNP being rs149447933 (P = 7.5 × 10−8). These peaks were somewhat broad, did not have clear supporting base of SNPs, and did not locate within a known coding gene; the closest being roughly 200 kb from s149447933 on Chr6 (a non-coding RNA gene, LINC01108). Close up (1 Mb) images of these two peaks are shown in Additional file 2: Figure S1 and Additional file 3: Figure S2. There were an additional 138 SNPs with levels of association considered suggestive (P < 10−5), a full listing of which are included in Additional file 1: Table S2. Finally, we stratified model 1 by race (Additional file 1: Tables S6 and S7).
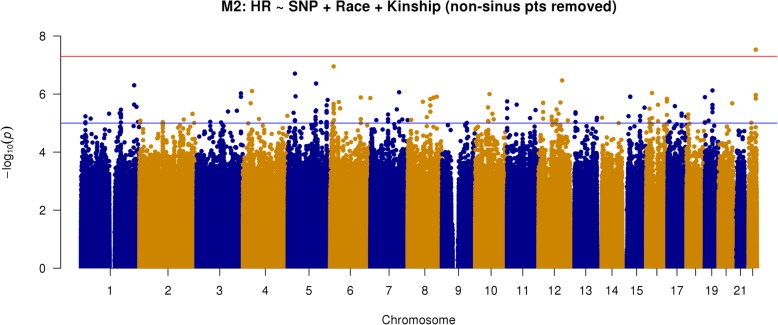
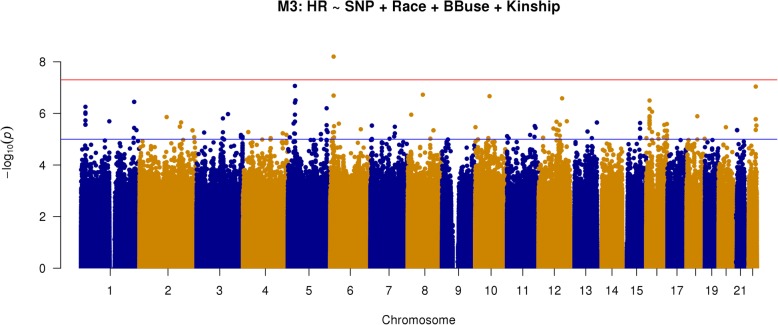
Sensitivity and other additional analyses
We performed several additional genome wide analyses to mitigate any contributions from possible confounding factors and assess the robustness of the above findings. First, we performed a subgroup analysis excluding patients classified as possible non- sinus rhythm. Because ECG was not obtained as part of study enrollment and thus could not guarantee sinus rhythm in all subjects, we performed additional investigations collecting and examining all clinically available ECG in patients with any prior diagnosis of atrial arrhythmia. These patients were classified as possible non-sinus or likely sinus based on ECG evidence of heart rhythm near the time of enrollment. We then repeated our primary statistical analysis excluding patients deemed as possible non-sinus rhythm. This analysis (model 2) has results shown in Fig. 4 and the top 20 loci listed in Table 4. Another key secondary analysis was similar to the primary analysis (i.e., all subjects) but adjusted for beta-blocker exposure (model 3). These results are depicted in Fig. 5 and top loci listed in Table 5. Overall, the results of models 2 and 3 appear similar to the results of the primary analysis (model 1). We still see the same three loci of potential interest though there is variation in terms of priority and whether they meet genome-wide statistical significance. Specifically, the most strongly associated SNP in model 1 was still so for model 2 (rs541284506) but was third in model 3, achieving P = 9.97 × 10−8), while rs149447933 achieved statistical significance in this model (P = 6.29 × 10−9).
Fig. 4.
Manhattan plot of GWAS results from model 2: SNP + race + kinship; excluding possible non-sinus patients (n = 901; AA = 484, white = 417). Blue reference line 1 × 10−5; red reference line 5 × 10−8
Table 4.
Top 20 GWAS results from model 2: SNP + race + kinship; excluding possible non-sinus patients (n = 901; AA = 484, white = 417)
| SNP | A1 | A2 | MAF_AA | MAF_W | MAF_All | Coef | P value | Group |
|---|---|---|---|---|---|---|---|---|
| rs535263906 | A | G | 0.02381 | NA | NA | 15.372 | 2.94E−08 | AA only |
| rs149447933 | G | C | 0.01524 | NA | NA | 18.040 | 1.12E−07 | AA only |
| rs541284506 | A | G | 0.01714 | NA | NA | 18.282 | 1.97E−07 | AA only |
| rs11110004 | C | T | 0.01143 | NA | NA | 19.375 | 3.39E−07 | AA only |
| rs79031501 | C | T | NA | 0.02294 | NA | 14.281 | 4.33E−07 | EA only |
| rs965460 | G | A | NA | 0.02294 | NA | 14.281 | 4.33E−07 | EA only |
| rs114726259 | T | C | NA | 0.02199 | NA | 14.281 | 4.33E−07 | EA only |
| rs148467525 | A | G | 0.01429 | NA | NA | 18.407 | 4.99E−07 | AA only |
| rs8105292 | C | T | 0.3371 | 0.1128 | 0.2252 | 3.687 | 7.52E−07 | Complete |
| rs78829380 | T | C | 0.06571 | NA | NA | 8.326 | 7.89E−07 | AA only |
| rs111681691 | T | C | 0.02381 | 0.0392 | 0.03149 | 8.908 | 8.67E−07 | Complete |
| rs148133894 | C | T | 0.00952 | NA | NA | 20.344 | 9.22E−07 | AA only |
| rs189566544 | C | A | 0.0219 | NA | NA | 14.624 | 9.43E−07 | AA only |
| rs11006544 | C | T | 0.01714 | NA | NA | 15.681 | 9.98E−07 | AA only |
| rs150381023 | C | T | 0.02 | NA | NA | 14.870 | 1.08E−06 | AA only |
| rs150109621 | T | C | 0.02 | NA | NA | 14.870 | 1.08E−06 | AA only |
| rs112434206 | G | A | 0.02286 | NA | NA | 14.067 | 1.20E−06 | AA only |
| rs117130066 | A | G | NA | 0.02677 | NA | 12.323 | 1.23E−06 | EA only |
| rs74866062 | C | A | NA | 0.01625 | NA | 16.806 | 1.24E−06 | EA only |
| rs117289820 | C | G | NA | 0.01625 | 0.01625 | 16.806 | 1.24E−06 | EA only |
Fig. 5.
Manhattan plot of GWAS results from model 3: SNP + race + kinship + BB exposure (n = 990; AA = 494, white = 496). Blue reference line 1 × 10−5; red reference line 5 × 10−8
Table 5.
Top 20 GWAS results from model 3: SNP + race + kinship + BB exposure (n = 990; AA = 494, white = 496)
| SNP | A1 | A2 | MAF_AA | MAF_EA | MAF_All | Coef | P value | Group |
|---|---|---|---|---|---|---|---|---|
| rs149447933 | G | C | 0.01524 | NA | NA | 19.714 | 6.29E−09 | AA only |
| rs541284506 | A | G | 0.01714 | NA | NA | 17.634 | 8.59E−08 | AA only |
| rs535263906 | A | G | 0.02381 | NA | NA | 14.516 | 9.12E−08 | AA only |
| rs187251765 | A | C | 0.01333 | NA | NA | 19.092 | 1.88E−07 | AA only |
| rs139130723 | G | A | 0.01714 | NA | NA | 16.629 | 2.04E−07 | AA only |
| rs142803096 | C | G | 0.01714 | NA | NA | 16.629 | 2.04E−07 | AA only |
| rs11006544 | C | T | 0.01714 | NA | NA | 16.148 | 2.15E−07 | AA only |
| rs11110004 | C | T | 0.01143 | NA | NA | 19.544 | 2.60E−07 | AA only |
| rs112434206 | G | A | 0.02286 | NA | NA | 14.507 | 3.12E−07 | AA only |
| rs6498482 | T | C | 0.3752 | 0.588 | 0.4814 | − 2.987 | 3.16E−07 | Complete |
| rs143554223 | G | A | 0.01333 | NA | NA | 19.333 | 3.56E−07 | AA only |
| rs148467525 | A | G | 0.01333 | NA | NA | 19.333 | 3.56E−07 | AA only |
| rs188482801 | A | C | 0.03238 | NA | NA | 12.604 | 3.81E−07 | AA only |
| rs74056623 | A | G | 0.05238 | NA | NA | 9.378 | 5.55E−07 | AA only |
| rs114821210 | A | C | 0.01714 | NA | NA | 15.541 | 6.32E−07 | AA only |
| rs7188980 | C | T | 0.4143 | 0.6195 | 0.5167 | 2.859 | 6.63E−07 | Complete |
| rs148133894 | C | T | 0.00952 | NA | NA | 20.392 | 8.60E−07 | AA only |
| rs74056624 | A | G | 0.04952 | NA | NA | 9.350 | 9.24E−07 | AA only |
| rs188344082 | A | G | 0.04952 | NA | NA | 9.389 | 1.03E−06 | AA only |
| rs189919070 | T | C | 0.00762 | NA | NA | 22.630 | 1.06E−06 | AA only |
We also performed an additional subgroup analysis restricted to patients with EF ≤ 35% (n = 589). The analysis of this much smaller group yielded no variants that met whole genome significance. There was one locus with two SNPs in proximity to each other, rs76008716 and rs57957360, which were near statistical significance (P = 5.4 × 10−8) and had not appeared in the top loci of other analyses. We performed a sensitivity analysis treating HR as an ordinal variable (rather than continuous variable), thereby mitigating the influence of very low or very high values and not overestimating precision of measure. These results were overall similar to the above with two of the top three SNPs being the same (Additional file 1: Table S5).
Gene-wise analysis of heart rate
As an alternative approach to try to identify genes impacting heart rate, we performed another genome-wide analysis testing gene regions rather than individual SNPs. A total of 42,774 genes/functional genomic regions were defined based upon the ENCODE project annotation. The critical P value for global error rate was 1.17 × 10−6, and overall results are depicted in Additional file 4: Figure S3 (Q-Q plot depicted in Additional file 5: Figure S4). No genes met genome-wide significance. The top 40 genes, which had P < 0.001, are shown in Additional file 1: Table S3. There were four genes with P values < 1 × 10−4. All four of these gene regions are currently of unknown function (Additional file 1: Table S4). One gene on chromosome 12 (C12orf74) was predicted to be a protein-encoding gene, though its structure and function remain unknown. The other three gene-regions of interest were in non-coding RNA genes, also of unknown function.
Discussion
Although similar types of studies have been performed previously in population samples [10–13], our study is the first that we know of to attempt to identify genomic regions that influence HR in stable patients with HFrEF. Analysis of this diverse patient cohort revealed a modest but statistically significant difference in HR between self-identifying white and AAs (with AA showing a slightly higher HR) as well as three genomic loci at or near genome-wide significance in at least one analysis for association to HR, of particular interest is a novel locus on Chr. 22q13 in the gene CELSR1.
Putting this study in context of pre-existing work, we were able to replicate one of the previously published genetic loci, in the gene GJA1, which had been reported to be associated with resting HR in multiple studies. This not only reconfirms the validity of this association but also suggests that GJA1 genetic variation may have impact on HR in patients with HFrEF. High resting heart rate is a well-recognized modifiable risk factor for cardiovascular morbidity and mortality in heart failure patients [3–6]. GJA1 encodes connexin 43, a connexin family protein and a major component of the cardiac gap junction which is a central in the electrical coupling of cardiac myocytes [22]. The fact that we did not replicate the other GW significant hits from previous studies could be due in part to the relatively smaller size of our cohort, but importantly, there are design differences that may also contribute to differential findings. Most important is that this cohort was all the HFrEF patients, and the genetic factors influencing HR may be different in the setting of this disease. This is in fact the primary reason we performed this analysis, to attempt to identify HR mechanism relevant to HF that may thus impact therapy or patient outcomes. Another important difference is the fact that our cohort is racially diverse while most previous studies were in only patients of European ancestry. This diverse cohort allows us to potentially detect important associations that may be amplified or selective to AA patients and is another potential reason for differential finding in ours vs. previous studies. The strongest associated loci are in fact specific to African American patients in this cohort.
The SNP-wise GWA analysis identified two SNPs that met whole genome significance for association with HR in one or more models (see Tables 3–5) and another that was very close in each analysis. The strongest association appeared to be for the association peak on Chr 22. The peak SNP in this analysis (rs535263906) was only present and tested in African American patient samples, and while imputed (rather than directly genotyped), it was of high imputation confidence (R2 = 0.816) and had a supporting peak of SNPs beneath it. This association peak is near a large number of genes but lies almost completely within CELSR1, which encodes a receptor of the cadherin super-family and appears to have gene expression (mRNA) in a wide range of tissues including in cardiac and smooth muscle cells (The Genotype-Tissue Expression [GTEx] project). The association peak encompasses most of the 5′ half of CELSR1, so attempting to infer possible functional impact of the yet unidentified causative variant (presumably linked to rs535263906 but accounting for the phenotype association) would be speculative and remains the work of future investigation. Interestingly, CELSR1 has been reported in other GWAS studies as being associated with a variety of traits; these include stroke [23] and a suggestive association with fenofibrate response in diabetics [24]. Further investigation into this gene and the other candidates is needed to assess their possible cardiac functional impact. While whole-genome significance was met, these findings should be viewed as preliminary until they can be tested for validation in another data set. Unfortunately, another similar data set, particularly including African Americans with HFrEF is not readily available to the investigative team.
Although no statistical significance was reached in the gene-wise analysis, these results can be viewed as a prioritization list for possible association to HR among HF patients with HFrEF. Similarly, the many additional individual SNPs that were in the range of possible interest for association with HR (i.e., having P values < 10−6.) may be of value for future investigation. A high proportion of these loci seemed specific to AA. This could be due to a higher number of SNPs in AA, statistical chance, or perhaps because HR is under a stronger genetic influence in this group of patients. The analysis of very low EF (< 35%) yielded two additional SNPs of interests, rs76008716 and rs57957360, which were very near statistical significance (P = 5.4 × 10−8). These loci are located in an intergenic region on chromosome 5 and are of unclear biological significance at this point. The results of this much smaller subcohort should be interpreted with caution until validated externally.
This study has several limitations. First, it is derived from a single center cohort of modest size for a GWAS. Mitigating this is that we are modeling a continuous variable as endpoint which provides more statistical power compared to dichotomous or event-driven analyses. In terms of phenotype, ECG was not performed on the day of enrollment in our study, and pulse rate was used as our HR measure. For most patients, pulse rate should be a reliable measure of HR but this may have differences compared to ECG-derived measures. Moreover, the lack of an ECG makes it impossible for us to state with certainty that subjects were in sinus rhythm at the time of assessment, but we have worked hard to mitigate this risk, including additional analyses excluding patients with any history of atrial arrhythmia. Another potential concern is that we used EF < 50% as enrollment criteria to categorize patients as HFrEF. While this is no longer the standard, it was so at the time of the study initiation and we performed additional analyses to assess any potential impact. Finally, while we adjusted for beta-blocker exposure, we did not have an actual level the day of enrollment. Despite this, the medication exposure metric used has been previously shown to correlate to clinical outcomes and inversely correlate with HR [25] and thus is likely to be a good estimate of true exposure.
Conclusions
In summary, HR in the setting of HFrEF appears to be impacted by genetic factors. One previous candidate gene was confirmed in the setting of HFrEF (GJA1), and GWAS of HR identified several novel genomic loci associated with HR, particularly a statistically significant peak in the gene CELSR1. These novel candidate genes for HR in the setting of HFrEF require additional investigation and validation.
Additional files
Table S1. Loci from of other GWAS studies tested in HFrEF patients. Table S2. Additional GWAS results of potential interest (P < 10− 5) from model 1 (n = 1043; AA = 520, white = 523). Table S3. Association of genes with heart rate in EF patients (from gene-wise analysis). Table S4. Classification of genes of interest from gene-wise analysis. Table S5. Sensitivity analysis of HR an ordinal variable, n = 1043 (AA 520, EA 523). Table S6. Top 20 SNPs from 520 AA patients: model 1 (SNP + race + kinship). Table S7. Top 20 SNPs from 523 EA patients: model 1 (SNP + race + kinship) (DOCX 59 kb)
Figure S1. Close up (1 Mb) Manhattan plot of Chr. 5 association peak (TIF 14502 kb)
Figure S2. Close up (1 Mb) Manhattan plot of Chr. 6 association peak (TIF 2869 kb)
Figure S3. Manhattan Plot of the gene-wise analysis of heart rate. Blue reference line: 1x10-5, Red reference line: 1x10-4. (TIFF 14100 kb)
Figure S4. Q-Q Plot of SKAT P values for approximately 43,000 genes from the gene-wise analysis of heart rate. (TIFF 16400 kb)
Acknowledgements
Not applicable
Funding
This study was funded by Amgen Inc., Thousand Oaks, California. The parent registry, (the Henry Ford Heart Failure Genomic Registry) was supported in part by grants from the Henry Ford Research Foundation (Lanfear) and the National Institutes of Health (NHLBI; Lanfear, R01HL103871). Dr. Lanfear’s time is supported in part by grants from the NIH (NHLBI; R01HL103871 and R01HL132154).
Availability of data and materials
The genetic dataset is available in the database of Genotypes and Phenotypes (dbGaP) repository (title “Impact of Race and Genetic Factors on Beta Blocker Effectiveness in Heart Failure”) with certain restrictions due to limitations within the consent form.
Abbreviations
- AA
African American
- BB
Beta-blocker
- BPM
Beats per minute
- COPD
Chronic obstructive pulmonary disease
- ECG
Electrocardiogram
- EF
Ejection fraction
- EMR
Electronic medical record
- GenHRate
Genetics of Heart Rate Observational Study
- HAP
Health Alliance Plan
- HFMG
Henry Ford Medical Group.
- HF
Heart failure
- HFHS
Henry Ford Health System
- HFrEF
Heart failure with reduced ejection fraction
- HR
Heart rate
- SNP
Single nucleotide polymorphisms
Author’s contributions
KE, HW, JM, AH, CD, and DL participated in the design of the study and drafting of the manuscript. KE, HW, and DL participated in the coordination of the study. JL, RS, and HG performed the statistical analysis and also participated in the drafting of the manuscript. DL, JL, and HG performed data interpretation. DL secured funding. All authors read and approved the final manuscript.
Ethics approval and consent to participate
The current study was accomplished using data from the Henry Ford Heart Failure Pharmacogenomics Registry. The registry was approved by the local ethics committee (Henry Ford Hospital Institutional Review Board) and registry participants provided written informed consent.
Consent for publication
Our manuscript does not contain any individual person’s data.
Competing interests
Several of the authors are currently employed by Amgen and a grant from Amgen to Henry Ford Hospital (LANFEAR PI) supported the study. KE, JL, RS, and HG have no disclosures to report. HSW is an employee of Amgen Inc. and reports stock ownership in Amgen Inc. and Teva Pharmaceutical Industries Ltd. AH is an employee and stockholder of Amgen Inc. JM was previously employed by Amgen Inc. during the development of the manuscript. CD is an employee of Amgen Inc. DL serves as a consultant for Amgen Inc., Ortho-McNeill, Abbott, Akros, DCRI, reports ownership in Hridaya, and has received research grants from Amgen Inc., Janssen Pharmaceuticals Inc., Novartis Corporation, and Akros.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Kaleigh L. Evans, Email: Kevans22@uic.edu
Heidi S. Wirtz, Email: hwirtz@amgen.com
Jia Li, Email: jli4@hfhs.org.
Ruicong She, Email: rshe1@hfhs.org.
Juan Maya, Email: maya.juan1@gmail.com.
Hongsheng Gui, Email: hgui1@hfhs.org.
Andrew Hamer, Email: ahamer@amgen.com.
Christophe Depre, Email: cdepre@amgen.com.
David E. Lanfear, Phone: 313-916-6375, Email: DLANFEA1@hfhs.org
References
- 1.Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics--2015 update: a report from the American Heart Association. Circulation. 2015;131:e29–322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 2.Webster G, Zhang J, Rosenthal D. Comparison of the epidemiology and co-morbidities of heart failure in the pediatric and adult populations: a retrospective, cross-sectional study. BMC Cardiovasc Disord. 2006;6:23. doi: 10.1186/1471-2261-6-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McAlister FA, Wiebe N, Ezekowitz JA, Leung AA, Armstrong PW. Meta-analysis: Β-blocker dose, heart rate reduction, and death in patients with heart failure. Ann Intern Med. 2009;150:784–794. doi: 10.7326/0003-4819-150-11-200906020-00006. [DOI] [PubMed] [Google Scholar]
- 4.Flannery G, Gehrig-Mills R, Billah B, Krum H. Analysis of randomized controlled trials on the effect of magnitude of heart rate reduction on clinical outcomes in patients with systolic chronic heart failure receiving beta-blockers. Am J Cardiol. 2008;101:865–869. doi: 10.1016/j.amjcard.2007.11.023. [DOI] [PubMed] [Google Scholar]
- 5.Lechat P, Hulot J-S, Escolano S, et al. Heart rate and cardiac rhythm relationships with bisoprolol benefit in chronic heart failure in CIBIS II trial. Circulation. 2001;103:1428. doi: 10.1161/01.CIR.103.10.1428. [DOI] [PubMed] [Google Scholar]
- 6.Swedberg K, Komajda M, Böhm M, et al. Ivabradine and outcomes in chronic heart failure (SHIFT): a randomised placebo-controlled study. Lancet. 2010;376:875–885. doi: 10.1016/S0140-6736(10)61198-1. [DOI] [PubMed] [Google Scholar]
- 7.Nolte IM, Jansweijer JA, Riese H, et al. A comparison of heritability estimates by classical twin modeling and based on genome-wide genetic relatedness for cardiac conduction traits. Twin Res Hum Genet. 2017;20:489–498. doi: 10.1017/thg.2017.55. [DOI] [PubMed] [Google Scholar]
- 8.Jensen MT, Wod M, Galatius S, Hjelmborg JB, Jensen GB, Christensen K. Heritability of resting heart rate and association with mortality in middle-aged and elderly twins. Heart. 2018;104:30–36. doi: 10.1136/heartjnl-2016-310986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kurnik D, Cunningham AJ, Sofowora GG, et al. GRK5 Gln41Leu polymorphism is not associated with sensitivity to beta (1)-adrenergic blockade in humans. Pharmacogenomics. 2009;10:1581–1587. doi: 10.2217/pgs.09.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Eijgelsheim M, Newton-Cheh C, Sotoodehnia N, et al. Genome-wide association analysis identifies multiple loci related to resting heart rate. Hum Mol Genet. 2010;19:3885–3894. doi: 10.1093/hmg/ddq303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Deo R, Nalls MA, Avery CL, et al. Common genetic variation near the connexin-43 gene is associated with resting heart rate in African Americans: a genome-wide association study of 13,372 participants. Heart Rhythm. 2013;10:401–408. doi: 10.1016/j.hrthm.2012.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kilpelainen TO Genome-wide association studies and resting heart rate. J Electrocardiol. 2016;49:860–863. doi: 10.1016/j.jelectrocard.2016.07.022. [DOI] [PubMed] [Google Scholar]
- 13.Mezzavilla M, Iorio A, Bobbo M, et al. Insight into genetic determinants of resting heart rate. Gene. 2014;545:170–174. doi: 10.1016/j.gene.2014.03.045. [DOI] [PubMed] [Google Scholar]
- 14.van den Berg ME, Warren HR, Cabrera CP, et al. Discovery of novel heart rate-associated loci using the exome Chip. Hum Mol Genet. 2017;26:2346–2363. doi: 10.1093/hmg/ddx113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Das S, Forer L, Schonherr S, et al. Next-generation genotype imputation service and methods. Nat Genet. 2016;48:1284–1287. doi: 10.1038/ng.3656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lanfear DE, Hrobowski T, Peterson EL, et al. Association of beta blocker exposure with outcomes in heart failure patients differs between African American and white patients. Circ Heart Fail. 2012;5:202–208. doi: 10.1161/CIRCHEARTFAILURE.111.965780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kang HM, Sul JH, Service SK et al. Variance component model to account for sample structure in genome-wide association studies. Nat Genet. 2010;42:348–354. doi: 10.1038/ng.548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kanai M, Tanaka T, Okada Y. Empirical estimation of genome-wide significance thresholds based on the 1000 genomes project data set. J Hum Genet. 2016;61:861–866. doi: 10.1038/jhg.2016.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wu MC, Kraft P, Epstein MP, et al. Powerful SNP-set analysis for case-control genome-wide association studies. Am J Hum Genet. 2010;86:929–942. doi: 10.1016/j.ajhg.2010.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Harrow J, Frankish A, Gonzalez JM, et al. GENCODE: the reference human genome annotation for the ENCODE project. Genome Res. 2012;22:1760–1774. doi: 10.1101/gr.135350.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Benjamini Y, Drai D, Elmer G, Kafkafi N, Golani I. Controlling the false discovery rate in behavior genetics research. Behav Brain Res. 2001;125:279–284. doi: 10.1016/S0166-4328(01)00297-2. [DOI] [PubMed] [Google Scholar]
- 22.Rohr S. Role of gap junctions in the propagation of the cardiac action potential. Cardiovasc Res. 2004;62:309–322. doi: 10.1016/j.cardiores.2003.11.035. [DOI] [PubMed] [Google Scholar]
- 23.Yamada Y, Fuku N, Tanaka M, et al. Identification of CELSR1 as a susceptibility gene for ischemic stroke in Japanese individuals by a genome-wide association study. Atherosclerosis. 2009;207:144–149. doi: 10.1016/j.atherosclerosis.2009.03.038. [DOI] [PubMed] [Google Scholar]
- 24.Rotroff DM, Pijut SS, Marvel SW, et al. Genetic variants in HSD17B3, SMAD3, and IPO11 impact circulating lipids in response to fenofibrate in individuals with type 2 diabetes. Clin Pharmacol Ther. 2018;103:712–721. doi: 10.1002/cpt.798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lanfear DE, Peterson E, Wells K, Williams LK. Discharge medication status compares poorly with claims-based outpatient medication exposure estimates. Washington D.C: AHA Quality of Care and Outcomes Research; 2011. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Loci from of other GWAS studies tested in HFrEF patients. Table S2. Additional GWAS results of potential interest (P < 10− 5) from model 1 (n = 1043; AA = 520, white = 523). Table S3. Association of genes with heart rate in EF patients (from gene-wise analysis). Table S4. Classification of genes of interest from gene-wise analysis. Table S5. Sensitivity analysis of HR an ordinal variable, n = 1043 (AA 520, EA 523). Table S6. Top 20 SNPs from 520 AA patients: model 1 (SNP + race + kinship). Table S7. Top 20 SNPs from 523 EA patients: model 1 (SNP + race + kinship) (DOCX 59 kb)
Figure S1. Close up (1 Mb) Manhattan plot of Chr. 5 association peak (TIF 14502 kb)
Figure S2. Close up (1 Mb) Manhattan plot of Chr. 6 association peak (TIF 2869 kb)
Figure S3. Manhattan Plot of the gene-wise analysis of heart rate. Blue reference line: 1x10-5, Red reference line: 1x10-4. (TIFF 14100 kb)
Figure S4. Q-Q Plot of SKAT P values for approximately 43,000 genes from the gene-wise analysis of heart rate. (TIFF 16400 kb)
Data Availability Statement
The genetic dataset is available in the database of Genotypes and Phenotypes (dbGaP) repository (title “Impact of Race and Genetic Factors on Beta Blocker Effectiveness in Heart Failure”) with certain restrictions due to limitations within the consent form.