Abstract
Background
In multiple sclerosis (MS), half of affected people are unemployed within 10 years of diagnosis. The aim of this study was to assess the economic impact of MS in adult subjects with relapsing-remitting MS (RRMS) and primary progressive MS (PPMS).
Methods
A multicenter, non-interventional, cross-sectional study was conducted. The Expanded Disability Status Scale (EDSS) and the 23-item Multiple Sclerosis Work Difficulties Questionnaire (MSWDQ-23) were used to assess disability and work performance, respectively. Only indirect costs were considered using the human capital method, including work costs. Professional support costs and informal caregivers’ costs were also estimated.
Results
A total of 199 subjects were studied (mean age: 43.9 ± 10.5 years, 60.8% female, 86.4% with RRMS). Median EDSS score was 2.0 (interquartile range: 1.0–3.5) and median MSWDQ-23 total score was 31.5 (15.2, 50.0). The number of employed subjects decreased after MS diagnosis from 70.6 to 47.2%, and the number of retired people increased (23.6%). Mean age of retirement was 43.6 ± 10.5 years. Ten percent of the population had sick leaves (absenteeism was seen in 90.9% of the student population and 30.9% of the employed population). Professional support in their daily life activities was needed in 28.1% of subjects. Costs for sick leave, work absenteeism, premature retirement and premature work disability/pensioner were €416.6 ± 2030.2, €763.4 ± 3161.8, €5810.1 ± 13,159.0 and €1816.8 ± 9630.7, respectively. Costs for professional support and informal caregiving activities were €1026.93 ± 4622.0 and €1328.72, respectively.
Conclusions
MS is responsible for a substantial economic burden due to indirect and informal care costs, even in a population with low physical disability.
Keywords: Multiple sclerosis, Disability, Costs, Burden of illness, Caregiver
Background
Multiple sclerosis (MS) is a chronic autoimmune neurological disease with a high impact on the health-related quality of life of individuals, their families and society [1–5]. MS is typically diagnosed in young, active people between 20 and 40 years of age [6]. Therefore, the disease may hinder ability to maintain studies and work [1–4]. According to the Global MS Employment Report 2016, 43% of unemployed people with MS quit their employment in the first 3 years after diagnosis and 62% stated that fatigue was the main reason [7]. In addition, pwMS will require caregiving due to disability progression, mostly provided by informal caregivers, such as partners or other relatives [5].
Total average annual costs were €41,212 ± €18,761 in an observational study of 1152 pwMS and 265 caregivers conducted in 19 countries [3]. Over half of total costs were associated with direct medical costs, followed by indirect costs (€17,492) and direct non-medical costs (€2157). In some European countries, MS caregivers provide 150 h a month of care to pwMS, the equivalent of full-time employment [1]. The mean annual cost per patient in Spain was €30,050 [8]. Sicras et al. found that only 30% of MS people were employed or self-employed [9]. More than 30% of pwMS had an early retirement, in most cases due to disability. Indirect costs in Spain accounted for between 24 and 35% of disease costs, increasing as disability advanced, and reaching over €15,779 in subjects essentially restricted to a wheelchair [8]. However, available data related to the economic burden of MS, especially limitations in work activities and job performance remains limited. The objective of this study was to assess the indirect costs and informal care costs of MS in a sample of pwMS in Spain.
Methods
Study design
A non-interventional, cross-sectional study in subjects with relapsing-remitting (RRMS) and primary-progressive MS (PPMS) according to McDonald 2010 criteria was conducted (W-IMPACT study) [10, 11]. Nineteen MS units across Spain were invited to participate for their good clinical practice and expertise conducting non-interventional research by the study steering committee. Investigators included the first ten consecutive subjects that met the inclusion criteria. Competitive recruitment was established among centers.
Clinical variables
Disability was assessed using the Expanded Disability Status Scale (EDSS) [12]. Total score ranges from 1 (no disability) to 10 (death due to MS). The 29-item Multiple Sclerosis Impact Scale (MSIS-29) was used to measure the physical and the psychological impact of MS from the patients’ perspective [13]. Physical and psychological impact scores range from 20 to 80 and from 9 to 36, respectively. Higher scores indicate greater impact. Work performance related to physical, cognitive and psychological dimensions was studied with the 23-item Multiple Sclerosis Work Difficulties Questionnaire (MSWDQ-23) [11, 14]. Scores range from 0 to 100 with higher values indicating greater workplace problems [14]. When possible, caregivers completed the Caregiver Strain Index (CSI), a self-rated questionnaire for measuring the perceived level of burden [15]. A total score of seven or higher indicates a high level of caregiver burden.
Healthcare resources and costs
Cost descriptions were summarized in the student and employed populations, separately. Only indirect and informal care costs of MS were included in the study analysis. Indirect costs were calculated using the method of human capital where the production of a person is valued at the market price. Indirect costs for employed people were considered as the gross salary per hour, and for unemployed subjects as the minimum salary per hour, in order to avoid underestimating the indirect costs. The cost of pwMS who had a sick leave during the last year was calculated by multiplying the number of days lost by the salary indicated in the employment status section. The cost of lost study hours in people who were studying at the time of the study was calculated as the lost hours per week multiplied by 52. Costs of premature retirement and premature work disability/pensioner were calculated as the indicated annual salary.
PwMS who needed to be accompanied by a formal caregiver were considered in the study by also taking into account the type of resource used, the number of hours per week and the number of weeks they required the resource in the last year. Cost was calculated for each service using the indicated cost multiplied by 12. Costs of informal caregivers were calculated by multiplying the number of hours of work spent without working or with reduced productivity and the days of absence from work by the salary.
Additional costs such as direct non-healthcare costs (transportation and home or car modifications) and direct healthcare costs (use of non-reimbursed devices and aids, private physiotherapy and private psychological treatment) were calculated by multiplying the resources used per subject by their unit cost. All these unit costs were obtained from the health costs database eSalud [16]. All costs were calculated in euros per subject per year based on EDSS score and updated with the Consumer Price Index (CPI).
Statistical analysis
Continuous variables were described by the number of available values, mean, standard deviation, and median, 25th percentile (P25), 75th percentile (P75), minimum and maximum values. Categorical variables were described as the total number of available values and relative percentage per subgroup of interest.
Results
A total of 199 pwMS were included in the study. Subjects were predominantly female (60.2%), with a diagnosis of RRMS (86.1%) and a mean age of 43.9 ± 10.5 years. The median EDSS score was 2.0 (interquartile range 1.0, 3.5). Table 1 shows the main demographic and clinical characteristics of the sample.
Table 1.
Demographic and clinical characteristics
| Total (n = 199) | |
|---|---|
| Age (years); mean (SD) | 43.9 (10.5) |
| Gender (female); n (%) | 121 (60.8%) |
| Educational level; n (%) | |
| -Primary | 32 (16.1%) |
| -Secondary | 88 (44.2%) |
| -University/Postgraduate studies | 79 (39.7%) |
| Type of MS; n (%) | |
| -RRMS | 172 (86.4%) |
| -PPMS | 27 (13.6%) |
| Time since diagnosis (years); mean (SD) | 9.6 (7.2) |
| Number of relapses in the last 2 years; mean (SD) | 0.6 (0.9) |
| Time since last relapse (months); mean (SD) | 53.9 (56.1) |
| Patients on DMT; n (%) | 160 (80.4%) |
| EDSS score; median (IRQ) | 2.0 (1.0, 3.5) |
| MSWDQ-23 total score; median (IRQ) | 31.5 (15.2, 50.0) |
DMT Disease-modifying therapies, EDSS Expanded Disability Status Scale, IRQ Interquartile range, MS Multiple sclerosis, MSWDQ-23 23-item Multiple Sclerosis Working Difficulties, PPMS Primary progressive multiple sclerosis, RRMS Relapsing-remitting multiple sclerosis, SD Standard deviation
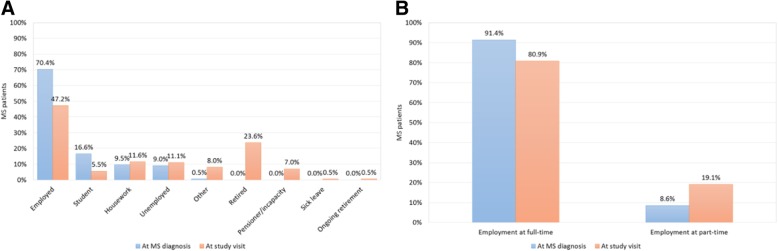
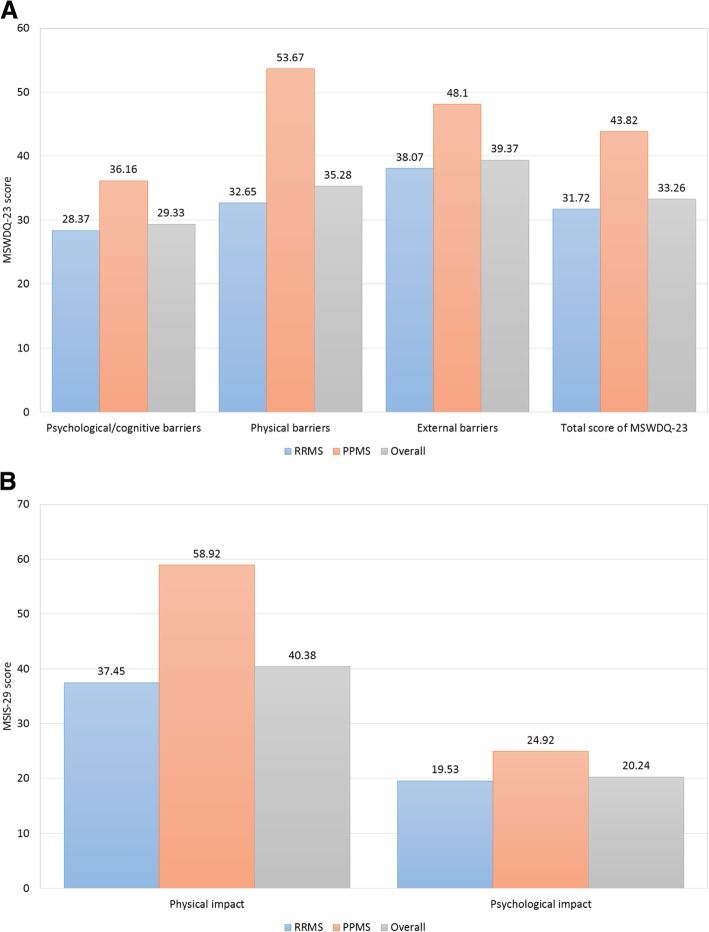
Most subjects (70.4%) were employed at MS diagnosis, but only 47.2% were employed at the time of the study visit (Fig. 1). Mean time between MS diagnosis and the study visit was 9.6 years (SD 7.2). The mean age for retirement was 43.6 ± 10.5 years, with disease progression as the main reason (95.7%). According to the results collected from the MSWDQ-23 and MSIS-29 questionnaires, the main impact of MS on subjects’ activities was due to external and physical barriers, especially in those patients with PPMS (Fig. 2).
Fig. 1.
Employment status: At MS diagnosis (a) and At study visit (b)
Fig. 2.
Impact of MS on patients: MSWDQ-23 (a) and MSIS-29 (b) questionnaires
During the last year prior to the study visit, the mean free time that subjects had was 45.7 ± 35.8 h/week. PwMS dedicated 35.5 ± 17.9 h/week to their studies and 36.2 ± 10.8 h/week to their work activity. Sick leaves were reported in 10.1% of the total MS population and absenteeism was seen in 90.9% of the student population and 30.9% of the employed population (Table 2).
Table 2.
Impact of MS on academic and work activity during the last year
| Student pwMS | |||||
|---|---|---|---|---|---|
| EDSS 0–1 (n = 7) |
EDSS 1.5–3.0 (n = 4) |
EDSS 3.5–5.5 (n = 0) |
EDSS ≥ 6 (n = 0) |
Overall (n = 11) |
|
| Academic absenteeism; n (%) | 0 (0%) | 1 (25.0%) | 0 (0.0%) | 0 (0%) | 1 (9.1%) |
| Time off study (hours/year); mean (SD) | 0 (0) | 13.0 (26.0) | 0 (0) | 0 (0) | 4.7 (15.7) |
| Lost time percentage in a week compared to a normal week (hours); mean (SD) | 0 (0) | 0.4 (0.8) | 0 (0) | 0 (0) | 0.2 (0.5) |
| Employed pwMS | |||||
|
EDSS 0–1 (n = 45) |
EDSS 1.5–3.0 (n = 39) |
EDSS 3.5–5.5 (n = 10) |
EDSS ≥ 6 (n = 0) |
Overall (n = 94) |
|
| Sick leave; n (%) | 5 (11.1%) | 11 (28.2%) | 4 (40.0%) | 0 (0%) | 20 (21.3%) |
| Time on sick leave (days); mean (SD) | 1.9 (6.4) | 28.9 (74.0) | 37.7 (93.3) | 0 (0) | 16.9 (57.6) |
| Work absenteeism; n (%) | 12 (26.7%) | 14 (35.9%) | 3 (30.0%) | 0 (0%) | 29 (30.9%) |
| Time lost from work (hours/year); mean (SD) | 101.7 (344.9) | 281.9 (618.3) | 312.0 (914.9) | 0 (0) | 198.8 (549.8) |
| Lost time percentage in a week compared to a normal week (hours); mean (SD) | 5.2 (16.2) | 14.6 (30.5) | 11.0 (31.4) | 0 (0) | 9.7 (24.9) |
| Premature retirement and work disability | |||||
|
EDSS 0–1 (n = 67) |
EDSS 1.5–3.0 (n = 77) |
EDSS 3.5–5.5 (n = 34) |
EDSS ≥ 6 (n = 21) |
Overall (n = 199) |
|
| Premature retirement due to MS; n (%) | 4 (6.0%) | 15 (19.5%) | 10 (29.4%) | 16 (76.2%) | 45 (22.6%) |
| Premature work disability/pensioner due to MS; n (%) | 0 (0%) | 7 (9.1%) | 5 (14.7%) | 2 (9.5%) | 14 (7.0%) |
EDSS Expanded Disability Status Scale, MS Multiple sclerosis, pwMS People with multiple sclerosis, SD Standard deviation
About a third (36.2%) of pwMS went to the study visit accompanied by a formal caregiver and almost half (44.7%) by an informal one (Table 3). The most frequent informal caregiving was provided by a direct relative (55.82%) (Table 3). The mean time spent on caregiving activities for these informal caregivers was: husband/wife (212.14 ± 516.86 h/year); other relative (154.19 ± 503.18 h/year), and neighbor (3.02 ± 21.97 h/year). A total of 72 caregivers completed the CSI (mean total score was 3.9 ± 3.4). The prevalence of a high level of strain was 23.6% (n = 17).
Table 3.
Professional and informal support
| Professional support | |||||
|---|---|---|---|---|---|
| EDSS 0–1 (n = 67) |
EDSS 1.5–3.0 (n = 77) |
EDSS 3.5–5.5 (n = 34) |
EDSS ≥ 6 (n = 21) |
Overall (n = 199) |
|
| Formal caregiver at study visit; n (%) | 15 (22.4%) | 25 (32.5%) | 20 (58.8%) | 12 (57.1%) | 72 (36.2%) |
| Support staff (professionals or transportation) paid by the patient; n (%) | 5 (7.5%) | 25 (32.5%) | 14 (41.2%) | 12 (57.1%) | 56 (28.1%) |
| Type of professional; n (%) | |||||
| - Caregiver | 0 (0%) | 0 (0%) | 1 (2.9%) | 0 (0%) | 1 (0.5%) |
| - Physiotherapist | 2 (3.0%) | 15 (19.5%) | 10 (29.4%) | 5 (23.8%) | 32 (16.1%) |
| - Person to do housework | 2 (3.0%) | 8 (10.4%) | 3 (8.8%) | 5 (23.8%) | 18 (9.0%) |
| - Private ophthalmologist | 0 (0%) | 2 (2.6%) | 1 (2.9%) | 1 (4.8%) | 4 (2.0%) |
| - Private neurologist | 0 (0%) | 1 (1.3%) | 0 (0%) | 0 (0%) | 1 (0.5%) |
| - Private psychologist | 2 (3.0%) | 5 (6.5%) | 1 (2.9%) | 0 (0%) | 8 (4.0%) |
| - Taxi driver | 1 (1.5%) | 4 (5.2%) | 6 (17.6%) | 4 (19.0%) | 15 (7.5%) |
| - Other | 0 (0%) | 7 (9.1%) | 5 (14.7%) | 1 (4.8%) | 13 (6.5%) |
| Informal support | |||||
|
EDSS 0–1 (n = 67) |
EDSS 1.5–3.0 (n = 77) |
EDSS 3.5–5.5 (n = 34) |
EDSS ≥ 6 (n = 21) |
Overall (n = 199) |
|
| Informal caregiver at study visit; n (%) | 13 (19.4%) | 30 (39.0%) | 28 (82.4%) | 18 (85.7%) | 89 (44.7%) |
| Relationship to patient; n (%) | |||||
| - Husband/wife | 8 (11.9%) | 19 (24.7%) | 21 (61.8%) | 12 (57.1%) | 60 (30.2%) |
| - Other relative | 5 (7.5%) | 18 (23.4%) | 19 (55.9%) | 9 (42.9%) | 51 (25.6%) |
| - Neighbor | 1 (1.5%) | 2 (2.6%) | 1 (2.9%) | 1 (4.8%) | 5 (2.5%) |
| - Volunteer | 0 (0%) | 0 (0%) | 0 (0%) | 1 (4.8%) | 1 (0.5%) |
| - Other | 1 (1.5%) | 1 (1.3%) | 1 (2.9%) | 0 | 3 (1.5%) |
| Use of non-reimbursed devices | |||||
|
EDSS 0–1 (n = 67) |
EDSS 1.5–3.0 (n = 77) |
EDSS 3.5–5.5 (n = 34) |
EDSS ≥ 6 (n = 21) |
Overall (n = 199) |
|
| Use of non-reimbursed devices; n (%) | 1 (1.5%) | 11 (14.3%) | 15 (44.1%) | 16 (76.2%) | 43 (21.6%) |
| Type of device; n (%) | |||||
| - Wheelchair | 0 (0%) | 0 (0%) | 1 (2.9%) | 3 (14.3%) | 4 (2.0%) |
| - Crutch/walking stick | 0 (0%) | 3 (3.9%) | 7 (20.6%) | 11 (52.4%) | 21 (10.6%) |
| - Toilet seats or grab bars | 0 (0%) | 2 (2.6%) | 4 (11.8%) | 5 (23.8%) | 11 (5.5%) |
| - Home adaptation | 0 (0%) | 6 (7.8%) | 5 (14.7%) | 5 (23.8%) | 16 (8.0%) |
| - Vehicle adaptation | 0 (0%) | 1 (1.3%) | 2 (5.9%) | 3 (14.3%) | 6 (3.0%) |
| - Articulated bed | 0 (0%) | 0 (0%) | 0 (0%) | 2 (9.5%) | 2 (1.0%) |
| - Other | 1 (1.5%) | 1 (1.3%) | 5 (14.7%) | 6 (28.6%) | 13 (6.5%) |
EDSS Expanded Disability Status Scale, MS Multiple sclerosis
Over a quarter (28.1%) of pwMS needed paid professional support to maintain their daily life activities, mainly a person to do housework (0.5 ± 2.3 h/week and 4.4 ± 14.5 weeks/year) and a physiotherapist (0.4 ± 1.0 h/week and 5.3 ± 14.8 weeks/year) (Table 4).
Table 4.
Description of number of hours per week and number of weeks that patient needed help from third parties (non-relatives), professionals or transportation paid by patient for a reason related to MS in the last year
| Hours per week Mean (SD) |
Weeks per year Mean (SD) |
|
|---|---|---|
| Type | ||
| Caregivers | 0.43 (6.03) | 0.26 (3.69) |
| Physiotherapist | 0.36 (0.97) | 5.25 (14.84) |
| Person to do housework | 0.51 (2.33) | 4.44 (14.50) |
| Private ophthalmologist | 0.02 (0.17) | 0.27 (3.69) |
| Private neurologist | 0.01 (0.07) | 0.26 (3.69) |
| Private psychologist | 0.09 (0.63) | 1.43 (8.15) |
| Other | 0.21 (1.35) | 2.47 (10.63) |
| Valid n | 199 | 199 |
| Missing n | 0 | 0 |
The mean (SD) annual cost associated with sick leaves due to MS was €416.6 ± 2030.2, with work absenteeism due to MS accounting for €763.4 ± 3161.8, premature retirement due to MS for €5810.1 ± 13,159, and premature work disability/ pensioner for €1816.8 ± 9630.7 per patient (Table 5). The sum of all these indirect costs resulted in an average cost per patient per year of €8806.9. Considering caregiving activities, professional staff cost was €1026.9 ± 4622.0 and informal caregiving activities had a cost of €301.7 ± 1160.0, resulting in a total average cost for caregiving activities of €1328.7. Finally, the mean cost of MS devices needed by pwMS was €736.6 ± 2756.4. All these costs were considered to be average for MS subjects.
Table 5.
MS costs by EDSS score
| EDSS 0–1 (n = 67) |
EDSS 1.5–3.0 (n = 77) |
EDSS 3.5–5.5 (n = 34) |
EDSS ≥6 (n = 21) |
Overall (n = 199) |
|
|---|---|---|---|---|---|
| Sick leave; mean (SD) | 80.25 (334.38) | 729.52 (2707.92) | 627.91 (2646.44) | 0 (0) | 416.58 (2030.18) |
| Annual cost (work absenteeism); mean (SD) | 510.89 (2089.42) | 1280.35 (4279.86) | 561.76 (2810.88) | 0 (0) | 763.40 (3161.83) |
| Annual cost of premature retirement due to MS; mean (SD) | 1006.27 (4144.32) | 5302.33 (12,546.38) | 8169.30 (16,952.79) | 19,178.96 (17,600.87) | 5810.12 (13,158.95) |
| Annual cost of premature work disability/pensioner due to MS; mean (SD) | 0 (0) | 2941.80 (14,243.37) | 2926.08 (7568.11) | 1692.58 (5896.10) | 1816.83 (9630.69) |
| Professional staff cost; mean (SD) | 290.15 (1576.30) | 679.64 (1406.23) | 3246.71 (10,532.42) | 1057.14 (1442.27) | 1026.93 (4622.00) |
| Informal support cost; mean (SD) | 125.76 (771.81) | 320.97 (1274.07) | 575.22 (1329.16) | 350.36 (1427.77) | 301.79 (1160.04) |
| Use of non-reimbursed devices; mean (SD) | 0.39 (3.18) | 508.95 (2409.37) | 1195.59 (3543.34) | 3177.05 (4880.50) | 736.60 (2756.47) |
EDSS Expanded Disability Status Scale, MS Multiple sclerosis, SD Standard deviation
Discussion
The economic cost of MS is largely driven by indirect costs that are linked to early and very high unemployment rates [1–4, 17, 18]. As stated earlier, this study provides a better understanding of the impact of MS on Spanish patients’ working activity, allowing for an updated estimation of the indirect costs of MS. Our study shows an employment rate of 47.2% and a mean age of retirement of 43.6 years in a clinically stable sample of 199 pwMS mostly with a low level of physical disability (median EDSS score of 2.0). Almost a quarter (22.4%) of pwMS retired early because of the condition and 7% received an incapacity benefit or pension due to MS. Ten percent of the population had sick leaves (absenteeism was seen in 90.9% of the student population and 30.9% of the employed population). Costs associated with work limitations to employed subjects were almost seven times greater than costs from professional support and 30 times greater than costs from informal caregiving. Among all costs, those with the higher value are the costs associated with premature retirement according to our sample population (women fully incorporated into working life). These results are consistent with several prior studies. Kobelt et al. found that productivity losses and informal care dramatically increased from €593 at early-stage disease to nearly €34,228 at EDSS scores > 7 [19]. Subsequently, the TRIBUNE study also showed the correlation between disability and economic impact [20]. The overall annual indirect costs associated with MS were estimated at between €207 and €440 million due to productivity losses caused by lost work hours and early retirement (27 and 33% of the total cost, respectively) [21, 22].
A high rate of unemployment also occurs at a level of disability which is typically not associated with overt physical disability [1, 17]. Less visible symptoms and difficulties including cognitive impairment, fatigue, anxiety and depression are reasons for low productivity and unemployment at low EDSS scores. Kobelt et al. also found an employment rate of 45% in a sample of 462 pwMS in Spain with an EDSS score between 0 and 3 [23]. Fatigue and cognitive complaints were found in 92 and 64% of participants, respectively. Fatigue and cognitive disturbances are much more common than mobility problems in people who are working [8, 19]. MS-related productivity loss due to presenteeism was three times that of absenteeism in a study with 740 MS employees conducted in Australia [4]. The mean total work productivity loss was 2.5 days (14.2% loss in productive time), based on an absenteeism of 0.6 days (3.4%) and a presenteeism of 1.9 days (10.8%), leading to a €4578 loss per person annually. Work productivity was determined mostly by fatigue, cognitive impairment, pain and sensory symptoms [4].
There is increasing evidence to advocate the use of more effective therapies at earlier stages of the disease [24–27]. The IMPrESS study showed that pwMS treated earlier in the course of the disease showed a trend towards lower total (€39,037 vs €42,996), indirect (€15,733 vs €18,934) and disease-modifying therapy (€19,364 vs €20,491) costs and a better health-related quality of life status (0.62 vs 0.56; p < 0.01) compared to those receiving late treatment [3]. Chen et al. found that pwMS receiving high-efficacy disease-modifying therapy reported significant increases in amount of work, work attendance and work productivity compared with those using first-generation injectable treatments [27].
Our study has several limitations. Recall bias is a common concern of studies using self-reported data. The relatively small sample size and the cross-sectional design could be additional limiting factors of this study. A salary was set based on the range indicated by the participant (mid-point). For cases where only the salary at the time of diagnosis was available, the point of the range was adjusted using the CPI for the respective year. Another limitation is not having considered the time lost due to disease for pwMS without paid work, since it was unknown during the study.
Conclusions
MS has classically been reported as being responsible for high indirect costs and other substantial economic burden in Spain. Symptom severity has strong impact on both work productivity and workforce participation. This study shows that indirect and caregiving costs are incurred even at low levels of physical disability. Effective therapeutic interventions to improve the management of early symptoms as well as implementing workplace strategies focused on job retention may be essential to decrease the high economic burden of MS.
Acknowledgements
We thank the patients and their families for making the W-IMPACT study possible.
*The W-IMPACT Study Group: Adrián Ares (Complejo Asistencial Universitario de León), Carmen Arnal (Complejo Hospitalario Universitario de Granada), Ana B. Caminero (Hospital Nuestra Señora de Sonsoles, Ávila), María Carcelén (Hospital General Universitario de Valencia), Olga Carmona (Hospital de Figueres), José M García-Domínguez and María L Martínez-Ginés (Hospital Universitario Gregorio Marañón, Madrid), Pablo Eguía (Hospital Dr. José Molina Orosa, Lanzarote), María del Carmen Fernández (Hospital Universitario Virgen de Valme, Sevilla), Ricardo Ginestal (Hospital Universitario Clínico San Carlos, Madrid), Laura Lacruz (Hospital Francesc de Borja, Gandía), Miguel Llaneza (Hospital Arquitecto Marcide, Ferrol), Carlos López de Silanes (Hospital de Torrejón, Torrejón de Ardoz), Gisela Martín (Hospital Verge de la Cinta, Tortosa), Laura Navarro (Hospital General Universitario de Elche), Beatriz Romero (Hospital Son Llatzer, Palma de Mallorca), María Seral (Hospital General San Jorge, Huesca), Myriam Solar (Hospital Universitario de Cabueñes, Gijón).
Funding
The study was funded by Roche Farma, Spain (ML39424). The sponsor was involved in the design, execution, analysis, and interpretation of the results.
Availability of data and materials
The dataset of the current study is available from the corresponding author on reasonable request.
Abbreviations
- CSI
Caregiver Strain Index
- EDSS
Expanded Disability Status Scale
- IQR
Interquartile range
- MS
Multiple sclerosis
- MSIS-29
29-item Multiple Sclerosis Impact Scale
- MSWDQ-23
23-item Multiple Sclerosis Work Difficulties Questionnaire
- PPMS
Primary progressive multiple sclerosis
- pwMS
People with multiple sclerosis
- RRMS
Relapsing-remitting multiple sclerosis
- SD
Standard deviation
Authors’ contributions
JMG-D, MLM-G, JM, and ER-B developed the research question and designed the study. OC, ABC, and NM contributed to the analysis and interpretation of the results. All authors contributed to and approved the final manuscript.
Ethics approval and consent to participate
The study was approved by the institutional review board of the Fundación Jiménez Díaz (Madrid, Spain). Written informed consent was obtained from all subjects.
Consent for publication
Not applicable.
Competing interests
JM, NM, and ER-B are employees of Roche Farma Spain. None of the other authors report any conflict of interest.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
José M. García-Domínguez, Email: jose_garciadom@hotmail.com
Jorge Maurino, Phone: +34 91 324 81 00, Email: jorge.maurino@roche.com.
María L. Martínez-Ginés, Email: marisamgines@hotmail.com
Olga Carmona, Email: occodina@gmail.com.
Ana B. Caminero, Email: caminero.nrl@gmail.com
Nicolás Medrano, Email: nicolas.medrano@roche.com.
Elena Ruíz-Beato, Email: elena.ruiz-beato@roche.com.
for the W-IMPACT Clinical Investigators:
Adrián Ares, Carmen Arnal, Ana B. Caminero, María Carcelén, Olga Carmona, José M. García-Domínguez, María L. Martínez-Ginés, Pablo Eguía, María del Carmen Fernández, Ricardo Ginestal, Laura Lacruz, Miguel Llaneza, Carlos López de Silanes, Gisela Martín, Laura Navarro, Beatriz Romero, María Seral, and Myriam Solar
References
- 1.Kobelt G, Thompson A, Berg J, et al. New insights into the burden and costs of multiple sclerosis in Europe. Mult Scler. 2017;23:1123–1136. doi: 10.1177/1352458517694432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ernstsson O, Gyllensten H, Alexanderson K, et al. Cost of illness of multiple sclerosis - a systematic review. PLoS One. 2016;11:e0159129. doi: 10.1371/journal.pone.0159129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tinelli M, Kanavos P, Efthymiadou O, et al. Using IMPrESS to guide policy change in multiple sclerosis. Mult Scler. 2018;24:1251–1255. doi: 10.1177/1352458517737388. [DOI] [PubMed] [Google Scholar]
- 4.Chen J, Taylor BV, Palmer AJ, et al. Estimating MS-related work productivity loss and factors associated with work productivity loss in a representative Australian sample of people with multiple sclerosis. Mult Scler. 2018:1352458518781971. 10.1177/1352458518781971 [Epub ahead of print]. [DOI] [PubMed]
- 5.Uccelli MM. The impact of multiple sclerosis on family members: a review of the literature. Neurodegener Dis Manag. 2014;4:177–185. doi: 10.2217/nmt.14.6. [DOI] [PubMed] [Google Scholar]
- 6.Howard J, Trevick S, Younger DS. Epidemiology of multiple sclerosis. Neurol Clin. 2016;34:919–939. doi: 10.1016/j.ncl.2016.06.016. [DOI] [PubMed] [Google Scholar]
- 7.Atlas of MS 2016. MS international federation. Available at: https://www.msif.org/. [cited 2018 Nov 30].
- 8.Fernández O, Calleja-Hernández MA, Meca-Lallana J, et al. Estimate of the cost of multiple sclerosis in Spain by literature review. Expert Rev Pharmacoecon Outcomes Res. 2017;17:321–333. doi: 10.1080/14737167.2017.1358617. [DOI] [PubMed] [Google Scholar]
- 9.Sicras-Mainar A, Ruíz-Beato E, Navarro-Artieda R, et al. Impact on healthcare resource utilization of multiple sclerosis in Spain. BMC Health Serv Res. 2017;17:854. doi: 10.1186/s12913-017-2807-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Polman CH, Reingold SC, Banwell B, et al. Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. Ann Neurol. 2011;69:292–302. doi: 10.1002/ana.22366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Martínez-Ginés ML, García-Domínguez JM, Forero L, et al. Spanish validation of a specific measure to assess work-related problems in people with multiple sclerosis: the multiple sclerosis work difficulties questionnaire (MSWDQ-23) Mult Scler Relat Disord. 2018;22:115–119. doi: 10.1016/j.msard.2018.04.003. [DOI] [PubMed] [Google Scholar]
- 12.Kurtzke JF. Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS) Neurology. 1983;33:1444–1452. doi: 10.1212/WNL.33.11.1444. [DOI] [PubMed] [Google Scholar]
- 13.Hobart J, Lamping D, Fitzpatrick R, et al. The multiple sclerosis impact scale (MSIS-29): a new patient-based outcome measure. Brain J Neurol. 2001;124:962–973. doi: 10.1093/brain/124.5.962. [DOI] [PubMed] [Google Scholar]
- 14.Honan CA, Brown RF, Hine DW, et al. The multiple sclerosis work difficulties questionnaire (MSWDQ): development of a shortened scale. Disabil Rehabil. 2014;6:635–641. doi: 10.3109/09638288.2013.805258. [DOI] [PubMed] [Google Scholar]
- 15.García-Domínguez JM, Martínez-Ginés ML, Carmona O, et al. Measuring burden in caregivers of people with multiple sclerosis: psychometric properties of the CSI questionnaire. Patient Prefer Adherence. 2019;13:101–106. doi: 10.2147/PPA.S180863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.eSalud. Información económica del sector sanitario. Oblikue consultig. Available at http://esalud.oblikue.com/. [cited 2018 Nov 30].
- 17.Giovannoni G. Can we afford not to prevent MS-related disability? Mult Scler. 2017;23:1048–1049. doi: 10.1177/1352458517703804. [DOI] [PubMed] [Google Scholar]
- 18.Raggi A, Covelli V, Schiavolin S, et al. Work-related problems in multiple sclerosis: a literature review on its associates and determinants. Disabil Rehabil. 2016;38:936–944. doi: 10.3109/09638288.2015.1070295. [DOI] [PubMed] [Google Scholar]
- 19.Kobelt G, Berg J, Lindgren P, et al. Costs and quality of life of multiple sclerosis in Spain. Eur J Health Econ. 2006;7:S65–S64. doi: 10.1007/s10198-006-0381-y. [DOI] [PubMed] [Google Scholar]
- 20.Karampampa K, Gustavsson A, Miltenburger C, Mora S, Arbizu T. Treatment experience, burden and unmet needs (TRIBUNE) in MS study: results from Spain. Mult Scler. 2012;18:35–39. doi: 10.1177/1352458512441566d. [DOI] [PubMed] [Google Scholar]
- 21.Sobocki P, Pugliatti M, Lauer K, et al. Estimation of the cost of MS in Europe: extrapolations from a multinational cost study. Mult Scler. 2007;13:1054–1064. doi: 10.1177/1352458507077941. [DOI] [PubMed] [Google Scholar]
- 22.Parés-Badell O, Barbaglia G, Jerinic P, et al. Cost of disorders of the brain in Spain. PLoS One. 2014;9:e105471. doi: 10.1371/journal.pone.0105471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Oreja-Guevara C, Kobelt G, Berg J, et al. New insights into the burden and costs of multiple sclerosis in Europe: results for Spain. Mult Scler. 2017;23:166–178. doi: 10.1177/1352458517708672. [DOI] [PubMed] [Google Scholar]
- 24.Giovannoni G, Butzkueven H, Dhib-Jalbut S, et al. Brain health: time matters in multiple sclerosis. Mult Scler Relat Disord. 2016;9:S5–S48. doi: 10.1016/j.msard.2016.07.003. [DOI] [PubMed] [Google Scholar]
- 25.Cerqueira JJ, Compston DAS, Geraldes R, et al. Time matters in multiple sclerosis: can early treatment and long-term follow-up ensure everyone benefits from the latest advances in multiple sclerosis? J Neurol Neurosurg Psychiatry. 2018;89:844–850. doi: 10.1136/jnnp-2017-317509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ziemssen T, Derfuss T, de Stefano N, et al. Optimizing treatment success in multiple sclerosis. J Neurol. 2016;263:1053–1065. doi: 10.1007/s00415-015-7986-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chen J, Taylor BV, Blizzard L, et al. Effects of multiple sclerosis disease-modifying therapies on employment measures using patient-reported data. J Neurol Neurosurg Psychiatry. 2018;89:1200–1207. doi: 10.1136/jnnp-2018-318228. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset of the current study is available from the corresponding author on reasonable request.