Summary
Primary hyperparathyroidism (PHPT) is characterised by the overproduction of parathyroid hormone (PTH) due to parathyroid hyperplasia, adenoma or carcinoma and results in hypercalcaemia and a raised or inappropriately normal PTH. Symptoms of hypercalcaemia occur in 20% of patients and include fatigue, nausea, constipation, depression, renal impairment and cardiac arrythmias. In the most severe cases, uraemia, coma or cardiac arrest can result. Primary hyperparathyroidism in pregnancy is rare, with a reported incidence of 1%. Maternal and fetal/neonatal complications are estimated to occur in 67 and 80% of untreated cases respectively. Maternal complications include nephrolithiasis, pancreatitis, hyperemesis gravidarum, pre-eclampsia and hypercalcemic crises. Fetal complications include intrauterine growth restriction; preterm delivery and a three to five-fold increased risk of miscarriage. There is a direct relationship between the degree of severity of hypercalcaemia and miscarriage risk, with miscarriage being more common in those patients with a serum calcium greater than 2.85 mmol/L. Neonatal complications include hypocalcemia. Herein, we present a case series of three women who were diagnosed with primary hyperparathyroidism in pregnancy. Case 1 was diagnosed with multiple endocrine neoplasia type 1 (MEN1) in pregnancy and required a bilateral neck exploration and subtotal parathyroidectomy in the second trimester of her pregnancy due to symptomatic severe hypercalcaemia. Both case 2 and case 3 were diagnosed with primary hyperparathyroidism due to a parathyroid adenoma and required a unilateral parathyroidectomy in the second trimester. This case series highlights the work-up and the tailored management approach to patients with primary hyperparathyroidism in pregnancy.
Learning points:
Primary hyperparathyroidism in pregnancy is associated with a high incidence of associated maternal fetal and neonatal complications directly proportionate to degree of maternal serum calcium levels.
Parathyroidectomy is the definitive treatment for primary hyperparathyroidism in pregnancy and was used in the management of all three cases in this series. It is recommended when serum calcium is persistently greater than 2.75 mmol/L and or for the management of maternal or fetal complications of hypercalcaemia. Surgical management, when necessary is ideally performed in the second trimester.
Primary hyperparathyroidism is genetically determined in ~10% of cases, where the likelihood is increased in those under 40 years, where there is relevant family history and those with other related endocrinopathies. Genetic testing is a useful diagnostic adjunct and can guide treatment and management options for patients diagnosed with primary hyperparathyroidism in pregnancy, as described in case 1 in this series, who was diagnosed with MEN1 syndrome.
Women of reproductive age with primary hyperparathyroidism need to be informed of the risks and complications associated with primary hyperparathyroidism in pregnancy and pregnancy should be deferred and or avoided until curative surgery has been performed and calcium levels have normalised.
Background
Primary hyperparathyroidism is characterised by hypercalcaemia in the context of a raised or inappropriately normal PTH. It is important to note that the physiological changes of pregnancy can mask its diagnosis, as hypoalbuminaemia, increased glomerular filtration rate, calcium transport across the placenta and oestrogen inhibition of PTH-mediated bone resorption can all result in the appearance of lower calcium levels (1). Furthermore, radiological localisation of parathyroid disease is limited in pregnancy as computed tomography and the gold standard 99mTc Sestamibi scan are contraindicated because of the radiation risk to the foetus, and therefore, ultrasound remains the only suitable radiological imaging modality in pregnancy (2).
Primary hyperparathyroidism during pregnancy can be managed conservatively with oral or intravenous rehydration with or without forced diuresis, a low-calcium diet and vitamin D supplementation (3). Other treatment options including calcitonin and cinacalcet are not used in pregnancy due to limited safety data and the use of bisphosphonate therapy should be avoided due to the risk of adverse effects on fetal skeletal development (4).
Parathyroidectomy is the definitive treatment for primary hyperparathyroidism and is recommended in pregnancy when serum calcium is greater than 2.75 mmol/L, particularly in patients with prior pregnancy loss (5). Recent retrospective data have demonstrated that patients treated with parathyroidectomy have lower rates of pre-eclampsia and preterm delivery compared to patients managed medically (6). Surgery is preferably performed in the second trimester due to incomplete organogenesis in the first trimester, and the risk of preterm delivery in the third trimester (2). However, urgent parathyroidectomy is recommended regardless of the gestational age of the foetus if all efforts at medical management prove unsuccessful or if maternal and or fetal complications arise (7).
Primary hyperparathyroidism can be genetically determined in ~10% of cases and thus genetic testing plays a role in the diagnostic classification of this disease (8). A family history of primary hyperparathyroidism, age <50 years, multi-glandular disease, parathyroid carcinoma, a low urinary calcium/creatinine ratio (<0.001) or the presence of other MEN1, multiple endocrine neoplasia type 2 (MEN2) or hyperparathyroidism jaw tumour syndrome (HPT-JT)-associated tumours are the current indications for genetic testing (6, 8). Confirming a genetic diagnosis enables patients to be screened for the development of other syndrome-related diseases (e.g. neuroendocrine tumours in MEN1) and allows genetic counselling of at-risk family members for cascade predictive genetic testing and targeted endocrine screening. Furthermore, a genetic diagnosis can also guide the management of primary hyperparathyroidism as surgical management of inherited primary hyperparathyroidism often requires an open neck exploration because of a higher risk of multiple parathyroid gland hyperplasia and/or ectopic parathyroid glands. A genetic diagnosis also enables reproductive options in a future pregnancy such as prenatal testing or pre-implantation genetic diagnosis.
Case presentation
Case 1
Medical history and patient demographics
A 20-year-old female presented with nausea and abdominal discomfort in early pregnancy and was diagnosed with primary hyperparathyroidism at 5-weeks gestation (Table 1). She had visited her general practitioner 1 month prior to conception with abdominal discomfort, vomiting and diarrhoea. She had no significant medical or family history.
Table 1.
PTH, serum calcium, vitamin D, phosphate and urinary calcium/creatinine levels at diagnosis.
| PTH (1.48–7.63 pmol/L) | Serum calcium (2.20–2.60 mmol/l) | Vitamin D (ng/mL) | Phosphate (0.8–1.5 mmol/L) | Urinary calcium/creatinine ratio* | |
|---|---|---|---|---|---|
| Case 1 | 15.69 | 2.74 | 33.4 | 0.87 | 0.09 |
| Case 2 | 11.87 | 3.08 | 13.8 | 0.62 | 0.07 |
| Case 3 | 8.5 | 2.79 | 37.3 | 0.63 | 0.05 |
*Calculated using the Hammersmith urine calcium to creatinine ratio (urine calcium (mmol/L) × (serum creatinine (µmol/L)/1000 divided by serum calcium (mmol/L) × urine creatinine (mmol/L))).
Investigations
Maternal investigations included serial biochemical investigations (Fig. 1), negative ultrasonography of the neck and genetic testing which revealed the patient to be heterozygous for a novel, likely pathogenic frameshift variant in the MEN1 gene c.236_237delCC, p. (Pro79Argfs*37) in exon 2. This variant is not listed in population frequency databases (Genome Aggregation Database, Exome Variant Server, 1000 Genome) and the c.236_237delCC nucleotide change is predicted to result in a prematurely truncated MEN1 protein. Fetal investigations and amniotic fluid indices were normal.
Figure 1.
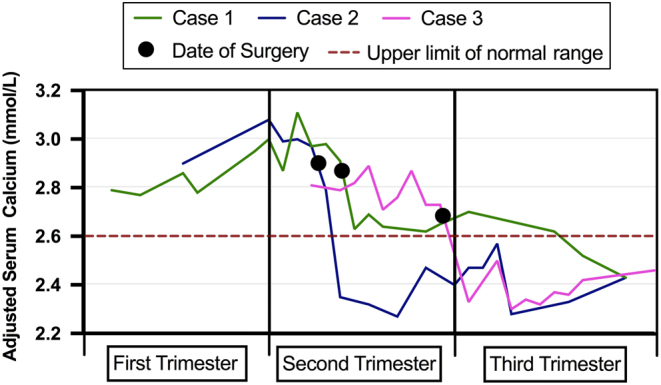
Serial calcium levels throughout pregnancy for cases 1–3.
Treatment
This patient was managed medically with oral and intravenous fluid rehydration. An open neck exploration and three gland parathyroidectomy was performed at week 18 gestation, due to persistent symptoms of hypercalcaemia, namely nausea and headaches and a persistently elevated serum calcium level (Fig. 1). After a multi-disciplinary discussion, a decision was reached to perform intra-operative PTH measurements to guide surgery and the number of parathyroid glands excised, aiming for a drop in PTH levels of >50%. The standard surgical approach of removing three and a half glands was avoided in this case because of the risk of inducing hypoparathyroidism. The operation was successful and intraoperative PTH dropped by 53.8% from 12.4 pmol/L at the time of neck incision to 5.72 pmol/L after removal of the third parathyroid gland. The histology results were consistent with parathyroid hyperplasia in the context of MEN1 syndrome, showing mildly enlarged but diffusely hyperplastic left superior, left inferior and right superior parathyroid glands, weighing 1.04, 0.11 and 0.15 g respectively (Fig. 2B).
Figure 2.
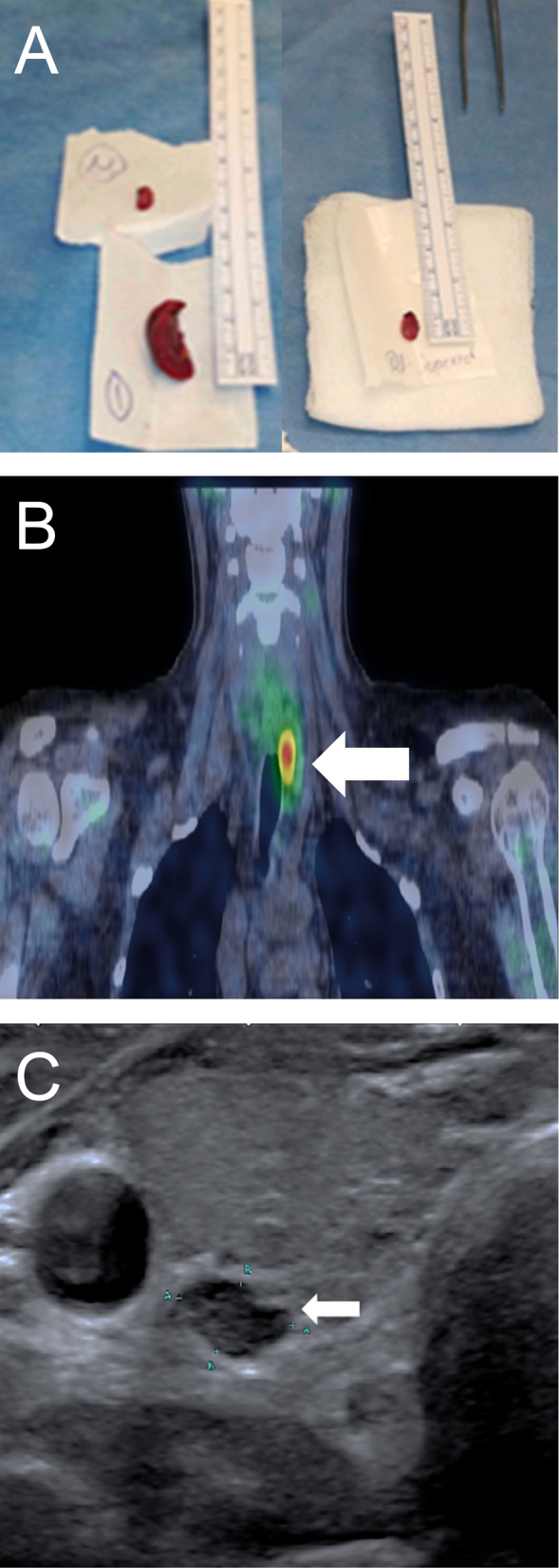
(A) Left superior (LS), left inferior (LI) and right superior (RS) parathyroid glands post-parathyroidectomy in case 1. (B) Enlarged parathyroid gland on 99mTc-sestamibi SPECT/CT scan performed in case 2 prior to pregnancy, consistent with a parathyroid adenoma based on histology results. (C) Transverse image from an ultrasound of the neck performed in case 3 showing a 9 mm × 5 mm enlarged right parathyroid gland.
Outcome and follow-up
This patient had an uneventful post-operative course. The patient’s calcium levels improved post parathyroidectomy and symptoms resolved. She had close maternal/fetal surveillance, with regular fetal growth scans and screening for preeclampsia (blood pressure and protein in urine assessment) for the remainder of the pregnancy. Induction of labour was offered at 38 weeks due to persistent reduced fetal movements and resulted in a vaginal delivery of a healthy baby girl weighing 3160 g. Surveillance for other MEN1-associated conditions, including a blood test for prolactin, has been postponed until after the perinatal period as results would be unreliable. The patient was counselled on her increased risk of pancreatic and pituitary tumours, and her first-degree relatives are undergoing genetic screening (8).
Case 2
Medical history and patient demographics
A 40-year-old female presented to the endocrine clinic at 7-week gestation. She had a known diagnosis of primary hyperparathyroidism (Table 1) and was awaiting parathyroidectomy for a localised abnormal parathyroid gland on imaging (Fig. 2C). She had no significant medical or family history.
Investigations
Maternal investigations included serial biochemical investigations (Fig. 1), ultrasonography, which showed a left-sided enlarged parathyroid gland and a 99mTc-sestamibi SPECT/CT scan, performed prior to pregnancy, which also showed features consistent with a left-sided enlarged parathyroid gland, concordant with ultrasound findings (Fig. 2C). Genetic testing was not performed in this case during pregnancy as the patient was 40 years of age at diagnosis and had no family history suggestive of inherited causes of hyperparathyroidism. Fetal investigations and amniotic fluid indices were normal.
Treatment
This patient was initially managed conservatively with oral and intravenous fluid rehydration. However, due to persistent and severe hypercalcaemia and associated symptoms of fatigue and polydipsia, a targeted left sided parathyroidectomy was performed at 16-week gestation. The histology confirmed a left-sided parathyroid adenoma, consistent with the findings on the ultrasound and 99mTc-sestamibi SPECT/CT scans (Fig. 2C).
Outcome and follow-up
This patient’s symptoms resolved and calcium (Fig. 1) and parathyroid hormone levels normalised. She remained under close maternal/fetal surveillance with regular fetal growth scans and preeclampsia screening. The pregnancy was complicated by a large fetal abdominal circumference on growth scans and the patient was subsequently diagnosed at 35 weeks gestation with gestational diabetes, managed by diet alone. Induction of labour was planned for 38 weeks gestation but the patient presented in early labour at 37+4 weeks gestation and underwent a caesarean section due to fetal bradycardia. The baby girly was healthy, weighing 2802g at birth.
Case 3
Medical history and patient demographics
A 34-year-old female with a past medical history of primary hypothyroidism presented to the endocrine clinic following an incidental finding of raised serum calcium at 16 weeks gestation (Table 1). There was no significant family history.
Investigations
This patient had serial biochemical investigations throughout pregnancy (Fig. 1). Initial ultrasonography of the parathyroid glands at her local hospital between 18 and 19 weeks gestation was negative for an enlarged parathyroid gland, but repeat ultrasound at 25-week gestation showed an enlarged 9 mm × 5 mm gland posterior to the right lobe of the thyroid. Genetic testing was performed as the patient was <40 years and was negative.
Treatment
Initial management was conservative and included oral fluid rehydration. In view of persistent hypercalcaemia and progressive worsening of symptoms including fatigue, polyuria and headaches, a right sided parathyroidectomy was performed at 27-week gestation. Histology confirmed a right parathyroid adenoma, correlating with ultrasound findings.
Outcome and follow-up
This patient had an uneventful post-operative course and her calcium and parathyroid levels normalised and clinical symptoms resolved (Fig. 1). She gave birth to a baby boy weighing 3960 g at 40 + 3 weeks gestation by caesarean section due to slow progression of labour. No case of neonatal hypocalcaemia was observed in this series, although it was monitored for in all three cases.
Discussion
In all cases in this series, parathyroidectomy greatly improved the patients’ symptoms and corrected the hypercalcaemia, without evidence of fetal compromise or maternal complication.
The majority of primary hyperparathyroidism cases (~90%) occur sporadically, usually due to parathyroid adenomas. The remaining ~10% of cases occur as hereditary disorders, which include multiple endocrine neoplasias (MEN1, MEN2A, MEN4), familial hypocalciuric hypercalcaemia (FHH), hyperparathyroidism jaw tumour (HPT-JT) and familial isolated primary hyperparathyroidism (FIPH) (8). Genetic testing in pregnant women with primary hyperparathyroidism should be considered as familial parathyroid disorders are often associated with an earlier age of onset compared to sporadic disease (8). Furthermore, genetic testing can guide the management of primary hyperparathyroidism. As demonstrated in case 1, genetic testing diagnosed MEN1, which informed both the surgical approach of subtotal parathyroidectomy and the need for bilateral neck exploration due to the higher risk of multiple parathyroid gland disease in MEN1 (8). This genetic diagnosis also allowed the patient to receive counselling on her increased risk of pancreatic and pituitary tumours, and enabled cascade family screening.
In conclusion, genetic testing is helpful in the tailored management of primary hyperparathyroidism in pregnancy. Finally, this series highlights the beneficial role of timely surgical management for severe or symptomatic primary hyperparathyroidism in pregnancy and the need for a multi-disciplinary approach to ensure the best possible maternal and fetal outcomes.
Declaration of interest
The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of the research reported.
Funding
Dr Ruth Casey receives funding from GIST Support UK.
Patient consent
Informed and written consent has been obtained from each of the three patients and these are available for review as needed.
Author contribution statement
A M C wrote the first draft of this manuscript. A M C, S K and S H were involved in collection of clinical data. All authors were involved in the writing of this manuscript and final review of the manuscript. R C, C M, D W, S M P, B F, S K, S O O and K G K were involved in the clinical care of these patients and collection of data.
References
- 1.Norman J, Politz D, Politz L. Hyperparathyroidism during pregnancy and the effect of rising calcium on pregnancy loss: a call for earlier intervention. Clinical Endocrinology 2009. 71 104–109. ( 10.1111/j.1365-2265.2008.03495.x) [DOI] [PubMed] [Google Scholar]
- 2.Som M, Stroup JS. Primary hyperparathyroidism and pregnancy Baylor University Medical Center Proceedings 2011. 24 220–223. ( 10.1080/08998280.2011.11928719) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Diaz-Soto G, Linglart A, Sénat MV, Kamenicky P, Chanson P. Primary hyperparathyroidism in pregnancy. Endocrine 2013. 44 591–597. ( 10.1007/s12020-013-9980-4) [DOI] [PubMed] [Google Scholar]
- 4.Djokanovic N, Klieger-Grossmann C, Koren G. Does treatment with bisphosphonates endanger the human pregnancy? Journal of Obstetrics and Gynaecology Canada 2008. 30 1146–1148. ( 10.1016/S1701-2163(16)34026-9) [DOI] [PubMed] [Google Scholar]
- 5.McMullen TP, Learoyd DL, Williams DC, Sywak MS, Sidhu SB, Delbridge LW. Hyperparathyroidism in pregnancy: options for localization and surgical therapy. World Journal of Surgery 2010. 34 1811–1816. ( 10.1007/s00268-010-0569-2) [DOI] [PubMed] [Google Scholar]
- 6.Rigg J, Gilbertson E, Barrett HL, Britten FL, Lust K. Primary hyperparathyroidism in pregnancy: maternofetal outcomes at a quaternary referral obstetric hospital, 2000 through 2015. Journal of Clinical Endocrinology and Metabolism 2019. 104 721–729. ( 10.1210/jc.2018-01104) [DOI] [PubMed] [Google Scholar]
- 7.Patel NA, Bughi S, Shaw SJ. Hyperparathyroidism in pregnancy. Endocrinologist 2005. 15 313–316. ( 10.1097/01.ten.0000179015.90760.bd) [DOI] [Google Scholar]
- 8.Marini F, Cianferotti L, Giusti F, Brandi ML. Molecular genetics in primary hyperparathyroidism: the role of genetic tests in differential diagnosis, disease prevention strategy, and therapeutic planning. A 2017 update. Clinical Cases in Mineral and Bone Metabolism 2017. 14 60–70. ( 10.11138/ccmbm/2017.14.1.060) [DOI] [PMC free article] [PubMed] [Google Scholar]



 This work is licensed under a
This work is licensed under a