Abstract
Objective
Polycystic kidney disease (PKD) is the major cause of kidney failure and mortality in humans. It has always been suspected that the development of cystic kidney disease shares features with tumorigenesis, although the evidence is unclear.
Methods
We crossed p53 mutant mice (p53N236S, p53S) with Werner syndrome mice and analyzed the pathological phenotypes. The RNA-seq, ssGSEA analysis, and real-time PCR were performed to dissect the gene signatures involved in the development of disease phenotypes.
Results
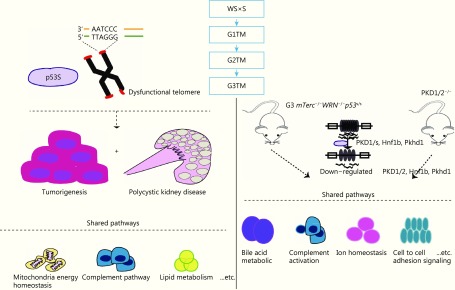
We found enlarged kidneys with fluid-filled cysts in offspring mice with a genotype of G3mTerc-/-WRN-/-p53S/S (G3TM). Pathology analysis confirmed the occurrence of PKD, and it was highly correlated with the incidence of tumorigenesis. RNA-seq data revealed the gene signatures involved in PKD development, and demonstrated that PKD and tumorigenesis shared common pathways, including complement pathways, lipid metabolism, mitochondria energy homeostasis and others. Interestingly, this G3TM PKD and the classical PKD1/2 deficient PKD shared common pathways, possibly because the mutant p53S could regulate the expression levels of PKD1/2, Pkhd1, and Hnf1b.
Conclusions
We established a dual mouse model for PKD and tumorigenesis derived from abnormal cellular proliferation and telomere dysfunction. The innovative point of our study is to report PKD occurring in conjunction with tumorigenesis. The gene signatures revealed might shed new light on the pathogenesis of PKD, and provide new molecular biomarkers for clinical diagnosis and prognosis.
Keywords: p53 mutation, telomere dysfunction, polycystic kidney disease, tumorigenesis
Introduction
Polycystic kidney disease (PKD) is a disease where enlarged kidneys develop characteristic fluid-filled cysts. Cysts in the liver or pancreas, cerebral aneurysms, abnormal cardiac development, and hypertension are also frequently found in PKD patients. Genetic studies have shown that approximately 80% of autosomal dominant PKD (ADPKD) is caused by mutations in the PKD1 gene (encoding polycystin-1, PC1), and about 20% of ADPKD was due to mutations in PKD2 gene (encoding polycystin-2, PC2). It has been extensively shown that PC1/2 act as the key regulators for calcium homeostasis, and the dysfunction of PC1/2 might play an essential role in calcium imbalance and cAMP signaling, resulting in the development of PKD phenotypes1,2. Increasing evidence suggests that PC1/2 proteins might interact with key regulators in cell cycle regulation, especially in cell proliferation and secretion-related signaling pathways1. PKD1 has been found to play a role in preventing immortalized proliferation of renal cells through p53 and JNK, suggesting a novel link between PKD1 and p533. It has also been found that the tumor suppressor protein p53 participates in a negative feedback loop to regulate PKD1 gene expression, thus preventing renal cysts formation4. Interestingly, another study has shown that Mekk1 acts as a co-repressor with p53 to downregulate PKD1 transcription. This PKD1 repression could be promoted by stress stimuli, suggesting that abnormally elevated stress responses might directly downregulate the PKD1 gene, possibly causing haploinsufficiency and cyst formation5. In an endothelial cell-culture system, elevated expression of mechanosensory polycystins in human carotid atherosclerotic plaques is associated with p53 activation and disease severity6. At the animal level, Bcl2 knockout mice manifested PKD and PKD phenotypes that could not have been rescued by p53 deficiency7,8. The mutant p53 protein, especially the missense point mutation, is the major form of p53 deficiency in human disease. It promotes the progress of disease by both loss and gain of function9. However, no evidence has been found to connect mutant p53 with the progress of PKD.
Werner syndrome (WS) protein is a member of the RecQ helicase family implicated in the maintenance of genome stability. WRN plays an essential role in telomere DNA replication, and WRN defects cause human pathologies linked to cancer predisposition and premature aging, such as WS10-12. By masking the chromosome ends from the DNA repair machinery through repression of the ATM/ATR signaling pathways, telomere DNA has a crucial function in DNA damage response (DDR). Telomere DNA is elongated by telomerase and protected by the protein complex shelterin, which regulates telomere length and protects telomeres from activating DDR13.
The mouse model of WS is established by double knockout of WRN and the RNA component of telomerase. The late generation (G4-6) of WS mice with both telomerase and WRN deficiency (mTR-/-WRN-/-) exhibited the clinical features observed in WS patients14-16. Our previous study has shown that ALT tumorigenic cell lines derived from senescent WS MEFs gained the same point mutation in tumor suppressor gene Trp53, encoding a mutant p53 protein known as p53N236S (p53S hereafter). The p53S/S mice manifested highly invasive lymphomas and metastatic sarcomas with dramatically increased double minute chromosomes17.
We introduced this p53S mutation back into WS mice to study the intrinsic role of p53S in modulating WS symptoms, by crossing mice carrying p53S mutation with WS mice. Surprisingly, we found that the offspring of p53S and WS mice (mTR-/-WRN-/-p53S/S) manifested both PKD and tumor phenotypes. Here we report the phenotypes of this novel mouse model. By RNA-seq and ssGSEA analysis, we have identified the gene signatures and pathways that connect mutant p53 and telomere dysfunction with the development of PKD.
Materials and methods
Mice
Transgenic p53S mice and WS (mTR-/-WRN-/-) mice were bred to generate mTR-/-WRN-/-p53S/S mice. We crossed mice carrying p53S mutation (p53S/S) with WS mice (mTR-/-WRN-/-) and obtained the first generation of mice with telomerase knockout, WRN knockout, and p53S mutation (G1 mTR-/-WRN-/-p53S/S), referred to as G1 triple mutation (G1TM). The mice were then bred generation-by-generation to obtain G2 and G3 TM mice. The telomerase knockout and WRN knockout mice (double mutation, DM) and wild type (WT) mice were used as control. All experiments were carried out with the approval of the Kunming University of Science and Technology and Use Committee (Approval ID: M2015-011) in accordance with the guidelines of the Association for Assessment and Accreditation of Laboratory Animal Care.
MEF cells
The MEF cells with different genotypes were harvested in 13.5 days and cultured in Dulbecco’s modified Eagle’s medium (DMEM) with 10% fetal bovine serum (FBS) at 37 °C with 5% CO2 and 3% O2. To maintain their original characteristics, only the early passages (≤ passage 5) of MEF cells were used for experiments.
Pathology analysis
Mouse kidney samples were fixed in 4% neutral buffered formalin for 6 hours, then alcohol-dehydrated and paraffin-embedded. The paraffin-embedded tissue blocks were sectioned into 4 μm slices for later experiments. For hematoxylin-eosin (HE) staining, the tissue sections were deparaffinized and rehydrated, and H&E staining was applied. The H&E stained slides were observed via microscopy and the histological changes and kidney lesions were evaluated by pathologists.
RNA-seq and gene expression signature analysis
Cell or tissue (sarcoma and cystic kidney) samples were collected and sent for commercia RNA-seq service (Novogene, China). Briefly, the total RNA was extracted and enriched by oligo-dT labeled magnetic beads, and used to construct a library for RNA-seq. The sequenced reads (raw reads) were evaluated for quality control. The adapters and low quality reads were filtered to obtain clean reads. The clean data were then aligned with the reference mouse genome by TopHat2. The RNA-seq counts were annotated and the FPKM file was generated for bioinformatic analysis.
The Bioinformatics ExperT SYstem (BETSY) was applied to automate the development of workflows18. The single sample gene set enrichment analysis (ssGSEA)19was applied to analyze the RNA-seq data. Hallmark (designed for well-defined biological states and processes), C2 (BIOCARTA, KEGG, REACTOME, etc.), and C5 (GO) gene sets from the Molecular Signatures Database20were used for ssGSEA analysis. The heat maps were plotted with BETSY by centering with mean but without hierarchical clustering. The common pathways between cystic kidneys and tumors were ranked and plotted based on their ssGSEA scores.
Ingenuity pathway analysis
The essential genes involved in PKD development were selected according to the literature1,21. The fold change in their expression between G3TM and G3DM was calculated from RNA-seq data. After applying the cutoff (2 ×) for gene expression fold change, the remaining genes and their fold changes, and P values were imported to Ingenuity Pathway Analysis (IPA) software. The knowledge base of IPA were used to draw their expression regulation and interaction network. The network with largest numbers of genes is included, such as developmental disorders, immunological diseases, inflammatory diseases, inflammatory response, and renal and urological disease.
Quantitative real-time PCR analysis
RNA was isolated from cell or tissue samples, and cDNA was synthesized by reverse transcription. Real-time PCR was performed on an ABI Prism 7300 sequence detection system with SYBR-Green PCR master mix according to the manufacturer’s instructions (Applied Biosystems, CA). The primers used are as follows:
PKD1, forward primer: 5’-CCCTCTCGGAGCAGAATCAAT-3’, reverse primer: 5’-GTGTTGAGCTAATGGGCAGG-3’;
PKD2, forward primer: 5’-GGGGAACAAGACTCATGGAAG-3’, reverse primer: 5’-GCCGTAGGTCAAGATGCACAA-3’;
Pkhd1, forward primer:5’-GGGAGGTCGATGGTGCATAAG-3’, reverse primer: 5’-GATGTCCGTTCTTCCCCCAAG-3’;
Hnf1b, forward primer: 5’-AGGGAGGTGGTCGATGTCA-3’, reverse primer: 5’-TCTGGACTGTCTGGTTGAACT-3’;
C2, forward primer: 5’-CGGTGGTAATTTCACCCTCAG-3’, reverse primer: 5’-GGTGTGATGTGAGCTAGACCT-3’;
C5, forward primer: 5’-GAACAAACCTACGTCATTTCAGC-3’, reverse primer 5’-GTCAACAGTGCCGCGTTTT-3’;
Pgc1a, forward primer: 5’-TATGGAGTGACATAGAGTGTGCT-3’, reverse primer: 5’-CCACTTCAATCCACCCAGAAAG-3’;
Tfam, forward primer: 5’-ATTCCGAAGTGTTTTTCCAGCA-3’, reverse primer: 5’-TCTGAAAGTTTTGCATCTGGGT-3’;
Wnt1, forward primer: 5’-GGTTTCTACTACGTTGCTACTGG-3’, reverse primer: 5’-GGAATCCGTCAACAGGTTCGT-3’;
Ctnnb1, forward primer: 5’-ATGGAGCCGGACAGAAAAGC-3’, reverse primer: 5’-CTTGCCACTCAGGGAAGGA-3’;
Srebf1, forward primer: 5’-GATGTGCGAACTGGACACAG-3’, reverse primer: 5’-CATAGGGGGCGTCAAACAG-3’;
Srebf2, forward primer: 5’-GCAGCAACGGGACCATTCT-3’, reverse primer: 5’-CCCCATGACTAAGTCCTTCAACT-3’;
β-actin, forward primer: 5’-AGAGGGAAATCGTGCGTGAC-3’, reverse primer: 5’-CAATAGTGATGACCTGGCCGT-3’.
Results
Generation of a mouse model manifesting PKD phenotypes
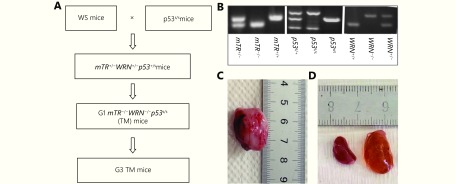
We crossed mice carrying p53S mutation with WS mice and obtained the first generation of mice with telomerase, WRN knockout, and p53S mutations (G1mTR-/-WRN-/-p53S/S), referred to as G1 triple mutation (G1TM). The mice were then bred generation-by-generation to obtain G2 and G3 TM mice (Figure 1A and 1B).
1.
Generation of a mouse model manifesting PKD.
As expected, we observed the incidence of sarcomas when telomere length was shortened to a certain level, which occurred in G3TM (G3mTR-/-WRN-/-p53S/S) mice (Figure 1C). The affected mice were sacrificed and anatomical analysis showed that the mice also manifested unilateral or bilateral enlarged kidneys with multiple fluid-filled cysts (Figure 1D). Thus, surprisingly, PKD phenotypes were found in G3TM mice at around 4 months old.
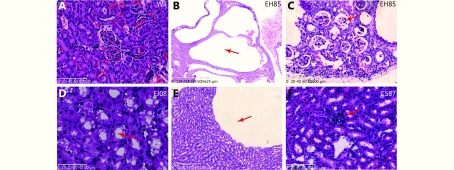
The H&E of the kidney sections showed that the kidneys from wild type mice developed normal renal tubules and glomeruli (Figure 2A), while the kidneys from G3TM mice displayed a range of phenotypes associated with renal dysplasia and renal cyst formation. In the G3TM mouse EH85, the normal histological structure of the right kidney was completely replaced by fluid-filled cysts of various sizes (Figure 2B). At higher magnification, we could observe that the renal tubules and glomeruli were compressed and atrophied, and the glomerulus lost its capillary loop structure completely (Figure 2C). These data show the severe fluid-filled cyst formation and total loss of renal function in this kidney. In the kidney from G3TM mouse EJ08, cellular swelling or hydropic degeneration and vacuolation were observed (Figure 2D), suggesting the dysfunction of ion and water regulation in these renal cells. In the kidneys from G3TM mouse EM06, the cyst is surrounded by flat epithelial cells, which suggests that cellular morphological changes are caused by fluid pressure from the cyst (Figure 2E). In the kidney from G3TM mouse CS87, we found the abnormal glomerulus with poorly defined capillary loop (Figure 2F). The abnormal glomerulus with semi-enclosed capillary loop was also frequently observed, indicating the loss of glomerulus function and downregulation of blood filtering function.
2.
Hematoxylin and eosin staining of kidney sections from mice with PKD phenotype.
Together these data suggest that kidneys from G3mTR-/-WRN-/-p53S/S mice were hypoplastic and developed PKD phenotypes.
The correlation of tumorigenesis and PKD phenotypes
As described earlier, the G3TM mice should manifest phenotypes that correlate with abnormal DNA damage response and abnormal proliferation. In our case, it manifested as increased tumorigenesis and PKD formation. To further understand the relationship between abnormal DNA damage response, tumorigenesis, and PKD phenotypes, we analyzed the frequencies and co-occurrence of cystic kidney and tumorigenesis in mice groups with different genotypes.
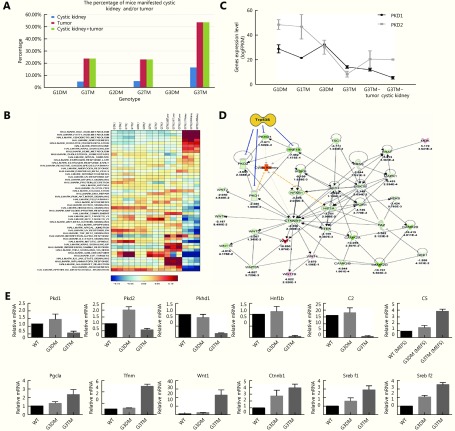
We did not find any tumorigenesis or PKD in those mice with WRN and telomerase double knockout, including G1DM mice (n=41), G2DM mice (n=52), and G3DM (n=63). However, we observed a few PKD or tumor incidences in G1TM and G2TM mice; this number increased dramatically in G3TM mice (Table 1, Figure 3A). The incidence increased along with telomere shortening (G1-G2-G3) and the introduction of p53S (TM vs. DM). These data strongly suggest that interplay of telomere DNA damage and p53S mutation contributed to the development of PKD. Furthermore, most PKD co-occurred with tumor phenotypes (Table 1, Figure 3A), showing that the occurrence of PKD phenotype was highly correlated with increased tumorigenesis.
1.
The occurrence of cystic kidney and/or tumor in mice with different genotypes
| Number of mice | G1DM | G1 TM | G2 DM | G2 TM | G3 DM | G3 TM |
| Cystic kidney | 0 | 1 | 0 | 2 | 0 | 4 |
| Tumor | 0 | 5 | 0 | 9 | 0 | 23 |
| Cystic kidney+ tumor | 0 | 5 | 0 | 9 | 0 | 23 |
| Total | 41 | 21 | 52 | 39 | 63 | 43 |
3.
Co-occurrence of tumorigenesis with PKD and gene signature analysis.
Gene signatures of PKD caused by telomere dysfunction and p53S mutation
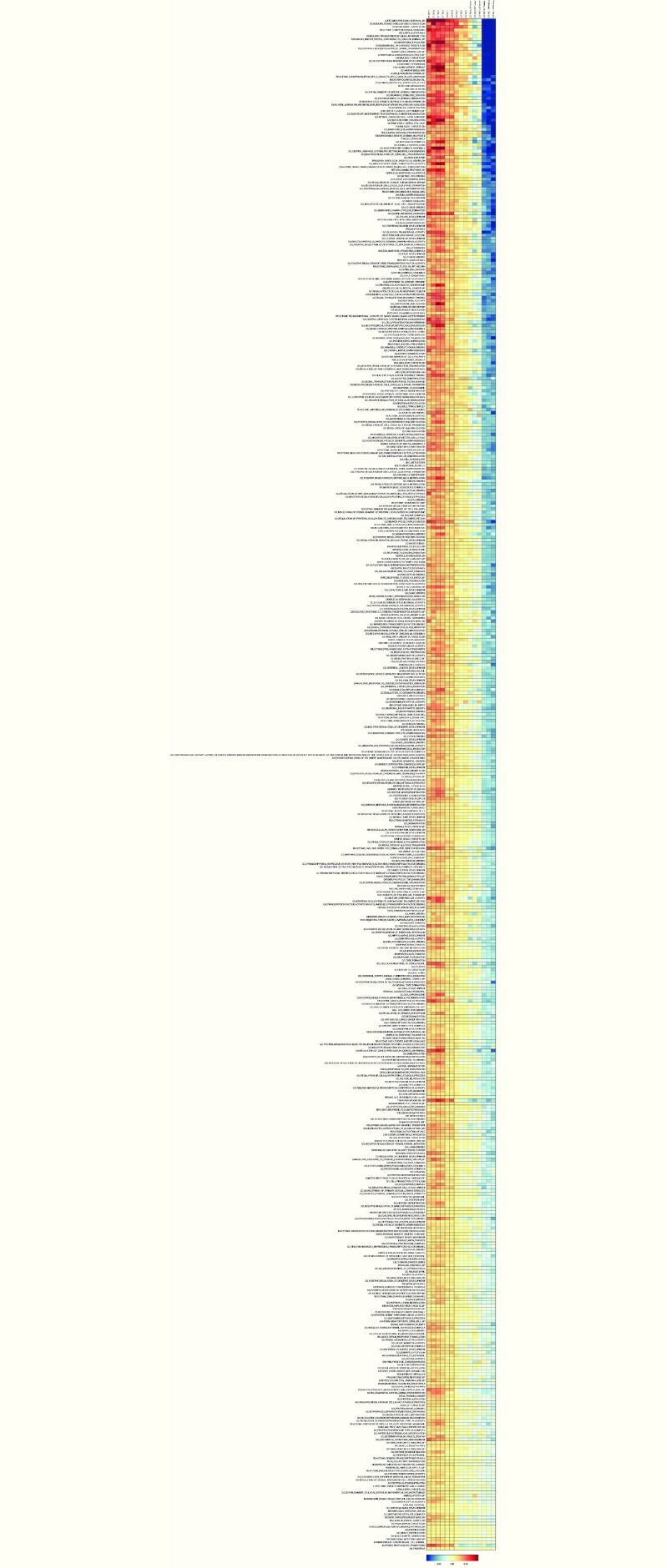
Since the genetic defect in this PKD model is very different from classical PKD models with polycystins defects, we were interested in investigating the gene signatures in MEFs (G3TM), cystic kidneys, and tumors from G3TM. We compared the gene expression profiles in MEFs from G1DM to G3TM mice using RNA-seq and ssGSEA analysis, as well as the tumors and cystic kidneys from G3TM mice.
First, we analyzed the gene signatures that were upregulated or downregulated in cystic kidneys using the Hallmark dataset. We found that the metabolism-related pathways, particularly lipid metabolism, were strikingly upregulated in cystic kidneys. These included bile acid metabolism, fatty acid metabolism and others (Figure 3B). Cell cycle-related pathways were clearly downregulated, such as mitotic spindle, G2M checkpoint, and E2F targets. (Figure 3B). These data suggest that abnormal metabolic regulation contributed greatly to PKD progress in G3TM mice.
Interestingly, the pathways such as oxidative phosphorylation, complement, and interferon alpha gamma were upregulated in both cystic kidneys and tumors (Figure 3B). These common regulated pathways suggest that the development of cystic kidney shares common mechanisms with tumorigenesis.
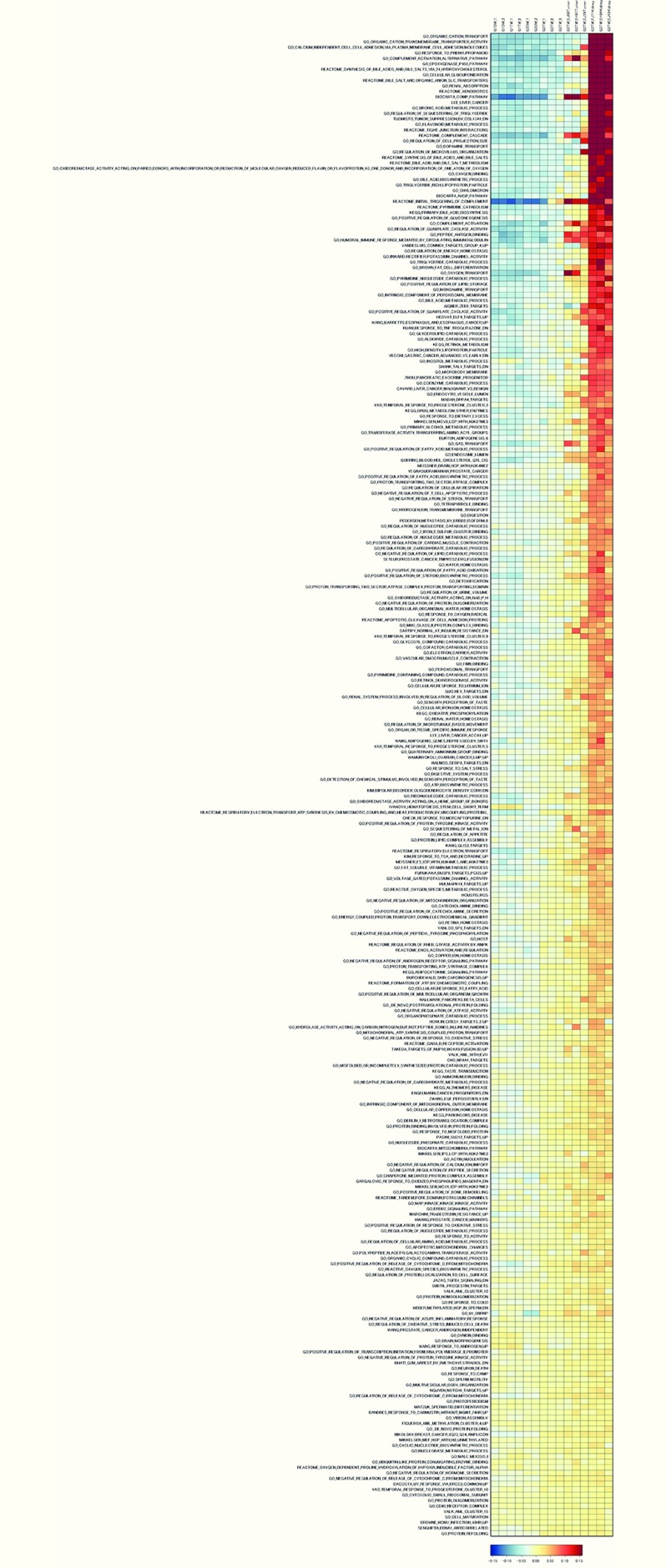
We then expanded the ssGSEA analysis by combining the Hallmark, C2, and C5 datasets20, and mapping the gene signatures that were gradually upregulated or downregulated in G3TM cells, tumors, and cystic kidneys (Supplementary Figure S1 and S2). The data revealed that most strikingly upregulated pathways shared by tumors and cystic kidneys included complement pathways, the immune response, lipid metabolism, and mitochondrial energy homeostasis. Interestingly, we observed that kidney function-related pathways, such as microvillus organization and water homeostasis, were upregulated in both tumors and kidneys. The data also show that organic cation transport and glucuronidation pathways were highly upregulated in cystic kidneys (Supplementary Figure S1).
S1.
A heatmap of gene expression profiles (ssGSEA analysis results of the RNA-seq data using Hallmark, C2, and C5 datasets) in MEFs from G1DM, G2DM, G3DM, G1TM, G2TM, and G3TM mice, as well as the tumors and cystic kidneys from G3TM mice. The pathways were ranked by scores, showing upregulation in cystic kidney, as well as in the tumor and G3TM MEFs.
On the other hand, the pathways obviously downregulated in tumor and kidneys included cytoskeleton regulation, extracellular signal transduction and others (Supplementary Figure S2). Together, regulation of these pathways revealed that G3TM PKD shares common mechanisms with tumorigenesis. These dysfunctions of gene regulation composed the gene signatures of G3TM PKD.
Comparison of gene signatures in PKD caused by telomere dysfunction and p53S mutation with classical PKD caused by PKD1 or PKD2 deficiency
After analyzing the gene signatures in the G3TM PKD model (G3mTR-/-WRN-/-p53S/S), we compared the gene signatures in this model with classic PKD models with PKD1 or PKD2 deficiency. We analyzed RNA-seq data of the classic PKD models with PKD1 or PKD2 deficiency22 by the same ssGSEA analysis, and compared gene signatures between the three mouse models. The data, analyzed by the Hallmark dataset, showed that the common upregulated pathways among these three PKD models included complement, coagulation, and apical surface, whereas the common downregulated pathways included angiogenesis (Supplementary Table S1).
S1.
The common pathways shared by G3TM PKD and Pkd1/2-deficient PKD revealed by ssGSEA analysis results of the RNA-seq data using the Hallmark dataset
| Up-regulated in G3TM PKD | Down-regulated in G3TM PKD | ||
| Up-regulated
in Pkd1 deficient PKD |
Up-regulated
in Pkd2 deficient PKD |
Down-regulated
in Pkd1 deficient PKD |
Down-reulated
in Pkd2 deficient PKD |
| HALLMARK_APICAL_SURFACE | HALLMARK_ANDROGEN_RESPONSE | HALLMARK_ANGIOGENESIS | HALLMARK_ANGIOGENESIS |
| HALLMARK_COAGULATION | HALLMARK_APICAL_SURFACE | HALLMARK_GLYCOLYSIS | HALLMARK_
SPERMATOGENESIS |
| HALLMARK_COMPLEMENT | HALLMARK_
CHOLESTEROL_HOMEOSTASIS |
HALLMARK_MITOTIC_SPINDLE | |
| HALLMARK_
ESTROGEN_RESPONSE_LATE |
HALLMARK_COAGULATION | HALLMARK_MYOGENESIS | |
| HALLMARK_
KRAS_SIGNALING_DN |
HALLMARK_COMPLEMENT | HALLMARK_PI3K_AKT_
MTOR_SIGNALING |
|
| HALLMARK_
ESTROGEN_RESPONSE_EARLY |
HALLMARK_UV_RESPONSE_DN | ||
| HALLMARK_
ESTROGEN_RESPONSE_LATE |
|||
| HALLMARK_
INTERFERON_ALPHA_RESPONSE |
|||
| HALLMARK_
INTERFERON_GAMMA_RESPONSE |
|||
| HALLMARK_
PANCREAS_BETA_CELLS |
|||
| HALLMARK_
PROTEIN_SECRETION |
|||
The expanded analysis with Hallmark, C2, and C5 datasets revealed that common upregulated pathways included complement activation, bile acid metabolism, and ion homeostasis. The common downregulated pathways included cell-to-cell adhesion signaling and epithelial structural maintenance (Supplementary Table S2).
S2.
The common pathways shared by G3TM PKD and Pkd1/2-deficient PKD revealed by ssGSEA analysis results of the RNA-seq data using Hallmark, C2, and C5 dataset
| Up-regulated in G3TM PKD | Down-regulated in G3TM PKD | ||
| Up-regulated
in Pkd1 deficient PKD |
Up-regulated
in Pkd2 deficient PKD |
Down-regulated
in Pkd1 deficient PKD |
Down-regulated
in Pkd2 deficient PKD |
| AIGNER_ZEB1_TARGETS | AIGNER_ZEB1_TARGETS | AMIT_SERUM_
RESPONSE_240_MCF10A |
BECKER_TAMOXIFEN_
RESISTANCE_UP |
| BANDRES_RESPONSE_TO_
CARMUSTIN_WITHOUT_ MGMT_24HR_UP |
BIOCARTA_COMP_PATHWAY | BARIS_THYROID_CANCER_DN | BIOCARTA_
CELL2CELL_PATHWAY |
| BIOCARTA_COMP_PATHWAY | BROWNE_HCMV_
INFECTION_48HR_UP |
BECKER_TAMOXIFEN_
RESISTANCE_UP |
BIOCARTA_GCR_PATHWAY |
| DACOSTA_UV_RESPONSE_
VIA_ERCC3_COMMON_UP |
DACOSTA_UV_RESPONSE_
VIA_ERCC3_COMMON_UP |
BIOCARTA_
ELL2CELL_PATHWAY |
BIOCARTA_NO2IL12_PATHWAY |
| DURCHDEWALD_SKIN_
CARCINOGENESIS_UP |
DURCHDEWALD_SKIN_
CARCINOGENESIS_UP |
BIOCARTA_IL2RB_PATHWAY | BIOCARTA_
P53HYPOXIA_PATHWAY |
| FIGUEROA_AML_METHYLATION_CLUSTER_4_UP | ENGELMANN_CANCER_
PROGENITORS_DN |
BIOCARTA_SODD_PATHWAY | BIOCARTA_TALL1_PATHWAY |
| FURUKAWA_DUSP6_
TARGETS_PCI35_UP |
FIGUEROA_AML_
METHYLATION_CLUSTER_4_UP |
BOWIE_RESPONSE_
TO_EXTRACELLULAR_MATRIX |
BROWNE_INTERFERON_
RESPONSIVE_GENES |
| GO__DE_NOVO_
POSTTRANSLATIONAL_ PROTEIN_FOLDING |
FURUKAWA_DUSP6_
TARGETS_PCI35_UP |
BROWNE_INTERFERON_
RESPONSIVE_GENES |
CHAN_INTERFERON_
PRODUCING_DENDRITIC_CELL |
| GO__DE_NOVO_
PROTEIN_FOLDING |
GO__DE_NOVO_P
OSTTRANSLATIONAL_ PROTEIN_FOLDING |
BURTON_ADIPOGENESIS_12 | CHEMELLO_SOLEUS_VS_
EDL_MYOFIBERS_DN |
| GO_2_IRON_2_SULFUR_
CLUSTER_BINDING |
GO__DE_NOVO_
PROTEIN_FOLDING |
CHAN_INTERFERON_
PRODUCING_DENDRITIC_CELL |
CHIANG_LIVER_CANCER_
SUBCLASS_INTERFERON_UP |
| GO_AMMONIUM_ION_BINDING | GO_ACTIN_NUCLEATION | CHEMELLO_SOLEUS_VS_
EDL_MYOFIBERS_DN |
CLIMENT_BREAST_CANCER_
COPY_NUMBER_UP |
| GO_APOPTOTIC_
MITOCHONDRIAL_CHANGES |
GO_APOPTOTIC_
MITOCHONDRIAL_CHANGES |
CLIMENT_BREAST_CANCER_
COPY_NUMBER_UP |
DAUER_STAT3_TARGETS_DN |
| GO_BILE_ACID_
METABOLIC_PROCESS |
GO_BILE_ACID_
METABOLIC_PROCESS |
CROONQUIST_STROMAL_
STIMULATION_DN |
DOANE_BREAST_CANCER_
CLASSES_DN |
| GO_BRAIN_MORPHOGENESIS | GO_BROWN_FAT_
CELL_DIFFERENTIATION |
DAUER_STAT3_TARGETS_DN | DUTTA_APOPTOSIS_VIA_NFKB |
| GO_BROWN_FAT_
CELL_DIFFERENTIATION |
GO_CELL_MATURATION | DORN_ADENOVIRUS_
INFECTION_32HR_UP |
EINAV_INTERFERON_
SIGNATURE_IN_CANCER |
| GO_CALCIUM_INDEPENDENT_
CELL_CELL_ADHESION_VIA_ PLASMA_MEMBRANE_CELL_ ADHESION_MOLECULES |
GO_CELLULAR_IRON_ION_HOMEOSTASIS | DORN_ADENOVIRUS_INFECTION_48HR_UP | FARMER_BREAST_CANCER_CLUSTER_1 |
| GO_CATECHOLAMINE_BINDING | GO_CHAPERONE_MEDIATED_PROTEIN_COMPLEX_ASSEMBLY | DUTTA_APOPTOSIS_VIA_NFKB | FERRANDO_LYL1_NEIGHBORS |
| GO_CELLULAR_IRON_ION_HOMEOSTASIS | GO_COMPLEMENT_ACTIVATION | EINAV_INTERFERON_SIGNATURE_IN_CANCER | GAUSSMANN_MLL_AF4_FUSION_TARGETS_F_DN |
| GO_CHAPERONE_MEDIATED_PROTEIN_COMPLEX_ASSEMBLY | GO_COMPLEMENT_ACTIVATION_ALTERNATIVE_PATHWAY | FIGUEROA_AML_METHYLATION_CLUSTER_5_DN | GO_ACETYLGALACTOSAMINYLTRANSFERASE_ACTIVITY |
| GO_CHYLOMICRON | GO_CYTOSOLIC_SMALL_RIBOSOMAL_SUBUNIT | FINETTI_BREAST_CANCER_KINOME_GREEN | GO_ACTIN_FILAMENT_POLYMERIZATION |
| GO_COMPLEMENT_ACTIVATION | GO_DETECTION_OF_CHEMICAL_STIMULUS_INVOLVED_IN_SENSORY_PERCEPTION_OF_TASTE | FUNG_IL2_SIGNALING_2 | GO_ACTIVATION_OF_CYSTEINE_TYPE_ENDOPEPTIDASE_ACTIVITY_INVOLVED_IN_APOPTOTIC_SIGNALING_PATHWAY |
| GO_COMPLEMENT_ACTIVATION_ALTERNATIVE_PATHWAY | GO_DYNEIN_BINDING | GAUSSMANN_MLL_AF4_FUSION_TARGETS_F_DN | GO_ADENYLATE_CYCLASE_ACTIVATING_DOPAMINE_RECEPTOR_SIGNALING_PATHWAY |
| GO_CYTOSOLIC_SMALL_RIBOSOMAL_SUBUNIT | GO_ERBB2_SIGNALING_PATHWAY | GAVIN_FOXP3_TARGETS_CLUSTER_T7 | GO_ADENYLATE_CYCLASE_ACTIVATING_G_PROTEIN_COUPLED_RECEPTOR_SIGNALING_PATHWAY |
| GO_DETECTION_OF_CHEMICAL_STIMULUS_INVOLVED_IN_SENSORY_PERCEPTION_OF_TASTE | GO_FAT_SOLUBLE_VITAMIN_METABOLIC_PROCESS | GENTILE_UV_RESPONSE_CLUSTER_D1 | GO_ADENYLATE_CYCLASE_MODULATING_G_PROTEIN_COUPLED_RECEPTOR_SIGNALING_PATHWAY |
| GO_DETOXIFICATION | GO_GAS_TRANSPORT | GO_14_3_3_PROTEIN_BINDING | GO_ADRENERGIC_RECEPTOR_SIGNALING_PATHWAY |
| GO_ENDOCYTIC_VESICLE_LUMEN | GO_HUMORAL_IMMUNE_RESPONSE_MEDIATED_BY_CIRCULATING_IMMUNOGLOBULIN | GO_ACETYLGALACTOSAMINYLTRANSFERASE_ACTIVITY | GO_AXON_REGENERATION |
| GO_EPOXYGENASE_P450_PATHWAY | GO_HYDROLASE_ACTIVITY_ACTING_ON_CARBON_NITROGEN_BUT_NOT_PEPTIDE_BONDS_IN_LINEAR_AMIDINES | GO_ACROSOME_ASSEMBLY | GO_B_CELL_RECEPTOR_SIGNALING_PATHWAY |
| GO_FAT_SOLUBLE_VITAMIN_METABOLIC_PROCESS | GO_MAP_KINASE_KINASE_KINASE_ACTIVITY | GO_ACTIN_FILAMENT_POLYMERIZATION | GO_BASEMENT_MEMBRANE_ORGANIZATION |
| GO_HIGH_DENSITY_LIPOPROTEIN_PARTICLE | GO_MHC_CLASS_II_PROTEIN_COMPLEX_BINDING | GO_ACTIVATION_OF_ADENYLATE_CYCLASE_ACTIVITY | GO_BETA_1_3_GALACTOSYLTRANSFERASE_ACTIVITY |
| GO_HUMORAL_IMMUNE_RESPONSE_MEDIATED_BY_CIRCULATING_IMMUNOGLOBULIN | GO_MULTIVESICULAR_BODY_ORGANIZATION | GO_ACTIVATION_OF_CYSTEINE_TYPE_ENDOPEPTIDASE_ACTIVITY_INVOLVED_IN_APOPTOTIC_SIGNALING_PATHWAY | GO_CELLULAR_RESPONSE_TO_EXOGENOUS_DSRNA |
| GO_HYDROLASE_ACTIVITY_ACTING_ON_CARBON_NITROGEN_BUT_NOT_PEPTIDE_BONDS_IN_LINEAR_AMIDINES | GO_NEGATIVE_REGULATION_OF_ACUTE_INFLAMMATORY_RESPONSE | GO_ADENYLATE_CYCLASE_ACTIVATING_G_PROTEIN_COUPLED_RECEPTOR_SIGNALING_PATHWAY | GO_CELLULAR_RESPONSE_TO_PROSTAGLANDIN_E_STIMULUS |
| GO_INTRINSIC_COMPONENT_OF_MITOCHONDRIAL_OUTER_MEMBRANE | GO_NEGATIVE_REGULATION_OF_ANDROGEN_RECEPTOR_SIGNALING_PATHWAY | GO_ADENYLYLTRANSFERASE_ACTIVITY | GO_COPPER_ION_TRANSPORT |
| GO_MHC_CLASS_II_PROTEIN_COMPLEX_BINDING | GO_NEGATIVE_REGULATION_OF_CALCIUM_ION_IMPORT | GO_ANTIGEN_BINDING | GO_CYTOLYSIS |
| GO_MITOCHONDRIAL_ATP_SYNTHESIS_COUPLED_PROTON_TRANSPORT | GO_NEGATIVE_REGULATION_OF_CARBOHYDRATE_METABOLIC_PROCESS | GO_B_CELL_ACTIVATION | GO_CYTOPLASMIC_SEQUESTERING_OF_TRANSCRIPTION_FACTOR |
| GO_MULTIVESICULAR_BODY_ORGANIZATION | GO_NEGATIVE_REGULATION_OF_HORMONE_SECRETION | GO_B_CELL_RECEPTOR_SIGNALING_PATHWAY | GO_DISRUPTION_OF_CELLS_OF_OTHER_ORGANISM |
| GO_NEGATIVE_REGULATION_OF_ACUTE_INFLAMMATORY_RESPONSE | GO_NEGATIVE_REGULATION_OF_PEPTIDE_SECRETION | GO_BETA_1_3_GALACTOSYLTRANSFERASE_ACTIVITY | GO_DISRUPTION_OF_CELLS_OF_OTHER_ORGANISM_INVOLVED_IN_SYMBIOTIC_INTERACTION |
| GO_NEGATIVE_REGULATION_OF_ANDROGEN_RECEPTOR_SIGNALING_PATHWAY | GO_NEGATIVE_REGULATION_OF_PROTEIN_OLIGOMERIZATION | GO_CELLULAR_COMPONENT_DISASSEMBLY_INVOLVED_IN_EXECUTION_PHASE_OF_APOPTOSIS | GO_DNA_TEMPLATED_TRANSCRIPTIONAL_PREINITIATION_COMPLEX_ASSEMBLY |
| GO_NEGATIVE_REGULATION_OF_CALCIUM_ION_IMPORT | GO_NEGATIVE_REGULATION_OF_RELEASE_OF_CYTOCHROME_C_FROM_MITOCHONDRIA | GO_CELLULAR_RESPONSE_TO_ACID_CHEMICAL | GO_DOPAMINE_RECEPTOR_BINDING |
| GO_NEGATIVE_REGULATION_OF_HORMONE_SECRETION | GO_NUCLEOBASE_METABOLIC_PROCESS | GO_CELLULAR_RESPONSE_TO_EXOGENOUS_DSRNA | GO_DOPAMINE_RECEPTOR_SIGNALING_PATHWAY |
| GO_NEGATIVE_REGULATION_OF_LIPID_CATABOLIC_PROCESS | GO_NUCLEOSIDE_PHOSPHATE_CATABOLIC_PROCESS | GO_CELLULAR_RESPONSE_TO_GLUCOSE_STARVATION | GO_DRUG_BINDING |
| GO_NEGATIVE_REGULATION_OF_PEPTIDE_SECRETION | GO_ORGANIC_CYCLIC_COMPOUND_CATABOLIC_PROCESS | GO_CELLULAR_RESPONSE_TO_PROSTAGLANDIN_E_STIMULUS | GO_ENDOPLASMIC_RETICULUM_CHAPERONE_COMPLEX |
| GO_NEGATIVE_REGULATION_OF_RELEASE_OF_CYTOCHROME_C_FROM_MITOCHONDRIA | GO_OXYGEN_TRANSPORT | GO_CELLULAR_RESPONSE_TO_PROSTAGLANDIN_STIMULUS | GO_EPITHELIAL_STRUCTURE_MAINTENANCE |
| GO_NEGATIVE_REGULATION_OF_RESPONSE_TO_OXIDATIVE_STRESS | GO_PEPTIDE_ANTIGEN_BINDING | GO_COPPER_ION_TRANSPORT | GO_ERYTHROCYTE_DEVELOPMENT |
| GO_ORGAN_OR_TISSUE_SPECIFIC_IMMUNE_RESPONSE | GO_POSITIVE_REGULATION_OF_CARDIAC_MUSCLE_CONTRACTION | GO_CYCLIN_DEPENDENT_PROTEIN_SERINE_THREONINE_KINASE_INHIBITOR_ACTIVITY | GO_EXECUTION_PHASE_OF_APOPTOSIS |
| GO_OXIDOREDUCTASE_ACTIVITY_ACTING_ON_PAIRED_DONORS_WITH_INCORPORATION_OR_REDUCTION_OF_MOLECULAR_OXYGEN_REDUCED_FLAVIN_OR_FLAVOPROTEIN_AS_ONE_DONOR_AND_INCORPORATION_OF_ONE_ATOM_OF_OXYGEN | GO_POSITIVE_REGULATION_OF_CATECHOLAMINE_SECRETION | GO_CYTOPLASMIC_SEQUESTERING_OF_TRANSCRIPTION_FACTOR | GO_GRANULOCYTE_DIFFERENTIATION |
| GO_OXYGEN_BINDING | GO_POSITIVE_REGULATION_OF_TRANSCRIPTION_INITIATION_FROM_RNA_POLYMERASE_II_PROMOTER | GO_DEAMINASE_ACTIVITY | GO_INTERACTION_WITH_SYMBIONT |
| GO_OXYGEN_TRANSPORT | GO_PROTEIN_BINDING_INVOLVED_IN_PROTEIN_FOLDING | GO_DEFENSE_RESPONSE_TO_VIRUS | GO_ISOPRENOID_BINDING |
| GO_POSITIVE_REGULATION_OF_CARDIAC_MUSCLE_CONTRACTION | GO_REGULATION_OF_APPETITE | GO_DOPAMINE_RECEPTOR_BINDING | GO_LYMPHOID_PROGENITOR_CELL_DIFFERENTIATION |
| GO_POSITIVE_REGULATION_OF_FATTY_ACID_METABOLIC_PROCESS | GO_REGULATION_OF_CELL_PROJECTION_SIZE | GO_ENDOLYSOSOME | GO_MACROPHAGE_DIFFERENTIATION |
| GO_POSITIVE_REGULATION_OF_FATTY_ACID_OXIDATION | GO_REGULATION_OF_CELLULAR_AMINO_ACID_METABOLIC_PROCESS | GO_ENDOPLASMIC_RETICULUM_CHAPERONE_COMPLEX | GO_MAINTENANCE_OF_CELL_POLARITY |
| GO_POSITIVE_REGULATION_OF_LIPID_STORAGE | GO_REGULATION_OF_MICROTUBULE_BASED_MOVEMENT | GO_EPITHELIAL_STRUCTURE_MAINTENANCE | GO_MAINTENANCE_OF_GASTROINTESTINAL_EPITHELIUM |
| GO_POSITIVE_REGULATION_OF_RELEASE_OF_CYTOCHROME_C_FROM_MITOCHONDRIA | GO_REGULATION_OF_URINE_VOLUME | GO_EXTRINSIC_APOPTOTIC_SIGNALING_PATHWAY_VIA_DEATH_DOMAIN_RECEPTORS | GO_MAP_KINASE_ACTIVITY |
| GO_POSITIVE_REGULATION_OF_RESPONSE_TO_OXIDATIVE_STRESS | GO_RENAL_SYSTEM_PROCESS_INVOLVED_IN_REGULATION_OF_BLOOD_VOLUME | GO_FEMALE_GAMETE_GENERATION | GO_MULTICELLULAR_ORGANISMAL_MOVEMENT |
| GO_POSITIVE_REGULATION_OF_TRANSCRIPTION_INITIATION_FROM_RNA_POLYMERASE_II_PROMOTER | GO_RESPONSE_TO_ACTIVITY | GO_G_PROTEIN_BETA_GAMMA_SUBUNIT_COMPLEX_BINDING | GO_NATURAL_KILLER_CELL_DIFFERENTIATION |
| GO_PROTEIN_BINDING_INVOLVED_IN_PROTEIN_FOLDING | GO_RESPONSE_TO_CAMP | GO_G_PROTEIN_COUPLED_RECEPTOR_SIGNALING_PATHWAY_COUPLED_TO_CYCLIC_NUCLEOTIDE_SECOND_MESSENGER | GO_NECROTIC_CELL_DEATH |
| GO_PROTEIN_REFOLDING | GO_RESPONSE_TO_COLD | GO_GALACTOSYLTRANSFERASE_ACTIVITY | GO_NEGATIVE_REGULATION_OF_CALCIUM_ION_TRANSMEMBRANE_TRANSPORT |
| GO_PROTON_TRANSPORTING_ATP_SYNTHASE_COMPLEX | GO_RESPONSE_TO_DIETARY_EXCESS | GO_GLYCOPROTEIN_CATABOLIC_PROCESS | GO_NEGATIVE_REGULATION_OF_GLYCOPROTEIN_BIOSYNTHETIC_PROCESS |
| GO_QUATERNARY_AMMONIUM_GROUP_BINDING | GO_RESPONSE_TO_MISFOLDED_PROTEIN | GO_GRANULOCYTE_DIFFERENTIATION | GO_NEGATIVE_REGULATION_OF_HOMEOSTATIC_PROCESS |
| GO_REACTIVE_OXYGEN_SPECIES_BIOSYNTHETIC_PROCESS | GO_RESPONSE_TO_SALT_STRESS | GO_GTPASE_ACTIVATING_PROTEIN_BINDING | GO_NEGATIVE_REGULATION_OF_INTERLEUKIN_1_PRODUCTION |
| GO_REACTIVE_OXYGEN_SPECIES_METABOLIC_PROCESS | GO_RETINA_HOMEOSTASIS | GO_I_KAPPAB_KINASE_NF_KAPPAB_SIGNALING | GO_NEGATIVE_REGULATION_OF_INTERLEUKIN_10_PRODUCTION |
| GO_REGULATION_OF_APPETITE | GO_RETINOL_DEHYDROGENASE_ACTIVITY | GO_ISOPRENOID_BINDING | GO_NEGATIVE_REGULATION_OF_INTRINSIC_APOPTOTIC_SIGNALING_PATHWAY |
| GO_REGULATION_OF_CELLULAR_AMINO_ACID_METABOLIC_PROCESS | GO_SENSORY_PERCEPTION_OF_TASTE | GO_JNK_CASCADE | GO_NEGATIVE_REGULATION_OF_INTRINSIC_APOPTOTIC_SIGNALING_PATHWAY_IN_RESPONSE_TO_DNA_DAMAGE |
| GO_REGULATION_OF_ENERGY_HOMEOSTASIS | GO_SEQUESTERING_OF_METAL_ION | GO_KINASE_INHIBITOR_ACTIVITY | GO_NEGATIVE_REGULATION_OF_LEUKOCYTE_APOPTOTIC_PROCESS |
| GO_REGULATION_OF_MICROTUBULE_BASED_MOVEMENT | GO_TETRAPYRROLE_BINDING | GO_KINASE_REGULATOR_ACTIVITY | GO_NEGATIVE_REGULATION_OF_LYASE_ACTIVITY |
| GO_REGULATION_OF_OXIDATIVE_STRESS_INDUCED_CELL_DEATH | GO_U1_SNRNP | GO_LYMPH_NODE_DEVELOPMENT | GO_NEGATIVE_REGULATION_OF_LYMPHOCYTE_APOPTOTIC_PROCESS |
| GO_REGULATION_OF_RELEASE_OF_CYTOCHROME_C_FROM_MITOCHONDRIA | GO_UBIQUITIN_LIKE_PROTEIN_CONJUGATING_ENZYME_BINDING | GO_LYMPHOCYTE_HOMEOSTASIS | GO_NEGATIVE_REGULATION_OF_MYELOID_CELL_APOPTOTIC_PROCESS |
| GO_REGULATION_OF_SEQUESTERING_OF_TRIGLYCERIDE | GO_VIRION_ASSEMBLY | GO_MAINTENANCE_OF_GASTROINTESTINAL_EPITHELIUM | GO_NEGATIVE_REGULATION_OF_OSTEOCLAST_DIFFERENTIATION |
| GO_REGULATION_OF_URINE_VOLUME | GOERING_BLOOD_HDL_CHOLESTEROL_QTL_CIS | GO_MEMBRANE_TUBULATION | GO_NEGATIVE_REGULATION_OF_RESPONSE_TO_BIOTIC_STIMULUS |
| GO_RENAL_SYSTEM_PROCESS_INVOLVED_IN_REGULATION_OF_BLOOD_VOLUME | HALLMARK_PANCREAS_BETA_CELLS | GO_MITOGEN_ACTIVATED_PROTEIN_KINASE_KINASE_BINDING | GO_NEGATIVE_REGULATION_OF_RESPONSE_TO_DNA_DAMAGE_STIMULUS |
| GO_RESPONSE_TO_CAMP | HALMOS_CEBPA_TARGETS_DN | GO_MITOTIC_SISTER_CHROMATID_COHESION | GO_NEGATIVE_REGULATION_OF_SIGNAL_TRANSDUCTION_BY_P53_CLASS_MEDIATOR |
| GO_RESPONSE_TO_COLD | HOUSTIS_ROS | GO_MODULATION_BY_HOST_OF_VIRAL_PROCESS | GO_NEGATIVE_REGULATION_OF_STAT_CASCADE |
| GO_RESPONSE_TO_DIETARY_EXCESS | HUI_MAPK14_TARGETS_UP | GO_MRNA_TRANSCRIPTION | GO_NEGATIVE_REGULATION_OF_TRANSMEMBRANE_TRANSPORT |
| GO_RESPONSE_TO_MISFOLDED_PROTEIN | HWANG_PROSTATE_CANCER_MARKERS | GO_MRNA_TRANSCRIPTION_FROM_RNA_POLYMERASE_II_PROMOTER | GO_NEGATIVE_T_CELL_SELECTION |
| GO_RESPONSE_TO_OXYGEN_RADICAL | KANG_GLIS3_TARGETS | GO_NATURAL_KILLER_CELL_ACTIVATION | GO_NEURON_PROJECTION_REGENERATION |
| GO_RESPONSE_TO_PHENYLPROPANOID | KEGG_ADIPOCYTOKINE_SIGNALING_PATHWAY | GO_NATURAL_KILLER_CELL_DIFFERENTIATION | GO_NUCLEAR_INCLUSION_BODY |
| GO_RETINA_HOMEOSTASIS | KEGG_RETINOL_METABOLISM | GO_NECROTIC_CELL_DEATH | GO_NUCLEOTIDASE_ACTIVITY |
| GO_RETINOL_DEHYDROGENASE_ACTIVITY | KIM_BIPOLAR_DISORDER_OLIGODENDROCYTE_DENSITY_CORR_DN | GO_NEGATIVE_REGULATION_OF_HOMEOSTATIC_PROCESS | GO_PHOSPHOLIPASE_C_ACTIVATING_G_PROTEIN_COUPLED_RECEPTOR_SIGNALING_PATHWAY |
| GO_SENSORY_PERCEPTION_OF_TASTE | KIM_RESPONSE_TO_TSA_AND_DECITABINE_UP | GO_NEGATIVE_REGULATION_OF_LEUKOCYTE_APOPTOTIC_PROCESS | GO_PHOSPHOLIPASE_C_ACTIVITY |
| GO_SPERM_MOTILITY | LEE_LIVER_CANCER_ACOX1_UP | GO_NEGATIVE_REGULATION_OF_LIPID_BIOSYNTHETIC_PROCESS | GO_PHOSPHOTRANSFERASE_ACTIVITY_NITROGENOUS_GROUP_AS_ACCEPTOR |
| GO_TETRAPYRROLE_BINDING | MATZUK_SPERMATID_DIFFERENTIATION | GO_NEGATIVE_REGULATION_OF_LYMPHOCYTE_APOPTOTIC_PROCESS | GO_POLY_A_MRNA_EXPORT_FROM_NUCLEUS |
| GO_U1_SNRNP | MEISSNER_ES_ICP_WITH_H3K4ME3_AND_H3K27ME3 | GO_NEGATIVE_REGULATION_OF_LYMPHOCYTE_MEDIATED_IMMUNITY | GO_POSITIVE_REGULATION_OF_B_CELL_PROLIFERATION |
| GO_UBIQUITIN_LIKE_PROTEIN_CONJUGATING_ENZYME_BINDING | MIKKELSEN_IPS_LCP_WITH_H3K27ME3 | GO_NEGATIVE_REGULATION_OF_MYELOID_CELL_APOPTOTIC_PROCESS | GO_POSITIVE_REGULATION_OF_CAMP_MEDIATED_SIGNALING |
| GO_VIRION_ASSEMBLY | MIKKELSEN_MEF_HCP_WITH_H3_UNMETHYLATED | GO_NEGATIVE_REGULATION_OF_OSTEOCLAST_DIFFERENTIATION | GO_POSITIVE_REGULATION_OF_ERYTHROCYTE_DIFFERENTIATION |
| HALMOS_CEBPA_TARGETS_DN | NGUYEN_NOTCH1_TARGETS_UP | GO_NEGATIVE_REGULATION_OF_RESPONSE_TO_BIOTIC_STIMULUS | GO_POSITIVE_REGULATION_OF_INTRINSIC_APOPTOTIC_SIGNALING_PATHWAY |
| HEDVAT_ELF4_TARGETS_UP | NIKOLSKY_BREAST_CANCER_8Q23_Q24_AMPLICON | GO_NEGATIVE_REGULATION_OF_RESPONSE_TO_DNA_DAMAGE_STIMULUS | GO_POSITIVE_REGULATION_OF_LYASE_ACTIVITY |
| HOUSTIS_ROS | PEDERSEN_METASTASIS_BY_ERBB2_ISOFORM_6 | GO_NEGATIVE_REGULATION_OF_STAT_CASCADE | GO_POSITIVE_REGULATION_OF_LYMPHOCYTE_MIGRATION |
| HOWLIN_CITED1_TARGETS_2_UP | REACTOME_APOPTOTIC_CLEAVAGE_OF_CELL_ADHESION_PROTEINS | GO_NEGATIVE_REGULATION_OF_TRANSMEMBRANE_TRANSPORT | GO_POSITIVE_REGULATION_OF_MEMBRANE_INVAGINATION |
| HUI_MAPK14_TARGETS_UP | REACTOME_COMPLEMENT_CASCADE | GO_NEGATIVE_REGULATION_OF_TYPE_I_INTERFERON_PRODUCTION | GO_POSITIVE_REGULATION_OF_NUCLEOTIDE_METABOLIC_PROCESS |
| HWANG_PROSTATE_CANCER_MARKERS | REACTOME_INITIAL_TRIGGERING_OF_COMPLEMENT | GO_NUCLEOTIDASE_ACTIVITY | GO_POSITIVE_REGULATION_OF_OXIDATIVE_STRESS_INDUCED_CELL_DEATH |
| KANG_GLIS3_TARGETS | REACTOME_REGULATION_OF_RHEB_GTPASE_ACTIVITY_BY_AMPK | GO_OLIGOSACCHARIDE_BIOSYNTHETIC_PROCESS | GO_POSITIVE_REGULATION_OF_PROTEIN_DEACETYLATION |
| KEGG_PARKINSONS_DISEASE | REACTOME_TANDEM_PORE_DOMAIN_POTASSIUM_CHANNELS | GO_OOCYTE_MATURATION | GO_POSITIVE_REGULATION_OF_THYMOCYTE_AGGREGATION |
| KEGG_TASTE_TRANSDUCTION | SHANK_TAL1_TARGETS_DN | GO_PARTURITION | GO_PROSTANOID_METABOLIC_PROCESS |
| KIM_BIPOLAR_DISORDER_OLIGODENDROCYTE_DENSITY_CORR_DN | SUBTIL_PROGESTIN_TARGETS | GO_PHOSPHATE_ION_BINDING | GO_PROTEIN_DESTABILIZATION |
| KIM_RESPONSE_TO_TSA_AND_DECITABINE_UP | VALK_AML_CLUSTER_10 | GO_PHOSPHATIDIC_ACID_BINDING | GO_PROTEIN_HOMOTRIMERIZATION |
| LEE_LIVER_CANCER_ACOX1_UP | VALK_AML_CLUSTER_15 | GO_PHOSPHATIDYLINOSITOL_4_PHOSPHATE_BINDING | GO_PYRIMIDINE_CONTAINING_COMPOUND_SALVAGE |
| MATZUK_SPERMATID_DIFFERENTIATION | VALK_AML_WITH_EVI1 | GO_PHOSPHOLIPASE_C_ACTIVATING_G_PROTEIN_COUPLED_RECEPTOR_SIGNALING_PATHWAY | GO_REGULATION_OF_ADENYLATE_CYCLASE_ACTIVITY |
| MEISSNER_ES_ICP_WITH_H3K4ME3_AND_H3K27ME3 | WANG_BARRETTS_ESOPHAGUS_AND_ESOPHAGUS_CANCER_UP | GO_PHOSPHOLIPASE_C_ACTIVITY | GO_REGULATION_OF_ALPHA_AMINO_3_HYDROXY_5_METHYL_4_ISOXAZOLE_PROPIONATE_SELECTIVE_GLUTAMATE_RECEPTOR_ACTIVITY |
| MIKKELSEN_MEF_HCP_WITH_H3_UNMETHYLATED | WANG_PROSTATE_CANCER_ANDROGEN_INDEPENDENT | GO_PHOSPHOTRANSFERASE_ACTIVITY_NITROGENOUS_GROUP_AS_ACCEPTOR | GO_REGULATION_OF_B_CELL_RECEPTOR_SIGNALING_PATHWAY |
| NGUYEN_NOTCH1_TARGETS_UP | WANG_RESPONSE_TO_ANDROGEN_UP | GO_POSITIVE_REGULATION_OF_ALCOHOL_BIOSYNTHETIC_PROCESS | GO_REGULATION_OF_BONE_DEVELOPMENT |
| NIKOLSKY_BREAST_CANCER_8Q23_Q24_AMPLICON | WEBER_METHYLATED_HCP_IN_SPERM_DN | GO_POSITIVE_REGULATION_OF_B_CELL_DIFFERENTIATION | GO_REGULATION_OF_BONE_RESORPTION |
| PEDERSEN_METASTASIS_BY_ERBB2_ISOFORM_6 | YAO_TEMPORAL_RESPONSE_TO_PROGESTERONE_CLUSTER_10 | GO_POSITIVE_REGULATION_OF_B_CELL_PROLIFERATION | GO_REGULATION_OF_DEFENSE_RESPONSE_TO_VIRUS_BY_HOST |
| REACTOME_COMPLEMENT_CASCADE | YAO_TEMPORAL_RESPONSE_TO_PROGESTERONE_CLUSTER_5 | GO_POSITIVE_REGULATION_OF_CELLULAR_EXTRAVASATION | GO_REGULATION_OF_ERYTHROCYTE_DIFFERENTIATION |
| REACTOME_FORMATION_OF_ATP_BY_CHEMIOSMOTIC_COUPLING | YAO_TEMPORAL_RESPONSE_TO_PROGESTERONE_CLUSTER_9 | GO_POSITIVE_REGULATION_OF_ERYTHROCYTE_DIFFERENTIATION | GO_REGULATION_OF_FEVER_GENERATION |
| REACTOME_INITIAL_TRIGGERING_OF_COMPLEMENT | ZHOU_PANCREATIC_EXOCRINE_PROGENITOR | GO_POSITIVE_REGULATION_OF_INTERFERON_ALPHA_PRODUCTION | GO_REGULATION_OF_INTRINSIC_APOPTOTIC_SIGNALING_PATHWAY |
| REACTOME_OXYGEN_DEPENDENT_PROLINE_HYDROXYLATION_OF_HYPOXIA_INDUCIBLE_FACTOR_ALPHA | GO_POSITIVE_REGULATION_OF_INTERFERON_BETA_PRODUCTION | GO_REGULATION_OF_INTRINSIC_APOPTOTIC_SIGNALING_PATHWAY_BY_P53_CLASS_MEDIATOR | |
| REACTOME_REGULATION_OF_RHEB_GTPASE_ACTIVITY_BY_AMPK | GO_POSITIVE_REGULATION_OF_LAMELLIPODIUM_ASSEMBLY | GO_REGULATION_OF_INTRINSIC_APOPTOTIC_SIGNALING_PATHWAY_IN_RESPONSE_TO_DNA_DAMAGE | |
| REACTOME_RESPIRATORY_ELECTRON_TRANSPORT | GO_POSITIVE_REGULATION_OF_LYASE_ACTIVITY | GO_REGULATION_OF_INTRINSIC_APOPTOTIC_SIGNALING_PATHWAY_IN_RESPONSE_TO_DNA_DAMAGE_BY_P53_CLASS_MEDIATOR | |
| REACTOME_RESPIRATORY_ELECTRON_TRANSPORT_ATP_SYNTHESIS_BY_CHEMIOSMOTIC_COUPLING_AND_HEAT_PRODUCTION_BY_UNCOUPLING_PROTEINS_ | GO_POSITIVE_REGULATION_OF_LYMPHOCYTE_MIGRATION | GO_REGULATION_OF_LYASE_ACTIVITY | |
| REACTOME_TANDEM_PORE_DOMAIN_POTASSIUM_CHANNELS | GO_POSITIVE_REGULATION_OF_MEMBRANE_INVAGINATION | GO_REGULATION_OF_MEMBRANE_INVAGINATION | |
| REACTOME_TIGHT_JUNCTION_INTERACTIONS | GO_POSITIVE_REGULATION_OF_NATURAL_KILLER_CELL_MEDIATED_IMMUNITY | GO_REGULATION_OF_PROTEIN_TYROSINE_KINASE_ACTIVITY | |
| REACTOME_XENOBIOTICS | GO_POSITIVE_REGULATION_OF_NUCLEOTIDE_METABOLIC_PROCESS | GO_REGULATION_OF_RECEPTOR_BINDING | |
| SHANK_TAL1_TARGETS_DN | GO_POSITIVE_REGULATION_OF_PROTEIN_AUTOPHOSPHORYLATION | GO_REGULATION_OF_T_CELL_APOPTOTIC_PROCESS | |
| SUBTIL_PROGESTIN_TARGETS | GO_POSITIVE_REGULATION_OF_RESPONSE_TO_CYTOKINE_STIMULUS | GO_REGULATION_OF_THYMOCYTE_AGGREGATION | |
| VALK_AML_CLUSTER_10 | GO_POSITIVE_REGULATION_OF_T_CELL_MEDIATED_IMMUNITY | GO_REGULATION_OF_THYMOCYTE_APOPTOTIC_PROCESS | |
| VALK_AML_WITH_EVI1 | GO_POSITIVE_REGULATION_OF_THYMOCYTE_AGGREGATION | GO_RESPONSE_TO_SALT | |
| VANLOO_SP3_TARGETS_DN | GO_PROSTANOID_BIOSYNTHETIC_PROCESS | GO_RETINAL_BINDING | |
| WAMUNYOKOLI_OVARIAN_CANCER_LMP_UP | GO_PROSTANOID_METABOLIC_PROCESS | GO_SKELETAL_MUSCLE_CONTRACTION | |
| WANG_BARRETTS_ESOPHAGUS_AND_ESOPHAGUS_CANCER_UP | GO_PROTEIN_C_TERMINUS_BINDING | GO_SULFATION | |
| WEBER_METHYLATED_HCP_IN_SPERM_DN | GO_PROTEIN_DESTABILIZATION | GO_SUMO_TRANSFERASE_ACTIVITY | |
| YAO_TEMPORAL_RESPONSE_TO_PROGESTERONE_CLUSTER_10 | GO_PYRIMIDINE_CONTAINING_COMPOUND_SALVAGE | GO_SUPEROXIDE_METABOLIC_PROCESS | |
| YAO_TEMPORAL_RESPONSE_TO_PROGESTERONE_CLUSTER_5 | GO_REGULATION_OF_ACTIVATED_T_CELL_PROLIFERATION | GO_THYMIC_T_CELL_SELECTION | |
| YAO_TEMPORAL_RESPONSE_TO_PROGESTERONE_CLUSTER_9 | GO_REGULATION_OF_ANTIGEN_PROCESSING_AND_PRESENTATION | GO_THYMOCYTE_AGGREGATION | |
| GO_REGULATION_OF_B_CELL_PROLIFERATION | GO_TRANSCRIPTIONAL_REPRESSOR_ACTIVITY_RNA_POLYMERASE_II_CORE_PROMOTER_PROXIMAL_REGION_SEQUENCE_SPECIFIC_BINDING | ||
| GO_REGULATION_OF_B_CELL_RECEPTOR_SIGNALING_PATHWAY | GO_XENOPHAGY | ||
| GO_REGULATION_OF_BONE_DEVELOPMENT | HANSON_HRAS_SIGNALING_VIA_NFKB | ||
| GO_REGULATION_OF_BONE_REMODELING | HERNANDEZ_MITOTIC_ARREST_BY_DOCETAXEL_2_UP | ||
| GO_REGULATION_OF_BONE_RESORPTION | HOFMANN_MYELODYSPLASTIC_SYNDROM_HIGH_RISK_DN | ||
| GO_REGULATION_OF_ERYTHROCYTE_DIFFERENTIATION | HOFMANN_MYELODYSPLASTIC_SYNDROM_RISK_DN | ||
| GO_REGULATION_OF_FEVER_GENERATION | HOLLEMAN_DAUNORUBICIN_B_ALL_DN | ||
| GO_REGULATION_OF_INTERFERON_ALPHA_PRODUCTION | HOLLEMAN_VINCRISTINE_RESISTANCE_ALL_DN | ||
| GO_REGULATION_OF_INTERFERON_BETA_PRODUCTION | HUMMERICH_BENIGN_SKIN_TUMOR_DN | ||
| GO_REGULATION_OF_LYASE_ACTIVITY | HUMMERICH_MALIGNANT_SKIN_TUMOR_DN | ||
| GO_REGULATION_OF_LYMPHOCYTE_CHEMOTAXIS | IYENGAR_RESPONSE_TO_ADIPOCYTE_FACTORS | ||
| GO_REGULATION_OF_MEMBRANE_INVAGINATION | KAYO_CALORIE_RESTRICTION_MUSCLE_UP | ||
| GO_REGULATION_OF_MRNA_CATABOLIC_PROCESS | KEGG_AMYOTROPHIC_LATERAL_SCLEROSIS_ALS | ||
| GO_REGULATION_OF_NITRIC_OXIDE_SYNTHASE_BIOSYNTHETIC_PROCESS | KORKOLA_CHORIOCARCINOMA_DN | ||
| GO_REGULATION_OF_PROTEIN_TYROSINE_KINASE_ACTIVITY | KRIEG_KDM3A_TARGETS_NOT_HYPOXIA | ||
| GO_REGULATION_OF_T_CELL_APOPTOTIC_PROCESS | KUROKAWA_LIVER_CANCER_CHEMOTHERAPY_UP | ||
| GO_REGULATION_OF_T_CELL_CHEMOTAXIS | LU_TUMOR_ENDOTHELIAL_MARKERS_UP | ||
| GO_REGULATION_OF_T_CELL_MEDIATED_IMMUNITY | LU_TUMOR_VASCULATURE_UP | ||
| GO_REGULATION_OF_T_CELL_MIGRATION | MA_MYELOID_DIFFERENTIATION_UP | ||
| GO_REGULATION_OF_TOLL_LIKE_RECEPTOR_SIGNALING_PATHWAY | MATZUK_MALE_REPRODUCTION_SERTOLI | ||
| GO_REGULATION_OF_TRANSCRIPTION_INITIATION_FROM_RNA_POLYMERASE_II_PROMOTER | MATZUK_OVULATION | ||
| GO_REGULATION_OF_TYPE_I_INTERFERON_MEDIATED_SIGNALING_PATHWAY | MEISSNER_NPC_ICP_WITH_H3K4ME3 | ||
| GO_REGULATION_OF_TYPE_I_INTERFERON_PRODUCTION | MMS_MOUSE_LYMPH_HIGH_4HRS_UP | ||
| GO_RESPONSE_TO_ACIDIC_PH | MOSERLE_IFNA_RESPONSE | ||
| GO_RESPONSE_TO_EXOGENOUS_DSRNA | NAKAMURA_LUNG_CANCER_DIFFERENTIATION_MARKERS | ||
| GO_RESPONSE_TO_MURAMYL_DIPEPTIDE | NIKOLSKY_BREAST_CANCER_1Q21_AMPLICON | ||
| GO_RESPONSE_TO_PLATELET_DERIVED_GROWTH_FACTOR | PID_LPA4_PATHWAY | ||
| GO_RESPONSE_TO_VIRUS | PID_PI3KCI_PATHWAY | ||
| GO_RETINAL_BINDING | RADAEVA_RESPONSE_TO_IFNA1_UP | ||
| GO_RETINOL_BINDING | REACTOME_ADENYLATE_CYCLASE_ACTIVATING_PATHWAY | ||
| GO_RNA_DESTABILIZATION | REACTOME_ADENYLATE_CYCLASE_INHIBITORY_PATHWAY | ||
| GO_SUMO_TRANSFERASE_ACTIVITY | REACTOME_DSCAM_INTERACTIONS | ||
| GO_THYMOCYTE_AGGREGATION | REACTOME_G_ALPHA_Z_SIGNALLING_EVENTS | ||
| GO_THYROID_HORMONE_RECEPTOR_BINDING | REACTOME_INTRINSIC_PATHWAY_FOR_APOPTOSIS | ||
| GO_TOLL_LIKE_RECEPTOR_4_SIGNALING_PATHWAY | REACTOME_PLATELET_ADHESION_TO_EXPOSED_COLLAGEN | ||
| GO_TRANSCRIPTION_FACTOR_ACTIVITY_RNA_POLYMERASE_II_CORE_PROMOTER_SEQUENCE_SPECIFIC | REACTOME_PROSTACYCLIN_SIGNALLING_THROUGH_PROSTACYCLIN_RECEPTOR | ||
| GO_TUMOR_NECROSIS_FACTOR_RECEPTOR_BINDING | REACTOME_REGULATION_OF_KIT_SIGNALING | ||
| GO_TUMOR_NECROSIS_FACTOR_RECEPTOR_SUPERFAMILY_BINDING | REACTOME_RIP_MEDIATED_NFKB_ACTIVATION_VIA_DAI | ||
| GRANDVAUX_IFN_RESPONSE_NOT_VIA_IRF3 | REACTOME_TAK1_ACTIVATES_NFKB_BY_PHOSPHORYLATION_AND_ACTIVATION_OF_IKKS_COMPLEX | ||
| HALLMARK_INTERFERON_ALPHA_RESPONSE | REACTOME_TRAF6_MEDIATED_NFKB_ACTIVATION | ||
| HALLMARK_INTERFERON_GAMMA_RESPONSE | RICKMAN_HEAD_AND_NECK_CANCER_C | ||
| HANSON_HRAS_SIGNALING_VIA_NFKB | RODRIGUES_THYROID_CARCINOMA_UP | ||
| HOFMANN_MYELODYSPLASTIC_SYNDROM_HIGH_RISK_DN | SCHEIDEREIT_IKK_TARGETS | ||
| HOFMANN_MYELODYSPLASTIC_SYNDROM_RISK_DN | SCHLESINGER_METHYLATED_IN_COLON_CANCER | ||
| HOLLEMAN_ASPARAGINASE_RESISTANCE_B_ALL_DN | SHIN_B_CELL_LYMPHOMA_CLUSTER_2 | ||
| IYENGAR_RESPONSE_TO_ADIPOCYTE_FACTORS | SIG_CD40PATHWAYMAP | ||
| KEGG_GLYCOSAMINOGLYCAN_BIOSYNTHESIS_CHONDROITIN_SULFATE | SPIELMAN_LYMPHOBLAST_EUROPEAN_VS_ASIAN_2FC_DN | ||
| KORKOLA_CHORIOCARCINOMA_DN | ST_B_CELL_ANTIGEN_RECEPTOR | ||
| KRIEG_KDM3A_TARGETS_NOT_HYPOXIA | ST_T_CELL_SIGNAL_TRANSDUCTION | ||
| KUROKAWA_LIVER_CANCER_CHEMOTHERAPY_UP | XU_CREBBP_TARGETS_DN | ||
| KYNG_WERNER_SYNDROM_UP | ZEMBUTSU_SENSITIVITY_TO_MITOMYCIN | ||
| LEE_CALORIE_RESTRICTION_MUSCLE_DN | ZHAN_LATE_DIFFERENTIATION_GENES_DN | ||
| LU_TUMOR_ENDOTHELIAL_MARKERS_UP | ZHOU_INFLAMMATORY_RESPONSE_FIMA_DN | ||
| LU_TUMOR_VASCULATURE_UP | |||
| MA_MYELOID_DIFFERENTIATION_UP | |||
| MAHADEVAN_RESPONSE_TO_MP470_UP | |||
| MARIADASON_RESPONSE_TO_CURCUMIN_SULINDAC_7 | |||
| MATZUK_MALE_REPRODUCTION_SERTOLI | |||
| MATZUK_OVULATION | |||
| MOSERLE_IFNA_RESPONSE | |||
| MULLIGHAN_MLL_SIGNATURE_2_UP | |||
| NAKAMURA_ADIPOGENESIS_EARLY_UP | |||
| OUELLET_OVARIAN_CANCER_INVASIVE_VS_LMP_DN | |||
| PARK_TRETINOIN_RESPONSE | |||
| PID_EPO_PATHWAY | |||
| PID_LPA4_PATHWAY | |||
| PID_PI3KCI_PATHWAY | |||
| PID_S1P_S1P3_PATHWAY | |||
| PID_WNT_NONCANONICAL_PATHWAY | |||
| RADAEVA_RESPONSE_TO_IFNA1_UP | |||
| RASHI_RESPONSE_TO_IONIZING_RADIATION_4 | |||
| RAY_TUMORIGENESIS_BY_ERBB2_CDC25A_UP | |||
| REACTOME_ACTIVATION_OF_IRF3_IRF7_MEDIATED_BY_TBK1_IKK_EPSILON | |||
| REACTOME_ADENYLATE_CYCLASE_ACTIVATING_PATHWAY | |||
| REACTOME_ADENYLATE_CYCLASE_INHIBITORY_PATHWAY | |||
| REACTOME_APOPTOSIS | |||
| REACTOME_APOPTOTIC_EXECUTION_PHASE | |||
| REACTOME_DSCAM_INTERACTIONS | |||
| REACTOME_EARLY_PHASE_OF_HIV_LIFE_CYCLE | |||
| REACTOME_IL_2_SIGNALING | |||
| REACTOME_IL_3_5_AND_GM_CSF_SIGNALING | |||
| REACTOME_IL_RECEPTOR_SHC_SIGNALING | |||
| REACTOME_PD1_SIGNALING | |||
| REACTOME_PHOSPHORYLATION_OF_CD3_AND_TCR_ZETA_CHAINS | |||
| REACTOME_REGULATION_OF_KIT_SIGNALING | |||
| REACTOME_RIP_MEDIATED_NFKB_ACTIVATION_VIA_DAI | |||
| REACTOME_TAK1_ACTIVATES_NFKB_BY_PHOSPHORYLATION_AND_ACTIVATION_OF_IKKS_COMPLEX | |||
| REACTOME_TRAF6_MEDIATED_INDUCTION_OF_TAK1_COMPLEX | |||
| REACTOME_TRAF6_MEDIATED_NFKB_ACTIVATION | |||
| REACTOME_TRAFFICKING_AND_PROCESSING_OF_ENDOSOMAL_TLR | |||
| RODRIGUES_THYROID_CARCINOMA_UP | |||
| ROSS_AML_WITH_CBFB_MYH11_FUSION | |||
| SANA_RESPONSE_TO_IFNG_UP | |||
| SCHEIDEREIT_IKK_TARGETS | |||
| SIG_PIP3_SIGNALING_IN_CARDIAC_MYOCTES | |||
| ST_B_CELL_ANTIGEN_RECEPTOR | |||
| ST_T_CELL_SIGNAL_TRANSDUCTION | |||
| ST_TUMOR_NECROSIS_FACTOR_PATHWAY | |||
| TONKS_TARGETS_OF_RUNX1_RUNX1T1_FUSION_ERYTHROCYTE_DN | |||
| TURASHVILI_BREAST_NORMAL_DUCTAL_VS_LOBULAR_UP | |||
| WU_HBX_TARGETS_3_UP | |||
| WUNDER_INFLAMMATORY_RESPONSE_AND_CHOLESTEROL_UP | |||
| XU_AKT1_TARGETS_6HR | |||
| XU_CREBBP_TARGETS_DN | |||
| YANG_BCL3_TARGETS_UP | |||
| ZEMBUTSU_SENSITIVITY_TO_NIMUSTINE | |||
| ZHAN_LATE_DIFFERENTIATION_GENES_DN | |||
| ZHAN_MULTIPLE_MYELOMA_HP_UP | |||
| ZHONG_SECRETOME_OF_LUNG_CANCER_AND_MACROPHAGE | |||
| ZHOU_INFLAMMATORY_RESPONSE_FIMA_DN | |||
Together these data reveal that although the G3TM PKD model was derived from different genetic aberrations to classical PKD models, they share common pathways in regulating complement activation, lipid metabolism, cell-to-cell adhesion signaling etc. These pathways might play an essential role in PKD development.
Furthermore, we found that from G1DM to G3TM, along with the introduction of p53S mutation and telomere shortening, the expression levels of PKD1 and PKD2 decreased significantly (Figure 3C), suggesting that p53S mutation could downregulate PKD1 and PKD2 expression. In the end-stage tumor and cystic kidney tissues, the PKD2 level was slightly upregulated, but was still lower than the level in G3DM (Figure 3C).
Since G3TM is the genotype with most incidences of tumor and cystic kidney disease, but not G3DM, comparison of gene regulation in G3TM with G3DM might provide the mechanisms for PKD attributed to p53S. We evaluated the genes essential for classical PKD development1,21, and mapped their interaction networks with IPA (Figure 3D). Based on expression fold-changes of genes in this interaction network, the molecule activity predictor showed that cystic kidney module was significantly activated (P-value: 3.31E-11). Other than PKD1 and PKD2, the ARPKD protein Pkhd1 (polyductin) and its transcriptional factor Hnf1b (hepatocyte nuclear factor 1 homeobox B)23 were also downregulated. These data suggest that p53S plays a role in transcriptional regulation of PKD-related genes.
To validate the key genes in altered pathways as revealed by RNA-seq data, we further analyzed the regulation of genes involved in the PKD pathway, complement pathway, mitochondria pathway, Wnt signaling pathway, and lipid metabolism pathway by quantitative real-time PCR. Compared with WT and G3DM MEFs, the expression of PKD genes PKD1, PKD2, Pkhd1, and Hnf1b was suppressed in G3TM MEFs. However, complement pathway genes C2 and C5; mitochondria pathway genes Pgc1a and Tfam; Wnt signaling pathway genes Wnt1 and Ctnnb1; and lipid metabolism pathway genes Srebf1 and Srebf2 were upregulated in G3TM MEFs (Figure 3E). These data further confirmed the RNA-seq data, and suggest that p53S regulates genes involved in the aforementioned pathways attributed to the development of cystic kidney.
Discussion
It has always been suspected that the development of cystic kidney disease shares features with tumorigenesis, although the evidence is unclear24,25. Recent understanding of aberrant downstream pathways in ADPKD demonstrates that transcriptional functions that regulate cell cycle progression, energy metabolism, and secretion-related signaling are abnormal in PKD1, and p53 is the essential node in all these transcriptional regulations26.
It has always been documented that wild type p53 could bind to the PKD1 promoter, and the kidneys of p53 null mice expressed higher PKD1 mRNA levels than wild-type littermates, suggesting that wild type p53 suppressed the expression of PKD14. It has also been shown that depletion of PKD1 led to increased cell proliferation and caused a premature G1/S transition, and the elevated expression of mechanosensory polycystins in human carotid atherosclerotic plaques was associated with p53 activation6,27. Thus, it is conceivable that mutant p53, which loses the wild type function of p53 and gains oncogenic function, plays an important role in the development of PKD.
Here we revealed a novel PKD and tumor combined mouse model (PKD derived from G3mTR-/-WRN-/-p53S/S mice) (Figure 1 and 2). The co-occurrence of cystic kidneys and tumors suggests common genetic mechanisms, which in this case could be DNA damage caused by telomere dysfunction and the abnormal DNA damage response, cellular proliferation, or metabolic dysregulation caused by p53N236S mutation. This model provides direct evidence to connect mutant p53 DNA damage response with PKD development. The fact that the incidences of cystic kidneys increased along with telomere shortening suggests that DNA damage triggered the development of PKD.
To dissect the common genetic causes of PKD and tumorigenesis, we identified the upregulated pathways in tumors and cystic kidneys. Among the common pathways in cystic kidneys and tumors, the pathways of activation of complement, inflammatory response, and mitochondrial function were most significantly upregulated (Figure 3B and 3E, Supplementary Figure S1). It has been documented that activation of the alternative complement pathway and the consequent inflammatory response plays an essential role in the progress of kidney diseases, such as atypical hemolytic uremic syndrome, C3 glomerulopathies, and atypical post infectious GN, as well as ADPKD28,29. These data suggest the importance of complement cascade in the regulation of inflammatory response of both cystic kidney disease and tumors.
Mitochondrial function is essential in energy metabolism, oxygen consumption, ROS regulation, and ATP synthesis. Aside from kidney disease, mitochondrial dysfunction is also related to the processes of aging and tumor development 30,31. By ssGSEA analysis, we found that the pathways involved in mitochondrial function and related fatty acid metabolisms are highly activated in tumors and cystic kidneys from G3TM mice; however, they are not significantly up-regulated in PKD1- or PKD2-deficient PKD22(Supplementary Table S1, S2).
It is very promising that we found that PKD1, PKD2, Pkhd1, and Hnf1b were all downregulated by the introduction of p53S (Figure 3D). It has been documented that Hnf1b is the transcription factor for both Pkhd1 and PKD2. Mutation of Hnf1b results in kidney phenotypes that include renal agenesis, dysplasia, and cysts32. These phenotypes are consistent with our pathological analysis (Figure 2).
Putting these data together, we report a novel PKD and tumor combined mouse model, and reveal the gene signatures involved in the development of PKD. The G3TM PKD model shared common pathways with classical PKD. These common pathways might be essential in PKD progress, and thus could be common targets for PKD prevention, drug screening, and patient care strategies. In depth analyses of these pathways could provide new biomarkers for the clinical diagnosis and prognosis of PKD (Figure 4).
4.
A schematic of the establishment of G3TM PKD model, and the gene signatures shared between development of PKD and tumorigenesis, and with PKD1/2 PKD model.
Acknowledgements
This work was supported by National Natural Science Foundation of China (NSFC) (Grant No. 30771194 and 31170735). We thank Dr. Sandy Chang from Yale University and Dr. Ronald A Depinho from The University of Texas MD Anderson Cancer Center for kindly providing WS mice.
Conflict of interest statement
No potential conflicts of interest are disclosed.
S2.
A heatmap of gene expression profiles (ssGSEA analysis results of the RNA-seq data using Hallmark, C2, and C5 datasets) in MEFs from G1DM, G2DM, G3DM, G1TM, G2TM, and G3TM mice, as well as tumors and cystic kidneys from G3TM mice. The pathways were ranked by scores showing the downregulation in the cystic kidney, as well as in tumor and in G3TM MEFs.
Contributor Information
Julun Yang, Email: yingluo@kmust.edu.cn.
Ying Luo, Email: yangjulun@sina.com.
References
- 1.Harris PC, Torres VE Genetic mechanisms and signaling pathways in autosomal dominant polycystic kidney disease. J Clin Invest. 2014;124:2315–24. doi: 10.1172/JCI72272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mangolini A, de Stephanis L, Aguiari G Role of calcium in polycystic kidney disease: From signaling to pathology. World J Nephrol. 2016;5:76–83. doi: 10.5527/wjn.v5.i1.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nishio S, Hatano M, Nagata M, Horie S, Koike T, Tokuhisa T, et al Pkd1 regulates immortalized proliferation of renal tubular epithelial cells through p53 induction and JNK activation. J Clin Invest. 2005;115:910–8. doi: 10.1172/JCI22850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Van Bodegom D, Saifudeen Z, Dipp S, Puri S, Magenheimer BS, Calvet JP, et al The polycystic kidney disease-1 gene is a target for p53-mediated transcriptional repression. J Biol Chem. 2006;281:31234–44. doi: 10.1074/jbc.M606510200. [DOI] [PubMed] [Google Scholar]
- 5.Islam MR, Jimenez T, Pelham C, Rodova M, Puri S, Magenheimer BS, et al MAP/ERK kinase kinase 1(MEKK1) mediates transcriptional repression by interacting with polycystic kidney disease-1(PKD1) promoter-bound p53 tumor suppressor protein. J Biol Chem. 2010;285:38818–31. doi: 10.1074/jbc.M110.145284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Varela A, Piperi C, Sigala F, Agrogiannis G, Davos CH, Andri MA, et al Elevated expression of mechanosensory polycystins in human carotid atherosclerotic plaques: Association with p53 activation and disease severity. Sci Rep. 2015;5:13461. doi: 10.1038/srep13461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li X, Miao X, Wang HS, Xu ZX, Li B The tissue dependent interactions between p53 and Bcl-2 in vivo. Oncotarget. 2015;6:35699–709. doi: 10.18632/oncotarget.5372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Veis DJ, Sorenson CM, Shutter JR, Korsmeyer SJ Bcl-2-deficient mice demonstrate fulminant lymphoid apoptosis, polycystic kidneys, and hypopigmented hair. Cell. 1993;75:229–40. doi: 10.1016/0092-8674(93)80065-M. [DOI] [PubMed] [Google Scholar]
- 9.Kim MP, Lozano G Mutant p53 partners in crime. Cell Death Differ. 2018;25:161–8. doi: 10.1038/cdd.2017.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chu WK, Hickson ID Recq helicases: Multifunctional genome caretakers. Nat Rev Cancer. 2009;9:644–54. doi: 10.1038/nrc2682. [DOI] [PubMed] [Google Scholar]
- 11.Ozgenc A, Loeb LA Werner syndrome, aging and cancer. Genome Dyn. 2006;1:206–17. doi: 10.1159/000092509. [DOI] [PubMed] [Google Scholar]
- 12.Crabbe L, Verdun RE, Haggblom CI, Karlseder J Defective telomere lagging strand synthesis in cells lacking wrn helicase activity. Science. 2004;306:1951–3. doi: 10.1126/science.1103619. [DOI] [PubMed] [Google Scholar]
- 13.Palm W, de Lange T How shelterin protects mammalian telomeres. Annu Rev Genet. 2008;42:301–34. doi: 10.1146/annurev.genet.41.110306.130350. [DOI] [PubMed] [Google Scholar]
- 14.Lebel M, Leder P A deletion within the murine werner syndrome helicase induces sensitivity to inhibitors of topoisomerase and loss of cellular proliferative capacity. Proc Natl Acad Sci USA. 1998;95:13097–102. doi: 10.1073/pnas.95.22.13097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chang S, Multani AS, Cabrera NG, Naylor ML, Laud P, Lombard D, et al Essential role of limiting telomeres in the pathogenesis of werner syndrome. Nat Genet. 2004;36:877–82. doi: 10.1038/ng1389. [DOI] [PubMed] [Google Scholar]
- 16.Du XB, Shen J, Kugan N, Furth EE, Lombard DB, Cheung C, et al Telomere shortening exposes functions for the mouse werner and bloom syndrome genes. Mol Cell Biol. 2004;24:8437–46. doi: 10.1128/MCB.24.19.8437-8446.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhao LJ, Wang BY, Zhao XL, Wu XM, Zhang QS, Wei CY, et al Gain of function in the mouse model of a recurrent mutation p53N236S promotes the formation of double minute chromosomes and the oncogenic potential of p19ARF. Mol Carcinog. 2018;57:147–58. doi: 10.1002/mc.v57.2. [DOI] [PubMed] [Google Scholar]
- 18.Chen X, Chang JT Planning bioinformatics workflows using an expert system. Bioinformatics. 2017;33:1210–5. doi: 10.1093/bioinformatics/btw817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Subramanian A, Tamayo P, Mootha VK, Mukherjee S, Ebert BL, Gillette MA, et al Gene set enrichment analysis: A knowledge-based approach for interpreting genome-wide expression profiles. Proc Natl Acad Sci USA. 2005;102:15545–50. doi: 10.1073/pnas.0506580102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liberzon A, Subramanian A, Pinchback R, Thorvaldsdottir H, Tamayo P, Mesirov JP Molecular signatures database (MSigDB) 3.0. Bioinformatics. 2011;27:1739–40. doi: 10.1093/bioinformatics/btr260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ong ACM, Harris PC A polycystin-centric view of cyst formation and disease: The polycystins revisited. Kidney Int. 2015;88:699–710. doi: 10.1038/ki.2015.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Woo YM, Kim DY, Koo NJ, Kim YM, Lee S, Ko JY, et al Profiling of miRNAs and target genes related to cystogenesis in ADPKD mouse models. Sci Rep. 2017;7:14151. doi: 10.1038/s41598-017-14083-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gresh L, Fischer E, Reimann A, Tanguy M, Garbay S, Shao XL, et al A transcriptional network in polycystic kidney disease. EMBO J. 2004;23:1657–68. doi: 10.1038/sj.emboj.7600160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kovács J, Gomba S, Zilahy M Comparison of the morphology of renal cysts and cystic renal tumors. Pathol Oncol Res. 1997;3:272–7. doi: 10.1007/BF02904286. [DOI] [PubMed] [Google Scholar]
- 25.Lanoix J, D'Agati V, Szabolcs M, Trudel M Dysregulation of cellular proliferation and apoptosis mediates human autosomal dominant polycystic kidney disease (ADPKD) Oncogene. 1996;13:1153–60. [PubMed] [Google Scholar]
- 26.Kastenhuber ER, Lowe SW Putting p53 in context. Cell. 2017;170:1062–78. doi: 10.1016/j.cell.2017.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kim H, Bae Y, Jeong W, Ahn C, Kang S Depletion of PKD1 by an antisense oligodeoxynucleotide induces premature G1/S-phase transition. Eur J Hum Genet. 2004;12:433–40. doi: 10.1038/sj.ejhg.5201136. [DOI] [PubMed] [Google Scholar]
- 28.De Vriese AS, Sethi S, Van Praet J, Nath KA, Fervenza FC Kidney disease caused by dysregulation of the complement alternative pathway: An etiologic approach. J Am Soc Nephrol. 2015;26:2917–29. doi: 10.1681/ASN.2015020184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Su Z, Wang X, Gao X, Liu Y, Pan C, Hu H, et al Excessive activation of the alternative complement pathway in autosomal dominant polycystic kidney disease. J Intern Med. 2014;276:470–85. doi: 10.1111/joim.2014.276.issue-5. [DOI] [PubMed] [Google Scholar]
- 30.Emma F, Montini G, Parikh SM, Salviati L Mitochondrial dysfunction in inherited renal disease and acute kidney injury. Nat Rev. 2016;12:267–80. doi: 10.1038/nrneph.2015.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bhargava P, Schnellmann RG Mitochondrial energetics in the kidney. Nat Rev. 2017;13:629–46. doi: 10.1038/nrneph.2017.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Faguer S, Chassaing N, Bandin F, Prouheze C, Garnier A, Casemayou A, et al The HNF1B score is a simple tool to select patients for HNF1B gene analysis. Kidney Int. 2014;86:1007–15. doi: 10.1038/ki.2014.202. [DOI] [PubMed] [Google Scholar]