Abstract
Purpose:
Transgender and gender-nonconforming (TGNC) adolescents and young adults experience mental health problems, including anxiety and depression, at an elevated rate as compared to their cisgender counterparts. A growing literature suggests that vulnerability to psychiatric problems in TGNC individuals results from social discrimination and minority stress.
Methods:
The sample consisted of adolescent TGNC patients (N = 109) who completed behavior health screening questionnaires as standard of care at their first clinical visit to an interdisciplinary gender program within a pediatric academic medical center in a metropolitan Midwestern city. Binary logistic regressions were used to assess whether the likelihood that participants met clinical diagnostic criteria for Major Depressive Disorder (MDD) and Generalized Anxiety Disorder (GAD) was predicted by gender identity appearance congruence, proximal forms of minority stress (e.g., negative expectations of the future related to gender identity; internalized transphobia) and community connectedness (i.e., resilience) .
Results:
Overall, 33% (n = 36) of the sample met diagnostic criteria for MDD and 48% (n = 53) met diagnostic criteria for GAD. Those with high levels of internalized transphobia were significantly more likely to meet diagnostic criteria for both MDD and GAD. Those with low levels of gender identity appearance congruence were significantly more likely to meet diagnostic criteria for MDD but not GAD.
Conclusion:
There are several unique factors that may predict mental illness among TGNC youth. Understanding these factors may offer opportunities for targeted clinical and structural interventions.
Keywords: Transgender, Gender-nonconforming, Adolescents, Anxiety, Depression, Minority stress, Health disparity
Transgender and gender-nonconforming (TGNC) youth are individuals whose gender identity or expression does not align with their sex assigned at birth. Research suggests that TGNC individuals experience higher rates of mental illness than cis-gender individuals (individuals whose gender identity aligns with their sex assigned at birth), particularly anxiety and depression [1,2]. For instance, in a sample of youth seeking care at a gender clinic, 35% of individuals exhibited symptoms of depression [3]. Likewise, a study of Dutch TGNC adolescents found that 21% had an anxiety disorder diagnosis [4]. These figures underscore the degree to which TGNC youth are particularly vulnerable when they are compared to national prevalence estimates of the two most commonly diagnosed adolescent mental health problems—Major Depressive Disorder (MDD) (12.5%) and Generalized Anxiety Disorder (GAD) (2.2%) [5,6]. In addition to depression and anxiety, many TGNC youth experience gender dysphoria, the clinically significant distress experienced when one’s physical appearance and/or anatomical sex is incongruent with one’s gender identity. Gender dysphoria, itself, has been hypothesized to be related to the elevated rates of mental illness within the TGNC population [7].
Evidence suggests that a key factor inversely associated with mental health problems in TGNC adults is gender identity appearance congruence (AC) [8], or the self-perceived alignment of one’s gender identity with aspects of physical and/or anatomic appearance. For example, low levels of AC in TGNC adults were associated with higher levels of depression and anxiety symptoms; moreover, higher levels of AC were associated with higher levels of overall life satisfaction [8]. Social gender transition (SGT) is defined as living as one’s affirmed gender, rather than sex assigned at birth, in some or all social contexts. Regarded as a reversible form of transition, components of SGT may include dressing as one’s affirmed gender and changing one’s name, both of which may increase one’s feeling of physical alignment with their affirmed gender. In addition to improving AC, SGT has been hypothesized to attenuate risk for psychological adversity among TGNC youths. Indeed, a study examining social transition among prepubescent TGNC children found that youth who had socially transitioned had rates of depression and anxiety that were comparable to their cisgender counterparts [9].
Cognitive factors, such as negative expectations for the future (NE), are also strongly associated with elevated levels of hopelessness, depression, and anxiety in both TGNC and cisgender individuals [10–12]. TGNC individuals may be particularly vulnerable to internalizing negative thoughts considered “proximal” results of minority stress, a chronic stress response that results in negative physical and mental health in lesbian, gay, bisexual, and transgender (LGBT) individuals through both proximal and “distal” (i.e., sociopolitical) forms of sexual and gender minority-based discrimination [13,14] As suggested by minority stress theory, TGNC and LGB individuals who are exposed to victimization or discrimination (i.e., transphobia and homophobia, respectively) exhibit negative mental health outcomes [15,16]. In some cases, individuals may begin to believe the negative and stigmatizing messages they hear regarding their gender identity or sexuality (i.e., internalized transphobia (IT) and internalized homophobia, respectively), which may also contribute to negative outcomes [13]. Several research studies have suggested that IT is a key factor in the elevated levels of mental illness experienced by TGNC individuals [17,18]. It has been suggested that support, specifically by a community of LGBT peers, may aid in decreasing distress associated with minority stress among TGNC and LGB individuals [14,19,20].
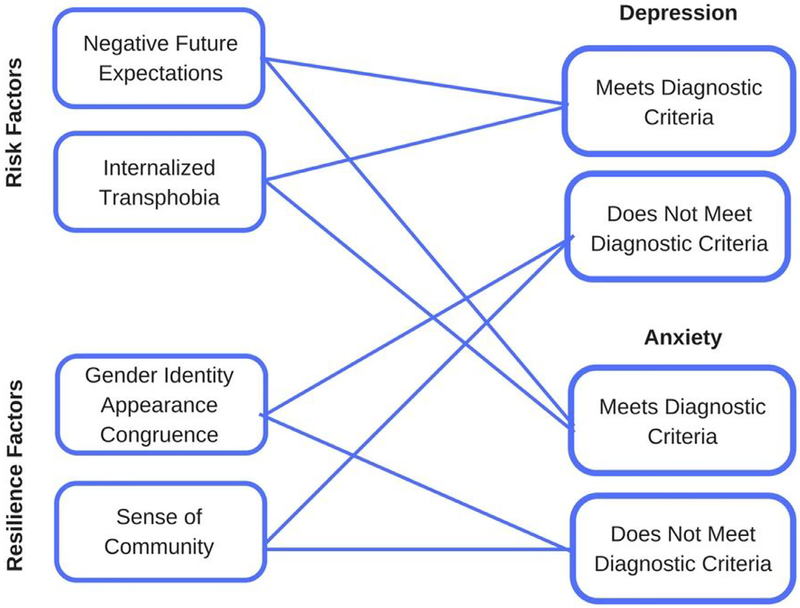
The causes of the significant mental health disparities between TGNC and cisgender adolescents are largely unknown. Much of the mental health research conducted to date on TGNC individuals has relied on pre-pubescent child or adult samples; the results, therefore, may not generalize to the unique experiences of TGNC adolescents. The dearth of research on TGNC youth prompted a recent call [21] and NIH funding opportunity announcement [22] to motivate the investigation of factors associated with health disparities experienced by TGNC individuals, including youth. Toward that aim, this study examined the factors associated with experiences of MDD and GAD among a sample of TGNC youth presenting for care at a large Midwestern gender clinic. A clinically derived sample of youth was utilized in the study due to existing literature examining mental health outcomes among TGNC youth in gender clinics. However, it is important to note that the experiences of TGNC youth receiving care in gender clinic may not be generalizable to the greater population of TGNC youths. There were two primary hypotheses in the study. First, it was hypothesized that higher levels of IT and NE would be associated with meeting diagnostic criteria for both MDD and GAD. The second hypothesis was that at higher levels of AC and TGNC community connectedness, diagnostic criteria for generalized anxiety and depression would not be met. Figure 1 provides an illustration of the model being tested within the present study based upon the adolescent risk and resilience model articulated by Fergus and Zimmerman (see Figure 1) [23].
Figure 1.
Visual depiction of the model tested in the present study
Methods
Participants and recruitment
Study participants were adolescent patients presenting for the initiation of care at a multidisciplinary gender clinic within a large Midwestern academic children’s hospital. Participants were included in the study if they were between 12 and 18 years old and self-identified as TGNC. Data were collected by several self-report psychosocial measures completed as standard of care at the initial clinical visit. All study activities were approved by the institutional review board at the academic children’s hospital as a retrospective chart review of standard of care clinical data.
Measures
Demographic.
Demographic characteristics and social and medical histories were collected through a measure completed by youths’ parents. The demographic characteristics examined in the current study included sex assigned at birth, age, and racial or ethnic identity.
Mental health.
MDD and GAD symptoms were measured using the Youth Inventory (YI-4), a self-report scale employed as an initial screening tool to evaluate DSM-IV criteria for several emotional and behavioral disorders among youth aged 12–18 [24]. Participants reported the frequency of each symptom occurrence on a four-point scale: 0 (never), 1 (sometimes), 2 (often), and 3 (very often). Per the scoring guide, a sum of several endorsed symptoms qualified an individual to meet diagnostic criteria for a specific mental illness. The YI scoring guide also provides tables on which raw scores can be standardized based on normative data segregated by sex assigned at birth; however, this scoring route was not pursued given the lack of professional consensus in mental health assessment regarding the use of sex-normative data in TGNC individuals [25].
Gender identity appearance congruenc.
AC was measured using the nine item AC subscale of the Transgender Congruence Scale (TCS) [8]. The TCS is an empirically-validated measure assessing the degree of comfort TGNC individuals perceive regarding their gender identity and appearance. An example item is “My outward appearance represents my gender identity.” Participants were asked the extent to which they agreed with each item on a 5-point Likert scale: 1 (strongly disagree), 2 (somewhat disagree), 3 (neither agree nor disagree), 4 (somewhat agree), and 5 (strongly agree). Per scoring instructions, a mean AC scale score (ranging from 1 to 5) was calculated, with higher scores indicative of greater AC [8].
Minority stress and resilience.
The Gender Minority Stress and Resilience measure is a validated scale assessing experiences of minority stress among TGNC individuals. The Gender Minority Stress and Resilience contains subscales measuring negative expectations for the future related to gender identity (NE) (sample item: “If I express my gender history, most people would think less of me”), IT (sample item: “My gender identity or expression makes me feel like a freak”), and community connectedness to other TGNC individuals (sample item: “I feel connected to other people who share my gender identity”) [14]. Participants were asked the extent to which they agreed with each item on a 5-point Likert scale: 0 (strongly disagree), 1 (somewhat disagree), 2 (neither agree nor disagree), 3 (somewhat agree), and 4 (strongly agree). Item responses were summed and higher scores indicated higher levels of NE, IT, and community connectedness [14].
Analysis plan
This study employed binary logistic regressions to examine the impact of several demographic and minority stress-related variables (AC, NE, IT, and community connectedness) in predicting dichotomous diagnostic outcomes for MDD and GAD (i.e., meets criteria, does not meet criteria).
Results
Demographics
Table 1 displays the demographic characteristics of the entire sample (N = 109) as well as those who met clinical diagnostic criteria for MDD (n = 36) and GAD (n = 53). The average age for the entire sample was 15.46 years (SD = 1.55), participants were 12–18 years old. Overall, the sample was largely assigned female at birth (71.6%). Further, most the sample identified as transgender (86.2%), with a smaller portion (13.8%) identifying as otherwise gender nonconforming (i.e., gender nonconforming, agender, questioning, nonbinary, and gender queer).With regards to race/ethnicity, 78 (71.6%) were white/European American and 25 (22.9%) were racial or ethnic minority youth (the majority of which identified as Hispanic American).
Table 1.
Demographic characteristics for the full sample
| Total (N = 109) | |
|---|---|
| Age, M (SD) | 15.46 (1.55) |
| Sex assigned at birth, n (%) | |
| Female | 78 (71.6) |
| Male | 31 (28.4) |
| Race/ethnicity, n (%) | |
| White/European-American | 78 (71.6) |
| Black/African-American | 2 (1.8) |
| Hispanic-American | 9 (8.3) |
| Asian-American | 3 (2.8) |
| Other ethnic background | 11 (10.1) |
| Missing | 6 (5.5) |
| Gender identity | |
| Transgender | 94 (86.2) |
| Gender nonconforming | 2 (1.8) |
| Agender | 4 (3.7) |
| Unsure/questioning | 5 (4.6) |
| On-binary | 3 (2.8) |
| Gender queer | 1 (09) |
Binary logistic regressions
Table 2 presents the results of two binary logistic regressions of the effects of AC, NE, IT, and community connectedness on the likelihood that participants meet clinical diagnostic criteria for MDD and GAD. With regard to MDD, the logistic regression model was statistically significant, x2(4) = 25.38, p <. 005, with good model fi per the Hosmer and Lemeshow test. The model explained 29.1% of the variance in MDD and correctly classified 75.0% of cases. As hypothesized, those with higher levels of AC were 2.25 times less likely to meet diagnostic criteria for MDD than those with lower levels of AC. Thus, with each one unit increase in AC, there is 2.25 increased odds of meeting diagnostic criteria. Further-more, those with higher scores of IT were 1.06 times more likely to meet diagnostic criteria for MDD. Higher levels of NE approached significance as a predictor of meeting diagnostic criteria for MDD. With regard to GAD, the logistic regression model was also statistically significant, x2(4) = 11.43, p = .02, with good model fit. The model explained 13.4% of the variance in GAD and correctly classified 64.8% of cases. Also as hypothesized, those with higher levels of IT were 1.06 times more likely to meet diagnostic criteria for GAD.
Table 2.
Odds ratios and 95% confidence intervals for predictors in binary logistic regression model (N = 109)
| Meets diagnostic criteria - depression | Meets diagnostic criteria - anxiety | |||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | |
| Gender identity appearance congruence | .45 | .23–.86 | .01 | 1.00 | .59–1.71 | .99 |
| Negative future expectations | 1.06 | .99–1.13 | .09 | 1.01 | .97–1.09 | .33 |
| Internalized transphobia | 1.06 | 1.00–1.12 | .04 | 1.06 | 1.01–1.11 | .02 |
| Community connectedness | 1.02 | .92–1.13 | .75 | 0.99 | .90–1.09 | .87 |
Discussion
The present study investigated the impact of various minority stress and resilience factors on the likelihood that TGNC adolescents receiving care in a gender clinic meet clinical diagnostic criteria for MDD and GAD—the two most commonly diagnosed psychiatric problems in adolescents. Several factors associated with gender minority stress were significant in predicting the likelihood of MDD and GAD diagnosis among TGNC youth in this sample. The findings suggested that gender identity AC and IT may uniquely predict MDD and GAD symptoms, respectively. For example, youth who perceived their physical appearance to be highly congruent with their gender identity were less likely to meet diagnostic criteria for MDD; however, youth with elevated internalized transphobic beliefs were perhaps particularly vulnerable as they were more likely to meet diagnostic criteria for both MDD and GAD. Neither negative future expectations related to gender identity (NE) nor sense of community connectedness contributed to the likelihood that a TGNC youth would be diagnosed with either MDD or GAD. These findings suggest that there are several factors influencing TGNC youth mental health which may offer opportunities for targeted clinical and structural interventions.
IT, conceptualized as a personal (i.e., “proximal”) manifestation of gender minority stress, is considered to significantly contribute to heightened levels of mental health problems experienced by TGNC populations more broadly [13, 14]. To our knowledge, this is the first study to demonstrate the connection between IT and mental health problems among TGNC youth. This finding is consistent with prior studies that have proposed IT to be a key factor in contributing to mental health problems among TGNC adults [17,18]. The connection between IT and both MDD and GAD diagnoses in the sample suggests that individual and more socioecological interventions aimed at decreasing IT will, in turn, yield more favorable mental health outcomes for TGNC youth receiving care in gender clinics.
On an individual level, clinicians working in traditional psychotherapeutic settings may employ techniques to decrease the negative emotions associated with minority stress among adolescent TGNC patients. Transgender Affirmative Cognitive Therapy, an adaptation of cognitive behavioral therapy, has been proposed as a therapy model uniquely tailored to address the mental health needs of TGNC individuals through contextualizing the mental health problems experienced by the TGNC individuals within the greater stigmatization that the TGNC population faces [26]. Transgender Affirmative Cognitive Therapy specifically targets IT by utilizing cognitive restructuring to challenge negative, transphobic self-beliefs [26].
In tandem to these individual-level interventions, those targeting larger socioecological systems may be implemented to decrease the stigmatization TGNC individuals experience through “distal” forms of minority stress. For example, a study recently identified messages in popular media as being a key contributor to transphobia, suggesting that interventions targeting media outlets may be especially effective [27]. Alternatively, a proposed means of decreasing transphobia has been door-to-door canvassing, which has proven to be effective in at least one study [28]. School-based interventions aimed at diminishing TGNC-based discrimination may be especially effective for TGNC youth. Some schools have elected to adopt comprehensive policies for embracing and protecting TGNC students, which may include the development of a Gay-Straight Alliance/Gender and Sexuality Alliance or policies outlining gender transitioning within the school [29].
Considering youth within the sample who experienced greater gender identity AC were less likely to meet diagnostic criteria for MDD it may be that, for a subgroup of TGNC youth, AC serves a protective role against MDD. For some youth, this alignment may include superficial aspects of appearance (e.g., style of dress, hair style) resulting from reversible gender transition efforts such as SGT. SGT has been proposed as a means of increasing gender identity AC among TGNC youth, as SGT may include changes in gender expression (e.g., name change, gender pronoun change). This finding supports previous research suggesting that SGT may be associated with a decrease in the mental health disparities experienced by TGNC youth [9,30]. For other youth, increasing AC may include changes to anatomical/phenotypical characteristics resulting from gender-affirming medical interventions including pubertal suppression, hormone therapy, or surgery. The findings suggest these forms of transition may also decrease depression among TGNC youth. Gender-affirming medical interventions, such as hormone blockers and gender-affirming hormones, are becoming increasingly common. However, gender-affirming medical interventions are often administered by physicians who specialize in gender development and endocrinologists in specialized gender clinics, usually located in metropolitan areas. Researchers have recently called for increased training of general practitioners in gender-affirming care as a means of increasing widespread accessibility of gender-affirming interventions to TGNC youth [31].
It was surprising that NE were not related to MDD or GAD within this sample, as the relationship between negativistic thinking patterns and mental illness has been well established within the broader adolescent population [10–12]. It should be noted that NE was significantly related to depression in preliminary analyses, when IT and community connectedness were not included in the model. That NE did not remain significant when other factors were included suggests that, at least for TGNC youth in this sample, NE may not be as influential on mental health as are other forms of minority stress. Similarly, unlike previous research findings [14], experiences of community connectedness with other TGNC individuals was not a significant variable in the present study. It is possible that youth in this sample may rely on individuals outside the TGNC community for social support and sense of belonging. Future research investigating broader social support networks of TGNC adolescents may better elucidate the impact of peer support and community connectedness on mental health outcomes.
Limitations
Although findings from the present study were significant, research must continue to examine minority stress factors impacting mental health among TGNC youth. A significant limitation of the present study is that two of the measured used (TCS and Gender Minority Stress and Resilience) have only been validated for individuals over the age of 18. These measures were used to measure AC, IT, NE, and community connectedness because there are no arable measures available that capture these constructs and have been validated for youths under 18. The TCS has also been validated for use among transgender individuals but not gender nonconforming individuals. However, there was variability in gender identity among the participants in the present study. Mental health outcomes may be different among TGNC youth with distinct gender identities, including those who identify along a gender binary (e.g., male and female) versus nonbinary (e.g., agender or genderqueer). Variability in gender diversity was not explored in the present study due to the limited sample size of GNC youth. The present study also utilized a clinically derived sample of mostly European American youth in a metropolitan area, thereby limiting the generalizability of the findings to the greater population of TGNC youth. When possible, future studies should aim to recruit a more diverse, population-based cohort when investigating mental health outcomes among TGNC youth.
IMPLICATIONS AND CONTRIBUTION.
The present study identifies several factors associated with meeting diagnostic criteria for Major Depressive Disorder and Generalized Anxiety Disorder among a clinically derived sample of transgender and gender-non-conforming youth. Further research is necessary to develop targeted clinical and structural interventions focused on the unique needs of the population.
Funding Sources
Funding for the present study was provided by NICHD grant number R01HD082554.
Footnotes
Conflicts of interest: The authors declare that there is no conflict of interest.
References
- [1].Connolly MD, Zervos MJ, Barone CJ, Johnson CC, Joseph CLM. The mental health of transgender youth: Advances in understanding. J Adolesc Health 2016;59:489–95. [DOI] [PubMed] [Google Scholar]
- [2].Reisner SL, Vetters R, Leclerc M, et al. Mental health of transgender youth in care at an adolescent urban community health center: A matched retrospective cohort study. J Adolesc Health 2015;56:274–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Olson J, Schrager SM, Simons LK, Clark LF. Baseline physiologic and psychosocial characteristics of transgender youth seeking care for gender dysphoria. J Adolesc Health 2015;57:374–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].de Vries ALC, Doreleijers TAH, Steensma TD, Cohen-Kettenis PT. Psychiatric comorbidity in gender dysphoric adolescents. J Child Psychol Psychiatry 2011;52:1195–202. [DOI] [PubMed] [Google Scholar]
- [5].Center for Behavioral Health Statistics and Quality Key substance use and mental health indicators in the United States: Results from the 2015 National Survey on Drug Use and Health. Rockville, MD: Substance Abuse and Mental Health Services Administration, 2016. [Google Scholar]
- [6].National Institute of Mental Health. Prevalence of generalized anxiety disorder among adolescents. National Institute of Mental Health, 2017. https://www.nimh.nih.gov/health/statistics/generalized-anxiety-disorder.shtml. [Google Scholar]
- [7].de Vries ALC, Cohen-Kettenis PT. Clinical management of gender dysphoria in children and adolescents: The Dutch approach. J Homosex 2012;59:310–20. [DOI] [PubMed] [Google Scholar]
- [8].Kozee HB, Tylka TL, Bauerband LA. Measuring transgender individuals’ comfort with gender identity and appearance: Development and validation of the transgender congruence scale. Psychol Women Q 2012;36:179–96. [Google Scholar]
- [9].Durwood L, McLaughlin KA, Olson KR. Mental health and self-worth in socially transitioned transgender youth. J Am Acad Child Adolesc Psychiatry 2017;56:116–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Horwitz AG, Berona J, Czyz EK, Yeguez CE, King CA. Positive and negative expectations of hopelessness as longitudinal predictors of depression, suicidal ideation, and suicidal behavior in high-risk adolescents. Suicide Life Threat Behav 2016;47:168–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Kosnes L, Whelan R, O’Donovan A, McHugh LA. Implicit measurement of poisitive and negative future thinking as a predictor of depressive symptoms and hopelessness. Conscious Cogn 2013;22:898–912. [DOI] [PubMed] [Google Scholar]
- [12].MacLeod AK, Byrne A. Anxiety, depression, and the anticipation of future positive and negative experiences. J Abnorm Psychol 1996;105:286–9. [DOI] [PubMed] [Google Scholar]
- [13].Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychol Bull 2003;129:674–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Testa RJ, Habarth J, Peta J, Balsam K, Bockting W. Development of the gender minority stress and resilience measure. Psychol Sex Orient Gend Divers 2015;2:65–77. [Google Scholar]
- [15].Hill DB, Willoughby BL. Development and validation of the genderism and transphobia scale. Sex Roles 2005;53:531–44. [Google Scholar]
- [16].Meyer IH, Dean L. Internalized homophobia, intimacy, and sexual behavior among gay and bisexual men In: Herek GM, ed. Stigma and sexual orientation: Understanding prejudice against lesbians, gay men, and bisexuals, Thousand Oaks, CA: Sage; 1998:160–89. [Google Scholar]
- [17].Bockting W, Miner M, Swinburne R, Hamilton A, Coleman E. Stigma, mental health, and resilience in an online sample of the U.S. transgender population. Am J Public Health 2013;103:943–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Austin A, Goodman R. The impact of social connectedness and internalized transphobic stigma on self-esteem among transgender and gender non-conforming adults. J Homosex 2017;64:825–41. [DOI] [PubMed] [Google Scholar]
- [19].Mizock L, Mueser KT. Employment, mental health, internalized stigma, and coping with transphobia among transgender individuals. Psychol Sex Orientat Gend Divers 2014;1:146–58. [Google Scholar]
- [20].Bry LJ, Mustanski B, Garofalo R, Burns MN. Resilience to discrimination and rejection among young sexual minority males and transgender females: A qualitative study on coping with minority stress. J Homosex 2018;65:1435–56. [DOI] [PubMed] [Google Scholar]
- [21].Olson-Kennedy J, Cohen-Kettenis PT, Kreukels BPC, et al. Research priorities for gender nonconforming/transgender youth: Gender identity development and biopsychosocial outcomes. Curr Opin Endocrinol Diabetes Obes 2016;23:172–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].National Institute of Health. Research on the health of transgender and gender nonconforming populations (R01) [Research project grant]. 2017. https://grants.nih.gov/grants/guide/pa-files/PA-17-478.html
- [23].Fergus S, Zimmerman MA. Adolescent resilience: a framework for understanding healthy development in the face of risk. Annu Rev Public Health 2005;26:399–419. [DOI] [PubMed] [Google Scholar]
- [24].Gadow KD, Sprafkin J. The Youth’s Inventory 4 screening manual. Stony Brook, NY: Checkmate Plus, 2016. http://www.checkmateplus.com/product/yi-4.htm. [Google Scholar]
- [25].Keo-Meier CL, Fizgerald KM. Affirmative psychological testing and neurocognitive assessment with transgender adults. Psychiatr Clin North Am 2017;40:51–64. [DOI] [PubMed] [Google Scholar]
- [26].Austin A, Craig SL. Transgender affirmative cognitive behavioral therapy: Clinical considerations and applications. Prof Psychol Res Pr 2017;46:21–9. [Google Scholar]
- [27].Rood BA, Reisner SL, Puckett JA, Surface FI, Berman AK, Pantalone DW. Internalized transphobia: Exploring perceptions of social messages in transgender and gender-nonconforming adults. Int J Transgend 2017;18:411–26. [Google Scholar]
- [28].Broockman D, Kalla J. Durably reducing transphobia: A field experiment on door-to-door canvassing. Science 2016;352:220–4. [DOI] [PubMed] [Google Scholar]
- [29].McGuire JK, Anderson CR, Toomey RB. Russell ST School climate for transgender youth: A mixed method investigation of student experiences and school responses. J Youth Adolesc 2010;38:1175–88. [DOI] [PubMed] [Google Scholar]
- [30].Olson KR, Durwood L, DeMeules M, McLaughlin KA. Mental health of transgender children who are supported in their identities. Pediatrics 2016;137:e20153223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Deutsch MB. Guidelines for the primary and gender-affirming care of transgender and gender-nonbinary people. 2nd ed San Francisco, CA: Center of Excellence for Transgender Health, 2016. [Google Scholar]